Abstract
Background: In December 2019, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), or COVID-19, raised worldwide concern. Since then, the COVID-19 pandemic has negatively influenced health and wellness across the globe and caused nearly three million deaths. This study focuses on informal caregivers of people with dementia, a disease that affects about 50 million older adults worldwide and requires much caregiving support. Objective: Examine the current literature on the impact of COVID-19 on the health and well-being of informal caregivers for people with dementia. Method: This rapid review was conducted across five electronic databases for quantitative and qualitative articles published through March 15, 2021. Results: The 10 studies included in this review reported quantitative descriptive data from across the globe; however, no studies existed from the U.S. or East Asia countries. All of the studies examined the psychological rather than physical impact of COVID-19 and highlighted risk and protective factors in the areas of psychosocial (resilience, neuropsychiatric, and social isolation), sociodemographic (gender and education), and environmental (home confinement, living arrangement, and dementia stage). Conclusion: COVID-19 has had a considerable negative impact on the psychological well-being of informal caregivers of people with dementia, namely causing more depression and anxiety than pre-pandemic.
Keywords: Alzheimer’s/dementia, caregiving and management, mental health, active life/physical activity
Introduction
Dementia is a major cause of disability and dependency and affects about 50 million older adults worldwide, with about 10 million new cases each year. The most common form of dementia is Alzheimer’s disease, contributing to 60% to 70% of dementia cases (World Health Organization, 2021). Much care is necessary for people with dementia (PWD), and informal caregivers (ICs) often shoulder this responsibility. Such caregivers are sometimes called “second patients” and have high rates of psychological morbidity and social isolation due to their difficult caregiving role (Brodaty & Donkin, 2009). Increasingly, caregivers of PWD are older themselves, and they report more chronic disease, more disability, and worse health status than their non-caregiving counterparts (Centers for Disease Control and Prevention, 2020).
While the COVID-19 pandemic has negatively influenced health and wellness across the globe, ICs, in particular, are a group whose care burden levels have been significantly increased along with more social isolation and emotional stress (AARP, 2020; Czeisler et al., 2020). ICs of PWC are likely at greater risk for adverse effects on their health due to the pandemic as they have been found to have particularly more stress and suffer from more depression and physical problems than ICs of people without dementia prior to COVID-19 (Pinquart & Sörensen, 2003). To better understand the impact of COVID-19 on the health and well-being of ICs of PWD, we conducted a rapid systematic review.
A systematic meta-review of interventions targeting self-management of ICs of PWD found that such interventions can improve their stress levels, social support, and quality of life (Verkaik et al., 2015). Another systematic review specifically examined the delivery modality of Internet-based remote self-management education and peer support for informal caregivers of individuals with dementia and found it can help reduce informal caregivers’ stress levels and improve feelings of support (Klimova et al., 2019). Given the efficacy of interventions designed to improve the health and well-being of ICs of PWD, better understanding how the pandemic has impacted such caregivers can inform future interventions to address stress and health problems stemming from caregiving through the pandemic along with the everyday issues normally encountered.
Research Design
Search Strategy
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Liberati et al., 2009) and conducted database searches in PubMed (including MEDLINE), CINAHL, ProQuest, and PsychInfo for full-length, published articles. We placed no limit on the date of the article given the COVID-19 focus. All articles were collected by March 15, 2021. We restricted articles to peer-reviewed articles written in English. Articles that were only expert commentary were excluded. This study is registered at PROSPERO (CRD42021237102).
Our search was structured using the SPIDER’s approach for systematic searches (Sample, Phenomenon of Interest, Design, Evaluation, Research type) (Cooke et al., 2012), where: sample was caregivers or family caregiver of people with dementia or Alzheimer’s disease; phenomenon of interest was COVID-19, or novel coronavirus or SARS-CoV-2; design was every study design; evaluation was health, well-being, wellness; and research type was quantitative, qualitative, and mixed methods.
Types of Studies
We performed a rapid review of the literature with the aim of determining how COVID-19 has impacted the health and well-being of informal caregivers of PWD. The review focused on health-related issues that have arisen during the pandemic for caregivers of PWD. The impact of COVID-19 on PWD was outside the scope of this review, unless it related to their caregiver’s health and well-being.
