Abstract
Introduction
The Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) had caused an increased burden on healthcare organizations. Thus, a new strategy is needed to ensure all COVID-19 positive cases appropriately followed up , to receive the proper medical and psychological support, and to comply with the isolation guidelines. Here, we describe the characteristics and outcome of COVID-19 patients who were managed at home. In addition, we describe the differences between asymptomatic and those with mild symptoms.
Materials and methods
This is descriptive study of all COVID-19 positive cases who were monitored utilizing the home care concept.
Results
During the study period from June 8 to October 18, 2020, there was a total of 5368 COVID-19 patients who were referred to the home isolation/monitoring program. Of those, 2397 (45%) were female and 2971 (55%) were male. Of the total cases, 295 (5%) required hospital admission, 45 (1%) were admitted to zone 2 (an intermediate care facility), and the majority 5028 (94%) were continued in the home monitoring program till recovery. Of the total cases, 3137 (59%) were asymptomatic and the remaining 41% were symptomatic. Asymptomatic patients in comparison to symptomatic patients showed significant differences in relation to mean age (+ SD) of 31.5 (+ 18.6) and 46.45 (+ 17.1), respectively (P < 0.001)), gender, being healthcare workers, and the presence of significant medical conditions. However, a logistic regression analysis showed that only age and the presence of diabetes mellitus were associated with the presence of symptoms. The mean age (±SD) of those who required hospital admission was higher than those who were continued in home monitoring or cared for in zone 2.
Conclusion
The utilization of home monitoring program was effective and safe in patients who were either asymptomatic or had mild symptoms.
Keywords: SARS-CoV-2, COVID-19, Home monitoring program, Asymptomatic
1. Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) caused the current pandemic since its emergence in December 2019 in Wuhan city, China [1,2]. Three months later, initial cases of the Coronavirus Disease 19 (COVID-19) were reported in the Arabian Gulf Countries [3,4]. Similarly, the first case in the Kingdom of Saudi Arabia (KSA) was reported on March 2nd, 2020 and since then the number of COVID-19 cases increased over the following months and peaked in June–July 2020. As precautionary measures, all returning travelers to KSA were required to be quarantined in designated hotels [4]. Such quarantine was very demanding with low positivity rates. One study from KSA showed that 1.2% of 1918 returning travelers tested positive for SARS-CoV-2 [4]. Similarly, in another study from Bahrain, 0.6% of 10,449 travelers who entered quarantine facilities tested positive for SARS-CoV-2 [5]. In KSA, initial cases of SARS-CoV-2 patients were required to be admitted to the hospital irrespective of the presence or absence of symptoms [6]. Globally, COVID-19 had also resulted in a great disparity in the outcome as it relates to gender and minorities [7] in addition to the unique characteristics of COVID-19 patients in rural and urban communities [8]. At a time when the pandemic is raging in several parts of the world with overcrowded hospitals and scarce beds, many of the patients with high risk factors for progression but not sick enough to be in the hospital may benefit from home monitoring. Patients being discharged from the hospital could also be ideal candidates for such approach. Moreover, the majority of COVID-19 cases are either asymptomatic or have mild symptoms. Thus, there is a need for a new strategy to manage those patients and to ensures all COVID-19 cases appropriately followed up to receive proper medical and psychological support, and to comply with the isolation guidelines in order to prevent the spread of the infection. Thus, KSA allowed patients who did not need admission for clinical indications to be managed at home. In this study, we describe the characteristics and outcome of COVID-19 patients who were managed at home. In addition, we aimed to describe the differences between asymptomatic and those with mild symptoms.
2. Materials and methods
The study included all positive SARS-CoV-2 patients who were diagnosed in the ambulatory setting as well as in the emergency department and were deemed not needing admission at the time of the presentation. The study took place at the Johns Hopkins Aramco Healthcare (JHAH). JHAH provides medical care to about 200,000 eligible medical recipients including Saudi Aramco employees and their dependents. Home monitoring program for COVID-19 positive cases at JHAH was launched on 8th June 2020. The program was a physician-led service with a team including other physicians, case manager, registered nurses, and admin personnel. Upon the receipt of the laboratory results of SARS-CoV-2 PCR tests, these results were forwarded to the case-management admission team for assessment of the patients and to determine suitable disposition (Home Isolation, Zone 2 Facility (a designated hotel) or Hospital admission (otherwise designated as Zone 3). The case management admission team used pre-defined criteria for the disposition of patients as shown in Table 1 . In addition, patients with chronic diseases were assessed for home monitoring isolation program on case-by-case basis (Table 2 ). Home monitoring program was considered for all COVID-19 positive patients who were asymptomatic or had mild symptoms and thus deemed at low-risk of complications.
