Abstract
目的
比较机器人辅助下经皮微创椎弓根螺钉内固定与传统开放内固定治疗胸腰椎骨折的短期疗效。
方法
回顾分析 2018 年 1 月—5 月收治的 52 例无神经损伤症状胸腰椎骨折患者临床资料,根据手术方式不同分为微创组(24 例,采用机器人辅助下经皮微创椎弓根螺钉内固定治疗)和开放组(28 例,采用传统开放内固定治疗)。两组患者性别、年龄、致伤原因、骨折节段、胸腰椎损伤分类和损伤程度评分(TLICS)及术前腰痛视觉模拟评分(VAS)、Oswestry 功能障碍指数(ODI)、固定节段高度及固定节段后凸 Cobb 角等一般资料比较差异均无统计学意义(P>0.05),具有可比性。记录并比较两组患者手术时间、术中出血量、住院时间,以及两组患者术前,术后 3 d、1 个月、6 个月、10 个月腰痛 VAS 评分、ODI 评分、固定节段高度及固定节段后凸 Cobb 角。术后 1~3 d 复查 CT,根据 Gertzbein-Robbins 分类标准判断并计算植钉准确率。
结果
微创组手术时间显著长于开放组,但术中出血量和住院时间均显著短于开放组,差异均有统计学意义(P<0.05)。微创组和开放组分别植入椎弓根螺钉 132 枚和 158 枚,根据 Gertzbein-Robbins 分类标准,植钉准确率分别为 97.7%(129/132)和 96.8%(153/158),比较差异无统计学意义(χ2=0.505,P=0.777)。两组患者均获随访 10 个月,术后均未出现排斥反应、内固定物断裂等情况。微创组于术后 10 个月取出内固定物,开放组不取出。术后各时间点两组腰痛 VAS 评分、ODI 评分、固定节段高度及固定节段后凸 Cobb 角均较术前有不同程度改善(P<0.05)。除术后 3 d 微创组腰痛 VAS 评分和 ODI 评分显著优于开放组(P<0.05)外,其余各时间点各指标两组间比较差异均无统计学意义(P>0.05)。
结论
机器人辅助下经皮微创椎弓根螺钉内固定治疗胸腰椎骨折在术中出血量、住院时间、术后早期临床疗效等方面优势显著,骨折复位效果良好。
Keywords: 机器人, 胸腰椎骨折, 微创, 内固定
Abstract
Objective
To compare short-term effectiveness between robot-guided percutaneous minimally invasive pedicle screw internal fixation and traditional open internal fixation in the treatment of thoracolumbar fractures.
Methods
The clinical data of 52 cases of thoracolumbar fracture without neurological injury symptoms admitted between January 2018 and May 2018 were retrospectively analyzed. According to the different surgical methods, they were divided into minimally invasive group (24 cases, treated with robot-assisted percutaneous minimally invasive pedicle screw internal fixation) and open group (28 cases, treated with traditional open internal fixation). There was no significant difference between the two groups in the general data such as gender, age, cause of injury, fracture segment, thoracolumbar injury classification and severity score (TLICS), preoperative back pain visual analogue scale (VAS) score, Oswestry disability index (ODI) score, fixed segment height, and fixed segment kyphosis Cobb angle (P>0.05). The operation time, intraoperative blood loss, and hospitalization time of the two groups were recorded and compared; as well as the VAS score, ODI score, fixed segment height, and fixed segment kyphosis Cobb angle of the two groups before operation and at 3 days, 1 month, 6 months, and 10 months after operation. CT scan was reexamined at 1-3 days after operation, and the pedicle screw insertion accuracy rate was determined and calculated according to Gertzbein-Robbins classification standard.
