Abstract
While slow processing speed (PS) is well-documented in youth with ADHD, growing evidence suggests that this difficulty affects children with other neuropsychiatric conditions. Clarifying the relationship between slow PS and different forms of psychopathology is important clinically, given the potential impact of PS on academic functioning, and conceptually. In 751 youth, ages 6 to 21, consecutively referred for neuropsychiatric evaluation, we examined the association between slow PS (i.e., Wechsler PS Index < 85) and seven neuropsychiatric diagnostic groups. In 492 of these youth, we also related slow PS to eight psychopathology symptom dimensions. Finally, we modeled the relationship between PS, other cognitive functions and academic achievement. Data are from the Longitudinal Study of Genetic Influences on Cognition. Analyses included one-sample t-tests, ANOVA, logistic regression, mixed modeling, and structural equation modeling (SEM), controlling for age, sex, and medication. Compared to normative data, all clinical groups showed PS decrements. Compared to referred youth without full diagnoses and accounting for other psychopathology, risk for slow PS was elevated in youth with autism spectrum disorder (OR= 1.8), psychotic disorders (OR= 3.4) and ADHD-Inattentive Type (OR= 1.6). Having multiple comorbidities also increased risk for slow PS. Among dimensions, inattention (OR= 1.5) associated with slow PS but did not fully explain the association with autism or psychosis. In SEM, PS had direct effects on academic achievement and indirect effects through working memory. Findings extend evidence that PS relates to multiple aspects of child psychopathology and associates with academic achievement in child psychiatric outpatients.
Keywords: processing speed, cross-disorder, child psychiatry, outpatients, academic achievement, working memory
There is growing evidence that processing speed (PS; i.e., the time it takes for an individual to perceive, process and respond to a stimulus) impacts real-world functioning across the lifespan [1]. While a substantial empirical literature has demonstrated that PS affects activities of daily living among aging adults [2, 3], there is increasing recognition of the importance of PS in children and adolescents [1, 4, 5]. Perhaps most notably, reduced PS in school-aged youth shows a relationship to academic success [6, 7], even beyond general intellectual ability [7].
Because children and adolescents with slow PS may require academic support, it is important to determine the characteristics of those most likely to manifest this neurocognitive weakness. To date, there is strong evidence that PS is commonly reduced in children diagnosed with attention deficit-hyperactivity disorder (ADHD) [8]. Moreover, among youth with this condition, variation in PS associates with academic achievement. For example, a recent review and meta-analysis revealed that PS in children with ADHD was inversely associated with academic abilities, including math, written expression, and reading [9]. Notably, with regard to reading, the correlations between timed versus untimed reading measures and PS did not differ markedly [9], suggesting that the detrimental impact of slow PS extends beyond performance on timed tasks.
To a more limited extent, PS deficits have been documented in other child neuropsychiatric conditions. For example, PS was found to be slower in youth with autism spectrum disorder (ASD) compared to those without ASD (e.g. [10]). In youth with high-functioning ASD, PS was the most impaired domain of the Wechsler intelligence scales and PS weaknesses related more to social communication and adaptive difficulties than did ADHD symptoms [11]. Additionally, PS is commonly impaired among individuals with psychotic disorders [12] and has been related to functional outcomes in patients with schizophrenia [13]. In adolescents with prodromal symptoms versus healthy controls, PS was again among the most impaired cognitive domains [14]. Finally, youth with social-emotional disorders, including major depressive disorder, have been found to show reduced PS [15].
Together, this literature suggests that, like weaknesses in working memory (WM) and other aspects of executive functions [16, 17], slow PS may occur across a range of different psychopathological conditions; however, the available literature is predominantly comprised of individual studies of separate diagnoses. To date, only two studies from the same research group have examined PS deficits across youth with a range of conditions within the same cohort. In the first [18], youth with ADHD (with and without hyperactivity), ASD, bipolar disorder, depression, and learning disorders all manifested lower PS relative to their own general ability. Youth with anxiety, oppositional defiant disorder (ODD) and intellectual disability did not show this discrepancy. In an extension of this work that compared youth with different diagnoses to community controls [19], children with ADHD and ASD showed slower PS, whereas youth with anxiety/ depression and ODD did not.
Notably, in those cross-disorder samples, some of the psychopathology groups were small (e.g. n = 25 with anxiety/depression; n = 19 youth with ODD[19]). Furthermore, analyses did not address the extent to which comorbidity, which is commonly found in outpatients, could have accounted for cross disorder findings. Finally, given the underlying dimensionality of psychopathology [20], it is important to examine whether variation in symptoms could account for neurocognitive impairments emerging across conditions. To date, only a limited number of studies have examined PS in relation to psychopathology symptom dimensions. Such studies have primarily focused on ADHD, e.g. [21, 22], and found PS was related to variation in inattention symptoms.
Determining the extent to which cognitive impairments, such as slow PS, relate to different forms of psychopathology has scientific and practical importance. Relating slow PS to multiple conditions could highlight PS as a target for investigations of cross-disorder risk mechanisms [23]. In the child psychiatry clinic, awareness of the characteristics of outpatients at highest risk for slow PS might prompt earlier identification of this difficulty, which is important given its potential impact on academics. Furthermore, establishing cross-disorder effects provides a rationale for modeling the impact of slow PS on academic difficulties in youth clinical samples broadly in order to identify targets for intervention.
The current paper aimed to advance this literature in a large sample of youth consecutively referred for neuropsychiatric evaluation. First, we examined the relevance of PS to different forms of psychopathology (i.e., categorical diagnostic groupings and dimensional psychopathology symptoms), where possible addressing the potential role of comorbidity/co-occurring symptoms. Second, we modeled the extent to which PS in referred youth generally relates to academic achievement in conjunction with other aspects of cognition known to impact academic functioning (i.e., general ability[24] and WM [25, 26]). Specifically, we aimed to determine the extent to which PS exerts an independent, direct effect on reading and math. We also examined evidence for an indirect effect through WM, which has been shown to mediate the impact of PS on academic outcomes in typically developing youth as well as children with congenital heart disease [27, 28]. Together, these analyses aimed to extend the literature on slow PS as a domain of cognition that is impaired across different forms of child psychopathology and relevant to functional outcome.
Methods
Subjects
Participants were from the Longitudinal Study of Genetic Influences on Cognition (LOGIC). LOGIC recruits youth referred for evaluation at a pediatric assessment clinic within the Psychiatry Department at Massachusetts General Hospital (MGH). Patients with neuropsychiatric symptomatology are referred to this clinic for a comprehensive evaluation to assist with differential diagnosis and/or treatment or educational planning. Patients are approached in the clinic waiting room and receive a gift card if they agree to participate. To enroll, youth must contribute their clinical data and are asked to contribute supplemental assessments to create a uniform battery of measures across participants. They are also asked to provide DNA; however, genomic information was not part of the current analyses. Study procedures were in compliance with the Partners Institutional Review Board. This study has therefore been performed in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its later amendments. Parents and youth 18 and older provide written informed consent after a description of risks and benefits; youth 7–17 provide written assent.
Subjects in the current analysis were consecutively enrolled, unrelated patients ages 6 to 21 with full scale IQ ≥ 70. LOGIC is an ongoing project. At the time of these analyses, there were 751 unrelated youth who met these criteria. Their mean age was 11.5 ± 3.3 years and 280 (37.3%) were female.
