Background:
More than 65% of persons with opioid use disorder (OUD) in the United States do not receive any treatment, including recommended treatment with 1 of the following U.S. Food and Drug Administration-approved medications: buprenorphine; methadone; or injectable, extended-release naltrexone (1). Efforts to expand treatment with medication have included a strong focus on primary care physicians who can prescribe injectable, extended-release naltrexone and, after obtaining a waiver from the Drug Enforcement Administration, buprenorphine for OUD in the office setting (1). (Methadone for OUD can be dispensed only in specialty programs [1].)
Objective:
To conduct a national survey examining primary care physicians' beliefs and attitudes about OUD medication.
Methods and Findings:
In February 2019, we mailed a questionnaire, $2 cash incentive, and stamped return envelope to a nationally representative, random sample of 1000 U.S. physicians selected from the American Medical Association Physician Masterfile, a database of all U.S. licensed physicians. Physicians were eligible if they identified as family, internal, or general medicine practitioners and were actively practicing primary care at the address on file during the study period. Nonrespondents were mailed identical packets in 5 follow-up waves in March, April, June, July, and August 2019. Survey domains (Supplement, available at Annals.org) included perceived effectiveness of OUD medications, OUD medication treatment practices (for example, whether a physician prescribes buprenorphine for OUD), and support for policies related to OUD medication. Perceived effectiveness and policy items used 5-point Likert scales. Respondents selected current practices from a list of options.
Of the 668 eligible physicians, 54% (n = 361) responded to the survey. Surveys with more than 50% of data missing (n = 25) were excluded from the analysis. There were no differences in response by specialty, age, sex, degree (MD or DO), or practice type. Responders were less likely to be from the South (22.1%) than nonresponders (37.2%). To address nonresponse bias, analyses incorporated weights that aligned the regional distribution of physicians in the responding sample to the distribution in the overall sample.
Respondent characteristics were similar to national data on primary care physicians (Table) (2). Two thirds of physicians believed that treatment of OUD is more effective with medication than without (67.1%) and that persons can safely use medication to manage OUD in the long term (63.7%) (Figure). Physicians were more likely to perceive buprenorphine (77.5%) as effective than methadone (62.1%) or injectable, extended-release naltrexone (51.4%). One fifth (20.2%) of physicians expressed interest in treating patients with OUD. Few reported prescribing buprenorphine (7.6%) or naltrexone (4.0%) for OUD, and few expressed interest in obtaining a buprenorphine waiver (11.8%). Most physicians supported increasing insurance coverage of (81.8%) and government investment in (76.4%) OUD medication, but fewer than half supported allowing physicians to prescribe methadone for OUD in primary care settings (47.7%) or eliminating the buprenorphine waiver requirement (38.0%).
Table.
Characteristics of Primary Care Physician Survey Respondents
| Characteristic | Survey Respondents (n = 336), % |
National Primary Care Physician Population, %* |
|---|---|---|
| Specialty | ||
| Family practice | 52.4 | 51.5 |
| General practice | 4.5 | 3.6 |
| Internal medicine | 43.2 | 44.9 |
| Age | ||
| <35 y | 7.6 | 5.7 |
| 35-44 y | 19.1 | 22.6 |
| 45-54 y | 29.4 | 30.7 |
| 55-64 y | 28.5 | 27.3 |
| ≥65 y | 15.5 | 13.7 |
| Sex | ||
| Female | 41.2 | 39.1 |
| Male | 58.8 | 60.9 |
| Region | ||
| Northeast | 22.1 | 19.0 |
| South | 29.8 | 35.6 |
| Midwest | 22.1 | 20.9 |
| West | 26.1 | 24.6 |
| Practice type† | ||
| Solo or 2-physician | 17.5 | Not available |
| Group | 50.9 | Not available |
| Nongovernmental hospital | 4.6 | Not available |
| Government-based | 11.4 | Not available |
| Other‡ | 15.6 | Not available |
| Buprenorphine waivers§ | ||
| Physicians with X waiver | 10.6 | Not available |
| Mean estimated percentage of patients in panel with OUD | 7.1 | Not available |
OUD = opioid use disorder.
