Abstract
This paper presents a four-stage plyometric program to be undertaken as part of criterion-based rehabilitation for athletes with anterior cruciate ligament reconstruction (ACLR). After ACLR, the patient experiences alterations of joint mobility, gait and movement patterns, neuromuscular function and general physical fitness. Plyometric training is an important component for neuromuscular and movement re-conditioning after ACLR. Effective use of plyometrics can support enhancements in explosive sporting performance, movement quality and lower risk of injury. Plyometric training, as a component of the ACL functional recovery process, can aid in restoring function and supporting timely return to sport. However, few patients undertake or complete a plyometric program prior to return-to-sport. To truly impact individual patients, a stronger focus on research implementation is needed from researchers to translate efficacious interventions into practice. In designing a plyometric program, it is important to match the specific plyometric tasks to the functional recovery status of the ACLR patient. To do this, it is important to understand the relative intensity of plyometrics tasks, align these tasks to the ACL functional recovery process and monitor the athlete as part of criterion based rehabilitation. Plyometric intensity is based on the intensity of efforts, the vertical and/or horizontal momentum prior to ground contact, the ground contact time and the surface or environment on which they are performed on/in. Furthermore, how the person technically performs the task will influence joint loading. There should be a gradual increase in task intensity and specificity throughout the program, with all tasks used for both neuromuscular and motor control re-conditioning. The aim of this paper is to provide recommendations to clinicians on how to design and implement plyometric training programs for the ACLR patient, as part of the functional recovery process.
Level of evidence
5
Keywords: rehabilitation, reconditioning, neuromuscular performance, movement performance, injury prevention
INTRODUCTION
A key goal within sports medicine is to improve the outcomes of patients after major injury. It appears that many patients fail to return-to-sport (RTS) and/or previous sporting performance levels after anterior cruciate ligament reconstruction (ACLR).1–4 Those who RTS, do so often at much elevated risk of re-injury, with typically around nearly one in three young athletes experiencing a knee re-injury,5,6 generally within the first two years after RTS.7 Current opinion is that in order to improve athlete outcomes after ACLR, there is a need to optimize the processes and practices of rehabilitation.8,9 Key areas suggested in need of improvement are the restoration of neuromuscular performance (e.g., strength and power) and movement quality of patients prior to RTS after ACLR.8–11 Following ACLR, at the time of RTS, patients often present with deficits in knee extensor maximal strength12–14 and rate of force development (RFD),15,16 as well as lower limb/closed chain strength15 and power.17 Furthermore, patients often RTS with movement asymmetries during an array of functional tasks18–23 thought to predispose them to increased risk of injury.7,24–26
One highly valued element of rehabilitation after ACLR is the use of plyometric training.8 Plyometric exercises involve a stretch-shortening cycle, which is a commonly observed phenomenon involving a rapid lengthening of a muscle tendon unit, immediately followed by a rapid shortening (for a review see Davies et al.).27 Plyometric training has long been used to optimize explosive sporting performance (e.g., speed, jump height) of athletes and is regarded as an excellent training method, due to the wide ranging neuromuscular and motor control benefits.28–32 In particular, plyometric training has been reported to be superior to more traditional resistance training for development of explosive lower limb performance (power/RFD),30,31,33 as well as effective at eliciting gains in maximal strength,32 and sports performance variables, such as linear34 and multiple directional29 movement speeds.
Ebert et al.35 reported that only 30% of patients completed a plyometric program prior to RTS after ACLR.35 A key issue with implementing plyometric training into the functional recovery process of ACLR patients is a lack of guidance within the literature on how and when to do it. Plyometric tasks vary in their intensity and specificity, with typical peak ground reaction forces (GRF) ranging from 1.5-7 times body mass.36–40 Inappropriate plyometric task choice could thus be expected to cause adverse reactions on an unprepared person after major lower limb injury. There is a need to support practitioners on how to effectively use plyometrics after major lower limb injury, such as ACLR. To do this, there is a need to understand the types of plyometrics available, their relative loading/intensity and understand how to systematically incorporate plyometric training as part of the ACL functional recovery pathway. Therefore, the aim of this paper is to provide recommendations to clinicians on how to design and implement plyometric training programs for the ACLR patient, as part of the functional recovery process. This will hopefully aid a reduction in the barriers between research and effective implementation into practice.
PLYOMETRIC TRAINING AFTER ACL RECONSTRUCTION – KEY CONSIDERATIONS IN PROGRAM DESIGN
Designing a plyometric training program to develop neuromuscular performance and movement quality, while respecting tissue healing, is an important consideration for the rehabilitation specialist.9,41 In planning effective plyometric use and progressions, it is important to have consideration of optimal loading (defined as the load applied to structures that maximizes physiological adaptation)41 to bring about specific neural, morphological and mechanical adaptations.41 Optimal plyometric program design entails an understanding of the specific loading demands of the various plyometric tasks, so a series of optimal progressions can be planned. It is important to consider the intensity of movement or the specific external and internal loading of the task(s). External forces are the result of equal and opposite forces acting on the body according to the laws of motion (e.g., Newton’s laws), while the internal joint loads will depend on how the GFR loads are distributed throughout the body. Load is actively accepted/dissipated via the neuromuscular system and absorbed passively via the tendons, ligaments and joints during movements. Internal hip-, knee-, and ankle-extension (plantarflexion) moments must be produced via eccentric, isometric and concentric muscle contractions to control joint motion, absorb the kinetic energy of the body at impact and produce force and power to propel the body ballistically during plyometric tasks.42 Inability to accept load either due to deficits in strength, would mean a greater reliance on joint complexes (tendon, ligament and joint structures) for passive force absorption.43 It is important to understand the specific loading demands of the various tasks, the patients capacity to tolerate these loading demands (e.g., strength and movement quality) and understand how the patient has responded to the specific loads on an individual level (e.g., monitoring loading response).
Plyometric task intensity and complexity
In terms of plyometric loading, it is important to consider the peak external loads of the tasks, the joint specific internal moments, the neuromuscular activation/muscle forces as well as the neuromuscular control challenge. In addition, consideration of volume load is important.
During movement, an individual must produce and accept force via its application to the ground according Newtons laws of motion. Newtons third law dictates that there will be an equal and opposite reaction, whilst Newtons second law, the law of acceleration, dictates movement acceleration will be a product of force application relative to body mass (Force = mass x acceleration). Intensity of plyometric tasks can be considered on the basis of peak GRFs, which typically occur during the eccentric/landing phase, but also peak concentric forces (and power) are important on a performance level. In addition, the rate of force acceptance and development is important. This is essentially the rate of change in force during the landing and jumping phases of a plyometric task.
Peak external loading is largely dictated by task selection, the neuromuscular capacity to accept and develop force (e.g., strength), surface/environment and ground contact time (GCT)/instruction:
Task selection: Plyometric tasks can be considered based on stance and body positioning at take-off/landing, consisting of unilateral and different bilateral versions (Table 1 and Figure 1). During the eccentric phase of a plyometric task, the athlete will need to decelerate the center of mass, prior to producing force and power to ballistically propel oneself as part of the plyometric action. The peak eccentric forces will largely be dictated via the velocity or the relative momentum of the system, as a whole at impact/landing.40 The higher the momentum (mass x velocity) prior to/ at impact, the greater the eccentric work required to decelerate the body. As such, intensity of effort and height of landing and/or horizontal speed prior to deceleration are major determinants of peak loading of plyometric tasks.
