Abstract
Transforming growth factor-β1 (TGF-β1)-induced epithelial-mesenchymal transition (EMT) serves a significant role in pulmonary fibrosis (PF). Increasing evidence indicates that microRNAs (miRNAs or miRs) contribute to PF pathogenesis via EMT regulation. However, the role of miR-483-5p in PF remains unclear. Therefore, the present study investigated the potential effect of miR-483-5p on TGF-β1-induced EMT in PF. It was found that the expression of miR-483-5p was upregulated in both PF tissue and A549 cells treated with TGF-β1, whereas expression of Rho GDP dissociation inhibitor 1 (RhoGDI1) was downregulated. miR-483-5p mimic transfection promoted TGF-β1-induced EMT; by contrast, miR-483-5p inhibitor inhibited TGF-β1-induced EMT. Also, miR-483-5p mimic decreased RhoGDI1 expression, whereas miR-483-5p inhibitor increased RhoGDI1 expression. Furthermore, dual-luciferase reporter gene assay indicated that miR-483-5p directly regulated RhoGDI1. Moreover, RhoGDI1 knockdown eliminated the inhibitory effect of the miR-483-5p inhibitor on TGF-β1-induced EMT via the Rac family small GTPase (Rac)1/PI3K/AKT pathway. In conclusion, these data indicated that miR-483-5p inhibition ameliorated TGF-β1-induced EMT by targeting RhoGDI1 via the Rac1/PI3K/Akt signaling pathway in PF, suggesting a potential role of miR-483-5p in the prevention and treatment of PF.
Keywords: microRNA-483-5p, epithelial- mesenchymal transition, pulmonary fibrosis, TGF-β1
Introduction
Pulmonary fibrosis (PF) is a chronic, progressive and fatal disease with an unclear etiology (1). The most common type of PF is idiopathic PF, with an annual incidence of 16.3–17.4 per 100,000 individuals, as determined using broad case definitions in the USA (1). PF is characterized by repetitive alveolar epithelial cell injury, fibroblast activation and increased extracellular matrix deposition, resulting in lung function distortion (2–4). While anti-inflammatory and antifibrinolytics agents and glucocorticoids are utilized for PF, no effective lung fibrosis treatment exists and patients with PF have a median survival of only 2–4 years (5). Therefore, elucidation of mechanisms underlying PF and the identification of potential early detection PF biomarkers are necessary.
Epithelial-mesenchymal transition (EMT), characterized by loss of epithelial characteristics (E-cadherin expression) and gain of mesenchymal features [vimentin and α-smooth muscle actin (α-SMA) expression], serves a key role in fibrosis pathogenesis (6). Transforming growth factor-β1 (TGF-β1) has been implicated as a ‘master switch’ in the induction of fibrosis in various organs, including the lung (7).
MicroRNAs (miRNAs or miRs) are a class of small, non-coding RNAs that inhibit gene expression by binding to the 3′-untranslated regions (3′-UTRs) of target genes (8). miRNAs have been implicated in various biological processes, including cell proliferation and differentiation (9). Accumulating evidence has shown that miRNAs are critical in the EMT and PF processes (10). For example, miR-26a overexpression has been found to inhibit TGF-β1-induced EMT via the regulation of high-mobility group protein A2 in PF (11). Wang et al (12) reported that a miR-483-5p inhibitor serves a role in lung cancer by targeting RBM5 to induce apoptosis. Another previous study indicated that miR-483-5p is upregulated in serum from patients with systemic sclerosis and is a potential fibrosis driver in systemic sclerosis (13). To the best of our knowledge, however, the underlying role of miR-483-5p in PF development has not been studied.
The present study aimed to determine the expression level of miR-483-5p in normal lung tissues and PF tissues. Then, the role of miR-483-5p in TGF-β1-induced EMT was examined in A549 cells. Finally, the mechanism of miR-483-5p in TGF-β1-induced EMT was determined.
Materials and methods
Ethics statement
The present study was approved by the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University (approval no. 2020-147) and was performed in accordance with the Declaration of Helsinki. All patients provided written informed consent.
Tissues, cell lines and cell culture
A total of 12 PF tissue samples were collected from patients undergoing lung biopsy (including 8 females and 4 males). A total of 17 control lung tissue samples (including 10 females and 7 males) were obtained from the normal areas of the peripheral lung removed during lung cancer resection. The average age of patients with PF was 60.5 years and control subjects was 55.5 years. Detailed information on the control subjects and patients with PF, who were diagnosed with PF via pathology examinations, is provided in Table SI. The inclusion criteria for control subjects was individuals who underwent the lung cancer resection and without other pulmonary disease, and the normal areas of the peripheral lung were collect. All tissue samples were collected between June 2020 and December 2020 at The First Affiliated Hospital of Chongqing Medical University.
Human alveolar epithelial cells (A549) were purchased from the Cell Bank of the Chinese Academy of Sciences. The cells were maintained in RPMI-1640 (Hyclone; Cytiva) medium containing 10% FBS (PAN-Biotech GmbH), 100 U/ml penicillin and 100 µg/ml streptomycin at 37°C in a humidified 5% CO2 atmosphere. The A549 cells were treated with 10 ng/ml TGF-β1 (PeproTech, Inc.) at 37°C for 48 h to establish the EMT cell model, as previously described (6,14).
Cell transfection
The A549 cells were transfected with either at the final concentration of 50 nM miR-483-5p mimic or inhibitor (Shanghai GenePharma Co., Ltd.) using Lipofectamine® 3000 (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. The sequences of miR-483-5p mimic, inhibitor, and corresponding negative control (NC) are provided in Table SII. In brief, miRNA and Lipofectamine 3000 were separately mixed with 250 µl RPMI-1640 serum-free medium. Then, both mixtures were combined and incubated for 15 min at room temperature. Finally, the Lipofectamine 3000 and miRNA mixture was added to the cells and incubated for 24 h at 37°C. After 24 h transfection, the cells were treated in the presence or absence of 10 ng/ml TGF-β1 for 48 h at 37°C, then collected and utilized for further experiments.
