Abstract
Objectives
We aimed to investigate the psychological problems on people infected with SARS-CoV-2 during the pandemic.
Methods
In this living systematic review and meta-analyses, we searched seven electronic databases for cross-sectional studies and longitudinal studies on psychological problems on COVID-19 patients from Jan 1, 2020 to Oct 7, 2020. The primary outcome was prevalence of various psychological problems such as anxiety, depression, stress, insomnia, somatization, and fear. We pooled data for prevalence with their 95% confidence interval (CI) using random effect models and assessed the study quality based on the 11-item checklist recommended by the Agency for Healthcare Research and Quality.
Results
Fourty-four studies, including studies from China(35), Italy(2), Iran(2), India(1), Korea(1), Ecuador(1), Switzerland(1), Germany(1), were identified by comprising a total of 8587 completed questionnaires and 38 studies for meta-analyses. The prevalence of anxiety, depression, post-traumatic stress disorder(PTSD), insomnia, somatization, and fear in patients with COVID-19 was 16.6% (10.1%-23.1%), 37.7% (29.3%-46.2%), 41.5% (9.3%-73.7%), 68.3% (48.6%-88.0%), 36.5% (20.2%-52.8%), 47.6% (9.4%-85.7%), respectively. The prevalence of anxiety, depression, and insomnia in severe COVID-19 patients (intensive care unit inpatients) was higher than mild or clinically stable COVID-19 patients.
Limitations
A significant degree of heterogeneity in terms of populations, sampling methods, scales was noted across studies.
Conclusions
There existed high proportions of COVID-19 patients with psychological problem. The prevalence of psychological problems was closely related to the patients themselves, their surroundings and social support. It is imperative to provide ontime psychological care service for COVID-19 patients and to follow-up them for a longer period.
Keywords: COVID-19, SARS-CoV-2 infection, Meta-analyses, Psychological problems, Living systematic review, Mental health
1. Introduction
The cumulative number of people infected with SARS-CoV-2 has exceeded 100 million across the globe(WHO, 2021). Many studies have confirmed that the global pandemic has caused a wide range of psychosocial problems (Brooks et al., 2020; Galea et al., 2020; Kisely et al., 2020; Naqos and Khouchani, 2020). As for people infected by SARS-CoV-2, who have attracted the most concern, great attention must be paid to their psychological problems, regardless of asymptomatic patients, patients with mild symptoms, or clinically cured patients (Bo et al., 2020; Mazza et al., 2020; Wu et al., 2020).
Conditions and degrees vary greatly among the people infected with SARS-CoV-2. The psychological problems of COVID-19 patients are closely related to the medical and social environment. Some studies have shown that COVID-19 patients have obvious adverse mental health effects and apparent sleep difficulties after being discharged from the hospital (Cai et al., 2020; Liu et al., 2020). SARS-CoV-2 is so highly infectious that families are prone to infection in clusters. Meanwhile, COVID-19 patients whose family members also infected with COVID-19 or died of COVID-19 are more likely to suffer from depression and anxiety than other patients (Nie et al., 2020). The quality of life in COVID-19 patients who suffer from depression was significantly lower than that of non-depressed patients (Ma et al., 2020). A meta-analyses showed that more than 40% of COVID-19 patients had depression or anxiety, and nearly a third had sleep disorders (Deng et al., 2020). With a clearer understanding of SARS-CoV-2, vaccine research and development, and large-scale vaccination, is there any change in the psychological experience of people infected by SARS-CoV-2? What psychological problems do COVID-19 patients have after the pandemic? If we fail to add the time dimension to evaluate the existing research, it is difficult to answer these questions. According to previous studies, survivors of severe acute respiratory syndrome (SARS) in China reported their anxiety and/or depression symptoms and post-traumatic stress disorder (PTSD) (Cheng et al., 2004; Hong et al., 2009). We need to focus long-term attention on psychological problems caused by the COVID-19 outbreak, especially the psychological problems of SARS-CoV-2 infected.
Living systematic review is a continuously updated systematic review, which involves the latest research evidence in a timely manner (Elliott et al., 2017; Siemieniuk et al., 2020). The research method of living systematic review can be applied to any systematic review. The literature retrieval frequency and the time of integrating new information into systematic review can exert an important effect on the application of systematic review. At present, there is no designated time frequency for living systematic review updates.
In the context of COVID-19 pandemic, living research evidence update plays an essential role in better understanding the impacts of the disease. Due to the changing evidence and increasing quantity and quality, the living systematic review research paradigm has more prominent advantages. There was a report on a living systematic review on the psychological health of COVID-19 patients (Thombs et al., 2020). However, in September 2020, the team announced that it would stop updating the research on "Factors Related to the Degree or Changes of Psychological Symptoms", because cross-sectional studies related to the research problem have a rapidly growing number and lower quality, and the team was shorthanded. In other words, this living systematic review could no longer provide the latest evidence of psychological symptom changes in different groups.
Therefore, there has been no living systematic review of the psychological abnormal states of COVID-19 patients as other team has stopped updating. This research aims to explore the characteristics and related factors of psychological problems in the global COVID-19 patients by using the living systematic review method, thus may exerting a positive effect on improving the psychological health of COVID-19 patients.
2. Methods
A protocol provides the details methods of this systematic review (see supplementary file). Methods and results were formatted based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines 2020 (PRISMA) (Page et al., 2021) and Meta-analyses of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al., 2000).
2.1. Search strategy
Based on the comprehensive search of seven electronic databases, including PubMed, Embase, PsycInfo, Wanfang Data, Chongqing VIP, Sinomed, and China National Knowledge Infrastructure (CNKI), the COVID-19 mental health database was established via the NoteExpress software (V3.3.0, Beijing Aiqinhai Lezhi Technology Co., Ltd.), which included the literature on mental health studies related to COVID-19 since January 1, 2020. The search strategy for all electronic databases were shown in the supplementary file. The COVID-19 mental health database will update the search every six months. The publication language included in the study was English or Chinese. The latest version of the COVID-19 mental health database had been updated to 7th October 2020. The building of the COVID-19 mental health database can allow us to quickly find the related research papers related to this living systematic review. We conducted the research based on the data selection from this database according to inclusion and exclusion criteria. To ensure the comprehensiveness of published data, this research expanded and retrieved the reference list of literature.
2.2. Selection criteria
Inclusion Criteria
-
1)
Population: people infected by SARS-CoV-2, regardless of age, gender, race, including suspected SARS-CoV-2 infected patients without a clear nucleic acid diagnosis but with highly suspected clinical performance;
-
2)
Research design: Observational studies, including cross-sectional studies (such as epidemiological survey, questionnaire survey, online survey, etc) and longitudinal studies;
-
3)
Published or pre-print published articles, conference articles or other gray documents;
-
4)
Outcome indicators: prevalence of different psychological problems and associated factors, such as depression, anxiety, stress, insomnia, somatization, and fear.
Exclusion criteria
-
1)
Repeated studies;
-
2)
Unrepresentative or unclear sample population, which could not be determined whether the patient had SASR-CoV-2 infection;
-
3)
Letters to the editors or correspondence, without providing any original data.
2.3. Data selection and extraction
The two authors (F Dong and HL Liu) independently selected literature and extracted data and cross-checked the repetition. If two or more papers came from the same research, the most complete paper with the most detailed reports were selected. Any disagreement would be settled through adjudication based on discussion or consultation with a third member of the research group. First, the titles and abstracts of the literature were read. Then the full texts were read to determine whether they could be included in the research. If the important information involved in the research was missing or unclear, we would contact the author of the original study through emails and telephone. Data extraction table included: 1) first author, research subject, date of publication; 2) research characteristics: population category, country, research location, number of participants; 3) key factors of assessing bias and risks: response rate, research method, sampling method, survey scale, survey method, the number of effective questionnaires, survey time, survey node; 4) result indicators and result measurement data: the number of reports of anxiety, depression, stress disorder, insomnia, etc., and relevant grouping data and risk factors were also included.
2.4. Methodology quality assessment
The two authors assessed the quality of the methodology and independently cross-checked the results. In terms of the methodology quality of the cross-sectional or longitudinal studies included in the research, it was evaluated using the list of 11 items recommended by Agency for Healthcare Research and Quality(AHRQ) (Rostom et al., 2004). An item would be scored "0" if its answer was "NO" or "UNCLEAR"; otherwise, it would be "1". The quality assessment of the studies were as follows: Low quality = 0-3; Medium quality = 4-7; High quality = 8-11.
2.5. Data analysis
The prevalence rate was defined as the number of cases detected divided by sample size and standard error. To incorporate a study into the meta-analyses, two conditions have to be met: 1) it should determine the results using a recognized scale rather than self-designed questionnaires; 2) the number of result indicators or the scores of specific items in the scale should be accurately reported. The inverse variance method of DerSimonian and Laird (adjustment) (DerSimonian and Laird, 2015)was adopted to calculate the prevalence rate and the integrated prevalence of estimates and 95% confidence interval (CI). Heterogeneity between studies was expressed in I², and the results of the meta-analyses were represented by forest plot. We considered using the subgroup analysis for the different stages and degrees of patients with SARS-CoV-2 infection, and divided the patients into overall patients with no distinguishing feature, patients with mild symptoms or clinically stable patients, severe patients (patients admitted to an intensive care unit diagnosed according to the COVID-19 diagnostic and treatment protocol), discharged patients, patients with suspected infection based on their characteristics; sensitivity analysis was conducted to test the abnormal values that may occur, excluding the research that failed to clearly report the investigation time or survey time point; according to the investigation time, the studies were divided into the first stage (from January to the beginning of February 2020), the second stage (from mid-February to mid-March 2020), the third stage (after late March 2020); or according to the time point of the investigation, the studies were divided into the studies during hospitalization or just completed the definite diagnosis, and the follow-up investigation conducted when or after the patients left the hospital. Due to the existence of publication bias, Begg's test and Egger's test were used for analysis. P < 0.05 was considered to be statistically significant. Meta-analyses were performed using Stata v16.0 (StataCorp LLC). Because of the heterogeneity of the studies on patients from different countries, we used the narrative analysis to summarize the outstanding findings of the studies included in the systematic review, and presented the results with tables.