Table 1: The four types of plyometric task based on stance position at landing and/or take-off, with description and examples.
| Plyometric type | Description | Example(s) |
|---|---|---|
| Unilateral | Involve eccentrically accepting load on one limb and then concentrically developing force and power to accelerate again on one limb. This includes jumping from one limb to the other (e.g., bounding/ running), or continuous same limb plyometrics (e.g., hops). | Bounding (alternating bounds, speed bounds, bounds for height etc.); SL SJ, SL CMJ, SL drop jump; lateral jumping and hopping; rotational hopping/ jumping |
| Bilateral (symmetrical) | Both limbs accept and produce force simultaneously from a symmetrical stance position | BL SJ, BL CMJ, BL drop jump; tuck jump |
| Bilateral (asymmetrical) | Both feet take off and/or contact the ground simultaneously but in different positions. As such, the demand placed on each leg is different and shared. | Split jumps, same stance landing, alternating leg position |
| Bilateral (with timing off-set) | Typically involve landing on one limb before taking off on the other limb. These exercises can be defined as skipping type movements and do not characterize the typical stretch shortening cycle motion on a single limb. | Skipping Alternating box split jumps |
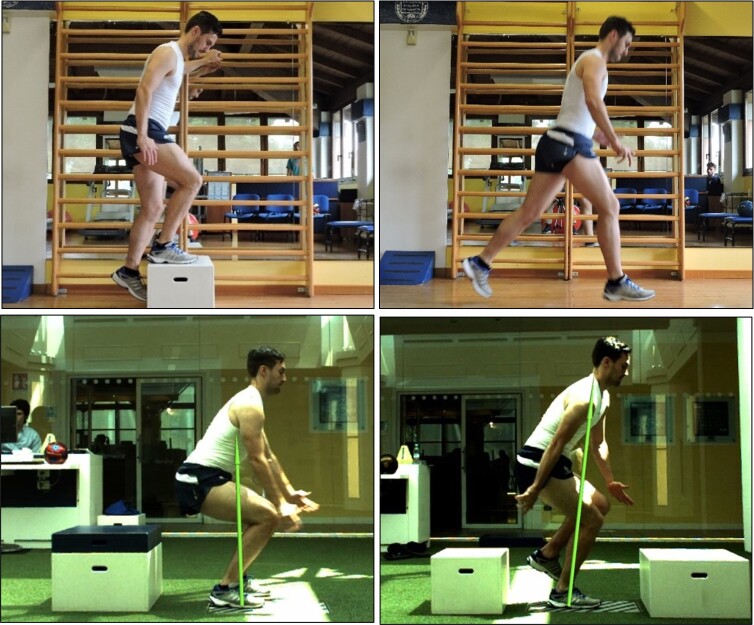
Figure 1: Four types of plyometrics, A) bilateral off-set (alternating box jump), B) bilateral asymmetrical (split jump), c) bilateral symmetrical (30 cm drop jump) and d) unilateral (30 cm drop jump.
Strength: greater total lower extremity energy absorption in the sagittal plane has been associated with smaller vertical GRF and greater knee-flexion displacements during landing.44,45
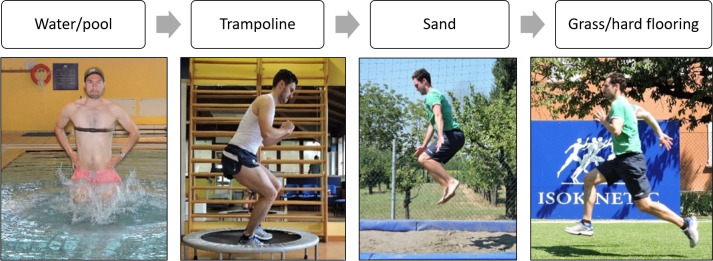
Surface: a compliant surface will deform under load and as such joint loading is influenced by the surface stiffness. Performing plyometrics in water or on sand has been shown to reduce the high impacts and results in less muscle soreness than performing plyometrics on more rigid surfaces.46 For example, at the appropriate depth of water in the pool, there appears to be a reduction of around 45-60% in peak GRFs recorded from plyometric exercise in water versus on land.39,47
GCT: peak force and particularly RFD and rate of power development will also be dictated by GCT. The RFD and rate of power development will be a function of force/power produced divided by the GCT, derived as the reactive strength index. GCT and associated RFD are influenced by task choice but also instructions given for performance of the task (e.g., land and jump leaving the ground as quickly as possible).40 GCT (and associated RFD and neural activation during the task) are important considerations in terms of specificity of training adaptations. Improvements in explosive neuromuscular performance appear to be specific to the GCT,29 with longer GCT (>250-500 ms) suited to acceleration and multidirectional movement performance, whilst linear based (horizontal and vertical) fast (GCT < 200 ms) plyometrics may be better suited for developing linear peak running speeds.
As well as peak external loading, it is also important to consider the relative internal joint loading and associated neuromuscular activation and muscle forces. Internal joint loads should be considered across three planes of motion (sagittal, frontal and transverse). During functional tasks, there is a load sharing across joints and muscle groups.48 The relative ‘torque’ experienced at each joint and subsequent muscle forces will be a product of the resultant GRF and the respective distance away from the joint (torque = force x distance). The specific joint loading will be influenced by task selection,40 and kinematics during the task. For example, altering the trunk alignment during plyometric exercise would alter the center of mass and position it closer or further away from the joint.49 A more upright and stiff posture, described as a quadriceps dominant behavior,50 has been correlated with higher knee-extensor moments.51 Greater hip flexion to knee flexion ratios during plyometric type tasks has been shown to reduce knee-extensor moment and knee energy absorption52,53 and increase hip loading.49 Altered frontal- and transverse-plane knee loading has been shown to contribute to greater ACL loading.54–57 It is recommended to avoid at risk movement biomechanics, specifically a knee dominant motor strategy (e.g., upright trunk positioning) in conjunction with altered frontal (hip and tibial abduction) and transverse plane (tibial rotations and/or internal hip rotation) motions during plyometric tasks, as these will exacerbate knee and ACL loading.54–57
It is also important to consider the relative neuromuscular control challenge/loading, when prescribing plyometric progressions. It is thought that effective use of plyometrics can support improved movement quality and reduce ACL injury risk.31,32,58–60 It is known that strength training does not directly improve movement quality during sport-type movements.61 Instead, there is a need to incorporate more sport type movements to relearn and improve movement coordination during sport-type tasks.62 Plyometric drills can improve neuromuscular control in athletes, which can become a learned skill that transfers to sporting competitive movements,31 aiding in the restoration of sport-specific movement quality after injury. For optimal motor learning (defined as ’the process of an individual’s ability to acquire motor skills with a relatively permanent change in performance as a function of practice or experience),63 it is important that the tasks are performed repeatedly with good movement quality.64,65 Thus, it is important to provide the right challenge to neuromuscular control, with progressive increases in movement complexity, as well as rate and intensity of loading.66
While considering the specific loading of a singular task or repetition is important, as discussed, it is also important to consider the volume of loading. Volume load is the result of many actions during a session or over time (e.g. day/week/month). It is known that high recurrent loading of the ACL can lead to graft creeping and eventually failure.67 Furthermore, issues such as patellofemoral pain syndrome are typically the cumulation of chronic overload68 and common after ACLR.69–71 It is recommended to monitor the cumulative loading of respective tasks, which can be done through documenting the exercise sets/foot contacts alongside the task intensity.
Are they strong enough?
It is well accepted that sufficient strength of the lower limb(s) is important for implementation of plyometrics.72–75 Inability to accept load would mean a greater reliance on joint complexes (tendon, ligament and joint structures) for passive force absorption.43 Considering the various descriptors of load, it would seem appropriate to have an understanding of the patients ability for compound muscle strength, to be able to tolerate the external ground reaction forces. Assessing and tracking closed chain strength (e.g., squat and/or leg press strength) can support optimal task progressions.8,9,76 It is important that the plyometric tasks are aligned to the strength status of the athlete and that task intensity supports and tracks with improvements in strength and functionality. The assessment of closed chain strength (e.g., leg press/squat strength) has been suggested to determine the readiness for the introduction of running on treadmill (e.g., 1.25 times body mass single leg press),9,76 unilateral plyometrics (1.5 times body mass single leg press)8,76 and RTS (2 times body mass single leg press).8,76
Additionally, it is important to understand each joint’s ability to withstand loads. The ankle, knee and hip/trunk must accept and produce force in a load sharing manner,48 depending upon the task and the specific movement quality of the patient. Knee extensor strength is a major barrier to functional progressions after ACLR77 and so understanding the knee extensors strength of the ACLR athlete is important to implement and progress plyometric tasks. Patients will typically display large deficits in knee extensor strength in the early weeks after surgery (e.g., 50% deficits at four weeks post ACLR).78 Restoring knee extensor strength is essential to allow for movement based retraining and implementation of plyometrics.9,79 Assessing knee extensor strength using concentric or isometric assessment of the isokinetic dynamometer or recording knee extension loads used in rehabilitation (eg, 8 or 10 repetition maximum) can provide indication of knee extensor strength to support plyometric implementation and progressions. Knee extensor limb symmetry index (LSI) is often used to support progression through stages of an ACLR rehabilitation pathway.8,9 It can be used to support decision making of when patients are ready to perform certain functional tasks including jogging on the treadmill (LSI, 0.70),9,76,80 single leg landing and jumping drills (LSI, 0.80),8,9,76 RTS training (LSI, 0.90)8,76 and return to high level competitive sport (LSI, 1.0).8,80
Do they move well enough?
