Abstract
Purpose:
To assess agreement between Humphrey Visual Field Analyzer 10-2 and 24-2C test protocols for detecting glaucomatous defects in the central 10° of the visual field (CVFDs).
Methods:
VFs from 165 eyes of 18 healthy individuals, 12 glaucoma suspects and 62 glaucoma patients who completed 10-2 and 24-2C VF testing protocols within six months were included. CVFDs on 10-2 and 24-2C (within the central 22 points) test grids required a cluster of 3 contiguous points with p<5%, 5% and 1% or <5%, 2%, and 2% within a hemifield on the TD or PD plot. Cohen’s Kappa (k) was used to assess agreement between 10-2 and 24-2C test grids in identifying CVFDs. Specificity of each testing strategy was assessed in VFs from healthy eyes.
Results:
CVFDs in suspect and glaucoma eyes were combined and reported as localized to superior, inferior or both hemifields based on TD and PD plots for 10-2 and 24-2C test grids. Moderate to substantial agreement was observed between 10-2 and 24-2C grids for detecting any CVFD from PD (k=0.551) and TD (k=0.651) plots. Specificity was high in healthy eyes ranging from 0.94 to 1.0 for both test protocols.
Conclusion:
Substantial agreement for identifying CVFDs using the 24-2C and 10-2 protocols suggests that combining tests by adding central test points to the 24-2 test grid may supplant the need for two perimetry regimens for detecting central and peripheral glaucomatous visual field damage.
Keywords: Glaucoma, visual field, HFA, 24-2C, 10-2
PRECIŚ
Moderate to substantial agreement between 10-2 and 24-2C perimetry for detecting central field defects suggests that adding central test points to the 24-2 protocol may improve efficiency of visual field testing for glaucoma management.
INTRODUCTION
The presence of central visual field defects (CVFD) in glaucoma has been acknowledged for decades.1, 2 Recently there has been a resurgence of interest in the importance of CVFDs spearheaded by several researchers3-5 who have provided substantial evidence using results from the Humphrey Field Analyzer 10-2 automated perimetry test protocol that early glaucoma can result in a decrease in central visual sensitivity. This is particularly important because CVFDs cause a greater decrease in vision-related quality of life than peripheral VF defects6, 7 likely because central vision is more important than peripheral vision for conducting everyday tasks including facial identification, reading, writing, shopping and driving.8
The current standard of care for glaucoma detection and monitoring includes primarily visual field testing using the 24-2 testing protocol. Adding 10-2 testing to a perimetry testing regimen to detect CVFDs would almost double the testing time required which may not be feasible in clinical practice. To address this issue, central test points from the 10-2 test grid have been added to the 24-2 test resulting in a modified 24-C testing grid.9, 10 The 24-2C protocol adds the 10 most commonly abnormal central test points from the 10-2 grid to the standard 24-2 test grid. This enables peripheral and central VF testing within a single examination. Improved test time is achieved by employing the new SITA Faster testing algorithm.
The purpose of the current study was to assess the agreement between Humphrey Field Analyzer (HFA) 10-2 and HFA3 24-2C tests for detecting defects in the central 10 degrees of the visual field. Good agreement among tests would inform the relative usefulness of the 24-2C for detecting VF defects identified by the combined use of 24-2 and 10-2 testing.
MATERIALS AND METHODS
In this cross-sectional study, VFs from 165 eyes of 92 healthy individuals, glaucoma suspects and glaucoma patients from the ongoing Diagnostic Innovations in Glaucoma Study (DIGS), who completed 24-2, 10-2 and 24-2C VF testing within six months were analyzed. Eligible participants had best corrected visual acuity of 20/40 or better, spherical refraction within ±5.0 diopters (D), cylinder correction within ±3.0 D and open angles on gonioscopy. Study participants were excluded if they had a history of intraocular surgery (except for uncomplicated cataract or uncomplicated glaucoma surgery). Eyes with coexisting retinal disease, uveitis, or non-glaucomatous optic neuropathy also were excluded. Diabetic participants with no evidence of retinal involvement were included.
Healthy eyes had a healthy appearing optic disc and surrounding retinal nerve fiber layer (RNFL) based on masked assessment of digital stereoscopic photographs with no history of repeatable abnormal standard automated perimetry (SAP) VF results (HFA II with 24-2 testing using the Swedish Interactive Thresholding Algorithm, Carl Zeiss Meditec Inc., Dublin, CA) and no history of elevated intraocular pressure (IOP) (all IOP ≤ 21 mm Hg) OU. Normal VFs were defined as those with mean deviation (MD) and pattern standard deviation (PSD) within 95% confidence limits (95% CI) and a Glaucoma Hemifield Test (GHT) result within normal limits.