Table 1.
Summary of the Indication for the placement of COVID-19 positive cases in different locations.
| Criteria | |
|---|---|
| For home isolation |
|
| For zone 2 facility (stable patients not suitable for home isolation) |
|
| For Hospital assessment: |
|
Table 2.
A list of chronic diseases considered possibly unsuitable for home isolation as determined by the physician's decision (on case-by-case basis).
| Condition | Parameter |
|---|---|
| Uncontrolled hypertension | >160/100 mmHg |
| Uncontrolled diabetes Mellitus | HbA1c >9% and on Insulin treatment |
| Coronary artery disease (CAD) | history of CAD |
| Morbid obesity | Body mass index (BMI) >40 kg/m2 |
| Dementia | current |
| Chronic Kidney Disease (CKD) | stage 4 and 5 (estimated glomerular filtration rate (eGFR) of 15- 29, and < 15; respectively) or on dialysis |
| Liver diseases | active/cirrhosis |
| Respiratory diseases | Chronic obstructive pulmonary disease (COPD), interstitial pulmonary disease/fibrosis, Asthma requiring hospital admission within the last year |
| Heart failure | Current |
| Malignancy | Active |
| Immunodeficiency | on steroids, immunosuppressants, Human Immune Deficiency (HIV) |
Patients were regularly followed up to ensure they remained stable and suitable for home isolation. Suitability is determined by the patient's medical condition, other household members' medical conditions, whether home environment is suitable for home isolation, and the ability to download and use the required MOH smart phone applications such as Tatamman (meaning be sure) App and Tawakkalna App (an App that was developed by the National Information Center in collaboration with MOH to aid in the prevention of the spread of COVID-19). These applications help in tracking patients' symptoms and show the status of the individual in relation to the need for quarntine and immunity. The follow-up of patients was conducted via either a telephone consultation or through MyChart visit (part of the electronic medical record (EPIC)). Patients typically received a call on day 1 of enrollment into the program to assess symptoms, medical conditions, home situation, and to ensure they have downloaded relevant smart phone applications (Table 3 ).
Table 3.
A summary of daily home isolation monitoring of COVID-19 positive cases by the home isolation team.
| Activities | |
|---|---|
| Day 1 |
|
| Days 2 to 9 |
|
| Day 10 |
|
Patients’ concerns and questions were addressed, and an explanation was given on what to expect whilst under home monitoring service. Patients received a daily questionnaire via MyChart asking about their symptoms and they were contacted if they answer “yes” to any of the listed symptoms. On day 10, and if they remained asymptomatic for at least 72 h, they were discharged from the service and the patient was issued a clearance as well as his/her status was changed on the MOH database from “Active” to “Recovered”.
Statistical analysis was performed using JASP (an open-source project supported by the University of Amsterdam). We utilized descriptive analysis for demographics and patients’ clinical characteristics and these were expressed as frequencies and percentages for categorical data and mean and standard deviation (SD). Comparison of asymptomatic and mildly symptomatic disease was done using chi square (χ2) test or Fisher exact test as appropriate for categorical outcomes. Significant factors were then entered into a logistic regression analysis to determine significance. The Odds Ratio (OR) and 95% confidence intervals (95% CI) were presented. A Boxplot of the age was presented as a comparison between different groups (asymptomatic vs. symptomatic, and those who were admitted or continued in home monitoring program). A P value ≤ 0.05 was considered significant. The study was approved by the IRB of the Johns Hopkins Aramco Healthcare (IRB # 20-43).