As well as aligning plyometric loading to strength, it is also important to align plyometric task complexity to movement capabilities. So, it would appear important to know if an athlete is able to perform the task sufficiently well and safely prior to training prescription. Furthermore, it is important to monitor movement quality during the task. This would aid in ensuring that the athlete performs the task with appropriate kinematics before progressing to a subsequently harder task (either higher loading or greater movement complexity or both).
In assessing and training movement quality it is important to understand what movement quality is and which factors may affect performance.66 Movement quality after ACL injury has been defined as ‘the ability to control the limbs and achieve sufficient balance and kinematic alignment during functional activities, not displaying movement asymmetries or risk factors linked to ACL injuries’.8,66 Importantly, the definition makes no reference to what is acceptable loss of balance or deviation of kinematics away from normal, or actually what normal or ideal is.66 In fact, it is thought there likely exists no ’ideal’ or ‘perfect’ way to move.66 According to the dynamic systems theory,81 there are multiple factors which can influence the expression of movement quality, which should be considered when training and assessing movement quality.66 These can be summarized as a complex interaction between individual (organistic constraints), task constraints and the environment or context in which the task is been performed (environmental constraints).
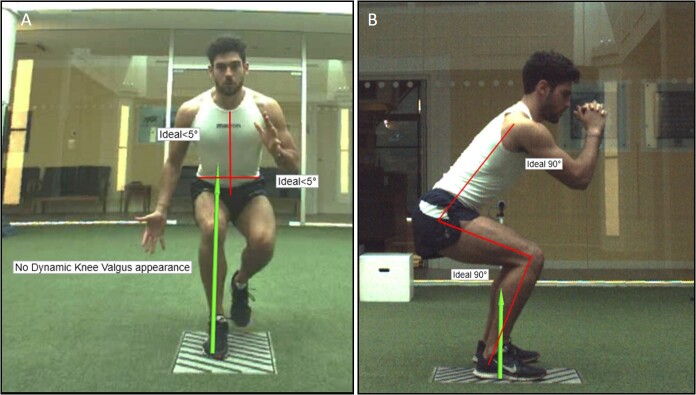
Despite the ambiguity in assessing movement quality, it is here and elsewhere8,9,76 proposed to utilize a relatively simple qualitative movement analysis method to support progression through tasks and through ACL rehabilitation stages as part of criterion based rehabilitation. This can provide information on movement quality during the tasks at hand, and to be able to provide feedback to the patient, to create a continuous learning environment to solve the task and optimally progress.76 It is suggested to monitor the patient’s ability to maintain control of the body utilizing teaching and training of optimal frontal plane (pelvis, trunk and lower limb, Figure 2a) and sagittal plane control (Figure 2b), depending upon the specific task.76 If the tasks cannot be performed at a minimum task competency, then the tasks should be simplified.8 Qualitatively assessing movement quality (frontal and sagittal plane) as part of the ACL functional recovery process during foundation, landing, plyometric and sport-specific tasks is also recommended. This can provide some objective guidance to support criterion driven ACL functional recovery.8,9,82
Figure 2: A, an easy to utilize and teach model of movement analysis based on three lines in the frontal plane, with a line to assess trunk stability/ alignment, pelvis stability/alignment and limb stability/alignment. B, depicts the sagittal plane view which is dependent upon the task but a function of ankle to knee and knee to hip alignments. From Buckthorpe et al.75.
Can they tolerate the level of loading?
A key part of optimal load management is adjusting the training according to the response to exercise. Any functional based progression has to be in line with the biological healing and ability of the joint to withstand the loading demands. Pain and swelling can be used to determine exercise based progressions as these factors will relate to the loading stress experienced by the knee.9,83 Progression to more intense or complex tasks should only be allowed when there is no or minimal pain (e.g., 0-2 on the numeric rating scale)83 or swelling (stroke test) increase in response to previous tasks.83 Pain and/or swelling response would indicate excessive previous loading levels to the knee joint and an adverse reactions, which may then limit optimal adaptation. Furthermore, after unaccustomed exercise, there may be an exercise induced muscle reaction, resulting in delayed onset muscle soreness.84 The degree of muscle reaction depends on many factors including exercise type, duration, intensity and habituation to the exercise.85,86 Tasks that are too strenuous will result in significant muscle reaction, which may take substantial time to recover and may limit the ability to train in the subsequent days. Monitoring the muscle soreness can provide an indication of the muscle specific loading and required recovery time, which can then support subsequent training modifications.
Plyometric progressions after ACLR- A Four-staged program aligned to the rehabilitation pathway after ACLR
For effective design of plyometric programs for the ACLR patient, it is imperative that any such program be aligned to the functional recovery approach and overall goals as a whole. These goals include restoring knee specific factors, neuromuscular function of many muscle groups and types of function (e.g., maximal isolated and functional strength and explosive neuromuscular performance), movement quality and sport-specific fitness.8,9 Although, there is still not an international consensus on ACL rehabilitation, there has been considerable research recently published toward standardizing the ACL rehabilitation journey. Current best practice for ACL rehabilitation appears to involve criterion-based rehabilitation through a series of stages.8,9,87 The functional recovery process can be broadly separated into pre-operative, early, mid and late stage rehabilitation and RTS training.8,9
Below is presented a four-staged plyometric program aligned to the ACL functional recovery process. This considers i) the plyometric tasks and associated intensity and complexity, ii) the required movement quality and strength to perform these tasks and iii) monitoring considerations, specifically daily monitoring (e.g., pain and swelling, soreness rules) but also monitoring as part of criterion-based ACL functional recovery. In general, the program has some rules or themes which include progressions in intensity and specificity of the movements with progressive increases in entry speeds (vertical loading height/ horizontal velocity), a gradual reduction in GCT, progression from bilateral to unilateral tasks and from linear (vertical to horizontal to lateral) to multi-planar tasks. Furthermore, it is recommended to use different surfaces, beginning with more compliant surfaces and progressing to stiffer surfaces (Figure 3).
Figure 3: Possible progressions on use of surfaces for plyometric training in ACL reconstructed athlete or load compromised individuals.
Progressions through stages and exercises within the stage is based on good quality performance of the tasks, ideally no or only minimal pain (e.g., <2/10 on numeric rating scale)83 and/or swelling of the joint to the specific loading demands83 and continued improvement in lower limb strength. Each stage should be completed in sequence and an athlete cannot perform any task in the stage without meeting the specific stage criteria (Table 2). As it aligns to the rehabilitation process after ACLR, meeting specific criteria as part of criterion based rehabilitation is recommended. The four-stage program compliments and aligns to the authors published ACL functional recovery programs.8,9 These involve comprehensive overviews of the mid-stage,8 late-stage and RTS training stages.9 The plyometric program begins in the mid-stage of rehabilitation (Stage 1), with Stages 2 and 3 aligned to the late-stage and Stage 4 to the RTS training stage.
Table 2: A plyometric program approach across four stages aligned to the functional recovery framework after ACL reconstruction. Particular training goals, use of plyometrics, progression criteria, training planning considerations, with specific movement exercises and progressions are presented.