Data Extraction
Two authors independently completed full-article coding of the 10 studies that met the inclusion criteria. For each study, we extracted the following: aim, health focus area, country, study design, results, and conclusion. We appraised each article’s quality using the Mixed Methods Appraisal Tool (MMAT) (Hong et al., 2018). We used the MMAT because our inclusion criteria allowed for a variety of study designs, and we wanted to appraise the quality of all of the articles.
Results
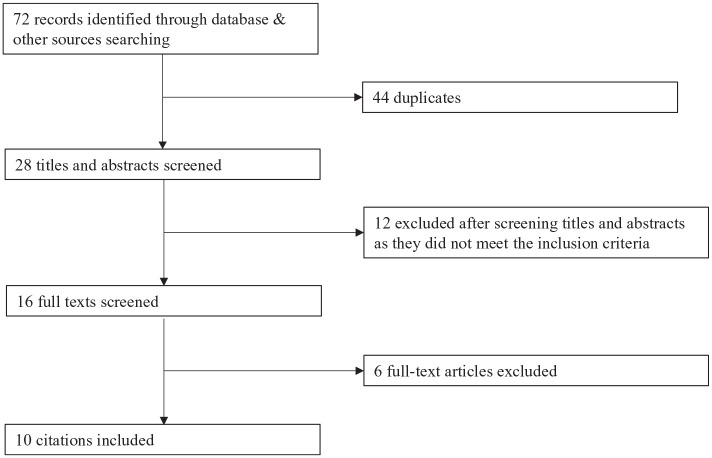
The initial search yielded 72 papers. After we removed 44 duplicates, at least two authors reviewed the titles and abstracts for each of these studies. Any discrepancies between the two authors were discussed by the three-person author team until they reached a consensus. After excluding 12 studies from the abstract reviews, at least two of the authors reviewed the remaining studies’ full text. The authors further excluded six studies due to four not being evaluative, one occurring before the COVID-19 pandemic, and one describing a survey design. We included the remaining 10 articles in the analysis. The screening process is detailed in Figure 1.
Figure 1.
Flow diagram article selection process.
Study Characteristics
In the cross-sectional studies, participant numbers ranged between 31 and 4,913. Of the 10 studies included, only two studies had an equal or higher percentage of male caregivers than female caregivers (Borges-Machado et al., 2020; Mazzi et al., 2020). Three of the studies described the family caregivers by their relationship to the care recipient (e.g., spouse, adult children) (Borges-Machado et al., 2020; Panerai et al., 2020; Rainero et al., 2021). All of the studies included articles that used online and telephone survey sampling methods.
Four of the studies were from Italy; the rest were from Greece (2), Portugal (1), India (1), Argentina (1), and England (1). No study was from the United States or East Asian countries. Several validated measures were used to assess anxiety, depression, stress, and burden. Table 1 provides an overview of the study characteristics. All of the studies fit into the Mixed-Methods Appraisal Tool’s quantitative descriptive study category and were deemed by two authors as having methodological rigor. There were no disagreements in quality assessment.
Table 1.
Study Characteristics.
| Reference | Country | Target population | Data collection mode | Outcome measure(s) | Key findings |
|---|---|---|---|---|---|
| Alexopoulos et al. (2021) | Greece | 67 ICs of individuals with mind and major neurocognitive disorder | Telephone questionnaire | Distress | Caregiver distress was influenced by memory deficits and neuropsychiatric symptoms. |
| Altieri and Santangelo (2021) | Italy | 84 ICs of PWD | Online survey | Anxiety, depression, resilience, and caregiver burden | The multivariate analysis of variance revealed an effect of time (before and during the lockdown) in the whole group on depression scores. Caregivers with high resilience showed a more significant increase of anxiety levels during lockdown than caregivers with low resilience. |
| Regression analysis revealed caregiver burden was associated negatively with resilience scores and positively with higher functional dependence. | |||||
| Borges-Machado et al. (2020) | Portugal | 36 ICs of individuals with neurocognitive disorder | Telephone interview | Caregiver burden | There was an increase in IC burden and a decline IC well-being. Pre- and post-confinement comparisons showed that care recipients significantly declined their independence in activities of daily living and increased Neuropsychiatric Inventory total score. |
| Cohen et al. (2020) | Argentina | 80 ICs of individuals with Alzheimer’s disease | Questionnaire | Stress | Overall, COVID-19 confinement increased IC stress independently of the dementia stage. However, ICs caring for severe cases had more stress compared to those caring for individuals with milder forms of Alzheimer’s disease. |
| ICs main concerns were for severe dementia cases, fear of absence of the paid caregiver during the epidemic, and, for those caring for mild cases of dementia, fear of spreading the disease while assisting patients with instrumental activities. | |||||
| Giebel et al. (2020) | England | 50 ICs of PWD | Telephone interview | Anxiety | ICs of PWD were greatly affected by the sudden removal of social support services and concerned about when services would re-open. ICs were worried about whether the person they cared for would still be able to re-join social support services. |
