Abstract
Objectives
To describe the trend in the impact of lower urinary tract symptoms attributed to benign prostatic hyperplasia (LUTS/BPH) on a global scale using the Global Burden of Disease (GBD) database.
Materials and Methods
Using the GBD database, worldwide data aggregated from registries and health systems from 1990 to 2017 were filtered for LUTS/BPH diagnoses. Calculation of years lived with disease (YLD) were compared with other urological diseases. YLD were calculated by a standardized method using assigned disability weights. The GBD-defined sociodemographic index (SDI) was used to assess impact of LUTS/BPH by global SDI quintile.
Results
Global Burden of Disease data over the 1990–2017 study period were summarized and global numbers and trends noted with other urological diseases for comparison. A total of 2 427 334 YLD were attributed to BPH in 2017 alone, almost three times more than those attributed to the next highest urological disease, prostate cancer (843 227 YLD). When stratified by SDI quintile, a much lower impact of BPH was found in the bottom three quintiles, despite this subset representing 66.9% of the 2017 world population.
Conclusions
Lower urinary tract symptoms attributed to benign prostatic hyperplasia exert a rapidly rising human burden far exceeding other urological diseases. As the population ages and men in a lower SDI enjoy increased life expectancy and decreased competing mortalities, a continually accelerating wave of LUTS/BPH can be forecast. These epidemiological trends have serious implications for the future allocation of resources and the global urological workforce.
Keywords: benign prostatic hyperplasia, lower urinary tract symptoms, global health, prostate, quality of life, #UroBPH
Introduction
Benign prostatic hyperplasia is the most common aetiological factor for LUTS in men [1]. The prevalence of histological BPH at autopsy increases substantially with age, reaching 90% in men aged 81–90 years [2]. Likewise, the prevalence of LUTS ranges from 44% in men aged 40–59 years, increasing to 70% in men aged >80 years [3,4]. LUTS have been shown to cause significant debility and have greater impacts on anxiety and depression than similar chronic illnesses such as diabetes, gout and hypertension [5–7]. Using Medicare 5% sample data, Feinsten and Matlaga [8] found that 28% of Medicare beneficiaries aged >65 years have a diagnosis of BPH. Treatment of LUTS/BPH is similarly expanding in the USA. In a 5-year follow-up of a longitudinal cohort of men found to have incidental LUTS, 57.1% filled a LUTS/ BPH-related prescription [9]. Fee-for-service costs of BPH/LUTS for the USA in 2013 are estimated at US$785 m ($285–301/patient/year), excluding medication costs [8].
Lower urinary tract symptoms attributed to benign prostatic hyperplasia have been primarily studied in high-income and high-longevity areas, mainly North America, Europe and ‘first-world’ Australasia. In the past, global health funding and research in low-income countries has been appropriately allocated towards infectious disease and primary care, with urological focus primarily on vesicovaginal fistula and stone disease [10]. To our knowledge, no epidemiological assessments have been conducted specific to LUTS/BPH in the developing world, home of the substantial majority of the world’s population. A recent survey of urologists from low- and middle-income countries identified urolithiasis, BPH and prostate cancer as the three most common pathologies they encountered [11]. Interestingly, deaths attributable to LUTS/ BPH cannot be assessed using current databases as these mortalities are typically assigned to renal failure and infection diagnoses. Unfortunately, although some episodes of these renal failure and infection-attributed mortalities are undoubtedly a consequence of LUTS/BPH obstruction, there are no current databases which make this distinction.
Global health initiatives have long assessed rates and causes of death, and significant improvements have been made at decreasing mortality worldwide. Diseases that cause disability but not necessarily death have only recently been emphasized in epidemiological studies and have not seen improvements of a similar magnitude as overall mortality. Put differently, improvements in global health have largely been recorded as a decrease in deaths, and less so as an improvement in disease-free life. To highlight this point, between 2005 and 2015, there was a 22.7% reduction in age-standardized rates of years of life lost from all diseases in the Global Burden of Disease (GBD) database, as compared to only a 2.1% reduction in years lived with disability (YLD) [12].
