Abstract
Background
Many countries have implemented various levels of lockdown to mitigate the spread of the global SARS‐CoV‐2 pandemic. In the United Kingdom, the national lockdown restrictions were implemented between 26 March 2020 and 4 July 2020. These restrictions required all restaurants to close except for takeaway and delivery services. Moreover, individuals were instructed to largely stay in their homes, unless they were identified as essential workers, and to only leave home once per day for exercise. These restrictions might have an impact on energy intake and expenditure, thereby affecting their body weight.
Aims
The aim of this study was to investigate the impact of the movement restrictions in the United Kingdom on food outlet usage and body mass index (BMI).
Materials and Methods
Food outlet usage surveys were filled out for 7 consecutive days before and during the lockdown. Changes in BMI and food outlet usage before and during the lockdown were measured. A total of 206 participants were included in this study.
Results
The mean overall BMI prior to lockdown was 25.8 ± 5.2 kg·m2, and during the lockdown, it was 25.9 ± 5.3 kg·m2 (t= 0.19, p= 0.85). Restaurant usage fell to zero as all establishments were closed. There was a corresponding increase in the use of delivery services to 1.18 ± 0.13 times per week, compared to 0.50 ± 0.05 prior to lockdown (t= 4.44, p< 0.0001). No significant difference in the number of takeaway meals ordered was observed (0.67 ± 0.06 before the lockdown and 0.74 ± 0.12 times per week during the lockdown; t= 0.52, p = 0.60). There was no significant relationship between change in use of fast‐food restaurants and full‐service restaurants and the change in BMI, either alone or in combination (β = −0.012, p = 0.62, R 2 = 0.11%).
Discussion
Despite the large changes in behavior, there was no overall adverse effect of the lockdown with respect to obesity levels.
Conclusion
Lockdown in the United Kingdom modified restaurant use but had no effect on obesity levels.
Keywords: COVID‐19, lockdown, obesity, physical activity, takeaway and delivery intake
1. INTRODUCTION
The global SARS‐CoV‐2 pandemic has led many countries to impose various levels of restriction on movement and association to stem the spread of the virus. In the United Kingdom, these restrictions (generally called “lockdown”) were implemented nationally on 26 March 2020 and lasted with only minor modifications, and small differences between the component countries of the United Kingdom, until 4 July 2020 (101 days). Subsequently, a more regional approach has been taken. The lockdown restrictions required all but essential workers to stay inside their homes for 23/24 h per day. Concerns have been raised about the impact of such confinement on a number of other health‐related issues, such as reduced physical activity, 1 elevated propensity to obesity, 2 increased domestic violence, 3 and mental health. 1 Moreover, the “lockdown” has impacted many other aspects of life such as employment 4 and schooling. 5 These off‐target effects have led some to suggest that the lockdown cure might be worse than the COVID‐19 illness. 6
With respect to the impact on obesity, there is relatively little direct evidence on the impacts of lockdown. On one hand, evidence from mobile phone use shows that physical activity has declined. 7 However, the complete closure of restaurants and cafes has meant that there has been no opportunity to take meals from such locations. As eating fast‐food and full‐service meals has been implicated as a potential driver of obesity, 8 , 9 then restricting access to such foods may have had a beneficial impact. However, although restaurants have closed for dining customers, food delivery and takeaway services have continued unabated during the lockdown period. Hence, it is possible that people in lockdown have simply replaced dining out, by dining in. Indeed, consumption of food prepared out of the home may have increased relative to that ingested prior to the lockdown, thereby exacerbating the reduced physical activity levels, and leading to elevated levels of overweight and obesity. Although some studies have been published on the dietary habits during lockdown restrictions, 2 only few studies have compared behavior during and prior to the imposition of lockdown. 10 , 11 The impact of the lockdown on obesity prevalence are particularly significant as it has emerged that obesity is a significant risk factor for mortality due to the SARS‐CoV‐2 virus. 12 Hence, reducing the spread of the virus by using lockdown measures might have the unintended consequence that it enlarges the pool of the population with underlying conditions that exacerbate the virus impact.
