Abstract
Rabies is a neglected tropical disease that causes mortality and high economic burden in many developing countries. Rabies is a vaccine-preventable disease if timely post-exposure prophylaxis is available after animal exposure. The control of rabies requires limiting the transmission of the virus in the animal reservoir, effective public health measures to control outbreaks and increasing accessibility and uptake of rabies post-exposure prophylaxis. Bhutan is a small Himalayan country where rabies is endemic. In this article, we describe the death of a 3-year-old female child due to probable rabies in a Bhutanese village located along the border with India. The child had a furious form of rabies with encephalitic syndrome developing 57 days after a category III dog bite on the chest. The child was managed at a district hospital with the available resources. This is the first rabies death in Bhutan in the last 5 years and the 18th since 2006. This case report focuses on the efforts required to increase the timely uptake of post-exposure prophylaxis in a free healthcare system in Bhutan.
Keywords: Dog diseases, rabies virus, vaccine-preventable diseases, zoonotic infection, One Health
Introduction
Rabies is a vaccine-preventable, zoonotic viral disease that occurs in more than 150 countries. 1 A review in 2015 estimated that rabies causes approximately 59,000 human deaths and 3.7 million disability-adjusted life years annually, the burden of which is mostly borne by countries in Asia and Africa.1,2 Canine rabies causes an estimated economic loss of USD 8.6 billion annually through premature death, direct costs of post-exposure prophylaxis (PEP), loss of income while seeking PEP, costs due to loss of livestock and costs for dog vaccination. 2 The burden of bites from suspect rabid animals disproportionately affects children under 15 years and people living in rural areas.1,3 Forty-five percent of global deaths due to rabies occur in the Indian sub-continent and 33% take place in India. 3
Bhutan is a country in the eastern Himalayas and shares borders with India and China. The border with China comprises mostly of high Himalayan mountains while the border with India comprises of porous Himalayan foothills that allows cross-border transmission of rabies.4,5 The import of rabies into Bhutan from India is documented in the re-emergence of rabies in cattle and dogs in Chhukha district in the south in 2008 and Trashigang district in the east in 2016.5,6 Phylogenic analysis of rabies virus circulating in Bhutanese districts bordering India revealed RABV isolates that were closely related to Arctic-like-1 rabies viruses circulating in India. 7
In Bhutan, rabies outbreaks are reported frequently in districts bordering India as well as in districts in the interior part of the country among migratory domestic animals. 8 Between 2006 and 2016, there were 17 human deaths attributed to rabies in the country. Rabies is a notifiable disease in the country and the government currently implements the multi-sectoral One Health Strategic Plan 2018–2023 in the control of rabies. 9 Bhutan has a government-funded healthcare system and victims of bites from suspect rabid animals are provided free of cost anti-rabies vaccine (Human Diploid Cell Vaccine, HDCV-Rabivac, intra-dermal using the Updated Thai Red Cross regimen) and rabies immunoglobulin. 8 However, despite awareness campaigns for timely uptake of PEP and reporting of suspicious animal behaviour in the community, we report a case of probable rabies death in a child in Samtse district, a district bordering India in November 2020.
Case
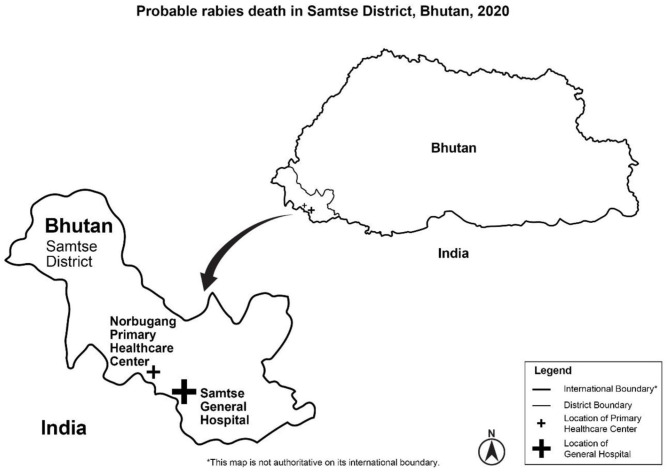
A 3-year-old female child, daughter of a farmer living in Norbugang gewog in Samtse district in Bhutan (see Figure 1), presented to the Samtse District Hospital on 08 November 2020 with 1-day history of intermittent fever, nausea, and being unable to eat or drink. She was admitted into the hospital’s isolation ward.
Figure 1.