3. Results
3.1. Study selection
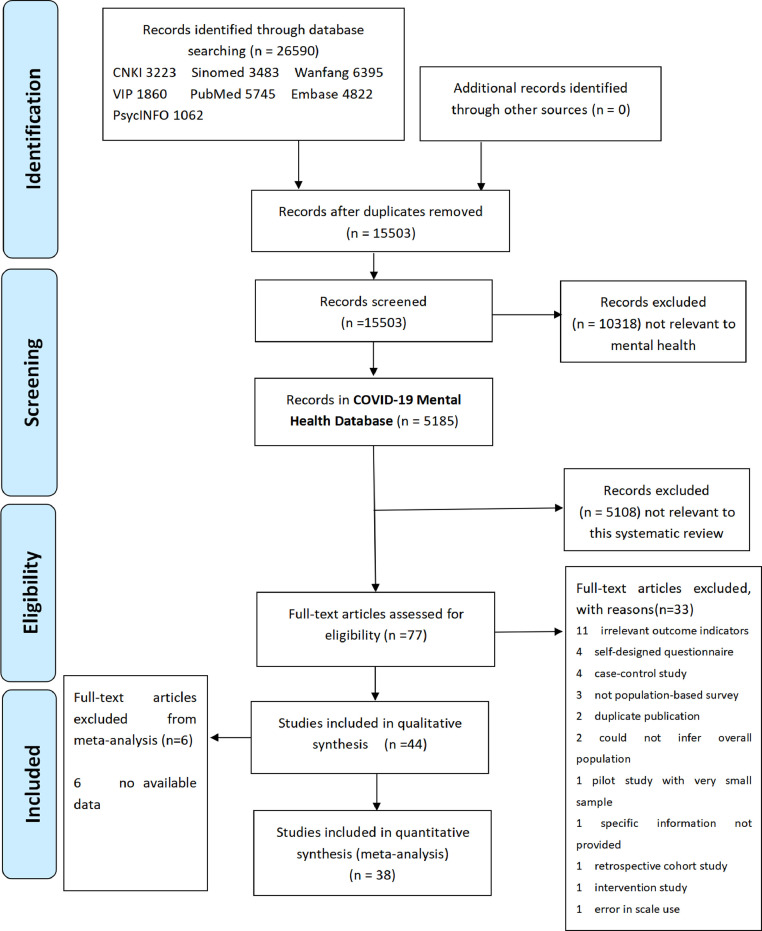
Through the preliminary screening of COVID-19 mental health database, 26,590 literature were selected. After the repetition was excluded, there were 15,503 left. After reviewing the titles and abstracts, we finally established the COVID-19 mental health database (dynamic version, Date 19/02/2021), including 5,185 papers. In this database, through browsing the titles and the abstracts, papers without obvious relations with the theme of this systematic review were excluded, then 77 articles were reviewed and classified, and 44 of them were finally included in this review.(see Fig. 1 )
Fig. 1.
Flow diagram of the selection of studies for the systematic review and meta-analyses.
3.2. Study characteristics
The systematic review included 44 studies. Table 1 provides the literature characteristics included in this review. One research (Zhang et al., 2020) conducted a longitudinal study and the other studies conducted cross-sectional studies. Forty-four studies included 8,587 completed questionnaires, and 33 (75.0%) reported response rates. Of the 44 papers, 23 (Bo et al., 2020, Cai et al., 2020, Chang and Park, 2020, Chen et al., 2020, Dai et al., 2020, Guo et al., 2020; Hu et al., 2020; Liu et al., 2020; Ma et al., 2020; Mazza et al., 2020; Nie et al., 2020; Paz et al., 2020; Qi et al., 2020; Ramezani et al., 2020; Sahoo et al., 2020; Speth et al., 2020; Tomasoni et al., 2020; Wang et al., 2020; Wesemann et al., 2020; Wu et al., 2020; Zarghami et al., 2020; Zhang et al., 2020; Zhang et al., 2020) were published in English and 21 (Cao et al., 2020; Cao et al., 2020; Chen et al., 2020; Cheng et al., 2020; Cheng et al., 2020; Gong et al., 2020; He et al., 2020; Hu et al., 2020; Li,W. et al., 2020; Li,X. et al., 2020; Lv et al., 2020; Miao et al., 2020; Qin et al., 2020; Qiu et al., 2020; Shao et al., 2020; Sun et al., 2020; Wang et al., 2020; Wu and Peng, 2020; Yuan et al., 2020; Zhang et al., 2020); Zhao et al., 2020)in Chinese. Two studies (Mazza et al., 2020; Tomasoni et al., 2020) came from Italy, two (Ramezani et al., 2020; Zarghami et al., 2020) from Iran, one (Sahoo et al., 2020) from India, one (Paz et al., 2020) from Ecuador, one (Chang and Park, 2020) from Korea, one (Speth et al., 2020) from Switzerland, one (Wesemann et al., 2020) from Germany, and the other studies (35,79.5%) from China. 20 (45.4%) of Chinese studies were from Hubei Province. Three studies (6.8%) did not report survey time; all the other studies were conducted from the end of January to the beginning of June 2020, and 30 studies (68.2%) were conducted from the end of January 2020 to March 2020. Twenty-five studies (56.8%) investigated COVID-19 patients with no distinguishing feature; two (4.5%) included discharged COVID-19 patients; two (4.5%) included severe COVID-19 patients; six (13.6%) studies included mild or clinically stable COVID-19 patients; nine (20.5%) included suspected COVID-19 patients. Twenty-three studies (52.3%) were investigated by online questionnaires issued through online applications; 17 (38.6%) were completed by researchers through face-to-face interviews with patients; two (4.5%) were conducted by researchers through telephone interview questionnaires, and five studies (11.4%) did not use the form of questionnaires. Twenty-three studies (52.3%) did not clearly state the sampling methods; nine (20.5%) used cluster sampling; nine (20.5%) used convenience sampling method; two (4.5%) used sequential sampling method, and one (2.3%) used non-probability sampling method (without defining a specific sampling method).
Table 1.
Characteristics of included studies reporting COVID-19 patients psychosocial distress during the COVID-19 pandemic
| No | First author | Year | Population | Study location | Research type | Number of participants(n) | Response rate(%) | Sampling method | Survey form | Survey tools | Completed questionnaire(n) | Gender (n, male/female) | Survey time | Survey point |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Yu Wu | 2020 | severe COVID-19 patients | Wuhan, Hubei, China |
CSS | 60 | 100.0 | convenience sampling | FIQS | HADS | 60 | 34/26 | 10/02/2020-13/02/2020 | DHQ |
| 2 | Sha Miao | 2020 | severe COVID-19 patients | Wuhan, Hubei, China |
CSS | 40 | 100.0 | NR | FIQS | HADS,AIS | 40 | 19/21 | 05/02/2020-05/03/2020 | DHQ |
| 3 | Yao-Zhi Zhang | 2020 | suspected COVID-19 patients | southwest China region | CSS | 93 | 100.0 | sequential sampling | OQS | PCL-5,PSS-10 | 93 | 51/42 | 16/02/2020-28/02/2020 | DHQ |
| 4 | Jing Yuan | 2020 | suspected COVID-19 patients | Shanghai,China | CSS | 145 | 90.6 | NR | OQS | SAS,SDS,SSRS | 145 | 64/81 | 27/01/2020-24/02/2020 | the day after the admission procedure |
| 5 | Jing Cao | 2020 | COVID-19 patients | Shenzhen,China | CSS | 148 | 94.9 | convenience sampling | FIQS | SAS,SDS | 148 | 70/78 | 02/2020 | DHQ |
| 6 | Yan-Xia Shao | 2020 | COVID-19 patients | Hubei,China | CSS | 62 | 100.0 | convenience sampling | FIQS | SASRQ | 62 | 28/34 | 19/02/2020-03/2020 | the day after the COVID-19 diagnosis |
| 7 | Lan Cheng | 2020 | suspected and mild COVID-19 patients | Shanghai,China | CSS | 139 | 88.5 | NR | FIQS | HAMA,HAMD,FoP-Q-SF | 139 | 81/58 | 26/01/2020-15/03/2020 | after a week of hospital quarantine |
| 8 | Qian Zhao | 2020 | COVID-19 patients | Wuhan, Hubei,China | CSS | 106 | 100.0 | NR | OQS | PHQ-9,GAD-7,PHQ-15 | 106 | 46/60 | 02/02/2020-16/02/2020 | DHQ |
| 9 | Xin Cai | 2020 | discharged COVID-19 patients | Shenzhen,China | CSS | 126 | 100.0 | NR | OQS | SAS,SDS,PTSD-SS | 126 | 60/66 | 01/03/2020-14/03/2020 | the day after the admission procedure |
| 10 | Shuang-Tao Sun | 2020 | COVID-19 patients | Wuhan, Hubei,China | CSS | 82 | 60.7 | cluster sampling | OQS | PCL-C | 82 | 34/48 | 21/02/2020-21/03/2020 | one month after the COVID-19 diagnosis |
| 11 | Dong Liu | 2020 | discharged COVID-19 patients | Wuhan, Hubei,China | CSS | 675 | 100.0 | cluster sampling | FIQS and OQS | PHQ-9,GAD-7,PCL-C | 675 | 371/358 | 11/04/2020-22/04/2020 | post-discharge |
| 12 | Yu-Fen Ma | 2020 | stable COVID-19 patients | Hubei,China | CSS | 770 | 98.2 | cluster sampling | OQS | PHQ-9,WHOQOL-BREF | 770 | 370/400 | 24/02/2020-08/03/2020 | DHQ |
| 13 | Xue-Dan Nie | 2020 | COVID-19 patients | Hubei, China | CSS | 78 | 95.1 | cluster sampling | FIQS | SAS,SDS | 78 | 33/45 | 14/02/2020-18/03/2020 | DHQ |
| 14 | Xin Li | 2020 | suspected COVID-19 patients | Gansu, China | CSS | 76 | 100 | sequential sampling | FIQS | HAMA,HAMD | 76 | 41/35 | 31/01/2020-22/02/2020 | DHQ |
| 15 | Yu Wang | 2020 | COVID-19 patients | Wuhan, Hubei,China | CSS | 484 | 99 | NR | OQS | ISI-7,GHQ-12,PHQ-9,GAD-7 | 484 | 241/243 | 03/2020 | before their discharge |
| 16 | Swapnajeet Sahoo | 2020 | COVID-19 patients | Chandigarh, India | CSS | 50 | 51.5 | cluster sampling | FIQS | PHQ-4 | 50 | 33/17 | 23/03/2020-05/05/2020 | the day of the admission procedure |
| 17 | U. Wesemann | 2020 | suspected and confirmed COVID-19 patients | Essen, Germany | CSS | 60 | NR | cluster sampling | QS | PCL-5,PHQ stress module | 60 | 33/27 | 08/03/2020-26/05/2020 | after hospital admission |
| 18 | Clara Paz | 2020 | suspected and confirmed COVID-19 patients | Ecuador | CSS | 759 | NR | NR | OQS | PHQ-9,GAD-7 | 759 | 386/373 | 22/03/2020-18/04/2020 | during persons under the epidemiological surveillance program |
| 19 | Arman Zarghami | 2020 | COVID-19 patients | Fasa, Iran | CSS | 82 | 72.6 | cluster sampling | FIQS and OQS | PHQ-9,GAD-7,PSS-14 | 82 | 32/50 | 18/03/2020-17/04/2020 | NR |
| 20 | Mario Gennaro Mazza # | 2020 | COVID-19 patients | Milan,Italy | CSS | 402 | NR | cluster sampling | FIQS | IES-R,PCL-5,SDS,BDI-13,STAI-Y,BDI-13,STAI-Y,MOS-SS,WHIIRS,OCI | 402 | 265/137 | 06/04/2020-09/06/2020 | at one month follow-up after hospital treatment |
| 21 | Daniele Tomasoni | 2020 | COVID-19 patients | Milan,Italy | CSS | 105 | NR | NR | FIQS | HADS | 105 | 77/28 | 04/2020-06/2020 | one to three months after hospitalization |
| 22 | Min Cheol Chang | 2020 | COVID-19 patients | Daegu, Korea | CSS | 64 | 58.9 | NR | TI | PCL-5 | 64 | 13/51 | 02/2020-04/2020 | NR |
| 23 | Mahtab Ramezani# | 2020 | COVID-19 patients | Tehran, Iran | CSS | 30 | NR | NR | QS | HADS | 30 | 17/13 | 03/2020 | NR |
| 24 | Marlene M. Speth | 2020 | COVID-19 patients | Aarau, Switzerland | CSS | 114 | NR | NR | TI | PHQ-2,GAD-2 | 114 | 52/62 | 03/03/2020-17/04/2020 | over a 6-week period |
| 25 | Jing-Long Lv# | 2020 | mild COVID-19 patients | Chongqing,China | CSS | 106 | NR | NR | FIQS | SAS,SSRS | 106 | 61/45 | 26/01/2020-02/02/2020 | two or three days after admission |
| 26 | Hao-Bin Zhang# | 2020 | COVID-19 patients | Wuhan, Hubei, China | LS | 30 | 100.0 | NR | FIQS | PHQ-9,GAD-7,ISI | 30 | 15/15 | 05/02/2020-06/03/2020 | DHQ |
| 27 | Ling-Ling Dai | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 307 | NR | NR | OQS | SAS,SDS,PSQI | 307 | 174/133 | 23/02/2020-26/02/2020 | DHQ |