Lentivirus transfection
In order to establish stable genetic Rho GDP dissociation inhibitor 1 (RhoGDI1) knockdown, lentivirus was utilized as a vector to carry the interference sequence. In brief, lentivirus vectors containing either the target gene or NC were constructed by Hanbio Biotechnology Co., Ltd. The lentiviral backbone used for short harpin (sh)RNA was pHBLV-U6-MCS-CMV-ZsGreen-PGK-PRUO (3rd). Sequences of RhoGDI1 and NC are listed in Table SII. In order to measure the infection efficiency and select the cells, each lentivirus vector expressed the green fluorescent protein and puromycin resistance gene. The multiplicity of infection for A549 cells is 50. A549 cells (1×105 per well) in the logarithmic growth phase were digested with trypsin and seeded in six-well plates. The next day, the cells were incubated at 37°C in 2 ml RPMI-1640 complete medium containing lentivirus and 5 µg/ml Polybrene. After 24 h, the medium was replaced with fresh complete medium without both lentivirus and Polybrene, and cultured for another 48 h at 37°C. Following this, expression of green fluorescent protein was observed via a fluorescence microscope (magnification, ×20). The cells were cultured with 1 µg/ml puromycin to select stable knockdown lines. Finally, reverse transcription-quantitative (RT-q)PCR and western blot assay were utilized to determine the shRNA knockdown efficiency.
RT-qPCR
In order to detect the mRNA or miRNA levels, total RNA from lung tissue or A549 cells was extracted using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. The RNA concentration was determined via a NanoDrop 2000 micro-spectrophotometer (Thermo Fisher Scientific, Inc.). Next, 1 µg total RNA was utilized to synthesize complementary (c)DNA via a PrimeScript RT Reagent kit (Takara Biotechnology Co., Ltd.). The gDNA elimination reaction was conducted at 42°C for 2 min and reverse transcription was performed at 37°C for 15 min and at 85°C for 5 sec. Subsequently, cDNA was amplified via the TB Green Premix EX Taq II PCR kit (Takara Biotechnology Co., Ltd.). Amplification cycle included an initial 30 sec incubation at 95°C for denaturation, followed by 40 cycles of 5 sec at 95°C for annealing and 30 sec at 60°C for elongation. Small nuclear RNA U6 was utilized for the internal normalization of miR-483-5p, and GAPDH was utilized as a control for mRNA expression. Relative quantification was calculated via the 2−ΔΔCq method (15). The primer sequences utilized are listed in Table SIII.
Western blot assay
Total protein was extracted from the A549 cells using RIPA lysis buffer supplemented with protease and phosphatase inhibitor. The proteins were quantified via a bicinchoninic acid kit (Beyotime Institute of Biotechnology). Then, the proteins (25 µg) were separated via 10% SDS-PAGE and transferred onto PVDF membranes (EMD Millipore). The membranes were blocked with 5% non-fat milk at room temperature for 2 h, then incubated overnight with specific primary antibodies at 4°C. The next day, membranes were washed three times with Tris-buffered saline with 1% Tween-20, then incubated with secondary antibodies (1:8,000; Zhong Shan-Golden Bridge Biological Technology Co., Ltd.; cat. no. ZB-2306) for 1 h at room temperature. The proteins were visualized via an electrochemiluminescence kit (Wuhan Boster Biological Technology Ltd.). Images were captured with the use of an automatic Fusion FX Edge chemiluminescence image analysis system (Vilber Lourmat Sa). The Fusion Capt software v.18.06 (Vilber Lourmat Sa) was used for the densitometric analysis of the blot images. The following primary antibodies were utilized: Anti-E-cadherin (1:10,000; Abcam; cat. no. ab40772), anti-α-SMA (1:2,000; Abcam; cat. no. ab32575), anti-vimentin (1:3,000; Abcam; cat. no. ab92547), anti-RhoGDI1 (1:7,000; Abcam; cat. no. ab133248), anti-Rac family small GTPase (Rac)1 (1:1,000; Cell Signaling Technology, Inc.; cat. no. 4651), anti-Akt (1:10,000; Abcam; cat. no. ab179463), anti-phosphorylated (p)-Akt (1:8,000; Abcam; cat. no. ab81283), anti-p-PI3K (1:2,000; GeneTex, Inc.; cat. no. GTx132597), anti-PI3K (1:1,000; Abcam; cat. no. ab191606) and anti-GAPDH (1:10,000; Abcam; cat. no. ab181602).
Rac activity assay
Rac activity was determined via a Rac activation assay kit (Cell Signaling Technology, Inc.) according to the manufacturer's instructions. In brief, the cells were washed twice with ice-cold PBS and were harvested using 1X lysis/binding/wash buffer containing phenylmethanesulfonyl fluoride (PMSF). Then, the GST-PAK1-PBD fusion protein was used to bind the GTP-bound Rac1, which was immunoprecipitated via glutathione resin. Finally, bound Rac1 protein was detected using western blot assay and anti-Rac1 antibodies.
Luciferase reporter assay
The potential target gene of miR-483-5p was identified using TargetScan (Version 7.2; http://www.targetscan.org/). The luciferase reporter assay was performed using a Dual-Luciferase Reporter Assay System according to the manufacturer's instructions (Promega Corporation) to validate the target association between miR-483-5p and RhoGDI1. The RhoGDI1 wild-type (wt) and mutant (mut) 3′-UTRs were constructed and cloned from genomic DNA and inserted into the pSI-Check2 vector. The 293T cells were cultured in 96-well plates and co-transfected with miR-483-5p mimics/NC and wt or mut pSI-Check2-RhoGDI1-3′-UTR using Lipofectamine 3000 (Invitrogen; Thermo Fisher Scientific, Inc.). After 48 h, the luciferase activity was detected via a dual-luciferase reporter system (Promega Corporation). Luciferase activity was normalized to that of Renilla.