The GBD project is a bold undertaking that was initially released in 1990 and has been methodologically updated over the intervening years. The goal of this project is to assess and track the health status of humanity as a whole, and to provide aggregated data that researchers and public health entities can utilize for policy and scientific purposes. Three primary methods are utilized to quantify disease impact: years of life lost, years lived with disease, and disability-adjusted life-years. Years of life lost is the number of years that a fatal malady deducts from the average life expectancy, YLD is the decrement in health that is accrued by living a year with a disease or its consequences, and disability-adjusted life-years are the sum of the two. A truly enormous volume of data resides in the GBD database; however, many processes still lack the sub-diagnosis specific detail that many first-world payor-operated systems require [13].
To our knowledge, there is no existing contemporary literature regarding the global trends in LUTS/BPH examined through the lens of morbidity or based on global socio-economic index. In the present study, we sought to assess the impact of LUTS/BPH globally, and additionally to investigate how LUTS/BPH diagnosis is affected by the differences in health and wealth that exist between regions of differing socio-economic status. Using the GBD database, we assess and compare best estimates of YLDs for LUTS/BPH, trended over 27 years from 1990 to 2017, with subset analysis by sociodemographic index (SDI) status.
Materials and Methods
The full methodology of the GBD database has previously been published, including recent updates to expand cause and sequelae list, and improvements in statistical methodology [14–17]. The GBD database is an aggregate collection of worldwide data and registries and includes household and cluster survey microdata, hospital and health systems (including national health systems) discharge and diagnosis codes, and including WHO case notification report data. These data were filtered with respect to BPH disease codes and diagnosis. While this collection of multinational and multilingual codes is reported in the dataset only as ‘BPH’ we will refer to this disease and associated complications, for purposes of clarity and convention, as ‘LUTS/BPH’.
Calculation of YLD for LUTS/BPH was compared with other urological disease. YLD were calculated using the WHO standardized method where YLD = number of prevalent cases multiplied by the assigned significance of the disease (disability weight 0.067 for LUTS/BPH) [18]. The methodology underlying disability weighting is derived from the aggregation of over 60 000 surveys completed over time [18]. Secondly, the SDI was calculated as a regional or national composite average of income per capita, average level of educational attainment, and fertility rate measures [19].
Results
Years Lived with Disease Attributed to BPH
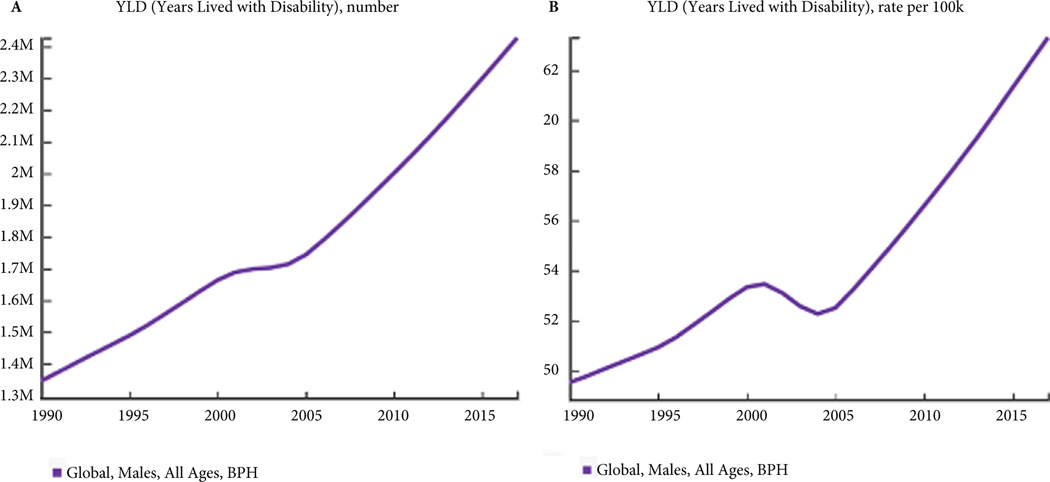
From 1990 to 2017 the YLD attributed to LUTS/BPH for males of all ages have been rising steadily. In absolute numbers after disability weight adjustment, the years lived with LUTS/BPH have risen from 1.35 million in 1990 to 2.43 million in 2017 (Fig. 1A). When analysed by incidence per 100 000, the incident rate increases from 24.94 in 1990 to 31.77 in 2017 (Fig. 1B).