| Mazzi et al. (2020) | Italy | 239 ICs of PWD | Telephone interview | Anxiety and depression | Education was associated with significantly lower overall anxiety and depression scores while days of isolation and female gender were associated with the higher scores for ICs. A marked reduction of health services was observed in all care recipients. |
| Panerai et al. (2020) | Italy | 128 ICs of individuals with major neurocognitive disorder | Telephone interview | Distress | ICs are at an increased risk of burnout due to changes related to the COVID-19 pandemic. |
| Rainero et al. (2021) | Italy | 4,913 ICs of PWD | Telephone interview | Anxiety, depression, and distress | ICs reported a high increase in anxiety, depression, caregiver burden, and distress. |
| Tsapanou et al. (2020) | Greece | 204 ICs | Questionnaire | Psychological burden | ICs reported a great increase in psychological and physical burden during the COVID-19 pandemic. |
| Vaitheswaran et al. (2020) | India | 31 ICs of PWD | Telephone survey | Caregiver burden | ICs had multiple needs during the changes related to the COVID-19 pandemic. A multilayered approach to support is necessary. |
Psychological Impact on Family Caregivers
All of the studies included examined the psychological impact on family caregivers. Psychological symptoms were assessed using various validated measures, as shown in Table 1. The most common outcomes assessed were anxiety, burden, and depression. One study found more ICs of PWD experienced symptoms of depression related to the restrictions in place surrounding the COVID-19 pandemic rather than the increased amount of time spent caregiving (Altieri & Santangelo, 2021). The study authors concluded that this was likely due to the decrease in social support. The same study found that ICs of PWD with higher rates of resilience reported a significant increase in anxiety during the lockdown, suggesting that a pandemic can have a negative psychological effect even on mentally strong ICs. An additional study found that IC of PWD distress arose during the quarantine period, regardless of whether the care receiver’s neurocognitive symptoms changed (Alexopoulos et al., 2021). This study also found increased IC anxiety symptoms were unrelated to the severity of their care receiver’s neurocognitive disorder. Instead, the increase was attributed to the changes in routine due to COVID-19.
In a study performed in Argentina after four weeks of quarantine, rates of IC of PWD burden were higher, especially for ICs providing care to loved ones with advanced stages of dementia (Cohen et al., 2020). Another study that surveyed 4913 ICs of PWD found they reported a significant increase in anxiety, depression, distress, and irritability from the pandemic quarantine (Rainero et al., 2021). An additional study found three themes in the IC experience during COVID-19: loss of control, uncertainty, and adapting to the new normal (Giebel et al., 2020). This study determined a majority of ICs of PWD were concerned about whether their care receivers would still be able to access and enjoy social support service programs after not experiencing them during the pandemic’s closure period.
Risk and Protective Factors
The review identified both risk factors and protective factors against adverse health and well-being outcomes among ICs of PWD during COVID-19. The risk and protective factors can be categorized into three themes: psychosocial, sociodemographic, and environmental factors.
Psychosocial factors of resilience, neuropsychiatric factor, and social isolation
Altieri and Santangelo (2021) found a significant interaction between time and resilience in examining anxiety scores, revealing that ICs of PWD with high resilience showed a more significant increase in anxiety levels during lockdown than ICs of PWD with low resilience. However, Altieri and Santangelo (2021) also found that caregiver burden was associated negatively with resilience scores and positively with higher functional dependence.
IC’s distress during quarantine was influenced by memory deficits and neuropsychiatric symptoms (Alexopoulos et al., 2021). Caregiver’s symptoms of depression and anxiety also increased as the length of time in isolation increased (Mazzi et al., 2020). Panerai et al. (2020) found that home confinement due to the COVID-19 pandemic increased the risk of caregiver burnout by 10%. In one of the studies from Greece, it was found that 80% of caregivers reported an increase in their psychological burden (Tsapanou et al., 2020). Borges-Machado et al. (2020) found ICs experienced an increase in their levels of caregiver burden, while they reported a decrease in self-rated well-being. An additional study found that time was significantly associated with the severity of depression symptoms among ICs (Altieri & Santangelo, 2021).