| 28 | Yan-Yu Hu | 2020 | COVID-19 patients | Wuhan, Hubei,China | CSS | 85 | NR | NR | FIQS and OQS | PHQ-9,GAD-7,ISI | 85 | 43/42 | 07/03/2020-24/03/2020 | DHQ |
| 29 | Qian Guo | 2020 | mild COVID-19 patients | Shanghai, China | CSS | 103 | 100.0 | convenience sampling | OQS | PHQ-9,GAD-7,PSS-14,PCL-5 | 103 | 59/44 | 10/02/2020-28/02/2020 | NR |
| 30 | Fang Chen | 2020 | suspected COVID-19 patients | Hangzhou, Zhejiang, China | CSS | 31 | NR | NR | FIQS | PHQ-9,GAD-7,SRQ-20 | 31 | 12/19 | 28/01/2020-09/02/2020 | NR |
| 31 | Hai-Xin Bo | 2020 | stable COVID-19 patients | Wuhan, Hubei, China | CSS | 714 | 97.8 | NR | OQS | PCL-5 | 714 | 350/364 | 03/2020 | NR |
| 32 | Rong-Feng Qi | 2020 | COVID-19 patients | China | CSS | 41 | 52.4 | cluster sampling | OQS | GHQ-12,PCL-C,SAS,SDS,FS-14,SSRS,SCSQ | 41 | 45/37 | 02/2020 | NR |
| 33 | Jie Zhang | 2020 | mild COVID-19 patients | Wuhan, Hubei, China | CSS | 296 | 99.0 | convenience sampling | OQS | CD-RISC,HADS | 296 | 173/123 | 03/03/2020-05/03/2020 | NR |
| 34 | Hui Wang | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 652 | 99.2 | convenience sampling | OQS | SCL-90,CFQ,MCMQ | 652 | 346/306 | 17/02/2020-25/02/2020 | NR |
| 35 | Xue-Mei Qin | 2020 | COVID-19 patients | Changsha,Hunan, China | CSS | 112 | 100.0 | convenience sampling | OQS | SCL-90 | 112 | 59/53 | 10/02/2020 | NR |
| 36 | Xue-Qian Hu | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 356 | 100.0 | NR | QS | SCL-90 | 356 | 188/168 | 11/02/2020-08/03/2020 | seven days after admission |
| 37 | Wen-Hao Li# | 2020 | mild COVID-19 patients | Wuhan, Hubei, China | CSS | 118 | 100.0 | convenience sampling | OQS | SAS | 118 | 65/53 | 23/02/2020-27/02/2020 | NR |
| 38 | Xi-Fei He | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 214 | 100.0 | nonprobability sampling | OQS | PSQI,FoP-Q-SF,PHQ-9,DDI | 214 | 99/115 | 17/02/2020-29/02/2020 | NR |
| 39 | Shu-Yao Chou# | 2020 | suspected COVID-19 patients | Shenzhen, China | CSS | 46 | 100.0 | convenience sampling | QS | PSQI,SAS | 46 | 20/26 | 18/02/2020-25/02/2020 | NR |
| 40 | Lin Chen | 2020 | COVID-19 patients | Haozhou, Anhui, China | CSS | 50 | 100.0 | NR | OQS | SAS,SIS | 50 | 28/22 | NR | the day after the admission procedure |
| 41 | Xin-Yu Cao | 2020 | suspected COVID-19 patients | Chengdu,Sichuan, China | CSS | 65 | 100.0 | NR | FIQS | SCL-90 | 65 | 28/27 | NR | NR |
| 42 | Li Cheng | 2020 | COVID-19 patients | Hangzhou, Zhejiang, China | CSS | 76 | 100.0 | NR | OQS | SAS | 76 | 31/45 | 01/02/2020-16/02/2020 | NR |
| 43 | Dao-Min Gong | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 65 | 81.3 | NR | QS | IES-R,SSRS,SES,HADS | 65 | 33/32 | NR | NR |
| 44 | Chao-Min Wu | 2020 | COVID-19 patients | Wuhan, Hubei, China | CSS | 370 | NR | NR | OQS | PHQ-9,GAD-7 | 370 | 203/167 | 20/02/2020-15/03/2020 | during post-discharge follow-up |
Note: AIS: Athens insomnia scale; BDI-13: 13-item Beck's depression inventory;CCS: case-control study;CFQ: cognitive fusion questionnaire;CSS: cross-sectional study;DDI: the distress disclosure index;DHQ:duration of hospital quarantine;FIQS: face-to-face interview and questionnaire survey; FoP-Q-SF: fear of progression questionnaire-short form; FS-14: fatigue scale-14;GAD-7:generalized anxiety scale-7; GHQ-12: general health questionnaire-12;HADS: hospital anxiety and depression scale; HAMA:Hamilton anxiety scale;HAMD:Hamilton depression scale; HoNOS: health of the nation outcome scale;IES-R: impact of events scale-revised; ISI-7: insomnia severity index-7; LS: longitudinal study; MCMQ: medical coping modes questionnaire; MOS-SS: women's health initiative insomnia rating scale;NR: not reported;OCI: obsessive-compulsive inventory;OQS: online questionnaire survey;PCL-5:the PTSD checklist for DSM-5; PCL-C: the PTSD checklist-civilian version; PHQ:patient health questionnaire; PSQI: Pittsburgh sleep quality index;PSS:perceived stress scale; PTSD-SS: post-traumatic stress disorder self-rating scale; QS: questionnaire survey; SAS: self-rating anxiety scale; SASRQ: Stanford's acute stress response questionnaire;SCL-90:symptom checklist-90;SCSQ: simple coping style questionnaire;SDS: self-rating depression scale; SES: self-esteem scale;SIS: social impact scale;SRQ-20: the self-reporting questionnaire-20;SSRS: social support revalued scale; STAI-Y: state-trait anxiety inventory form-Y; TI: telephone interviews; WHIIRS: women's health initiative insomnia rating scale; WHOQOL-BREF: World Health Organization quality of life-brief version; # indicates that the study was not included in the meta-analyses.
3.3. Methodology quality assessment
The methodology quality scores of all studies included are shown in Table 2 . Among these studies, one (2.3%) was rated as high-quality; 33 (75.0%) as medium-quality, and 10 (22.7%) as low-quality.
Table 2.
Methodological quality assessment of included studies in this systematic review
| No | First Author | a | b | c | d | e | f | g | h | i | j | k | Score | Overall quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Yu Wu | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 2 | Sha Miao | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 3 | Yao-Zhi Zhang | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 4 | Jing Yuan | Y | N | Y | Y | Y | N | N | Y | N | Y | N | 6 | medium |
| 5 | Jing Cao | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 6 | Yan-Xia Shao | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 7 | Lan Cheng | Y | Y | Y | Y | Y | N | Y | Y | N | Y | N | 8 | high |
| 8 | Qian Zhao | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 9 | Xin Cai | Y | Y | Y | Y | Y | N | N | Y | N | N | N | 6 | medium |
| 10 | Shuang-Tao Sun | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 11 | Dong Liu | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 12 | Yu-Fen Ma | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 13 | Xue-Dan Nie | Y | N | Y | Y | Y | N | N | Y | N | Y | N | 6 | medium |
| 14 | Xin Li | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 15 | Yu Wang | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 16 | Swapnajeet Sahoo | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 17 | U. Wesemann | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 18 | Clara Paz | Y | N | Y | Y | Y | N | N | Y | N | N | N | 5 | medium |
| 19 | Arman Zarghami | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 20 | Mario Gennaro Mazza | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 21 | Daniele Tomasoni | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 22 | Min Cheol Chang | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 23 | Mahtab Ramezani | Y | Y | Y | Y | Y | N | N | N | N | N | N | 5 | medium |
| 24 | Marlene M. Speth | Y | Y | Y | Y | Y | N | N | N | N | N | N | 5 | medium |
| 25 | Jing-Long Lv | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 26 | Hao-Bin Zhang | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 27 | Ling-Ling Dai | Y | Y | Y | Y | Y | N | N | Y | N | N | N | 6 | medium |
| 28 | Yan-Yu Hu | Y | Y | Y | Y | Y | N | N | Y | N | N | N | 6 | medium |
| 29 | Qian Guo | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 30 | Fang Chen | Y | Y | Y | Y | Y | N | N | N | N | N | N | 5 | medium |
| 31 | Hai-Xin Bo | Y | N | Y | Y | Y | N | N | N | N | Y | N | 5 | medium |
| 32 | Rong-Feng Qi | Y | N | Y | Y | Y | N | N | Y | N | Y | N | 6 | medium |
| 33 | Jie Zhang | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 34 | Hui Wang | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 35 | Xue-Mei Qin | Y | Y | Y | Y | Y | N | N | N | N | N | N | 5 | medium |
| 36 | Xue-Qian Hu | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 37 | Wen-Hao Li | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 38 | Xi-Fei He | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 39 | Shu-Yao Chou | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
| 40 | Lin Chen | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 41 | Xin-Yu Cao | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 42 | Li Cheng | Y | Y | Y | Y | Y | N | N | Y | N | Y | N | 7 | medium |
| 43 | Dao-Min Gong | Y | Y | Y | Y | Y | N | N | N | N | Y | N | 6 | medium |
| 44 | Chao-Min Wu | Y | N | Y | Y | Y | N | N | N | N | N | N | 4 | low |
Note: a) Define the source of information (survey, record review); b) List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications; c) Indicate time period used for identifying patients; d) Indicate whether or not subjects were consecutive if not population-based; e) Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants; f) Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements); g) Explain any patient exclusions from analysis; h) Describe how confounding was assessed and/or controlled. i) If applicable, explain how missing data were handled in the analysis; j) Summarize patient response rates and completeness of data collection; k) Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained.