Fig. 1.
The global increase in years lived with disease (YLD) attributed to BPH over the previous 27 years, reported in (A) absolute numbers and (B) rate per 100 000 persons.
LUTS/BPH Years Lived with Disease as Compared to Other Urological Disease Processes
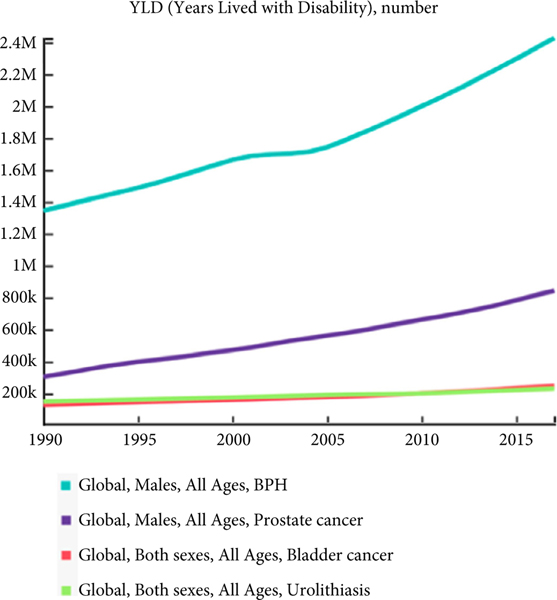
When assessed globally and compared to other significant urological diseases such as urolithiasis, prostate cancer and bladder cancer, LUTS/BPH have a vastly higher global total of YLD, even after disability weight adjustment. Data regarding YLD were calculated based on the affected genders: LUTS/BPH and prostate cancer data were examined for men of all ages, while bladder cancer, kidney cancer, and urolithiasis were calculated for both genders of all ages. The GBD database does not include data regarding less morbid or mortal diseases such as erectile dysfunction and urinary incontinence. In 2017, total weighted YLD attributed to LUTS/BPH were 2 247 334, compared to 843 226 for prostate cancer and 230 893 for urolithiasis. The 2017 YLD for common urological diseases are represented in Table 1. Additionally, the rate of rise is also higher and increasing in comparison to these other major causes of disease and urological morbidity (Fig. 2).
Table 1.
Global years lived with disease attributed to urological diseases in 2017, all ages.
| YLD | CI | |
|---|---|---|
| LUTS/BPH | 2 427 334 | 948 607 |
| Prostate cancer | 843 226 | 531 978 |
| Bladder cancer | 247 041 | 143 414 |
| Urolithiasis | 230 893 | 78 687 |
| Kidney cancer | 141 048 | 88 949 |
YLD, years lived with disease. Global Burden of Disease database standardized methodology and disability indices used.
Fig. 2.
The global increase in years lived with disease (YLD) attributed to BPH over the previous 27 years compared to major urological diseases, reported in absolute numbers. (LUTS/BPH disability weight = 0.067).