| Stage | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| Typical weeks* | 10-14 | 15-18 | 19-22 | 23-29 | |
| General goals of stage | Full recovery of joint R.O.M Restoration of muscle strength imbalances to within 20% of ‘trained’ contralateral limb (or pre-injury strength values) Recovery of basic motor patterning and running gait Avoid physical fitness de-training |
Develop functional strength Develop closed chain eccentric strength Develop bilateral power Develop unilateral eccentric control Continue to restore lower limb muscle imbalances |
Restore neuromuscular function markers to within at least 10% (knee and adjacent joint specific strength and closed kinetic chain and power) Restore high load movement quality Restore aerobic fitness |
Restore sports specific movement quality, fitness, skills and develop movement ‘volumes’ to prepare for RTS | |
| Plyometric use | Low intensity predominantly bilateral plyometrics at sub-maximal intensity to support eccentric/motor control and preparation for running | Moderate intensity bilateral and unilateral plyometrics with view to developing lower limb power and eccentric control, particularly unilateral deceleration capabilities | Higher intensity bilateral and unilateral plyometrics with view to developing lower limb power and multipolar motor control and acceleration capabilities | Optimise lower limb explosive neuromuscular performance and support sport-specific movement re-training. Mindful of load management | |
| Criteria to enter plyometric stage | 0-1 pain NRS @ rest <2 pain during activities of daily living Full knee extension Knee flexion > 120° Good BL squat (body weight and loaded) with < 20% asymmetry in loading8 Isometric knee extensor LSI >70% |
Ability to run of treadmill for 10 mins @8km/h8 Good BL landing kinematics Good SL squat kinematics Closed chain strength > 1.25 times body mass (8RM) or 1.5 x times body mass (1RM/peak isometric force) Isokinetic LSI knee extensor and flexor >80% |
Good BL drop jump mechanics Good SL landing control Closed chain strength > 1.5 times body mass (8RM) or 2 x times body mass (1RM/peak isometric force) |
Isokinetic LSI knee extensor and flexor >90%9 Closed chain strength > 1.5 times body mass (8RM) or 2 x times body mass (1RM/peak isometric force)9 Good pre-planned movement quality (UL landing/deceleration/ BL and UL drop jump/ CoD mechanics indoor and/or OF) |
|
| Training planning | Intensity | Low | Moderate | High | Very high |
| Plyometric type | BL off-set BL asymmetrical BL symmetrical (sub-max) |
BL off-set BL asymmetrical BL symmetrical UL (linear) |
Bilateral off-set Bilateral asymmetrical Bilateral symmetrical UL (multi-planar) |
Bilateral off-set Bilateral asymmetrical Bilateral symmetrical UL (multi-planar) |
|
| Volume (foot contacts) | 50 | 100 | 150 | 200 | |
| Plyometric Tasks | Lunge push back SJ to box CMJ to box Skips in place Step up jump (same leg) Step up jump (alternating) Step and hold (forward) |
BL SJ (in place, forward) BL CMJ (in place, forward) BL drop jump (30 cm box) Split jump (same leg land) Split jump (alternating) Step and land (forward, lateral, standing and from running on spot) Step-land-push back (forward, lateral, standing and from running on spot) |
UL SJ/CMJ to BL landing UL SJ/CMJ to box Rotational jump and land Lateral step-jump-back Tuck jump Step cut (30°/45°/60°/90°) Hop singular (in place/ forward/ lateral/45°/90°) Hop multiple (in place/ forward/ lateral/45°/90°) SL drop jump (box/in place/lateral to box) Advanced bounding OF |
CMJ (hurdles) SJ/CMJ weighted BL/UL DJ (increased height to box) Lateral hop (band/rope/ med ball) SL 90 lateral drop jump Step cut (perturbation) OF agility drills OF CoD drills with perturbation/ external focus and sport-specific environment |
|
| Other movement tasks | SL movement progressions (from BL squat to UL squat) Bilateral landing from step Trampoline SL landing Re-integration to treadmill running Stage 2 plyometrics in pool (~60% body height) |
Treadmill running (12-20 km/h) Outdoor linear movements (running, ladder drills, lateral shuffle) Stage 3 plyometrics in pool (~60% body height) |
Outdoor pre-planned coordination program (multi-directional movement demands) High speed linear running/sprinting |
On-field sport-specific training with re-active movements, contact/perturbation drills, as well as skills training | |
R. O. M, range of motion; NRS, numeric rating scale; BL, bilateral; LSI, limb symmetry index; SJ, squat jump; CMJ, countermovement jump; RM, repetition maximum; SL, single leg; UL, unilateral; OF, on-field; RTS, return-to-sport; CoD, change of direction; DJ, drop jump * time is only indicative, and the protocol should be always customized on patient’s response.
Stage 1 of the program uses low intensity plyometrics, characterized as bilateral off-set and bilateral asymmetrical, but also with sub-maximal bilateral symmetrical tasks (to support movement re-training). The rise in height of the center of mass above neutral position is typically minimal. GCTs should be long (> 1-2s) and the main theme is to support movement retraining, primarily with a focus to support treadmill gait re-education.9 Estimated GRFs are less than two-times body mass per limb. The program is completed alongside foundation movement re-education, functional strengthening (e.g., squat, deadlift, single leg progressions), bilateral landing tasks and isolated strength training.7 Importantly, during this first stage, which occurs during the mid-stage of rehabilitation after ACLR, the patient will have significant knee extensor strength deficits. Knee extensor weakness is a significant barrier to been able to perform functional tasks.77 Furthermore, significant strength deficits result in biomechanical compensatory strategies. This may include compensatory use of the hip extensors instead of the knee extensors during unilateral tasks or compensatory loading of the un-injured limb during bilateral tasks.88–90 Even when achieving the optimal kinematics (e.g. correcting the compensatory movement pattern of greater hip to knee flexion), there is still typically inhibition of the quadriceps, resulting in lower neuromuscular recruitment, which may result in insufficient stimulus for adaptation.89 As such, the benefits of plyometric training for strength development is likely minimal in this stage. It is essential to ensure optimal technique during the movements,64,65 ideally using real-time biofeedback,64 to support appropriate motor learning. Poor task selection may result in movement compensations,49,64 which could interfere with optimal motor repatterning.65 Thus, quality over quantity and intensity is recommended. It is essential to focus on isolated strengthening techniques to overcome the quadriceps weakness and restore normal quadriceps strength during this stage.7 In terms of recommended plyometric tasks for this stage, these can be seen in figures 4 to 6 and within Table 2.
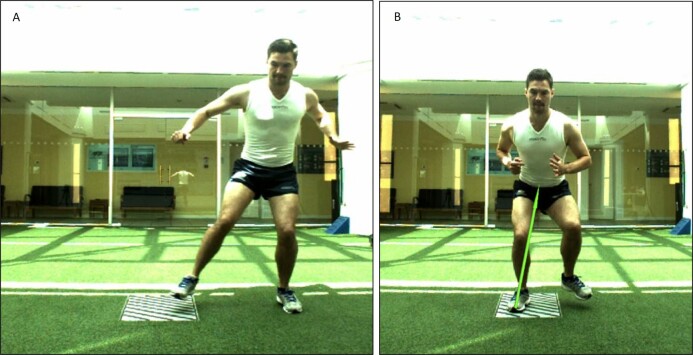
Figure 4: A lunge push-back. The patient steps forward as if performing a lunge (A) and then decelerates their momentum and pushes back with power to arrive back at the starting standing position (B).
Stage 2 of the program commences when the athlete can achieve the necessary late-stage rehabilitation criteria (Table 2). This means they must have a good single leg squat (defined as good control of the movement with no presence of excessive dynamic knee valgus, altered motor strategy or trunk and pelvis deviations),8 sufficient closed kinetic chain (single leg loads > 1.25 times body mass) and knee extensor limb symmetric index (>80%, LSI) and able to run on the treadmill with good kinematics.8,9 Key themes of late-stage ACL rehabilitation are developing single limb eccentric control (deceleration/landing) and restoring power and maximal eccentric strength.9 However, there is a strong use of bilateral plyometric tasks for developing explosive lower limb strength and high load mechanics. The stage now allows for maximal effort bilateral plyometrics for automatization of the motor pattern, but more specifically for improving kinetics in explosive movement tasks. Consideration though of landing height is needed. A key aim of the stage is to achieve a good bilateral drop jump (kinetics and kinematics) (30 cm) and single leg landing/deceleration control. Example tasks can be seen in Figures 7 to 10 and within Table 2.
Figure 7: Images of a countermovement or squat jump in place with maximal height. The removal of the box results in higher landing forces due to landing from a higher height.
Figure 10: A lateral jump from left to right limb (A) with controlled landing and stabilization (B).
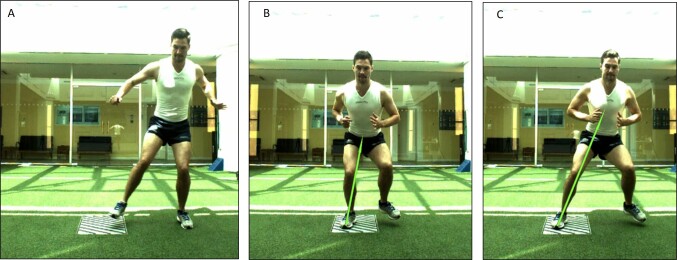
Figure 5: A sub-maximal bilateral jump (countermovement or squat) with controlled landing with a focus on eccentric acceptance and good ankle, knee and hip flexion angles. Preforming this on sand or similar surface will reduce peak ground reaction forces allowing for a longer dissipation of force.
Figure 6: Example of performing a bilateral jump onto a box, either from squat or countermovement jump. The box will allow for an increased focus on concentric power development and slow stretch-shortening cycle with the countermovement jump, while reducing the landing impact forces due to limiting the height the patient will land from.

Figure 8: A single leg drop jump in the pool which can be performed one stage earlier at an appropriate depth (around 1 m) or waist height.