Results
The operation time of the minimally invasive group was significantly longer than that of the open group, but the intraoperative blood loss and hospitalization time were significantly shorter than those of the open group (P<0.05). There were 132 pedicle screws and 158 pedicle screws implanted in the minimally invasive group and the open group respectively. According to the Gertzbein-Robbins classification standard, the accuracy of pedicle screws was 97.7% (129/132) and 96.8% (153/158), respectively, showing no significant difference between the two groups (χ2=0.505, P=0.777). The patients in both groups were followed up 10 months, and there was no rejection or internal fixation fracture. In the minimally invasive group, the internal fixator was removed at 10 months after operation, but not in the open group. The VAS score, ODI score, fixed segment heigh, and fixed segment kyphotic Cobb angle of the two groups were improved in different degrees when compared with preoperative ones (P<0.05). Except that the VAS score and ODI score of the minimally invasive group were significantly better than those of the open group at 3 days after operation (P<0.05), there was no significant difference between the two groups at other time points (P>0.05).
Conclusion
Robot-assisted percutaneous minimally invasive pedicle screw internal fixation for thoracolumbar fractures has significant advantages in intraoperative blood loss, hospitalization time, and early postoperative effectiveness and other aspects, and the effect of fracture reduction is good.
Keywords: Robot, thoracolumbar fracture, minimally invasive, internal fixation
胸腰椎骨折可导致椎体塌陷、破裂、脊柱失稳、脊髓损伤,后路椎弓根螺钉内固定术是治疗胸腰椎骨折的主流术式。近年来,脊柱微创理念逐渐被应用于经皮椎弓根螺钉内固定治疗无神经损伤的胸腰椎骨折中。我院自 2017 年 9 月开始使用我国自主研发的“天玑”第 3 代骨科机器人辅助脊柱内固定手术,治疗无神经损伤的胸腰椎骨折患者。现回顾分析 2018 年 1 月—5 月我院采用机器人辅助下经皮微创椎弓根螺钉内固定与传统开放内固定治疗的无神经损伤症状胸腰椎骨折患者临床资料,比较二者的短期疗效。报告如下。
1. 临床资料
1.1. 患者选择标准
纳入标准:① T10~L2 单节段新鲜骨折;② 胸腰椎损伤分类和损伤程度评分(TLICS)≥4 分且患者及家属要求手术治疗;③ AO 分型为 A 型,符合脊柱内固定手术指征且无神经损伤症状。排除标准:① 肿瘤性或重度骨质疏松患者;② 资料不全或难以配合诊治者。2018 年 1 月—5 月共 52 例患者符合选择标准纳入研究,根据手术方式不同分为微创组(24 例,采用机器人辅助下经皮微创椎弓根螺钉内固定治疗)和开放组(28 例,采用传统开放内固定治疗)。
1.2. 一般资料
微创组:男 11 例,女 13 例;年龄 25~68 岁,平均 57.5 岁。致伤原因:高处坠落伤 13 例,交通事故伤 6 例,跌倒伤 5 例。骨折节段:T10 3 例,T11 5 例,T12 9 例,L1 4 例,L2 3 例。TLICS 评分 4 分 17 例,5 分 7 例。
开放组:男 13 例,女 15 例;年龄 29~66 岁,平均 56.9 岁。致伤原因:高处坠落伤 15 例,交通事故伤 8 例,跌倒伤 5 例。骨折节段:T10 2 例,T11 6 例,T12 12 例,L1 5 例,L2 3 例。TLICS 评分 4 分 19 例,5 分 9 例。
两组患者术前影像学检查提示均为椎体骨折,伴有后柱韧带复合体损伤等。两组患者性别、年龄、致伤原因、骨折节段、TLICS 评分及术前腰痛视觉模拟评分(VAS)、Oswestry 功能障碍指数(ODI)、固定节段高度及固定节段后凸 Cobb 角等一般资料比较差异均无统计学意义(P>0.05),具有可比性。见表 1~4。
表 1.