Diagnostic Procedures
Data on youth in the current sample were collected prior to the publication of DSM-5 and reflect DSM-IV-TR criteria. Diagnoses were made by licensed clinical psychologists who are MGH/ Harvard Medical School (HMS) faculty or pre- or post-doctoral clinical fellows under their supervision. Our source clinic is a training site for neuropsychiatric assessment for pre- and post-doctoral Clinical Psychology Fellows. Thus, accurate and thorough diagnostic assessment is one of the “deliverables” of the clinic. Diagnostic procedures include: 1) clinical interviews with a parent/ legal guardian and patient which included a review of DSM criteria for suspected and differential diagnoses; 2) review of available medical records and 3) review of omnibus and targeted behavioral rating scales (including the Child Behavior Checklist/6–18 or Adult Behavior Scale, and the Child Symptom Inventory-IV, which includes specific DSM-IV-TR criteria). Diagnoses were made by clinicians if full DSM-IV-TR criteria were met, with two exceptions. First, we allowed for a diagnosis of ADHD in the presence of an ASD diagnosis, in anticipation of DSM-5. Second, conduct disorder (CD) and oppositional defiant disorder (ODD) were not coded in the diagnostic record if they were considered secondary to other issues, including factors not specifically named in DSM-IV. For research purposes, diagnoses of CD and ODD were coded as research diagnoses if patients met diagnostic criteria based on number of parent-reported DSM symptoms in the extended clinical record.
We examined the reliability of the diagnostic process by having four independent licensed clinical psychologists blindly review and rate a subsample of 30 youth per diagnosis. These cases were randomly selected regardless of comorbidity. Following the guidelines of Landis and Koch [29] we interpreted kappa coefficients between .61–.80 as representing a substantial agreement and kappa coefficients between .81–1.00 as indicative of almost perfect agreement. The inter-rater reliability using Cohen’s Kappa was .93 for ADHD, ASD, and mood disorders (95% CI: [.80–1.06]) indicative of almost perfect agreement, and .80 for the presence or absence of psychosis (95% CI: [.59–1.01]), indicative of substantial agreement. Further corroboration of clinician diagnoses of ADHD from our source clinic occurred in twelve youth who were not part of the current study. These outpatients received a semistructured diagnostic interview (Kiddie Schedule for Affective Disorders and Schizophrenia-Epidemiologic Version; KSADS-E) as part of a separate study, which confirmed clinician diagnoses of ADHD in 100% of cases.
Sample Characteristics.
Broad diagnostic groupings, which were used as predictors in different analyses, and rates of comorbid conditions are shown in Table 1. Regarding the overall sample, within the ADHD category, n = 166 (37.5%) had Inattentive Type (ADHD-I), n = 6 (1.4%) had Hyperactive/Impulsive Type, 269 (60.7%) Combined Type (ADHD-C) and n = 2 (0.4%) had missing subtype data. Within the ASD category, n = 13 (1.7%) had autistic disorder, n = 61 (8.1%) had Asperger’s syndrome, and n = 51 (6.8%) had pervasive developmental disorder- not otherwise specified (NOS). Within the mood disorder category, diagnoses included n = 23 (3.1%) bipolar disorder; n = 65 (8.7%) major depressive disorder, n = 7 (0.9%) dysthymic disorder, and n = 72 (9.6%) mood disorder NOS. Regarding anxiety, diagnoses included n = 2 (0.3%) panic disorder, n = 20 (2.7%) obsessive-compulsive disorder, n = 68 (9.1%) generalized anxiety disorder and n = 147 (19.6%) anxiety disorder NOS. Regarding psychosis, diagnoses included 1.1% (n = 8) schizophrenia/ schizoaffective disorder and n = 23 (3.1%) psychotic disorder NOS. Furthermore, n = 8 (1.6%) were diagnosed with a substance abuse disorder (SUD) due to alcohol, marijuana or other substances. Additionally, 15.3% (n = 115) of referred youth did not meet full criteria for any of these diagnoses, despite having neuropsychiatric symptoms. We note that these diagnoses are based on lifetime criteria but that the vast majority are current (e.g. percentage based on meeting current full criteria: psychosis 96.8%, ASD 96.0%, mood disorders 91.0%, ADHD 96.2%, anxiety disorders 96.2%).
Table 1.
Characteristics of cohort
| Characteristics | Total sample (n = 751) | Dimensional analysis (n = 492) |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Age | 11.5 (3.3) | 11.4 (3.2) |
| FSIQ | 99.6 (13.7) | 100.1 (13.8) |
| Frequency | Frequency | |
| Processing speed problems (% <85) | 193 (25.7%) | 137 (27.8%) |
| Sex (% Boys) | 471 (62.7%) | 321 (65.2%) |
| Psychotropic med (% Yes) | 321 (42.7%) | 215 (43.7%) |
| Rates of psychiatric diagnosesa | ||
| Psychosis | 31 (4.1%) | 17 (3.5%) |
| ASD | 125 (16.6%) | 91 (18.5%) |
| Mood disorders | 167 (22.2%) | 112 (22.8%) |
| ADHD | 443 (59.0%) | 290 (58.9%) |
| Anxiety disorders | 237 (31.6%) | 173 (35.2%) |
| Conduct disorder | 130 (17.3%) | 97 (19.7%) |
| Oppositional defiant disorder | 101 (13.4%) | 60 (12.2%) |
| Substance use disorders | 11 (1.5%) | 8 (1.6%) |
| Other b | 115 (15.3%) | 70 (14.2%) |
| Number of diagnoses | ||
| None | 115 (15.3%) | 70 (14.2%) |
| 1 | 265 (35.3%) | 163 (33.1%) |
| 2 | 207 (27.6%) | 141 (28.7%) |
| ≥ 3 | 164 (21.8%) | 118 (24.0%) |
Due to comorbidity, numbers exceed 100%
Other = no full psychiatric diagnosis; may have subclinical symptoms
Other Key Phenotypes
Dimensional Ratings of Psychopathology.
Ratings of dimensional psychopathology symptoms for each youth were obtained from her/his primary caregiver. Ratings were made via measures with acceptable psychometric properties that are widely used in both child clinical and research settings. Here, we selected measures that represented core domains of the psychopathological conditions that comprised our diagnostic groupings. Specifically, we used the Child Symptom Inventory-IV (CSI-IV; [30]) to derive ratings of depression symptoms (Cronbach’s alpha .86), symptoms of inattention and hyperactivity (Cronbach’s alpha .92 and .91) and psychosis (Cronbach’s alpha .68). We used the Child Behavior Checklist (CBCL)/6–18 [31] Aggression and Anxiety Problems scales for ratings of those constructs (Cronbach’s alpha .94 and .72, respectively). We used the Social Communication/Interaction subscale of the Social Responsiveness Scale [32] to represent a core, dimensional component of ASD [33] (Cronbach’s alpha .89). Finally, we used the eight symptoms that reflect criteria for a manic episode from the Child Mania Rating Scale [34] (Cronbach’s alpha .72).
PS and other Wechsler Scores.
We examined index scores based on the Wechsler Intelligence Scale for Children – Fourth Edition [35] for youth 6 to 16 and the Wechsler Adult Intelligence Scale – Fourth Edition [36] for youth 17 to 21. Our primary variable of interest was the PS Index, which is comprised of the Coding and Symbol Search tasks. Of note, these tasks require rapid performance but also accurate performance (points are lost for errors). Additionally, we examined two other major domains of the Wechsler battery for purposes of comparison to the prior literature [18], and because these constructs associate with academic outcome [24–26]. These included the Working Memory Index (WMI) and the General Ability Index (GAI), which estimates cognitive ability without the inclusion of PS and WM tests [37, 38]. Finally, we examined the Word Reading and Numerical Operations subtests of the Wechsler Individual Achievement Test (WIAT)– Third Edition [39], which evaluates academic achievement in reading and math using a generally comparable normative sample.