3.4. Meta-analyses
Thirty-eight studies were included in the meta-analyses, and integrated analysis was made on the prevalence rates of abnormal psychological problems, such as anxiety, depression, PTSD, insomnia, somatization, and fear.
3.4.1. Prevalence of different psychological problems
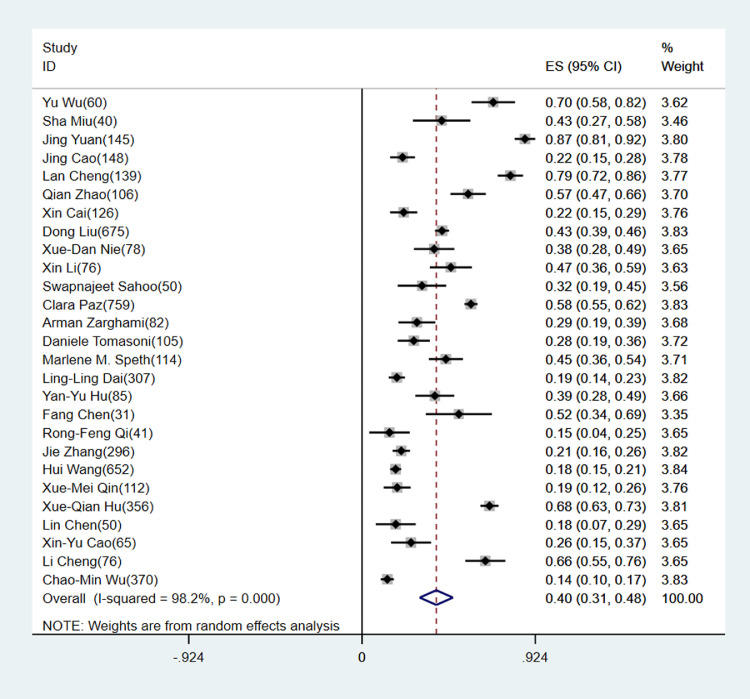
3.4.1.1. Anxiety
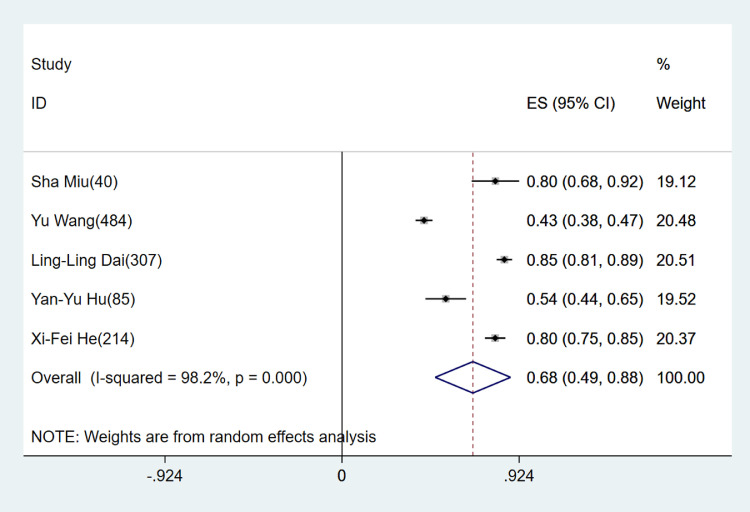
Twenty-seven studies reported the prevalence of anxiety in 5,144 patients, and the scales used to measure anxiety states included self-rating depression scale (SAS, n=8, 29.6%), generalized anxiety scale-7 (GAD-7, n=7, 25.9%), hospital anxiety and depression scale (HADS, n=4, 14.8%), symptom checklist-90 (SCL-90, n=4, 14.8%), Hamilton anxiety scale (HAMA, n=2, 7.4%), and generalized anxiety scale-2 (GAD-2, n=2, 7.4%). The meta-analyses showed that the combined prevalence was 39.6% (30.8%-48.5%, see Fig. 2 ). Among them, 11 studies reported the degree of anxiety, and the meta-analyses showed that the combined prevalence of mild anxiety was 28.1% (23.2%-33.0%), and that of above moderate anxiety was 16.6% (10.1%-23.1%).
Fig. 2.
Forest plot of anxiety prevalence rate in patients infected with SARS-CoV-2.
According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 32.7% (23.3%-42.1%), the combined prevalence of severe patients was 56.7% (29.8%-83.7%), that of patients with mild symptoms or clinically stable patients was 20.9% (16.3%-25.6%), that of discharged patients was 32.7% (12.7%-52.7%), and that of patients with suspected infection was 58.8% (42.6%-74.9%).
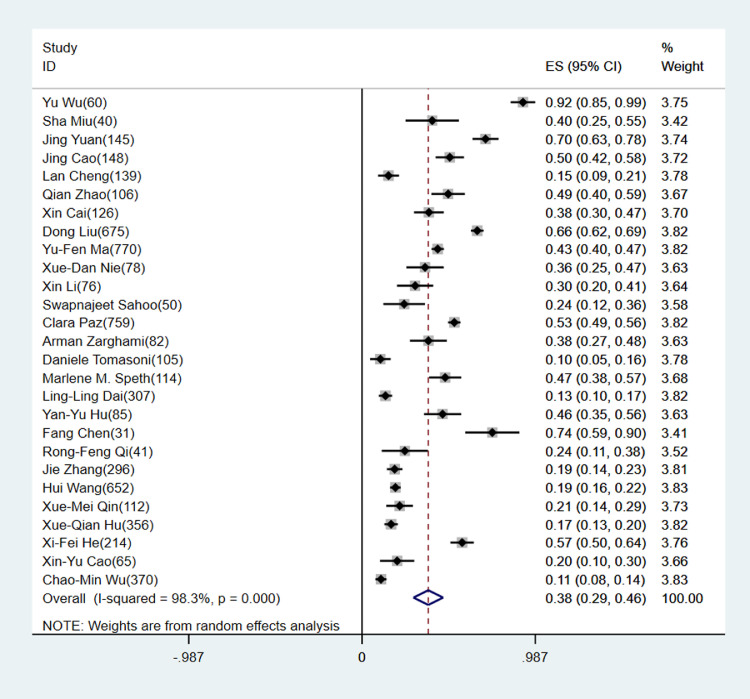
3.4.1.2. Depression
Twenty-seven studies reported the prevalence of depression in 6,002 patients. The scales used to measure depression states were patient health questionnaire-9 (PHQ-9, n=9, 33.3%), self-rating depression scale (SDS, n=6,22.2%), HADS (n=4, 14.8%), SCL-90 (n=4,14.8%), Hamilton depression scale (HAMD, n=2, 7.4%), and patient health questionnaire-2 (PHQ-2, n=2, 7.4%). The meta-analyses showed that the combined prevalence was 37.7% (29.3%-46.2%, see Fig. 3 ). Among them, 11 studies reported the degree of depression, and the meta-analyses showed that the combined prevalence of mild depression was 30.3% (23.8%-36.8%), and that of above moderate depression was 23.1% (18.0%-28.1%). According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 30.5% (23.0%-38.0%), the combined prevalence of severe patients was 66.3% (15.7%-116.9%), that of patients with mild symptoms or clinically stable patients was 30.9% (6.8%-54.9%), that of discharged patients was 52.1% (25.2%-79.1%), and that of patients with suspected infection was 43.4% (24.6%-62.2%).
Fig. 3.
Forest plot of depression prevalence rate in patients infected with SARS-CoV-2.
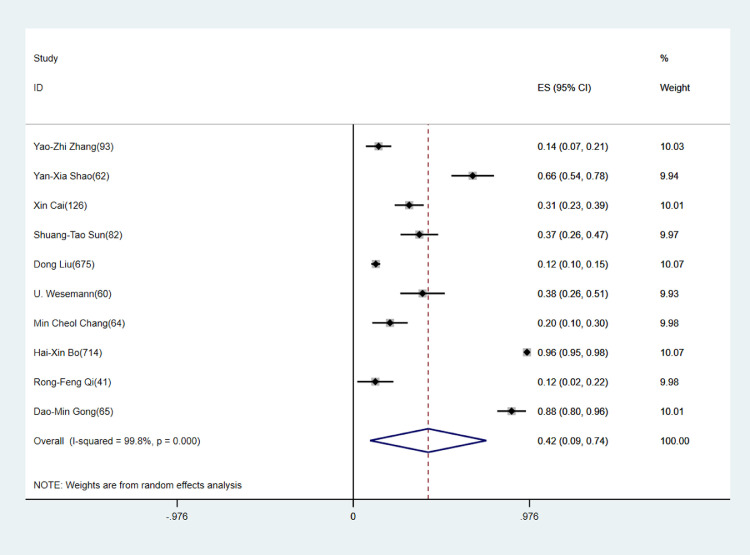
3.4.1.3. PTSD
Ten studies reported the prevalence of PTSD in 1,982 patients. The scales used to measure depression states were the PTSD checklist for DSM-5 (PCL-5, n=4, 40.0%), PTSD checklist-civilian version (PCL-C, n=3, 30.0%), impact of events scale-revised (IES-R, n=1, 10.0%), post-traumatic stress disorder self-rating scale (PTSD-SS, n=1, 10.0%), and Stanford's acute stress response questionnaire (SASRQ, n=1, 10.0%). The meta-analyses showed that the combined prevalence of PTSD was 41.5% (9.3%-73.7%, see Fig. 4 ). According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 44.6% (14.4%-74.9%), that of patients with mild symptoms or clinically stable patients was 96.2% (94.8%-97.6%), that of discharged patients was 21.3% (3.2%-39.4%), and that of patients with suspected infection was 25.6% (1.8%-49.5%).
Fig. 4.
Forest plot of post-traumatic stress disorder prevalence rate in patients infected with SARS-CoV-2.
3.4.1.4. Insomnia
Five studies reported the prevalence of insomnia in 1,130 patients. The scales used to measure depression states were insomnia severity index-7 (ISI-7, n=2, 40.0%), Pittsburgh sleep quality index (PSQI, n=2, 40.0%) and Athens insomnia scale (AIS, n=1, 20.0%). The meta-analyses showed that the prevalence of insomnia was 68.3% (48.6%-88.0%, see Fig. 5 ). According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 65.5% (42.9%-88.1%), and the combined prevalence of severe patients was 80.0% (67.6%-92.4%).
