Abstract
Objective
To investigate the prevalence of post-traumatic stress disorder (PTSD) in the general population during the COVID-19 pandemic by a systematic review and single-arm meta-analysis.
Methods
CNKI, PubMed, EMBASE, and MEDLINE were searched to collect literature on the prevalence of PTSD in the general population during the epidemic. The retrieval time is from the database construction to 31/08/2020. Meta-analysis was performed on the included articles by using Review Manger 5.3 and Stata 16.0 software.
Results
The prevalence of PTSD in the general population during the COVID-19 pandemic was 15% (95% CI: 11–21%, p<0.001).
Conclusion
The COVID-19 pandemic brought certain mental pain to general population, leading to a rise in the incidence of PTSD in a short time.
Keywords: Post-traumatic stress disorder, Prevalence, General population, Meta-analysis, COVID-19
INTRODUCTION
As the COVID-19 spread extremely fast and nearly unstoppable, in the past week, the highest number of new COVID-19 cases have been reported globally, amounting to over 2 million new cases from October 18, 2020 to October 25, 2020, the shortest intervals for this exponential increase since the start of the pandemic, and it has infected more than 42 million people, causing over 1.1 million deaths in 212 countries [1]. The situation of alarm generated by COVID-19 has turned into a crisis with unprecedented consequences throughout the world [2].
Actually, of the three major coronavirus epidemics erupted in the 21st century, the COVID-19 pandemic is the similar to the Acute Respiratory Syndrome (SARS) and Middle Eastern Respiratory Syndrome (MERS), and it has higher infectiousness and wider spread, which affect the whole world. However, the epidemics may not only be physically damaging, but also do harm to people’s psychological status. Some studies have suggested that the outbreak of contagious diseases like SARS is able to bring about PTSD symptomatology and during the MERS epidemic 80.2% of the general public reported fear of being infected, and 46% reported emotional distress [3-5].
Quarantine has been used in response to the COVID-19 outbreak. Quarantine is the segregation and limitation of travel of individuals who might have been subjected to an infectious illness to decide if they are ill, thus decreasing their chance of contaminating others [6]. Brooks in a recent review reported that quarantine is associated with increased psychological distress, diagnostic symptoms of PTSD, depression and in general greater levels of stress [2].
PTSD refers to the delayed appearance and persistence of mental disorders caused by individuals who experience, witness or encounter one or more actual deaths involving themselves or others, or are threatened with death, or serious injuries, or physical integrity. From the DSM-5, a diagnosis of PTSD requires symptoms from the following four groups to be present: persistent re-experiencing of the event, avoidant symptoms, negative change in general responsiveness and increased arousal and reactivity [7].
Both the fear of contracting the virus and the measures adopted to counteract the spread of infection may have been perceived as traumatic events. During the COVID-19 pandemic, several studies have focused on the prevalence of PTSD in both medical staff and patients. Interestingly, there was a research found that the vicarious traumatization scores of the general public were significantly higher than those of the front-line nurses [8].
Consequently, we reviewed and meta-analyzed studies on the prevalence of PTSD in the general population during the COVID-19 pandemic, including studies from February to August in order to make a comprehensive evaluation about it, plan timely interventions and address the optimal coping strategies to guide the public.
METHODS
Data sources and search strategy
In this meta-analysis, we searched from CNKI, PubMed, EMBASE, and MEDLINE to collect literature on the prevalence of PTSD in the general population after the outbreak of COVID-19. The search period was from database establishment to August 31, 2020. References were also searched to ensure that all relevant articles were included in the study. For MEDLINE, the terms were: (“novel coronavirus” OR “2019 novel coronavirus” OR “novel coronavirus pneumonia” OR “new coronavirus” OR “Wuhan coronavirus” OR “Wuhan seafood market coronavirus” OR “coronavirus disease 2019” OR “SARS2” OR “2019-nCoV” OR “SARS-CoV-2” OR “COVID-19” OR “NCP”) AND (“PTSD” OR “PTS” OR “post-traumatic stress”). And The study publication time was limited to “in the last one year.” The search strategy was decided after discussion by three investigators. Full-texts were examined for eligibility for 478 papers and 12 studies met the inclusion criteria.