Psychotropic Medication.
Detailed data (dose, type, onset, offset) regarding use of psychotropic medication was obtained as part of the clinical evaluation. A total of n = 177 (23.6%) children were taking stimulants, n = 83 (11.1%) were on non-stimulant medication to treat ADHD (e.g. atomoxetine), n = 69 (9.2%) were taking an atypical antipsychotic, n = 106 (14.1%) were taking a Selective Serotonin Reuptake Inhibitor (SSRI), n = 35 (4.7%) were taking a non-SSRI antidepressant, n=19 (2.5%) were taking a benzodiazepine, and n = 44 (5.9%) were taking another type of psychotropic medication. Totals exceed 100% because some youth were taking more than one type of medication. Based on this information, we created a binary variable to indicate current use of one or more types of psychotropic medications versus non-use. This variable yielded a total of n = 321 (42.7%) youth using psychotropic medication.
Primary analyses
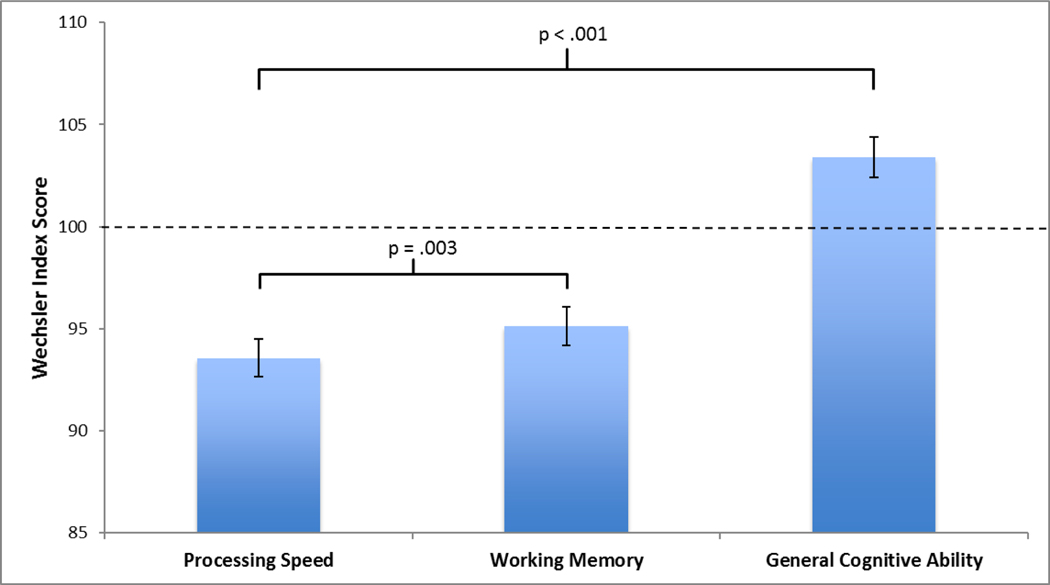
To extend evidence from prior studies, we examined the profile of Wechsler Index scores (PSI, WMI and GAI) within this clinical cohort. We used mixed effects modeling, with a within-subjects factor consisting of PSI, WMI, and GAI where PSI was the reference variable, while controlling for age, sex, and use of psychotropic medication. The Wald χ2 was used to evaluate the main effect for cognitive domain (i.e., do the three domains differ from each other) followed by simple comparisons of PSI with WMI and PSI with GAI in order to assess (relative) weaknesses in this clinical cohort.
Second, we transformed PSI into a dichotomous variable, representing a weakness in PS as a score that was more than one standard deviation below the population mean (i.e., PSI < 85). This variable, representing slow PS, was entered as the dependent variable in a logistic regression analysis with each diagnostic group as an independent variable. Results were intended to show associations between slow PS and specific diagnostic groupings after other conditions were controlled for.
Third, we examined the eight common dimensions of psychopathology symptoms to determine which were predictive of slow PS. These included depression, inattention, hyperactivity, anxiety, aggressive behavior, mania, social communication/interaction, and psychosis. Because of the relatively lower rates of psychosis symptoms in the sample, we examined those symptoms using a categorical variable with 3 levels (0 = no symptoms; 1 = mild symptoms, mean CSI psychosis score ≤ .50; 2 = moderate symptoms, mean CSI psychosis score ≥ .51 and ≤ 3.0). We standardized all dimensional variables (transforming them to z-scores) and used them as predictors of slow PS in a logistic regression, controlling for age, sex and medication. For these dimensional analyses, we only included participants with complete data across every scale, resulting in a subset of 492 youth; however, we also present the results of this analysis using multiple imputation to include youth with missing data.
Lastly, we used structural equation modeling (SEM) to document whether and how PS impacts academic achievement across child psychiatry outpatients broadly. We report a direct effect of PS on Word Reading and Numerical Operations as well as an indirect effect through WM, given prior studies [27, 28]. We examined separate models for our two academic outcomes, controlling for age, sex, and psychotropic medication. To further document the impact of slow PS per se, we also examined the models after controlling for inattention symptoms and GAI given their potential to influence academic functioning. As our goal was to estimate specific (i.e., direct and mediation) effects of PS on academic functioning rather than a global model, no goodness-of-fit statistics were reported [40]. Stata 14 was used for all analyses and findings were considered significant if they exceeded an alpha of .05.
Results
Analysis 1. Wechsler profile in a clinical sample
Mixed modeling analyses yielded a significant main effect for cognitive domain ((2) = 406.84, p < .001), after controlling for age, sex and use of medication. As shown in Figure 1, PS Wald χ2was significantly more impaired than WM (Mdifference = −1.5, p = .003) and general cognitive ability (Mdifference = −9.8, p < .001) among referred youth.
Figure 1.
Performance of youth referred for neuropsychiatric evaluation on Wechsler indices
Analysis 2. Comparison of mean PS Index in different diagnostic groups to normative data
As shown in Table 2, the mean PS score of youth in all of the diagnostic subgroups, as well as in the referred youth with no psychiatric diagnoses, was significantly below the Wechsler normative mean of 100.
Table 2.
One-sample t-tests comparing the mean of each diagnostic group with population mean of 100
| Diagnosis | Mean (SD) | t-value | p-value |
|---|---|---|---|
| No full psychiatric diagnoses | 97.2 (12.9) | 2.34 | .02 |
| Psychosis | 84.5 (13.1) | 6.57 | <.0001 |
| Autism spectrum disorder | 88.7 (15.3) | 8.29 | <.0001 |
| Mood disorders | 90.6 (14.6) | 8.32 | <.0001 |
| ADHD (all) | 92.2 (13.2) | 12.51 | <.0001 |
| ADHD-C | 92.3 (13.5) | 9.29 | <.0001 |
| ADHD-I | 91.7 (12.8) | 8.34 | <.0001 |
| Anxiety disorders | 92.3 (14.4) | 8.22 | <.0001 |
| Conduct disorder | 92.3 (13.8) | 6.40 | <.0001 |
| Oppositional defiant disorder | 94.4 (14.3) | 3.97 | .0001 |
ADHD-C = ADHD combined type; ADHD-I = ADHD inattentive type
Analysis 3. Logistic regression examining odds of slow PS in different diagnostic groups
Table 3 shows the results of the logistic regression in which all diagnostic groups were entered into the model and compared to the referred youth with no diagnoses (“clinic controls”). Thus, significant effects reflected the independent contribution of each diagnosis after accounting for other conditions. Here, the odds of slow PS were significantly higher for children with psychosis and ASD compared to the referred youth with no psychiatric diagnoses. The odds for those with ADHD emerged as a statistical trend (OR 1.42, [95% CI 0.97 – 2.07], p = .07).