Glaucoma suspect eyes had suspicion of glaucomatous optic neuropathy (GON) without evidence of repeatable VFs outside of normal limits. GON was defined based on a global or local decrease in neuroretinal rim width or notching or a localized or diffuse retinal nerve fiber layer defect indicative of glaucoma based on stereophotograph assessment by two independent graders. In cases of disagreement a GON or no GON decision was made by consensus discussion or adjudication by a third grader.
Glaucoma patient eyes had at least 2 consecutive and reliable (defined below) 24-2 VF examinations with either PSD ≤ 5% or a GHT result outside of the 99% normal limits with similar patterns of glaucoma-related defects in consecutive exams determined by investigator assessment.
All VFs were evaluated by UC San Diego Visual Field Assessment Center (VisFACT) personnel based on a standardized protocol. Visual fields with more than 33% fixation losses or false-negative errors or more than 20% false-positive errors were automatically excluded. Visual fields exhibiting a learning effect (i.e. follow-up VFs showing consistent improvement compared to baseline VFs) also were excluded until results were stable. Visual fields were further reviewed qualitatively for lid and rim artefacts, fatigue effects, inattention, and evidence that abnormal VF results attributable to a disease other than glaucoma (e.g. homonymous hemianopia).
Classifying Central Visual Fields Defect for 10-2 and 24-2C Visual Field Tests
A CVFD (i.e., a VF defect within the central 10 degrees) required a cluster of 3 contiguous abnormal points with p < 5%, 5% and 1% or < 5%, 2%, and 2% within a hemifield on either the TD or PD plot. The test points used to identify CVFDs overall and specific CVFD patterns from the Humphrey Visual Field Analyzer 10-2 and the central 10 degrees of the 24-2C testing grids are described below and shown in Figures 1 and 2. Two independent graders reviewed the 10-2 and 24-2C TD and PD plots from printouts using criteria adapted from Hood et al.1 and Traynis et al.11 A consensus grade was reached when there was disagreement between observers regarding the reported pattern of CVFD.
Figure 1.
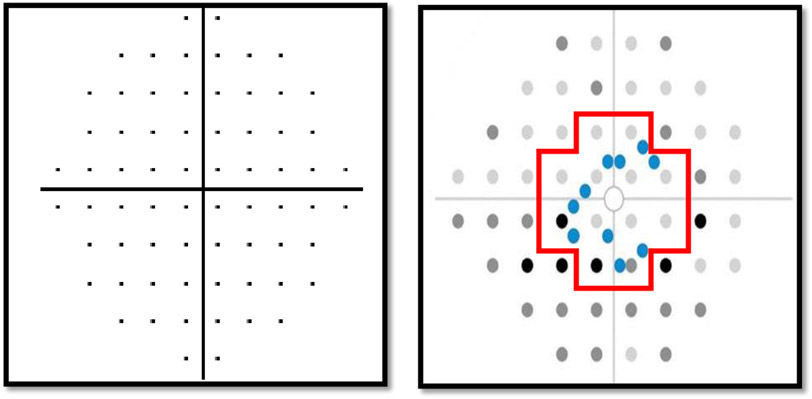
Central visual field in 10-2 and 24-2C protocol test grids. The 10-2 test grid includes 68 central test locations (Left). The 24-2C testing grid includes 62 test locations with 22 points within the central 10 degrees (Right). The 10 added central test locations are colored blue. All contributing 24-2C central test locations are outlined in red.
Figure 2.