Inclusion and exclusion criteria
Studies were eligible for inclusion if they met the following criteria: 1) The subjects were general population; 2) study time is after the outbreak of COVID-19; 3) the method was a questionnaire survey; 4) the scale used in the study included the impact of event scale- revised (IES-R), the PTSD Checklist-Civilian Version (PCL-C) and the PTSD Checklist (PCL-5), as well as other related scales that can be used to diagnose PTSD; 5) The prevalence of PTSD or the number of cases in the general population could be obtained in the experimental results. Excluded studies met any of the following criteria: 1) without full text or data not available; 2) serious flaws in the study’s design; 3) statistical methods are wrong; 4) overlapping or duplicate publications; 5) reviews, abstracts, letters, case reports, case series, editorials, and commentaries; 6) qualitative research.
Study selection and data extraction
All articles were screened independently by three investigators according to the inclusion and exclusion criteria. If the investigator has different opinions, discuss them together, and consult other experts when agreement cannot be reached after discussion. Each study contains the following features: title, first author, publication year, country of the study, sample size, research method, object of study, research content, important results and conclusions. Cross-check after data extraction.
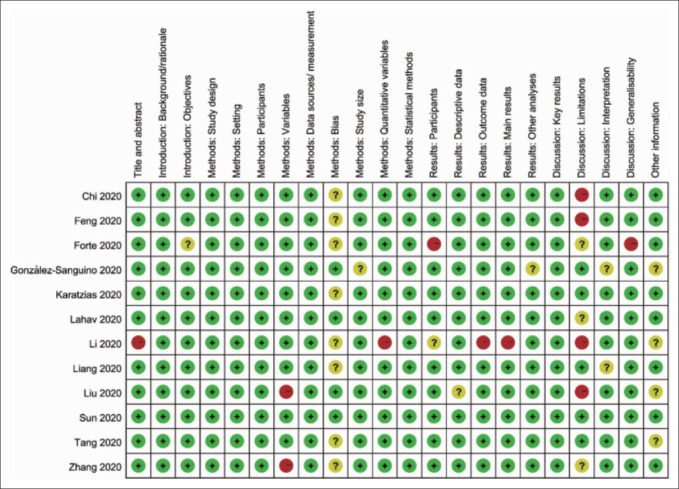
Quality assessment of included studies
One author determined the methodological quality of all studies with discussion and verification by another two authors to achieve consensus establish agreement with overall rating scores. The quality of included studies was assessed by three investigators independently using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement version 4 [9]. The assessment included 22 items covering study design, setting, participants, variables, data sources/measurements, bias, study size, quantitative variables, and statistical methods. For each item, an assessment of “low risk,” “unclear risk,” or “high risk” was given, and the final result of the assessment was decided after discussion.
Statistical analysis
All statistical analyses were conducted using Review Manager 5.3 software (The Cochrane Collaboration London, United Kingdom). We pooled data about the general population prevalence of PTSD and risk difference (RD, with 95% confidence interval) was used as the effect size, and then the inverse variance method (Generic Inverse Variance) is selected to calculate the pooled effect. Because, at this time, the rate difference (RD) and its standard error are equivalent to the effect of a single rate and the standard error [10]. The heterogeneity among studies was checked by the Q test and forest plots. If the p value for the heterogeneity test was >0.10, we considered that the included studies have good homogeneity and performed the fixed effects model. Otherwise, the random effects model was performed. Funnel chart and Egger test were done to evaluate for possible publication bias, and the test level was α=0.05.
RESULTS
Literature inclusion
Through the retrieval of the above databases, 478 documents were finally identified according to the search strategy. Eventually, 12 studies were included in our meta-analysis, 2 of which were in Chinese and 10 in foreign languages. Our initial search and the process of study selection are summarized in Figure 1. The main characteristics and the quality assessment of the included studies are shown in Table 1 [11-22], Figure 2.
Figure 1.