Table 3.
Relative risk of slow PS for each psychopathology group, controlling for comorbid disorders, age, sex, and psychotropic medication (n=751)
| Predictors | Odds ratio | z-value | p-value | 95% CI |
|---|---|---|---|---|
| Step 1 | ||||
| Age | 1.05 | 1.69 | .09 | 0.99 – 1.11 |
| Sex | 0.46 | 3.90 | <.001 | 0.31 – 0.68 |
| Psychotropic med usage | 1.30 | 1.33 | .18 | 0.88 – 1.93 |
| Step 2 | ||||
| Psychosis | 3.02 | 2.70 | .007 | 1.35 – 6.73 |
| ASD | 1.85 | 2.77 | .006 | 1.20 – 2.87 |
| Mood disorders | 1.26 | 0.99 | .32 | 0.80 – 1.97 |
| ADHD | 1.42 | 1.79 | .07 | 0.97 – 2.07 |
| Anxiety disorders | 1.38 | 1.66 | .10 | 0.95 – 2.00 |
| Conduct disorder | 1.04 | 0.18 | .86 | 0.65 – 1.67 |
| Oppositional Defiant disorder | 0.86 | 0.56 | .58 | 0.51 – 1.45 |
Note. ASD = Autism Spectrum Disorder; ADHD= Attention Deficit/ Hyperactivity Disorder.
Follow-up analyses:
ADHD subtypes:
Given the strong evidence for an association between ADHD and PS in the literature, we followed up the near significant association with ADHD by re-running the above analysis including ADHD subtypes with adequate frequencies (i.e., ADHD-I and ADHD-C). Here, the ADHD variable included three categories (0 = no ADHD, 1 = ADHD-I and 2 = ADHD-C), with a sample size of n = 743. Similar to the results in Table 3, we found a significant risk for psychosis (OR 3.03, [95% CI 1.36 – 26.75], p = .007) and ASD (OR 1.80, [95% CI 1.16 – 2.79], p = .009), but in this case, youth diagnosed with ADHD-I also showed an elevated risk for slow PS (OR 1.60, [95% CI 1.01 – 2.55], p = .045). The combined subtype of ADHD was not significantly associated with an increased risk for slow PS (OR 1.31, [95% CI 0.85 – 2.03], p = .22) compared to clinic controls.
PSI as a continuous variable:
Given the underlying dimensionality of the PSI, we ran linear regressions using our major diagnostic categories from Table 3 to predict PSI as a continuous variable (shown in Supplementary Table 1). Similar to the dichotomous analyses, we found significant effects for psychosis and ASD; however, in this case, the overall ADHD group also showed a significant association, with a lower PSI score of ~3.6 index points (t = 3.47, p < .001) when accounting for other disorders.
Impact of comorbidity burden:
Although our logistic regression models addressed comorbidity by examining independent effects of different diagnostic groupings after accounting for other conditions, we also examined the impact of having multiple disorders on risk for slow PS. We examined comorbidity as a three-level variable (having 1 condition [no comorbidity], 2 conditions [1 comorbid disorder] or 3 or more conditions [more than 1 comorbid disorder]). After excluding youth with no diagnosis, we first used logistic regression to compare youth with any comorbidity (i.e., youth with 2 or ≥3 conditions) to those without comorbidity (i.e. youth with 1 condition), again controlling for age, sex and use of psychotropic medication. In 636 youth with one, two and three or more conditions (i.e., excluding the clinical controls), the presence of any second diagnosis (i.e., two conditions) over any one condition did not significantly increase the risk for slow PS (OR = 1.19, 95% CI 0.77 – 1.85, p = .42); however, having any 3 or more disorders did increase risk for slow PS (OR = 2.20, 95% CI 1.39 – 3.48, p < .001). Using the same strategy within specific diagnostic groupings yielded similar results. In the 443 children diagnosed with ADHD, having an additional diagnosis did not significantly increase the risk for slow PS (OR = 1.15, 95% CI 0.68 – 1.96, p = .59); however, having two or more additional diagnoses beyond ADHD did (OR = 1.88, 95% CI 1.09 – 3.26, p = .02). A similar pattern emerged for anxiety disorders, with no significant increase in the risk for slow PS when one additional disorder was present (OR = 2.05, 95% CI 0.78 – 5.39, p = .14), but a ~2.7 fold increase when two or more additional diagnoses were (OR = 2.72, 95% CI 1.04 – 7.09, p = .04). No significant effects of number of comorbidities on the risk for low PS were found for ASD in the presence of one (OR = 0.36, 95% CI 0.11 – 1.13, p = .08) or ≥ 2 additional diagnoses (OR = 1.22, 95% CI 0.41 – 3.66, p = .72). We were not able to perform similar analyses for other diagnostic groups because the sample sizes for the non-comorbid subgroups were too small (all n < 14) to function as the reference categories.
Analysis 4. Association between dimensional psychopathology symptoms and slow PS
No significant differences were found between the 492 youth with complete data on dimensional symptom ratings and the remaining 259 youth who had one or more missing scales in terms of the percent with slow PS (χ2(1) = 3.44, p = .06), though there was a statistical trend towards a lower rate of slow PS in youth with missing data. Groups did not differ in terms of current use of psychotropic medication (χ2(1) = .53, p = .47). There was a statistically significant difference in the distribution of sex (χ2(1) = 3.90, p = .05) with relatively fewer girls in the complete data group. No difference for age (t(749) = 1.60, p = .11) was found. Furthermore, no differences between these groups were found on the rates of diagnoses [psychosis; χ2(1) = 1.63, p = .20, ASD; χ2(1) = 3.52, p = .06, mood disorders; (χ2(1) = 0.23, p = .63, ADHD; χ2(1) = 0.00, p = .97), ODD (χ2(1) = 1.93, p = .17], with the exception of anxiety disorders (χ2(1) = 8.58, p = .003), CD (χ2(1) = 5.77, p = .02). There was a larger proportion of participants with an anxiety disorder and CD in the group with complete data; however, the effect sizes were small (Cramer’s V = .08, and Cramer’s V = .10, respectively). Based on these comparisons, we determined that the youth with complete dimensional data were generally representative of the overall sample; however, given minor differences, we also carried out supplemental analysis of the whole group using multiple imputation to handle missing data.
Table 4 provides the correlation matrix for the eight dimensional symptom scales in the 492 youth (descriptive data in Table 1), which indicates small to moderate relationships across constructs. As shown in Table 5, when we related all dimensions to slow PS in a single model, only inattention symptoms showed a significant association. Here, an increase of one SD in inattention symptoms increased the risk of endorsing PS problems 1.4 fold ([95% CI 1.10 – 1.87], p = .007). In addition to this effect, there was a significant effect for sex (OR 0.46, [95% CI 0.29 – 0.74], p =.001), indicating that girls were significantly less at risk for slow PS than boys, as well as an effect for medication use, with children on psychotropic medication being more likely to have slow PS (OR = 2.00, [95% CI 1.26 – 3.19], p = .003).
Table 4.