A survey of the use of restaurants and delivery/takeaway services was conducted prior to the lockdown (06 January 2019 to 12 December 2019; ethical review approval: CERB/2018/08/1601). This study aimed to investigate the association between the frequency of usage of different types of food outlets and body weight among UK adults. 13 Given the availability of this baseline pre‐restriction data, the aim of this study was to investigate the impact of the UK lockdown restrictions on individual changes in food outlet usage and BMI.
2. METHODS
Volunteers were invited to participate in this cross‐sectional study through social media, by encountering individuals in the main street of Aberdeen city and inviting them to participate, and by distributing flyers online. Once consent was obtained, they were sent a link to the initial sociodemographic survey where they recorded their weight, height, age, sex, ethnicity, postcode district, employment status, workplace, number of household members, dietary habits, and level of physical activity. Only males and females who were 18 years and older were included. This survey included an electronic consent statement prior to commencing the questions. There was a further statement of agreed participation before each daily food outlet use questionnaire. Once they submitted their responses, they were sent a link to the Food Outlet Usage survey. In this survey, the participants were asked whether they used any of food outlets or services over the previous 24 h with five options of fast‐food restaurant (FFR), full‐service restaurant (FSR), delivery (premises where customers can order meals online or using the telephone, which are delivered to their location via a food delivery company or personnel from the same restaurant), 14 takeaways, or none. To stimulate participants' adherence, an autoreminder text message with a link to the survey was automatically generated for 7 consecutive days. These messages were sent via the Text Magic encrypted website (www.textmagic.com). For full methodological details, see Albalawi et al. (2020). 13
This survey was repeated with the same individuals during the middle of the lockdown period (22 April 2020–3 June 2020), and we report here the changes in food consumption patterns and self‐reported BMI from before to during the lockdown period.
2.1. Statistical analysis
Paired sample t‐test was used to compare the self‐reported BMI, and the use of takeaways and delivery before and during the lockdown. Least squares linear regression was used to examine the change in BMI against age and change in food outlet usage.
3. RESULTS
In total, 681 individuals took part in this survey prior to the lockdown (390 females and 291 males). 13 Ethical permission was also obtained to approach all these previous participants to ask if they would repeat the survey during the lockdown (CERB/2020/4/1941). In total, 206 individuals consented to repeat the survey (30%). Hence, 108 females and 98 males completed both week‐long surveys prior to and during the lockdown. Participation was not biased by sex relative to the initial survey (χ2 = 1.5, p = 0.22). Because all restaurants and cafes were closed to on‐site diners during the lockdown, use of these outlets fell to zero from prelockdown levels of 1.15 ± 0.07 (SEM) and 0.93 ± 0.07 per week. There was a corresponding increase in the use of delivery services (Figure 1A), which increased to 1.18 ± 0.13 times per week, compared to 0.50 ± 0.05 times per week prior to lockdown (t = 4.44, p < 0.0001). However, there was no significant difference in the number of takeaway meals ordered (0.67 ± 0.06 before the lockdown and 0.74 ± 0.12 times per week during the lockdown; t = 0.52, p = 0.60) (Figure 1B).
FIGURE 1.
