Abstract
The authors report a case of a 75-year-old male with pulmonary embolism (PE) successfully treated using the INARI FlowTriever System, a mechanical thrombectomy device. Imaging confirmed deep vein thrombosis and PE presented after two days of left lower extremity (LLE) pain and dyspnea on exertion with history of peripheral vascular disease, coronary artery disease, insulin dependent diabetes mellitus, hyperlipidemia and LLE percutaneous coronary intervention with coronary stent placement. PE treatment with single session clot burden reduction resulted in immediate improvement in oxygenation and echocardiogram confirmed relief of right heart strain. The patient's immediate hemodynamic improvement without thrombolytic therapy, which can take hours for morbidity reduction, supports the expansion of the use of thrombectomy devices for the treatment of submassive symptomatic PE in clinical practice, with further research indicated.
Keywords: Flowtriever, INARI, Pulmonary embolism, Thrombectomy, Interventional radiology, Embolectomy
Introduction
Pulmonary Embolism (PE) carries a significant burden on the American population. It is estimated that for every 100,000 Americans, 60-70 individuals will develop a PE within that calendar year [1]. PE accounts for 100,000 deaths per year in the United States alone [2]. PE’s are classified into 3 classes as massive, submassive, and low risk; with massive having the most hemodynamic instability and low risk having no hemodynamic instability.
Thrombolytics have been the novel method for removal and prevention of blood clots via enhanced native lysis reducing clot burden. Although the first line for acute massive PE, thrombolytics come with a feared compilation of life-threatening bleeding [3]. This risk necessitates a careful risk-benefit assessment prior to the use of these agents. Inari has developed the FlowTriever System to treat pulmonary embolism through the peripheral vasculature without the use of thrombolytics. The Triever aspiration catheter features a large lumen catheter and large-bore syringe to quickly remove large volumes of clots while mitigating blood loss. The catheter has three self-expanding nitinol mesh disks that remove and deliver the clot to the device. Our case demonstrates a successful removal of a PE with the FlowTriever system.
Case description
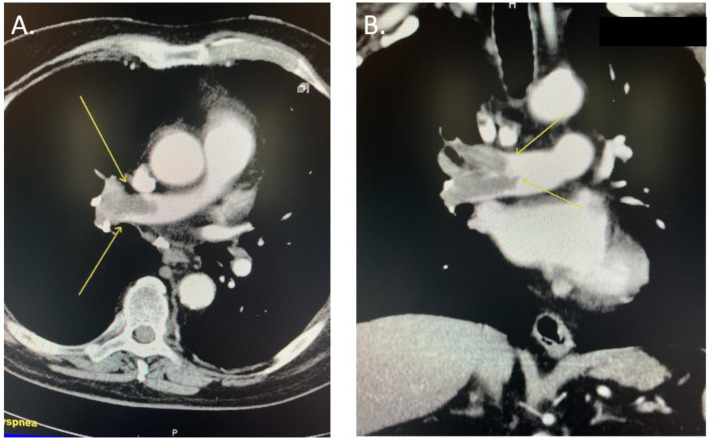
A 75-year-old male presented to the emergency department complaining of dyspnea and left lower extremity pain without chest pain. He noted his left leg was swollen and the pain began two days prior which worsened with ambulation. His dyspnea with exertion also began two days ago. He has a past medical history of peripheral vascular disease, coronary artery disease, insulin dependent diabetes mellitus, and hyperlipidemia. He had previous left lower extremity percutaneous coronary intervention with coronary artery stent placement. His vitals were stable at a blood pressure of 145/71 mmHg, heart rate of 84 bpm, respiratory rate of 20 br/min, and an O2 saturation of 93%. Initial labs showed low platelets of 133 k/mcL, low CO2 of 21 mmol/L, low calcium of 8.4 mg/dL, and normal coagulation study Partial thromboplastin time of 27.2 seconds, Prothrombin time of 12.5 seconds, and international normalized ratio of 1.1. Troponin was normal at 0.03 ng/mL and brain natriuretic peptide was elevated at 327 pg/mL. Intravenous heparin was started. Computed tomography angiogram of the chest was ordered and showed a right main pulmonary artery embolism with evidence of right heart strain that was confirmed on echocardiogram (Fig. 1). Lower extremity venous doppler confirmed the presence of deep venous thrombosis (DVT) involving the common femoral, popliteal, and trifurcation veins.
Fig. 1.
Spiral CT image of chest without contrast showing suspected pulmonary embolism (PE). A. Transverse section view of the PE highlighted by the yellow arrows. B. Coronal section of the PE highlighted by the yellow arrows.
Interventional radiology was consulted for further management of the patients DVT and PE. The patients DVT was removed using the ClotTriever device by Inari however, this paper will focus on the PE removal using the FlowTriever device by Inari. The FlowTriever system was used over other therapies because of previous success of the therapy in similar cases. Right common femoral vein access was performed under ultrasound guidance using a 0.035 guidewire. An 8 French introducer sheath was advanced into the common femoral vein. Fluoroscopic guided access into the main and right pulmonary artery was achieved using a curved pigtail catheter. Right pulmonary angiogram illustrated significant blockage within the right main pulmonary artery. Hemodynamic pressures of the right pulmonary artery were obtained, showing a pre-systolic pressure of 38mmHg and a mean pressure of 18mmHg. Wire access was obtained using a super stiff Amplatz wire, and the curved pigtail catheter was removed. The 8 French inducer sheath was removed, and serial dilatations were performed, and a 20 French dry sheath was successfully advanced into the iliac vein.