Fig. 5.
Forest plot of insomnia prevalence rate in patients infected with SARS-CoV-2.
3.4.1.5. Somatization
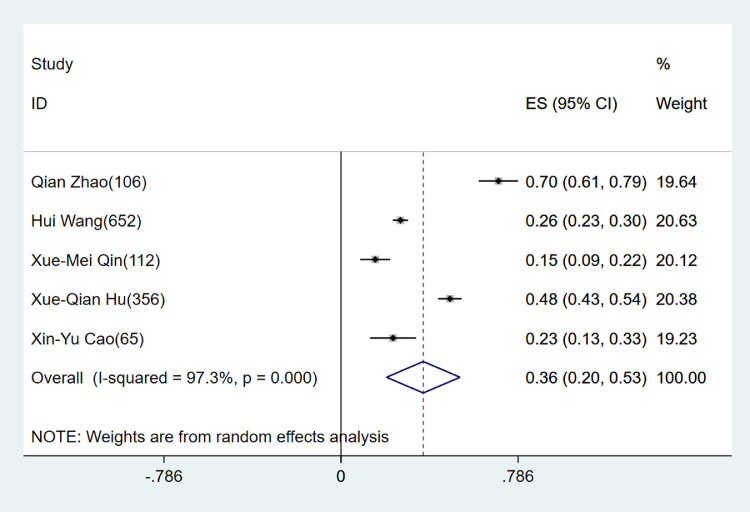
Five studies reported the prevalence of somatization in 1,291 patients. The scales used to measure depression states were SCL-90 (n=4,80.0%) and patient health questionnaire-15 (PHQ-15, n=1, 20.0%). The meta-analyses showed that the combined somatization prevalence was 36.5% (20.2%-52.8%, see Fig. 6 ). According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 39.7% (20.7%-58.8%), and that of patients with suspected infection was 23.1% (12.8%-33.3%).
Fig. 6.
Forest plot of somatization prevalence rate in patients infected with SARS-CoV-2.
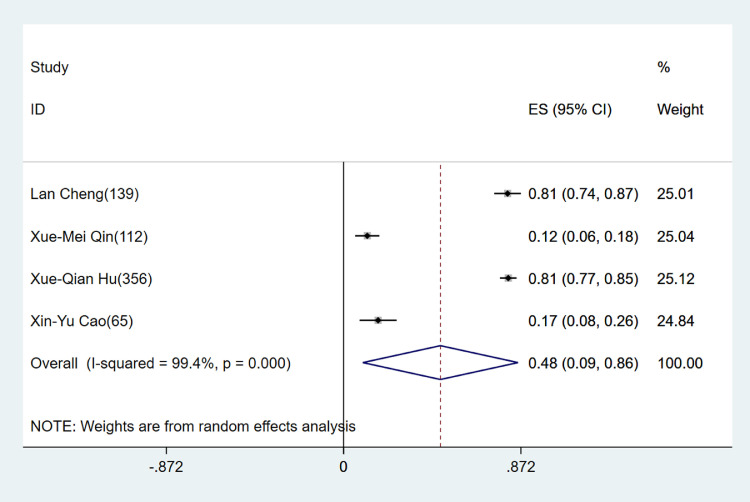
3.4.1.6. Fear
Four studies reported the prevalence of fear in 672 patients. The scales used to measure depression states were SCL-90 (n=3, 75.0%) and fear of progression questionnaire-short form (FoP-Q-SF, n=1, 25.0%). The meta-analyses showed that the combined fear prevalence was 47.6% (9.4%-85.7%, see Fig. 7 ). According to the subgroup analysis of the degree of patients' condition, the combined prevalence of overall patients with no distinguishing feature was 46.3% (-21.6%-114.2%), and that of patients with suspected infection was 48.8% (-13.5%-111.2%).
Fig. 7.
Forest plot of fear prevalence rate in patients infected with SARS-CoV-2.
3.4.2. Sensitivity analysis
After excluding studies with no reported investigation time, the first stage (from January to early February 2021): the combined prevalence of anxiety was 45.4% (29.4%-61.4%), that of depression was 42.6% (28.5%-56.7%), that of PTSD was 13.4% (7.6%-19.2%), that of insomnia was 82.7% (79.4%-86.0%), and that of somatization was 36.9% (12.0%-61.7%). The second stage (from mid-February to mid-March 2021): the combined prevalence of anxiety was 33.6% (14.2%,53.0%), that of depression was 29.5% (17.9%-41.0%), that of PTSD was 50.1% (11.8%-88.4%), that of insomnia was 47.4% (36.5%-58.3%), and that of somatization was 48.3% (43.1%-53.5%). The third stage (late March 2021): the combined prevalence of anxiety was 39.6% (29.3%-50.0%), that of depression was 39.8% (22.3%-57.4%), and that of PTSD was 24.7% (-0.7%-50.0%).
After excluding the studies with no reported investigation time point, as for patients who had just a definite diagnosis or completed the survey during their hospital stay, their combined prevalence of anxiety was 45.3% (29.5%-61.0%), that of depression was 42.2% (29.3%-55.1%), that of PTSD was 37.0% (16.4%-57.6%), and that of insomnia was 73.2% (54.2%-92.2%). As for the patients who received the follow-up investigation conducted when or after they left the hospital, their combined prevalence of anxiety was 44.9% (33.6%-56.3%), that of depression was 33.7% (11.9%-55.4%), that of PTSD was 24.0% (0.3%-47.6%), and that of insomnia was 42.8% (38.4%-47.2%).
3.4.3. Publication bias
Begg's Test was performed on the 27 anxiety-related studies included, and the results were z = 0.63, P = 0.532, and Egger's Test result was P = 0.000; Begg's Test was performed on the 27 depression-related studies included, and the results were z = 1.25, P = 0.210, and Egger's Test result P = 0.015; Begg's Test was performed on the 10 depression-related studies included, and the results were z = 1.07, P = 0.283, and Egger's Test result P = 0.010. The results showed that the funnel plot including data on prevalence was asymmetric and may not have publication bias, but other reasons for the funnel plot asymmetry may include small survey sample size, varied scales used, and varied characteristics of study subjects.
Begg's Test was performed on the five insomnia-related studies included, and the results were z = 1.22, P = 0.221, and Egger's Test result was P = 0.064; Begg's Test was performed on the five somatization-related studies included, and the results were z = 0.24, P = 0.806, and Egger's Test result P =0.721; Begg's Test was performed on the four fear-related studies included, and the results were z = 0.34, P = 0.734, and Egger's Test result P = 0.551. The results showed that the funnel plot including data on prevalence was symmetric and may not have publication bias. However, due to the small number of studies included, a more cautious attitude should be taken to the results of the study.
3.5. Qualitative synthesis of influencing factors of adverse psychological problems in COVID-19 patients
Through text analysis and integration of 44 studies, the influencing factors of adverse psychological problems of COVID-19 patients were summarized, as shown in Table 3 .
Table 3.
Influencing Factors of Adverse Psychological States of COVID-19 Patients
| Psychological state | Influencing Factors | Reference |
|---|---|---|
| Anxiety | Persistent physical symptoms: such as fatigue, palpitation, chest tightness, severe loss of taste or smell, poor sleep quality | (Cai et al., 2020; Chang and Park, 2020; Chen et al., 2020; Dai et al., 2020; Hui Wang et al., 2020; Zhang et al., 2020; Jing Cao et al., 2020; Lan Cheng et al., 2020; Cheng et al., 2020; Liu et al., 2020; Lv et al., 2020; Mazza et al., 2020; Miao et al., 2020; Nie et al., 2020; Qi et al., 2020; Speth et al., 2020; Tomasoni et al., 2020; Wu et al.,2020; Li et al., 2020; Hu et al., 2020; Yuan et al., 2020; Zarghami et al., 2020) |
| Physiological indexes: high cortisol level, high interleukin (IL) -1β level | ||
| Combined basic diseases: such as non-communicable diseases with high burden for many years | ||
| Gender: female | ||
| Marital status: divorced | ||
| Age: early recovery of patients under 60 years old had more serious infection | ||
| Educational level polarization: ① lower, junior high school and below; ② bachelor's degree and above, with fixed occupation | ||
| Cognition of disease: the degree of cognitive fusion is high, and the degree of self-perceived disease severity of COVID-19 is high | ||
| Subjective feelings: such as the sense of isolation from the outside world, feeling discriminated against, feeling ashamed of high disease, worrying about the infection by family members, worrying about whether they can be cured, worrying about the recurrence of symptoms or infecting other people | ||
| Social support: low perceived social support or utilization of support, family members or colleagues diagnosed with COVID-19, family members died due to COVID-19, family members need to be taken care of | ||
| Low mental resilience | ||
| Depression | Persistent physical symptoms: such as fatigue, palpitation, chest tightness, severe loss of taste or smell, poor sleep quality | (Cai et al., 2020; Dai et al., 2020; Guo et al., 2020; Hui Wang et al., 2020; Zhang et al., 2020; Jing Cao et al., 2020; Lan Cheng et al., 2020; Liu et al., 2020; Ma et al., 2020; Mazza et al., 2020; Miao et al., 2020; Nie et al., 2020; Qi et al., 2020; Ramezani et al., 2020; Sahoo et al., 2020; Speth et al., 2020; Tomasoni et al., 2020; Wu et al.,2020; Li et al., 2020; Hu et al., 2020; Yuan et al., 2020; Zarghami et al., 2020) |
| Physiological indexes: high cortisol level, high interleukin (IL) -1β level, high C-reactive protein level | ||
| Combined basic diseases: such as non-communicable diseases with high burden for many years | ||
| Marital status: divorced or widowed | ||
| Age: early recovery of patients under 60 years old had more serious infection | ||
| Educational level polarization: ① lower, junior high school and below; ② bachelor's degree and above, with fixed occupation | ||
| Cognition of disease: the degree of cognitive fusion is high, and the degree of self-perceived disease severity of COVID-19 is high | ||
| Subjective feelings: such as the sense of isolation from the outside world, feeling discriminated against, feeling ashamed of high disease, worrying about the infection by family members, worrying about whether they can be cured, worrying about the recurrence of symptoms or infecting other people | ||
| Social support: low perceived social support or utilization of support, family members or colleagues diagnosed with COVID-19, family members died due to COVID-19, family members need to be taken care of | ||
| Daily behavior: frequent use of social media to obtain COVID-19-related information, home isolation lifestyle after discharge | ||
| Low mental resilience | ||
| Stress | Combined basic diseases: such as non-communicable diseases with high burden for many years | (Cai et al., 2020; Gong et al., 2020; Liu et al., 2020; Mazza et al., 2020; Qi et al., 2020; Shao et al., 2020) |
| Age: advanced age | ||
| Combine with anxiety or depression | ||
| Social support: low perceived social support or utilization of support, family members or colleagues diagnosed with COVID-19, family members died due to COVID-19 | ||
| Negative coping | ||
| Insomnia | Persistent physical symptoms: such as fatigue | (He et al., 2020; Miao et al., 2020; (Hu et al., 2020); (Wang et al., 2020)) |
| Gender: female | ||
| Combine with anxiety or depression | ||
| Cognition of disease: the degree of self-perceived disease severity of COVID-19 is high | ||
| Physiological indexes:high interleukin (IL)-1β level |
4. Discussion
4.1. COVID-19 patients were experiencing various psychological problems
The results show that the COVID-19 patients with different infection degrees and stages were experiencing different degrees of anxiety, depression, PTSD, insomnia, somatization and fear. The prevalence of anxiety and depression in severe patients was significantly higher than that of other types of patients. The prevalence of anxiety and depression in patients with suspected infection was also higher than other types of patients, possibly because the time of investigation was mainly in the early stage of medical quarantine. The ambiguous diagnosis results may cause anxiety and depression (Chen et al., 2020; Paz et al., 2020; Wesemann et al., 2020). The prevalence of depression and anxiety in patients with mild or stable clinical conditions was significantly lower than that of other patients (Bo et al., 2020; Guo et al., 2020; Ma et al., 2020), which suggested that the effective control of clinical symptoms was closely related to the psychological problems of patients.