Map of Bhutan showing the border town of Samtse district and Samtse General Hospital that recorded the ‘probable rabies death’ in a child in November 2020.
The parents reported that 57 days prior to the presentation, they witnessed the child being mauled by a dog while she was playing near the house. The dog had an aggressive behaviour and had bitten the child without it being provoked. This resulted in multiple puncture wounds and scratches with some bleeding. The mother had washed the child’s wound with soap and water but did not report to the nearby Primary Healthcare Centre for rabies PEP. Although the parents knew about rabies PEP injections, the parents were of the opinion that the wound was not severe enough to cause death from rabies. The dog was not from the locality. The child’s father killed the dog with a stone and a knife and disposed of its carcass in the nearby forest. Four weeks prior to this incident, three unknown dogs were seen in the community and had bitten one pet dog and a calf both of which developed rabid signs and died.
The child had normal growth and development and did not have any major illnesses or hospitalizations in the past. The child had received all scheduled vaccines but had not received any anti-rabies vaccine in the past.
On examination, the child had spontaneous eye-opening, able to recognize her parents and was following commands. She weighed 12.5 kg. She had GCS E4V5M6, temperature 101 °F, pulse rate 148/min, blood pressure 92/64 mmHg, respiratory rate 26/min, SpO2 98% on room air, and capillary blood sugar 146 mg/dL. She had three healed linear scars with five healed puncture wounds on the anterior chest and upper abdomen; three of the puncture wounds had evidence of bleeding with remains of healed scabs (Figure 2). There was no nuchal rigidity; her pupils were equal and reacting to light; there were no cranial nerve deficits; muscle power in the limbs was 4+ with normal deep tendon jerks and flexor plantar response. There were no abnormal findings of the cardiovascular, respiratory or abdominal examinations.
Figure 2.

Linear scratch marks and puncture wounds with evidence of bleeding and scab formation on the anterior chest and upper abdomen in the 3-year-old female child who died of probable rabies in November, 2020 in Samtse district, Bhutan.
On the first night of admission, she developed an aggressive behaviour and became irritable even to slight sound and light. She resisted all attempts to feed her. Investigation showed normal leukocyte count with neutrophilia (leukocyte 12,300/µL, neutrophils 85%, lymphocytes 10%, Hb 11.5 g/dL, platelets 471,000/µL). She had normal liver and renal functions. She was negative for malaria parasite rapid test, dengue, scrub typhus and had normal C-reactive protein levels. She was managed as a case of ‘probable rabies’ with a differential diagnosis of bacterial encephalitis and septic encephalopathy. She was given sedation with diazepam 0.1 mg/kg IV q8h, dexamethasone, empirical weight-based Ceftriaxone, Acyclovir, paracetamol, intravenous fluids and other supportive treatment facilities that were available at the hospital.
On the second day, she continued to have intermittent fever and had two episodes of generalized tonic-clonic seizures with jerky movements of all four limbs. She had worsening sensorium with hypersalivation and frequent episodes of irritability and aggression. On the third day of admission, she had the third episode of generalized tonic-clonic seizures and developed stridor with classic aerophobia, tachycardia (pulse rate 160/min) and tachypnoea (respiratory rate 70/min). Subsequently, she developed coma and despite adequate resuscitation, the child died on the fourth day of admission. The body was handled as per National Guideline for Management of Rabies 2014; the family members and six healthcare workers were provided PEP following this case. 8
To confirm the diagnosis and evaluate for other causes of encephalitic syndrome, we did not have neuroimaging facilities (currently are not available in district hospitals) or rapid antigen tests for rabies on saliva or the cerebrospinal fluid. At presentation, the child was too irritable to allow a lumbar puncture while later, the child was managed as a ‘probable rabies’ and lumbar puncture was not attempted.
Discussion
This is the first human death attributed to rabies in the last 5 years in Bhutan, and the 18th death since 2006. While previous deaths have only been recorded, this is the first case report of human death due to ‘probable rabies’ in Bhutan. This case presented with prodromal symptoms of fever and anorexia after an incubation period of 57 days. The historical description of dog bite and the extent of healed scar suggested a Category III exposure requiring PEP anti-rabies vaccine and rabies immunoglobulin based on the National Guideline for Management of Rabies 2014. 8 After admission to the hospital, the child developed encephalitic symptoms with fever, aggressive behaviour, photophobia and phonophobia, episodes of pharyngeal spasms, seizures, hydrophobia and autonomic instability with hypersalivation, tachycardia and tachypnoea.