Figure 9: The tuck jump performed on sand. The patient lands (A) and immediately jumps again (B) raising their legs with symmetrical heights and alignments before landing (C) and repeating the action for a series of jumps. As the patient would land from the maximal height of the jump, the landing intensity is typically higher than that of the drop jump.
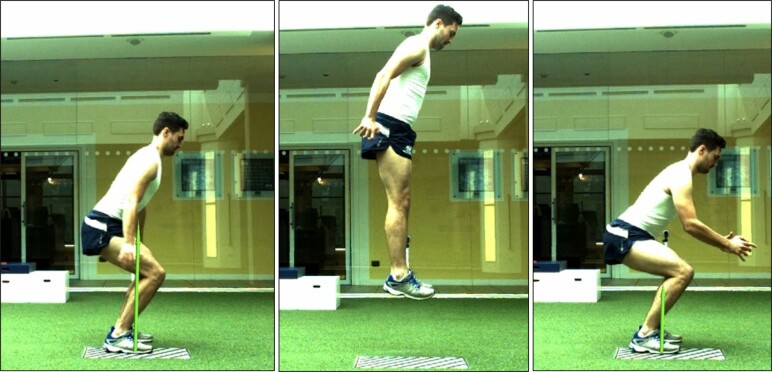
Stage 3 transitions to a greater use of unilateral plyometrics and is performed in conjunction with a multi-directional on-field coordination program (pre-planned coordination tasks). It transitions from forward and vertical unilateral plyometric to lateral and then multidirectional unilateral plyometric tasks. The key aim by the end of the stage is to have good kinematics during high speed change of direction and good single leg drop jump and hop performance (multiplanar). Ideally movement quality would be confirmed using qualitative analysis of sagittal and frontal plane kinematics, using high speed (e.g., 240Hz) camera systems.9,66 Unilateral plyometrics play a key role in supporting movement progressions and unilateral control, whilst bilateral plyometrics are used to support enhancements in neuromuscular function (strength, power and RFD) in this stage. Key aspects of the unilateral exercises are to support enhanced motor control with gradually reducing GCT to mimic sport-type tasks (e.g., progressing from 1-2 s GCT to 0.25-0.4 s GCT). Example tasks can be seen in figures 11 to 14 and within Table 2.
Figure 11: Loaded bilateral countermovement or squat jumps.
Figure 14: Use of on-field for higher intensity running and bounding exercises.
Figure 12: A lateral jump from left to right limb (A) with landing (B) and immediate jump back to the right limb (C), as opposed to just landing in which occurs during Stage 2.
Figure 13: A single leg drop jump with use of other box to challenge control and reduce final landing heights.
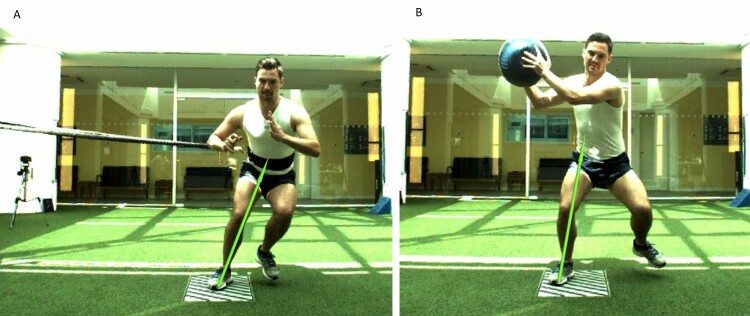
Stage 4 builds on Stage 3 and focuses on the use of maximal unilateral plyometric tasks for motor pattern automatization as well as enhancement in neuromuscular performance. Furthermore, in terms of motor patterning, a key aim of the stage as a whole is to progress to re-active movements and prepare for sport-specific training (Table 2). Creating perturbations during plyometric tasks to challenge neuromuscular control is recommended (Figure 15). A key aim of the stage is to achieve good re-active movement performance under sporting type tasks to prepare for sport-specific practice. To RTS, it is recommended to possess good movement quality during sport-type tasks and under sport-specific situations.8 It is recommended to visually assess and use video recordings of sport-specific movements (e.g., reactive cutting or change of direction at an obstacle) during on-field sessions and/or specific field based assessments.66 Patients should also have completed an on-field rehabilitation process,91 corrected muscle strength imbalances8,12,80 and restored their physical fitness.9 This of course is typically after medical clearance from sports medicine physician and/or surgeon has been allowed.8
Figure 15: A lateral jump and return with A) a rope and B) medicine ball to create perturbation and/or exaggerated lateral momentum.
SUMMARY
This clinical commentary presents a four-stage plyometric program for the ACLR athlete, which can be undertaken as part of criterion-based rehabilitation. Plyometric training should form a key component of the functional recovery process after ACLR. Used effectively, plyometrics can support enhancements in strength, movement quality, explosive neuromuscular function and athletic performance.27–30,33,34,59,60 Plyometric intensity is based on the intensity of efforts, the vertical and or horizontal momentums/velocities prior to impact, the ability of the neuromuscular system to accept those loads, the GCT, the surface compliance/environment (e.g., land or pool) and movement quality during the task. It is important to align the plyometric program to the overall ACL functional recovery program and overall functional recovery status of the athlete. There should be a gradual increase in task intensity and specificity and all tasks should be used for neuromuscular and/or motor control re-conditioning.
Conflict of interest
The authors report no conflict of interests relevant to the content of this review.
References
- Return to pre-injury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Ardern Clare L., Webster Kate E., Taylor Nicholas F., Feller Julian A. 2011The American Journal of Sports Medicine. 39(3):538–543. doi: 10.1177/0363546510384798. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- Career length and injury incidence after anterior cruciate ligament reconstruction in major league soccer players. Arundale A.J.H., Silvers-Granelli H.J., Snyder-Mackler L. Jan;2018 Orthop J Sports Med. 24;6(1):2325967117750825 doi: 10.1177/2325967117750825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knee function, strength and resumption of preinjury sports participation in young athletes following anterior cruciate ligament reconstruction. Ithurburn Matthew P., Longfellow Matthew A., Thomas Staci, Paterno Mark V., Schmitt Laura C. Mar;2019 Journal of Orthopaedic & Sports Physical Therapy. 49(3):145–153. doi: 10.2519/jospt.2019.8624. doi: 10.2519/jospt.2019.8624. [DOI] [PubMed] [Google Scholar]
- Waldén Markus, Hägglund Martin, Magnusson Henrik, Ekstrand Jan. British Journal of Sports Medicine. 12. Vol. 50. BMJ; ACL injuries in men's professional football: A 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture; pp. 744–750. [DOI] [PubMed] [Google Scholar]
- Webster Kate E., Feller Julian A. The American Journal of Sports Medicine. 11. Vol. 44. SAGE Publications; Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction; pp. 2827–2832. [DOI] [PubMed] [Google Scholar]
- Wiggins Amelia J., Grandhi Ravi K., Schneider Daniel K., Stanfield Denver, Webster Kate E., Myer Gregory D. The American Journal of Sports Medicine. 7. Vol. 44. SAGE Publications; Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis; pp. 1861–1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterno Mark V., Rauh Mitchell J., Schmitt Laura C., Ford Kevin R., Hewett Timothy E. The American Journal of Sports Medicine. 7. Vol. 42. SAGE Publications; Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport; pp. 1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckthorpe Matthew. Sports Medicine. 7. Vol. 49. Springer Science and Business Media LLC; Optimising the late-stage rehabilitation and return-to-sport training and testing process after ACL reconstruction; pp. 1043–1058. [DOI] [PubMed] [Google Scholar]
- Optimising the 'mid-stage' training and testing process after ACL reconstruction. Buckthorpe Matthew, Della Villa Francesco. 2020Sports Medicine. 50(4):657–678. doi: 10.1007/s40279-019-01222-6. doi: 10.1007/s40279-019-01222-6. [DOI] [PubMed] [Google Scholar]
