Abstract
Electronic health records (EHRs) allow for meaningful usage of healthcare data. Their adoption provides clinicians with a central location to access and share data, write notes, order labs and prescriptions, and bill for patient visits. However, as non-clinical requirements have increased, time spent using EHRs eclipsed time spent on direct patient care. Several solutions have been proposed to minimize the time spent using EHRs, though each have limitations. Digital scribe technology uses voice-to-text software to convert ambient listening to meaningful medical notes and may eliminate the physical task of documentation, allowing physicians to spend less time on EHR engagement and more time with patients. However, adoption of digital scribe technology poses many barriers for physicians. In this study, we perform a scoping review of the literature to identify barriers to digital scribe implementation and provide solutions to address these barriers. We performed a literature review of digital scribe technology and voice-to-text conversion and information extraction as a scope for future research. Fifteen articles met inclusion criteria. Of the articles included, four were comparative studies, three were reviews, three were original investigations, two were perspective pieces, one was a cost-effectiveness study, one was a keynote address, and one was an observational study. The published articles on digital scribe technology and voice-to-text conversion highlight digital scribe technology as a solution to the inefficient interaction with EHRs. Benefits of digital scribe technologies included enhancing clinician ability to navigate charts, write notes, use decision support tools, and improve the quality of time spent with patients. Digital scribe technologies can improve clinic efficiency and increase patient access to care while simultaneously reducing physician burnout. Implementation barriers include upfront costs, integration with existing technology, and time-intensive training. Technological barriers include adaptability to linguistic differences, compatibility across different clinical encounters, and integration of medical jargon into the note. Broader risks include automation bias and risks to data privacy. Overcoming significant barriers to implementation will facilitate more widespread adoption.
Supplementary information
The online version contains supplementary material available at 10.1007/s12553-021-00568-0.
Keywords: Digital scribe, Health information technology, Speech recognition software, Professional burnout, Documentation, Electronic health record
Introduction
As the inadequacies of paper medical charts became apparent, electronic health records (EHRs) began to revolutionize healthcare delivery [1]. They provided clinicians with decision support tools, allowed for data sharing between both providers and patients, and served as large repositories of healthcare data [2–4]. Despite their central role in reshaping modern healthcare, EHRs posed many problems for physicians. As documentation increased due to regulatory requirements, physicians found themselves spending more time charting than on clinical care; [4] for each hour they spent on direct patient care, they spent up to two hours on EHR-related tasks both during and outside of clinic hours [5]. They noted too many clicks per task, redundancy within the patient record, and excessive data entry for quality control, screening, and billing purposes [6], ultimately lowering the amount of time spent on direct patient care and subsequently affecting the quality of care delivered [3, 5, 7, 8]. Further, adoption of the EHR came with high upfront costs, resulted in loss of physician productivity due to adoption and training, and increased physician turnover due to low satisfaction [8–10]. As the inefficiencies of the EHR became apparent, solutions including medical scribes were proposed.
Medical scribes alleviated the data entry burden that was placed on physicians with the emergence of EHRs and assisted with documentation, billing, data capture, and other tasks such as placing orders and pending medications, allowing physicians to spend more time on clinical care [11]. While medical scribes improved physician workflow and maintained patient satisfaction, studies demonstrated many issues with their use including time-intensive training, high turnover rates, and costs of up to $50,000 per year depending on the scribe’s scope and employee classification [12–14]. Amid mounting pressures to limit exposure and enforce social distancing during the COVID-19 pandemic, many medical scribes were transitioned to “telescribes,” paralleling the dramatic rise in virtual visits and telemedicine-based clinical encounters. To use telescribes, physicians use recording devices (which may included dedicated hardware or the physician’s own mobile device) to capture audio during patient visits, which then gets transcribed later by a remote telescribe. While this solution enabled documentation to be completed remotely and limited the number of medical professionals in a patient room, its adoption also posed several drawbacks [15] such as a time lag between the patient visit and the note transcription. Therefore, physicians still had to complete some of the traditional documentation duties such as ordering medications, lab work, and/or imaging to ensure that patients were treated in a timely manner. Further, this time lag was not conducive to real time collaboration with the physician, preventing scribes from clarifying terminology, the location of lesions and pertinent exam findings, resulting in incomplete or even inaccurate clinical notes.
