Abstract
Objective
A central adrenergic hyperactivation is described in the neurobiology of posttraumatic stress disorder (PTSD) with probable variable symptomatic impact. Few studies have evaluated using the alpha-1 adrenergic antagonist prazosin for such symptoms; however, given the likely pathophysiology involved, this drug may play an important role in the pharmacological approach to PTSD.
Methods
This study assessed articles already published on the use of prazosin through a systematic review along a timeline in view of the symptomatic target of difficult access by standardized treatments. The impact of using this medication for the general symptoms of PTSD is also discussed. Several databases were searched for articles in the literature on the use of prazosin to treat PTSD.
Results
A total of 168 articles were found containing search terms in the title or abstract. Overall, 85 articles met the criteria described, and 48 studies were explored to conduct the present systematic review. Most articles showed some improvement after prazosin administration, especially in relation to sleep symptoms (nightmares and night waking). Only one article demonstrated no improvement after the use of this drug. More randomized studies are needed.
Conclusion
Several clinical studies demonstrated the relevant role of prazosin for treating PTSD symptoms. Prazosin is an affordable and cost-effective pharmacological option compared to other drugs used to treat PTSD.
Keywords: Prazosin alpha-adrenergic blocker, Posttraumatic stress disorder, Insomnia, Nightmares.
INTRODUCTION
Posttraumatic stress disorder (PTSD) can be defined by symptomatic cognitive, behavioral, somatic, and affective perpetuation resulting from a psychologically traumatic event. It is characterized by intrusive thoughts, nightmares, and flashbacks involving the traumatic event, avoidant behaviors, hypervigilance, and sleep disorders, causing a functional impact in the social, occupational, and interpersonal spheres, with significant loss of quality of life for patients [1-4]. Studies on the epidemiological relevance differ regarding the prevalence of the disorder. A study based on data from the World Health Organization stated that the lifetime prevalence of PTSD in the general population is 3.9% and may reach 5.6% in populations exposed to trauma [5]. US studies reported a higher prevalence in the general population, 8.3% in the US [6] and 9.2% in Canada [7], with even higher estimates (10–40%) among at-risk populations as victims of disasters, kidnappings, and military veterans [8].
An association between trauma and acute mental symptoms has been observed for more than 200 years. The relationship between neurosis and trauma was described by Sigmund Freud in the context of wars in an attempt to characterize emotional components of traumatic situations. Psychiatrist Abram Kardiner continued Freud’s studies during World War II and in 1941 published “The Traumatic Neuroses of War,” an important book on the evolution of PTSD symptom characterization describing symptoms such as chronic hypervigilance and hypersensitivity related to traumatic situations [9,10].
In the initial neurobiological studies, there was an increase in the basal heart rate and systolic blood pressure values in combat veterans, which led to the hypothesis that peripheral autonomic hyperactivation could be related to central noradrenergic hyperexcitation, an impression that was reinforced with findings of increased activity in the locus coeruleus, increased urinary excretion of norepinephrine metabolites, and increased monoamine concentrations in the cerebrospinal fluid of these patients [11,12]. Several symptoms of the disorder can be explained by this exacerbation of adrenergic activity in the central nervous system promoting greater norepinephrine release and increased responsiveness of adrenergic receptors. Furthermore, in this context, studies have shown that adrenergic hyperactivity begins at night, leading to increased responsiveness of alpha-1-adrenergic receptors, which promotes rapid eye movement (REM) sleep alteration, increases the frequency of nightmares, and intensifies feelings such as fear [13,14]. Sleep disorders (insomnia, restless sleep, and nightmares) occur in up to 70% of patients associated with a higher risk of suicide in PTSD [15-17]. Given the clinical importance of sleep symptoms and the poor response to the first line pharmacological treatment for PTSD (selective serotonin reuptake inhibitors, SSRIs) [14] prazosin has emerged as the main agent for treating PTSD-related nightmares because of its role in stopping the consolidation of fear memories and reducing the primitive response to fear [18]. Prazosin, an alpha-1-adrenergic receptor antagonist, was first introduced in the 1970s as a US Food and Drug Administration (FDA)-approved agent for the treatment of hypertension. Although rarely used today for this indication, there are numerous case reports, open trials, and randomized controlled trials have shown the efficacy of prazosin for treating nightmares of PTSD patients [19-22].
Therefore, the present study assessed articles already published on the use of prazosin through a systematic review along a timeline in view of the symptomatic target of difficult access by standardized treatments. The impact of using this medication for the general symptoms of PTSD is also discussed.
METHODS
Data sources and search strategy
To select papers that addressed the “use of prazosin in the treatment of posttraumatic stress disorder and associations” in the literature, the PubMed, Embase, OVID, and Cochrane Library databases were searched. The keywords used were “prazosin alpha-adrenergic blocker,” “posttraumatic stress disorder,” “insomnia,” and “nightmares.” A combination of the keywords with “AND” and the Boolean operator “NOT” was used to exclude papers that had the word “pre-clinical” and its respective synonyms, which were previously consulted in Medical Subject Headings (MeSH) terms. The title and abstracts were examined under all conditions. Systematic Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) review rules were followed.