Comparison of VAS score between the two groups before and after operation (
 )
)
两组患者手术前后 VAS 评分比较(
 )
)
| 组别
Group |
例数
n |
术前
Preoperative |
术后 3 d
Postoperative at 3 days |
术后 1 个月
Postoperative at 1 month |
术后 6 个月
Postoperative at 6 months |
术后 10 个月
Postoperative at 10 months |
统计值
Statistic |
|
*与术前比较P<0.05
*Compared with preoperative value,P<0.05 | |||||||
| 微创组
Minimally invasive group |
24 | 5.2±1.2 | 3.1±0.8* | 1.3±0.5* | 0.9±0.6* | 0.6±0.7* |
F=114.498
P=0.000 |
| 开放组
Traditional group |
28 | 5.8±1.4 | 4.1±1.2* | 1.2±0.6* | 0.8±0.5* | 0.7±0.8* |
F=195.658
P=0.000 |
| 统计值
Statistic |
t=–0.632
P=0.470 |
t=–1.951
P=0.028 |
t=0.832
P=0.331 |
t=0.765
P=0.372 |
t=–0.185
P=0.832 |
||
表 4.
Comparison of fixed segment kyphosis Cobb angle between the two groups before and after operation (
 , °)
, °)
两组患者手术前后固定节段后凸 Cobb 角比较(
 ,°)
,°)
| 组别
Group |
例数
n |
术前
Preoperative |
术后 3 d
Postoperative at 3 days |
术后 1 个月
Postoperative at 1 month |
术后 6 个月
Postoperative at 6 months |
术后 10 个月
Postoperative at 10 months |
统计值
Statistic |
|
*与术前比较P<0.05
*Compared with preoperative value,P<0.05 | |||||||
| 微创组
Minimally invasive group |
24 | 7.5±1.1 | –3.9±0.6* | –4.0±0.3* | –3.9±0.7* | –4.0±0.5* |
F=2 296.354
P=0.000 |
| 开放组
Traditional group |
28 | 7.9±0.9 | –4.2±0.8* | –4.1±0.7* | –4.1±0.8* | –4.2±0.6* |
F=2 591.522
P=0.000 |
| 统计值
Statistic |
t=–1.053
P=0.152 |
t=1.332
P=0.102 |
t=0.463
P=0.632 |
t=0.598
P=0.415 |
t=0.521
P=0.496 |
||
表 2.
Comparison of ODI score between the two groups before and after operation (
 )
)
两组患者手术前后 ODI 评分比较(
 )
)
| 组别
Group |
例数
n |
术前
Preoperative |
术后 3 d
Postoperative at 3 days |
术后 1 个月
Postoperative at 1 month |
术后 6 个月
Postoperative at 6 months |
术后 10 个月
Postoperative at 10 months |
统计值
Statistic |
|
*与术前比较P<0.05
*Compared with preoperative value,P<0.05 | |||||||
| 微创组
Minimally invasive group |
24 | 63.9±13.7 | 18.1±4.0* | 8.9±2.4* | 8.2±3.5* | 9.0±3.2* |
F=241.510
P=0.000 |
| 开放组
Traditional group |
28 | 65.6±14.5 | 25.6±5.5* | 9.1±1.4* | 9.2±2.5* | 9.4±2.7* |
F=235.669
P=0.000 |
| 统计值
Statistic |
t=–0.169
P=0.856 |
t=–2.963
P=0.003 |
t=–0.431
P=0.624 |
t=–0.405
P=0.651 |
t=–0.357
P=0.697 |
||
表 3.
