Abstract
Background
Maintaining and enhancing competence in the breadth of emergency medicine (EM) is an ongoing challenge. In particular, resuscitative care in EM involves high‐risk clinical encounters that demand strong procedural skills, effective team leadership, and up‐to‐date clinical knowledge. Simulation‐based medical education is an effective modality for enhancing technical and nontechnical skills in crisis situations and has been effectively embedded in undergraduate and postgraduate medical curricula worldwide. To our knowledge, there are few existing systematic department‐wide simulation programs to address continuing professional development (CPD) for practicing academic EM faculty.
Development Process
We developed our novel, simulation‐based CPD program following Kern’s six‐step model. Based on the results of a multimodal needs assessment, a longitudinal curriculum was mapped and tailored to the available resources. Institutional support was provided in the form of a departmental grant to fund a physician program lead, monthly session instructors, and operating costs.
Outcomes
CPD simulation sessions commenced in January 2017. Our needs assessment identified two key types of educational needs: 1) crisis resource management skills and 2) frequent practice of high‐stakes critical care procedures (e.g., surgical airways). Simulation sessions involve two high‐fidelity simulated resuscitations and one skills lab per day. To date, 21 sessions have been delivered, reaching 161 practicing EPs. Feedback from our faculty has been positive.
Reflective Discussion
We have successfully introduced a curriculum of monthly simulation‐based CPD based on the educational needs of our EPs. Future work will include more detailed program evaluation linked to clinical outcomes and program expansion to support nearby institutions.
Resuscitative care in the emergency department (ED) involves high‐risk clinical encounters with critically ill patients who require a skilled team to deliver timely and effective care. The maintenance and enhancement of resuscitative competencies is challenging for emergency physicians (EPs) due to infrequent and unpredictable clinical exposure to high‐stakes cases and rare procedures, lack of meaningful performance feedback or coaching opportunities, 1 and competing demands for continuing professional development (CPD). In other high‐stakes industries, practitioners are expected to participate in regular training for the purposes of maintaining certification. However, EPs in most jurisdictions are not required to complete specific training to maintain or enhance their competencies in resuscitative care. 2 , 3
Simulation‐based medical education (SBME) is an effective modality for enhancing technical and nontechnical skills and has been effectively embedded in medical curricula worldwide. 4 This training platform enables trainees to engage in a process of deliberate practice and feedback in a safe environment. SBME has a growing role in medical education, interprofessional training, and increasingly, in situ in the actual clinical environment with on‐duty clinical teams. 5 While there are growing calls for enhanced simulation‐based CPD, 6 , 7 and some burgeoning efforts to meet this demand, 8 few published examples exist 9 , 10 , 11 of comprehensive CPD simulation curricula particularly for EPs.
NEED FOR INNOVATION
Within our academic department, we have 85 full‐time EPs, approximately 55 residents, two to four foreign‐trained fellows, and numerous off‐service trainees. Consistent with literature on maintenance of competency, our attending EPs identified waning opportunities for hands‐on critical care and concerns for skill degradation. 3 , 4
OBJECTIVE OF INNOVATION
We developed a novel simulation‐based CPD curriculum designed specifically for academic EPs, to address the particular deficit in skill maintenance for resuscitative critical care and “high‐acuity, low‐opportunity” clinical procedures for EPs.
DEVELOPMENT PROCESS
We developed and implemented our simulation‐based CPD curriculum following Kern’s six‐step model: After identifying the problem (step 1), we performed a multimodal, targeted needs assessment (step 2) to clarify both perceived and ascribed educational needs of our group. This consisted of consultations and information gathering from department leaders, patient safety incident reports, morbidity and mortality rounds, and observational data from our in situ simulation program. 12 Based on these data, we created a survey to all department members to identify and prioritize educational needs. Next, we conducted focus groups with local experts to identify themes best addressed through simulation (step 3) and to create a broad outline of goals and objectives. This outline was brought to departmental stakeholders for feedback. Next, specific content and teaching methods were identified to address particular topics (step 4) over a 2‐year implementation. Departmental academic funds were allocated to support teaching time and operational costs.
THE IMPLEMENTATION PHASE
We implemented our program (step 5) in January 2017 and have run continuously since. Simulation sessions are 3 hours, recurring monthly. Participation is voluntary and nonremunerated, but encouraged through “nudge” methods including regular supportive messaging from department leadership, direct personal outreach, and consideration of individual faculty participation at performance reviews. We obtained accreditation by the two governing national professional colleges to offer CPD credits.