Study selection and risk of bias in each study
Two independent reviewers (1 and 2) conducted the research and study selection. The data extraction was performed by reviewer 1 and fully reviewed by reviewer 2. A third investigator resolved some conflicting points and made the final decision to choose the articles. Only studies reported in Portuguese and English were evaluated. The Cochrane instrument was adopted to assess the quality of the included studies [23].
Risk of bias
Considering the Cochrane tool for risk of bias, the overall evaluation resulted in five studies with a high risk of bias and three studies with uncertain risk. Five studies had a limited number of participants. The source of financing was absent in two studies. Two studies did not disclose information on the conflicts of interest statement.
RESULTS
A total of 168 articles were found containing search terms in the title or abstract. Thus, 85 articles met the criteria described, and 47 studies were explored to compose the present systematic review according to Figure 1. Any articles that did not have a methodology compatible with the present review’s criteria were excluded.
Figure 1.
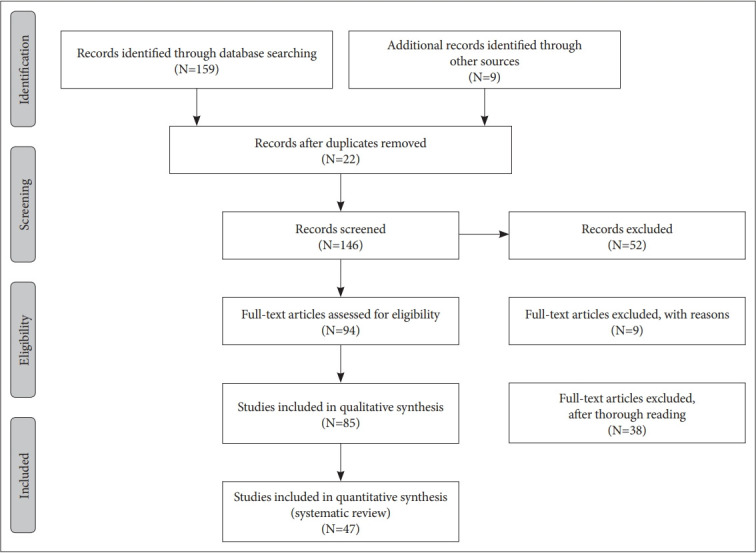
Flowchart of the article selection process.
Table 1 describes the characteristics of the main reviewed articles and brings the results involving the Prazosin benefits to PTSD’s symptoms. Among the seven Randomized Controlled Trials (RCT) included, there were two that didn’t find improvements with this medication. However, five RCT’s concluded that Prazosin is an effective drug for many of PTSD’s symptoms, especially the sleep disturbances. The patients had improvements in the sleep quality and quantity but also presented clinical significance on reducing nightmares.
Table 1.
Summary of main reviewed papers-Prazosin as the treatment of posttraumatic stress disorder (PTSD)
| Reference | Study design | Dose | Total patients | Major findings |
|---|---|---|---|---|
| Raskind et al. [20] | Open-label | 2 or 5 mg | 4 | The 4 patients improved on CAPS and CGI scales |
| George et al. [19] | Meta-analysis | - | 191 | Prazosin superior to placebo to treat nightmares and general symptoms of the disorder |
| Peskind et al. [24] | Open-label | Mean dose 9, 5 mg/day | 9 | Reduced nightmares and severity of PTSD’s symptoms |
| Raskind et al. [25] | Crossover trial | Mean dose 13 mg/day | 10 | Improved sleep quality |
| Reduced nightmares and hyperarousal symptoms | ||||
| Taylor et al. [26] | Crossover trial | 1–5 mg | 11 | Improved Mood States Scores (POMS) |
| Taylor et al. [27] | Crossover trial | 2–6 mg | 13 | Increased sleep time and reduced nigthmares |
| Raskind et al. [28] | Randomized | 13 mg | 34 (17 prazosin; 17 placebo) | Reduced nightmares. Improved sleep quality and global clinical status |
| Controlled | ||||
| Trial | ||||
| Germain et al. [29] | Randomized | 1–15 mg | 50 (18 prazosin, 17 CBT, 15 placebo) | Improved sleep quality |
| Controlled | ||||
| Trial | ||||
| Raskind et al. [30] | Randomized | 15.6 mg | 67 | Reduced nightmares. Improved sleep quality and PTSD scores (CAPS) |
| Controlled | ||||
| Trial | ||||
| Ahmadpanah et al. [31] | Randomized Controlled | 1–15 mg | 100 (33: prazosin; 34 hydroxyzine; 33 placebo) | Reduced nightmares; Improved sleep quality |
| Trial | ||||
| Khachatryan et al. [34] | Meta-analysis | - | 240 | Improved sleep quality and reduced PTSD symptoms |
| Raskind et al. [35] | Randomized | 14.8 mg - | 271 (135 prazosin; 136 placebo) | Not effective for sleep symptoms |
| Controlled | 12 mg (women) | |||
| Trial | 20 mg (men) | |||
| McCall et al. [37] | Randomized | 1–20 mg | 20 (10 prazosin; 10 placebo) | Improved sleep quality |
| Controlled | Not effective for suicidal ideation | |||
| Trial | ||||
| Verplaetse et al. [45] | Randomized | 0 | 96 (48 prazosin; 48 placebo) | Not effective for PTSD symptoms (CAPS) |
| Controlled | ||||
| Trial |
CAPS: Clinician Administered PTSD Scale, CGI: Clinical Global Impressions Scale, POMS: Profile of Mood States, CBT: Cognitive Behavioral therapy
As the main scientific findings on the actual effect of prazosin on PTSD treatment, the most relevant studies to date are presented herein.