Cohen et al. (2020) studied how the obligatory social isolation affected the stress levels and burden of care of ICs of PWD after the initial four weeks of quarantine. Their study found that social isolation due to COVID-19 confinement increased IC stress independently of the dementia stage of their care recipient. However, those ICs caring for severe cases had more stress compared to those caring for individuals in milder forms of dementia.
Sociodemographic factors of gender and education
In accordance with previous studies, women were found to be at higher risk for anxiety, depression, and stress than male ICs. Additionally, caregivers with more years spent obtaining an education experienced lower rates of anxiety and depression (Mazzi et al., 2020).
Environmental factors of home confinement, living arrangement, and stage of dementia
Borges-Machado et al. (2020) in Portugal analyzed home confinement impact on individuals with neurocognitive disorders (NCD) through the IC’s perspective and examined how it affected caregiving burden. Their study found that home confinement was associated with a significant decline in independence in activities of daily living (ADL) and increased Neuropsychiatric Inventory (NPI) total score among care recipients. Additionally, it was found that as length of home confinement increased, caregivers were spending more time providing care each day. Results also showed an increased caregiving burden and a decline in well-being among ICs of PWD. In Italy, Panerai et al. (2020) also investigated the levels of burden and distress of ICs of PWD following the confinement of the COVID-19 pandemic. They found that ICs of PWD were at an increased risk of burnout due to the pandemic. Mazzi et al. (2020) also found that days of isolation was associated with higher levels of anxiety and depression.
In a study from Italy, it was found that 75% of caregivers lived within the same home of the care-receiver during the COVID-19 pandemic (Altieri & Santangelo, 2021). Results from Cohen and colleague’s study found 60% of family members discontinued visiting their loved one during the pandemic, however as severity of dementia increased the discontinuation of visits decreased (Cohen et al., 2020). Mazzi et al.’s (2020) study from Italy found there was not a significant difference in anxiety levels among caregivers during the COVID-19 pandemic, when comparing those who lived in the home with the care-receiver to caregivers who did not live in the same household.
Cohen et al. (2020) found that there was no difference in the level of burden before coronavirus pandemic for ICs of persons in the three stages of dementia. However, the level of burden of the IC after four weeks in quarantine was higher, especially for advanced stages of dementia.
Caregiver Needs
A study conducted in Italy points out that online support groups could aid in reducing depressive symptoms for ICs of PWD experiencing social isolation during the pandemic (Altieri & Santangelo, 2021). Cohen et al. (2020) found that ICs of PWD were particularly concerned about paid caregivers being absent during the pandemic.
Discussion
This rapid review aimed to examine the impact of COVID-19 on the health and well-being of ICs of PWD. Our review revealed that there are relatively few studies on this topic worldwide, and none in the United States or East Asian countries. The lack of studies in these regions is surprising given that the country with the highest death rate from COVID-19 is the United States (BBC News, 2021) and the pandemic started in China (Mallapaty, 2020). Although the studies in this review differed in sample sizes and specific ICs of PWD health conditions of focus, they were overall quite similar using a cross-sectional design and focusing on mental health rather than physical health.
Most of the studies included in this review did not indicate the relationships between the ICs and care recipients. While two of the three studies that specified this relationship were predominantly concerned with adult children ICs, one study had higher number of spousal caregivers in their study sample. The lack of focus on certain types of ICs regarding their relationship to the care recipient is a concern as there is evidence of differences in burden between spouse and adult-child ICs of PWD (Pinquart & Sörensen, 2011). Spouse ICs of PWD differ from children ICs of PWD significantly regarding sociodemographic variables with the most prominent differences being spouses tend to be older and not working. Additionally, spouse ICs of PWD provide more support but report fewer care recipient behavior problems. However, spouse ICs of PWD report more depression symptoms, greater financial and physical burden, and lower levels of psychological well-being (Conde-Sala et al., 2010). Furthermore, studies on ICs of PWD conducted in different contexts and cultures may reveal different findings. For example, in some countries, like East Asian countries, adult children are more likely to be the ICs of their aging parents than in other Western countries (Chan, 2010) like the U.S. where the spouse is sometimes the primary IC (AARP & National Alliance for Caregiving, 2020).