Comparison of fixed segment height between the two groups before and after operation (
 , mm)
, mm)
两组患者手术前后固定节段高度比较(
 ,mm)
,mm)
| 组别
Group |
例数
n |
术前
Preoperative |
术后 3 d
Postoperative at 3 days |
术后 1 个月
Postoperative at 1 month |
术后 6 个月
Postoperative at 6 months |
术后 10 个月
Postoperative at 10 months |
统计值
Statistic |
|
*与术前比较P<0.05
*Compared with preoperative value,P<0.05 | |||||||
| 微创组
Minimally invasive group |
24 | 40.8±2.2 | 48.1±1.9* | 47.9±2.1* | 48.3±1.8* | 48.2±2.2* |
F=35.614
P=0.000 |
| 开放组
Traditional group |
28 | 40.6±3.2 | 49.1±2.2* | 49.3±3.2* | 49.5±2.6* | 49.3±2.9* |
F=38.916
P=0.000 |
| 统计值
Statistic |
t=0.536
P=0.362 |
t=–0.843
P=0.141 |
t=–0.967
P=0.102 |
t=–0.395
P=0.203 |
t=–0.351
P=0.195 |
||
1.3. 治疗方法
1.3.1. 主要材料
微创组使用我国自主研发的“天玑”第 3 代骨科机器人辅助手术,该系统由机械臂系统、光学跟踪系统、手术规划系统以及导航系统等构成。其中 18 例采用 LontC 矫形脊柱内固定系统(常州鼎健医疗器械有限公司)经伤椎固定,6 例采用提拉复位脊柱内固定系统 CD HORIZON SEXTANT Ⅱ System(美敦力公司,美国)跨伤椎固定。开放组均采用 VALEN 矫形脊柱内固定系统(常州鼎健医疗器械有限公司)经伤椎固定。内固定材料材质均为 Ti-6AI-4V 钛合金材料,包括椎弓根螺钉、预弯钛棒及螺塞 3 部分组成,具有强度高、组织相容性好等优点。
1.3.2. 手术方法
患者于气管插管全麻后取俯卧位,采用脊柱外科专用手术床。开放组:C 臂 X 线机定位拟行内固定椎体的椎弓根体表位置并标记后,用尖刀切开皮肤 10 cm,逐层切开腰背筋膜,钝性分离肌间隙至关节突外缘。均固定伤椎及伤椎上下椎体,注意避免损伤关节囊,植入螺钉(术前评估有 10 处伤椎椎弓根已存在破裂,不予以植钉)。正侧位 X 线透视确认螺钉位置无误后,选择合适长度的固定钛棒安装,使用撑开器撑开复位。C 臂 X 线机透视复位满意,锁紧螺钉并固定,予以椎板间异体骨(湖北联结生物材料有限公司)植骨,安置引流管,逐层缝合。
微创组:C 臂 X 线机定位骨折椎体,在需植钉椎体的上位椎体棘突处作一长约 1 cm 切口,切开筋膜,显露棘突,在棘突上安装示踪器。准备机器人系统,安装定位标尺,三维 C 臂扫描需固定的节段,其中 18 例经伤椎固定,6 例跨伤椎固定。将数据传输至机器人工作站,进行定位规划,规划完毕后下达指令,机械臂运行至指定位置;在机械臂定位下作 3 cm 小切口,钝性分离,使用电钻置入导针;透视确认位置无误后拧入椎弓根螺钉,C 臂 X 线机透视确定椎弓根螺钉位置良好,选择合适长度的固定棒安装于置棒器上,将固定棒置入上、下椎弓根螺钉尾槽中,依次拧入固定螺帽;撑开器撑开复位后旋紧,C 臂 X 线机透视复位满意,锁紧螺钉并固定,逐层缝合。
1.4. 术后处理及随访指标
术后根据患者病情给予抗菌药物 1~3 d,及常规术后预防感染、镇痛、预防皮肤褥疮、功能锻炼等治疗。微创组术后第 2 天可佩带支具下床活动,开放组 3~4 d 拔出引流管后佩戴支具下床活动,支具佩戴时间为 3~6 个月。
记录并比较两组患者手术时间、术中出血量、住院时间、椎弓根螺钉植入准确率;以及两组患者术前,术后 3 d、1 个月、6 个月、10 个月腰痛 VAS 评分、ODI 评分、固定节段高度及固定节段后凸 Cobb 角。术后 1~3 d 复查 CT,椎弓根螺钉植入准确性根据 Gertzbein-Robbins 分类标准[1],评估在外侧、内侧、头侧和尾侧 4 个方向上椎弓根螺钉是否存在穿透骨皮质的情况。具体标准:A 类,无皮质侵及;B 类,皮质穿透<2 mm;C 类,2 mm≤皮质穿透<4 mm;D 类,4 mm≤皮质穿透<6 mm;E 类,皮质穿透≥6 mm。植钉准确率=(A 类+B 类螺钉数量)/组内全部植入螺钉数量×100%。
1.5. 统计学方法
采用 SPSS22.0 统计软件进行分析。计量资料以均数±标准差表示,组内手术前后比较采用单因素方差分析,两两比较采用 LSD 检验,两组间比较采用独立样本 t 检验;计数资料组间比较采用 χ2 检验;检验水准 α=0.05。
2. 结果
微创组手术时间显著长于开放组,但术中出血量和住院时间均显著短于开放组,差异均有统计学意义(P<0.05)。见表 5。微创组共植入椎弓根螺钉 132 枚,根据 Gertzbein-Robbins 分类标准,A 类 124 枚、B 类 5 枚、C 类 3 枚,植钉准确率为 97.7%;开放组共植入椎弓根螺钉 158 枚,其中 A 类 145 枚、B 类 8 枚、C 类 5 枚,植钉准确率 96.8%;两组植钉准确率比较差异无统计学意义(χ2=0.505,P=0.777)。
表 5.