DISCUSSION
Raskind et al. [20] first reported the clinical relevance of prazosin in PTSD with the prescription of the drug to improve the symptoms of benign prostatic hyperplasia in two Vietnam veterans. During the psychiatric follow-up of these patients, there was a decrease in complaints of PTSD nightmares and, based on these case reports, the group of researchers started a series of studies involving prazosin and patients’ with the disorder. In 2000, the group published a report of four patients who participated in an open-label, dose-escalating clinical trial and who had a good response to sleep symptoms; the study yielded good results on scales that assessed general symptoms of the disorder, such as hypervigilance, and revealed good drug tolerability. Despite the small number of participants, the perception between the dose increase and the symptomatic improvement assessed was clear [20]. George et al. [19] published a meta-analysis containing six clinical trials, which included a total of 191 patients. The results suggested that prazosin was superior to placebo for treating nightmares associated with PTSD as well as for improving the severity of the general symptoms of the disorder. In spite of the small number of articles included and the small number of patients in the studies, the conclusion corroborates that prazosin may have relevant clinical applicability for PTSD. Another study with prazosin was published by Peskind et al. [24]. Nine patients with PTSD used 2–4 mg of prazosin 1 hour before bedtime. There was a significant reduction in nightmares as measured by the Clinician-Administered PTSD Scale (CAPS). Symptom improvement was evident while patients were taking the drug, and nightmares returned a few nights after drug discontinuation. It is noteworthy that three of these patients had already used another alpha blocker (terazosin) for benign prostatic hyperplasia, without any reported improvement of symptoms, reinforcing the hypothesis that prazosin is a drug with good action on the central nervous system. The small number of participants was a limitation of this study. Raskind et al. [25] conducted another study involving 10 Vietnam veterans who developed PTSD with chronic symptoms for more than 25 years. This was the first randomized, doubleblind, placebo-controlled study in which participants were followed for 20 weeks. The mean dose of prazosin was 9.5 mg taken at night. This study demonstrated significant improvement in several aspects of the CAPS scale: nightmares, early insomnia, avoidant symptoms, intrusive thoughts, and hypervigilance. Regarding the disadvantages of the study, a small number of patients (10) had a diagnosis of chronic PTSD and higher clinical stability, which would make extending the findings to PTSD difficult [25]. In a study published in 2006, Taylor et al. [26] followed 11 patients with PTSD who had improved sleep-related symptoms with prazosin but maintained daytime symptoms of the disorder. Using the Profile of Mood States (POMS) scale, daytime use of prazosin was associated with lower anxiety and fear scores, although there was no statistical significance for the improvement found in dysautonomic symptoms. This study presented a selection bias when choosing patients who used a dose of prazosin that had already improved nocturnal symptoms of PTSD as well as the limitation related to the small sample number.
A study by Taylor et al. [27] published in 2008 followed 13 PTSD patients for 7 weeks. When termin was administered at cross-over, there was a 94-minute increase in the total sleep time, increasing REM sleep time, with fewer nightmares and night waking. This was the first study to use objective measures regarding sleep. Its limitations include the small number of patients as well as the clinical heterogeneity of the studied population regarding the duration of the clinical condition and the type of trauma associated.
Raskind et al. [28] published a clinical trial in 2007 involving 40 former US military personnel with PTSD associating other methods of symptom assessment. In addition to the CAPS scale, we used the Pittsburg Quality Index (PSQI), Clinical Global Impression of Change (CGI-C), Nightmare Frequency Questionnaire-Revised (NFQ), and the Hamilton scale; three patients were lost to follow-up and four discontinued the study due to side effects (of which three used prazosin and one used placebo). Prazosin significantly improved the frequency and intensity of trauma-related nightmares, sleep quality, and the patient’s overall clinical status. There was an improvement in depressive symptoms and an overall reduction in the CAPS score, but both results were not statistically significant in the present study. Side effects reported in this study were dizziness due to postural hypotension in 15 patients, 9 of whom were on prazosin and 6 were on placebo. Of the nine who took prazosin, one also used two other anti-hypertensive medications (hydrochlorothiazide and lisinopril) and three used medications with alpha-1-adrenergic antagonism functions (nefazodone, nortriptyline, and quetiapine). The study indicated that there was no difference in the mean blood pressure values in any group regardless of how blood pressure was measured (supine or rising position).