3. Results
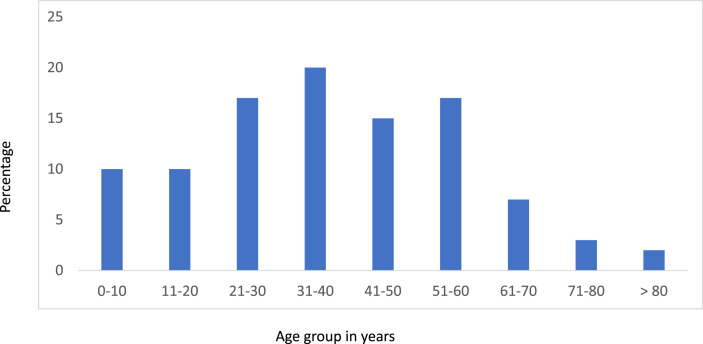
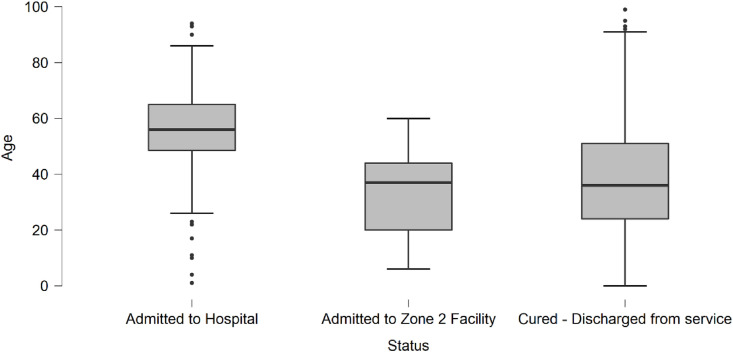
During the study period from June 8 to October 18, 2020, there was a total of 5368 COVID-19 positive cases who were referred to the home isolation/monitoring program. The mean age (±SD) was 37.7 ± 19.4 years and 2397 (45%) were female and 2971 (55%) were male. The distribution (percentage) of cases in reference to age group is shown in Fig. 1 . The majority of cases were between 21 and 60 years of age with 20% being 31-40 years and 17% being 20-31 years of age. Of the total cases, 295 (5%) required hospital admission, 45 (1%) were admitted to zone 2, and the majority 5028 (94%) continued home monitoring till clearance of infection. The mean age and SD of those who required hospital admission was 56.2 + 15.8 days and was more than those who were discharged (36.7 + 19.1) or cared for in zone 2 (33.6 + 15.5) (figure 2) (P value < 0.001) (Fig. 2 ).
Fig. 1.
The percentage of cases in reference to age group (N = 5368).
Fig. 2.
A Boxplot of the age of patients who required hospital admission, admission to zone 2 facility and those who remained in the home monitoring program till recovery.
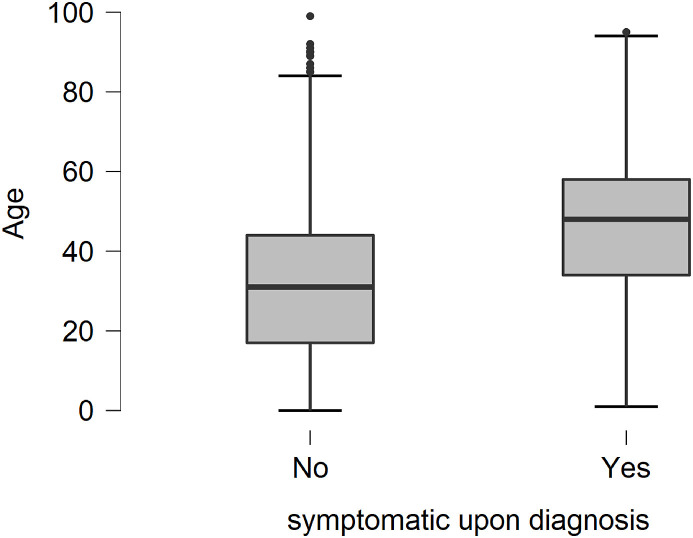
Of the total cases, 3137 (59%) were asymptomatic and the remaining 41% were symptomatic. A comparison between these two groups is shown in Table 4 . Asymptomatic patients tend to be younger with mean age (±SD) of 31.5 (18.6) and 46.45 (17.1), respectively (P < 0.001) (Fig. 3 ). In addition, there were significant differences between asymptomatic and symptomatic patients in relation to gender, being healthcare workers, and presence of significant medical conditions (Table 4). However, a logistic regression analysis showed that only age and presence of diabetes mellitus were associated with the presence of symptoms (Table 5 ).
Table 4.
