Abstract
Elder abuse is prevalent, and victims have high rates of depression and low quality of life. We established an academic-community partnership to test the feasibility, acceptability, and impact of a brief psychotherapy for depression (PROTECT) among elder abuse victims with capacity to make decisions.
Elder abuse service providers referred depressed (PHQ-9≥10) older victims (age ≥ 55) for potential pilot study participation. Forty eligible victims who consented were randomized to PROTECT psychotherapy (N=25) or a Usual Care (N=15) condition involving a community psychotherapy referral. Follow-up research assessments were conducted at 6 weeks (mid-treatment) and 9 weeks (end of treatment) after study initial assessment. We used mixed-effects regression models to examine treatment effects on depression severity and quality of life over time.
Most victims (75%) reported two or more types of abuse. The a-priori acceptability benchmark was met at the end of PROTECT therapy. All PROTECT participants initiated therapy; this engagement rate is greater than the a-priori 75% standard set for feasibility. We found a significant reduction in depression severity (MADRS), with PROTECT leading to greater benefits compared to Usual Care. Both study groups had a similar improvement in quality of life.
The pilot project results found that PROTECT psychotherapy is feasible, acceptable, and effective in reducing depression. With the support of our partnership, we found that PROTECT could be delivered along side elder abuse services with victims willing to initiate therapy that leads to meaningful treatment effects.
Keywords: Late-life Depression, Psychotherapy Outcome, Elder Abuse, Community Intervention, Aging, Behavioral Therapy
Introduction
Elder abuse affects an estimated one in ten older adults in the United States. Elder abuse agencies work with victims to reduce the risk of revictimization by providing legal and support services, and referrals to community-based services. In collaboration with the New York City Department for the Aging (DFTA) Elder Justice Service, we implemented routine mental health screenings finding that one-third of victims reported significant depressive symptoms.1 Depressed victims have higher mortality rates.2 When offered abuse resolution services, victims underutilize them, sometimes believing that they have no options for change. Depressive symptoms, including depressed mood, a sense of hopelessness, and helplessness further reduce the use of services.
We have developed PROTECT, Providing Options to Elderly Clients Together, with our community partners to address depression among victims seeking elder abuse services. PROTECT is a 9-week behavioral psychotherapy tailored to the needs of elder abuse victims. It is simple, easy to learn, and can be delivered by community clinicians with high adherence.3 Using our model of late-life depression4, PROTECT is designed to address the impact of chronic stress by activating the reward system through the increase of pleasurable activities and taking actions towards personalized goals. PROTECT therapists work with victims to increase self-protective behaviors, to reduce stress, and to engage in activities with non-abusive others.5 PROTECT includes ongoing communication with agency staff to maintain a cohesive treatment approach aimed to reduce risk of re-victimization among patients.
This study was designed to test the feasibility, acceptability, and preliminary efficacy of PROTECT on depression severity and quality of life among elder abuse victims with capacity. We hypothesized that victims receiving PROTECT would be more likely to initiate therapy, report higher satisfaction, have greater reductions in depression, and have greater improvement in quality of life as compared to victims who are referred to community therapists.
METHODS
Subjects
Eligible victims of abuse were screened using the Patient Health Questionnaire-9 (PHQ-9) by their elder abuse resolution case workers. Case workers obtained verbal permission from eligible clients (PHQ-9≥10) to allow Cornell research staff to contact the client directly. Clients who agreed to be contacted met with a research assistant to review the study and obtain written informed consent.
Eligible participants: 1) were ≥ 55 years of age; 2) had capacity to consent (per abuse agency staff); 3) reported significant depression (PHQ-9 ≥10); and 4) received abuse resolution services from a community based agency. Exclusion criteria included: 1) active suicidal ideation (Montgomery-Åsberg Depression Rating Scale (MADRS) item 10 ≥ 4); 2) lack of basic proficiency in English; 3) an Axis 1 DSM-5 diagnoses other than unipolar depression or generalized anxiety disorder; 4) a Montreal Cognitive Assessment (MoCA) score < 24; or 5) a severe or life-threatening medical illness.
Treatments
Subjects were randomized to either “PROTECT” or the Usual Care condition (community referral). The randomization schedule was 2:1 in favor of PROTECT to provide an adequate sample for testing of feasibility and acceptability. PROTECT was provided by two licensed social workers who completed training with the Principal Investigator and demonstrated competence.
Prior to initiating therapy, PROTECT therapists contacted the elder abuse case workers to review the safety of the home, status of the alleged abuser and elder abuse prevention goals. PROTECT sessions were delivered in the home, or at a safe public location that was easily accessible and convenient to the participant.