The diagnosis of rabies was based on patient history, clinical course, epidemiologic evidence of rabies in a dog and a calf in the locality and the southern districts of Bhutan being highly endemic with rabies. The diagnosis of human rabies reported in literature are mostly based on medical history and clinical manifestations as facilities and expertise for virological confirmation is not easily accessible in many countries that have high burden of rabies. 10 The Bhutanese National Guideline for Management of Rabies 2014 defines cases of rabies based on clinic-epidemiological parameters and does not mandate the requirement of laboratory testing. In this victim, laboratory testing for RABV in serum or saliva could not be performed due to the non-availability of test reagents at the time while cerebrospinal fluid could not be drawn due to the irritable and aggressive stage of the child. The carcass of the dog that bit the child had been disposed of by the father and could not be tested. Laboratory confirmation of rabies through fluorescent antibody test and reverse-transcription polymerase chain reaction are available for animal brain samples at the National Centre for Animal Health in Thimphu. 8
In this particular case, the victim had not received PEP anti-rabies vaccine despite the fact that the nearest Primary Healthcare Centre was accessible within 1-h distance, and the parents were aware of rabies endemicity in the region. Community surveys in the past from Chhukha, Gelegphu and Trashigang districts in Bhutan have shown high level of awareness about rabies, infection through rabid dogs and handling or consumption of meat and milk products from rabid cattle.6,11,12 However, it is also reported that 8% of victims of dog bites did not seek PEP and some presented to hospitals for receiving PEP as late as 32 days after animal exposure with a compliance of only 40% to completion of the PEP course. 13 This reflects that while surveys have reported good knowledge about rabies, delayed presentation to avail PEP services and poor compliance to the PEP course are a serious concern that has led to the present case of rabies mortality.
Rabies is a priority zoonotic disease of concern for both human and animal health sectors in Bhutan and is a notifiable disease. 8 Rabies exposures in humans are investigated through a team of health and livestock officials as per standard operating procedures outlined in the National Guideline for Management of Rabies 2014. The Bhutan One Health Strategic Plan 2018–2023 aims to achieve zero human deaths due to dog-mediated rabies before 2030.9,14 To meet this target, concerted efforts are required in the control of dog population, mass vaccination of dogs, and prevention cross-border import of rabies. The Department of Livestock, Ministry of Agriculture and Forests implements Catch Neuter Vaccinate and Release programme to stall the increasing number of street dogs coupled with rabies vaccination. However, increase in dog population both in urban and rural areas and disease outbreaks in dogs continue to be reported in national media. Following this case of human mortality, mass dog and livestock vaccinations were conducted in Samtse district and Phuentsholing towns that are located along the border. 15 The department also implements registration and vaccination of pet animals.
The Department of Public Health, Ministry of Health implements public health awareness programmes on the prevention of human exposure to rabid animals. In Bhutan, the access and availability of PEP is not a major issue. As of 2021, rabies PEP was accessible through a network of 48 hospitals, 186 Primary Health Centres, 542 Outreach Clinics and three Thromdey (municipality) Health Centres covering 95% of the population within 3 h of transport from their homes. 16 However, even though PEP are given free of cost, delayed uptake and non-compliance to PEP regime are serious concerns.13,17 Apart of the mortality and economic losses related to loss of livestock, with the large volume of animal bites (mainly dog bites) occurring all over the country, it is estimated that the Bhutan spends Nu 68 million (USD 1 million) per year on PEP alone. 12
One major limitation in the management of this case was the lack of laboratory confirmation of the rabies virus infection. Currently, the testing facilities for human samples are not available in the country. For Bhutan to achieve the 2030 targets, it may be worthwhile to invest in improving clinical diagnostic capabilities, training of infectious disease specialists and virologists, designation of infectious disease hospitals and improving availability of proper terminal care to such patients.
Conclusions
Rabies is still a major public health concern in Bhutan. To meet its 2030 goal of zero deaths from rabies, increased efforts are required to strengthen the surveillance of epizootic spread of rabies in animal reservoirs, prevent spill over to human population, prevent the cross-border import of rabies and to encourage uptake of rabies PEP. There is also a need for physicians to adhere to diagnostic and treatment guidelines for human rabies and improve the rates of intra-vitam and post-mortem diagnosis.
Acknowledgments
We thank the general doctors, paediatrician and the staff of Samtse District Hospital for providing additional information on this case; the parents for providing consent to publish this case; and Thinley Jamtsho Tshering for generating the map.