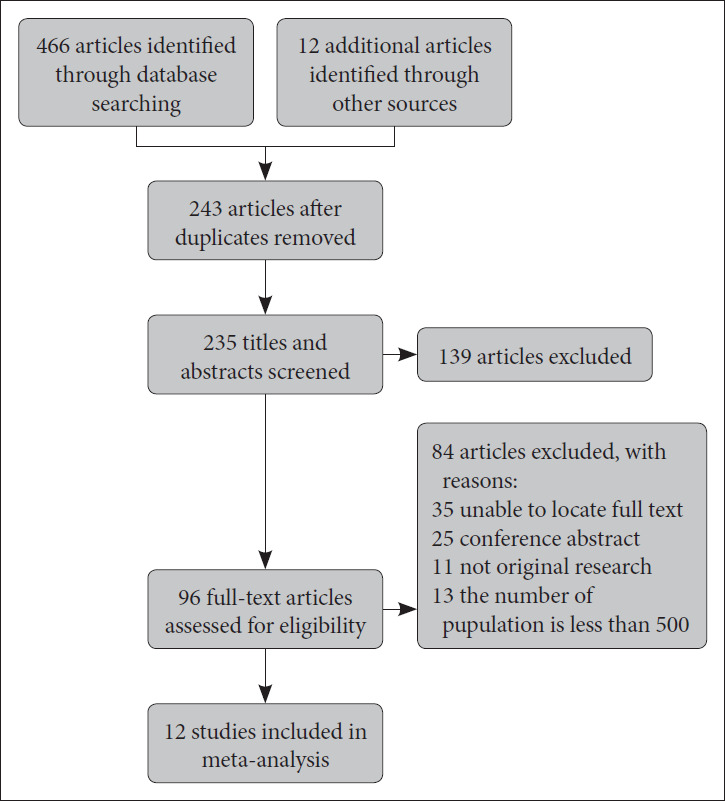
Flow chart of studies selection process.
Table 1.
Basic characteristics of included studies
| Author | Year | Total | Event | p | Country | Scale |
|---|---|---|---|---|---|---|
| Chi et al. [11] | 2020 | 2,038 | 628 | 0.3081 | China | PCL-C |
| Feng et al. [12] | 2020 | 53,427 | 2,536 | 0.0475 | China | PCL-C |
| Forte et al. [13] | 2020 | 2,286 | 629 | 0.2752 | Italy | PCL-5 |
| González-Sanguino et al. [14] | 2020 | 3,480 | 550 | 0.1580 | Spain | PCL-C |
| Karatzias et al. [15] | 2020 | 1,041 | 184 | 0.1768 | Ireland | ICD-11 |
| Lahav [16] | 2020 | 976 | 112 | 0.1148 | Israel | PCL-5 |
| Li [17] | 2020 | 1,109 | 744 | 0.6709 | China | IER-S |
| Liang et al. [18] | 2020 | 570 | 73 | 0.1281 | China | PCL-C |
| Liu et al. [19] | 2020 | 898 | 286 | 0.3185 | the US | PCL-C |
| Sun et al. [20] | 2020 | 2,091 | 96 | 0.0459 | China | PCL-5 |
| Tang et al. [21] | 2020 | 2,485 | 73 | 0.0294 | China | PCL-C |
| Zhang et al. [22] | 2020 | 4,255 | 452 | 0.1062 | China | PCL-C |
Figure 2.
The quality assessment of these studies.
Meta-analysis results
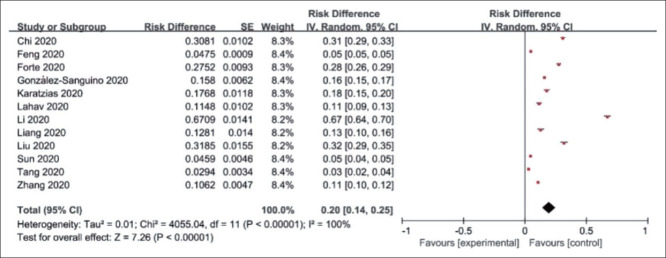
Review Manager 5.3 software was applied to test the heterogeneity of the 12 studies, I2=100.0%, p<0.001, which indicated that there was significant heterogeneity among the studies. Therefore, the random effects model was performed. Our results of Meta-analysis revealed that the prevalence of PTSD in the general population during the COVID-19 pandemic was 20% (95% CI: 14–25%, p<0.001) (Figure 3).
Figure 3.
Meta-analysis of the prevalence of PTSD in the general population during the COVID-19 pandemic.