Fortunately, a recent development addresses the inefficiencies of the EHR and their suboptimal solutions: the digital scribe – a novel piece of technology that uses voice-to-text software, artificial intelligence, and machine learning to transform clinical interactions into meaningful medical notes through ambient listening and subsequent voice-to-text conversion [16–18]. While digital scribe technology has the potential to once again revolutionize medical charting, order entry, and the physician–patient relationship, many barriers exist to its implementation. In this manuscript, we perform a scoping review of the literature to identify barriers to digital scribe implementation and provide solutions to address these barriers.
Methods
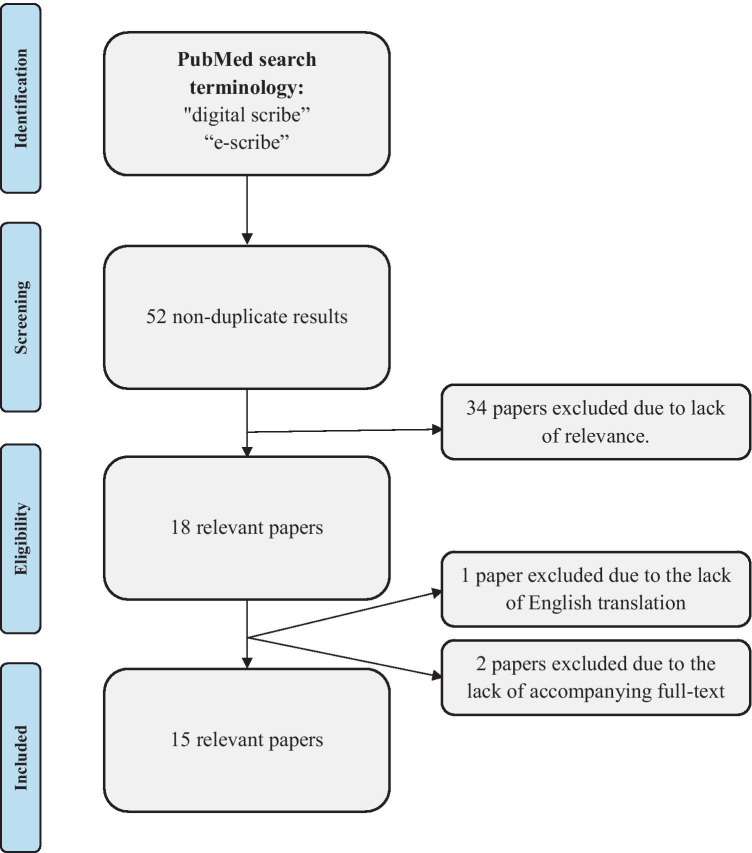
To investigate and assess the barriers to digital scribe implementation in healthcare, we conducted a scoping review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (Fig. 1) [20]. We searched Medline using the search terms "digital scribe", “e-scribe”, and “voice to text transcription” (October 2020). We also scanned reference lists of relevant publications for additional articles. The abstracts were read by the authors and articles that did not focus on digital scribe technology were excluded. The abstracts of the remaining papers were read for relevance. Non-English papers and abstracts lacking an accompanying full text were excluded. Because of the rapidly evolving nature of this field, proceedings and perspective pieces were included. Two reviewers (SG and AF) independently screened all articles using inclusion and exclusion criteria.
Fig. 1.
Inclusion Flowchart following the PRISMA-ScR statement
Results
Our search resulted in 52 non-duplicate results. After screening the titles and abstracts of these articles, we assessed 34 for eligibility. We included 15 papers in our analysis (Fig. 1, Supplementary Table I). Of the articles included, four were comparative studies, three were reviews, three were original investigations, two were perspective pieces, one was a cost-effectiveness study, one was a keynote address, and one was an observational study.