- Benefits and use of aquatic therapy during rehabilitation after ACL reconstruction -a clinical commentary. Buckthorpe Matthew, Pirotti Elisa, Villa Francesco Della. Dec;2019 International Journal of Sports Physical Therapy. 14(6):978–993. doi: 10.26603/ijspt20190978. doi: 10.26603/ijspt20190978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The time has come to incorporate a greater focus on rate of force development training in the sports injury rehabilitation process. Buckthorpe M., Roi G.S. 2018Muscle Ligaments and Tendons Journal. 7(3):435–441. doi: 10.32098/mltj.03.2017.05. doi: 10.32098/mltj.03.2017.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckthorpe Matthew, La Rosa Giovanni, Villa Francesco Della. International Journal of Sports Physical Therapy. 1. Vol. 14. The Sports Physical Therapy Session; Restoring knee extensor strength after anterior cruciate ligament reconstruction: A clinical commentary; pp. 159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristiani Riccardo, Mikkelsen Christina, Forssblad Magnus, Engström Björn, Stålman Anders. Knee Surgery, Sports Traumatology, Arthroscopy. 11. Vol. 27. Springer Science and Business Media LLC; Only one patient out of five achieves symmetrical knee function 6 months after primary anterior cruciate ligament reconstruction; pp. 3461–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maximizing quadriceps strength after ACL reconstruction. Palmieri-Smith Riann M., Thomas Abbey C., Wojtys Edward M. Jul;2008 Clinics in Sports Medicine. 27(3):405–424. doi: 10.1016/j.csm.2008.02.001. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Angelozzi Massimo, Madama Marco, Corsica Cristiana, Calvisi Vittorio, Properzi Gianfranco, McCaw Steven T., Cacchio Angelo. Journal of Orthopaedic & Sports Physical Therapy. 9. Vol. 42. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction; pp. 772–780. [DOI] [PubMed] [Google Scholar]
- Kadija Marko, Knezevic Olivera M., Milovanovic Darko, Nedeljkovic Aleksandar, Mirkov Dragan M. Srpski arhiv za celokupno lekarstvo. 3-4. Vol. 144. National Library of Serbia; The effect of anterior cruciate ligament reconstruction on hamstring and quadriceps muscle function outcome ratios in male athletes; pp. 151–157. [DOI] [PubMed] [Google Scholar]
- Jordan M. J., Aagaard P., Herzog W. Scandinavian Journal of Medicine & Science in Sports. 3. Vol. 25. Wiley; Lower limb asymmetry in mechanical muscle function: A comparison between ski racers with and without ACL reconstruction; pp. e301–e309. [DOI] [PubMed] [Google Scholar]
- Landing adaptations after ACL reconstruction. Decker MICHAEL J., Torry MICHAEL R., Noonan THOMAS J., Riviere AMY, Sterett WILLIAM I. Sep;2002 Medicine & Science in Sports & Exercise. 34(9):1408–1413. doi: 10.1097/00005768-200209000-00002. doi: 10.1097/00005768-200209000-00002. [DOI] [PubMed] [Google Scholar]
- Motion alterations after anterior cruciate ligament reconstruction: Comparison of the injured and uninjured lower limbs during a single-legged jump. de Fontenay Benoît Pairot, Argaud Sebastien, Blache Yoann, Monteil Karine. Jun 1;2014 J Athl Train. 49(3):311–316. doi: 10.4085/1062-6050-49.3.11. doi: 10.4085/1062-6050-49.3.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goerger Benjamin M, Marshall Stephen W, Beutler Anthony I, Blackburn J Troy, Wilckens John H, Padua Darin A. British Journal of Sports Medicine. 3. Vol. 49. BMJ; Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: The JUMP-ACL study; pp. 188–195. [DOI] [PubMed] [Google Scholar]
- Persons with reconstructed ACL exhibit altered knee mechanics during high speed maneuvers. Lee S.-P., Chow J., Tillman M. Jan 9;2014 International Journal of Sports Medicine. 35(6):528–533. doi: 10.1055/s-0033-1358466. doi: 10.1055/s-0033-1358466. [DOI] [PubMed] [Google Scholar]
- Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Paterno Mark V, Ford Kevin R, Myer Gregory D, Heyl Rachel, Hewett Timothy E. Jul;2007 Clin J Sports Med. 17(4):258–262. doi: 10.1097/jsm.0b013e31804c77ea. doi: 10.1097/jsm.0b013e31804c77ea. [DOI] [PubMed] [Google Scholar]
- Stearns Kristen M., Pollard Christine D. The American Journal of Sports Medicine. 4. Vol. 41. SAGE Publications; Abnormal frontal plane knee mechanics during sidestep cutting in female soccer athletes after anterior cruciate ligament reconstruction and return to sport; pp. 918–923. [DOI] [PubMed] [Google Scholar]
- Hewett Timothy E., Myer Gregory D., Ford Kevin R., Heidt Robert S. Jr., Colosimo Angelo J., McLean Scott G., van den Bogert Antonie J., Paterno Mark V., Succop Paul. The American Journal of Sports Medicine. 4. Vol. 33. SAGE Publications; Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study; pp. 492–501. [DOI] [PubMed] [Google Scholar]
- Biomechanical measures during landing and postural stability predict second anterior cruciate ligament after anterior cruciate ligament reconstruction and return to sport. Paterno Mark V., Schmitt Laura C., Ford Kevin R., Rauh Mitchell J., Myer Gregory D., Huang Bin, Hewett Timothy E. Aug 11;2010 The American Journal of Sports Medicine. 38(10):1968–1978. doi: 10.1177/0363546510376053. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prospectively identified deficits in sagittal plane hip–ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Paterno Mark V., Kiefer Adam W., Bonnette Scott, Riley Michael A., Schmitt Laura C., Ford Kevin R., Myer Gregory D., Shockley Kevin, Hewett Timothy E. Dec;2015 Clinical Biomechanics. 30(10):1094–1104. doi: 10.1016/j.clinbiomech.2015.08.019. doi: 10.1016/j.clinbiomech.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Current concepts of plyometric exercise. Davies G., Riemann B.L., Manske R. 2015Int J Sports Phys Ther. 10(6):760–786. [PMC free article] [PubMed] [Google Scholar]
- The effects of plyometric training on change-of-direction ability: a meta-analysis. Asadi Abbas, Arazi Hamid, Young Warren B., de Villarreal Eduardo Sáez. Jul;2016 Int J Sports Physiol Perform. 11(5):563–573. doi: 10.1123/ijspp.2015-0694. doi: 10.1123/ijspp.2015-0694. [DOI] [PubMed] [Google Scholar]
- The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Hewett Timothy E., Lindenfeld Thomas N., Riccobene Jennifer V., Noyes Frank R. Nov;1999 The American Journal of Sports Medicine. 27(6):699–706. doi: 10.1177/03635465990270060301. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- Comparison of land-based and aquatic-based plyometric programmes during 8-week training period. Miller Michael G., Berry David C., Bullard Susan, Gilders Roger. Nov;2002 J Sport Rehabil. 11(4):268–283. doi: 10.1123/jsr.11.4.268. doi: 10.1123/jsr.11.4.268. [DOI] [Google Scholar]
- Myer Gregory D., Ford Kevin R., McLean Scott G., Hewett Timothy E. The American Journal of Sports Medicine. 3. Vol. 34. SAGE Publications; The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics; pp. 445–455. [DOI] [PubMed] [Google Scholar]
- Does plyometric training improve strength performance? A meta-analysis. Sáez-Sáez de Villarreal Eduardo, Requena Bernardo, Newton Robert U. Sep;2010 Journal of Science and Medicine in Sport. 13(5):513–522. doi: 10.1016/j.jsams.2009.08.005. doi: 10.1016/j.jsams.2009.08.005. [DOI] [PubMed] [Google Scholar]
- Muscle power and fiber characteristics following 8 weeks of plyometric training. Potteiger J.A., Lockwood R.H., Haub M.D.., et al. 1999J Strength Cond Res. 13:275–9. [Google Scholar]
- The effects of plyometric training on sprint performance: A meta-analysis. Sáez de Villarreal Eduardo, Requena Bernardo, Cronin John B. Feb;2012 J Strength Cond Res. 26(2):575–584. doi: 10.1519/jsc.0b013e318220fd03. doi: 10.1519/jsc.0b013e318220fd03. [DOI] [PubMed] [Google Scholar]
- Ebert Jay R., Edwards Peter, Yi Luke, Joss Brendan, Ackland Timothy, Carey-Smith Richard, Buelow Jens-Ulrich, Hewitt Ben. Knee Surgery, Sports Traumatology, Arthroscopy. 8. Vol. 26. Springer Science and Business Media LLC; Strength and functional symmetry is associated with post-operative rehabilitation in patients following anterior cruciate ligament reconstruction; pp. 2353–2361. [DOI] [PubMed] [Google Scholar]
- Ground reaction forces in distance running. Cavanagh Peter R., Lafortune Mario A. Jan;1980 Journal of Biomechanics. 13(5):397–406. doi: 10.1016/0021-9290(80)90033-0. doi: 10.1016/0021-9290(80)90033-0. [DOI] [PubMed] [Google Scholar]