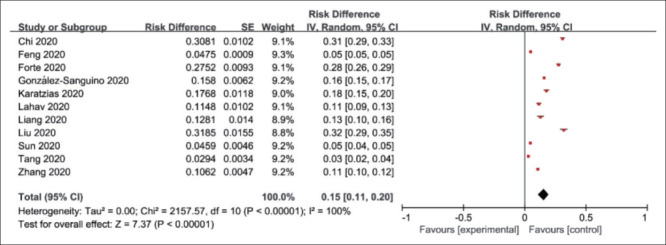
Sensitivity analyses
The impact of individual studies on combined RD was assessed by sensitivity analyses. Because of the poor homogeneity of the studies included in this study, we conducted multiple analyses, excluding one study from the combined meta-analysis in each analysis. Though the directions of forest plots were almost the same, the corresponding RD changed significantly when excluded Li Q’s study, which decreased from 20% to 15%. And when excluded one of other studies at a time, the pooled RD was almost consistent. Consequently, we decided to remove Li Q’s study (its quality was also relatively poorer) for the sake of eliminating the influence of the overall result, which revealed that the prevalence of PTSD in the general population during the pandemic was 15% (95% CI: 11–20%, p<0.001) (Figure 4).
Figure 4.
Meta-analysis of the prevalence of PTSD in the general population during the COVID-19 pandemic (excluded Li Q’s study).
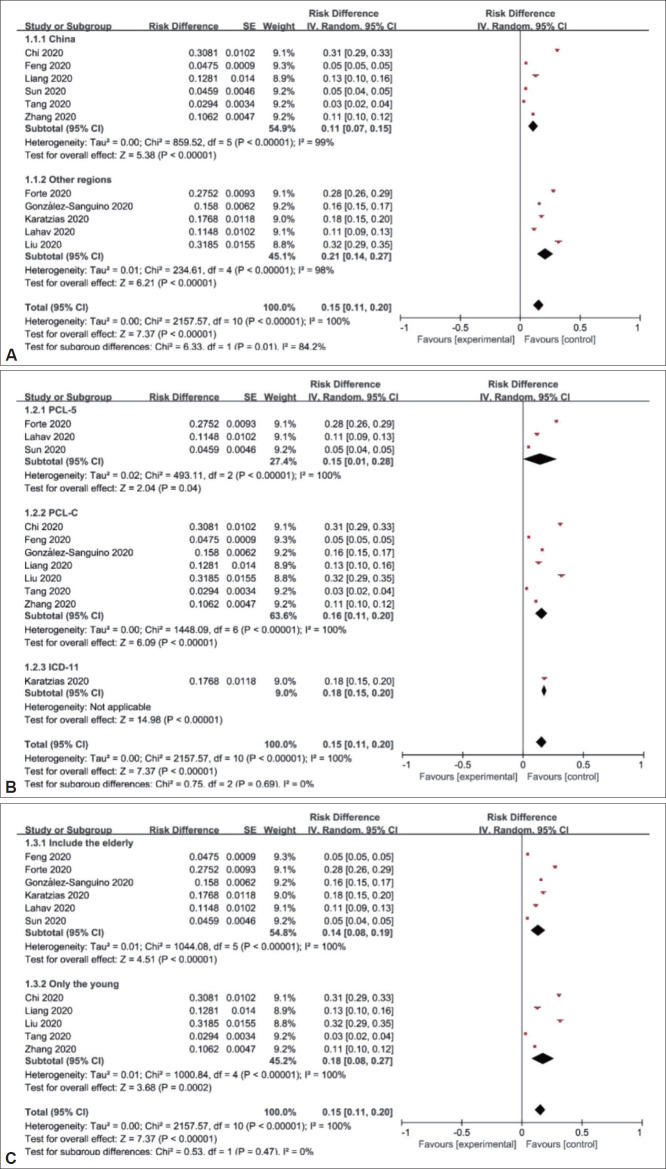
Subgroup analyses
Considering people from different countries may have various psychological changes when traumatic events happen, we performed a subgroup analysis with China and other regions which revealed that the prevalence of PTSD in the general population during the COVID-19 pandemic were 11% (95% CI: 7–15%, p<0.001) in China and 21% (95% CI: 14–27%, p<0.001) in other regions (Figure 5A). Because the focus of different scales for PTSD is not the same, we divided the included studies into three subgroups: PCL-5, PCL-C, ICD-11. Our analysis reflected the prevalence in different subgroups separately were 15% (95% CI: 1–28%, p<0.001) of PCL-5, 16% (95% CI: 11–20%, p<0.001) of PCL-C, 18% (95% CI: 15–20%, p<0.001) of ICD-11 (Figure 5B). Besides, there are six include studies investigated several age groups including the elderly, while five only investigated the young, for which we performed a subgroup analysis (Figure 5C) that showed the prevalence of the former was 14% (95% CI: 8–19%, p<0.001), and the latter was 18% (95% CI: 8–27%, p<0.001). Unfortunately, all the subgroup analyses above failed to reduce the heterogeneity, indicating that the different region, scale, and study subject (include the elderly or only the young) may not be the sources of heterogeneity. And we found that no differences existed in both the scale subgroups and the study subject subgroups, and high heterogeneity existed in the region subgroups (I2=84.2%).