Footnotes
Author contributions: Both authors were involved equally in the writing of the case and review of literature. The manuscript was drafted by T.D. Both authors were involved in the critical review of the manuscript and approve the final draft for publication.
Availability of data and materials: The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication: Written informed consent was obtained from the child’s father for publication of photo insert as per the consent process approved by the ethics board.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The ethics approval was obtained from the Research Ethics Board of Health, Ministry of Health, Bhutan. Administrative approval was obtained from the Policy and Planning Division, Ministry of Health and from the hospital administrator.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the parents of the child for anonymized information to be published in this article.
ORCID iDs: Karma Lhendup  https://orcid.org/0000-0002-0794-8094
https://orcid.org/0000-0002-0794-8094
Thinley Dorji  https://orcid.org/0000-0003-4932-8704
https://orcid.org/0000-0003-4932-8704
References
- 1. World Health Organization. Rabies, 2020, https://www.who.int/news-room/fact-sheets/detail/rabies (accessed 22 November 2020).
- 2. Hampson K, Coudeville L, Lembo T, et al. Estimating the global burden of endemic canine rabies. PLoS Negl Trop Dis 2015; 9(4): 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rahman SA, Isloor S. Rabies on the Indian subcontinent. Rev Sci Tech 2018; 37(2): 529–542. [DOI] [PubMed] [Google Scholar]
- 4. Tenzin T, Dhand NK, Ward MP. Patterns of rabies occurrence in Bhutan between 1996 and 2009. Zoon Publ Health 2011; 58(7): 463–471. [DOI] [PubMed] [Google Scholar]
- 5. Tenzin T, Sharma B, Dhand NK, et al. Reemergence of rabies in Chhukha district, Bhutan, 2008. Emerg Infect Dis 2010; 16(12): 1925–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tenzin T, Namgyal J, Letho S. Community-based survey during rabies outbreaks in Rangjung town, Trashigang, eastern Bhutan, 2016. BMC Infectious Diseases 2017; 17(1): 281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tenzin T, Wacharapluesadee S, Denduangboripant J, et al. Rabies virus strains circulating in Bhutan: implications for control. Epidemiol Infect 2011; 139(10): 1457–1462. [DOI] [PubMed] [Google Scholar]
- 8. Royal Government of Bhutan. National Guideline for Management of Rabies. 2nd ed. Thimphu, Bhutan: Royal Government of Bhutan, 2014. [Google Scholar]
- 9. Dorjee S, Jamtsho RK, Tenzin T, et al. Bhutan One Health Strategic Plan 2018–2023. 2nd ed. Thimphu, Bhutan, http://www.bohnet.bt/boh/wp-content/uploads/2020/11/Bhutan_One_Health_Strategy_Plan-1.pdf [Google Scholar]
- 10. Tian Z, Chen Y, Yan W. Clinical features of rabies patients with abnormal sexual behaviors as the presenting manifestations: a case report and literature review. BMC Infect Dis 2019; 19(1): 679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tenzin T, Dhand NK, Rai BD, et al. Community-based study on knowledge, attitudes and perception of rabies in Gelephu, south-central Bhutan. Int Health 2012; 4(3): 210–219. [DOI] [PubMed] [Google Scholar]
- 12. Rinchen S, Tenzin T, Hall D, et al. A community-based knowledge, attitude, and practice survey on rabies among cattle owners in selected areas of Bhutan. PLoS Negl Trop Dis 2019; 13(4): e0007305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Penjor K, Tenzin T, Jamtsho RK. Determinants of health seeking behavior of animal bite victims in rabies endemic South Bhutan: a community-based contact-tracing survey. BMC Publ Health 2019; 19(1): 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization. WHO expert consultation on rabies. Geneva: World Health Organization, 2018, https://apps.who.int/iris/bitstream/handle/10665/272364/9789241210218-eng.pdf?ua=1 [Google Scholar]
- 15. Department of Livestock, Ministry of Agriculture and Forests. Mass dog anti-rabies vaccination drive in Samtse and Chhukha, 2021, http://www.dol.gov.bt/?p=1980 (accessed 26 April 2021).
- 16. Ministry of Health. Annual Health Bulletin 2020. Thimphu, Bhutan: Ministry of Health, Royal Government of Bhutan, 2020. [Google Scholar]
- 17. Tenzin T, Dhand NK, Ward MP. Human rabies post exposure prophylaxis in Bhutan, 2005-2008: trends and risk factors. Vaccine 2011; 29(24): 4094–4101. [DOI] [PubMed] [Google Scholar]