LUTS/BPH Years Lived with Disease Stratified by Sociodemographic Index
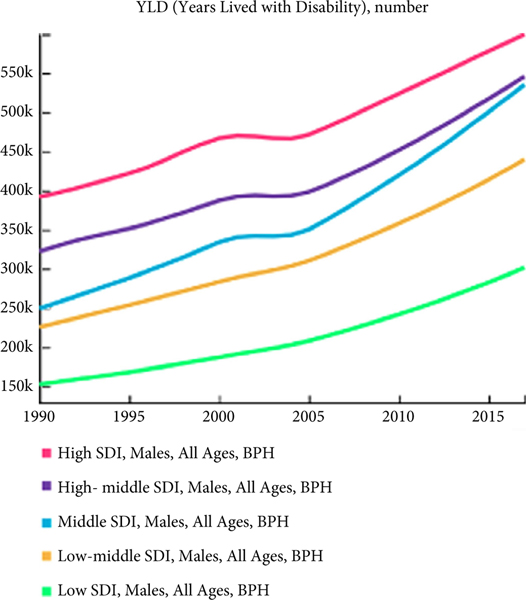
To be diagnosed with LUTS/BPH requires both access to, and the ability to pay for, medical care. In the developing world, these healthcare necessities are not commonly available. When a diagnosis is obtainable in the developing world, this rarely reported yet mortal disease is appropriately overshadowed by more acute survival concerns, such as infectious disease and trauma. However, as the sociodemographic standing of a region or society rises, opportunities increase for a patient to reach an age at which the disease can manifest while the patient is in good enough health and also possesses access to medical care. In global populations, when broken down by SDI quintile, LUTS/BPH show the highest impact when ordered by SDI level, with 25.1% of YLD in the highest quintile compared to 12.2% in the lowest quintile. Absolute numbers are steadily increasing in all quintiles (Fig. 3).
Fig. 3.
The global increase in years lived with disease (YLD) attributed to BPH over the previous 27 years divided by sociodemographic index (SDI) quintile, reported in absolute numbers.
Discussion
The human impact of disease currently attributed to LUTS/BPH is enormous, and has increased by 80% over the past 17 years based on data from a well-validated global dataset. When compared to other major causes of urological morbidity including prostate cancer, bladder cancer, and urolithiasis, YLD attributed to LUTS/BPH in 2017 were three times higher than prostate cancer, the next highest source of YLD. Viewed over the course of 17 years, YLD attributed to LUTS/BPH are rising at a faster rate than other urological sources of morbidity. Finally, our findings include analysis by SDI quintile, demonstrating a significant differential between the highest and the lowest members of sociodemographic strata, which has implications for the future. Analyses of this type have significance and utility for healthcare systems, payors and governments to plan for future needs.
Lower urinary tract symptoms attributed to benign prostatic hyperplasia cause great impairment to male health and quality of life and are responsible for more population-wide morbidity than any other urological disease. The implications of this disease burden, felt directly by the patient and secondarily by the urological workforce, is poised to grow rapidly and accelerate further for a variety of reasons. First, the global population is ageing, and, specifically, the percentage of the population aged >65 years is projected to increase from a 2018 estimate of 9.06% (680 million) to 17% of the total population, resulting in a total of 1.6 billion humans aged >65 years in the next 30 years [20,21]. This increase in the absolute number of men in the age range where LUTS/BPH most commonly present will result in a great expansion of patients with this condition.
Second, as progress is recorded in the battle against premature mortality, we create an ever larger cohort of men of advancing age and better health who will experience LUTS/BPH and the complications thereof. Our analysis of the GBD data showed that men in the lower SDI levels were far less likely to be bothered by LUTS/BPH. However, as the developing portions of the world overcome other more severe and/or mortal diseases, and health systems provide expanding subsistence care, the diagnosis of and need for treatment for LUTS/BPH is expected to expand in excess of the raw demographic increase described above.