Each simulation session follows a standard model: eight participants are divided into groups of four. Each group rotates through two 90‐minute stations: one “low‐fidelity” station focused on deliberate practice of specific procedural skills using part‐task trainers and two back‐to‐back “high‐fidelity simulation” cases with a SimMan 3G (Laerdal Co). EPs self‐select to participate in a session through online sign‐up based on personal interest or as encouraged by departmental leadership. Stations are facilitated by an experienced simulation educator and offer opportunities for hands‐on skill development, coaching, and facilitated debriefing. High‐fidelity simulation cases are selected from a preexisting repository of over 70 locally developed cases to align with educational needs and coupled thematically with the clinical skills being taught in the accompanying skill station. The high‐fidelity simulation is delivered in conjunction with one “nurse confederate.” After each session, an anonymous feedback survey is sent to all participants to generate aggregate quantitative and narrative feedback (step 6).
OUTCOMES
Since implementation, we have successfully delivered 21 faculty simulation sessions, with 161 participants. Five sessions were canceled due to scheduling challenges. Eighty‐five percent of faculty have participated in at least one session, and 52% have participated in two or more. Postsession surveys (n = 53) demonstrate a strongly positive reception to the sessions (Figure 1), with a majority agreeing that the sessions met stated learning objectives (96%), were clinically relevant (92%), and addressed participants’ knowledge gaps (96%). Facilitator efficacy was very highly rated (98%). Importantly, participants responded that the experience would lead to changes in their clinical practice (92%).
Figure 1.
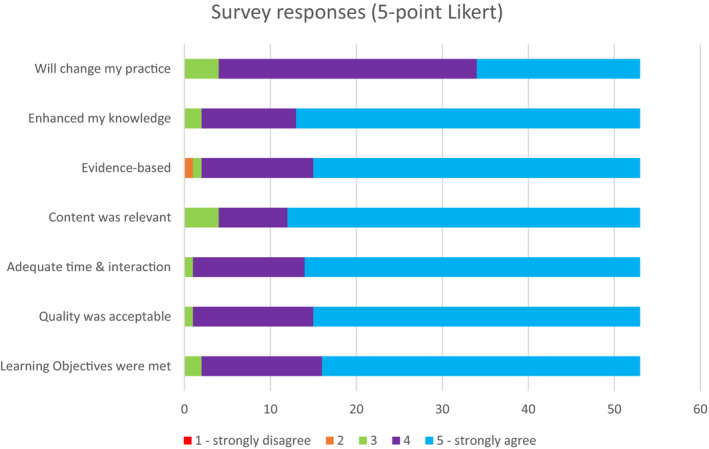
Distribution of feedback on CPD simulation sessions (5‐point Likert scale; n = 53).
Narrative feedback collected both face to face and anonymously reflects a similar sentiment. Commonly reported feedback included statements such as:
“Absolutely necessary and should continue to be provided in order to fill gaps in our clinical exposure.”
“I haven’t done one of these in years so this helps my confidence.”
“I think it is a good team‐building opportunity.”
“Greatly appreciate the teaching especially in areas that we do not see very often.”
“Noted my communication is clearer, crisper as a leader.”
“The sim was awesome, made me uncomfortable. That was perfect.”
“This session highlighted some knowledge gaps for me as well as provided me with resources that I can take going forward!”
REFLECTIVE DISCUSSION
These findings demonstrate that simulation is aligned with the CPD needs of in‐practice EPs and that SBME has an important role for maintenance of clinical competence. Our EP group has embraced simulation and expressed a strong interest to increase exposure. Our program has also demonstrated an impact on self‐reported confidence with high‐acuity, low‐opportunity skills.
A theme we have encountered through this program is the importance of delivering CPD simulation in a dedicated environment. In some centers, in situ simulation is used as a crude “CPD” offering for EPs, alongside other health professions. While such interventions can add tremendous value in developing interprofessional competencies, the environment necessarily creates a conflict between educational objectives and psychological safety: is the in situ simulation offered to address the particular learning needs of attending physicians or the broader interprofessional team? Does it create an environment in which EPs, accustomed to being the authoritative expert in high‐stakes scenarios, are willing to be put under a microscope in terms of their own knowledge or skill deficiencies? In contrast, our program delivers CPD content in a dedicated, safe environment where physicians have an opportunity to focus on their own shortcomings among peers. Numerous participants informally highlighted their appreciation for the opportunity to make mistakes and discuss them, without feeling like it detracted from the perception of interprofessional colleagues. Moreover, with a diversity of experience levels and domains of expertise among the physicians participating in these sessions, our participants noted the value in learning from the perspectives of their physician peers, which is often missing during in situ simulation.