Comparison of operation time, intraoperative blood loss, and hospitalization time between the two groups (
 )
)
两组患者手术时间、术中出血量、住院时间比较(
 )
)
| 组别
Group |
例数
n |
手术时间(min)
Operation time (minutes) |
术中出血量(mL)
Intraoperative blood loss (mL) |
住院时间(d)
Hospitalization time (days) |
| 微创组
Minimally invasive group |
24 | 130±21 | 30±6 | 3.4±0.3 |
| 开放组
Traditional group |
28 | 110±18 | 130±23 | 6.5±1.2 |
| 统计值
Statistic |
t=3.872
P=0.004 |
t=–9.685
P=0.000 |
t=–4.362
P=0.009 |
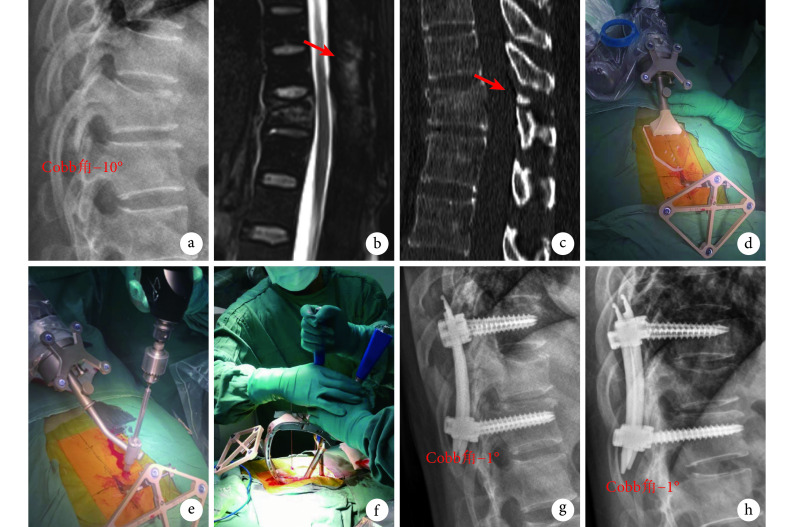
两组患者均获随访 10 个月,术后均未出现排斥反应、内固定物断裂等情况。微创组于术后 10 个月取出内固定物,开放组不取出。术后各时间点两组腰痛 VAS 评分、ODI 评分、固定节段高度及固定节段后凸 Cobb 角均较术前有不同程度改善,差异均有统计学意义(P<0.05)。除术后 3 d 微创组腰痛 VAS 评分和 ODI 评分显著优于开放组,差异有统计学意义(P<0.05)外,其余各时间点各指标两组间比较差异均无统计学意义(P>0.05)。见表 1~4,图 1。
图 1.