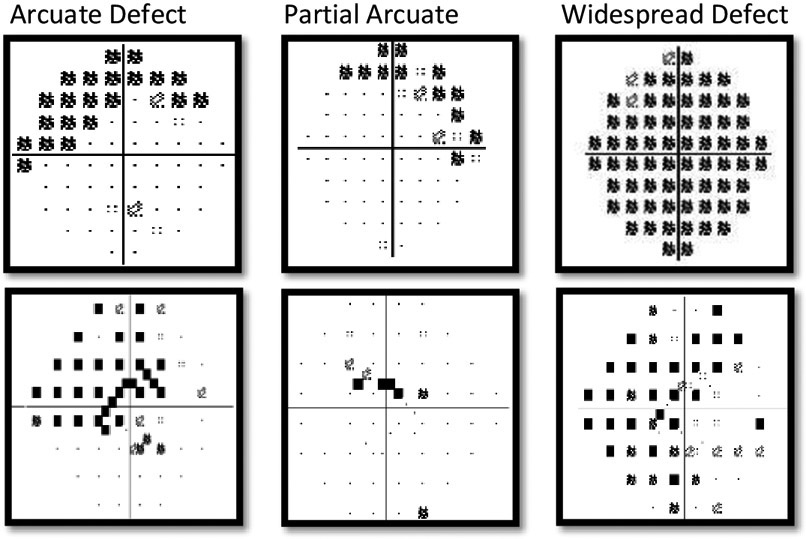
Examples of central visual field defect (CVFD) patterns on the 10-2 (top) and 24-2C (bottom) testing grids.
We did not consider CVFD agreement with the 24-2 testing grid because it is not possible to create an identical definition for 24-2 CVFDs and it is not possible to identify the selected defect patterns with only 12 test points in the central ten degrees. Moreover, we felt the comparison of interest was the agreement between the 24-2C and the 10-2 test grids which has not been investigated previously.
Patterns of Central Visual Field Defects in 10-2 and 24-2 C Tests
A CVFD was detected when any one of the following defect patterns were identified.
Arcuate defect:
A continuous, dense superior or inferior hemifield defect on the TD or PD plot (p≤1%) that includes both the nasal and temporal quadrants.
Partial arcuate defect:
A continuous superior or inferior hemifield defect on the TD or PD plot (p<1%) that includes both the nasal and temporal quadrants but is less dense (fewer abnormal points) than an arcuate defect.
Widespread defect:
VF sensitivity loss in all four quadrants on the TD or PD plot.
No central visual field defect:
A visual field that did not display any defect described above.
Statistical Analyses
Cohen’s Kappa (k) statistic was used to assess agreement among 24-2, 10-2 and 24-2C tests in identifying CVFDs, with bias-corrected confidence intervals determined by a clustered bootstrap procedure. Landis and Koch criteria2 were used to describe kappa agreement as no agreement (<0), slight agreement (0–0.20), fair agreement (0.21–0.40), moderate agreement (0.41–0.60), substantial agreement (0.61–0.80) and almost perfect agreement (0.81–1). Specificity of 10-2 and 24-2 tests was determined based on false positive rates observed in healthy eyes described above.
Results:
Measurements from 165 eyes of 92 study participants were included. Eighteen (19.6%) participants were healthy, 12 (13.0%) were glaucoma suspects and 62 (67.4%) were glaucoma patients as described above. Patient demographic and ophthalmic measurement by eye are shown in Table 1. Based on 24-2 VF MD, 54 (63.5%) glaucoma eyes had early disease (MD better than −6.0 dB), 21 (24.7%) eyes had moderate disease (MD between – 6.0 dB and −12.0 dB) and 10 (11.8%) had advanced disease (MD worse than −12.0 dB).
Table 1.
Patient demographic and clinical characteristics
| Patient characteristics | (n=92) |
|---|---|
| Age | 66.9 (63.9, 69.9) |
| Gender | |
| Female n (%) | 46 (50.0%) |
| Male | 46 (50.0%) |
| Race | |
| Asian | 16 (17.4%) |
| Black or African American | 22 (23.9%) |
| Native Hawaiian or Other Pacific Islander | 1 (1.1%) |
| White | 49 (53.3%) |
| Unknown or Not Reported | 4 (4.3%) |
| Diagnosis | |
| Healthy | 18 (19.6%) |
| Glaucoma Suspects | 12 (13.0%) |
| Glaucoma Patients | 62 (67.4%) |
| Hypertension | |
| No | 50 (54.3%) |
| Yes | 42 (45.7%) |
| Diabetes | |
| No | 78 (84.8%) |
| Yes | 14 (15.2%) |
| Eye Characteristics | (n=165) |
| VF 24-2 MD (dB) | −3.67 (−4.65, −2.69) |
| VF 10-2 MD (dB) | −2.89 (−3.86, −1.93) |
| Glaucoma Eyes (based on 24-2 MD) | |
| Early (better than −6 dB) | 54 (63.5%) |
| Moderate (−6 dB to −12 dB) | 21 (24.7%) |
| Advanced (worse than −12 dB) | 10 (11.8%) |
| Global MRW (n=148) | 231.2 (215.3, 247.2) |
| RNFL Thickness (μm) (n=127) | 79.2 (75.6, 82.9) |
| BMO Area (mm2) (n=148) | 2.18 (2.05, 2.30) |
| Axial length (mm) (n=162) | 25.1 (24.8, 25.5) |
| Spherical Equivalent (D) (n=162) | −2.62 (−3.33, −1.91) |
| IOP (mmHg) (n=146) | 14.6 (13.8, 15.5) |
| CCT (μm) (n=156) | 537.5 (527.8, 547.1) |
The distribution of CVFDs in glaucoma and glaucoma suspect eyes by hemifield based on TD and PD plots for all test protocols are presented in Table 2. The largest number of hemifield specific CVFDs was observed on the superior 10-2 TD plots (n=45) and the largest overall number of CVFDs was observed on the 10-2 TD plot (n=58).