In 2012, Germain et al. [29] published a randomized 8-week study of 50 patients involving the use of prazosin (n=18), a behavioral psychological approach to sleep (n=17), and placebo (n=15). Sleep quality was measured by the PSQI, CGI, and PCL (PTSD checklist) questionnaires and with polysomnography before and after the intervention. The results showed significant improvement in PTSD insomnia and daytime symptoms in both therapeutic groups, with no statistically significant difference between the psychological approach and the use of prazosin.
A clinical trial published in 2013 by Raskind et al. [30] monitored for 15 weeks active US Army Iraq and Afghanistan military service members diagnosed with PTSD. A total of 67 patients were administered the CAPS, PSQI, and CGI questionnaires. There was significant improvement over the study’s three primary outcomes: trauma-related nightmares, sleep quality, and overall clinical status. Prazosin was effective in reducing all the other PTSD symptoms (CAPS scale), which was not the case in a previous study by the same group, where they noted improvement in sleep quality, nightmares, and overall clinical status without improvement in the total CAPS score compared to placebo.
Ahmadpanah et al. [31] conducted a clinical trial involving the use of prazosin, hydroxyzine (antihistamine), and placebo to evaluate the sleep quality of 100 PTSD patients. Total sleep duration and reduction in the number of nightmares occurred in prazosin and hydroxyzine groups, with better results for prazosin. However, the reduction in overall symptoms of PTSD occurred exclusively in the prazosin group. The study had a small sample so that further generalizations could be inferred and used a short, unspecified questionnaire based on the old DSM-IV (Mini International Neuropsychiatric Interview, MINI) criteria to assess the response of medications to the general symptoms of PTSD. In this sense, it has been shown that high noradrenergic activity may be associated with hyperexcitation, trauma nightmares, and sleep disorders in PTSD individuals, probably through stimulation of alpha-1-adrenergic receptors in the prefrontal cortex of the brain. Prazosin decreases the effects of norepinephrine on brain alpha-1 adrenoreceptors and may be a promising agent for the treatment of PTSD, as some studies found it to be effective and well tolerated.
A study examined the role of the noradrenergic system in the pathophysiology of PTSD and conducted a systematic review to evaluate the efficacy and tolerability of prazosin in PTSD patients. A meta-analysis combined data from various studies to better estimate the effect of prazosin on specific outcomes. Prazosin was significantly more effective than placebo in reducing distressing dreams in PTSD patients, although our results should be interpreted with caution due to the small number of studies included in our quantitative synthesis [32].
In 2015, a meta-analysis compared the short-term effectiveness of prazosin versus imagery rehearsal therapy (IRT) on nightmares, sleep quality, and PTSD. Four studies used prazosin, 10 used IRT alone or in combination with another psychological treatment, and one included one group receiving prazosin and another group receiving IRT. The total effect size of both treatments had moderate magnitude for nightmare frequency, sleep quality, and PTSD (p<0.01). The effect size was not significantly different with regard to the type of treatment (psychological vs. pharmacological) on nightmare frequency (p=0.79), sleep quality (p=0.65), or PTSD (p=0.52). IRT combined with cognitive behavioral therapy for insomnia showed more improvement in sleep quality compared with prazosin (p=0.03), IRT alone (p=0.03), or IRT combined with other psychological interventions (p<0.01). Although IRT and prazosin interventions produce comparable acute effects for the treatment of nightmares, the addition of cognitive-behavioral therapy for insomnia appears to improve treatment outcomes for sleep quality and PTSD [33].
Another meta-analysis examined the effectiveness of prazosin for nightmares and other sleep disorders in adults with PTSD. A systematic review of databases for double-blind, placebo-controlled, randomized controlled trials of adults diagnosed with PTSD who reported prazosin-treated sleep disorders was conducted in January 2015. Six randomized controlled trials of prazosin for sleep disorders in PTSD patients were included (sample n=240). Prazosin was found to be statistically significantly more effective than placebo in improving sleep quality [p=0.987, 95% confidence interval (CI): 0.324–1.651] and reducing overall PTSD symptoms (p=0.699, 95% CI: 0.139–1.260) and sleep disorders in particular (p=0.799, 95% CI: 0.391–1.234). Prazosin showed medium to large and statistically significant effects on PTSD symptoms in general and sleep disorders in particular. Although promising, the results should be interpreted with caution considering the limited number of participants and the limitations induced by most participants as male and non-civilian [34]. Raskind et al. [35] conducted a new randomized, double-blind, placebo-controlled clinical trial that found results contrasting with the published literature. A total of 304 patients were followed for 26 weeks. Those randomized to a prazosin group received up to 12 mg/day (women) and 20 mg/day (men). Using the same assessment questionnaires, at the end of 10 weeks of treatment, there was no significant difference between the groups regarding the CAPS, PSQI, and CGI-C scores. After 26 weeks, the results were maintained with an additional reduction in systolic BP (6.7 mmHg in the prazosin group) and an increase or onset of suicidal ideation in the placebo group (15% vs. 8%). Although no differences in drug tolerability using the highest doses ever tested in clinical trials were found, this study showed the ineffectiveness of prazosin for sleep symptoms in PTSD. A possible justification for the negative result may involve the study selection bias, because clinically stable patients were recruited, which would make them less susceptible to improvements provided by anti-adrenergic treatment.