- Hip and knee joint loading during vertical jumping and push jerking. Cleather Daniel J., Goodwin Jon E., Bull Anthony M.J. Jan;2013 Clinical Biomechanics. 28(1):98–103. doi: 10.1016/j.clinbiomech.2012.10.006. doi: 10.1016/j.clinbiomech.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colado J. C., Garcia-Masso X., González L.-M., Triplett N. T., Mayo C., Merce J. International Journal of Sports Medicine. 02. Vol. 31. Georg Thieme Verlag KG; Two-leg squat jumps in water: An effective alternative to dry land jumps; pp. 118–122. [DOI] [PubMed] [Google Scholar]
- Donoghue Orna A., Shimojo Hirofumi, Takagi Hideki. Sports Health: A Multidisciplinary Approach. 3. Vol. 3. SAGE Publications; Impact forces of plyometric exercises performed on land and in water; pp. 303–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quantifying plyometric intensity via rate of force development, knee joint, and ground reaction forces. Jensen R.L., Ebben W.P. 2007J Strength Cond Res. 21(3):763–767. doi: 10.1519/R-18735.1. [DOI] [PubMed] [Google Scholar]
- Glasgow Philip, Phillips Nicola, Bleakley Christopher. British Journal of Sports Medicine. 5. Vol. 49. BMJ; Optimal loading: Key variables and mechanisms; pp. 278–279. [DOI] [PubMed] [Google Scholar]
- Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Devita PAUL, Skelly WILLIAM A. Jan;1992 Medicine & Science in Sports & Exercise. 24(1):108–115. doi: 10.1249/00005768-199201000-00018. doi: 10.1249/00005768-199201000-00018. [DOI] [PubMed] [Google Scholar]
- Understanding and preventing acl injuries: Current biomechanical and epidemiologic considerations - update 2010. Hewett T.E., Ford K.R., Hoogenboom B.J.., et al. 2010N Am J Sports Phys Ther. 5(4):234–251. [PMC free article] [PubMed] [Google Scholar]
- Sex differences in lower extremity biomechanics during single leg landings. Schmitz Randy J., Kulas Anthony S., Perrin David H., Riemann Bryan L, Shultz Sandra J. Jul;2007 Clinical Biomechanics. 22(6):681–688. doi: 10.1016/j.clinbiomech.2007.03.001. doi: 10.1016/j.clinbiomech.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Contributions of lower extremity joints to energy dissipation during landings. Zhang SONG-NING, Bates BARRY T., Dufek JANET S. Apr;2000 Medicine & Science in Sports & Exercise. 32(4):812–819. doi: 10.1097/00005768-200004000-00014. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- Effect of plyometric training on sand versus grass on muscle soreness and jumping and sprinting ability in soccer players. Impellizzeri F M, Rampinini E, Castagna C, Martino F, Fiorini S, Wisloff U. Jun 5;2007 British Journal of Sports Medicine. 42(1):42–46. doi: 10.1136/bjsm.2007.038497. doi: 10.1136/bjsm.2007.038497. [DOI] [PubMed] [Google Scholar]
- Thein Jill M., Brody Lori Thein. Journal of Orthopaedic & Sports Physical Therapy. 1. Vol. 27. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Aquatic-based rehabilitation and training for the elite athlete; pp. 32–41. [DOI] [PubMed] [Google Scholar]
- A 'plane' explanation of anterior cruciate ligament injury mechanisms: a systematic review. Quatman Carmen E., Quatman-Yates Catherine C., Hewett Timothy E. Sep;2010 Sports Medicine. 40(9):729–746. doi: 10.2165/11534950-000000000-00000. doi: 10.2165/11534950-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Powers Christopher M. Journal of Orthopaedic & Sports Physical Therapy. 2. Vol. 40. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The influence of abnormal hip mechanics on knee injury: A biomechanical perspective; pp. 42–51. [DOI] [PubMed] [Google Scholar]
- Read Paul J., Oliver Jon L., De Ste Croix Mark B. A., Myer Gregory D., Lloyd Rhodri S. Sports Medicine. 8. Vol. 46. Springer Science and Business Media LLC; Neuromuscular risk factors for knee and ankle ligament injuries in male youth soccer players; pp. 1059–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Worp H., de Poel H., Diercks R., van den Akker-Scheek I., Zwerver J. International Journal of Sports Medicine. 08. Vol. 35. Georg Thieme Verlag KG; Jumper’s knee or lander’s knee? A systematic review of the relation between jump biomechanics and patellar tendinopathy; pp. 714–722. [DOI] [PubMed] [Google Scholar]
- Sagittal-plane trunk position, landing forces, and quadriceps electromyographic activity. Blackburn J. Troy, Padua Darin A. Mar 1;2009 J Athl Train. 44(2):174–179. doi: 10.4085/1062-6050-44.2.174. doi: 10.4085/1062-6050-44.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva Rodrigo Scattone, Ferreira Ana Luisa G., Nakagawa Theresa H., Santos José E. M., Serrão Fábio V. Journal of Orthopaedic & Sports Physical Therapy. 11. Vol. 45. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Rehabilitation of patellar tendinopathy using hip extensor strengthening and landing-strategy modification: Case report with 6-month follow-up; pp. 899–909. [DOI] [PubMed] [Google Scholar]
- The mechanical consequences of dynamic frontal plane limb alignment for non-contact ACL injury. Chaudhari Ajit M., Andriacchi Thomas P. Jan;2006 Journal of Biomechanics. 39(2):330–338. doi: 10.1016/j.jbiomech.2004.11.013. doi: 10.1016/j.jbiomech.2004.11.013. [DOI] [PubMed] [Google Scholar]
- Markolf Keith L., Burchfield Daniel M., Shapiro Matthew M., Shepard Michael F., Finerman Gerald A. M., Slauterbeck James L. Journal of Orthopaedic Research. 6. Vol. 13. Wiley; Combined knee loading states that generate high anterior cruciate ligament forces; pp. 930–935. [DOI] [PubMed] [Google Scholar]
- Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. McLean Scott G., Huang Xuemei, Su Anne, van den Bogert Antonie J. Oct;2004 Clinical Biomechanics. 19(8):828–828. doi: 10.1016/j.clinbiomech.2004.06.006. doi: 10.1016/j.clinbiomech.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Restrained tibial rotation may prevent ACL injury during landing at different flexion angles. Mokhtarzadeh Hossein, Ng Andrew, Yeow Chen Hua, Oetomo Denny, Malekipour Fatemeh, Lee Peter Vee Sin. Jan;2015 The Knee. 22(1):24–29. doi: 10.1016/j.knee.2014.09.012. doi: 10.1016/j.knee.2014.09.012. [DOI] [PubMed] [Google Scholar]
- Hewett Timothy E., Di Stasi Stephanie L., Myer Gregory D. The American Journal of Sports Medicine. 1. Vol. 41. SAGE Publications; Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction; pp. 216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster Kate E., Hewett Timothy E. Journal of Orthopaedic Research®. 10. Vol. 36. Wiley; Meta-analysis of meta-analyses of anterior cruciate ligament injury reduction training programs; pp. 2696–2708. [DOI] [PubMed] [Google Scholar]
- Sugimoto Dai, Myer Gregory D, Barber Foss Kim D, Pepin Michael J, Micheli Lyle J, Hewett Timothy E. British Journal of Sports Medicine. 20. Vol. 50. BMJ; Critical components of neuromuscular training to reduce ACL injury risk in female athletes: Meta-regression analysis; pp. 1259–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willy Richard W., Davis Irene S. Journal of Orthopaedic & Sports Physical Therapy. 9. Vol. 41. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The effect of a hip-strengthening program on mechanics during running and during a single-leg squat; pp. 625–632. [DOI] [PubMed] [Google Scholar]
- Effects of muscle strengthening on vertical jump height: A simulation study. Bobbert M.F., Van Soest A.J. 1994Med Sci Sports Exerc. 26:1012–1010. [PubMed] [Google Scholar]
- Schmidt R.A.W.C. Motor learning and performance. Human Kinetics;2005; Champaign: [Google Scholar]
- Gluteus maximus dysfunction: its relevance to athletic performance and injury and how to treat it—a clinical commentary. Buckthorpe Matthew, Stride Matthew, Villa Francesco Della. Jul;2019 International Journal of Sports Physical Therapy. 14(4):655–669. doi: 10.26603/ijspt20190655. doi: 10.26603/ijspt20190655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolpert Daniel M., Diedrichsen Jörn, Flanagan J. Randall. Nature Reviews Neuroscience. 12. Vol. 12. Springer Science and Business Media LLC; Principles of sensorimotor learning; pp. 739–751. [DOI] [PubMed] [Google Scholar]