Figure 5.
Forest maps of subgroup analysis. A: Subgroup analysis by region. B: Subgroup analysis by scale. Forest maps of subgroup analysis. C: Subgroup analysis by study subject.
Publication bias
Funnel plots were drawn to assess publication bias of included studies (Figure 6). Most of the studies were distributed at the top of the funnel plot, indicating that the sample size of the included studies was sufficient. However, its shape showed some signs of asymmetry, suggesting a possible publication bias. Quantitative Egger test was further performed with Stata software, and the p value of Egger test was 0.004. Therefore, to some degree, there is publication bias in this meta-analysis. The reason may be that methodological or clinical heterogeneity existed among the included studies.
Figure 6.
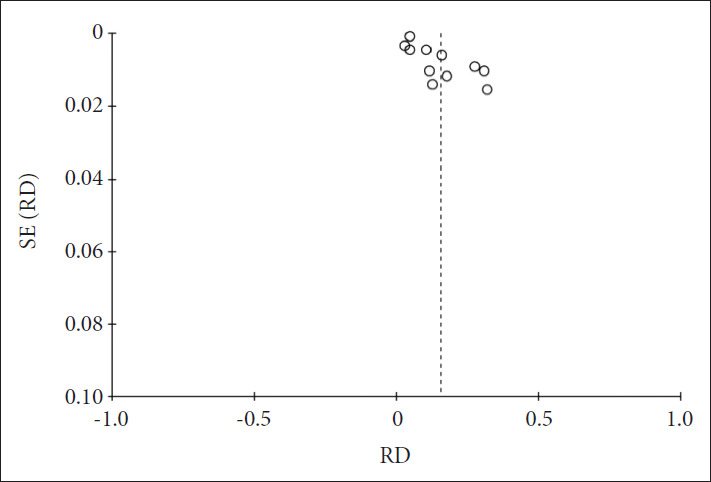
Funnel plot of potential publication bias for included studies. RD: risk difference.
DISCUSSION
PTSD is a common emotional disorder in the general population after a disaster and it is considered as the second tsunami in the SARS-Cov-2 pandemic [23]. This study demonstrated that the prevalence of PTSD in the general population during the COVID-19 pandemic was 15% (95% CI: 11–20%, p<0.001), contrast to results from the recent meta-analysis documented high levels of post-traumatic stress symptoms (23.88%) [24]. The likely reasons are as follows: the sample sizes of included studies in our meta-analysis are all above 500, while some studies in previous meta-analysis are small, which is more possible to obtain higher scores. Furthermore, our included studies are already published, and the results may be more credible than the unpublished data in previous meta-analysis.
When we did the sensitivity analysis, we found that the prevalence of PTSD in Li’s study was significantly higher than in other studies. As for the Impact of Events Scale-Revised (IES-R), which was used in Li Q’s study, the scale includes 22 items, serve as an effective means to examine the PTSD symptoms and the diagnostic criteria score is 33 [25-27]. Unfortunately, Li Q’s study just reported the prevalence above the cutoff score (a score of 20) of post-traumatic stress symptoms which was the reason why the result in his study was 67.09%. As a result, the outcome affected greatly to our meta-analysis and eventually was excluded. The other heterogeneity in our meta-analysis comes from the different criterion of scales among studies, especially the PCL-C, for example, some studies reported that with scores of 38 or above being considered indicative of probable PTSD, while the cutoff scores of others were 14, 45, or 51 [11,12,18,19,21,22]. Besides, possibly cultural differences also make difference to the heterogeneity. Regional differences may exist with respect to the general public’s psychological health during a massive disease outbreak due to varying degrees of outbreak severity, national economy, government preparedness, availability of medical supplies/facilities, and proper dissemination of COVID-related information, it can be proved from the region subgroup in our study (I2=84.2%) [28].