Statistical analysis
Data were analyzed via SPSS 23.0 software (IBM Corp.). Data are presented as the mean ± SD (n=3). The comparisons between two groups were analyzed via unpaired Student's t-test. Multiple comparisons were assessed via one-way ANOVA followed by post hoc Tukey's test. P<0.05 was considered to indicate a statistically significant difference.
Results
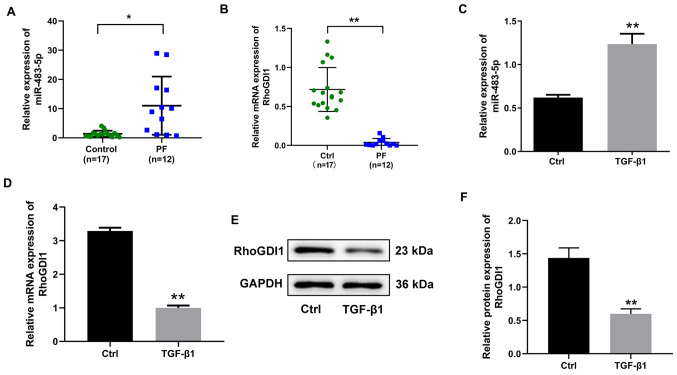
miR-483-5p expression is upregulated and RhoGDI1 expression is downregulated in PF tissue and TGF-β1-induced EMT in A549 cells
In order to investigate whether miR-483-5p participated in PF development, the expression of miR-483-5p in PF tissue and TGF-β1-induced EMT were detected. Expression of miR-483-5p was significantly increased in PF compared with control tissue (Fig. 1A). The expression of miR-483-5p in TGF-β1 treated with A549 cells in vitro was determined; TGF-β1 upregulated miR-483-5p expression compared with the control group (Fig. 1C). Subsequently, RhoGDI1 was predicted to be a miR-483-5p target gene via online tools. In order to validate this prediction, the expression of RhoGDI1 was detected in PF tissue and TGF-β1-treated A549 cells and was observed to be significantly decreased at both the mRNA and protein level in PF tissue and TGF-β1 treated A549 cells (Fig. 1B and D-F). Considered together, these findings indicated that expression of miR-483-5p was upregulated in both the PF tissue and TGF-β1-stimulated A549 cells, whereas the expression of RhoGDI1 was downregulated.
Figure 1.
Expression of miR-483-5p and RhoGDI1 in human PF tissue and A549 cells treated with TGF-β1. The relative expression of (A) miR-483-5p and (B) RhoGDI1in PF (n=12) and normal lung tissue (n=17) was determined by RT-qPCR. *P<0.05 and **P<0.01. (C) Relative expression of miR-483-5p in A549 cells treated with 10 ng/ml TGF-β1 for 48 h was determined by RT-qPCR. The relative (D) mRNA and (E and F) protein expression of RhoGDI1 in A549 cells treated with 10 ng/ml TGF-β1 for 48 h were detected by RT-qPCR and western blot. Data are presented as the mean ± SD (n=3). **P<0.01 vs. Ctrl. PF, pulmonary fibrosis; RhoGDI1, Rho GDP dissociation inhibitor 1; RT-qPCR, reverse transcription-quantitative PCR; TGF-β1, transforming growth factor-β1; miR, microRNA; Ctrl, control.
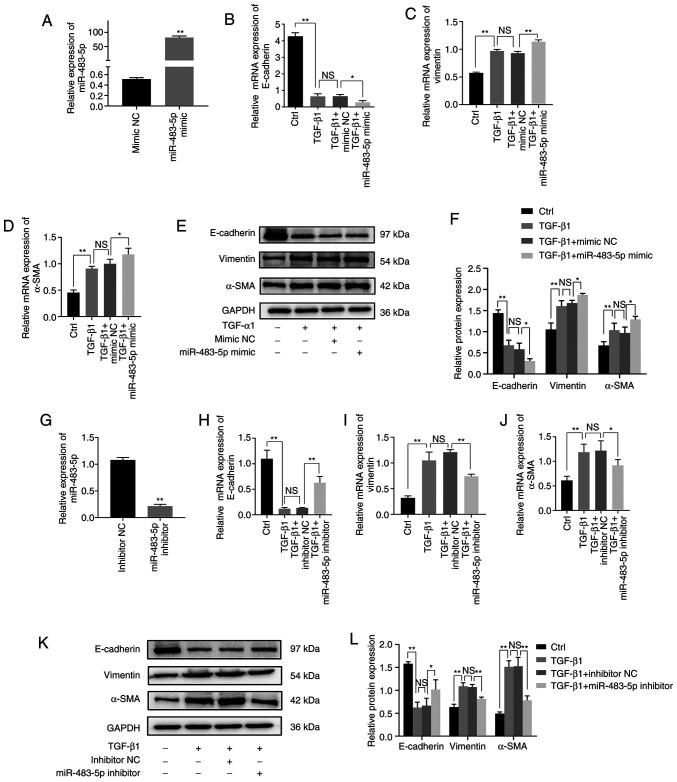
miR-483-5p promotes TGF-β1-induced EMT
In order to assess the role of miR-483-5p in TGF-β1-induced EMT in A549 cells, miR-483-5p mimics or inhibitors were transfected into A549 cells, which were then treated with TGF-β1. miRNA transfection efficiency was assessed via RT-qPCR. Following 24 h transfection, the miR-483-5p level increased by ~90 times in the miR-483-5p mimics group compared with the mimic-NC group (Fig. 2A). Additionally, the miR-483-5p level decreased by ~6 times in the miR-483-5p inhibitor-transfected compared with the inhibitor-NC group (Fig. 2G). These results indicated that the transfection was efficient.
Figure 2.