Table 2.
Total number of Superior, Inferior and both superior and inferior central visual field defects in total deviation (TD) and pattern deviation (PD) plots in glaucoma suspects and patients (n=74 patients, 132 eyes)
| Test Pattern |
Superior Defect | Inferior defect | Both Superior and Inferior | Any Defect | ||||
|---|---|---|---|---|---|---|---|---|
| TD | PD | TD | PD | TD | PD | TD | PD | |
| 24-2C | 31 (23.5%) | 25 (18.9%) | 29 (22.0%) | 27 (20.5%) | 18 (13.6%) | 10 (7.6%) | 42 (31.8%) | 42 (31.8%) |
| 10-2 | 45 (34.1%) | 32 (24.2%) | 42 (31.8%) | 36 (27.3%) | 33 (25.0%) | 24 (18.2%) | 58 (44.0%) | 56 (42.4%) |
Specifically, the number of glaucoma and glaucoma suspect eyes with any CVFD from the 10-2 and 24-2C test protocols based on TD plots was 58 (43.9%) and 42 (31.8%) respectively. These values were 56 (42.4%) and 42 (31.8%), respectively, based on PD plots (Venn diagrams showing number of CVFDs based on TD and PD plots from each testing protocol are shown in Figure 3).
Figure 3.
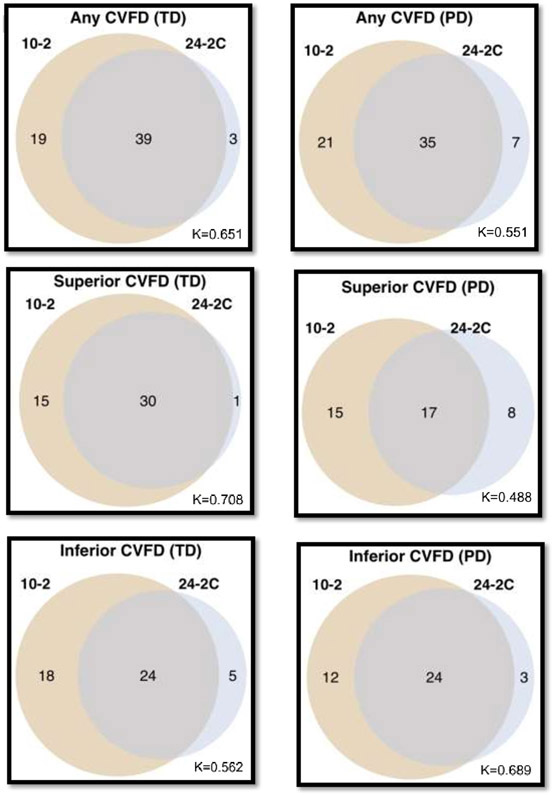
Venn Diagrams illustrating the moderate to substantial agreement for identifying the presence of any, any superior or any inferior central visual field defects in glaucoma and glaucoma suspect eyes between 10-2 and 24-2C testing protocols.
Table 3 and Figure 3 show moderate to substantial agreement for identifying superior, inferior or any CVFD between 10-2 and 24-2C VFs, with kappa values ranging between 0.488 and 0.708. Table 3 indicates that for TD plots, agreement between 24-2 and 10-2 VFs was best for detecting superior CVFDs (K=0.708) and worst for detecting inferior CVFDs (K=0.562) with both values indicating substantial agreement. For PD plots, agreement was best for detecting inferior CVFDs (K=0.689) and worst for detecting superior CVFDs (K=0.488) indicating substantial to moderate agreement, respectively. Figure 3 illustrates examples of agreement and disagreement among 10-2 and 24-2C test protocols for detecting CVFDs based on the TD and PD plots.