Patients who were unable or unwilling to discontinue the use of trazodone, an anti-depressant with alpha-1-adrenergic antagonist action, were not included in the study. These patients could be potential responders to prazosin, given a good response to the same pharmacological target [35].
The results of a study by Raskind et al. [35] showed that prazosin did not improve sleep-related problems in PTSD patients. The placebo response rate was quite high in this study. Prazosin could be effective in patients with psychosocial instability who might have a low placebo response rate that were included in the study because sleep disorders and psychosocial problems seem to co-occur frequently in this population. In addition, patients received relatively high doses of prazosin, with hypotensive effects. Nevertheless, the authors could not rule out the possibility that chronic symptoms of nocturnal PTSD may have been aggravated as an adverse effect of nocturnal hypotension caused by prazosin [36].
McCall et al. [37] evaluated prazosin’s single nocturnal intake and the impact on suicidal ideation in 20 PTSD patients, randomizing 10 patients to a control group and followed up for 8 weeks in both groups. The Scale for Suicide Ideation (SSI) and Columbia Suicide Severity Rating Scale (C-SSRS) demonstrated no association between the use of prazosin and improvements in suicidal ideation. Limitations of the study were a small number of patients involved and the single administration of medication. Previous studies showed overall clinical improvement in patients when the medication was also administered during the day but did not assess the specific suicidal ideation variable. Despite this finding, most studies showed the beneficial action of prazosin on PTSD.
A meta-analysis analyzed evidence from the literature on the role of prazosin for the treatment of PTSD. Of 402 articles selected, 6 studies were included in the systematic review and meta-analysis. The results showed that PTSD patients receiving prazosin showed significant improvement in nightmares [standardized mean difference (SMD)=1.01; 95% CI, 0.72–1.30], general PTSD symptoms (SMD=0.77; 95% CI, 0.48–1.06), and overall clinical improvement (MDS=0.94; 95% CI, 0.6–1.29) compared with a placebo/control group. Prazosin improved sleep quality (SMD=0.87; 95% CI, 0.55–1.19), hyperarousal symptoms (SMD=1.04; 95% CI, 0.23–1.84), content dreams (SMD=1.33; 95% CI, 0.69–1.97), and total sleep time (60.98 minutes; 95% CI, 18.69–103.26). Minor side effects were reported that were similar between prazosin and placebo groups. Prazosin may improve nightmares and general symptoms of PTSD, including hyperexcitation, sleep disturbance, total sleep time, and sleep quality [38].
A literature review of PTSD, prazosin, treatment, and resistance was also conducted. At least 10 clinical studies of prazosin for the treatment of PTSD have been published, including open and randomized controlled trials. These studies supported the effectiveness of prazosin for treating nightmares and improving sleep or reducing the severity of PTSD. They also showed that PTSD treatment with prazosin usually starts at a dose of 1 mg, with monitoring hypotension after the first dose. The dose is then gradually increased to maintenance levels of 2–6 mg at night. Studies of military veterans with PTSD used higher doses (10–16 mg at night). Prazosin was also studied in young and old adults with PTSD and in patients with alcohol problems; it reduced cravings and stress responses. Prazosin offers some hope for the treatment of resistant PTSD cases in which recurrent nightmares are problematic, with a relatively rapid response within weeks [39].
Another study and review explored the literature on the effectiveness of prazosin for treating nightmares in military veterans. Prazosin has been shown to be effective for treating PTSD trauma-related nightmares. Because of its low side-effect profile and ability to improve sleep and reduce nightmares of trauma, prazosin has been recommended as an adjuvant therapy. Prazosin should be started as an adjuvant treatment to promote sleep in those with PTSD nightmares. It should be started at 1 mg and titrated upward until the desired absence or reduction of nightmares is attained, with a maximum dosing recommendation of 20 mg at bedtime and 5 mg in the middle of the morning [40].
A review paper evaluated the clinical efficacy and safety of prazosin as the primary pharmacological treatment for PTSD. As a criterion for inclusion, studies had to test the efficacy of prazosin alone or added to ongoing treatment in adults with PTSD using validated tools to assess and monitor disorders, allow comparisons based on univariate analyses, and highlight identified adverse reactions. Twelve studies were included: five randomized controlled trials, four open prospective trials, and three retrospective archival reviews. The evaluation involved 276 patients exposed to civil (19%) or combat trauma (81%). Prazosin significantly decreased trauma nightmares, avoided hypervigilance, and improved patient status in all of the studies. No significant differences in blood pressure were observed at the end of the trials. In addition to the methodological and clinical biases of these studies, the present review not only confirmed the efficacy and good tolerability of prazosin but also suggested its possible use as a primary pharmacological treatment for PTSD [41].