Several risk and protective factors emerged in this review, many in keeping with what has been found in previous studies, including those related to gender, education, and social isolation. A new risk factor related to the COVID-19 pandemic is home confinement, which has led to more social isolation among the ICs and their care recipients. Consistent with previous studies of health outcomes of ICs of PWD, female ICs experienced higher level of depressive symptoms, stress, and anxiety compared to male ICs. In addition, our findings added to the evidence that higher level of educational attainment was a protective factor of the adverse health outcomes of ICs of PWD (Gottlieb & Rooney, 2004; Mazzi et al., 2020).
A surprising result was found regarding the impact of resilience on the mental health of the ICs of PWD. Previous studies have reported that resilience and social support play an important role in reducing physical and psychological burden in caregivers (Joling et al., 2016; Manzini et al., 2016; Ong et al., 2018; Petriwskyj et al., 2016). Altieri and Santangelo’s (2021) study found that ICs of PWD with high resilience showed a more significant increase in anxiety levels during lockdown than ICs of PWD with low resilience. This indicates that programs designed to help improve the health of ICs of PWD should target ICs with all levels of resiliency, especially during stressful times.
All of the studies included in this review used a cross-sectional research design. In investigating policies and programs that can be implemented to improve the health and well-being of ICs of PWD, we recommend that related studies include randomized controlled trials. Our research shows that the studies examining the impact of COVID-19 on the health and well-being of ICs of PWD indicate that the pandemic has increased stress and burden levels. The interventions designed to reach ICs of PWD must be evaluated with rigor so that those strategies that are effective can then be disseminated widely. Furthermore, studies examining the pandemics’ impact on ICs of PWD are still needed for many world regions.
Strengths and Limitations
Strengths of this review study include its rapid and comprehensive nature. The knowledge from identifying all studies worldwide over the last year that examined the impact of COVID-19 on the health and well-being of ICs of PWD is important to develop interventions that can improve the situation for ICs.
This study had a few limitations. First, our review was limited to articles from peer-reviewed journals and does not include any unpublished research. Second, we only reviewed studies written in English. Third, some major countries and regions such as the United States and East Asia are not represented because, to our knowledge, there were no studies published on this topic during our time frame. This lack of representation limits the generalizability of the findings to all areas around the globe.
Conclusion
This rapid review confirms that there has been a negative impact on the health and well-being of ICs of PWD during the COVID-19 pandemic. Published studies suggest that psychological conditions like depression and anxiety have been particularly prevalent among ICs. Going into the pandemic, social isolation was an increasing problem for ICs of PWD (Brodaty & Donkin, 2009; Vasileiou et al., 2017), and the pandemic has magnified that issue with quarantines, stay-at-home orders, and the canceling of social support services. In the future, it is important that policymakers and health promotion professionals design policies, programs, and other services that can withstand the impact of global crises such as a pandemic. Such efforts could help ICs of PWD maintain their health and well-being and may indirectly benefit their care recipients by having an IC in better health.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: M. Courtney Hughes  https://orcid.org/0000-0002-8699-5701
https://orcid.org/0000-0002-8699-5701
Yujun Liu  https://orcid.org/0000-0003-4115-9459
https://orcid.org/0000-0003-4115-9459
References
- AARP. (2020, November 18). New AARP research reveals family caregivers are struggling with stress, change, holiday planning amid pandemic. AARP. https://press.aarp.org/2020-11-18-New-AARP-Research-Reveals-Family-Caregivers-Are-Struggling-with-Stress-Change-Holiday-Planning-Amid-Pandemic [Google Scholar]
