Abstract
Background:
Bursitis is a chronic inflammatory condition characterized by the deposition of cholesterol, macrophage infiltration, and bursal wall calcification. Bursitis is, however, rarely found in the sacrococcygeal region where it may present as a space-occupying mass.
Case Description:
A 64-year-old male with rheumatoid arthritis presented with 3 years’ duration of difficulty sitting and walking due to a soft-tissue mass involving the coccyx region. Once the patient’s MR demonstrated a cystic lesion with erosion of the coccyx, the patient underwent gross total resection of the lesion that proved to be pathologically consistent with bursitis. Postoperatively, the patient’s complaints fully resolved.
Conclusion:
Bursitis may present as a soft-tissue tumor-like lesion in the coccyx that favorably responds to gross total surgical excision.
Keywords: Bursitis, Rheumatoid arthritis, Sacrococcygeal

INTRODUCTION
Bursae are fluid-filled sacs located around joints, and between bone and surrounding soft tissues.[3,9] Degeneration of the muscle, tendons, and skin overlying bony processes may lead to repeated friction and thickening of the bursa’s connective tissue wall.[6] The resulted increased secretion of synovial fluid then contributes to the formation of a bursal cyst, with chronic inflammation leading to bursitis that is pathologically characterized by the deposition of cholesterol, macrophage infiltration, and bursal wall calcification.[6]
Here, we present a 64-year-old male with a history of rheumatoid arthritis (RA) whose low back pain attributed to a large bursal cyst/erosion of the coccyx responded favorably to surgical excision.
CASE REPORT
A 64-year-old male with a history of RA presented with pain attributed to an enlarging coccygeal soft-tissue mass for the past 3 years.
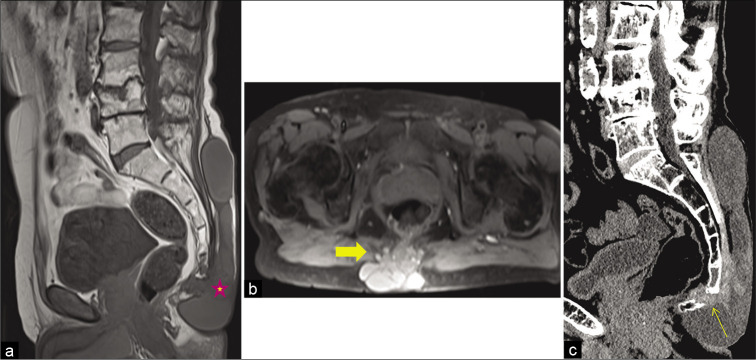
The lesion was soft and mobile, and there were no signs of infection. The magnetic resonance imaging demonstrated a cystic lesion, extending from the coccyx up to the L5 vertebral body. The lesion was hyperintense on T2-weighted images, similar to cerebrospinal fluid but there was no evidence of a connection between the lesion and the subarachnoid space [Figure 1a and b]. The computed tomography (CT) scan further documented focal erosion of the coccyx at the lesion site [Figure 1c].
Figure 1:
Preoperative: (a) sagittal T1-weighted image of the lower lumbar spine, sacrum, and coccyx reveals an extensive, well-circumscribed subcutaneous lesion (star) at the dorsal aspect of the pelvis, which returns homogenous low signal and infiltrates the middle osseous part of the coccyx. (b) Axial T2-weighted image with fat saturation at the level of the coccyx shows the communication of the subcutaneous multiseptated lesion (thick arrow), which returns high signal indicative of fluid and/or proteinaceous material with the destroyed infiltrated central part of the coccyx. (c) Sagittal CT reconstruction of the same ROI shows the different density between the fluid-filled main subcutaneous lesion and the higher, soft-tissue like density of the lesion that causes osteolysis of the coccyx (arrow).
Aspiration
Initially, the patient underwent aspiration of the fluid component of the cyst; it was yellow, thick, and contained amorphous floaters. The culture revealed no microorganisms.