A 48-year-old female patient with T11 vertebral compression fracture and posterior ligamentous complex injury by traffic accident injury in minimally invasive group
微创组患者,女,48 岁,交通事故伤致 T11 椎体压缩性骨折伴后柱韧带复合体损伤
a. 术前侧位 X 线片;b. 术前 MRI 示后柱韧带复合体损伤(箭头);c. 术前 CT 示 T11 椎板骨折(箭头);d. 在 T10 棘突上安装示踪器及定位标尺;e. 机器人辅助定位下植入导针;f. 植入空心椎弓根螺钉和钛棒;g. 术后 3 d 侧位 X 线片示椎间高度及后凸 Cobb 角复位良好;h. 术后 10 个月侧位 X 线片示椎间高度及后凸 Cobb 角维持良好
a. Preoperative lateral X-ray film; b. Preoperative MRI, showed posterior ligamentous complex injury (arrow); c. Preoperative CT scan, showed laminar fracture of T11 (arrow); d. Tracer and positioning ruler were installed on the spinous process of T10; e. Inserting guide wire with robot-assisted; f. Implanting cannulated pedicle screw and titanium rod; g. Lateral X-ray film at 3 days after operation, showed the segment height and Cobb angle of segment kyphosis were well recovered; h. Lateral X-ray film at 10 months after operation, showed the segment height and Cobb angle of segment kyphosis were well maintained
3. 讨论
胸腰段在脊柱节段内承担着非常重要的生物学应力,这也是胸腰椎骨折发病率较高的主要原因之一。前路手术因具有能为硬脊膜前方减压、清理伤椎碎骨片等优势,在既往治疗中应用广泛;但随后发现其存在手术时间较长,易损伤前路血管以及胸腔、腹腔脏器的问题,应用逐渐减少[2]。传统后路手术提供了三柱固定,对于后方复合损伤的患者提供了更加稳定的固定强度;但在显露过程中对椎旁肌的损伤比较严重,术后硬膜瘢痕形成,可能存在长期腰背部疼痛。近年,微创外科技术得到迅速发展,具有损伤小、恢复快的特点。微创经皮植钉技术是脊柱外科新发展起来用于治疗胸腰椎骨折的微创技术,主要包括 C 臂透视辅助下微创经皮植钉技术[3-7]、导航系统辅助技术[8]以及骨科机器人辅助技术[7,9-23]等。
骨科手术机器人作为先进技术的集成产物,具有灵敏度高、定位准确、运行平稳、学习曲线短等优点。“天玑”第 3 代骨科机器人是一种基于三维图像进行空间映射和路径规划的定位系统,该系统具有主动定位和人机协同运动的功能,可实现内固定物按预定的理想路径获得精确固定,提高手术疗效。本研究结果显示,“天玑”骨科机器人系统辅助经皮微创椎弓根螺钉植入的准确率为 97.7%,与杨俊松等[7]报道相似。Kantelhardt 等[9]对 112 例患者的 536 枚椎弓根螺钉进行对照分析,发现机器人辅助下螺钉植入的准确率为 94.5%,开放徒手植钉组为 91.4%,与其他文献报道类似[10-15]。Kim 等[16]研究指出微创机器人辅助与开放徒手植钉准确性无明显差异,但机器人辅助组进针点偏外,内倾角度大于开放组。当植钉内倾角度增大时,有利于保护关节囊,具有更强的把持力[24-25]。
除植钉准确率外,相关文献还指出骨科手术机器人在手术医生接触辐射、出血量、疼痛反应、康复方面具有更明显的优势[19-25]。Schatlo 等[19]研究发现与传统开放手术相比,机器人组患者能减少手术时间、术中出血量以及止痛药物使用时间,与 Takahashi 等[20]的报道结果相似。Roser 等[21]研究表明,机器人辅助植入椎弓根螺钉较 C 臂 X 线机透视辅助的放射线暴露时间减少了近 50%。本研究中微创组手术时间高于开放组,可能与初次接触机器人辅助系统,需要一定学习曲线有关。但在术中出血量、住院时间及术后早期腰痛 VAS 评分、ODI 评分改善方面,微创组具有明显优势。
查阅既往文献,对于机器人辅助下胸腰椎骨折复位效果的评价较少。本研究中胸腰椎 X 线片测量显示,术后两组患者固定节段高度及后凸 Cobb 角均较术前明显改善(P<0.05),微创组术后固定节段高度及后凸 Cobb 角稍低于开放组,但两组比较差异均无统计学意义(P>0.05)。微创组复位效果稍差的原因主要有两点可能:① 经伤椎固定的 18 例患者使用的手术复位器械需要改进,复位器械与螺钉尾部延长杆的接触面过大,撑开受力点在延长杆尾部,因此复位效果可能受到影响;② 跨伤椎固定的 6 例患者可能缺少伤椎固定螺钉,因此伤椎后向腹侧的复位力量较弱。
综上述,“天玑”第 3 代骨科机器人系统在经皮微创椎弓根螺钉内固定治疗胸腰椎骨折中,植钉准确性高,能减少术中出血量,减少术后早期疼痛,达到快速康复的目标。随着机器人手术配套工具的改进,相信今后能达到更好的复位效果。
作者贡献:林书负责数据收集、整理、统计分析、文章撰写等;胡豇、万仑、唐六一负责科研设计、既往研究成果收集;王跃、俞阳、张伟负责文章整体设计与内容修改、审阅。