PROTECT therapy consists of an evaluation session and eight subsequent clinical sessions. The initial phase of treatment includes discussion and psychoeducation about stress and depression, and identification of client treatment goals related to the abuse. Goals included steps to promote safety, self-care to increase self-efficacy, or steps to manage interactions with the alleged abuser. In follow up sessions, participants identify and increase pleasurable activities as they review action plans and steps to achieve prior goals. Following a planning worksheet together, the therapist and client develop new plans and rewarding activities. In final sessions, the therapist reviews the patient’s successfully used strategies and facilitates independence in selecting goals and developing action plans post-treatment.
The Usual care condition was a referral to a mental health provider who accepted the client’s insurance or a mental health clinic. A referral is the usual strategy used in elder abuse agencies without on-staff mental health services. Participants were given the referral by research staff upon randomization.
Measures
Trained research assistants, blinded to treatment assignment, conducted study assessments in the participant’s home or a safe public location at baseline, mid-treatment (Week 6), and at treatment end (Week 9).
Elder abuses were reported by victims at the beginning and end of the intervention using a modified versions of the measure used in Under the Radar: New York State Elder Abuse Prevalence Study. Feasibility was defined as a high rate of therapy initiation (≥75% began therapy). Acceptability was defined using the Client Satisfaction Questions (CSQ) and defined as a score of ≥ 3 on a 4-point scale. Depression diagnosis was determined using the SCID V and depression severity outcome was assessed using the Montgomery Åsberg Depression Rating Scale (MADRS). Quality of life was assessed using the World Health Organization Quality of Life-BREF (WHOQOL-BREF). The Cornell Services Index (CSI)6 was used to record therapy visits and treatment initiation.
Statistical Analyses
Descriptive statistics for continuous (median and interquartile range; IQR) and categorical (frequency and percentage) were reported on demographics and clinical characteristics of two treatment groups at baseline. A Mann-Whitney test and Fisher’s exact test were conducted to test the difference between PROTECT and Usual care for continuous and categorical variables, respectively.
Remission rate was defined as the percentage of participants with MADRS scores ≤ 10 at Week 9. Response was defined as a reduction of ≥ 50% in MADRS scores from baseline to Week 9. We conducted two mixed-effects linear regression models to compare the trajectories of change in MADRS scores and WHOQOL scores between PROTECT and Usual care, respectively. Each model included fixed effects of treatment (PROTECT vs. Usual care), time, and their interaction, as well as a participant-specific random intercept. Both models were adjusted for age and gender. Site and its interaction with treatment were initially included in the model but were dropped as their effects were statistically non-significant. A two-sided p-value less than 0.05 was considered statistically significant. Intent-to-treat analyses are presented with all available data in the mixed-effects models. Remission and response rates were calculated based on 30 patients with complete data. All analyses were conducted in R 3.6.1 (R Foundation for Statistical Computing; http://www.r-project.org/).
Results.
Among the 40 clients who were eligible and consented to the study, there were no significant demographic or clinical differences between the two treatment groups (PROTECT therapy N=25 and Referral group N=15) at baseline (Table 1). At the beginning of the study, 75% of clients reported being subjected to two or more types of abuse. More than three quarters (77.5%) reported verbal/emotional abuse; 57.5% reported physical abuse; 65% reported financial abuse and 12.5% reported neglect as part of the abuse pattern.
Table 1.
Demographic characteristics for the sample at baseline
| PROTECT | Referral | p value | |
|---|---|---|---|
| Variable | N=25 | N=15 | |
| Age | 70.0 [67.0;80.0] | 72.0 [67.5;78.5] | 0.89 |
| Education | 14.0 [12.0;16.0] | 12.0 [8.50;14.0] | 0.16 |
| Gender | 0.69 | ||
| Female | 19 (76.0%) | 13 (86.7%) | |
| Male | 6 (24.0%) | 2 (13.3%) | |
| Marital Status | 0.355 | ||
| Divorced | 4 (16.0%) | 2 (13.3%) | |
| Married | 3 (12.0%) | 5 (33.3%) | |
| Separated | 4 (16.0%) | 0 (0.00%) | |
| Single | 5 (20.0%) | 2 (13.3%) | |
| Widowed | 9 (36.0%) | 6 (40.0%) | |
| MADRS Total Score | 24.0 [20.0;27.0] | 23.0 [21.0;25.0] | 0.66 |
| WHOQOL Total Score | 46.0 [38.8;55.0] | 48.0 [43.5;50.5] | 0.78 |
| Endorsed suicidal ideation | 4 (16.0%) | 2 (13.3%) | 1 |
Note. Median and 1st and 3rd Quartiles in parentheses are presented for numeric variables. Frequencies (n; %) are presented for categorical variables. The significance of differences between treatment conditions was calculated with Mann-Whitney test for categorical variables and Fisher’s exact test for continuous variables. MADRS = Montgomery-Asberg Depression Rating Scale; WHOQOL = The World Health Organization Quality of Life
The a-priori acceptability benchmark (≥ 3 out of 4) was met, as we found a mean of 3.14 (SD = 1.20) on the CSQ at the end of PROTECT. We were able to demonstrate feasibility as 100% of PROTECT participants initiated therapy and met with a PROTECT therapist. This engagement rate is greater than the a-priori 75% standard set for feasibility. This rate higher than the 20% (3/15) of those participants in the Referral control group who connected with a mental health provider.