A comparison between asymptomatic and symptomatic COVID-19 patients cared for as part of the home monitoring program (Data presented are number (%) except for the Mean days of home monitoring program (± SD)
| Asymptomatic N= 3147 |
Symptomatic N= 2221 |
P value |
|
|---|---|---|---|
| Number (%) | Number (%) | ||
| Female | 1368 (43.5) | 1029 (46.3) | 0.038 |
| Saudi | 2810 (89.3) | 1900 (85.5) | < 0.001 |
| Health Care Worker | 148 (4.7) | 150 (6.7) | 0.001 |
| Significant Past medical history | 219 (6.9) | 1239 (55.7) | < 0.001 |
| Cardiovascular disease | 21 (0.67) | 522 (23.5) | < 0.001 |
| Diabetes Mellitus | 12 (0.38) | 777 (34.9) | < 0.001 |
| Asthma | 42 (1.3) | 127 (5.7) | < 0.001 |
| Hospital Admission | 29 (1) | 266 (12) | < 0.001 |
| Zone 2 Facility Admission | 0 (0) | 45 (2) | < 0.001 |
| Home Isolation | 3118 (99) | 1910 (86) | < 0.001 |
| Mean and (Standard Deviation) | Mean and (Standard Deviation) | ||
| Age in years | 31.5 (18.6) | 46.45 (17.1) | < 0.001 |
| Days of home monitoring program∗ | 10.25 (1.37) | 10.21 (1.34) | 0.337 |
Data based on 3118 asymptomatic and 1910 symptomatic who stayed in the home monitoring program throughout their illnesses
Fig. 3.
A Boxplot of the age of patients who were asymptomatic or symptomatic upon diagnosis.
Table 5.
a logistic regression analysis of associated factors with symptomatic COVID-19 patients
| 95% Confidence interval |
||||
|---|---|---|---|---|
| Parameters | Odds Ratio | Lower bound | Upper bound | p |
| Age | 1.075 | 0.054 | 0.09 | < .001 |
| Health care workers (Yes versus No) | 0.786 | -0.949 | 0.468 | 0.506 |
| Cardiovascular disease (Yes versus No) | 2.46 | -0.07 | 1.87 | 0.069 |
| Diabetes (Yes versus No) | 12.097 | 1.31 | 3.676 | < .001 |
| BMI∗ (Obese versus others) | 1.37 | -0.199 | 0.828 | 0.229 |
| BMI∗ (Overweight versus others) | 0.893 | -0.594 | 0.368 | 0.645 |
| Asthmatic/chronic respiratory disease (Yes versus No) | 1.028 | -0.804 | 0.859 | 0.948 |
| Smoker (Yes versus No) | 1.231 | -0.33 | 0.745 | 0.449 |
| Nationality (non-Saudi versus Saudi) | 1.114 | -0.521 | 0.738 | 0.736 |
Based on the WHO classification, “underweight” is defined as having a body mass index (BMI, kg/m2) below 18.5, “normal” corresponds to a BMI between 18.5 and 25, “overweight” corresponds to a BMI ≥ 25, and “obese” refers to those with a BMI ≥ 30
4. Discussion
With increasing demands on healthcare system, different countries had adopted different strategies to deal with increasing number of COVID-19 cases. These strategies included deferring certain procedures and elective surgeries [9,10]. Since asymptomatic COVID-19 patients could transmit SARS-CoV-2, this had resulted in mandating social distancing, universal masking, and hand hygiene [11,12]. The initial cases in Saudi Arabia were followed by lockdowns of affected areas [3], the mandates that all positive cases to be admitted to the hospitals and that returning travelers were quarantined in designated hotels [4,6]. Subsequently, COVID-19 patients were required to be in a facility if they had been asymptomatic or had mild symptoms. This was then changed to home isolation monitoring. Here, we studied the outcome and epidemiology of patients with COVID-19 who were monitored at home.
Our data showed that of the total 5368 COVID-19 patients, 5% required hospital admission and 1% were admitted to zone 2. In another study looking at the rate of hospitalization after discharge showed 7.6% were readmitted [13]. However, these two studies are not comparable. In a smaller study of 173 patients who were monitored remotely, only 3 (1.9%) required hospitalization [14]. There are multiple advantages for home-monitoring program. It avoids the need for hospitalization and thus decreases the burden on the healthcare system and preserves hospital beds for the most severe cases. In addition, the program brings peace of mind and may alleviate the mental impact of isolation during this pandemic.