Mean (SD) and correlations between psychopathology symptom dimensions (n = 492).
| Dimension | Mean (SD) | Aggressive Behavior | Anxiety problems | Social Communication/Interaction | Depression | Inattention | Hyperactivity | Mania symptoms | Psychosis symptoms |
|---|---|---|---|---|---|---|---|---|---|
| T-score | |||||||||
| Aggression | 59.7 (10.0) | - | |||||||
| Anxiety problems | 62.0 (9.3) | .36 | - | ||||||
| SCI | 60.0 (12.3) | .46 | .47 | ||||||
| Raw score | |||||||||
| Depression | 4.2 (4.5) | .29 | .44 | .41 | - | ||||
| Inattention | 14.0 (6.6) | .36 | .24 | .45 | .24 | - | |||
| Hyperactivity | 8.5 (6.9) | .50 | .26 | .41 | −.01ns | .52 | - | ||
| Mania symptoms | 3.1 (3.6) | .45 | .23 | .39 | .09<.05 | .32 | .59 | - | |
| Ordinal variablea | |||||||||
| Psychosisb | (71.3%) | .36 | .36 | .48 | .38 | .20 | .26 | .33 | - |
| 1 (17.7%) | |||||||||
| 2 (11.0%) | |||||||||
Spearman correlations
0 = no psychosis symptoms, 1 = some psychosis symptoms, 2 = mild psychosis symptoms
= not significant; all correlations significant at <.001 unless otherwise stated.
Table 5.
Logistic regression analysis dimensional predictor variables predicting PS (n=492)
| Predictors | Odds Ratio | z-value | p-value | 95% CI |
|---|---|---|---|---|
| Covariates | ||||
| Age | 1.04 | 1.02 | .31 | 0.96 – 1.12 |
| Sex | 0.46 | 3.20 | .001 | 0.29 – 0.74 |
| Psychotropic medication | 2.00 | 2.93 | .003 | 1.26 – 3.19 |
| Continuous predictors | ||||
| Aggression (CBCL) | 0.98 | 0.15 | .88 | 0.75 – 1.27 |
| Depression (CSI) | 0.98 | 0.12 | .90 | 0.76 – 1.27 |
| Inattention (CSI) | 1.44 | 2.69 | .007 | 1.10 – 1.87 |
| Hyperactivity (CSI) | 0.92 | 0.48 | .63 | 0.67 – 1.28 |
| Anxiety (CBCL) | 1.01 | 0.07 | .95 | 0.78 – 1.30 |
| Mania (CMRS) | 0.90 | 0.76 | .45 | 0.69 – 1.18 |
| Social Communication/Interaction (SRS) | 0.88 | 0.85 | .39 | 0.67 – 1.17 |
| Three-level ordinal predictor | ||||
| Psychosis (CSI)a,b | ||||
| mild symptoms vs no symptoms | 1.41 | 1.18 | .24 | 0.79 – 2.51 |
| moderate symptoms vs no symptoms | 1.67 | 1.30 | .19 | 0.77 – 3.59 |
Note. CBCL = Child Behavior Checklist; CSI = Childhood Symptom Inventory; CMRS = Child Mania Rating Scale; SRS = Social Responsiveness Scale;
= Given its low rate of symptoms, psychosis was represented as an ordinal “dimension” with 3 levels (i.e., no/mild/moderate symptoms) – OR’s are compared to reference group with no psychosis symptoms.
Wald X2(2) = 2.21, p = .33.
To determine the extent to which inattention symptoms accounted for the associations between diagnostic groups and slow PS found in Table 2, we re-ran the logistic regressions for diagnostic groups and slow PS with inattention symptoms in the model. Associations that had previously shown an association to slow PS remained significant suggesting that inattention symptoms were not driving these associations. Specifically, significant OR’s were found for psychosis (OR = 5.51, 95% CI 2.16 – 14.05, p < .001), ASD (OR = 1.98, 95% CI 1.25 – 3.14, p = .004) and inattention symptoms (OR = 1.31, 95% CI 1.06 – 1.63, p = .01). Although the association with ADHD initially showed a statistical trend (OR = 1.42, [95% CI 0.97 – 2.07], p = .07), adding inattention symptoms to the model reduced this association further (OR = 1.11, [95% CI 0.71– 1.73], p = .66).
Follow-up analyses:
Psychotropic medications:
We followed up the association with psychotropic medication use by controlling for specific medication types separately (stimulants, use of non-stimulant medication, atypical antipsychotic medication and SSRIs). Results suggest that the significant OR for use of psychotropic medication was driven by use of atypical antipsychotic medication (OR = 3.24, 95% CI 1.59 – 6.63, p = .001) and not by any of the other three medication types. However, the significant finding for inattention symptoms (OR = 1.51, 95% CI 1.15 – 1.98, p = .003) remained even after controlling for this medication type.
PSI as a continuous variable:
A linear regression analysis with PSI as a continuous dependent variable did not change results based on the dichotomous PSI variable (Supplementary Table S2). Inattention remained as the only symptom domain that significantly associated with variation in PS. Results showed that a one-SD increase in inattentive symptoms was associated with a decrease of ~2.4 PS index points (t = 3.19, p = .002).
Imputation of missing data:
Results of Little’s MCAR test suggest that the missing data is completely random (χ2(104) = 100.99, p = .57) making our dataset suitable for multiple imputation. Results of multiple imputation analysis (Supplementary Table S3), which allowed us to use our full sample, were similar to the analyses on the 492 youth, with inattention being the only significant predictor of slow PS (OR 1.34, 95% CI 1.07 – 1.68, p = .01).
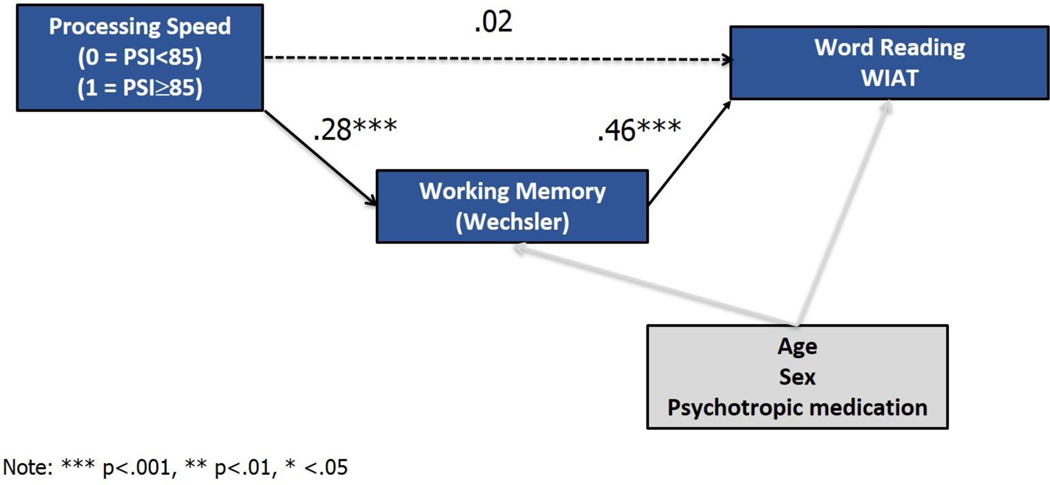
Analysis 5. SEM of slow PS, WM, and academic functioning
We ran SEMs examining the relationship between slow PS and different academic achievement test results, considering the extent to which PS has direct effects as well as indirect effects through WM (after controlling for age, sex, and psychotropic medication). As shown in Figure 2a, a significant indirect effect for PS on Word Reading was found, mediated by WM (ß = .13, z = 6.53, p < .001). This indirect effect accounted for 86.7% of the total effect (ß = .15, z = 3.93, p < .001) of PS on Word Reading. No significant direct effect of slow PS on Word Reading was found (ß = .02, z = 0.57, p = .57).