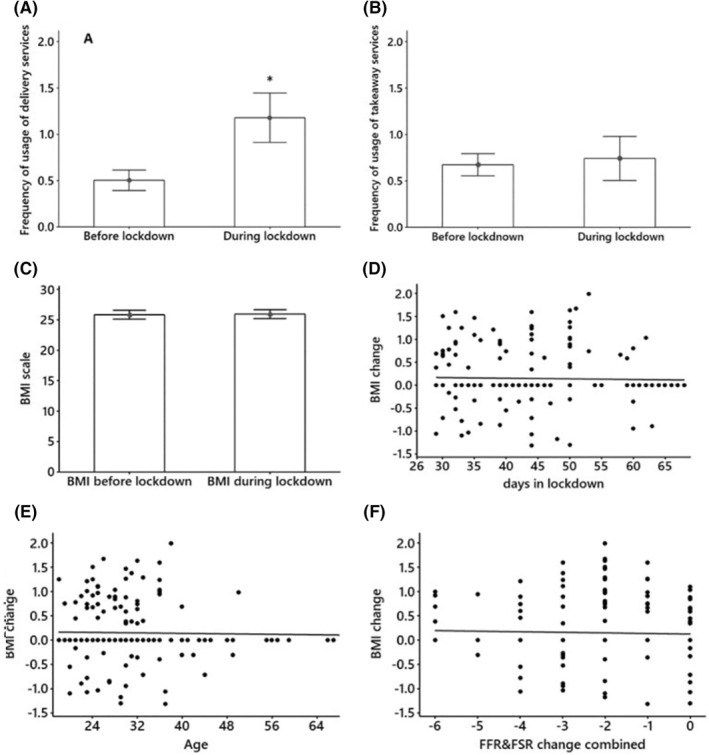
Frequency of usage of (A) food delivery services and (B) takeaway services, before and during the lockdown in the United Kingdom. Only the use of delivery services was significantly increased. (C) BMI before and after the lockdown. (D) Change in BMI before and during the lockdown regressed against the number of days participants had been in lockdown when the survey was conducted. (E) Change in BMI before and during the lockdown regressed against age. (F) Change in BMI before and during the lockdown regressed against change in the use of FFR and FSR. Error bars in all panels = SEM. *p < 0.0001. 583 × 825 mm (72 × 72 DPI). BMI, body mass index; FFR, fast‐food restaurant; FSR, full‐service restaurant
Participants were also asked about whether they were concerned of ordering takeaway or delivery meals during the lockdown. Of the 206 participants, 38 (18.4%) were very concerned, 75 (36.4%) were slightly concerned, and 93 (45%) participants were not concerned at all.
Before the lockdown, the mean overall BMI was 25.8 ± 5.2 (SD) kg·m2, and during the lockdown, it was 25.9 ± 5.3 kg·m2 (paired t‐test: t = 0.19, p = 0.85) (Figure 1C). The change in BMI before and during the lockdown was not significantly associated with the period in lockdown (β = −0.001, p < 0.70, R 2 = 0.07%) (Figure 1D) or age (β = −0.001, p = 0.71, R 2 = 0.07%) (Figure 1E).
Individuals varied in their use of FFR and FSR prior to the lockdown. However, there was no significant relationship between change in use of FFR and FSR and the change in BMI, either alone or in combination (β = −0.012, p = 0.62, R 2 = 0.11%) (Figure 1F).
4. DISCUSSION
Overall, the present data showed that during the UK lockdown, there was a reduction in the consumption of meals prepared out of the home, a modest increase in the use of delivery services, but no change in self‐reported BMI. The reported increase in delivery use was insufficient to offset the reduction in restaurant and fast‐food dining. The incomplete compensation of dining out by delivery and takeaway use may have been because more than a third of survey participants expressed concern and 18.4% expressed extreme concern about potential SARS‐CoV‐2 infection from delivered or takeaway food and its packaging. This seems a valid concern as it was subsequently shown that the virus can survive on various surfaces for up to 28 days 15 However, thus far, there is no evidence of the virus being transferred from food packages. 16 , 17 In light of it, the lockdown provided an unexpected opportunity to test the hypothesis that fast‐food and restaurant consumption is a significant driver of the obesity epidemic, 18 as the lockdown was in effect an intervention which prevents such activities. Several studies have suggested that consumption of out of home foods may be a significant driver of obesity. 8 , 19 For example, a study in Cambridgeshire suggested that people living in the proximity of takeaway food outlets consumed more food than those living further away, 8 while another study suggested that consumption of food in restaurants and cafes may increase daily energy intake by 3.2%–4.4%. 20 The absence of any effect of the lockdown on BMI might then be taken as support for other studies, which have suggested that fast‐food and restaurant consumption are not a significant driver of excess calorie intake. For example, in the study that led to the baseline data, it was shown that the individual usage of fast‐food and full‐service establishments was not associated with differences in BMI. 13 In addition, the level of obesity prevalence at the county level in the United States, 21 and at the postcode level in the United Kingdom, 22 is largely unaffected by the density of FFR and FSR. This interpretation is reinforced by the fact that those individuals who used FFR and FSR most frequently prior to their accessibility being denied in lockdown, were not the ones who lost most weight.