Of all the included patients, 5% required hospital admission. In a previous study of remote monitoring, 13 (0.35%) of 3701 symptomatic COVID-19 patients were admitted [15]. In another study, 2–3% of COVID-19 patients required readmission [16]. The requirement for zone 2 (less intense designated isolation facilities) was needed in 1% of the patients. The use of community dormitory-like medical facilities was tried in South Korea for those with mild symptoms [17].
The average days of home monitoring program was 10 days and in a community management of COVID-19, the length of stay was 8 days in a study from Australia [14]. In another study of 83 patients, the mean days of monitoring patients at home after discharge from emergency room was 21.8 days with an average of 14.5 daily survey responses [18]. In this study, we used the presence of comorbidities as indicator for admission at the discretion of the home monitoring team. In a previous study, a numeric prediction tool was used to screen COVID-19 patients who were cared for at home and showed higher admission rate among high-risk group of 23% vs. 1% in the lower risk group [19]. The use of an intermediate (zone 2) isolation program was ideal to decompress the hospital and provide better care than home when the latter is not suitable. The idea of using an intermediate zone was also tried to isolate and quarantine homeless individuals as well during the COVID-19 pandemic [20] especially that COVID-19 had resulted in disparity among rural and urban patients [7,8].
COVID-19 has a spectrum of presentations from asymptomatic cases to severe disease requiring intensive care unit admission [6,[21], [22], [23]]. The current study showed that 59% of the patients included in the home monitoring program were asymptomatic. In KSA, all SARS-COV-2 positive patients were initially required by the Saudi Ministry of Health to be hospitalized including asymptomatic [4]. However, giving the increased demand on healthcare, asymptomatic patients could be safely managed at home. At the beginning of the pandemic, the exact percentage of asymptomatic disease was not known [21,24]. In a previous study from KSA, 54% of 82 admitted COVID-19 patients were asymptomatic [6]. It had been shown that the prevalence of asymptomatic COVID-19 patients was related to the testing strategy and the population being tested. For example, 50% of patients in the ship cruise and nursing facilities [[25], [26], [27], [28], [29]] and only 7.9% of the 500 patients were asymptomatic [30] and another study from Saudi Arabia showed that 9.3% were asymptomatic [31]. In a meta-analysis of 28 studies, asymptomatic SARS-CoV-2 infection was 1.4%–78.3% of 6071 COVID-19 cases [32]. In the current study, diabetes mellitus was significantly associated with the presence of symptoms. In a previous study, diabetes mellitus did not predict the presence or absence of symptoms in COVID-19 patients [33] and this is different from a study from KSA that showed diabetes mellitus to be more common among asymptomatic COVID-19 patients [6] and in a study from China [34].
Home monitoring service has been very well received and appreciated by both patients and other healthcare workers, hospitalists and Zone-2 quarantine facility staff. At the patient level the program is more suited for those patients who are low risk, especially when it comes to families with young children or elderly relatives. In these situations being quarantined in a facility can be very stressful and challenging. At the institutional level this service helped decreasing the load on the hospital and Zone-2 facility, and avoided the necessity for the opening of a second Zone-2 facility and the opening of a dedicated medical floor in the current Zone-2 quarantine facility.
In conclusion, the utilization of home monitoring program was effective and safe in patients with no symptomats or had mild symptoms and those who were low risk of complications. This service is of particualr importance as the pandemic grew and affected a substanial number of patients allowing capacity and resilience of the helathcare systems.
Funding source
None.
Ethical approval
The study was approved by the Johns Hopkins Aramco Healthcare Institutional Review Board (IRB # 20-43).
Author statement
Jaffar A. Al-Tawfiq: conceptual design, data analysis, helped with the first draft of the manuscript.
Hatim Kheir: conceptual design, data collection and analysis, drafted the first manuscript.
Talal Al-Dakheel: data collection, helped with the first draft of the manuscript.
Saeed Al-Qahtani: conceptual design, helped with the first draft of the manuscript.
Hussain AlKhadra: data collection, helped with the first draft of the manuscript.
Ahlam Sarhan: data collection, helped with the first draft of the manuscript.
Maryam Bu Halaiga: data collection, helped with the first draft of the manuscript.
Rana Ibrahim: data collection, helped with the first draft of the manuscript.