Table 3.
Agreement between central visual field defect (CVFD) patterns using 24-2C and 10-2 visual field tests in glaucoma suspects and glaucoma patients
| TD: 24-2C Value | PD: 24-2C Value | |||||
|---|---|---|---|---|---|---|
| No | Yes | Cohen’s κ* | No | Yes | Cohen’s κ* | |
| 10-2: Superior arcuate or partial arcuate | ||||||
| No | 95 (84.8%) | 5 (25.0%) | 0.480 (0.262,0.657) | 92 (85.2%) | 10 (41.7%) | 0.397 (0.164, 0.596) |
| Yes | 17 (15.2%) | 15 (75.0%) | 16 (14.8%) | 14 (58.3%) | ||
| 10-2: Any Superior CVFD | ||||||
| No | 86 (85.1%) | 1 (3.2%) | 0.708 (0.570, 0.828) | 92 (86.0%) | 8 (32.0%) | 0.488 (0.263, 0.664) |
| Yes | 15 (14.9%) | 30 (96.8%) | 15 (14.0%) | 17 (68.0%) | ||
| 10-2: Inferior arcuate or partial arcuate | ||||||
| No | 99 (87.6%) | 6 (31.6%) | 0.477 (0.280, 0.658) | 93 (86.9%) | 4 (16.0%) | 0.615 (0.445, 0.775) |
| Yes | 14 (12.4%) | 13 (68.4%) | 14 (13.1%) | 21 (84.0%) | ||
| 10-2: Any Inferior CVFD | ||||||
| No | 85 (82.5%) | 5 (17.2%) | 0.562 (0.412, 0.701) | 93 (88.6%) | 3 (11.1%) | 0.689 (0.550, 0.816) |
| Yes | 18 (17.5%) | 24 (82.8%) | 12 (11.4%) | 24 (88.9%) | ||
| 10-2: Any CVFD | ||||||
| No | 71 (78.9%) | 3 (7.1%) | 0.651 (0.524, 0.770) | 69 (76.7%) | 7 (16.7%) | 0.551 (0.422, 0.679) |
| Yes | 19 (21.1%) | 39 (92.9%) | 21 (23.3%) | 35 (83.3%) | ||
Agreement between CVFD patterns (any, arcuate, partial arcuate) detected in the 24-2C and 10-2 tests also is presented in Table 3. Based on the TD plots, agreement between 10-2 and 24-2C VFs was best for detecting any superior CVFDs (K=0.708) and worst for detecting inferior arcuate and partial arcuate CVFDs (K=0.477). For PD plots, agreement was best for detecting any inferior CVFDs (K=0.689) and worst for detecting superior arcuate and partial arcuate CVFDs (K=0.397) with agreement ranging from moderate to substantial.
Specificity (1 - false positive results) of each testing protocol for detecting CVFDs in 33 eyes of 18 healthy individuals was 1.0 for 10-2 and 0.94 for 24-2C based on the TD criterion. Similar specificities were observed for CVFDs defined using the PD criterion with specificity = 1.0 and 0.97 for 10-2 and 24-2C, respectively.
DISCUSSION
The current study showed that the overall agreement between 10-2 and 24-2C VFs for detecting central visual field defects in glaucoma and glaucoma suspect eyes was moderate to substantial by hemifield and by patterns of defect for both TD and PD criteria. These results suggest that adding 10 central visual field test points using the 24-2 algorithm can facilitate the detection of central visual field loss in glaucoma patients in a single, relatively fast 24-2C test. Specificity of all testing protocols was excellent in our relatively small sample of healthy eyes ranging from 0.94 for 24-2C TD criterion to 1.00 for 10-2 TD and PD criteria.
Several recent studies have suggested that 10–2 visual field tests may improve clinical detection of glaucoma because eyes with within normal limits 24-2 VF results often display abnormal 10–2 VF results. For instance, De Moraes and colleagues9, 10 reported that, using a cluster criteria to define 10-2 and 24-2 VF defects, 61.5% percent of glaucoma eyes (defined as GON in addition to repeatable abnormal VFs by global PSD or GHT) and 39.5% of GON eyes with 10-2 defects were classified as normal by 24-2 testing. In addition, Grillo et al12 reported that 52.5% of early glaucoma eyes with corresponding 10-2 and OCT-measured GC-IPL defects were classified as normal by one or more of several metrics used to define 24-2 defects. Comparing the novel 24-2C protocol that includes additional central test points to standard 24-2 testing, Phu and Kalloniatis13found a small but statistically significant difference in reported glaucoma severity (i.e. MD) of −0.73 dB using 24-2C testing compared to 24-2 testing in glaucoma and glaucoma suspect eyes although PSD and GHT indices were not significantly different. This result may suggest that 24-2C testing can improve sensitivity for detecting glaucomatous loss of central VF sensitivity although the authors acknowledge that this small difference likely is not clinically relevant.