The research showed that the proportion of severe patients suffering from insomnia reached 80%, and there were obvious respiratory system and multiple organ symptoms caused by SARS-CoV-2 infection (Miao et al., 2020; Wu and Peng, 2020). Thus, it is necessary to provide drugs to improve sleep conditions for patients with severe insomnia. Patients may suffer from fatigue and chest distress due to SARS-CoV-2 infection. Therefore, the report on somatization symptoms was found in the study. The explanation of these somatization symptoms should be carried out based on physical and psychological aspects, especially after the detection of SARS-CoV-2 nucleic acid turned negative, the somatization still lasted for a long time, which can be considered to be closely related to psychological factors (Huang et al., 2021). The research showed that nearly half of the patients had strong fear, which may be related to the unclear understanding of the disease among the public, especially the SARS-CoV-2 patients, and too much negative media information could also affect the patients' cognition of COVID-19 (Garfin et al., 2020; Iqbal et al., 2020; Sahoo et al., 2020).
A systematic review of the mental health of the general population in 8 countries suggests significant differences in the prevalence of different mental disorders, such as anxiety(6.33%-50.9%), depression(14.6%-48.3%), PTSD(7%-53.8%), psychological disturbance(34.43%-38%) and stress(8.1%-81.9%) (Xiong et al., 2020). A meta-analyses on the mental conditions of the general population from communities suggests a 25%(18%-33%) complicated prevalence of anxiety (Bueno-Notivol et al., 2020). A comparison between the meta-analyses results and the survey data on the mental conditions of the general population during COVID-19 leads to the conclusion that the COVID-19 patients suffer from severer mental diseases. A meta-analyses of the prevalence of mental diseases among different population groups during the COVID-19 pandemic indicates that the complicated prevalence of depression, anxiety and sleep disorder among COVID-19 patients (42%,37%,82%) was much higher than that of the healthcare workers (25%,24%,43%) and the general population (24%,37%,34%) (Krishnamoorthy et al., 2020).
At the same time, some studies have shown that COVID-19 patients may also have delirium and other mental symptoms (Garcez et al., 2020; Parra et al., 2020), which may be related to the neurophysiological changes caused by the SARS-CoV-2 virus (Varatharaj et al., 2020; (Zhang et al., 2020)). This suggested that when patients' psychological states were assessed, we cannot ignore the neuropathological states caused by the infection virus itself. The symptoms of patients should be comprehensively evaluated and more active clinical intervention should be given if necessary (Kim and Su, 2020; Raony et al., 2020).
With the control of COVID-19 pandemic and the in-depth understanding of the SARS-CoV-2 virus, the long-term psychological impacts on COVID-19 patients should be evaluated for a longer follow-up period.
4.2. Conceptual framework and clinical implications for influencing factors of psychological problems in COVID-19 patients
Through the analysis of different psychological problems of COVID-19 patients, the study divided the influencing factors of psychological problems into the individual level, surrounding level, and social support level.
Individual level: it included physical and psychological parts, and the two exerted a mutual effect. If the COVID-19 patients had previous high burden basic diseases, or have physiological diseases in the past, they were more likely to have psychological problems. If COVID-19 patients had somatization, especially those who had been discharged from hospital or entered the recovery period, they were prone to psychological problems (Chen et al., 2020; Mazza et al., 2020; Speth et al., 2020; Tomasoni et al., 2020). A survey among the cancer patients shows that 86.5% of patients report fear of disease progression, while 67.5% suffer from anxiety, and 74.5% depression (Chen et al., 2020). A survey on the breast cancer patients in Hubei suggests that 46.2% of the patients have to adjust their therapy during the pandemic, with 56.2% reporting anxiety, 47.3% depression, 53.1% insomnia and 83.0% distress (Li et al., 2020)). Medical conditions and culture affect how patients with underlying disease cope with the mental impact of COVID-19 on them. A survey on the psychosocial impact of COVID-19 on HIV-infected youngsters in western Kenya shows that about 10% of youngsters suffer from depression, with the conditions of those aged between 20 and 24 were much worse (Dyer et al., 2020). Another survey among HIV patients in Turkey suggest that 25% of the respondents suffer from anxiety (Kuman et al., 2020). Suffering from sudden infectious diseases is a major stress event for patients. If patients have more negative emotions or are in a high-stress state before they get sick, infection with SARS-CoV-2 will become "the last straw", which will stimulate patients' strong reaction to early trauma events (Cheng et al., 2020; Gong et al., 2020; Mazza et al., 2020; Shao et al., 2020). A pilot study on the mental health of the Iraqi refugees suggested that the outbreak of COVID-19 caused the prevalence of PTSD among women to rise from 43.3% to 57.9%, and from 36.7% to 47.4% among men (Kizilhan and Noll-Hussong, 2020). This revealed that those who have suffered from grave trauma before the pandemic tend to have their conditions aggravated due to fear of being affected with SASR-CoV-2. There were great differences in the understanding of COVID-19 among patients with different cognitive levels. Research showed that the education levels of patients prone to psychological problems were polarized, which was related to the social roles of these two groups. COVID-19 has a multidimensional effect on the world. COVID-19 patients with fixed occupation and in the taking-off stage may be more likely to face uncertain factors of future life (Cai et al., 2020; Cheng et al., 2020). For such patients, attention should be focused on their personal life history and their understanding of themselves or the disease after SARS-CoV-2 infection. For the psychological problems of patients with lower education level or obvious stigma, more familiar and easy-to-understand words should be used to fully explain the disease.
Surrounding level: SARS-CoV-2 is so highly infectious that it is likely to cause the infection in clusters. COVID-19 patients may face the infection, isolation, and even death of their family members, friends, and colleagues, which had an important impact on the intimacy of each patient (Cai et al., 2020; Cao et al., 2020; Liu et al., 2020; Nie et al., 2020; Zhang et al., 2020). Family and pets that needed to be taken care of by COVID-19 patients were outside the medical quarantine space. Patients may be discriminated against when they returned to the community after treatment. If there was any positive virus detection in the recovery period, they may worry that they could infect the disease to others, which may cause intimate relationship alienation (Bagcchi, 2020; Sotgiu and Dobler, 2020; Villa et al., 2020). If the patients experienced the loss of relatives or other important things, attention should be paid to their grief response and the occurrence of abnormal grief response for more than 6 months (Goveas and Shear, 2020; Morris et al., 2020; Pirnia et al., 2020; Walsh, 2020; Zhai and Du X, 2020).
Social support level: media plays an important role in social psychology in the information age. Excessive negative information or unconfirmed information was released through We Media, which affected the correct understanding of the disease by patients (Azim et al., 2020; Looi et al., 2020; Schroyer, 2020; Yoshioka and Maeda, 2020). We should pay attention to the effective access of psychological assistance, track the patients' psychological state, and give corresponding medical help. Basic living security and necessary medical assistance should be given to patients under financial difficulties. The organization of patient mutual assistance should be established through social media, and the adaptation of COVID-19 patients in different countries or regions should be considered in combination with the localization characteristics of social psychology (Araujo et al., 2020; Krishnamoorthy et al., 2020; Lao et al., 2020; Schwartz et al., 2020). The psychological states of the patients were related to many factors. When the solution strategies are put forward for each patient's psychological problems, the relevant factors should be fully considered, such as social support and economic conditions.
4.3. Strength of this living systematic review
This research systematically reviewed the differences of psychological state among COVID-19 patients with different disease degrees for the first time, the differences of anxiety, depression, PTSD, insomnia, somatization and fear psychological problems in different investigation periods and different investigation time points, and demonstrated the psychological problems and its changes of COVID-19 patients in a multi-dimensional way.
This paper summarized this living systematic review for the first time, which will be updated continuously in the next two years. With the increasing number of related studies, it may be possible to answer the following questions, such as how different the distribution of psychological questions is in different countries or regions. This living systematic review aimed to guide the development of corresponding public health interventions and better prevent and control the mental diseases caused by the COVID-19 pandemic.
4.4. Limitations
According to the investigation time included in the study, the studies included were conducted within half a year after the outbreak of COVID-19, especially before March 2020. As this paper is the first known living systematic review, the updated version will be released as more bibliographic search results appear. Deeper analysis on the medical records (physical or mental diseases) of the SARS-CoV-2 patients will be made to explore the profound impacts of SARS-CoV-2 on patients with chronic disease or those who have suffered from previous trauma in long term. According to the severity of patients, different psychological scales were used to evaluate. For patients with a mild infection, online information collection tools could be used (Bo et al., 2020; Zhang et al., 2020). For severe patients, face-to-face interviews were used when their condition was stable(Miao et al., 2020; Wu and Peng, 2020). However, due to the lack of research into severe patients, the study on psychological problems of severe patients may have some deficiencies. Although the review has adopted more strict inclusion and exclusion criteria, the original studies included have found significant heterogeneity because of the characteristics of observational studies in epidemic situations. The source of heterogeneity was related to the following reasons: the small sample sizes of some studies were small, non-random sampling method, and different survey scales. This research only included one longitudinal study. It was found that the psychological state changes of COVID-19 patients needed long-term follow-up observation. If possible, more longitudinal studies should be carried out in the future.
5. Conclusion
There existed high proportions of COVID-19 patients with psychological problems such as anxiety, depression, PTSD, insomnia, somatization, fear. The psychological problems of the patients varied in different investigation periods and different course stages, which was closely related to the patients themselves, their surroundings and social support. Thus, it is imperative to actively carry out psychological assistance for COVID-19 patients and to observe them based on follow-up visits for a longer time.