The general population is an easily overlooked group during the COVID-19 epidemic. However, through our study, it was found that even if people were not infected with novel coronavirus, they would still be under great stress psychologically. We can see that the general population in all countries developed PTSD to varying degrees during the epidemic. When evaluating the psychological impacts incurred by the coronavirus outbreak, the duration of psychiatric symptoms should also be taken into consideration since acute psychological responses to stressful or traumatic events are sometimes protective and of evolutionary importance [29,30]. However, if the stressor persists, PTSD symptoms may become chronic, research has suggested that approximately 40% of affected individuals continue to exhibit significant symptoms 10 years after its onset [31]. In addition, individuals with PTSD are between 2 and 6 times more likely to present with psychiatric comorbidities, including depression, anxiety, and suicidality [32,33]. It is reported a projected increase in suicide from 418 to 2,114 in Canadian suicide cases associated with joblessness, and the rising trajectory of suicide also revealed in the USA, Germany, Italy and other countries [34,35].
Therefore, to identify the prevalence of PTSD in the general population may be beneficial to the health sector’s prevention strategy for PTSD and to reduce the risk of suicide and other mental illness. In a review of previous studies, we found that effective interventions can help reduce the psychological distress experienced by people during emerging disease outbreaks [36]. With the approach of winter, the second wave of the global epidemic is also in full swing. We should not only prevent and control the epidemic, but also conduct mental health interventions. For those affected by COVID-19, interventions should be based on a comprehensive assessment of the risk factors for psychological problems, including pre-crisis poor mental health, bereavement, harm to oneself or family members, life-threatening conditions, panic, separation from family and low family income [37]. These measures can make sense to help reduce or prevent mental illness in the future.
We must admit that there are still several limitations in this study. There was a large heterogeneity among the studies. Various measuring scales of the included studies and some different criterion of scales have been used when analyzing the outcomes. Thus, we conducted subgroup analyses to evaluate the influence of several variables on our results, however, the heterogeneity still failed to be reduced successfully.
The results demonstrated that COVID-19 had a huge impact on people psychologically, and causing a significant increase in the incidence of PTSD among the general population in a short period of time. PTSD has been shown to be associated with significant economic costs due to work impairment, hospitalization, and health care–related visits [38]. Hence, early intervention and appropriate management of PTSD is of vital importance. Follow-up studies after the outbreak may be needed to assess the long-term psychological impacts of the COVID-19 pandemic, including but not limited to the PTSD prevalence of general population, patients and medical workers.
Acknowledgments
None.
Footnotes
The authors have no potential conflicts of interest to disclose.
Authors’ contribution
Conceptualization: Liqing Zhang, Rong Pan. Data collection: Liqing Zhang, Rong Pan. Meta-analysis: Liqing Zhang, Yixian Cai. Writing—original draft: Liqing Zhang, Yixian Cai. Writing—review & editing: Liqing Zhang, Rong Pan, Jiyang Pan. All authors provided critical revision of the manuscript for important intellectual content.
REFERENCES
- 1.World Health Organization Coronavirus Disease (COVID-2019) Situation Reports. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed October 31, 2020.
- 2.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong H, Yim H, Song Y, Ki M, Min J, Cho J, et al. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Health. 2016;38:e2016048. doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asukai N, Kato H, Kawamura N, Kim Y, Yamamoto K, Kishimoto J, et al. Reliabiligy and validity of the Japanese-language version of the impact of event scale-revised (Ies-RJ): four studies of different traumatic events. J Nerv Ment Dis. 2002;190:175–182. doi: 10.1097/00005053-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Quarantine and isolation. Available at: https://www.cdc.gov/quarantine/. Centers for Disease Control and Prevention, 2020. Accessed Sep 20, 2020.