Effect of miR-483-5p on TGF-β1-induced EMT. (A) Relative expression of miR-483-5p in A549 cells after 24 h transfection with miR-483-5p mimic was detected via RT-qPCR. **P<0.01 vs. mimic NC. Following treatment with TGF-β1 for 48 h, relative of expression of (B) E-cadherin, (C) vimentin and (D) α-SMA were determined by RT-qPCR and (E and F) western blotting. A549 cells were transfected with miR-483-5p inhibitor for 24 h, and then treated with TGF-β1 for 48 h. *P<0.05; **P<0.01. (G) Relative expression of miR-483-5p in A549 cells following transfection with inhibitor. **P<0.01 vs. inhibitor NC. The relative of expression of (H) E-cadherin, (I) vimentin and (J) α-SMA were determined by RT-qPCR and (K and L) western blotting. Data are presented as the mean ± SD (n=3). *P<0.05; **P<0.01. NS, not significant; EMT, epithelial-mesenchymal transition; TGF-β1, transforming growth factor-β1; α-SMA, α-smooth muscle actin; miR, microRNA; RT-qPCR, reverse transcription-quantitative PCR; NC, negative control.
In order to investigate the functional effect of miR-483-5p on TGF-β1-induced EMT in A549 cells, EMT biomarkers, including E-cadherin, vimentin and α-SMA, were detected via RT-qPCR and western blot assay. Upregulation of miR-483-5p inhibited TGF-β1-stimulated E-cadherin expression but increased the expression of vimentin and α-SMA at both the mRNA and protein levels (Fig. 2B-F). Downregulation of miR-483-5p increased TGF-β1-induced E-cadherin expression but decreased TGF-β1-induced vimentin and α-SMA expression at both the mRNA and protein level (Fig. 2H-L). Collectively, these findings suggested that upregulation of miR-483-5p promoted TGF-β1-induced EMT, whereas downregulation of miR-483-5p suppressed TGF-β1-induced EMT.
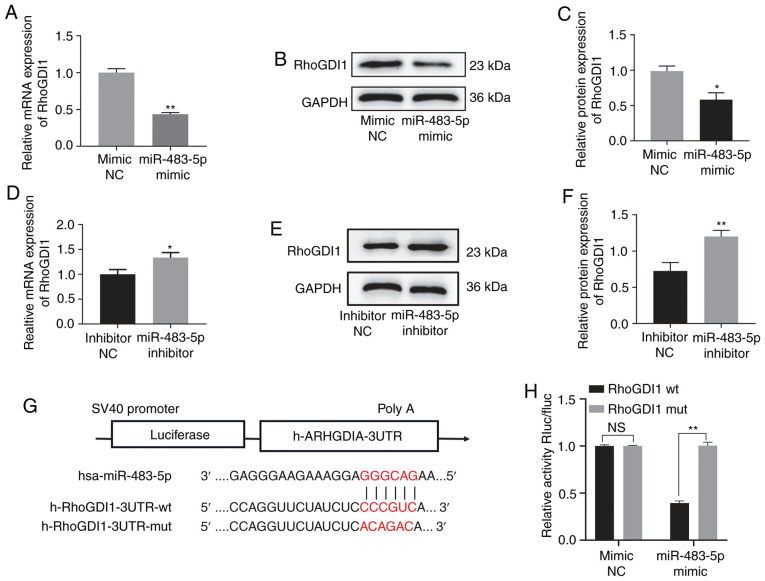
RhoGDI1 is a target gene of miR-483-5p
The miR-483-5p target gene was predicted via the online database TargetScan 7.2 and RhoGDI1 was identified as a potential miR-483-5p target gene (Fig. 3G). Therefore, the association between miR-483-5p and RhoGDI1 was determined via RT-qPCR and western blot assay. Expression of RhoGDI1 was decreased in the miR-483-5p mimic group compared with the mimic-NC group at both the mRNA and protein level, but was increased in the miR-483-5p inhibitor group compared with the inhibitor-NC group, indicating a negative association between miR-483-5p and RhoGDI1 (Fig. 3A-F). In order to confirm RhoGDI1 as a miR-483-5p target, luciferase reporter assays were performed. The results indicated that luciferase activity of the RhoGDI1-wt vector was significantly decreased by co-transfection with miR-483-5p mimics compared with the RhoGDI1-mut group (Fig. 3H). These findings suggested that RhoGDI1 was directly regulated by miR-483-5p.
Figure 3.
Identification of target gene for miR-483-5p. The relative expression of RhoGDI1 in A549 cells transfected with miR-483-5p mimic or mimic NC for 48 h was determined by (A) RT-qPCR and (B and C) western blot analysis. *P<0.05; **P<0.01 vs. mimic NC. The relative expression of RhoGDI1 in A549 cells transfected with miR-483-5p inhibitor or inhibitor NC for 48 h was determined by (D) RT-qPCR and (E and F) western blotting. *P<0.05; **P<0.01 vs. inhibitor NC. (G) RhoGDI1 3′-UTR region containing wt or mut binding site for miR-483-5p. (H) Luciferase activity resulting from the interaction between miR-483-5p and 3′UTR of RhoGDI1. Data are presented as the mean ± SD (n=3). **P<0.01. NS, not significant; RhoGDI1, Rho GDP dissociation inhibitor 1; UTR, untranslated region; NC, negative control; miR, microRNA; RT-qPCR, reverse transcription-quantitative PCR; wt, wild-type; mut, mutant.