The FlowTriever device was advanced into the right main pulmonary artery. Mechanical thrombectomy was performed. Four aspirations yielded a significant amount of clot return. After the clot was removed, the patient reported immediate benefits and stated, “it feels like an elephant was lifted off my chest.” After the clot was retrieved, right pulmonary arterial pressure was reassessed and showed a mean pressure of 12 mmHg. A repeat of the right pulmonary artery angiogram showed a significant reduction in clot burden (Fig. 2). Total blood loss from the procedure was 250 cc, total fluorescent time was 17.3 minutes, and 18 fluorographic images were obtained. The patient had no significant post-procedural complication. Pre-procedure vitals showed a blood pressure 141/89 mmHg, heart rate 68 bpm, respiratory rate18 respirations per min, and an O2 saturation of 91-97% on 4L nasal cannula. Post procedure vitals showed BP 135/80 mmHg, heart rate of 67 bpm, and respiratory rate of 15 br/min, and an O2 saturation of 96-99% on 2L nasal cannula. The patient stayed at the hospital for three days and experienced no complications.
Fig. 2.
An angiographic CT image of the chest. A. Shows the main pulmonary filling defect signaled by the white arrows. B Shows subsequent restoration of blood flow demonstrated by increased lung field lucency post relief of clot burden.
Discussion
The FlowTriever device is an effective alternative treatment modality for Pulmonary Embolism. The patient noted immediate improvement of their shortness of breath and marked improvement of his oxygenation. While traditional treatment with thrombolytics can take hours for morbidity reduction, the FlowTriever allowed for immediate improvement. Other treatments for PE include catheter-assisted thrombus removal with or without thrombolytics and surgical embolectomy. Deciding on these different treatment options is case specific and depends mostly on the severity and stability of the patient. The FlowTriever may be able to fill a niche in the treatment of PE, which traditional thrombolytic therapy would be contraindicated, such as newly diagnosed brain neoplasms, recent head trauma, recent stroke, or pregnancy [4].
Although the FlowTriever has many advantages, it is important for physicians to consider the risk of embolism to the benefits of thrombectomy. Depending on the location of the embolism, there is a risk of further movement of the embolism to the renal or pulmonary veins during aspiration. As suggested by a previous study, a solution would be to deploy a temporary embolic protection device upstream of the occlusion to protect the lungs [5]. There are many risks for damage to the delicate heart, respiratory and circulatory structures with the FlowTriever device. Pulmonary artery dissection is a risk from the catheter causing direct damage or extra negative pressure disrupting the vessel [6]. Excessive blood loss is another risk factor with previous cases losing up to 520 mL of blood [7].
This case complements a previous study known as the FLARE study, which showed the safety and effectiveness of the FlowTriever system with acute intermediate-risk PE. In this study, there was acute improved RV function and low bleeding complications after the procedure [8]. It will be helpful to have more studies demonstrating the effectiveness of the device in the future.
Conclusion
The FlowTriever device for PE removal has been shown to improve patient care and health outcomes, as documented in this case. It is important to share the potential benefits of the FlowTriever system within the medical field due to its benefits over traditional therapies. It is however important for further research into various mechanical thrombectomy devices to determine their efficacies in the treatment of acute pulmonary embolism.
Patient consent
Written informed consent was not obtained from the patient for publication of this case report and accompanying images since there are no patient identifying characteristics.
Footnotes
Competing Interests: None
References
- 1.Thompson T, Kabrhel C. Overview of acute pulmonary embolism in adults. In: Post TW, editor. UpToDate. UpToDate, Inc; Waltham, MA: 2020. https://www-uptodate-com./contents/overview-of-acute-pulmonary-embolism-in-adults Available at. Accessed January 9, 2021. [Google Scholar]
- 2.Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism. Exp Clin Cardiol. 2013;18(2):129–138. [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart LK, Kline JA. Fibrinolytics for the treatment of pulmonary embolism. Transl Res. 2020;225:82–94. doi: 10.1016/j.trsl.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tapson VF, Weinberg AS. Approach to thrombolytic (fibrinolytic) therapy in acute pulmonary embolism: Patient selection and administration. In: Post TW, editor. UpToDate. UpToDate, Inc; Waltham, MA: 2020. https://www-uptodate-com./contents/approach-to-thrombolytic-fibrinolytic-therapy-in-acute-pulmonary-embolism-patient-selection-and-administration Available at. Accessed January 9, 2021. [Google Scholar]
- 5.Murali N., Nezami N., Latich I., Brown J., Mojibian H. Simultaneous proximal embolic protection and inferior vena cava mechanical thrombectomy using the FlowTriever system. Diagn Interv Radiol. 2020;26(4):345. doi: 10.5152/dir.2019.19458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sista Akhilesh K. Aspiration thrombectomy for severe pulmonary embolism using the flow triever device: the good, the bad, and the unknown. J Vasc Interv Radiol. 2019;30(9):1376–1377. doi: 10.1016/j.jvir.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Wible BC, Buckley JR, Cho KH. Safety and efficacy of acute pulmonary embolism large-bore aspiration mechanical thrombectomy using the Inari FlowTriever device. J Vasc Interv Radiol. 2019;30:1370–1375. doi: 10.1016/j.jvir.2019.05.024. [DOI] [PubMed] [Google Scholar]
- 8.Tu T, Toma C, Tapson VF. A prospective, single-arm, multicenter trial of Catheter-directed mechanical thrombectomy for Intermediate-risk acute pulmonary embolism: the FLARE study. JACC Cardiovasc Interv. 2019;12(9):859–869. doi: 10.1016/j.jcin.2018.12.022. [DOI] [PubMed] [Google Scholar]