At the childhood and adolescent level, a systematic review identified published articles evaluating the use of prazosin to treat PTSD-associated nightmares. We identified nine published articles related to the use of prazosin for the treatment of PTSD nightmares in children and adolescents. Six of the nine articles that met our inclusion criteria were case reports. These six case reports showed marked improvement in nightmares when Prazine was used, although at a generally lower dose than that used in adults, with doses ranging from 1 to 4 mg/day. Therefore, prazosin showed promising results for treating PTSD-associated nightmares in children and adolescents, although this has not been thoroughly studied. Future placebo-controlled studies are needed to evaluate the efficacy and safety of prazosin for treating PTSD-related nightmares in children and adolescents [42].
To understand and expand the use of prazosin, a recent case report described the successful titration of prazosin for PTSD symptoms in a 49-year-old man who was simultaneously prescribed carvedilol for hypertension. The patient had a previous unsuccessful prazosin trial due to adverse effects. His second prazosin study was effective and well tolerated using individualized titration with careful monitoring by experts. This case detailed the importance of using caution and close monitoring in prazosin dose titration in patients prescribed concomitant alpha-1 antagonists [43].
A recent study assessed elevated salivary alpha-amylase (sAA) activity in PTSD patients. As an alpha-1 NE receptor antagonist, prazosin would be expected to alter sAA values in PTSD patients. Thus, daytime sAA was analyzed in 20 patients with suicidal PTSD who were randomized to prazosin versus placebo only at bedtime and found no effect on daytime sAA. These findings were consistent with studies showing an advantage of twice-daily prazosin dosing in PTSD [44].
In a recent randomized, double-blind clinical trial, alcoholdependent veterans with PTSD (n=96) were randomized to prazosin (16 mg) or placebo in a 12-week outpatient clinical trial. The main effects of abstinence versus non-abstentionist status, treatment, and their interactions on changes in PTSD symptoms over time were examined. There was a major effect of abstinent alcohol status on PTSD symptoms (p=0.03) so that non-abstainers had lower total scores on the physicianadministered PTSD Administrative Scale (CAPS) than abstainers. There was significant treatment by the interaction of alcohol abstention status (p=0.01)—specifically, among placebotreated individuals, those who did not abstain from alcohol had lower total CAPS scores than alcohol abstainers. In the prazosin-treated group, abstainers and non-abstainers did not differ in the total CAPS score. The results were similar in the evasion (p=0.02), reexperience (p=0.01), and hyperstimulation (p=0.04) subscales so that non-recipients treated with placebo had lower CAPS scores in general. Treatment with prazosin was not significantly related to changes in PTSD symptoms throughout the 12-week clinical trial in a comorbid population. Interestingly, placebo-treated nonalcoholics had a significant reduction in PTSD symptoms [45].
The use of slow-release or fractional doses of prazosin may, in general, yield better results in assessments reporting general symptoms of the disorder as well as the expansion of studies of patients diagnosed with acute stress disorder. This could suggest a therapeutic effect that would reduce the symptoms and likelihood of PTSD development in these patients.
The authors’ criticism is that several clinical studies showed the relevant role of prazosin for the treatment of PTSD symptoms, especially regarding sleep symptomatology, high morbidity factors, and prevalence in patients. Prazosin is an affordable and cost-effective pharmacological option compared with other drugs used to treat PTSD.
New randomized, multicenter clinical studies still need to be conducted to generate a meta-analysis regarding the use of prazosin to establish a systematic review or meta-analysis with level 1A scientific evidence according to the Oxford classification.
Acknowledgments
None.
Footnotes
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Henrique Soares Paiva. Formal analysis: Henrique Soares Paiva, Idiberto José Zotarelli Filho. Investigation: Henrique Soares Paiva, Idiberto José Zotarelli Filho. Methodology: Henrique Soares Paiva, Idiberto José Zotarelli Filho. Supervision: Carlos Filinto da Silva Cais. Visualization: Carlos Filinto da Silva Cais. Writing—original draft: Henrique Soares Paiva. Writing—review & editing: Idiberto José Zotarelli Filho, Carlos Filinto da Silva Cais.