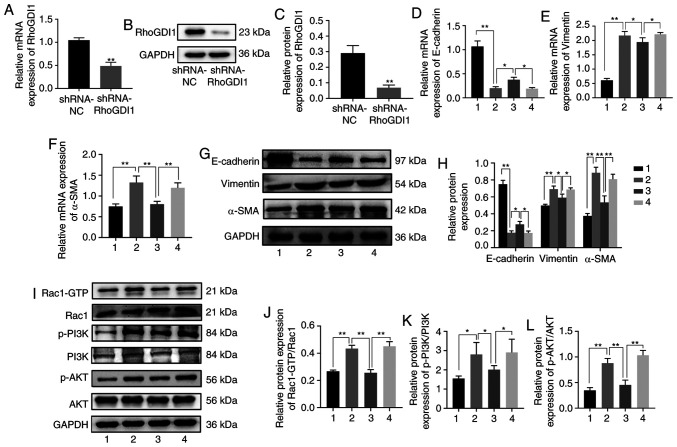
RhoGDI1 silencing eliminates the effect of the miR-483-5p inhibitor on TGF-β1-induced EMT
In order to confirm that the miR-483-5p inhibitor suppressed TGF-β1-induced EMT via a RhoGDI1-dependent pathway, miR-483-5p inhibitor was transfected into A549 cells with RhoGDI1 knockdown. First, the knockdown efficiency in the A549 cells was tested. Expression of RhoGDI1 was significantly downregulated in the shRNA-RhoGDI1 group compared with the shRNA-NC group at both the mRNA and protein levels, which demonstrated that the knockdown was efficient (Fig. 4A-C). The results of RT-qPCR and western blot assay indicated that the expression of E-cadherin was decreased, but expression of vimentin and α-SMA increased, in the TGF-β1 + miR-483-5p inhibitor + shRNA-RhoGDI1 group compared with the TGF-β1 + miR-483-5p inhibitor + shRNA-NC group (Fig. 4D-H). These findings indicated that RhoGDI1 knockdown eliminated the effect of miR-483-5p inhibitor on TGF-β1-induced EMT.
Figure 4.
miR-483-5p inhibitor inhibits TGF-β1-induced EMT by targeting RhoGDI1 via the Rac1/PI3K/AKT signaling pathway. The relative expression of RhoGDI1 in A549 cells infected with lentivirus carrying the interference sequence of RhoGDI1 was detected by (A) RT-qPCR and (B and C) western blotting. **P<0.01 vs. shRNA-NC. A549 cells or A549 cells with shRNA-RhoGDI1 silencing were transfected with miR-483-5p inhibitor for 24 h, and then treated with TGF-β1 for 48 h. The relative of expression of (D) E-cadherin, (E) vimentin and (F) α-SMA were determined by RT-qPCR and (G and H) western blotting. (I) Expression of (J) Rac1-GTP, Rac1, (K) p-PI3K, PI3K, (L) p-AKT and AKT were determined by western blot analysis. Data are presented as the mean ± SD (n=3). *P<0.05; **P<0.01. NS, not significant. 1=Ctrl, 2=TGF-β1 group, 3=TGF-β1+ miR-483-5p inhibitor+ shRNA-NC group, 4=TGF-β1+ miR-483-5p inhibitor + shRNA-RhoGDI1 group. EMT, epithelial-mesenchymal transition; RhoGDI1, Rho GDP dissociation inhibitor 1; TGF-β1, transforming growth factor-β1; α-SMA, α-smooth muscle actin; miR, microRNA; Rac1, Rac family small GTPase 1; RT-q, reverse transcription-quantitative; p-, phosphorylated; sh, short hairpin; NC, negative control; Ctrl, control.
miR-483-5p inhibitor suppresses TGF-β1-induced EMT via the Rac1/PI3K/AKT signaling pathway
In order to elucidate the mechanism underlying suppression of TGF-β1-induced EMT by miR-483-5p inhibitor, the RhoGDI1 downstream signaling pathway was detected. RhoGDI1 is a negative Rho GTPase regulator (16), which belongs to the Ras superfamily of small GTPases (17), and Rac1 is a family member of Rho GTPase. The PI3K/AKT axis is a key Ras effector (18). Therefore, the expression levels of Rac1/PI3K/AKT pathway-associated indicators were evaluated. Expressions of Rac1-GTP, p-PI3K and p-AKT were significantly higher in the TGF-β1 group than in the control group (Fig. 4I-L). However, in the TGF-β1 + miR-483-5p inhibitor + shRNA-NC group, expression levels of Rac1-GTP, p-PI3K, and p-AKT were lower than those in the TGF-β1 group (Fig. 4I-L). Furthermore, expression of Rac1-GTP, p-PI3K, and p-AKT was significantly increased in the TGF-β1 + miR-483-5p inhibitor + shRNA-RhoGDI1 group compared with the TGF-β1 + miR-483-5p inhibitor + shRNA-NC group (Fig. 4I-L). Considered together, these findings implied that miR-483-5p inhibition may suppress TGF-β1-induced EMT via the Rac1/PI3K/AKT signaling pathway in PF.
Discussion
PF is a progressive interstitial lung disease characterized by alveolar epithelial injury, fibroblast activation and extracellular matrix deposition (19). miRNAs are endogenous, small non-coding RNA that modulate genes at the post-transcription level in various physiological and pathological processes (20). Increasing evidence has indicated that miRNAs drive the onset and progression of PF (21,22).
In the present study, upregulation of miR-483-5p was observed in human PF tissue, and the functional role of miR-483-5p and the underlying mechanism of its effect on PF were identified. The results demonstrated that TGF-β1 increased expression of miR-483-5p and decreased expression of RhoGDI1 in A549 cells. Also, downregulation of miR-483-5p inhibited TGF-β1-induced EMT, which was regulated by targeting RhoGDI1. Upregulation of miR-483-5p promoted TGF-β1-induced EMT.
EMT serves a key role in organ fibrosis, including kidney and lung fibrosis (23). Moreover, TGF-β1 is an important cytokine for EMT induction (24). In PF development, alveolar epithelial cells take on the characteristics of mesenchymal cells by undergoing EMT (25). Although A549 is a cancer cell line, these cells possess normal characteristics (26) of type II alveolar epithelial cells (27), such as their general morphology, and have been utilized to investigate the mechanism of EMT in PF (28–32). Therefore, the A549 cell line was utilized to establish an EMT model in the present study. In general, downregulated E-cadherin and upregulated vimentin and α-SMA are used in epithelial cells as reliable markers of EMT occurrence. As A549 is an epithelial cell line (27), it exhibits high basal expression levels of E-cadherin, which is an epithelial cell marker (6,28). In A549 cells treated with TGF-β1 at 10 ng/ml for 48 h, E-cadherin was significantly downregulated, and vimentin and α-SMA were upregulated. Western blotting showed that the E-cadherin strip was thicker in control groups than in groups treated with TGF-β1. The reason for this result may be that the final concentration of TGF-β1 was relatively high when compared with the control group. These findings indicated that TGF-β1 induced EMT, which was consistent with a previous study (6). Furthermore, overexpression of miR-483-5p promoted TGF-β1-induced EMT; by contrast, downregulation of miR-483-5p inhibited TGF-β1-induced EMT.