However, caution should be applied in drawing such conclusions because the lockdown is not a clean intervention in the sense that it certainly reduced the out of home consumption of foods in restaurants and cafes, but it also precipitated a range of other confounding effects. Probably most significant of which is the documented reduction in physical activity levels. 7
Reduced physical activity leading to reduced energy expenditure may then have offset the anticipated reduction in consumption of food prepared out of the home. However, the association between physical activity levels and energy expenditure is complex. For example, despite evidence that work‐time physical activity has progressively declined, 23 levels of energy expenditure over the same period show no reduction. 24 Therefore, reductions in physical activity during lockdown would not inevitably mean levels of energy expenditure were reduced. An additional factor in the absence of any impact of the reduced restaurant and cafe usage on BMI may have been the relatively short duration of the “intervention.” The range of durations people had been in “lockdown” when they completed the survey was only 4–8 weeks (Figure 1D). However, the fact there was no relationship between lockdown duration and BMI change supports the idea that food intake from these sources was not an important factor driving BMI increases.
This study has several limitations. Reliance on self‐reported BMI to assess obesity status is an obvious potential limitation. However, previous work has shown that while the Scottish population, in common with most other populations, tend to underestimate their body weights in self‐reported data, when compared to direct measurement, in Scotland, they also tend to underestimate their heights. 25 Consequently, the estimated self‐reported BMI is not biased. 25 This latter work was, however, conducted 20 years ago in a different city to the current survey, and whether this still applies nowadays and in a different location is unknown. A second potential problem is that only 30% of the original participants in the previous study consented to take part in the repeat survey during lockdown. In the previous survey, the overall BMI of individuals who took part was 26.1, 13 while in those participating in the follow‐up, it was 25.9, suggesting no strong overall participation bias with respect to BMI. As detailed in the results, the participation relative to the original survey was also not biased by sex.
5. CONCLUSION
Although this is a small study, the patterns observed, particularly in food outlet usage, do not suggest any major adverse effects of the lockdown with respect to body weight. If correct, the public health relevance is that policy makers may need to worry less about the impact of lockdown measures on obesity status than the popular media are suggesting.
CONFLICT OF INTEREST
None declared.
ACKNOWLEDGMENTS
The authors thank Vasileios Kyparissis and Florina Birkert for their work with us in distributing and collecting the surveys. Ahmad Albalawi was supported by a studentship from the University of Tabuk, Saudi Arabia (KSA) project code CF10434‐63. John R, Speakman was supported by a Wolfson merit award from the Royal Society and a Presidents International Fellowship Initiative award from the Chinese Academy of Sciences.