Other studies did not find differences between 10-2 and 24-2 test protocols. For instance, Wu et al.14 observed that 10–2 and 24–2 tests identified a similar number of eyes with glaucoma as having central visual field defects using PSD values. Similarly, using a cluster criteria to define CVFDs on PD plots from glaucoma and glaucoma suspect eyes, Sullivan-Mee15 and colleagues observed defects in the central 10 degrees of 24-2 tests in 82% of eyes with 10-2 CVFDs. More recently Hood et al.16 reported a similar number of eyes with known macular structural defects defined by OCT imaging went undetected using both 24-2 and 10-2 testing, strongly suggesting that a combined analysis of central functional and structural integrity is important for detecting early glaucoma. In addition, West and colleagues17 reported little evidence to suggest that adding 10-2 testing to a 24-2 perimetry regimen revealed additional central visual field defects in eyes with early glaucoma.
In the current study more CVFDs were identified by the 10-2 test protocol in the superior and inferior hemifields than by the 24-2C test protocol. The larger number of CVFDs detected with 10-2 testing likely is attributable in part to the increased number of test points on the 10-2 test grid (n=64) compared to the central 10 degrees of the 24-2C test grid (n=22). Despite the larger number of CVFDs detected by the 10-2 protocol, agreement with the 24-2C protocol for detecting any CVFDs based on the TD and PD criteria was still moderate to substantial. Recently, Wu et al. reported a false positive rate of 31% in 24-2 VFs of healthy eyes using the cluster definition for 24-2C testing that we employed in the current study.18 We found specificities ≥0.94 (94%) for both 10-2 and 24-2C protocols for TD and PD plots resulting in a false positive rate of ≤6%. We do acknowledge however that out specificity test set was small.
The function of the PD plot is to identify localized defects that may be masked by either a generalised depression or an elevation of the hill of the vision. We observed that the prevalence of CVFDs was higher when defined using the TD plot criteria than the PD plot criteria for 10-2 and 24-2C testing particularly when defects were widespread (results not shown). In such cases, the PD plot often displayed mild defects or no defect at all in comparison to a widespread defect on TD plot. It is possible that this effect was related to the presence of early cataract in some eyes. Given that most clinicians depend primarily on the PD plot for identifying glaucomatous damage, further studies are needed to investigate the sensitivity of the TD plot compared to the PD plot for detecting CVFDs in 10-2 and 24-2C test protocols.
Possible limitations of the current study are that different thresholding algorithms are used for the 10-2 protocol and the newer 24-2C protocol (SITA Standard and SITA Faster, respectively) and this might result in different measurements of VF sensitivity. For instance, although 24-2C testing with SITA Faster reduces test time compared to 24-2 testing with SITA Standard (reduction in test time of 49% in glaucoma eyes and 53% in healthy eyes according to one study),19, 20 mean deviation has been shown to be slightly higher (less severe disease) using 24-2C with SITA Faster compared to 24-2 with SITA Standard.19-21 Although not directly applicable to the current study (because we did not include 24-2 results), this difference theoretically could decrease the agreement among test protocols when considering severity of individual test points contributing to a CVFD cluster. In addition, different normative databases used to define probability cut-offs for TD and MD test points also could decrease agreement among test protocols. Moreover, reduced agreement between test results could be caused by individual contiguous points composing a CVFD cluster not quite meeting the 3 test point criterion for abnormality thereby disqualifying a potential defect being classified as CVFD (e.g. Figures 4D and 4E). Finally, we did not provides estimates of the sensitivity of detecting CVFD using the 2 testing protocols as there is no independent gold standard definition of CVFD available. Studies comparing the sensitivity and specificity of 24-2C and 10-2 testing protocols for detecting central glaucomatous damage based on macula OCT scans are needed to address this issue.
Figure 4.