Rho GDP dissociation inhibitors (RhoGDIs) are involved in various cell processes, including migration, adhesion and proliferation, via regulation of Rho GTPase family functions (33). RhoGDIs contains three members, namely RhoGDI1, RhoGDI2 and RhoGDI3. RhoGDI1, also known as RhoGDIα or ARHGDIα, is ubiquitously expressed in many types of cell (34) and has been studied in different types of cancer. For instance, Song et al (35) reported that downregulation of RhoGDI1 promotes lung adenocarcinoma invasion and metastasis via EMT regulation. Jiang et al (36) reported that decreased expression of RhoGDI1 is correlated with nodal involvement and metastasis in human breast cancer. In the present study, RhoGDI1 was downregulated in PF tissue and TGF-β1-induced EMT in A549 cells. It was also directly regulated by miR-483-5p. Furthermore, RhoGDI1 knockdown eliminated the effect of miR-483-5p inhibitor on TGF-β1-induced EMT. These results indicated that RhoGDI1 participated in PF via the EMT process.
Rac1, a member of the Rho family of small GTPases, is involved in a variety of dynamic biological cell processes, including proliferation, EMT, cell-cell contact, motility and invasiveness (37). Rac1 activity is positively regulated by guanine nucleotide exchanges factors, which favor GDP/GTP exchange, GTPase-activating proteins, which favor the switching on/off of GTP/GDP, and guanosine nucleotide dissociation inhibitor (GDI) that binds to GDP-bound forms, preventing GDP/GTP exchange (off state) and sequestering small GTPases in the cytoplasm to form an inactive pool (37). Therefore, RhoGDI1 negatively regulates Rac1 by regulating the GDP/GTP exchange cycle (37). Numerous studies have indicated that the PI3K/AKT signaling pathway is essential in TGF-β1-induced EMT in PF (38,39), and PI3K activity can be stimulated via Rac1-GTP (40). Feng et al (41) reported that miRNA-630 suppresses EMT by regulating forkhead box M1 via inactivation of the Rac1/PI3K/AKT pathway in gastric cancer. Shen et al (42) demonstrated that cigarette smoke induces EMT by activating the Rac1/PI3K/AKT signaling pathway in chronic obstructive pulmonary disease. Another study indicated that neogenin-1 promotes EMT by upregulating zinc finger E-box-binding homeobox 1 via activation of the Rac1/PI3K/AKT pathway in gastric cancer (43). In addition, Xu et al (44) reported that Rac1 promotes a fibrogenic phenotype in fibroblasts via PI3K/AKT, which results in fibrotic disease. Another study demonstrated that endothelin-1 contributes to lung fibrosis through endothelin-1 receptor via Rac/PI3K/AKT-dependent signaling pathway (45). The results of the present study indicate that TGF-β1 upregulated expression of GTP-Rac1, p-PI3K and p-AKT, and that the miR-483-5p inhibitor downregulated levels of GTP-Rac1, p-PI3K and p-AKT. Moreover, RhoGDI1 knockdown reversed the effect of miR-483-5p inhibitor on the expression of GTP-Rac1, p-PI3K and p-AKT, indicating that miR-483-5p inhibitor suppressed TGF-β1-induced EMT by targeting RhoGDI1 via Rac1/PI3K/AKT inactivation.
In conclusion, the present results suggested that miR-483-5p promoted TGF-β1-induced EMT in PF via RhoGDI1 inhibition; this effect may be due to activation of the Rac1/PI3K/AKT pathway. Therefore, miR-483-5p inhibition may provide a novel approached for the prevention and treatment of lung fibrosis.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
The present study was supported by the National Major Science and Technology Projects of China (grant no. 2018ZX10302302003).
Funding
The present study was supported by the National Major Science and Technology Projects of China (grant no. 2018ZX10302302003).
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Authors' contributions
GH and SG designed the experiments and revised the manuscript. JZ, GQ and DL analyzed the data and revised the manuscript. GH and XW performed the experiments and wrote the manuscript. XW, YW, YL and YC analyzed and interpreted the data. GH and SG confirmed the authenticity of all the raw data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of The First Affiliated Hospital of Chongqing Medical University (approval no. 2020-147) and was performed in accordance with the Declaration of Helsinki. All patients provided written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Nalysnyk L, Cid-Ruzafa J, Rotella P, Dirk E. Incidence and prevalence of idiopathic pulmonary fibrosis: Review of the literature. Eur Respir Rev. 2012;21:355–361. doi: 10.1183/09059180.00002512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rydell-Törmänen K, Andréasson K, Hesselstrand R, Risteli J, Heinegård D, Saxne T, Westergren-Thorsson G. Extracellular matrix alterations and acute inflammation; developing in parallel during early induction of pulmonary fibrosis. Lab Invest. 2012;92:917–925. doi: 10.1038/labinvest.2012.57. [DOI] [PubMed] [Google Scholar]
- 3.Wynn TA, Ramalingam TR. Mechanisms of fibrosis: Therapeutic translation for fibrotic disease. Nat Med. 2012;18:1028–1040. doi: 10.1038/nm.2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King TE, Pardo A, Selman M. Idiopathic pulmonary fibrosis. Lancet. 2011;378:1949–1961. doi: 10.1016/S0140-6736(11)60052-4. [DOI] [PubMed] [Google Scholar]