REFERENCES
- 1.Cabizuca M, Mendlowicz M, Marques-Portella C, Ragoni C, Coutinho ESF, Souza WF, et al. The invisible patients: posttraumatic stress disorder in parents of individuals with cystic fibrosis. Rev Psiq Clín. 2010;37:6–11. [Google Scholar]
- 2.Spottswood M, Davydow D, Huang H. The prevalence of posttraumatic stress disorder in primary care: a systematic review. Harv Rev Psychiatry. 2017;25:159–169. doi: 10.1097/HRP.0000000000000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military CombatRelated PTSD Nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26:24–33. doi: 10.1176/appi.neuropsych.13010006. [DOI] [PubMed] [Google Scholar]
- 4.Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation of trauma. Am J Psychiatry. 1996;153(7 Suppl):83–93. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- 5.Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med. 2017;47:2260–2274. doi: 10.1017/S0033291717000708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–547. doi: 10.1002/jts.21848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Ameringen M, Mancini C, Patterson B, Boyle MH. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. 2008;14:171–181. doi: 10.1111/j.1755-5949.2008.00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry. 2014;59:460–467. doi: 10.1177/070674371405900902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schestatsky S, Shansis F, Ceitlin LH, Abreu PBS, Hauck S. Historical evolution of the concept of posttraumatic stress disorder. Braz J Psychiatry. 2003;25(Suppl I):8–11. doi: 10.1590/s1516-44462003000500003. [DOI] [PubMed] [Google Scholar]
- 10.Lifton RJ, Olson E. The human meaning of total disaster. The Buffalo Creek Experience. Psychiatry. 1976;39:1–18. doi: 10.1080/00332747.1976.11023872. [DOI] [PubMed] [Google Scholar]
- 11.Geracioti TD, Baker DG, Ekhator NN, West SA, Hill KK, Bruce AB, et al. CSF norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158:1227–1230. doi: 10.1176/appi.ajp.158.8.1227. [DOI] [PubMed] [Google Scholar]
- 12.Hendrickson RC, Raskind MA. Noradrenergic dysregulation in the pathophysiology of PTSD. Exp Neurol. 2016;284:181–195. doi: 10.1016/j.expneurol.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Boehnlein JK, Kinzie JD. Pharmacologic reduction of CNS noradrenergic activity in PTSD: the case for clonidine and prazosin. J Psychiatr Pract. 2007;13:72–78. doi: 10.1097/01.pra.0000265763.79753.c1. [DOI] [PubMed] [Google Scholar]
- 14.Lydiard RB, Hamner MH. Clinical importance of sleep disturbance as a treatment target in PTSD. Spring. 2009;7:176–183. [Google Scholar]
- 15.Schoenfeld FB, Deviva JC, Manber R. Treatment of sleep disturbances in posttraumatic stress disorder: a review. J Rehabil Res Dev. 2012;49:729–752. doi: 10.1682/jrrd.2011.09.0164. [DOI] [PubMed] [Google Scholar]
- 16.Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170:208–211. doi: 10.1016/j.psychres.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Liempt S, Vermetten E, Geuze E, Westenberg HGM. Pharmacotherapy for disordered sleep in posttraumatic stress disorder: a systematic review. Int Clin Psychopharmacol. 2006;21:193–202. doi: 10.1097/00004850-200607000-00001. [DOI] [PubMed] [Google Scholar]
- 18.El-Solh AA. Management of nightmares in patients with posttraumatic stress disorder: current perspectives. Nat Sci Sleep. 2018;10:409–420. doi: 10.2147/NSS.S166089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George KC, Kebejian L, Ruth LJ, Miller CW, Himelhoch S. Meta-analysis of the efficacy and safety of prazosin versus placebo for the treatment of nightmares and sleep disturbances in adults with posttraumatic stress disorder. J Trauma Dissociation. 2016;17:494–510. doi: 10.1080/15299732.2016.1141150. [DOI] [PubMed] [Google Scholar]
- 20.Raskind MA, Dobie DJ, Kanter ED, Petrie EC, Thompson CE, Peskind ER. The alpha1-adrenergic antagonist prazosin ameliorates combat trauma nightmares in veterans with posttraumatic stress disorder: a report of 4 cases. J Clin Psychiatry. 2000;61:129–134. doi: 10.4088/jcp.v61n0208. [DOI] [PubMed] [Google Scholar]
- 21.Raskind MA, Thompson C, Petrie EC, Dobie DJ, Rein RJ, Hoff DJ, et al. Prazosin reduces nightmares in combat veterans with posttraumatic stress disorder. J Clin Psychiatry. 2002;63:565–568. doi: 10.4088/jcp.v63n0705. [DOI] [PubMed] [Google Scholar]
- 22.Taylor F, Raskind MA. The alpha1-adrenergic antagonist prazosin improves sleep and nightmares in civilian trauma posttraumatic stress disorder. J Clin Psychopharmacol. 2002;22:82–85. doi: 10.1097/00004714-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions 2019 [version 6.0] doi: 10.1002/14651858.ED000142. Available at: www.training.cochrane.org/handbook. [DOI] [PMC free article] [PubMed]
- 24.Peskind ET, Bonner LT, Hoff DJ, Raskind MA. Prazosin reduces trauma-related nightmares in older men with chronic posttraumatic stress disorder. J Geriatr Psychiatry Neurol. 2003;16:165–171. doi: 10.1177/0891988703256050. [DOI] [PubMed] [Google Scholar]
- 25.Raskind MA, Peskind ER, Kanter ED, Petri EC, Radant A, Thompson C, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160:371–373. doi: 10.1176/appi.ajp.160.2.371. [DOI] [PubMed] [Google Scholar]