One study captured the structure of a physician visit to determine digital scribe feasibility; [21] it found that patient visits were non-linear, posing difficulty for traditional voice-to-text technology to capture, analyze, and include only relevant information [21]. Six studies examined the intricacies of digital scribe technology and compared different types of speech-to-text software [17, 18, 22–25]. The types of voice-to-text methodologies included a Connectionist temporal Classification phenome-based model, a Listen Attend and Spell grapheme based model [17], natural language processing [22], concatenation and speech unit extraction [23], automated indexing [25], NOMINDEX [24], and VoiceReport™ [18]. Two studies evaluated the efficacy of voice recognition software and determined that summarization technology is feasible in non-linear settings, and that computer-based systems can be successfully used in clinical practice [29, 30]. Five studies detailed practicalities of digital scribe integration and its associated challenges; [16, 19, 26–28] two of these detailed how the current way of practicing medicine must change in order to work with digital scribe technology [16, 27], one detailed how implementation can be done in discreet steps allowing for physicians to train the digital scribe to ultimately work together [19], and two outlined details of implementation and potential barriers [26, 28]. Finally, one study evaluated the cost effectiveness of implementing digital scribe technology into clinical practice [31].
Discussion
This scoping review provides an overview of the current utility and feasibility of digital scribe technology and barriers to its implementation. Digital scribes have the potential to disrupt the medical documentation market and address several underlying inefficiencies of the EHR. Through its novel technology, the digital scribe can transform physician–patient conversations into meaningful notes, significantly reducing the time spent charting and the need for additional care team members [14, 16].
Utility of the digital scribe
As EHR-based administrative requirements have increased, patients have become concerned that physicians are spending less time with them and more time with their digital devices [32]. While completion of many administrative tasks ensures the delivery of high quality clinical care, research has shown that a physician’s interaction with the EHR during visits can leave patients feeling as if the visit was impersonal and formulaic [33, 34]. With the introduction of digital scribe technology, physicians can spend less patient visit time on the EHR and more time with their patients improving many aspects of the visit (Fig. 1). Importantly, digital scribe technology requires minimal training, and costs significantly less than traditional medical scribes and newer telescribes [35, 36]. Although this technology has yet to gain widespread traction in the healthcare field, it has been broadly adopted in the software field, and is a plausible tool that can reduce documentation time, eliminate the need for a medical scribe, and transform the physician–patient visit, allowing physicians to work at the top of their license while enhancing the patient experience [6, 16]. Furthermore, the digital scribe has the ability to address one of the root causes of physician burnout. Over the past several years, the EHR has been cited as a significant source of burnout, and thus a hurdle in achieving the quadruple aim of healthcare: [1] population health, [2] experience of care, [3] per capita costs, [4] provider satisfaction [14, 37]. Despite the introduction of organization-directed solutions such as medical scribes and telescribes, studies continue to demonstrate that physicians experience burnout largely in part due to growing clinical and non-clinical (i.e. billing, quality control, screening) documentation requirements [6, 38]. By adopting digital scribe technology, a significant portion of physician-led documentation requirements may be eliminated, helping to reduce physician burnout driven by documentation and other EHR-based tasks.
Barriers and solutions
Although the studies evaluated discuss how digital scribes appear to be powerful aides for EHR navigation and charting related inefficiencies, the digital scribe’s impact on the healthcare field remains to be fully captured, as this technology is still novel and its use emerging. There are several important barriers to consider for digital scribe implementation (Table 1). First, physicians must be trained on how to use digital scribe technology. This time intensive process may require clinic modifications (e.g. reduced patient census, addition of trainees or superusers during initial implementation phases) or increased time spent outside of clinic hours learning how to use the technology, with or without compensation [27]. While the time spent learning how to interact with the digital scribe will be beneficial once perfected, learning how to use and incorporate a new technology can be a significant undertaking – a familiar experience for physicians who practiced through periods of initial EHR adoption [39, 40]. Although long term benefits may be realized, short term digital scribe adoption-related burnout cannot be excluded. Digital scribe implementation must be rolled-out thoughtfully, with user preferences held in high regard. Further, super users, role-based training, and process-based training can help ensure effective execution of digital scribe implementation [41].