Figure 2a.
PS shows indirect effects on word reading via working memory
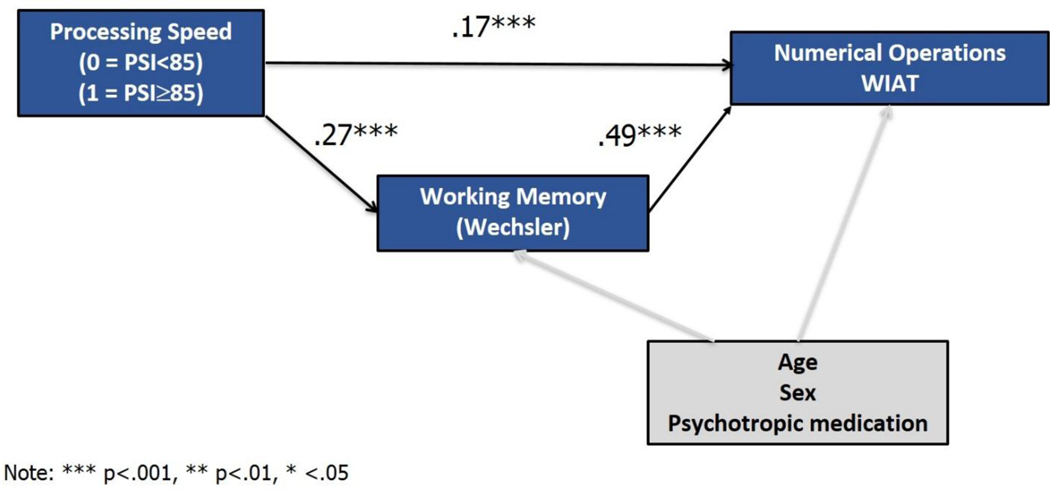
Second, we exmined the mediation effect of WM in the relation between PS and Numerical Operations. As shown in Figure 2b, there was a significant indirect effect of PS that was mediated by WM (ß = .13, z = 6.55, p < .001) as well as a significant direct effect of slow PS on Numerical Operations (ß = .17, z = 5.20, p < .001). This indirect effect accounted for 43.3% of the total effect (ß = .30, z = 8.28, p < .001) of PS on Numerical Operations and the direct effect was responsible for the remaining 56.7% of the total effect.
Figure 2b.
PS shows both direct effects on numerical operations and indirect effects via working memory
Follow up analyses:
Given our findings from the analyses of dimensional psychopathology symptoms above, and the potential for general ability to impact academic functioning, we repeated the two mediation models from Figures 2a and 2b but controlled for GAI and inattention symptoms. For Word Reading, results were similar with an indirect effect of PS through WM (indirect effect: ß = .04, z = 3.29, p = .001) and no significant direct effect of PS on Word Reading (ß = −.02, z = 0.44, p = .66). The total effect of PS on Word Reading was not significant (ß = .02, z = 0.61, p = .54) due to a suppression effect where the indirect and direct effect of PS on Word Reading have opposite signs. For Numerical Operations, even after controlling for GAI and inattention symptoms, a significant direct effect (ß = .12, z = 3.76, p < .001) for PS was found as well as an indirect effect through WM (ß = .03, z = 3.37, p = .001). The indirect effect of PS on Numerical Operations represented 18.8% of the total effect of PS on Numerical Operations (ß=.16, z=4.69, p < .001) indicating that the majority (81.2%) of the total effect of PS on Numerical Operations was direct.
Discussion
Slow PS has been known to relate to functioning in a range of settings, including school [9]. Although reduced PS has been linked to ADHD and other child neuropsychiatric conditions in separate studies, the current study advances the literature by documenting slow PS as a phenomenon relevant to multiple forms of child psychopathology. In an outpatient child psychiatry cohort, PS represented the lowest index score from the Wechsler cognitive battery. Youth representing all seven different psychopathology categories, as well as those who were referred but did not meet full DSM criteria for any condition, showed significantly slower PS compared to population norms. Compared to referred youth with no full diagnoses, diagnoses of ASD, psychosis-related diagnoses and ADHD-I significantly and independently increased the risk of slow PS after accounting for other conditions. Regarding psychopathology symptom dimensions, only inattention symptoms associated with slow PS; however, even when accounting for variation in inattention, the relationships between slow PS and ASD and psychosis remained. Finally, slow PS showed a direct relationship to academic achievement as well as an indirect relationship through its impact on WM. Together, these results highlight the relevance of slow PS to different aspects of neuropsychiatric illness as well as to real world academic functioning in child psychiatric outpatients.
Our sample included children and adolescents consecutively referred for an outpatient neuropsychiatric evaluation regardless of their diagnoses. This strategy allowed for examination of PS in relation to a range of different types of psychopathology compared to both population norms and clinic controls. Several aspects of our analyses echoed the prior literature. For example, the greater relative impairment in PS compared to other domains of the Wechsler Intelligence Scales, including WM (which is impaired in a range of child psychiatric conditions [16]), is consistent with prior studies of individual conditions [10, 14] and the one outpatient cohort previously studied [18]. Our analyses also echo associations between slow PS and conditions beyond ADHD. Most notably, in addition to ADHD-I, we found evidence for slow PS in relation to ASD and psychosis compared to population norms and relative to clinic controls, consistent with studies of individual [10, 14] and multiple conditions [19] compared to controls.
Several aspects of our analyses also extend the prior literature. First, our approach allows us to conclude that the relationships between slow PS and different diagnostic groups compared to referred youth were not simply the result of comorbidity. This result is notable because conditions such as ASD and psychosis are known to co-occur with ADHD [41, 42]. Nonetheless, we did document an impact of comorbidity in that the presence of two or more comorbid conditions significantly elevated risk for slow PS. Second, our documentation of relationships between specific diagnoses and slow PS (ASD, psychosis, and ADHD-I) among referred youth strengthens the evidence for slow PS in these conditions and highlights characteristics of those outpatients that are potentially at highest risk for this difficulty. Further, our use of both population norms as well as clinic controls allows us to conclude that there may be gradations of weaknesses in PS in psychiatrically referred youth. Even youth without full psychiatric diagnoses demonstrated reduced performance on a PS measure compared to population norms, suggesting that there is a PS decrement in referred youth generally; however, among these outpatients, weaknesses in PS were significantly more severe in the presence of ASD, psychosis and ADHD-I. Additionally, while mood, anxiety and oppositional disorders showed slow PS compared to population norms, these diagnoses did not independently elevate risk for slow PS among clinic referrals. These data and the fact that Mayes and Calhoun [19] found no associations for these conditions with PS in comparisons with neurotypical controls suggest that the PS weakness in these conditions may be of smaller magnitude than in others. Finally, although there is strong evidence for the underlying dimensional nature of psychopathology, prior studies have not, to our knowledge, examined slow PS in relation to a wide range of psychopathology dimensions. Symptom dimensions are important to consider because variation in a single trait could also account for cross-disorder findings. Our results showed that variation in only one symptom dimension –inattention—related to slow PS in our sample but did not explain the relationship of slow PS with other conditions.
It is noteworthy that we found an association with the diagnosis of ADHD and slow PS compared to population norms as well as ADHD and PS when PS was considered as a dimensional variable. However, compared to clinic controls after accounting for other conditions, we found associations between slow PS and ADHD-I, though not ADHD- C. Considered together with our dimensional symptom data (highlighting a relationship with inattention), such evidence suggests that risk for slow PS within ADHD is largely carried by level of inattention symptoms. Our data are not direct contradictions of the prior literature, as previous studies have considered PS in youth with ADHD in relation to non-ADHD controls [9]. Indeed, our result mirrors other studies [21, 22] that found PS to be related to inattention symptoms within the condition.