All authors finalized and approved the final draft of the manuscript.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;6736:1–9. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Tawfiq J.A., Memish Z.A. COVID-19 in the eastern mediterranean region and Saudi Arabia: prevention and therapeutic strategies. Int J Antimicrob Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Tawfiq J.A., Sattar A., Al-Khadra H., Al-Qahtani S., Al-Mulhim M., Al-Omoush O., et al. Incidence of COVID-19 among returning travelers in quarantine facilities: a longitudinal study and lessons learned. Trav Med Infect Dis. 2020;38 doi: 10.1016/j.tmaid.2020.101901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdulrahman A., AlSabbagh M., AlAwadhi A., Al-Tawfiq J.A., Rabaan A.A., Atkin S., et al. Quarantining arriving travelers in the era of COVID-19: balancing the risk and benefits a learning experience from Bahrain. Trop Dis Travel Med Vaccines. 2021;7 doi: 10.1186/s40794-020-00128-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.AlJishi J.M., Alhajjaj A.H., Alkhabbaz F.L., AlAbduljabar T.H., Alsaif A., Alsaif H., et al. Clinical characteristics of asymptomatic and symptomatic COVID-19 patients in the Eastern Province of Saudi Arabia. J Infect Public Health. 2021;14:6–11. doi: 10.1016/j.jiph.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tirupathi R., Muradova V., Shekhar R., Salim S.A., Al-Tawfiq J.A., Palabindala V. COVID-19 disparity among racial and ethnic minorities in the US: a cross sectional analysis. Trav Med Infect Dis. 2020;38:101904. doi: 10.1016/j.tmaid.2020.101904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohrn M.A., Benenson R., Bush C.M., Bell T., Black C., Doan B., et al. Demographics and clinical characteristics of adult patients hospitalized due to COVID-19 in a rural/suburban integrated Health system in southcentral Pennsylvania, March through may 2020. Open Forum Infect Dis. 2021 doi: 10.1093/ofid/ofab132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welt F.G.P., Shah P.B., Aronow H.D., Bortnick A.E., Henry T.D., Sherwood M.W., et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC's interventional council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Al-Tawfiq J.A., Al-Yami S.S., Rigamonti D. Changes in healthcare managing COVID and non–COVID-19 patients during the pandemic: striking the balance. Diagn Microbiol Infect Dis. 2020;98 doi: 10.1016/j.diagmicrobio.2020.115147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fastenberg J.H., Bottalico D., Kennedy W.A., Sheikh A., Setzen M., Rodgers R., et al. Otolaryngol Neck Surg; 2020. The impact on non-COVID-19 otolaryngology patients during the pandemic! 1 commentary and insights from orbital emergencies 2 3 4. [DOI] [PubMed] [Google Scholar]
- 12.Tirupathi R., Bharathidasan K., Palabindala V., Salim S.A., Al-Tawfiq J.A. Comprehensive review of mask utility and challenges during the COVID-19 pandemic. Infezioni Med Le. 2020;28:57–63. [PubMed] [Google Scholar]
- 13.Ye S., Hiura G., Fleck E., Garcia A., Geleris J., Lee P., et al. Hospital readmissions after implementation of a discharge care program for patients with COVID-19 illness. J Gen Intern Med. 2021 doi: 10.1007/s11606-020-06340-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutchings O.R., Dearing C., Jagers D., Shaw M.J., Raffan F., Jones A., et al. Virtual Health care for community management of patients with COVID-19 in Australia: observational cohort study. J Med Internet Res. 2021;23 doi: 10.2196/21064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Annis T., Pleasants S., Hultman G., Lindemann E., Thompson J.A., Billecke S., et al. Rapid implementation of a COVID-19 remote patient monitoring program. J Am Med Inf Assoc. 2020;27:1326–1330. doi: 10.1093/jamia/ocaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medina M., Babiuch C., Card M., Gavrilescu R., Zafirau W., Boose E., et al. Home monitoring for COVID-19: posted april 18, 2020. Cleve Clin J Med. 2020;87:1–4. doi: 10.3949/CCJM.87A.CCC028. [DOI] [PubMed] [Google Scholar]
- 17.Park P.G., Kim C.H., Heo Y., Kim T.S., Park C.W., Kim C.H. Out-of-hospital cohort treatment of Coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Kor Med Sci. 2020;35 doi: 10.3346/JKMS.2020.35.E140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aalam A.A., Hood C., Donelan C., Rutenberg A., Kane E.M., Sikka N. Remote patient monitoring for ED discharges in the COVID-19 pandemic. Emerg Med J. 2021;38:229–231. doi: 10.1136/emermed-2020-210022. [DOI] [PubMed] [Google Scholar]