Among 40 patients with available post-treatment data, mixed-effects models showed a significant reduction in depression severity (MADRS scores) over time (F[2,62] = 34.36, p<.001; Figure 1). Interaction between treatment and time was significant (F[2,61] = 8.02; p<.001). Post-hoc comparisons showed that, compared to those receiving Usual Care, participants who received PROTECT had an average reduction of 6.53 more points on the MADRS at Week 6 (t(71) = −3.02, p=.003) and 5.29 points at Week 9 (t(70) = −2.46, p=.02). Approximately 55% (10/18) of PROTECT participants met the criterion for response of depression (i.e. reduction of ≥%50 in MADRS score), compared to only 17% (2/12) of participants in the Usual Care condition. Further, 33% (6/18) of PROTECT participants achieved remission (MADRS ≤ 10), compared to 17% (2/12) of Usual Care participants.
Figure 1.
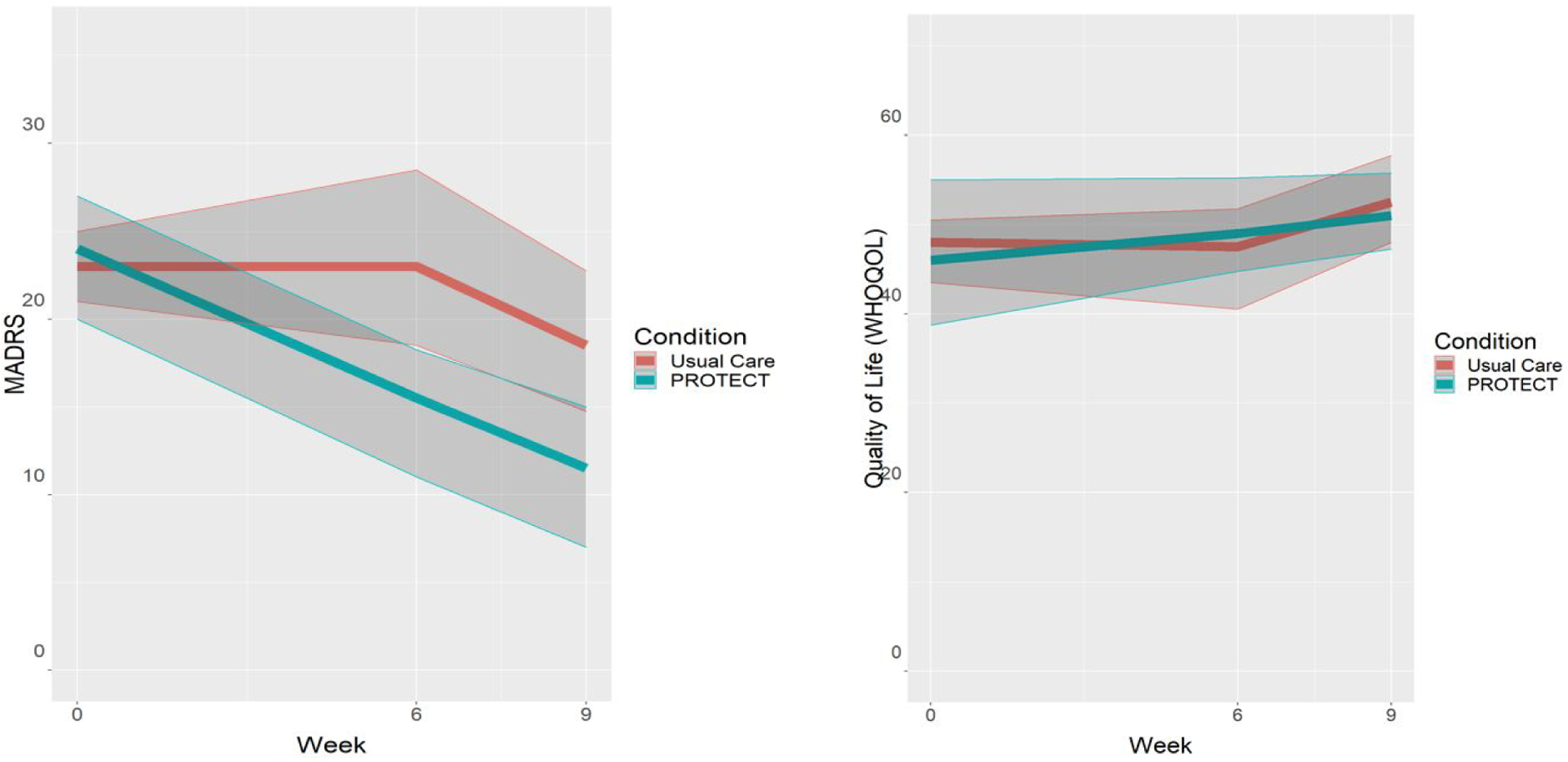
Reduction in Depression Severity and Improvement in Quality of Life (WHOQOL) over the course of 9 weeks
Note. Lines represent median reduction in depression, with Interquartile Range (IQR) band. MADRS = Montgomery-Asberg Depression Rating Scale. WHOQOL = The World Health Organization Quality of Life
We found significant improvement in quality of life (WHOQOL) over the course of treatment (F(2,57) = 5.00; p = .01). However, we observed no treatment difference at baseline or in the slopes of change (Figure 1).