Authorship contribution statement
Fei Dong, Jian-ping Liu designed the systematic review. Fei Dong and Hong-liang Liu participated in searching, selecting studies, data extraction and bias risk assessment. Fei Dong and Hong-liang Liu contributed to performing data analyses and first draft of manuscript. Fei Dong, Hong-liang Liu, Ning Dai, Ming Yang, Jian-ping Liu were all involved in advising and critically revising the manuscript. All authors have read and approved the final manuscript.
Declaration of Competing Interest
All authors declare that they have no conflict of interests.
Acknowledgements
Dr Fei Dong was funded by China Postdoctoral Science Foundation (2020T130009ZX). Jian-ping Liu was supported by the key program of the National Natural Science Foundation of China (No. 81830115). The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. F Dong and HL Liu had full access to the data and all authors had final responsibility for the decision to submit for publication.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.05.060.
Appendix. Supplementary materials
References
- Araujo H.M., García N.S., García-Navarro E.B. Approaching grief and death in family members of patients with COVID-19: narrative review. Enferm. Clin. 2020 doi: 10.1016/j.enfcli.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azim D., Nasim S., Kumar S., Hussain A., Jaipal M. Media on the frontline against mental health implications of COVID-19 in Pakistan. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect. Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2020 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai X., Hu X., Ekumi I.O., Wang J., An Y., Li Z., Yuan B. Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am. J. Geriatr. Psychiatry. 2020;28:1030–1039. doi: 10.1016/j.jagp.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao J., Wen M., Shi Y., Wu Y., He Q. Prevalence and factors associated with anxiety and depression in patients with Coronavirus disease 2019 (COVID-19) J. Nurs. Sci. 2020;35:15–17. [Google Scholar]
- Cao X., Tang X., Xue M., Cao J. Prevention measures, knowledge investigation and psychological status analysis of patients with suspected coronavirus disease 2019. J. Chongqing Med. Univ. 2020;45:894–898. [Google Scholar]
- Chang M.C., Park D. Vol. 8. Healthcare; (Basel): 2020. (Incidence of Post-Traumatic Stress Disorder After Coronavirus Disease). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Wang X.D., Zhu K.K., Hu J.B. Investigation of the psychological status of suspected patients during the Coronavirus disease 2019 epidemic. Medicine (Baltimore) 2020;99:e22260. doi: 10.1097/MD.0000000000022260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Wu Q., Jiang H., Zhang H., Peng J., Hu J., Chen M., Zhong Y., Xie C. Fear of disease progression and psychological stress in cancer patients under the outbreak of COVID-19. Psychooncology. 2020 doi: 10.1002/pon.5451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Ma M., Song H., Yang M., Wang W., Zhang T. Study on the correlation between stigma and anxiety in hospitalized patients with coronavirus disease 2019. Chin. J. Nurs. 2020;55:601–602. [Google Scholar]
- Cheng L., Zhang Y., Sha Y., Fu Y., Wang H. Analysis of negative emotion and influencing factors of patients with Novel coronavirus pneumonia during isolation treatment. China J. Health Psychol. 2020;28:1833–1837. [Google Scholar]
- Cheng L., Zheng L., Yan S., Fan X. Anxiety status and related factors in patients with coronavirus disease 2019. Zhejiang Med. J. 2020;42:315–317. [Google Scholar]
- Cheng S.K., Wong C.W., Tsang J., Wong K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34:1187–1195. doi: 10.1017/s0033291704002272. [DOI] [PubMed] [Google Scholar]
- Dai L.L., Wang X., Jiang T.C., Li P.F., Wang Y., Wu S.J., Jia L.Q., Liu M., An L., Cheng Z. Anxiety and depressive symptoms among COVID-19 patients in Jianghan Fangcang Shelter Hospital in Wuhan, China. PLOS ONE. 2020;15 doi: 10.1371/journal.pone.0238416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2020 doi: 10.1111/nyas.14506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DerSimonian R., Laird N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials. 2015;45:139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer J., Wilson K., Badia J., Agot K., Neary J., Njuguna I., Kibugi J., Healy E., Beima-Sofie K., John-Stewart G., Kohler P. The psychosocial effects of the COVID-19 pandemic on youth living with HIV in Western Kenya. AIDS Behav. 2020:1–5. doi: 10.1007/s10461-020-03005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott J.H., Synnot A., Turner T., Simmonds M., Akl E.A., McDonald S., Salanti G., Meerpohl J., MacLehose H., Hilton J., Tovey D., Shemilt I., Thomas J. Living systematic review: 1. Introduction-the why, what, when, and how. J. Clin. Epidemiol. 2017;91:23–30. doi: 10.1016/j.jclinepi.2017.08.010. [DOI] [PubMed] [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Garcez F.B., Aliberti M., Poco P., Hiratsuka M., Takahashi S.F., Coelho V.A., Salotto D.B., Moreira M., Jacob-Filho W., Avelino-Silva T.J. Delirium and Adverse outcomes in hospitalized patients with COVID-19. J. Am. Geriatr. Soc. 2020 doi: 10.1111/jgs.16803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychol. 2020;39:355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong D., Hu Y., Jiang L., Wu L. Investigation of the impact of event in patients with coronavirus disease 2019 and its analysis of the related factors. Chin. J. Nurs. 2020;55:590–592. [Google Scholar]
- Goveas J.S., Shear M.K. Grief and the COVID-19 pandemic in older adults. Am. J. Geriatr. Psychiatry. 2020;28:1119–1125. doi: 10.1016/j.jagp.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Fromson J.A., Xu Y., Liu X., Xu H., Zhang T., Lu Y., Chen X., Hu H., Tang Y., Yang S., Zhou H., Wang X., Chen H., Wang Z., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He X., Liu Q., Yang J., Wang Z., Zhang L., Ye Y., Tang Z., Zeng T. The sleep quality of patients with coronavirus disease 2019 in fangcang hospital and its related influencing factors. Chin. Clin. Nurs. 2020;12:190–195. [Google Scholar]
- Hong X., Currier G.W., Zhao X., Jiang Y., Zhou W., Wei J. Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen. Hosp. Psychiatry. 2009;31:546–554. doi: 10.1016/j.genhosppsych.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu X., Ma D., Liu G., Zhang S., Wang W. Investigation of psychological status and nursing countermeasures for patients with coronavirus disease 2019 in Fangcang hospital. J. Qilu Nurs. 2020;26:116–117. [Google Scholar]
- Hu Y., Chen Y., Zheng Y., You C., Tan J., Hu L., Zhang Z., Ding L. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., Kang L., Guo L., Liu M., Zhou X., Luo J., Huang Z., Tu S., Zhao Y., Chen L., Xu D., Li Y., Li C., Peng L., Li Y., Xie W., Cui D., Shang L., Fan G., Xu J., Wang G., Wang Y., Zhong J., Wang C., Wang J., Zhang D., Cao B. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal Y., Al A.M., Albrahim S., Latoo J., Kumar R., Haddad P.M. Psychiatric presentation of patients with acute SARS-CoV-2 infection: a retrospective review of 50 consecutive patients seen by a consultation-liaison psychiatry team. BJPsych Open. 2020;6:e109. doi: 10.1192/bjo.2020.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.W., Su K.P. Using psychoneuroimmunity against COVID-19. Brain Behav. Immun. 2020;87:4–5. doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kizilhan J.I., Noll-Hussong M. Psychological impact of COVID-19 in a refugee camp in Iraq. Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13142. [DOI] [PubMed] [Google Scholar]
- Krishnamoorthy Y., Nagarajan R., Saya G.K., Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuman T.Ö., PullukÇu H., Erdem H.A., Kurtaran B., TaŞbakan S.E., TaŞbakan M. COVID-19 related anxiety in people living with HIV: an online cross-sectional study. Turk. J. Med. Sci. 2020 doi: 10.3906/sag-2006-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lao Y., Jiang Y., Luo X., Liu X. Focus on the depressive symptoms in COVID-19 patients: Perspective based on a rapid meta-analysis. Asian J. Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Cesar A.S., Feng H., Wang L., Zhang P., Xu Y., Tan Y., Liu Z., Du B., Lan M., Yang Q., Yao F., Tu Y., Sun S., Li X., Chen C. Patient-reported outcomes of patients with breast cancer during the COVID-19 outbreak in the epicenter of China: a cross-sectional survey study. Clin. Breast Cancer. 2020;20:e651–e662. doi: 10.1016/j.clbc.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Huang Y., Wang C., Wang C. Anxiety investigation among COVID-19 patients in a cabin hospital. China J. Health Psychol. 2020;28:1191–1194. [Google Scholar]
- Li X., Dai T., Wang H., Shi J., Yuan W., Li J., Chen L., Zhang T., Zhang S., Kong Y., Yue N., Shi H., He Y., Hu H., Liu F., Yang C. Clinical analysis of suspected COVID-19 patients with anxiety and depression. J. Zhejiang Univ. (Med. Sci.) 2020;49:203–208. doi: 10.3785/j.issn.1008-9292.2020.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D., Baumeister R.F., Veilleux J.C., Chen C., Liu W., Yue Y., Zhang S. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiat. Res. 2020;292 doi: 10.1016/j.psychres.2020.113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Looi J.C., Allison S., Bastiampillai T., Maguire P. Fire, disease and fear: effects of the media coverage of 2019-2020 Australian bushfires and novel coronavirus 2019 on population mental health. Aust. N. Z. J. Psychiatry. 2020;54:938–939. doi: 10.1177/0004867420931163. [DOI] [PubMed] [Google Scholar]
- Lv J., Wan S., Yi Q., Liao X., Zhong H., Xiang Y. Correlation analysis of anxiety and social support of severe acute respiratory syndrome coronavirus 2-infected patients. Hainan Med. J. 2020;31:2025–2027. [Google Scholar]
- Ma Y.F., Li W., Deng H.B., Wang L., Wang Y., Wang P.H., Bo H.X., Cao J., Wang Y., Zhu L.Y., Yang Y., Cheung T., Ng C.H., Wu X., Xiang Y.T. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J. Affect. Disord. 2020;275:145–148. doi: 10.1016/j.jad.2020.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M.G., De Lorenzo R., Conte C., Poletti S., Vai B., Bollettini I., Melloni E., Furlan R., Ciceri F., Rovere-Querini P., Benedetti F. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miao S., Luo X., Wang Z., Lv J., Liu X., Li C., Jia Z., Tang J., Xiang M. Analysis of psychological status and influencing factors of COVID-19 patients in the intensive care unit. Acta Acad. Med. Xuzhou. 2020;40:612–616. [Google Scholar]