Table 1.
Barriers and Potential Solutions to Digital Scribe Implementation
| Barriers to Digital Scribe Implementation: | Potential Solutions: |
|---|---|
| Upfront costs |
• Staged furlough of medical scribes and/or telescribes • Increased clinic efficiency may offset implementation costs within a short timeframe |
| Time-intensive training period for physicians with risk of digital scribe adoption-related burnout |
• Vendor super user, role-based, and process-based training • Financial compensation for training • Reduced patient census and/or addition of additional trainees during implementation period |
| Linguistic variation and unique medical jargon use |
• Adaptability to linguistic differences • Integration of medical jargon into the medical note • Compatibility with different types of clinical encounters (e.g. health maintenance, procedure, subspecialty visit) |
| Medicolegal compliance |
• Quality checks when utilizing digital scribe technology to ensure accuracy and reduce automation bias • HIPAA-certified technology • Protected database of raw files • Adverse event reporting process |
| Interoperability with existing computer systems |
• Buy-in from EHR providers • In house Help Desk training to address and rectify technological issues |
Because physicians work in several fields with different patient populations, the digital scribe must be trained to adapt to different languages, styles, accents, and visit types [19]. The software and algorithms underlying digital scribe technologies must also be trained to understand medical terminology and must formulate a comprehensive clinical encounter from a transcript in a way that accurately uses these words and phrases. This may prove to be difficult given the non-linear format of natural conversations and redundancy of conversations during a visit, as studies have shown that 80% of conversation capture is unnecessary for meaningful note generation [26]. Further, this task may require additional time-intensive editing by the clinician if the speech-to-text conversion is inaccurate due to deficiencies in the lexicon of the digital scribe [24, 30, 42].
Aside from the technical barriers to digital scribe implementation, there are both privacy and legal concerns (Table 1). Although digital scribes will be trained to accurately document a clinical encounter, there is a risk that the scribe could incorrectly interpret part of the visit, warranting the need for preserving raw transcript files to ensure legal compliance [42]. Importantly, automation bias can also occur if clinicians rely exclusively on the technology and its suggestions, necessitating the use of checkpoints to ensure accurate digital scribe assistance [30]. Further, there is always a risk of a data breach, which could compromise patient safety; care must be taken to ensure that digital scribe technology is adequately encrypted to prevent data breaches and ensure HIPAA compliance. Interoperability with existing computer systems is also vital for the success of digital scribe technology. Without interoperability, the digital scribe will simply add an additional step to the physician’s charting duties, increasing inefficiencies. Therefore, there must be proof-of-concept and subsequent buy-in from major EHR providers – steps that could be time and cost intensive. If there is no buy-in from these organizations, the digital scribe’s utility is limited and may prevent its adoption entirely amongst the medical community.
Strengths and limitations
The current work is the first review of available literature on the barriers to implementation of a digital scribe. While digital scribe development and implementation is still in its early stages, we believe our search strategy was comprehensive and captured current available literature detailing this novel technology. There are several limitations to this review. Given that this technology is novel, there are limited studies available for review. Further, many of the articles available are perspective pieces or theoretical in nature and therefore cannot provide significant quantitative data on the impact of digital scribes on clinical practice. The technology is in its early stages in clinical practice, and therefore additional data must be collected prior to making significant conclusions on the operational and financial utility of this technology. Further, the search was conducted using the English language and excludes all non-English articles.
Future areas of research & projects in development
There are many areas for future research using this novel technology. Because the digital scribe listens and transcribes throughout the entire visit, it limits the potential for billing subjectivity–an issue that has been addressed in the literature [43]. By shifting billing responsibilities from physicians and their clinical staff to the digital scribe, there is less room for interpretation, and there could be differences in claims data that would be important to examine. Thus, it is essential to compare claims data before and after digital scribe introduction to determine how costs (to the patient, provider, and overall healthcare system) differ with the adoption of this novel technology.