From reference 2.
National data on practice type among primary care physicians defined as family, internal, or general medicine physicians are not available.
Includes other patient care, locum tenens, and no classification.
In 2019, an estimated 8.3% of all U.S. physicians had a buprenorphine waiver. Data on the proportion of primary care physicians with a waiver nationally are not available (www.samhsa.gov/medication-assisted-treatment/practitioner-program-data/certified-practitioners).
Figure.
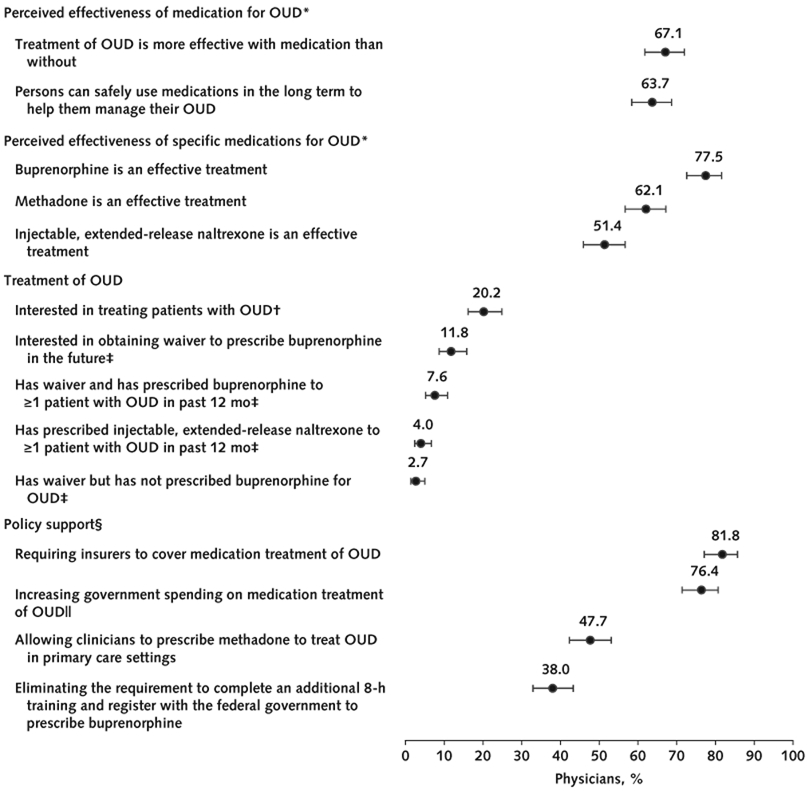
U.S. primary care physicians' attitudes about medication for treatment of OUD.
Stratified analyses comparing survey results among early (waves 1 to 3) versus late (waves 4 to 6) responders showed overlapping 95% CIs for all items. Point estimates differed by less than 6 percentage points for all items, with 1 exception: 64.9% (95% CI, 58.7% to 70.7%) of early responders versus 54.0% (CI, 43.3% to 64.4%) of late responders reported that methadone is an effective treatment of OUD. Error bars represent 95% CIs. To create dichotomous measures for each domain, response categories 1 and 2 were combined. OUD = opioid use disorder.
* Used a 5-point Likert scale (1 = strongly agree; 2 = somewhat agree; 3 = neither agree nor disagree; 4 = somewhat disagree; 5 = strongly disagree).
† Used a 5-point Likert scale (1 = very interested; 2 = somewhat interested; 3 = neither interested nor uninterested; 4 = somewhat uninterested; 5 = very uninterested).
‡ Physicians indicated their current practices and future plans about prescribing medication to treat OUD by selecting from a list of options.