- 26.Taylor FB, Lowe K, Thompson C, McFall M, Peskind ER, Kanter ED, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577–581. doi: 10.1016/j.biopsych.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 27.Taylor FB, Martin P, Thompson C, Williams J, Mellman TA, Gross C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63:629–632. doi: 10.1016/j.biopsych.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, et al. A parallel group placebo-controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry. 2007;61:928–934. doi: 10.1016/j.biopsych.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 29.Germain A, Richardson R, Moul DE, Mammen O, Haas G, Forman GD, et al. Placebo-controlled comparison of prazosin and cognitive-behavioral treatments for sleep disturbances in US Military Veterans. J Psychosom Res. 2012;72:89–96. doi: 10.1016/j.jpsychores.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170:1003–1010. doi: 10.1176/appi.ajp.2013.12081133. [DOI] [PubMed] [Google Scholar]
- 31.Ahmadpanaha M, Sabzeieea P, Hosseini SM, Torabian S, Haghighi M, Jahangard L, et al. Comparing the effect of prazosin and hydroxyzine on sleep quality in patients suffering from posttraumatic stress disorder. Neuropsychobiology. 2014;69:235–242. doi: 10.1159/000362243. [DOI] [PubMed] [Google Scholar]
- 32.De Berardis D, Marini S, Serroni N, Iasevoli F, Tomasetti C, de Bartolomeis A, et al. Targeting the noradrenergic system in posttraumatic stress disorder: a systematic review and meta-analysis of prazosin trials. Curr Drug Targets. 2015;16:1094–1106. doi: 10.2174/1389450116666150506114108. [DOI] [PubMed] [Google Scholar]
- 33.Seda G, Sanchez-Ortuno MM, Welsh CH, Halbower AC, Edinger JD. Comparative meta-analysis of prazosin and imagery rehearsal therapy for nightmare frequency, sleep quality, and posttraumatic stress. J Clin Sleep Med. 2015;11:11–22. doi: 10.5664/jcsm.4354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Khachatryan D, Groll D, Booij L, Sepehry AA, Schütz CG. Prazosin for treating sleep disturbances in adults with posttraumatic stress disorder: a systematic review and meta-analysis of randomized controlled trials. Gen Hosp Psychiatry. 2016;39:46–52. doi: 10.1016/j.genhosppsych.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Raskind MA, Peskind ER, Chow B, Harris C, Davis-Karim A, Holmes HA, et al. Trial of prazosin for post-traumatic stress disorder in military veterans. N Engl J Med. 2018;378:507–517. doi: 10.1056/NEJMoa1507598. [DOI] [PubMed] [Google Scholar]
- 36.Glue P, Barak Y. Prazosin for post-traumatic stress disorder. N Engl J Med. 2018;378:1649. doi: 10.1056/NEJMc1803171. [DOI] [PubMed] [Google Scholar]
- 37.McCall WV, Pillai A, Case D, McCloud L, Nolla T, Branch F, et al. A pilot, randomized clinical trial of bedtime doses of prazosin versus placebo in suicidal posttraumatic stress disorder patients with nightmares. J Clin Psychopharmacol. 2018;38:618–621. doi: 10.1097/JCP.0000000000000968. [DOI] [PubMed] [Google Scholar]
- 38.Singh B, Hughes AJ, Mehta G, Erwin PJ, Parsaik AK. Efficacy of prazosin in posttraumatic stress disorder: a systematic review and meta-analysis. Prim Care Companion CNS Disord. 2016;18 doi: 10.4088/PCC.16r01943. [DOI] [PubMed] [Google Scholar]
- 39.Green B. Prazosin in the treatment of PTSD. J Psychiatr Pract. 2014;20:253–259. doi: 10.1097/01.pra.0000452561.98286.1e. [DOI] [PubMed] [Google Scholar]
- 40.Breen A, Blankley K, Fine J. The efficacy of prazosin for the treatment of posttraumatic stress disorder nightmares in U.S. military veterans. J Am Assoc Nurse Pract. 2017;29:65–69. doi: 10.1002/2327-6924.12432. [DOI] [PubMed] [Google Scholar]
- 41.Simon PY, Rousseau PF. Treatment of post-traumatic stress disorders with the alpha-1 adrenergic antagonist prazosin. Can J Psychiatry. 2017;62:186–198. doi: 10.1177/0706743716659275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akinsanya A, Marwaha R, Tampi RR. Prazosin in children and adolescents with posttraumatic stress disorder who have nightmares: a systematic review. J Clin Psychopharmacol. 2017;37:84–88. doi: 10.1097/JCP.0000000000000638. [DOI] [PubMed] [Google Scholar]
- 43.Khaw C, Argo T. Prazosin initiation and dose titration in a patient with posttraumatic stress disorder on concurrent carvedilol. Ment Health Clin. 2019;9:326–330. doi: 10.9740/mhc.2019.09.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McCall WV, Pillai A, Pandya CD, McCloud L, Moraczewski JA, Tauhidul L, et al. Bedtime doses of prazosin do not affect daytime salivary amylase markers in PTSD. Heliyon. 2019;5:e01709. doi: 10.1016/j.heliyon.2019.e01709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verplaetse TL, Ralevski E, Roberts W, Gueorguieva R, McKee SA, Petrakis IL. Alcohol abstainer status and prazosin treatment in association with changes in posttraumatic stress disorder symptoms in veterans with comorbid alcohol use disorder and posttraumatic stress disorder. Alcohol Clin Expl Res. 2019;43:741–746. doi: 10.1111/acer.13969. [DOI] [PMC free article] [PubMed] [Google Scholar]