Additionally, there is a limited peer-reviewed data with respect to use of digital scribe technology in clinical settings. While it has the ability to transform the physician visit, it must be studied further. Further analyses are warranted to determine if this technology can create significant operational changes within clinical practice settings and improve physician satisfaction. Several studies have demonstrated that while there are substantial upfront costs (technology, integration with EHR, lost revenue due to physician training) that come with digital scribe implementation, the cost savings that the technology provides are significant [30, 31]. Therefore, additional post-implementation analyses should be conducted to determine the time necessary for practices to recover their upfront implementation costs.
Multiple technology companies, including manufacturers of EHRs, currently have digital scribe products in development and pilot studies have demonstrated accuracy in clinical documentation, ease of integration into existing EHRs, and additional time available for physicians to spend with their patients [35, 44, 45]. This technology has the potential to transform the healthcare industry and rigorous studies are warranted to determine the validity of the software and its integration with the EHR itself. Seeing digital scribe technology used in conjunction with EHRs will not only prove that this technology can be the new gold standard of healthcare documentation but will also be critical for achieving interoperability. Although this technology is promising, limitations to widespread adoption exist. While patients and physicians can interact during a visit, there is relevant information that is not explicitly vocalized during the visit (e.g., details of a recent hospital stay, messages sent through the patient portal, labs obtained at an outside location, etc.) and until this can be accurately integrated into patient notes, the capabilities of the digital scribe will remain limited.
Conclusion
Digital scribe technologies have the ability to decrease the amount of time physicians spend on documentation and order-entry tasks, allowing for more time spent on direct patient care. By minimizing documentation, physicians can limit time spent during and outside of clinical encounters on the EHR, improving physician satisfaction [39]. However, there are several barriers to implementation including upfront costs, time-intensive training period for physicians, linguistic variations, medicolegal compliance, and interoperability with existing computer systems. Thus, although the novel digital scribe technology boasts several benefits for patients, physicians, and the healthcare system overall, its barriers must be addressed in order to ensure efficient integration. Promoting future studies to capture the quantitative impacts of digital scribe implementation are necessary.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This study did not receive funding.
Declarations
Conflicts of interest
The authors have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ornstein SM, Oates RB, Fox GN. The computer-based medical record: current status. J Fam Pract. 1992;35(5):556–565. [PubMed] [Google Scholar]
- 2.Nguyen L, Bellucci E, Nguyen LT. Electronic health records implementation: An evaluation of information system impact and contingency factors. Int J Med Inform. 2014;83(11):779–796. doi: 10.1016/j.ijmedinf.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 3.King J, Patel V, Jamoom EW, Furukawa MF. Clinical benefits of electronic health record use: National findings. Health Serv Res. 2014;49(1 PART 2):392–404. 10.1111/1475-6773.12135. [DOI] [PMC free article] [PubMed]
- 4.Kuhn T, Basch P, Barr M, et al. Clinical documentation in the 21st century: Executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. 2015;162(4):301–303. doi: 10.7326/M14-2128. [DOI] [PubMed] [Google Scholar]