- AARP, & National Alliance for Caregiving. (2020). 2020 report: Caregiving in the U.S. AARP. https://www.aarp.org/content/dam/aarp/ppi/2020/05/full-report-caregiving-in-the-united-states [Google Scholar]
- Alexopoulos P., Soldatos R., Kontogianni E., Frouda M., Aligianni S. I., Skondra M., Passa M., Konstantopoulou G., Stamouli E., Katirtzoglou E., Politis A. (2021). COVID -19 crisis effects on caregiver distress in neurocognitive disorder. Journal of Alzheimer’s Disease, 79(1), 459–466. 10.3233/JAD-200991 [DOI] [PubMed] [Google Scholar]
- Altieri M., Santangelo G. (2021). The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. The American Journal of Geriatric Psychiatry 29(1), 27–34. 10.1016/j.jagp.2020.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC News. (2021, April 6). Covid map: Coronavirus cases, deaths, vaccinations by country. https://www.bbc.com/news/world-51235105
- Borges-Machado F., Barros D., Ribeiro O., Carvalho J. (2020). The effects of COVID-19 home confinement in dementia care: Physical and cognitive decline, severe neuropsychiatric symptoms and increased caregiver burden. American Journal of Alzheimer’s Disease and Other Dementias, 35(1), 1–9. 10.1177/1533317520976720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodaty H., Donkin M. (2009). Family caregivers of people with dementia. Dialogues in Clinical Neuroscience, 11(2), 217. 10.31887/DNCS.2009.11.2/hbrodaty [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020, November 17). Baby boomer caregivers report poor health. CDC. https://www.cdc.gov/aging/publications/features/caregivers-baby-boomers-report-poor-health/index.html [Google Scholar]
- Chan S. W. C. (2010). Family caregiving in dementia: The Asian perspective of a global problem. Dementia and Geriatric Cognitive Disorders, 30(6), 469–478. 10.1159/000322086 [DOI] [PubMed] [Google Scholar]
- Cohen G., Russo M. J., Campos J. A., Allegri R. F. (2020). Living with dementia: Increased level of caregiver staff in time of COVID-19. International Psychogeriatrics, 32(11), 1377–1381. 10.1017/S1041610220001593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conde-Sala J. L., Garre-Olmo J., Turró-Garriga O., Vilalta-Franch J., López-Pousa S. (2010). Differential features of burden between spouse and adult-child caregivers of patients with Alzheimer’s disease: An exploratory comparative design. International Journal of Nursing Studies, 47(10), 1262–1273. 10.1016/j.ijnurstu.2010.03.001 [DOI] [PubMed] [Google Scholar]
- Cooke A., Smith D., Booth A. (2012). Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qualitative Health Research, 22(10), 1435–1443. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- Czeisler M. É., Lane R. I., Petrosky E., Wiley J. F., Christensen A., Njai R., Weaver M. D., Robbins R., Facer-Childs E. R., Barger L. K., Czeisler C. A., Howard M. E., Rajaratnam S. M. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giebel C., Cannon J., Hanna K., Butchard S., Eley R., Gaughan A., Komuravelli A., Shenton J., Callahan S., Tetlow H., Limbert S., Whittington R., Rogers C., Rajagopal M., Ward K., Shaw L., Corcoran R., Bennett K., Gabbay M. (2020). Impact of COVID-19 related social support service closures on people with dementia and unpaid carers: A qualitative study. Journal of Aging and Mental Health, 1–8. 10.1080/13607863.2020.1822292 [DOI] [PubMed]
- Gottlieb B. H., Rooney J. A. (2004). Coping effectiveness: Determinants and relevance to the mental health and affect of family caregivers of persons with dementia. Aging & Mental Health, 8(4), 364–373. 10.1080/13607860410001709719 [DOI] [PubMed] [Google Scholar]
- Hong Q. N., Pluye P., Fabregues S., Bartlett G., Boardman F., Cargo M., Dagenais P., Gannon M., Griffiths F., Nicolua B., O’Cathain A., Rousseau M., Verdel I. (2018). Mixed methods appraisal tool (MMAT) version 2018. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/page/24607821/FrontPage [DOI] [PubMed]
- Joling K. J., Windle G., Dröes R. M., Meiland F., van Hout H. P., Vroomen J. M., van de Ven P. M., Moniz-Cook E., Woods B. (2016). Factors of resilience in informal caregivers of people with dementia from integrative international data analysis. Dementia and Geriatric Cognitive Disorders, 42(3–4), 198–214. 10.1159/000449131 [DOI] [PubMed] [Google Scholar]