Surgery
The patient underwent gross total resection of the cyst with removal of the coccyx. At surgery, the cyst was whitish-gray in color, multiloculated, adherent to the periosteum of the sacral bone and coccyx, and continuous with the fascia of the paravertebral muscles [Figure 2]. The postoperative CT confirmed adequate lesion removal [Figure 3].
Figure 2:

Intraoperative image showing a multiloculated cyst with secretion of yellowish thick fluid (star) through its wall.
Figure 3:
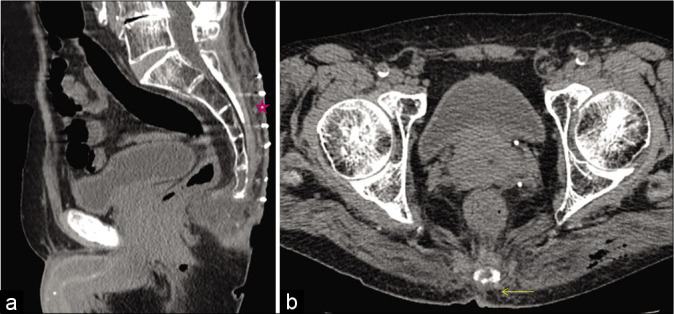
Postoperative: (a) postoperative sagittal CT reconstruction shows complete removal of the subcutaneous tissue (star) and surgical excision of the distal part of the coccyx. (b) The axial CT image shows minor changes at the level of the distal part of the coccyx without evidence of subcutaneous recurrent mass or collection (arrow).
Pathology
The pathological examination showed chronic inflammation and fibrosis consistent with a diagnosis of bursitis. In addition, there was amorphous necrotic material similar to fibrinoid necrosis surrounded by a histiocytic reaction with granulomatous features [Figure 4a and b]. This morphological appearance was similar to rheumatoid nodules, and consistent with the inflammation seen with RA.
Figure 4:
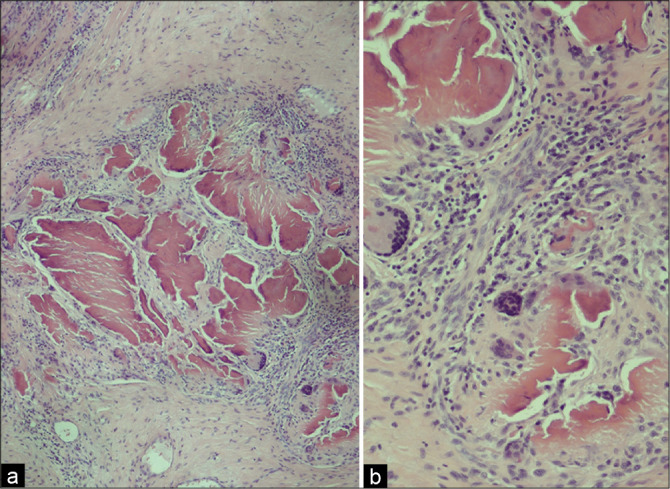
Necrobiotic areas containing amorphous eosinophilic material that is surrounded by inflammatory reaction with prominent macrophages, including multinucleated giant cells: (a) ×40 and (b) ×100.
Postoperatively, the patient recovered uneventfully, and the lesion did not recur over 8 months duration.
DISCUSSION
Bursae are lubricated fluid-filled thin sacs located between bone and surrounding soft tissue, tendons, and muscles around joints. With friction and microtrauma, the inflammatory pathway is activated, and the bursae wall becomes thickened thus resulting in bursitis.[3] Bursitis is thus characterized by a chronic inflammatory reaction resulting in deposition of cholesterol, macrophage infiltration, and bursal wall calcification.[6] The most common causes include trauma, inflammation, infection, and crystal deposition.[3,6,9]
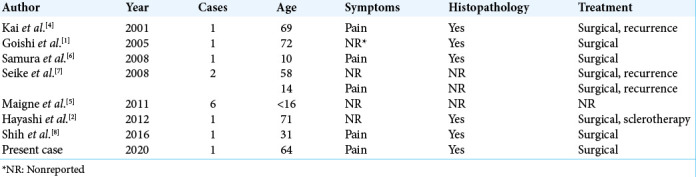
There are very few cases of isolated sacrococcygeal bursitis reported in the literature.[1,4,6-8] Maigne et al. reported six cases of sacrococcygeal bursitis without providing any further details.[5] Hayashi et al. described a 71-year-old patient with RA and multiple rheumatoid bursal cysts who had multiple bursal cysts on his elbow, knee, hand, back, and buttock; the patient was treated with a combination of surgery and sclerotherapy.[2] In our case, the patient additionally had underlying RA [Table 1].