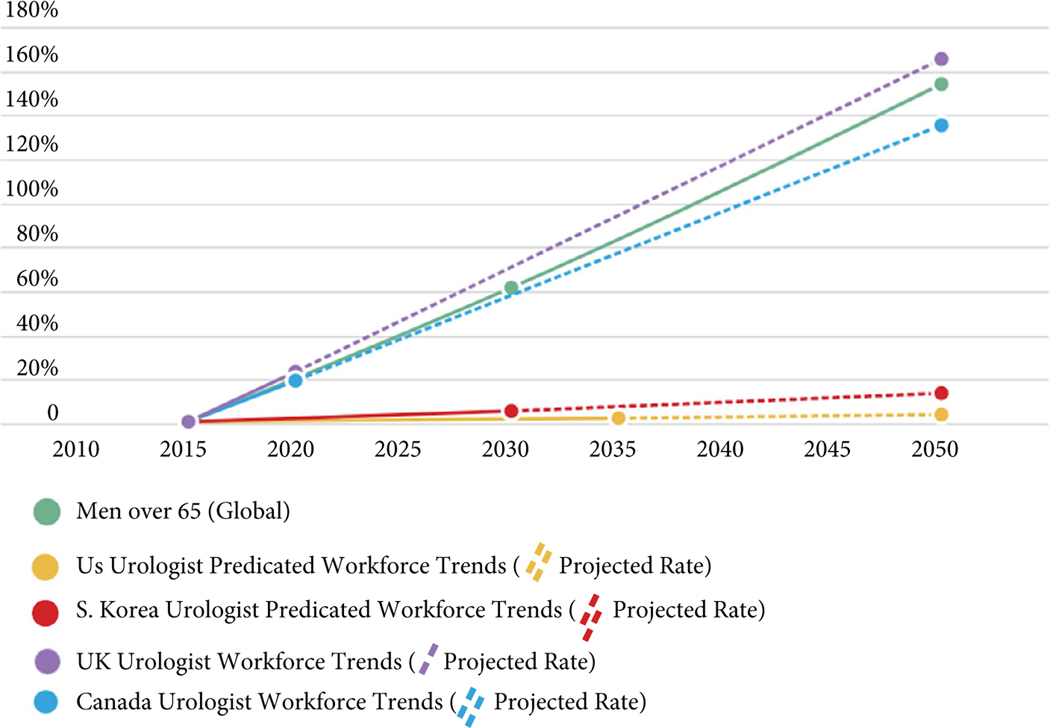
Trends in disease are critically important as delivery of care requires well-structured healthcare systems that can respond appropriately to changes in incidence and prevalence of specific maladies. While there are very few data regarding the urological workforce in developing countries, ‘first world’ countries show disparate trends and widely differing ratios of providers. In the USA and South Korea, the gap between the urological workforce growth and projected population is stark, while data from the UK and Canada suggest that they will maintain a stable balance (Fig. 4), although those regions begin with lower ratios of urological providers to population. In the USA, the urological workforce (here conceptualized as physician urologists plus advanced care providers) is projected to increase by 2.5% in the next 15 years, simultaneous to an increase of 61% in men aged >65 years in the USA (Fig. 4) [22–24]. In systems such as these, profound shortfalls are expected [25]. In Europe, reported urology provider to patient ratios throughout the region and beyond are highly variable, but, in settings where healthcare is at least in part centrally controlled, these systems may enjoy varying degrees of flexibility in response to changing needs. A survey published in 2000 showed a substantially lower density of urologists in Europe when compared to the USA; the UK specifically had a ratio of one urologist per 130 000 persons at that time [26]. However, continuing through 2015, the UK and Europe show a ratio of providers to population that has been increasing, although it is enormously variable by region and country [27–29]. There is a gap in the literature regarding the urological workforce in developing regions of South America, Africa and Asia where additional barriers to providing urological care often include access to laboratory and imaging studies, availability of support staff, and access to surgical training [11]. While it is well beyond the purview of this disease-based assessment to further consider these provider levels, quality disease data such as those provided by the GBD project should allow better allocation of each healthcare system’s resources, including subspecialty training, and are absolutely critical to meet the dynamic needs of population health.
Fig. 4.
Percentage change in global population of men over time as compared to first-world urological workforce trends.
In addition to the manpower implications, LUTS/BPH are associated with a significant financial burden. Were the 2019 world to assume a cost and treatment pattern reflective of US Medicare costs as last assessed in 2013, we observe that if the current prevalence of 61.1% of men aged >65 years using alpha-blocker medication were multiplied by the global population of 303 788 086 men aged >65 years, there would be a total of 185 614 521 men receiving this common medical LUTS/BPH therapy, resulting in fee-for-service costs of $73.8 bn per year ($243 per man aged >65 years) [9]. This value is greater than the defence budget of all but two countries in the world, and again calls attention to the enormous future challenges which may disproportionately impact urology in comparison to other specialities [30].