- Morris S.E., Moment A., Thomas J.D. Caring for bereaved family members during the COVID-19 pandemic: before and after the death of a patient. J. Pain Symptom Manag. 2020;60:e70–e74. doi: 10.1016/j.jpainsymman.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naqos N., Khouchani M. The study of physical and mental distress among cancer patients during the COVID-19 epidemic. Ann. Oncol. 2020;31:S1028–S1029. [Google Scholar]
- Nie X.D., Wang Q., Wang M.N., Zhao S., Liu L., Zhu Y.L., Chen H. Anxiety and depression and its correlates in patients with coronavirus disease 2019 in Wuhan. Int. J. Psychiatry Clin. Pract. 2020:1–6. doi: 10.1080/13651501.2020.1791345. [DOI] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parra A., Juanes A., Losada C.P., Álvarez-Sesmero S., Santana V.D., Martí I., Urricelqui J., Rentero D. Psychotic symptoms in COVID-19 patients. A retrospective descriptive study. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paz C., Mascialino G., Adana-Díaz L., Rodríguez-Lorenzana A., Simbaña-Rivera K., Gómez-Barreno L., Troya M., Paez M.I., Cárdenas J., Gerstner R.M., Ortiz-Prado E. Behavioral and sociodemographic predictors of anxiety and depression in patients under epidemiological surveillance for COVID-19 in Ecuador. PLoS One. 2020;15 doi: 10.1371/journal.pone.0240008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirnia B., Dezhakam H., Pirnia K., Malekanmehr P., Rezaeian M. Grief of COVID-19 is a mental contagion, first family suicide in Iran. Asian J. Psychiatr. 2020;54 doi: 10.1016/j.ajp.2020.102340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi R., Chen W., Liu S., Thompson P.M., Zhang L.J., Xia F., Cheng F., Hong A., Surento W., Luo S., Sun Z.Y., Zhou C.S., Li L., Jiang X., Lu G.M. Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv. 2020 [Google Scholar]
- Qin X., Shu K., Wang M., Chen W., Huang M., Yang A., Zhou Y., Zhang Y., Ju Y., Liu J. Mental health status of patients with coronavirus disease 2019 in Changsha. J. Cent. South Univ. (Med. Sci.) 2020;45:657–664. doi: 10.11817/j.issn.1672-7347.2020.200347. [DOI] [PubMed] [Google Scholar]
- Qiu S., Zhong J., Zhi M., Zhou Y., Mo L., Zeng J., Chen J., Zhou F., Liu D. Analysis of sleep quality and anxiety of suspected novel coronavirus pneumonia cases during quarantine treatment. Lingnan J. Emerg. Med. 2020;25:118–121. [Google Scholar]
- Ramezani M., Simani L., Karimialavijeh E., Rezaei O., Hajiesmaeili M., Pakdaman H. The role of anxiety and cortisol in outcomes of patients with COVID-19. Basic Clin. Neurosci. 2020;11:179–184. doi: 10.32598/bcn.11.covid19.1168.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raony Í., de Figueiredo C.S., Pandolfo P., Giestal-de-Araujo E., Oliveira-Silva B.P., Savino W. Psycho-Neuroendocrine-Immune Interactions in COVID-19: potential impacts on mental health. Front. Immunol. 2020;11:1170. doi: 10.3389/fimmu.2020.01170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostom A., Dubé C., Cranney A. 2004. Celiac Disease. Rockville (MD): Agency for Healthcare Research and Quality (US)(Evidence Reports/Technology Assessments, No. 104.) [Google Scholar]
- Sahoo S., Mehra A., Dua D., Suri V., Malhotra P., Yaddanapudi L.N., Puri G.D., Grover S. Psychological experience of patients admitted with SARS-CoV-2 infection. Asian J. Psychiatry. 2020;54 doi: 10.1016/j.ajp.2020.102355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroyer D. Media effects on individual worldview and wellness for long term care residents amid the COVID-19 virus. Gerontologist. 2020 doi: 10.1093/geront/gnaa095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz R., Sinskey J.L., Anand U., Margolis R.D. Addressing postpandemic clinician mental health: a narrative review and conceptual framework. Ann. Intern. Med. 2020;173:981–988. doi: 10.7326/M20-4199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y., Wang Q., Hu G., Sun W. Survey of acute stress disorder in patients with coronavirus disease 2019. J. Third Milit. Med. Univ. 2020;42:1817–1822. [Google Scholar]
- Siemieniuk R.A., Bartoszko J.J., Ge L., Zeraatkar D., Izcovich A., Kum E., Pardo-Hernandez H., Rochwerg B., Lamontagne F., Han M.A., Liu Q., Agarwal A., Agoritsas T., Chu D.K., Couban R., Darzi A., Devji T., Fang B., Fang C., Flottorp S.A., Foroutan F., Ghadimi M., Heels-Ansdell D., Honarmand K., Hou L., Hou X., Ibrahim Q., Khamis A., Lam B., Loeb M., Marcucci M., McLeod S.L., Motaghi S., Murthy S., Mustafa R.A., Neary J.D., Qasim A., Rada G., Riaz I.B., Sadeghirad B., Sekercioglu N., Sheng L., Sreekanta A., Switzer C., Tendal B., Thabane L., Tomlinson G., Turner T., Vandvik P.O., Vernooij R.W., Viteri-García A., Wang Y., Yao L., Ye Z., Guyatt G.H., Brignardello-Petersen R. Drug treatments for covid-19: living systematic review and network meta-analysis. BMJ. 2020:m2980. doi: 10.1136/bmj.m2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotgiu G., Dobler C.C. Social stigma in the time of coronavirus disease 2019. Eur. Respir. J. 2020;56 doi: 10.1183/13993003.02461-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speth M.M., Singer-Cornelius T., Oberle M., Gengler I., Brockmeier S.J., Sedaghat A.R. Mood, anxiety and olfactory dysfunction in COVID-19: evidence of central nervous system involvement? Laryngoscope. 2020 doi: 10.1002/lary.28964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D., Moher D., Becker B.J., Sipe T.A., Thacker S.B. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- Sun S., Guo L., Shang K., Lu J. Effects of post-traumatic stress disorder on neurological soft signs in patients with COVID-19. J. Psychiatry. 2020;33:81–83. [Google Scholar]
- Thombs B.D., Bonardi O., Rice D.B., Boruff J.T., Azar M., He C., Markham S., Sun Y., Wu Y., Krishnan A., Thombs-Vite I., Benedetti A. Curating evidence on mental health during COVID-19: a living systematic review. J. Psychosom. Res. 2020;133 doi: 10.1016/j.jpsychores.2020.110113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomasoni D., Bai F., Castoldi R., Barbanotti D., Falcinella C., Mulè G., Mondatore D., Tavelli A., Vegni E., Marchetti G., D'Arminio M.A. Anxiety and depression symptoms after virological clearance of COVID-19: a cross-sectional study in Milan, Italy. J. Med. Virol. 2020 doi: 10.1002/jmv.26459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varatharaj A., Thomas N., Ellul M.A., Davies N., Pollak T.A., Tenorio E.L., Sultan M., Easton A., Breen G., Zandi M., Coles J.P., Manji H., Al-Shahi S.R., Menon D.K., Nicholson T.R., Benjamin L.A., Carson A., Smith C., Turner M.R., Solomon T., Kneen R., Pett S.L., Galea I., Thomas R.H., Michael B.D. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiat. 2020;7:875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villa S., Jaramillo E., Mangioni D., Bandera A., Gori A., Raviglione M.C. Stigma at the time of the COVID-19 pandemic. Clin. Microbiol. Infect. 2020 doi: 10.1016/j.cmi.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh F. Loss and resilience in the time of COVID-19: meaning making, hope, and transcendence. Fam. Process. 2020;59:898–911. doi: 10.1111/famp.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Huang L., Hu L., Wang Y., Xu R., Cai S., Liao J., Zhao Y., Yang W., Wang C. Psychological stress status and its influencing factors among inpaitents with COVID-19. J. Nurs. Sci. 2020;35:75–79. [Google Scholar]
- Wang Y., Zhu L.Y., Ma Y.F., Bo H.X., Deng H.B., Cao J., Wang Y., Wang X.J., Xu Y., Lu Q.D., Wang H., Wu X.J. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. 2020;75:282–286. doi: 10.1016/j.sleep.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesemann U., Hadjamu N., Willmund G., Dolff S., Vonderlin N., Wakili R., Vogel J., Rassaf T., Siebermair J. Influence of COVID-19 on general stress and posttraumatic stress symptoms among hospitalized high-risk patients. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720003165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2021. WHO coronavirus (COVID-19) dashboard, https://covid19.who.int/ (2021-04-01).
- Wu C., Hu X., Song J., Yang D., Xu J., Cheng K., Chen D., Zhong M., Jiang J., Xiong W., Lang K., Tao Y., Lin X., Shi G., Lu L., Pan L., Xu L., Zhou X., Song Y., Wei M., Zheng J., Du C. Mental health status and related influencing factors of COVID-19 survivors in Wuhan, China. Clin. Transl. Med. 2020;10 doi: 10.1002/ctm2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Peng Y. Investigation on the status of anxiety and depression in hospitalized patients with severe coronavirus disease 2019. Chin. J. Nurs. 2020;55:606–607. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka T., Maeda Y. COVID-19 stigma induced by local government and media reporting in japan: it's time to reconsider risk communication lessons from the Fukushima Daiichi nuclear disaster. J. Epidemiol. 2020;30:372–373. doi: 10.2188/jea.JE20200247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Du Y., Xu W., Chen Y. Analysis of anxiety and depression levels and influencing factors of suspected patients with COVID-19 during isolation and observation. Chongqing Med. 2020;49:3156–3160. [Google Scholar]
- Zarghami A., Farjam M., Fakhraei B., Hashemzadeh K., Yazdanpanah M.H. A Report of the telepsychiatric evaluation of SARS-CoV-2 patients. Telemed. J. E Health. 2020 doi: 10.1089/tmj.2020.0125. [DOI] [PubMed] [Google Scholar]
- Zhai Y., Du X. Loss and grief amidst COVID-19: a path to adaptation and resilience. Brain Behav. Immun. 2020;87:80–81. doi: 10.1016/j.bbi.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Qin S., Zhang L., Feng Z., Fan C. A psychological investigation of coronavirus disease 2019 (COVID-19) patients in mobile cabin hospitals in Wuhan. Ann. Transl. Med. 2020;8:941. doi: 10.21037/atm-20-4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Yang Z., Wang X., Li J., Dong L., Wang F., Li Y., Wei R., Zhang J. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J. Clin. Nurs. 2020 doi: 10.1111/jocn.15425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K., Zhou X., Liu H., Hashimoto K. Treatment concerns for psychiatric symptoms in patients with COVID-19 with or without psychiatric disorders. Br. J. Psychiatry. 2020;217:351. doi: 10.1192/bjp.2020.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Liu X., Xue M., Luo L., He G., Feng P., Jiang X., Xie L. The correlation between post-traumatic stress disorder and perceived stress in suspected COVID-19 patients quarantined in hospital. Chin. J. Respir. Crit. Care Med. 2020;19:325–329. [Google Scholar]
- Zhao Q., Hu C., Feng R., Yang Y. Investigation of the mental health of patients with COVID-19. Chin. J. Neurol. 2020;53:432–436. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.