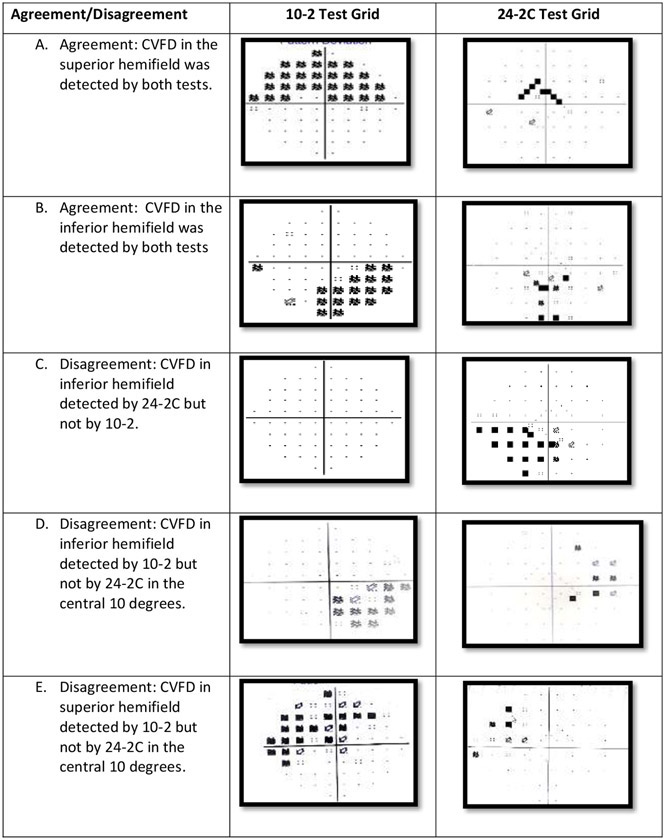
Case examples of agreement and disagreement between 10-2 and 24-2C tests for detecting CVFD using pattern deviation criterion. Rows A and B show examples of agreement between 10-2 and 24-2C tests for the detection of a CVFD in the superior and inferior hemifield, respectively. Rows C and D show examples of disagreement between 10-2 and 24-2C tests for the detection of a CVFD in the inferior hemifields. Note that Rows D and E show disagreement between 10-2 and 24-2C tests for detecting inferior and superior CVFD, where no CVFD is detected by the 24-2C test because only a single point is outside of normal limits.
In summary, the 24-2C and 10-2 testing protocols had moderate to substantial agreement for the detection of visual defects in the central 10 degrees of the investigated VFs. These results suggest that the 24-2C, with its SITA Faster thresholding algorithm and shorter test time, shows promise for documenting central visual field defects in glaucoma patients and may reduce the need to complete 10-2 testing. Longitudinal studies are needed to determine how well the 24-2C identifies central visual field defects over time.
Acknowledgments
Funding support:
National Institutes of Health/National Eye Institute, Bethesda MA: R21 EY027945, R01 EY026574, R01 EY027510, P30 EY022589, R01 EY029058.
An unrestricted grant from Research to Prevent Blindness (New York, NY).
Footnotes
Financial disclosures:
Tutul Chakravarti: None; Mohamad Moghadam: None; James A. Proudfoot: None; Robert N. Weinreb: Consultant: Aerie Pharmaceuticals, Allergan, Bausch & Lomb, Eyenovia, Implantdata, Novartis; Financial support in the form of research materials: Bausch & Lomb, Carl Zeiss Meditec, Centervue, Heidelberg Engineering, Konan Medical, Optovue; Christopher Bowd: None; Linda M. Zangwill: Financial support and/or research equipment: Carl Zeiss Meditec, Heidelberg Engineering, Optovue, Topcon Medical Systems.