While medical management of LUTS/BPH may often fall into the realm of primary care providers, surgical and procedural interventions for LUTS/BPH require specialized training and thus remain the domain of the urological workforce. Often employed after failed medical management, surgical treatment is a mainstay of LUTS/BPH therapy. Surgery and minimally invasive procedures produce greater improvement in symptom scores than medical management and are specifically recommended for treatment of BPH-related complications such as urinary retention, recurrent infection and other features of progression [31,32]. Global access to surgery of any form in the present day, however, is limited for most people. Assessing surgical care broadly, only 6% of the surgical procedures performed for any indication are carried out in the poorest 33% of the world, and approximately five billion people currently do not have any access at all to surgical or anaesthetic treatment [33]. As access to surgery increases along with the necessity for additional BPH procedures, a massive need for urological caregivers, and sites of care, will follow. Currently, the ratio of urologists to population is approximately one per 27 000 in the USA, and as low as one per 15 000 in Germany, Italy and Austria, while in Africa there are often millions of residents per urologist [22,29]. It is unclear how this gap will be filled.
Weaknesses of the present analysis include the significant variability in global data-gathering efforts that is intrinsic to the GBD databases and sources that underlie it, especially in the medical systems and databases of the developing world which may lack accessible record-keeping. Different cultures and health systems may use different systems to define diseases and measure symptoms, especially in resource-poor areas [16]. The most recent iteration of the GBD database still retains a paucity of claims data from hospital admissions in low-income areas and relies on a degree of extrapolation of medical claims information from data-rich regions to these areas [16]. Specific challenges related to non-fatal estimation such as this include distinguishing measurement or recording error from true variation of rates of disease.
Weaknesses specific to non-fatal analyses, such as the effects of LUTS/BPH, include the methodology by which disease severity weighting is derived predominantly from high-income countries, which likely underestimates the disability and thus YLD incurred in low- and middle-income countries with decreased access to medical and surgical treatment. In the case of LUTS/BPH, lack of access to alpha-blockers or TURP may significantly increase the impact on quality of life. This same critique can be applied to the development of the disability weight scores: the data on which they are based are predominantly derived from European regions, and, despite rigorous methodology, may not be representative of the impact of LUTS/BPH on life in other regions [18]. No additional insight into specific subsets of disease states attributed to BPH such as LUTS, retention, UTI or renal failure are able to be derived from these broad but robust population data in their current iteration, and other disease states may be falsely attributed to the broad diagnosis of ‘BPH’ as attributed within the GBD database.
Addressing mortality, in the current GBD methodology, no deaths are assigned to the diagnosis of BPH, which consequently underestimates the total impact of this disease and illustrates the challenges of integrating variable data from disparate sources. LUTS/BPH, especially untreated, represent a morbid and fatal disease as was well documented in the 19th and earlier 20th century [34,35]. Given the unfavourable access to healthcare, portions of the developing world may currently recapitulate these historical patterns. As data collection improves, the unquantified BPH-caused deaths that are most likely being tallied under infectious deaths and renal failure will eventually be applied more accurately to the appropriate causes and allow an enhanced assessment of this disease. In 2017, the GBD data estimated 599 071 male deaths occurred from renal failure (due to type 2 diabetes, hypertension and other/unspecified) and UTI. What percentage of these deaths is attributable to, or accelerated by, BOO consequent to BPH is currently unknown.