- 7.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-5®) Washington, DC: American Psychiatric Pub; 2013. [Google Scholar]
- 8.Li Z, Ge J, Yang M, Feng J, Qiao M, Jiang R, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Von Elm E, Altman D, Egger M, Pocock S, Gøtzsche P, Vandenbroucke J. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18:800–804. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Du L, Geng X, Liu G. Implement meta-analysis with non-comparative binary data in RevMan software. Chin J Evidence Based Med. 2014;14:889–896. [Google Scholar]
- 11.Chi X, Becker B, Yu Q, Willeit P, Jiao C, Huang L, et al. Prevalence and psychosocial correlates of mental health outcomes among Chinese college students during the Coronavirus Disease (COVID-19) Pandemic. Front Psychiatry. 2020;11:803. doi: 10.3389/fpsyt.2020.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feng Z, Liu X, Chen Z. Psychological problems among the massivepeople in COVID-19 pandemic. J Southwest Univ. 2020;46:109–115+195. [Google Scholar]
- 13.Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Environ Res Public Health. 2020;17:4151. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.González-Sanguino C, Ausín B, Castellanos M, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karatzias T, Shevlin M, Murphy J, McBride O, Ben-Ezra M, Bentall R, et al. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J Trauma Stress. 2020;33:365–370. doi: 10.1002/jts.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lahav Y. Psychological distress related to COVID-19 - The contribution of continuous traumatic stress. J Affect Disord. 2020;277:129–137. doi: 10.1016/j.jad.2020.07.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Q. Psychosocial and coping responses towards 2019 coronavirus diseases (COVID-19): a cross-sectional study within the Chinese general population. QJM. 2020;113:731–738. doi: 10.1093/qjmed/hcaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liang L, Gao T, Ren H, Cao R, Qin Z, Hu Y, et al. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. 2020;25:1164–1175. doi: 10.1177/1359105320937057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu C, Zhang E, Wong G, Hyun S, Hahm H. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun L, Sun Z, Wu L, Zhu Z, Zhang F, Shang Z, et al. Prevalence and risk factors for acute posttraumatic stress disorder during the COVID-19 outbreak. J Affect Disord. 2021;283:123–129. doi: 10.1016/j.jad.2021.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tang W, Hu T, Yang L, Xu J. The role of alexithymia in the mental health problems of home-quarantined university students during the COVID-19 pandemic in China. Pers Individ Dif. 2020;165:110131. doi: 10.1016/j.paid.2020.110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Zhuang L, Yang W. Symptoms of PTSD in middle school Students during COVID-19 epidemic - A case study of Shude middle school in Chengdu. Educ Sci Forum. 2020:45–48. [Google Scholar]
- 23.Dutheil F, Mondillon L, Navel V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med. 2020:1–2. doi: 10.1017/S0033291720001336. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooke J, Eirich R, Racine N, Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2020;292:113347. doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu K, Chan K. The development of the Chinese version of Impact of Event Scale--Revised (CIES-R) Soc Psychiatry Psychiatr Epidemiol. 2003;38:94–98. doi: 10.1007/s00127-003-0611-x. [DOI] [PubMed] [Google Scholar]
- 26.Pietrantonio F, De Gennaro L, Di Paolo M, Solano L. The Impact of Event Scale: validation of an Italian version. J Psychosom Res. 2003;55:389–393. doi: 10.1016/s0022-3999(02)00638-4. [DOI] [PubMed] [Google Scholar]
- 27.Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 28.Xiong J, Lipsitz O, Nasri F, Lui L, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brosschot JF, Verkuil B, Thayer JF. The default response to uncertainty and the importance of perceived safety in anxiety and stress: an evolution-theoretical perspective. J Anxiety Disord. 2016;41:22–34. doi: 10.1016/j.janxdis.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 30.Yaribeygi H, Panahi Y, Sahraei H, Johnston T, Sahebkar A. The impact of stress on body function: a review. EXCLI J. 2017;16:1057–1072. doi: 10.17179/excli2017-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 32.Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- 33.Karatzias T, Hyland P, Bradley A, Cloitre M, Roberts N, Bisson J, et al. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depress Anxiety. 2019;36:887–894. doi: 10.1002/da.22934. [DOI] [PubMed] [Google Scholar]
- 34.Thakur V, Jain A. COVID 2019-suicides: a global psychological pandemic. Brain Behav Immun. 2020;88:952–953. doi: 10.1016/j.bbi.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 35.Mamun M, Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? - The forthcoming economic challenges for a developing country. Brain Behav Immun. 2020;87:163–166. doi: 10.1016/j.bbi.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Talevi D, Socci V, Carai M, Carnaghi G, Faleri S, Trebbi E, et al. Mental health outcomes of the CoViD-19 pandemic. Riv Psichiatr. 2020;55:137–144. doi: 10.1708/3382.33569. [DOI] [PubMed] [Google Scholar]
- 37.Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. 2020;7:300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferry F, Brady S, Bunting B, Murphy S, Bolton D, O’Neill S. The economic burden of PTSD in Northern Ireland. J Trauma Stress. 2015;28:191–197. doi: 10.1002/jts.22008. [DOI] [PubMed] [Google Scholar]