§ Used a 5-point Likert scale (1 = strongly favor; 2 = somewhat favor; 3 = neither favor nor oppose; 4 = somewhat oppose; 5 = strongly oppose). The item about the buprenorphine training and registration requirement had an additional option (6 = I am not familiar with this requirement).
∥ Used a 5-point Likert scale (1 = very important; 2 = somewhat important; 3 = neither important nor unimportant; 4 = somewhat unimportant; 5 = very unimportant).
Discussion:
A third of primary care physicians did not perceive OUD medication treatment to be more effective than nonmedication treatment or safe for long-term use, despite conclusive evidence supporting continual medication use as the gold-standard OUD treatment (1). Physicians reported low interest in treating OUD and low support for policy proposals allowing office-based physicians to prescribe methadone for OUD (3) and eliminating the buprenorphine waiver (4). These findings suggest that policy changes alone are unlikely to lead to widespread availability of primary care-based medication treatment of OUD. Longer-term solutions, such as incorporating addiction medicine into physician training, and delivery system reforms, such as embedding addiction medicine professionals in primary care practices, may be needed.
To minimize concerns about social desirability and nonresponse bias, we ensured participant confidentiality, used nonleading questions, and used weights to account for minor differences in respondent versus nonrespondent characteristics. About one third (n = 332) of physicians in the original sample frame had an incorrect practice status, specialty, or practice location in the American Medical Association Physician Masterfile and were deemed ineligible. However, the characteristics of survey respondents were similar to those of primary care physicians in national data. Although we cannot eliminate the possibility of nonresponse bias, we found no differences in early (waves 1 to 3) versus late (waves 4 to 6) respondents' answers to survey items. Our findings suggest an urgent need to increase primary care physicians' endorsement of the effectiveness of medication for OUD and their willingness to prescribe it.
Supplementary Material
Footnotes
Financial Support: By a Johns Hopkins University Frontier Award to Dr. McGinty.
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M19-3975.
Reproducible Research Statement: Study protocol and data set: Not available. Statistical code: Available from Dr. McGinty (bmcginty@jhu.edu).
Contributor Information
Emma E. McGinty, Johns Hopkins Bloomberg School of Public Health and Johns Hopkins Center for Mental Health and Addiction Policy Research, Baltimore, Maryland.
Elizabeth M. Stone, Johns Hopkins Bloomberg School of Public Health and Johns Hopkins Center for Mental Health and Addiction Policy Research, Baltimore, Maryland.
Alene Kennedy-Hendricks, Johns Hopkins Bloomberg School of Public Health and Johns Hopkins Center for Mental Health and Addiction Policy Research, Baltimore, Maryland.
Marcus A. Bachhuber, Section of Community and Population Medicine, Louisiana State University Health Sciences Center-New Orleans, New Orleans, Louisiana.
Colleen L. Barry, Johns Hopkins Bloomberg School of Public Health and Johns Hopkins Center for Mental Health and Addiction Policy Research, Baltimore, Maryland.
References
- 1.National Academies of Sciences, Engineering, and Medicine. Medications for Opioid Use Disorder Save Lives. Washington, DC: National Academies Pr; 2019. [PubMed] [Google Scholar]
- 2.Petterson S, McNellis R, Klink K, et al. The State of Primary Care in the United States: A Chartbook of Facts and Statistics. Washington, DC: Robert Graham Center; 2018. [Google Scholar]
- 3.Samet JH, Botticelli M, Bharel M. Methadone in primary care–one small step for Congress, one giant leap for addiction treatment. N Engl J Med. 2018;379:7–8. [PMID: 29972744] doi: 10.1056/NEJMp1803982 [DOI] [PubMed] [Google Scholar]
- 4.Fiscella K, Wakeman SE, Beletsky L. Buprenorphine deregulation and mainstreaming treatment for opioid use disorder: X the X waiver. JAMA Psychiatry. 2019;76:229–30. [PMID: 30586140] doi: 10.1001/jamapsychiatry.2018.3685 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