Finally, SDI ascendance and resultant changes in lifestyle may impact this disease in dynamic ways, again likely contributing to higher incidence in the future. LUTS/BPH has a strong epidemiological relationship to diseases of resource abundance: diabetes, metabolic syndrome and erectile dysfunction (likely a marker for end organ dysfunction) to name a few [1]. While the causal interaction of these diseases with histological BPH is poorly understood, they are clearly associated and thus increases in these diseases may additionally impact the experienced rates of BPH diagnosis and treatment. Unfortunately, unlike some diseases where specific and modifiable behavioural or dietary factors such as smoking directly impact incidence rates, no clear interventional paths lead to reduction in LUTS/BPH incidence, although it should be noted that there are cross-sectional differences in LUTS/BPH incidence when compared by levels of physical activity, for example [36].
In conclusion, we find that the quantified morbidity of LUTS/ BPH is enormous when surveyed on a global scale. This health impact exceeds all other urological diseases at present and is likely to further expand as the population ages. Relevant to healthcare systems, while men in lower SDI groups currently appear to bear less of this burden than those in higher SDI groups, they appear poised to disproportionally contribute to future increases in disease incidence.
Healthcare systems will need to adapt to these demands. The urological workforce in the USA is fast becoming inadequate to keep up with demand and this discrepancy between providers and patients in need is accelerating [22,25]. In the UK, Canada and many other parts of the world urological provider-to-patient ratios are even lower, and likely reach their worst levels in the lowest SDI regions. Additionally, these data suggest that there will be increasing per-capita demand as more and more of the population is composed of men reaching advanced age with intact health [21,22]. LUTS/ BPH today represent the largest demand of first-world urology resources and appear poised to expand this position in the medical waiting rooms of the rest of the world. Preventative, complementary and cost-effective treatment strategies for this disease are ever-more important.
Abbreviations:
- GBD
Global Burden of Disease
- LUTS/BPH
LUTS attributed to BPH
- YLD
years lived with disease
Footnotes
Conflicts of Interest
Bryn Launer, William Ricke and Granville Lloyd have nothing to disclose. Kevin McVary declares the following: having served as a scientific study or trial, and principal investigator for NxThera, a principal investigator and consultant for NIDDK and Olympus, a principal investigator for Astellas, a principal investigator and fellowship grant consultant for Boston Scientific (formerly AMS), and being a patent holder for A1 Thermal-Actived Penile Prosthesis.
References
- 1.Parsons JK. Benign prostatic hyperplasia and male lower urinary tract symptoms: epidemiology and risk factors. Curr Bladder Dysfunct Rep 2010; 5: 212–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol 1984; 132: 474–9 [DOI] [PubMed] [Google Scholar]
- 3.Irwin DE, Milsom I, Hunskaar S et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 2006; 50: 1306–15 [DOI] [PubMed] [Google Scholar]
- 4.Parsons JK, Bergstrom J, Silberstein J, Barrett-Connor E. Prevalence and characteristics of lower urinary tract symptoms in men aged ≥80 years. Urology 2008; 72: 318–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower urinary tract symptom severity: results from the Health Professionals Follow-up Study. Urology 2002; 59: 245–50 [DOI] [PubMed] [Google Scholar]
- 6.Coyne KS, Wein AJ, Tubaro A et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int 2009; 103: 4–11 [DOI] [PubMed] [Google Scholar]
- 7.Rosen RC, Giuliano F, Carson CC. Sexual dysfunction and lower urinary tract symptoms (LUTS) associated with benign prostatic hyperplasia (BPH). Eur Urol 2005; 47: 824–37 [DOI] [PubMed] [Google Scholar]
- 8.Feinsten L, Matlaga B. Urologic Diseases in America. US Department of Health and Human Services. Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. 2018:97–160 [Google Scholar]
- 9.Welliver C, Feinstein L, Ward JB et al. Trends in lower urinary tract symptoms associated with benign prostatic hyperplasia, 2004 to 2013: the Urologic Diseases in America Project. J Urol 2020; 203: 171–8 [DOI] [PubMed] [Google Scholar]
- 10.Manganiello M, Hughes CD, Hagander L et al. Urologic disease in a resource-poor country. World J Surg 2013; 37: 344–8 [DOI] [PubMed] [Google Scholar]
- 11.Metzler I, Bayne D, Chang H, Jalloh M, Sharlip I. Challenges facing the urologist in low-and middle-income countries. World J Urol 2020: 1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vos T, Allen C, Arora M et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1545–602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Metrics: Disability-Adjusted Life Year (DALY). World Health Organization, 2004 [Google Scholar]
- 14.Fitzmaurice C, Akinyemiju TF, Al Lami FH et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: a systematic analysis for the global burden of disease study. JAMA Oncol 2018; 4: 1553–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naghavi M, Abajobir AA, Abbafati C et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1151–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vos T, Abajobir AA, Abate KH et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017; 390: 1211–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murray CJ, Barber RM, Foreman KJ et al. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet 2015; 386: 2145–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salomon JA, Haagsma JA, Davis A et al. Disability weights for the global burden of disease 2013 study. Lancet Glob Health 2015; 3: e712–23 [DOI] [PubMed] [Google Scholar]
- 19.GBD Compare Data Visualization, 2018. Available at: http://vizhub.healthdata.org/gbd-compare.