Our paper is not without limitations, chiefly due to presenting only self‐reported data. This paper shows that simulation‐based CPD is well received by practicing EPs, but our data are limited by only evaluating program impact at Kirkpatrick levels I and II. There is a strong need to link curricula more definitively with objective impacts on clinical performance during program evaluation—specifically evaluating impact on physician competencies, knowledge retention, error rates in the clinical environment, and ideally, patient‐oriented outcomes. Simulation‐based education is a resource‐intensive intervention, in terms both of operating costs and of the time required of participants, so it will be important to demonstrate its relevance to clinical outcomes. Second, overall participation in the feedback survey was low, likely due to technologic constraints (e‐mailed survey links) although self‐exclusion of disenfranchised or unsatisfied participants is possible. More robust methods for obtaining feedback and exploration of barriers to participation are warranted. Third, the generalizability to other academic centers or community hospitals is uncertain.
Overall, we demonstrated that comprehensive SBME can be used as a vehicle for CPD among practicing EPs and that such a program is well received by physicians with a self‐assessed positive impact on practice. It is reasonable to expect that in the future, ongoing participation in simulation‐based CPD will become a professional expectation for maintenance of competency, and we are confident that this will only strengthen the practice of emergency medicine.
AEM Education and Training. 2021;5:1–4
The authors have no relevant financial information or potential conflicts to disclose.
References
- 1. Brown GM, Lang E, Patel K, et al. A national faculty development needs assessment in emergency medicine. CJEM 2016;18:161–82. [DOI] [PubMed] [Google Scholar]
- 2. Lockyer J, Bursey F, Richardson D, et al. Competency‐based medical education and continuing professional development: a conceptualization for change. Med Teach 2017;39:617–22. [DOI] [PubMed] [Google Scholar]
- 3. Campbell C, Silver I, Sherbino J, Cate OT, Holmboe ES. Competency‐based continuing professional development. Med Teach 2010;32:657–62. [DOI] [PubMed] [Google Scholar]
- 4. Cook DA, Hatala R, Brydges R, et al. Technology‐enhanced simulation for health professions education: a systematic review and meta‐analysis. JAMA 2011;306:978–88. [DOI] [PubMed] [Google Scholar]
- 5. Josey K, Smith ML, Kayani AS, et al. Hospitals with more‐active participation in conducting standardized in‐situ mock codes have improved survival after in‐hospital cardiopulmonary arrest. Resuscitation 2018;133:47–52. [DOI] [PubMed] [Google Scholar]
- 6. Dow AW, Salas E, Mazmanian PE. Improving quality in systems of care: solving complicated challenges with simulation‐based continuing professional development. J Contin Educ Health Prof 2012;32:230–5. [DOI] [PubMed] [Google Scholar]
- 7. Chaplin T, Thoma B, Petrosoniak A, et al. Simulation‐based research in emergency medicine in Canada: priorities and perspectives. CJEM 2020;22:103–111. [DOI] [PubMed] [Google Scholar]
- 8. Forristal C, Russell E, McColl T, et al. Simulation in the continuing professional development of academic emergency physicians: a Canadian national survey. Simul Healthc 2020. [Online ahead of print]. 10.1097/SIH.0000000000000482 [DOI] [PubMed] [Google Scholar]
- 9. Khanduja PK, Bould D, Naik VN, Hladkowicz E, Boet S. The role of simulation in continuing medical education for acute care physicians: a systematic review. Crit Care Med 2015;43:186–93. [DOI] [PubMed] [Google Scholar]
- 10. Weinger MB, Banerjee A, Burden AR, et al. Simulation‐based assessment of the management of critical events by board‐certified anesthesiologists. Anesthesiology 2017;127:475–89. [DOI] [PubMed] [Google Scholar]
- 11. Iitani Y, Tsuda H, Ito Y, et al. Simulation training is useful for shortening the decision‐to‐delivery interval in cases of emergent cesarean section. J Matern Fetal Neonatal Med 2018;31:3128–32. [DOI] [PubMed] [Google Scholar]
- 12. Mastoras G, Poulin C, Norman L, et al. Stress testing the resuscitation room: latent threats to patient safety identified during interprofessional in situ simulation in a Canadian academic emergency department. AEM Educ Train 2020;4:254–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