Our findings also have implications for models of shared risk across different forms of psychopathology as well as clinical practice. Regarding psychopathology models, there is growing evidence that ASD, psychotic disorders and ADHD share aspects of their underlying genetic liability [43]. By tying slow PS to these conditions, our data suggest that this aspect of cognitive functioning should be investigated in relation to the risk shared by these conditions. Additionally, from a practical clinical perspective, because youth with ASD, psychosis and/or ADHD-I may have a higher likelihood of manifesting slow PS than other referred youth, youth with these features may benefit from direct evaluation of PS. If decrements in PS are confirmed, such youth may require added educational supports. Though how best to support children with slow PS remains an open question, strategies regarding acceptance, advocacy and accommodations are important tools that are available now to promote improved functioning in the school setting [1]. Accommodations for extended time, teaching time-management skills, and the use of assistive technology are all good examples of such strategies. Additionally, promising strategies that increase speed of processing directly have been piloted in adults with neurological illness (e.g. [44]), and work is needed to develop and extend such programs to children.
Developing models of the relationship between slow PS and academic functioning will also help to refine recommendations for affected youth. The current paper examined one possible model of the association between slow PS and academic functioning with WM as a mediator. Our results showed that slow PS has a direct relationship to math achievement and an indirect relationship to tests of math and reading achievement through its impact on WM. These results indicate that slow PS impacts academic outcomes independently and jointly in the context of other cognitive skills. Such results (which could suggest a developmental cascade [45] in which slow PS contributes to WM difficulties), require confirmation in longitudinal studies of psychiatric outpatients, though the mediation of the effect of PS on academic achievement by WM has been confirmed longitudinally in youth with congenital heart disease [27]. Additionally, given that computerized strategies exist to improve WM [46], these results also raise the intriguing possibility that improving WM can reduce the negative impact of slow PS on academic achievement. Finally, although we did not specifically test for this, our pattern of results suggests that PS may have a greater impact on some academic skills than others (i.e., in this case on Numerical Operations versus Word Reading). Nonetheless, we note that others have found that PS impacts both reading and math and that it is important to consider academic outcomes beyond the two subtests that we examined. Certainly Numerical Operations require more complex processing than Word Reading, and it may be that high-order academic skills are particularly vulnerable to slower PS. For example, reading comprehension requires the ability to rapidly process information simultaneously while engaged in the act of reading. Similarly, written language skills require the ability to process multiple tasks at once.
Results should be considered in light of their limitations. First, we acknowledge that we have used a single measure to operationalize the construct of slow PS. The advantage of using this index score from the Wechsler IQ battery is the large, nationally representative normative sample and the widespread use of this measure in clinical, school and research settings. Nonetheless, further work is needed to extend these findings to other measures of PS (e.g. naming speed or simple reaction time indices). Second, despite the value of our one sample t-tests, which allow us to compare mean PS scores for diagnostic groups with normative data, we were unable to control for comorbidity in these analyses. Thus, we cannot rule out the possibility that comorbidity is driving the significant difference between some of the groups and same age peers. Third, as noted above, our study examined only one potential model of the impact of slow PS on academic functioning in child psychiatry outpatients. Other possible mechanisms by which slow PS could impact academics should be considered.
Fourth, our analyses grouped mood disorders into one category and thus cannot rule out the possibility of differing relationships between slow PS and specific mood-related conditions. Fifth, some of the patients in our sample were taking medication. While a mediation-naïve sample would provide certain advantages, we did not limit our sample in this way in order to prioritize the generalizability of these results. To address the impact of medication, we did include it as a covariate in our analyses. We only found an association between medication (specifically atypical antipsychotics) in one analysis (of dimensional traits), and it did not mask the association between inattention symptoms and slow PS in that model. Additionally, there were no medication effects in our analyses of categorical diagnoses. Thus, we can conclude that psychotropic medication use did not fully account for the finding that PS relates to multiple aspects of psychopathology.
Finally, we note that our use of clinical diagnoses facilitated our ability to collect a large sample of consecutive referrals. We acknowledge that structured diagnostic interviews across the entire sample would have value. Nonetheless, structured diagnostic interviews confirmed the validity of ADHD diagnoses in a subsample of youth, kappa statistics support the reliability of our diagnostic process, and our use of clinical diagnoses may help to promote generalizability to other clinical samples.
In summary, the current work advances the literature on PS as a cognitive function relevant to different types of psychopathology (including inattention within and beyond ADHD, ASD, and psychosis) as well as to academic outcomes. Further, our findings suggest that PS has both direct and indirect effects on academic success. In today’s fast-paced classroom environments, it is not only the accuracy of a task that is essential, but also the speed at which it is performed that relates to success. Our data underscore that PS as an important topic of study that intersects the pediatric neuropsychology, child psychiatry and school psychology/educational fields. Future studies aimed at refining causal models and strategies for intervention will likely require a cross-disciplinary approach.
Supplementary Material
Acknowledgements:
This research was supported by funding from the David Judah Foundation to Alysa Doyle and Ellen Braaten and from the Stanley Center for Psychiatric Research and NIMH (R01 MH116037) to Alysa Doyle.
Footnotes
Disclosures: On behalf of all authors, the corresponding author states that there is no conflict of interest. The authors report no conflicts of interest. Drs. Doyle, Vuijk, Forchelli, Ward, Cook and O’Keefe and Ms. Lee, Ms. Lind, Ms. Samkavitz, and Mr. McGuinness have no additional affiliations to disclose. Dr. Braaten serves on the boards of Magination Press. She receives royalties from books published by Guilford Press Bright Kids Who Can’t Keep Up and The Child Clinician’s Report Writing Handbook and by Sage The Sage Encyclopedia of Intellectual and Developmental Disorders.