- 20.Lutz W, Samir KC. Dimensions of global population projections: what do we know about future population trends and structures? Philos Trans R Soc B Biol Sci 2010; 365: 2779–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.He W, Goodkind D, Kowal P. An Aging World: 2015 Census Bureau. Available at: https://www/censusgov/content/dam/Census/library/publications/2016/demo/p95-16-1pdf. Accessed August 2017
- 22.McKibben MJ, Kirby EW, Langston J et al. Projecting the urology workforce over the next 20 years. Urology 2016; 98: 21–6 [DOI] [PubMed] [Google Scholar]
- 23.2017. National Population Projections Tables. United States Census Bureau, 2017 [Google Scholar]
- 24.Oh Y. The future prospects of supply and demand for urologists in Korea. Investig Clin Urol 2017; 58: 400–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gonzalez CM, McKenna P. Challenges facing academic urology training programs: an impending crisis. Urology 2013; 81: 475–9 [DOI] [PubMed] [Google Scholar]
- 26.Kiely E. The European Board of Urology survey of current urological manpower, training and practice in Europe. BJU Int 2000; 85: 8–13 [DOI] [PubMed] [Google Scholar]
- 27.Goel A. Urology in India: numbers and practice. Indian J Urol 2019; 35: 245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CMA Workforce Survey 2017 – Urology Profile. In. Canadian Medical Association 2017. [Google Scholar]
- 29.Michael Palmer JM. British Association of Urological Surgeons and The Specialist Advisory Committee in Urology: Workforce Report, 2015 [Google Scholar]
- 30.Tian N, Fleurant A, Kuimova A, Wezeman P, Wezeman S. Trends in world military expenditure, 2018. SIPRI Fact Sheet. 2 May. In:2019. [Google Scholar]
- 31.Cornu J-N, Ahyai S, Bachmann A et al. A systematic review and meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic obstruction: an update. Eur Urol 2015; 67: 1066–96 [DOI] [PubMed] [Google Scholar]
- 32.Yuan J-Q, Mao C, Wong SY-S et al. Comparative effectiveness and safety of monodrug therapies for lower urinary tract symptoms associated with benign prostatic hyperplasia: a network meta-analysis. Medicine. 2015; 94: e974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meara JG, Leather AJ, Hagander L et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015; 386: 569–624 [DOI] [PubMed] [Google Scholar]
- 34.Ford E. Case of a diseased bladder, with enlargement of the prostate gland, and other morbid appearances. Med Phys J 1800; 4: 390. [PMC free article] [PubMed] [Google Scholar]
- 35.Stewart HH. Bladder-neck obstruction due to non-malignant disease of the prostate. Br Med J 1945: 724–7 [PubMed] [Google Scholar]
- 36.Maserejian NN, Kupelian V, Miyasato G, McVary KT, McKinlay JB. Are physical activity, smoking and alcohol consumption associated with lower urinary tract symptoms in men or women? Results from a population based observational study. J Urol 2012; 188: 490–5 [DOI] [PMC free article] [PubMed] [Google Scholar]