Discussion
Our pilot study data demonstrated that PROTECT therapy was feasible, acceptable, and led to a high rate of treatment initiation among this vulnerable and underserved older adult population with high rates of depression. Elder abuse victims who received PROTECT had a greater decrease in depression compared to those who received a referral to a community provider. Both interventions led to a similar improvement in quality of life.
Our results show clinically meaningful improvements in depression severity over the course of PROTECT. The results are consistent with previous reports of similar psychotherapy interventions, such as Engage, developed by our group and used with other populations,7 and showed clinically significant reductions when extended to community settings.8 Developing interventions and planning implementation in partnership increased the likelihood for PROTECT to be tailored to clients’ needs and to be successfully implemented within non-mental health systems.
PROTECT was designed as an intervention to be offered in conjunction with abuse resolution services. The similar improvement in quality of life in both conditions could be a consequence of the support and guidance elder abuse case managers provided to victims in both PROTECT and the Usual Care condition. It is also possible that the small sample limited our statistical power to capture differences in quality of life outcomes. In addition, we cannot evaluate the longer term outcomes of this intervention. While replication in a larger study is needed to confirm the benefits of PROTECT, to our knowledge ours is the first study to develop a mental health intervention designed specifically for elder abuse victims. Future studies could expand services by delivering PROTECT to a larger sample of elder abuse victims and to victims who speak a language other than English.
Acknowledgements:
We wish to thank our collaborators at the New York City Elder Justice Service and the abuse service case workers who support the research and make referrals. We are grateful to the study participants for their time and their trust in us. And our colleagues and staff who contribute to making it possible both at the Institute and beyond.
Footnotes
Conflict of interests:
Dr. Alexopoulos served on Advisory Board of Eisai and of Janssen Pharmaceuticals. He also served on the Speakers Bureaus of Allergan, Otsuka, and Takeda-Lundbeck. The other authors have no conflicts of interest.
References
- 1.Sirey JA, Berman J, Salamone A, et al. Feasibility of Integrating Mental Health Screening and Services Into Routine Elder Abuse Practice to Improve Client Outcomes. J Elder Abuse Negl. 2015(just-accepted). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong X, Simon M, Mendes de Leon C, et al. Elder self-neglect and abuse and mortality risk in a community-dwelling population. JAMA. 2009;302(5):517–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sirey JA, Halkett A, Chambers S, et al. PROTECT: A Pilot Program to Integrate Mental Health Treatment Into Elder Abuse Services for Older Women. J Elder Abuse Negl. 2015:null–null. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexopoulos GS. Mechanisms and treatment of late-life depression. Transl Psychiatry. 2019;9(1):188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solomonov N, Bress JN, Sirey JA, et al. Engagement in Socially and Interpersonally Rewarding Activities as a Predictor of Outcome in “Engage” Behavioral Activation Therapy for Late-Life Depression. Am J Geriatr Psychiatry. 2019;27(6):571–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sirey JA, Meyers BS, Teresi JA, et al. The Cornell Service Index as a measure of health service use. Psychiatr Serv. 2005;56(12):1564–1569. [DOI] [PubMed] [Google Scholar]
- 7.Alexopoulos GS, Raue PJ, Banerjee S, et al. Comparing the streamlined psychotherapy “Engage” with problem-solving therapy in late-life major depression. A randomized clinical trial. Molecular psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sirey JA, Raue PJ, Solomonov N, et al. Community delivery of brief therapy for depressed older adults impacted by Hurricane Sandy. Transl Behav Med. 2020;10(3):539–545. [DOI] [PMC free article] [PubMed] [Google Scholar]