- Klimova B., Valis M., Kuca K., Masopust J. (2019). E-learning as valuable caregivers’ support for people with dementia–A systematic review. BMC Health Services Research, 19(1), 781. 10.1186/s12913-019-4641-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P., Clarke M., Devereaux P., Kleijnen J., Moher D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Journal of Clinical Epidemiology, 62(10), e1–e34. 10.1136/bmj.b2700 [DOI] [PubMed] [Google Scholar]
- Mallapaty S. (2020). Where did COVID come from? WHO investigation begins but faces challenges. Nature, 587(7834), 341–342. [DOI] [PubMed] [Google Scholar]
- Manzini C. S. S., Brigola A. G., Pavarini S. C. I., Vale F. A. C. (2016). Factors associated with the resilience of family caregivers of persons with dementia: A systematic review. Brazilian Journal of Geriatrics and Gerontology, 19(4), 703–714. 10.1590/1809-98232016019.150117 [DOI] [Google Scholar]
- Mazzi M. C., Iavarone A., Musella C., De Luca M., de Vita D., Branciforte S., Coppola A., Scarpa R., Raimondo S., Sorrentino S., Lualdi F., Postiglione A. (2020). Time of isolation, education and gender influence the psychological outcome during COVID-19 lockdown in caregivers of patients with dementia. European Geriatric Medicine, 11, 1095–1098. 10.1007/s41999-020-00413-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong H. L., Vaingankar J. A., Abdin E., Sambasivam R., Fauziana R., Tan M. E., Chong S. A., Goveas R. R., Chiam P. C., Subramaniam M. (2018). Resilience and burden in caregivers of older adults: Moderating and mediating effects of perceived social support. BMC Psychiatry, 18(1), 27. 10.1186/s12888-018-1616-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panerai S., Prestianni G., Musso S., Muratore S., Tasca D., Catania V., Gelardi D., Ferri R. (2020). The impact of COVID-19 confinement on the neurobehavioral manifestations of people with major neurocognitive disorder and on the level of burden of their caregivers. Journal of Life Span & Disability, 23(2), 303–320. [Google Scholar]
- Petriwskyj A., Parker D., O’Dwyer S., Moyle W., Nucifora N. (2016). Interventions to build resilience in family caregivers of people living with dementia: A comprehensive systematic review. JBI Evidence Synthesis, 14(6), 238–273. 10.11124/JBISRIR-2016-002555 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2003). Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18(2), 250. 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- Pinquart M., Sörensen S. (2011). Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging, 26(1), 1–14. 10.1037/a0021863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainero I., Bruni A. C., Marra C., Cagnin A., Bonanni L., Cupidi C., Laganà V., Rubino E., Vacca A., Di Lorenzo R., Provero P., Isella V., Vanacore N., Agosta F., Appollonio I., Caffarra P., Bussè C., Sambati R., Quaranta D., Guglielmi V., . . . SINdem COVID -19 Study Group. (2021). The impact of COVID-19 quarantine on patients with dementia and family caregivers: A nation-wide survey. Frontiers in Aging Neuroscience, 12, 1–13. 10.3389/fnagi.2020.625781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsapanou A., Papatriantafyllou J. D., Yiannopoulou K., Sali D., Kalligerou F., Ntanasi E., Zoi P., Margioti E., Kamtsadeli V., Hatzopoulou M., Koustimpi M., Zagka A., Papageorgiou S. G., Sakka P. (2020). The impact of COVID-19 pandemic on people with mild cognitive impairment/dementia and on their caregivers. International Journal of Geriatric Psychiatry, 36(4), 583–587. 10.1002/gps.5457 [DOI] [PubMed] [Google Scholar]
- Vaitheswaran S., Lakshminarayanan M., Ramanujam V., Sargunan S., Venkatesan M. (2020). Experiences and needs of caregivers of persons with dementia in India during the COVID-19 pandemic—A qualitative study. The American Journal of Geriatric Psychiatry, 28(11), 1185–1194. 10.1016/j.jagp.2020.06.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasileiou K., Barnett J., Barreto M., Vines J., Atkinson M., Lawson S., Wilson M. (2017). Experiences of loneliness associated with being an informal caregiver: A qualitative investigation. Frontiers in Psychology, 8, 585. 10.3389/fpsyg.2017.00585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkaik R., Mistiaen P., van Meijel B., Francke A. L. (2015). The effectiveness of interventions in supporting self-management of informal caregivers of people with dementia; a systematic meta review. BMC Geriatrics, 15(1), 1–10. 10.1186/s12877-015-0145-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021, September 21). Dementia: Key facts. WHO. https://www.who.int/news-room/fact-sheets/detail/dementia [Google Scholar]