- 5.Richeldi L, Collard HR, Jones MG. Idiopathic pulmonary fibrosis. Lancet. 2017;389:1941–1952. doi: 10.1016/S0140-6736(17)30866-8. [DOI] [PubMed] [Google Scholar]
- 6.Wang YC, Liu JS, Tang HK, Nie J, Zhu JX, Wen LL, Guo QL. miR-221 targets HMGA2 to inhibit bleomycin-induced pulmonary fibrosis by regulating TGF-β1/Smad3-induced EMT. Int J Mol Med. 2016;38:1208–1216. doi: 10.3892/ijmm.2016.2705. [DOI] [PubMed] [Google Scholar]
- 7.Willis BC, Borok Z. TGF-beta-induced EMT: Mechanisms and implications for fibrotic lung disease. Am J Physiol Lung Cell Mol Physiol. 2007;293:L525–L534. doi: 10.1152/ajplung.00163.2007. [DOI] [PubMed] [Google Scholar]
- 8.Stefani G, Slack FJ. Small non-coding RNAs in animal development. Nat Rev Mol Cell Biol. 2008;9:219–230. doi: 10.1038/nrm2347. [DOI] [PubMed] [Google Scholar]
- 9.Gai YP, Zhao HN, Zhao YN, Zhu BS, Yuan SS, Li S, Guo FY, Ji XL. MiRNA-seq-based profiles of miRNAs in mulberry phloem sap provide insight into the pathogenic mechanisms of mulberry yellow dwarf disease. Sci Rep. 2018;8:812. doi: 10.1038/s41598-018-19210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miao C, Xiong Y, Zhang G, Chang J. MicroRNAs in idiopathic pulmonary fibrosis, new research progress and their pathophysiological implication. Exp Lung Res. 2018;44:178–190. doi: 10.1080/01902148.2018.1455927. [DOI] [PubMed] [Google Scholar]
- 11.Liang H, Gu Y, Li T, Zhang Y, Huangfu L, Hu M, Zhao D, Chen Y, Liu S, Dong Y, et al. Integrated analyses identify the involvement of microRNA-26a in epithelial-mesenchymal transition during idiopathic pulmonary fibrosis. Cell Death Dis. 2014;5:e1238. doi: 10.1038/cddis.2014.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang F, Zhang X, Zhong X, Zhang M, Guo M, Yang L, Li Y, Zhao J, Yu S. Effect of miR-483-5p on apoptosis of lung cancer cells through targeting of RBM5. Int J Clin Exp Pathol. 2018;11:3147–3156. [PMC free article] [PubMed] [Google Scholar]
- 13.Chouri E, Servaas NH, Bekker CPJ, Affandi AJ, Cossu M, Hillen MR, Angiolilli C, Mertens JS, van den Hoogen LL, Silva-Cardoso SL, et al. Serum microRNA screening and functional studies reveal miR-483-5p as a potential driver of fibrosis in systemic sclerosis. J Autoimmun. 2018;89:162–170. doi: 10.1016/j.jaut.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Tang H, He H, Ji H, Gao L, Mao J, Liu J, Lin H, Wu T. Tanshinone IIA ameliorates bleomycin-induced pulmonary fibrosis and inhibits transforming growth factor-beta-β-dependent epithelial to mesenchymal transition. J Surg Res. 2015;197:167–175. doi: 10.1016/j.jss.2015.02.062. [DOI] [PubMed] [Google Scholar]
- 15.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative Pcr and the 2(-delta delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 16.Lin X, Yang B, Liu W, Tan X, Wu F, Hu P, Jiang T, Bao Z, Yuan J, Qiang B, et al. Interplay between PCBP2 and miRNA modulates ARHGDIA expression and function in glioma migration and invasion. Oncotarget. 2016;7:19483–19498. doi: 10.18632/oncotarget.6869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hall A. Rho GTPases and the control of cell behaviour. Biochem Soc Trans. 2005;33:891–895. doi: 10.1042/BST0330891. [DOI] [PubMed] [Google Scholar]
- 18.Castellano E, Downward J. RAS Interaction with PI3K: More than just another effector pathway. Genes Cancer. 2011;2:261–274. doi: 10.1177/1947601911408079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Strieter RM, Mehrad B. New mechanisms of pulmonary fibrosis. Chest. 2009;136:1364–1370. doi: 10.1378/chest.09-0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomankova T, Petrek M, Kriegova E. Involvement of microRNAs in physiological and pathological processes in the lung. Respir Res. 2010;11:159. doi: 10.1186/1465-9921-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajasekaran S, Rajaguru P, Sudhakar Gandhi PS. MicroRNAs as potential targets for progressive pulmonary fibrosis. Front Pharmacol. 2015;6:254. doi: 10.3389/fphar.2015.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Y, Zhang Q, Zhou Y, Yang Z, Tan M. Inhibition of miR-182-5p attenuates pulmonary fibrosis via TGF-β/Smad pathway. Hum Exp Toxicol. 2019;39:683–695. doi: 10.1177/0960327119895549. [DOI] [PubMed] [Google Scholar]
- 23.Stone RC, Pastar I, Ojeh N, Chen V, Liu S, Garzon KI, Tomic-Canic M. Epithelial-mesenchymal transition in tissue repair and fibrosis. Cell Tissue Res. 2016;365:495–506. doi: 10.1007/s00441-016-2464-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang C, Zhu X, Hua Y, Zhao Q, Wang K, Zhen L, Wang G, Lü J, Luo A, Cho WC, et al. YY1 mediates TGF-β1-induced EMT and pro-fibrogenesis in alveolar epithelial cells. Respir Res. 2019;20:249. doi: 10.1186/s12931-019-1223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chapman HA. Epithelial-mesenchymal interactions in pulmonary fibrosis. Annu Rev Physiol. 2011;73:413–435. doi: 10.1146/annurev-physiol-012110-142225. [DOI] [PubMed] [Google Scholar]
- 26.Mason RJ, Walker SR, Shields BA, Henson JE, Williams MC. Identification of rat alveolar type II epithelial cells with a tannic acid and polychrome stain. Am Rev Respir Dis. 1985;131:786–788. doi: 10.1164/arrd.1985.131.5.786. [DOI] [PubMed] [Google Scholar]