REFERENCES
- 1.Coughlan M, Friedmnan AL. The Frequency Distribution of Early Visual Field Defects in Glaucoma. In: G EL, V G, editors. Fourth International Visual Field Symposium Bristol, April 13–16,1980. Dordrecht: Springer, 1981. [Google Scholar]
- 2.Drance SM. The early field defects in glaucoma. Invest Ophthalmol 1969;8:84–91. [PubMed] [Google Scholar]
- 3.De Moraes CG, Hood DC, Thenappan A, et al. 24-2 Visual Fields Miss Central Defects Shown on 10-2 Tests in Glaucoma Suspects, Ocular Hypertensives, and Early Glaucoma. Ophthalmology 2017;124:1449–1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hood DC, Nguyen M, Ehrlich AC, et al. A Test of a Model of Glaucomatous Damage of the Macula With High-Density Perimetry: Implications for the Locations of Visual Field Test Points. Transl Vis Sci Technol 2014;3:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hood DC, Raza AS, de Moraes CG, et al. Initial arcuate defects within the central 10 degrees in glaucoma. Invest Ophthalmol Vis Sci 2011;52:940–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garg A, Hood DC, Pensec N, Liebmann JM, Blumberg DM. Macular Damage, as Determined by Structure-Function Staging, Is Associated With Worse Vision-related Quality of Life in Early Glaucoma. American journal of ophthalmology 2018;194:88–94. [DOI] [PubMed] [Google Scholar]
- 7.Yanagisawa M, Kato S, Kunimatsu S, Tamura M, Ochiai M. Relationship Between Vision-Related Quality of Life in Japanese Patients and Methods for Evaluating Visual Field. Jpn J Ophthalmol 2011;55:132–137. [DOI] [PubMed] [Google Scholar]
- 8.Murata H, Hirasawa H, Aoyama Y, et al. Identifying Areas of the Visual Field Important for Quality of Life in Patients with Glaucoma. Plos One 2013;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen S, McKendrick AM, Turpin A. Choosing two points to add to the 24-2 pattern to better describe macular visual field damage due to glaucoma. Br J Ophthalmol 2015;99:1236–9. [DOI] [PubMed] [Google Scholar]
- 10.Ehrlich AC, Raza AS, Ritch R, Hood DC. Modifying the Conventional Visual Field Test Pattern to Improve the Detection of Early Glaucomatous Defects in the Central 10 degrees. Transl Vis Sci Technol 2014;3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Traynis I, De Moraes CG, Raza AS, Liebmann JM, Ritch R, Hood DC. Prevalence and nature of early glaucomatous defects in the central 10 degrees of the visual field. JAMA ophthalmology 2014;132:291–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grillo LM, Wang DL, Ramachandran R, et al. The 24-2 Visual Field Test Misses Central Macular Damage Confirmed by the 10-2 Visual Field Test and Optical Coherence Tomography. Translational Vision Science & Technology 2016;5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phu J, Kalloniatis M. Ability of 24-2C and 24-2 Grids to Identify Central Visual Field Defects and Structure-Function Concordance in Glaucoma and Suspects. Am J Ophthalmol 2020;219:317–331. [DOI] [PubMed] [Google Scholar]
- 14.Wu Z, Medeiros FA, Weinreb RN, Zangwill LM. Performance of the 10-2 and 24-2 Visual Field Tests for Detecting Central Visual Field Abnormalities in Glaucoma. Am J Ophthalmol 2018;196:10–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sullivan-Mee M, Tran MTK, Pensyl D, Tsan G, Katiyar S. Prevalence, Features, and Severity of Glaucomatous Visual Field Loss Measured With the 10-2. Achromatic Threshold Visual Field Test. American journal of ophthalmology 2016;168:40–51. [DOI] [PubMed] [Google Scholar]
- 16.Hood DC, Thenappan AA, Tsamis E, Liebmann JM, De Moraes CG. An Evaluation of a New 24-2 Metric for Detecting Early Central Glaucomatous Damage. Am J Ophthalmol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.West ME, Sharpe GP, Hutchison DM, et al. Utility of 10-2 Visual Field Testing in Glaucoma Patients with Early 24-2 Visual Field Loss. Ophthalmology 2020. [DOI] [PubMed] [Google Scholar]
- 18.Wu ZC, Medeiros FA, Weinreb RN, Girkin CA, Zangwill LM. Specificity of various cluster criteria used for the detection of glaucomatous visual field abnormalities. Brit J Ophthalmol 2020;104:822–826. [DOI] [PubMed] [Google Scholar]
- 19.Yu S, lee GC, Callan T, Covita A, Severin T. Comparison of SITA Faster 24-2C test times to legacy SITA tests. Invest Ophth Vis Sci 2019;60:2454. [Google Scholar]
- 20.Phu J, Khuu SK, Agar A, Kalloniatis M. Clinical Evaluation of Swedish Interactive Thresholding Algorithm-Faster Compared With Swedish Interactive Thresholding Algorithm-Standard in Normal Subjects, Glaucoma Suspects, and Patients With Glaucoma. Am J Ophthalmol 2019;208:251–264. [DOI] [PubMed] [Google Scholar]
- 21.Lee GC, Callan T, Yu S, et al. Comparison of 24-2C SITA Standard test times to legacy SITA tests. Invest Ophth Vis Sci 2019;61:3879. [Google Scholar]