- 19.O'Keefe J.B., Tong E.J., Taylor T.H., O'Keefe G.A.D., Tong D.C. Use of a telemedicine risk assessment tool to predict the risk of hospitalization of 496 outpatients with COVID-19: retrospective analysis. JMIR Public Heal Surveill. 2021 doi: 10.2196/25075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fuchs J.D., Carter H.C., Evans J., Graham-Squire D., Imbert E., Bloome J., et al. Assessment of a hotel-based COVID-19 isolation and quarantine strategy for persons experiencing homelessness. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.0490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Tawfiq J.A. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19) Trav Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Mutair A., Alhumaid S., Alhuqbani W.N., Zaidi A.R.Z., Alkoraisi S., Al-Subaie M.F., et al. Clinical, epidemiological, and laboratory characteristics of mild-to-moderate COVID-19 patients in Saudi Arabia: an observational cohort study. Eur J Med Res. 2020;25:61. doi: 10.1186/s40001-020-00462-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Omari A., Alhuqbani W.N., Zaidi A.R.Z., Al-Subaie M.F., AlHindi A.M., Abogosh A.K., et al. Clinical characteristics of non-intensive care unit COVID-19 patients in Saudi Arabia: a descriptive cross-sectional study. J Infect Public Health. 2020;13:1639–1644. doi: 10.1016/j.jiph.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the achilles' heel of current strategies to control covid-19. N Engl J Med. 2020 doi: 10.1056/nejme2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McMichael T.M., Currie D.W., Clark S., Pogosjans S., Kay M., Schwartz N.G., et al. Epidemiology of covid-19 in a long-term care facility in king county, Washington. N Engl J Med. 2020 doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimball A., Hatfield K.M., Arons M., James A., Taylor J., Spicer K., et al. Asymptomatic and presymptomatic SARS-COV-2 infections in residents of a long-term care skilled nursing facility - king County, Washington, March 2020. Morb Mortal Wkly Rep. 2020;69:377–381. doi: 10.15585/MMWR.MM6913E1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arons M.M., Hatfield K.M., Reddy S.C., Kimball A., James A., Jacobs J.R., et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med. 2020 doi: 10.1056/nejmoa2008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roxby A.C., Greninger A.L., Hatfield K.M., Lynch J.B., Dellit T.H., James A., et al. Detection of SARS-CoV-2 among residents and staff members of an independent and assisted living community for older adults - seattle, Washington, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:416–418. doi: 10.15585/mmwr.mm6914e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roxby A.C., Greninger A.L., Hatfield K.M., Lynch J.B., Dellit T.H., James A., et al. Outbreak investigation of COVID-19 among residents and staff of an independent and assisted living community for older adults in seattle, Washington. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mei X., Zhang Y., Zhu H., Ling Y., Zou Y., Zhang Z., et al. Observations about symptomatic and asymptomatic infections of 494 patients with COVID-19 in Shanghai, China. Am J Infect Contr. 2020;48:1045–1050. doi: 10.1016/j.ajic.2020.06.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alsofayan Y.M., Althunayyan S.M., Khan A.A., Hakawi A.M., Assiri A.M. Clinical characteristics of COVID-19 in Saudi Arabia: a national retrospective study. J Infect Public Health. 2020;13:920–925. doi: 10.1016/j.jiph.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alene M., Yismaw L., Assemie M.A., Ketema D.B., Mengist B., Kassie B., et al. Magnitude of asymptomatic COVID-19 cases throughout the course of infection: a systematic review and meta-analysis. PloS One. 2021:16. doi: 10.1371/journal.pone.0249090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Park H.C., Kim D.H., Cho A., Kim J., Yun K sang, Kim J., et al. Clinical outcomes of initially asymptomatic patients with COVID-19: a Korean nationwide cohort study. Ann Med. 2021;53:357–364. doi: 10.1080/07853890.2021.1884744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu C., Zhou M., Liu Y., Guo T., Ou C., Yang L., et al. Characteristics of asymptomatic COVID-19 infection and progression: a multicenter, retrospective study. Virulence. 2020;11:1006–1014. doi: 10.1080/21505594.2020.1802194. [DOI] [PMC free article] [PubMed] [Google Scholar]