Table 1:
Cases of sacrococcygeal bursitis.
CONCLUSION
In patients with a history of RA, soft-tissue tumor-like lesions over the coccygeal region may represent RA-related bursitis. For these individuals, gross total lesion excision will likely result in symptom resolution.
Footnotes
How to cite this article: Tzerefos C, Koukoulis GK, Vlychou M, Brotis AG, Fountas KN, Paterakis KN. Bursitis of the coccyx in an adult with rheumatoid arthritis mimicking a sacrococcygeal meningocele. Surg Neurol Int 2021;12:220.
Contributor Information
Christos Tzerefos, Email: chris.tzefos@gmail.com.
George K. Koukoulis, Email: geokoukoulis@gmail.com.
Marianna Vlychou, Email: mvlychou@uth.gr.
Alexandros G. Brotis, Email: alexgbrodis@yahoo.com.
Kostas N. Fountas, Email: fountas@uth.gr.
Konstantinos N. Paterakis, Email: kpaterakis@uth.gr.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Goishi K, Yamano M, Hashimoto I, Shikiji T, Nakanishi H. A case of sacrococcygeal bursitis. Jpn J Plast Reconstr Surg. 2005;48:1151–5. [Google Scholar]
- 2.Hayashi A, Matsumura T, Komoto M, Horiguchi M, Komuro Y, Mizuno H. Multiple rheumatoid bursal cysts that were finally effectively treated by combining surgical resection and sclerotherapy. J Plast Reconstr Aesthet Surg. 2012;65:e29–32. doi: 10.1016/j.bjps.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 3.Hirji Z, Hunjun JS, Choudur HN. Imaging of the bursae. J Clin Imaging Sci. 2011;1:22. doi: 10.4103/2156-7514.80374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kai Y, Satoh T, Shibuya H, Terashi H, Fujiwara S, Takayasu S. A case of sacrococcygeal bursitis. Nishinihon J Dermatol. 2001;63:282–5. [Google Scholar]
- 5.Maigne JY, Pigeau I, Aguer N, Doursounian L, Chatellier G. Chronic coccydynia in adolescents. A series of 53 patients. Eur J Phys Rehabil Med. 2011;47:245–51. [PubMed] [Google Scholar]
- 6.Samura K, Morioka T, Hashiguchi K, Yoshida F, Hokama M, Yamaguchi S, et al. Bursal cyst (bursitis) of the coccygeal region clinically mimics sacrococcygeal meningocele. Childs Nerv Syst. 2008;24:533–5. doi: 10.1007/s00381-007-0567-3. [DOI] [PubMed] [Google Scholar]
- 7.Seike T, Matsumoto K, Nakanishi H. Two cases of sacrococcygeal bursitis treated with a gluteal perforator-based flap. Jpn J Plast Surg. 2008;51:87–95. [Google Scholar]
- 8.Shih C, Shu HF, Chen MT. A case of coccygeal bursitis mimicking subcutaneous acute inflammatory lesion. J Cytol Histol. 2016;7:1–2. [Google Scholar]
- 9.Telischak NA, Wu JS, Eisenberg RL. Cysts and cystic-appearing lesions of the knee: A pictorial essay. Indian J Radiol Imaging. 2014;24:182–91. doi: 10.4103/0971-3026.134413. [DOI] [PMC free article] [PubMed] [Google Scholar]