This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Braaten EB and Willoughby BL, Bright Kids Who Can’t Keep Up. 2014, New York: Guilford Press. [Google Scholar]
- 2.Ball K, Edwards JD, and Ross LA, The impact of speed of processing training on cognitive and everyday functions. J Gerontol B Psychol Sci Soc Sci, 2007. 62 Spec No 1: p. 19–31. [DOI] [PubMed] [Google Scholar]
- 3.Owsley C, et al. , Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology, 2002. 48(4): p. 254–65. [DOI] [PubMed] [Google Scholar]
- 4.Fry AF and Hale S, Relationships among processing speed, working memory, and fluid intelligence in children. Biol Psychol, 2000. 54(1–3): p. 1–34. [DOI] [PubMed] [Google Scholar]
- 5.Kail R and Salthouse TA, Processing speed as a mental capacity. Acta Psychol (Amst), 1994. 86(2–3): p. 199–225. [DOI] [PubMed] [Google Scholar]
- 6.Geary DC, Cognitive predictors of achievement growth in mathematics: a 5-year longitudinal study. Dev Psychol, 2011. 47(6): p. 1539–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohde TE and Thompson LA, Predicting academic achievement with cognitive ability. Intelligence, 2007. 35: p. 83–92. [Google Scholar]
- 8.Shanahan MA, et al. , Processing speed deficits in attention deficit/hyperactivity disorder and reading disability. J Abnorm Child Psychol, 2006. 34(5): p. 585–602. [DOI] [PubMed] [Google Scholar]
- 9.Cook NE, Braaten EB, and Surman CBH, Clinical and functional correlates of processing speed in pediatric Attention-Deficit/Hyperactivity Disorder: a systematic review and meta-analysis. Child Neuropsychol, 2018. 24(5): p. 598–616. [DOI] [PubMed] [Google Scholar]
- 10.Doobay AF, et al. , Cognitive, adaptive, and psychosocial differences between high ability youth with and without autism spectrum disorder. J Autism Dev Disord, 2014. 44(8): p. 2026–40. [DOI] [PubMed] [Google Scholar]
- 11.Oliveras-Rentas RE, et al. , WISC-IV profile in high-functioning autism spectrum disorders: impaired processing speed is associated with increased autism communication symptoms and decreased adaptive communication abilities. J Autism Dev Disord, 2012. 42(5): p. 655–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sheffield JM, Karcher NR, and Barch DM, Cognitive Deficits in Psychotic Disorders: A Lifespan Perspective. Neuropsychol Rev, 2018. 28(4): p. 509–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bolt LK, et al. , Neurocognition as a predictor of transition to psychotic disorder and functional outcomes in ultra-high risk participants: Findings from the NEURAPRO randomized clinical trial. Schizophr Res, 2018. [DOI] [PubMed] [Google Scholar]
- 14.Kelleher I, et al. , Neurocognitive performance of a community-based sample of young people at putative ultra high risk for psychosis: support for the processing speed hypothesis. Cogn Neuropsychiatry, 2013. 18(1–2): p. 9–25. [DOI] [PubMed] [Google Scholar]
- 15.Baune BT, et al. , Neuropsychological functioning in adolescents and young adults with major depressive disorder--a review. Psychiatry Res, 2014. 218(3): p. 261–71. [DOI] [PubMed] [Google Scholar]
- 16.Willcutt EG, et al. , Recent developments in neuropsychological models of childhood psychiatric disorders, in Biological Child Psychiatry: Recent Trends and Developments, Banaschewski T and Rohde L, Editors. 2008, Basel, Karger. p. 195–226. [Google Scholar]
- 17.Doyle AE, et al. , Cross-Disorder Cognitive Impairments in Youth Referred for Neuropsychiatric Evaluation. J Int Neuropsychol Soc, 2018. 24(1): p. 91–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calhoun SL and Mayes SD, Processing speed in children with clinical disorders. . Psychology in the Schools, 2005. 42(4): p. 333–343. [Google Scholar]
- 19.Mayes SD and Calhoun SL, Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder. Child Neuropsychol, 2007. 13(6): p. 469–93. [DOI] [PubMed] [Google Scholar]
- 20.Cuthbert BN, The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry, 2014. 13(1): p. 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller AC, et al. , Reading comprehension in children with ADHD: cognitive underpinnings of the centrality deficit. J Abnorm Child Psychol, 2013. 41(3): p. 473–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kibby MY, Vadnais SA, and Jagger-Rickels AC, Which components of processing speed are affected in ADHD subtypes? Child Neuropsychol, 2018: p. 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.PGC CDG, Identification of risk loci with shared effects on five major psychiatric disorders: a genome-wide analysis. Lancet, 2013. 381(9875): p. 1371–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roth B, et al. , Intelligence and school grades: A meta-analysis. Intelligence, 2015. 53: p. 118–137. [Google Scholar]
- 25.Gathercole SE and Pickering SJ, Working memory deficits in children with low achievements in the national curriculum at 7 years of age. Br J Educ Psychol, 2000. 70 ( Pt 2): p. 177–94. [DOI] [PubMed] [Google Scholar]
- 26.Alloway TP and Alloway RG, Investigating the predictive roles of working memory and IQ in academic attainment. J Exp Child Psychol, 2010. 106(1): p. 20–9. [DOI] [PubMed] [Google Scholar]
- 27.Cassidy AR, et al. , Processing speed, executive function, and academic achievement in children with dextro-transposition of the great arteries: Testing a longitudinal developmental cascade model. Neuropsychology, 2016. 30(7): p. 874–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rose SA, Feldman JF, and Jankowski JJ, Modeling a cascade of effects: the role of speed and executive functioning in preterm/full-term differences in academic achievement. Dev Sci, 2011. 14(5): p. 1161–75. [DOI] [PubMed] [Google Scholar]
- 29.Landis JR and Koch GG, The measurement of observer agreement for categorical variables. Biometrics, 1977. 33: p. 159–174. [PubMed] [Google Scholar]
- 30.Gadow KD and Sprafkin JN, Child Symptom Inventory- Fourth Edition: Screening and norms manual. 2002, Checkmate Plus: Stony Brook, NY. [Google Scholar]
- 31.Achenbach TM and Rescorla LA, Manual for the ASEBA School-Age Forms & Profiles. 2001: Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- 32.Constantino JN and Gruber CP, Social Responsiveness Scale. 2005: Los Angeles. [Google Scholar]
- 33.Robinson EB, et al. , Stability of autistic traits in the general population: further evidence for a continuum of impairment. J Am Acad Child Adolesc Psychiatry, 2011. 50(4): p. 376–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pavuluri MN, et al. , Child mania rating scale: development, reliability, and validity. J Am Acad Child Adolesc Psychiatry, 2006. 45(5): p. 550–60. [DOI] [PubMed] [Google Scholar]
- 35.Wechsler D, The Wechsler Intelligence Scale for Children—Fourth Edition. 2004. [Google Scholar]
- 36.Wechsler D, Wechsler Adult Intelligence Scales -Fourth Edition 2008. [Google Scholar]
- 37.Prifitera A, Weiss LG, and Saklofske DH, The WISC-III in context, in W1SC-1II clinical use and interpretation: Scientist-practitioner perspective, Prifitera A and Saklofske DH, Editors. 1998, Academic Press: San Diego, CA. p. 1–38. [Google Scholar]
- 38.Tulsky DS, et al. , Development of a general ability index for the Wechsler Adult Intelligence Scale--Third Edition. Psychol Assess, 2001. 13(4): p. 566–71. [DOI] [PubMed] [Google Scholar]
- 39.Wechsler D, Wechsler Individual Achievement Test- Third Edition. 2009. [Google Scholar]
- 40.Agler R and De Boeck P, On the Interpretation and Use of Mediation: Multiple Perspectives on Mediation Analysis. Front Psychol, 2017. 8: p. 1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sokolova E, et al. , A Causal and Mediation Analysis of the Comorbidity Between Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD). J Autism Dev Disord, 2017. 47(6): p. 1595–1604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levy E, et al. , Psychotic disorders comorbid with attention-deficit hyperactivity disorder: an important knowledge gap. Can J Psychiatry, 2015. 60(3 Suppl 2): p. S48–52. [PMC free article] [PubMed] [Google Scholar]
- 43.Elia J, et al. , Rare structural variants found in attention-deficit hyperactivity disorder are preferentially associated with neurodevelopmental genes. Mol Psychiatry, 2010. 15(6): p. 637–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chiaravalloti ND, et al. , A Pilot Study Examining Speed of Processing Training (SPT) to Improve Processing Speed in Persons With Multiple Sclerosis. Front Neurol, 2018. 9: p. 685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Masten AS and Cicchetti D, Developmental Cascades: Part 1. Development and Psychopathology, 2010. 22(3): p. 491–495. [DOI] [PubMed] [Google Scholar]
- 46.Spencer-Smith M and Klingberg T, Benefits of a working memory training program for inattention in daily life: a systematic review and meta-analysis. PLoS One, 2015. 10(3): p. e0119522. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.