- 5.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: Primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med. 2017;15(5):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kroth PJ, Morioka-Douglas N, Veres S, et al. The electronic elephant in the room: Physicians and the electronic health record. JAMIA Open. 2018;1(1):49–56. doi: 10.1093/jamiaopen/ooy016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gold M, McLaughlin C. Assessing HITECH Implementation and Lessons: 5 Years Later. Milbank Q. 2016;94(3):654–687. doi: 10.1111/1468-0009.12214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177(12):1826–1832. doi: 10.1001/jamainternmed.2017.4340. [DOI] [PubMed] [Google Scholar]
- 9.Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47–55. doi: 10.2147/RMHP.S12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of Unintended Consequences Related to Computerized Provider Order Entry. J Am Med Inform Assoc. 2006;13(5):547–556. doi: 10.1197/jamia.M2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bossen C, Chen Y, Pine KH. The emergence of new data work occupations in healthcare: The case of medical scribes. Int J Med Inform. 2019;123:76–83. doi: 10.1016/j.ijmedinf.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Brady K, Shariff A. Virtual medical scribes: making electronic medical records work for you. J Med Pract Manage. 2013;29:133–136. [PubMed] [Google Scholar]
- 13.Walker KJ, Dunlop W, Liew D, et al. An economic evaluation of the costs of training a medical scribe to work in Emergency Medicine. Emerg Med J. 2016;33(12):865–869. doi: 10.1136/emermed-2016-205934. [DOI] [PubMed] [Google Scholar]
- 14.Bodenheimer T, Sinsky C. From triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Noordzij R, Plocienniczak MJ, Brook C. Virtual scribing within otolaryngology during the COVID-19 pandemic and beyond. Am J Otolaryngol - Head Neck Med Surg. 2020;41(5). 10.1016/j.amjoto.2020.102611. [DOI] [PMC free article] [PubMed]
- 16.Quiroz JC, Laranjo L, Kocaballi AB, Berkovsky S, Rezazadegan D, Coiera E. Challenges of developing a digital scribe to reduce clinical documentation burden. NPJ Digit Med. 2019;2(1):1–6. 10.1038/s41746-019-0190-1. [DOI] [PMC free article] [PubMed]
- 17.Chiu CC, et al. Speech recognition for medical conversations. arXiv preprint arXiv:1711.07274. 2017.
- 18.Klatt EC. Voice-activated dictation for autopsy pathology. Comput Biol Med. 1991;21(6):429–433. doi: 10.1016/0010-4825(91)90044-A. [DOI] [PubMed] [Google Scholar]
- 19.Coiera E, Kocaballi B, Halamaka J, Laranjo L. The digital scribe. NPJ Digit Med. 2018;1(1):1–5. doi: 10.1038/s41746-018-0066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 21.Kocaballi AB, Coiera E, Tong HL, et al. A network model of activities in primary care consultations. J Am Med Inform Assoc. 2019;26(10):1074–1082. doi: 10.1093/jamia/ocz046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedman C, Shagina L, Lussier Y, Hripcsak G. Automated encoding of clinical documents based on natural language processing. J Am Med Inform Assoc. 2004;11(5):392–402. doi: 10.1197/jamia.M1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Furui S, Kikuchi T, Shinnaka Y, Hori C. Speech-to-text and speech-to-speech summarization of spontaneous speech. In: IEEE Transactions on Speech and Audio Processing. 2004;12:401–8. 10.1109/TSA.2004.828699.
- 24.Happe A, Pouliquen B, Burgun A, Cuggia M, Le Beux P. Combining voice recognition and automatic indexing of medical reports. In: Studies in Health Technology and Informatics. IOS Press. 2002;90:382–7. 10.3233/978-1-60750-934-9-382. [PubMed]
- 25.Happe A, Pouliquen B, Burgun A, Cuggia M, Le Beux P. Automatic concept extraction from spoken medical reports. Int J Med Inform. 2003;70(2–3):255–263. doi: 10.1016/S1386-5056(03)00055-8. [DOI] [PubMed] [Google Scholar]
- 26.Quiroz JC, Laranjo L, Kocaballi AB, et al. Identifying relevant information in medical conversations to summarize a clinician-patient encounter. Health Informatics J. 2020;26(4):2906–2914. doi: 10.1177/1460458220951719. [DOI] [PubMed] [Google Scholar]
- 27.Coiera E. The Price of Artificial Intelligence. Yearb Med Inform. 2019;28(1):14–15. doi: 10.1055/s-0039-1677892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finley G, Edwards E, Robinson A, et al. An automated medical scribe for documenting clinical encounters. In: Association for Computational Linguistics (ACL). 2018:11–5. 10.18653/v1/n18-5003.