- 27.Foster KA, Oster CG, Mayer MM, Avery ML, Audus KL. Characterization of the A549 cell line as a type II pulmonary epithelial cell model for drug metabolism. Exp Cell Res. 1998;243:359–366. doi: 10.1006/excr.1998.4172. [DOI] [PubMed] [Google Scholar]
- 28.Tan X, Dagher H, Hutton CA, Bourke JE. Effects of PPAR gamma ligands on TGF-beta1-induced epithelial-mesenchymal transition in alveolar epithelial cells. Respir Res. 2010;11:21. doi: 10.1186/1465-9921-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kasai H, Allen JT, Mason RM, Kamimura T, Zhang Z. TGF-beta1 induces human alveolar epithelial to mesenchymal cell transition (EMT) Respir Res. 2005;6:56. doi: 10.1186/1465-9921-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu H, Königshoff M, Jayachandran A, Handley D, Seeger W, Kaminski N, Eickelberg O. Transgelin is a direct target of TGF-beta/Smad3-dependent epithelial cell migration in lung fibrosis. FASEB J. 2008;22:1778–1789. doi: 10.1096/fj.07-083857. [DOI] [PubMed] [Google Scholar]
- 31.Ando S, Otani H, Yagi Y, Kawai K, Araki H, Fukuhara S, Inagaki C. Proteinase-activated receptor 4 stimulation-induced epithelial-mesenchymal transition in alveolar epithelial cells. Respir Res. 2007;8:31. doi: 10.1186/1465-9921-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhu Y, Tan J, Xie H, Wang J, Meng X, Wang R. HIF-1α regulates EMT via the Snail and β-catenin pathways in paraquat poisoning-induced early pulmonary fibrosis. J Cell Mol Med. 2016;20:688–697. doi: 10.1111/jcmm.12769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cho HJ, Kim JT, Baek KE, Kim BY, Lee HG. Regulation of Rho GTPases by RhoGDIs in Human Cancers. Cells. 2019;8:1037. doi: 10.3390/cells8091037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leonard D, Hart MJ, Platko JV, Eva A, Henzel W, Evans T, Cerione RA. The identification and characterization of a GDP-dissociation inhibitor (GDI) for the CDC42Hs protein. J Biol Chem. 1992;267:22860–22868. doi: 10.1016/S0021-9258(18)50026-0. [DOI] [PubMed] [Google Scholar]
- 35.Song Q, Xu Y, Yang C, Chen Z, Jia C, Chen J, Zhang Y, Lai P, Fan X, Zhou X, et al. miR-483-5p promotes invasion and metastasis of lung adenocarcinoma by targeting RhoGDI1 and ALCAM. Cancer Res. 2014;74:3031–3042. doi: 10.1158/0008-5472.CAN-13-2193. [DOI] [PubMed] [Google Scholar]
- 36.Jiang WG, Watkins G, Lane J, Cunnick GH, Douglas-Jones A, Mokbel K, Mansel RE. Prognostic value of rho GTPases and rho guanine nucleotide dissociation inhibitors in human breast cancers. Clin Cancer Res. 2003;9:6432–6440. [PubMed] [Google Scholar]
- 37.Kotelevets L, Chastre E. Rac1 signaling: From intestinal homeostasis to colorectal cancer metastasis. Cancers (Basel) 2020;12:665. doi: 10.3390/cancers12030665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tan WJ, Tan QY, Wang T, Lian M, Zhang L, Cheng ZS. Calpain 1 regulates TGF-β1-induced epithelial-mesenchymal transition in human lung epithelial cells via PI3K/Akt signaling pathway. Am J Transl Res. 2017;9:1402–1409. [PMC free article] [PubMed] [Google Scholar]
- 39.Yang W, Li X, Qi S, Li X, Zhou K, Qing S, Zhang Y, Gao MQ. lncRNA H19 is involved in TGF-β1-induced epithelial to mesenchymal transition in bovine epithelial cells through PI3K/AKT Signaling Pathway. PeerJ. 2017;5:e3950. doi: 10.7717/peerj.3950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bokoch GM, Vlahos CJ, Wang Y, Knaus UG, Traynor-Kaplan AE. Rac GTPase interacts specifically with phosphatidylinositol 3-kinase. Biochem J. 1996;315:775–779. doi: 10.1042/bj3150775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Feng J, Wang X, Zhu W, Chen S, Feng C. MicroRNA-630 suppresses Epithelial-to-Mesenchymal transition by regulating FoxM1 in gastric cancer cells. Biochemistry Mosc. 2017;82:707–714. doi: 10.1134/S0006297917060074. [DOI] [PubMed] [Google Scholar]
- 42.Shen HJ, Sun YH, Zhang SJ, Jiang JX, Dong XW, Jia YL, Shen J, Guan Y, Zhang LH, Li FF, et al. Cigarette smoke-induced alveolar epithelial-mesenchymal transition is mediated by Rac1 activation. Biochim Biophys Acta. 2014;1840:1838–1849. doi: 10.1016/j.bbagen.2014.01.033. [DOI] [PubMed] [Google Scholar]
- 43.Qu H, Sun H, Wang X. Neogenin-1 promotes cell proliferation, motility, and adhesion by Up-regulation of Zinc Finger E-Box binding homeobox 1 via activating the Rac1/PI3K/AKT pathway in gastric cancer cells. Cell Physiol Biochem. 2018;48:1457–1467. doi: 10.1159/000492255. [DOI] [PubMed] [Google Scholar]
- 44.Xu SW, Liu S, Eastwood M, Sonnylal S, Denton CP, Abraham DJ, Leask A. Rac inhibition reverses the phenotype of fibrotic fibroblasts. PLoS One. 2009;4:e7438. doi: 10.1371/journal.pone.0007438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi-Wen X, Chen Y, Denton CP, Eastwood M, Renzoni EA, Bou-Gharios G, Pearson JD, Dashwood M, du Bois RM, Black CM, et al. Endothelin-1 promotes myofibroblast induction through the ETA receptor via a rac/phosphoinositide 3-kinase/Akt-dependent pathway and is essential for the enhanced contractile phenotype of fibrotic fibroblasts. Mol Biol Cell. 2004;15:2707–2719. doi: 10.1091/mbc.e03-12-0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during the present study are included in this published article.