- Recommendations for movement re-training after ACL reconstruction. Buckthorpe Matthew. Apr 11;2021 Sports Medicine. doi: 10.1007/s40279-021-01454-5. doi: 10.1007/s40279-021-01454-5. [DOI] [PubMed]
- Lipps David B., Wojtys Edward M., Ashton-Miller James A. The American Journal of Sports Medicine. 5. Vol. 41. SAGE Publications; Anterior cruciate ligament fatigue failures in knees subjected to repeated simulated pivot landings; pp. 1058–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklyn-Miller Andrew, Roberts Andrew, Hulse David, Foster John. British Journal of Sports Medicine. 6. Vol. 48. BMJ; Biomechanical overload syndrome: Defining a new diagnosis; pp. 415–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Predictors and effects of patellofemoral pain following hamstring-tendon ACL reconstruction. Culvenor Adam G., Collins Natalie J., Vicenzino Bill, Cook Jill L., Whitehead Timothy S., Morris Hayden G., Crossley Kay M. Jul;2016 Journal of Science and Medicine in Sport. 19(7):518–523. doi: 10.1016/j.jsams.2015.07.008. doi: 10.1016/j.jsams.2015.07.008. [DOI] [PubMed] [Google Scholar]
- Anterior knee pain following anterior cruciate ligament reconstruction does not increase the risk of patellofemoral osteoarthritis at 15- and 20-year follow-ups. Culvenor A.G., Øiestad B.E., Holm I., Gunderson R.B., Crossley K.M., Risberg M.A. Jan;2017 Osteoarthritis and Cartilage. 25(1):30–33. doi: 10.1016/j.joca.2016.09.012. doi: 10.1016/j.joca.2016.09.012. [DOI] [PubMed] [Google Scholar]
- Feller Julian A., Webster Kate E. The American Journal of Sports Medicine. 4. Vol. 31. SAGE Publications; A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction; pp. 564–573. [DOI] [PubMed] [Google Scholar]
- Cuoco Anthony, Tyler Timothy F. In: Physical Rehabilitation of the Injured Athlete. Andrews J.R., Harrelson G.L., Wilk K.E., editors. Elsevier; Philadelphia, PA: Plyometric training and drills; pp. 571–595. [DOI] [Google Scholar]
- Voight M., Tippett S. In: Rehabilitation Techniques in Sports Medicine. Prentice W.B., editor. St. Louis, MO; Plyometric exercise in rehabilitation. [Google Scholar]
- Voight M., Draovitch P. In: Eccentric Muscle Training in Sports and Orthopedics. Abert M., editor. Churchill Livingstone; New York: Plyometrics; p. 45. [Google Scholar]
- Literature review: Explosive/plyometric exercise. Wathen D. 1993National Strength & Conditioning Association Journal. 15(3):17–18. doi: 10.1519/0744-0049(1993)015. doi: 10.1519/0744-0049(1993)015. [DOI] [Google Scholar]
- The ten task-based progressions in rehabilitation after acl reconstruction: from post-surgery to return to play – a clinical commentary. Buckthorpe Matthew, Tamisari Antonio, Villa Francesco Della. May;2020 International Journal of Sports Physical Therapy. 15(4):1–13. doi: 10.26603/ijspt20200611. doi: 10.26603/ijspt20200611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps strength asymmetry following ACL reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Palmieri-Smith Riann M., Lepley Lindsey K. Apr 16;2015 The American Journal of Sports Medicine. 43(7):1662–1669. doi: 10.1177/0363546515578252. doi: 10.1177/0363546515578252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quadriceps and hamstring strength recovery during early neuromuscular rehabilitation after ACL hamstring-tendon autograft reconstruction. Harput Gulcan, Kilinc H. Erkan, Ozer Hamza, Baltaci Gul, Mattacola Carl G. Nov;2015 J Sport Rehabil. 24(4):398–404. doi: 10.1123/jsr.2014-0224. doi: 10.1123/jsr.2014-0224. [DOI] [PubMed] [Google Scholar]
- Rambaud Alexandre J M, Ardern Clare L, Thoreux Patricia, Regnaux Jean-Philippe, Edouard Pascal. British Journal of Sports Medicine. 22. Vol. 52. BMJ; Criteria for return to running after anterior cruciate ligament reconstruction: A scoping review; pp. 1437–1434. [DOI] [PubMed] [Google Scholar]
- Thomeé Roland, Kaplan Yonatan, Kvist Joanna, Myklebust Grethe, Risberg May Arna, Theisen Daniel, Tsepis Elias, Werner Suzanne, Wondrasch Barbara, Witvrouw Erik. Knee Surgery, Sports Traumatology, Arthroscopy. 11. Vol. 19. Springer Science and Business Media LLC; Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction; pp. 1798–1805. [DOI] [PubMed] [Google Scholar]
- Seifert Ludovic, Button Chris, Davids Keith. Sports Medicine. 3. Vol. 43. Springer Science and Business Media LLC; Key properties of expert movement systems in sport: An ecological dynamics perspective; pp. 167–178. [DOI] [PubMed] [Google Scholar]
- Task-based rehabilitation protocol for elite athletes following anterior cruciate ligament reconstruction: a clinical commentary. Herrington Lee, Myer Gregory, Horsley Ian. Nov;2013 Physical Therapy in Sport. 14(4):188–198. doi: 10.1016/j.ptsp.2013.08.001. doi: 10.1016/j.ptsp.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Buckthorpe Matthew, Della Villa Francesco, Della Villa Stefano, Roi Giulio Sergio. Journal of Orthopaedic & Sports Physical Therapy. 8. Vol. 49. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); On-field rehabilitation part 2: A 5-stage program for the soccer player focused on linear movements, multidirectional movements, soccer-specific skills, soccer-specific movements, and modified practice; pp. 570–575. [DOI] [PubMed] [Google Scholar]
- Muscle soreness, swelling, stiffness and strength loss after intense eccentric exercise. Cleak M J, Eston R G. Dec 1;1992 British Journal of Sports Medicine. 26(4):267–271. doi: 10.1136/bjsm.26.4.267. doi: 10.1136/bjsm.26.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treatment and prevention of delayed onset muscle soreness. Connolly D.A.J., Sayers S.P., McHugh M.P. 2003J Strength Cond Res. 17:197–208. doi: 10.1519/1533-4287(2003)017<0197:tapodo>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Metabolic consequences of exercise-induced muscle damage. Tee Jason C, Bosch Andrew N, Lambert Mike I. 2007Sports Medicine. 37(10):827–836. doi: 10.2165/00007256-200737100-00001. doi: 10.2165/00007256-200737100-00001. [DOI] [PubMed] [Google Scholar]
- van Melick Nicky, van Cingel Robert E H, Brooijmans Frans, Neeter Camille, van Tienen Tony, Hullegie Wim, Nijhuis-van der Sanden Maria W G. British Journal of Sports Medicine. 24. Vol. 50. BMJ; Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus; pp. 1506–1515. [DOI] [PubMed] [Google Scholar]
- Pratt Kristamarie A., Sigward Susan M. Journal of Orthopaedic & Sports Physical Therapy. 6. Vol. 47. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Knee loading deficits during dynamic tasks in individuals following anterior cruciate ligament reconstruction; pp. 411–419. [DOI] [PubMed] [Google Scholar]
- Bilateral kinematic and kinetic analysis of the squat exercise after anterior cruciate ligament reconstruction. Salem George J, Salinas Ruben, Harding F.Victor. Aug;2003 Archives of Physical Medicine and Rehabilitation. 84(8):1211–1216. doi: 10.1016/s0003-9993(03)00034-0. doi: 10.1016/s0003-9993(03)00034-0. [DOI] [PubMed] [Google Scholar]
- Sigward Susan M., Chan Ming-Sheng M., Lin Paige E., Almansouri Sara Y., Pratt Kristamarie A. Journal of Orthopaedic & Sports Physical Therapy. 9. Vol. 48. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction; pp. 713–718. [DOI] [PubMed] [Google Scholar]
- Onfield rehabilitation part 1: 4 pillars of high-quality on-field rehabilitation are restoring movement quality, physical conditioning, restoring sport-specific skills, and progressively developing chronic training load. Buckthorpe Matthew, Della Villa Francesco, Della Villa Stefano, Roi Giulio Sergio. Aug;2019 Journal of Orthopaedic & Sports Physical Therapy. 49(8):565–569. doi: 10.2519/jospt.2019.8954. doi: 10.2519/jospt.2019.8954. [DOI] [PubMed] [Google Scholar]