- 29.Afantenos S, Karkaletsis V, Stamatopoulos P. Summarization from medical documents: A survey. Artif Intell Med. 2005;33(2):157–177. doi: 10.1016/j.artmed.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 30.Al-Aynati MM, Chorneyko KA. Comparison of voice-automated transcription and human transcription in generating pathology reports. Arch Pathol Lab Med. 2003;127(6):721–725. doi: 10.5858/2003-127-721-COVTAH. [DOI] [PubMed] [Google Scholar]
- 31.Henricks WH, Roumina K, Skilton BE, Ozan DJ, Goss GR. The utility and cost effectiveness of voice recognition technology in surgical pathology. Mod Pathol. 2002;15(5):565–571. doi: 10.1038/modpathol.3880564. [DOI] [PubMed] [Google Scholar]
- 32.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14(1 SUPPL.):S34. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robbins JA, Bertakis K, Helms LJ, Azari R, Callahan EJ. The influence of physician practice behaviors on patient satisfaction. Fam Med. 1993;25(1):17–21. [PubMed] [Google Scholar]
- 34.Mawardi BH. Satisfactions, Dissatisfactions, and Causes of Stress in Medical Practice. JAMA J Am Med Assoc. 1979;241(14):1483–1486. doi: 10.1001/jama.1979.03290400043020. [DOI] [PubMed] [Google Scholar]
- 35.Amazon Transcribe Pricing – Amazon Web Services (AWS). Accessed 6 May 2021. https://aws.amazon.com/transcribe/pricing/.
- 36.PredictionHealth. Accessed 9 May 2021. https://www.predictionhealth.com/?utm_term=medicalscribe&utm_campaign=Telehealth-Leads-v1-simplify&utm_source=adwords&utm_medium=ppc&hsa_acc=4090761405&hsa_cam=9836647566&hsa_grp=99419083406&hsa_ad=436884752833&hsa_src=g&hsa_tgt=kwd-604159548&hsa_kw=medicalscribe&hsa_mt=b&hsa_net=adwords&hsa_ver=3&gclid=CjwKCAjwxuuCBhATEiwAIIIz0W4YIPLVGNdB3ytcF3WqoISV43LpUYLJyj-IWJiGnQ5Wb_h0UGL7CBoCIBcQAvD_BwE.
- 37.Berwick DM, Nolan TW, Whittington J. The triple aim: Care, health, and cost. Health Aff. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 38.DeChant PF, Acs A, Rhee KB, et al. Effect of Organization-Directed Workplace Interventions on Physician Burnout: A Systematic Review. Mayo Clin Proc Innov Qual Outcomes. 2019;3(4):384–408. doi: 10.1016/j.mayocpiqo.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meigs SL, Solomon M. Electronic Health Record Use a Bitter Pill for Many Physicians. Perspect Heal Inf Manag. 2016;13(Winter). Accessed 9 May 2021. /pmc/articles/PMC4739443/. [PMC free article] [PubMed]
- 40.Turner TB, Dilley SE, Smith HJ, et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: A decision analysis. Gynecol Oncol. 2017;146(3):642–646. doi: 10.1016/j.ygyno.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 41.How should I train my staff? | HealthIT.gov. Accessed 9 May 2021. https://www.healthit.gov/faq/how-should-i-train-my-staff.
- 42.Elwyn G, Barr PJ, Piper S. Digital clinical encounters: Managed safely, digital recordings could transform healthcare. BMJ. 2018;361. 10.1136/bmj.k2061. [DOI] [PubMed]
- 43.Valle L, Weng J, Jagsi R, et al. Assessment of Differences in Clinical Activity and Medicare Payments Among Female and Male Radiation Oncologists. JAMA Netw Open. 2019;2(3):e190932. doi: 10.1001/jamanetworkopen.2019.0932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.AI-Powered Medical Documentation Tech - DeepScribe. Accessed 9 May 2021. https://www.deepscribe.ai/technology.
- 45.Saykara | AI Assistant for Physicians. Accessed 9 May 2021. https://www.saykara.com/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.