References
- 1. Lippi G, Henry BM, Bovo C, Sanchis‐Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID‐19). Diagnosis. 2020;7(2):85‐90. [DOI] [PubMed] [Google Scholar]
- 2. Sidor A, Rzymski P. Dietary choices and habits during COVID‐19 lockdown: experience from Poland. Nutrients. 2020;12(6):1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vieira PR, Garcia LP, Maciel ELN. The increase in domestic violence during the social isolation: what does it reveals? Rev Bras Epidemiol. 2020;23. e200033 [DOI] [PubMed] [Google Scholar]
- 4. Ishii T. Measures against the spread of COVID‐19: simultaneous international action and lockdown postponement (posted online April 10, 2020). Available at SSRN 3572862. https://ssrn.com/abstract=3572862 [Google Scholar]
- 5. Nicola M, Alsafi Z, Sohrabi C, et al. The socio‐economic implications of the coronavirus pandemic (COVID‐19): a review. Int J Surg. 2020;78:185‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Katz DL. Is our fight against coronavirus worse than the disease? New York Times. 2020. www.nytimes.com/2020/03/20/opinion/coronavirus-pandemic-social-distancing.html [Google Scholar]
- 7. Jakobsson J, Malm C, Furberg M, Ekelund U, Svensson M. Physical activity during the coronavirus (COVID‐19) pandemic: prevention of a decline in metabolic and immunological functions. Front Sports Act Living. 2020;2:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burgoine T, Forouhi NG, Griffin SJ, Wareham NJ, Monsivais P. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ. 2014;348:g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mason KE, Pearce N, Cummins S. Associations between fast food and physical activity environments and adiposity in mid‐life: cross‐sectional, observational evidence from UK biobank. Lancet Public Health. 2018;3(1):e24‐e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zachary Z, Brianna F, Brianna L, et al. Self‐quarantine and weight gain related risk factors during the COVID‐19 pandemic. Obes Res Clin Pract. 2020;14(3):210–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Robinson E, Gillespie SM, Jones A. Weight‐related lifestyle behaviors and the COVID‐19 crisis: an online survey study of UK adults during social lockdown. Obesity Science & Practice. 735–740. [DOI] [PMC free article] [PubMed]
- 12. Cai Q, Chen F, Wang T, et al. Obesity and COVID‐19 severity in a designated hospital in Shenzhen, China. Diabetes Care. 2020;43(7):1392‐1398. [DOI] [PubMed] [Google Scholar]
- 13. Albalawi A, Hambly C, Speakman JR. Frequency of restaurant, delivery and takeaway usage is not related to BMI among adults in Scotland. Nutrients. 2020;12(9):2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NAICS . North American Industry Classification System; 2017. Updated. https://www.census.gov/eos/www/naics/. Accessed November 3, 2019. [Google Scholar]
- 15. Riddell S, Goldie S, Hill A, Eagles D, Drew TW. The effect of temperature on persistence of SARS‐CoV‐2 on common surfaces. Virology J. 2020;17(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Olaimat AN, Shahbaz HM, Fatima N, Munir S, Holley RA. Food safety during and after the era of COVID‐19 pandemic. Front Microbiol. 2020;11:1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rizou M, Galanakis IM, Aldawoud TM, Galanakis CM. Safety of foods, food supply chain and environment within the COVID‐19 pandemic. Trends Food Sci Technol. 2020;102:293‐299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Feng J, Glass TA, Curriero FC, Stewart WF, Schwartz BS. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16(2):175‐190. [DOI] [PubMed] [Google Scholar]
- 19. Robinson E, Jones A, Whitelock V, Mead BR, Haynes A. (Over) eating out at major UK restaurant chains: observational study of energy content of main meals. BMJ. 2018;363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Goffe L, Rushton S, White M, Adamson A, Adams J. Relationship between mean daily energy intake and frequency of consumption of out‐of‐home meals in the UK national diet and nutrition survey. Int J Behav Nutr Phys Activity. 2017;14(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mazidi M, Speakman JR. Higher densities of fast‐food and full‐service restaurants are not associated with obesity prevalence. Am J Clin Nutr. 2017;106(2):603‐613. [DOI] [PubMed] [Google Scholar]
- 22. Albalawi A, Hambly C, Speakman J. Associations of food outlet densities with obesity measures identify fish and chip shops as a uniquely important problem. Nutrients. 2020;12(4):890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee D, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure‐time running reduces all‐cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64(5):472‐481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Westerterp KR, Speakman JR. Physical activity energy expenditure has not declined since the 1980s and matches energy expenditures of wild mammals. Int J Obes. 2008;32(8):1256. [DOI] [PubMed] [Google Scholar]
- 25. Bolton‐Smith C, Woodward M, Tunstall‐Pedoe H, Morrison C. Accuracy of the estimated prevalence of obesity from self‐reported height and weight in an adult Scottish population. J Epidemiol Community Health. 2000;54(2):143‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]