利益冲突:所有作者声明,在课题研究和文章撰写过程中不存在利益冲突。课题经费支持没有影响文章观点和对研究数据客观结果的统计分析及其报道。
机构伦理问题:研究方案经四川省人民医院医学伦理委员会批准[伦审(研)2019 年第 298 号]。
Funding Statement
四川省科技厅科技支撑项目(2019YFS0268)
References
- 1.Goz V, Weinreb JH, McCarthy I, et al Perioperative complications and mortality after spinal fusions: analysis of trends and risk factors. Spine (Phila Pa 1976) 2013;38(22):1970–1976. doi: 10.1097/BRS.0b013e3182a62527. [DOI] [PubMed] [Google Scholar]
- 2.Marcus HJ, Cundy TP, Nandi D, et al Robot-assisted and fluoroscopy-guided pedicle screw placement: a systematic review. Eur Spine J. 2014;23(2):291–297. doi: 10.1007/s00586-013-2879-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herren C, Reijnen M, Pishnamaz M, et al Incidence and risk factors for facet joint violation in open versus minimally invasive procedures during pedicle screw placement in patients with trauma. World Neurosurg. 2018;112:e711–e718. doi: 10.1016/j.wneu.2018.01.138. [DOI] [PubMed] [Google Scholar]
- 4.Hyun SJ, Kim KJ, Jahng TA, et al Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine (Phila Pa 1976) 2017;42(6):353–358. doi: 10.1097/BRS.0000000000001778. [DOI] [PubMed] [Google Scholar]
- 5.钟睿, 王润生, 刘建恒, 等 不同入路微创经椎间孔腰椎间融合术治疗单节段腰椎管狭窄症的疗效比较. 中国修复重建外科杂志. 2019;33(7):807–813. doi: 10.7507/1002-1892.201903096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gelalis ID, Paschos NK, Pakos EE, et al Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques . Eur Spine J. 2012;21(2):247–255. doi: 10.1007/s00586-011-2011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.杨俊松, 郝定均, 刘团江, 等 脊柱机器人与透视辅助下经皮植钉治疗腰椎滑脱症中植钉精度的对比研究. 中国修复重建外科杂志. 2018;32(11):1371–1376. [Google Scholar]
- 8.Fichtner J, Hofmann N, Rienmüller A, et al Revision rate of misplaced pedicle screws of the thoracolumbar spine-comparison of three-dimensional fluoroscopy navigation with freehand placement: a systematic analysis and review of the literature. World Neurosurgery. 2018;109:e24–e32. doi: 10.1016/j.wneu.2017.09.091. [DOI] [PubMed] [Google Scholar]
- 9.Kantelhardt SR, Martinez R, Baerwinkel S, et al Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J. 2011;20(6):860–868. doi: 10.1007/s00586-011-1729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laudato PA, Pierzchala K, Schizas C Pedicle screw insertion accuracy using O-Arm, robotic guidance or freehand technique: a comparative study. Spine (Phila Pa 1976) 2018;43(6):E373–E378. doi: 10.1097/BRS.0000000000002449. [DOI] [PubMed] [Google Scholar]
- 11.Joseph JR, Smith BW, Liu X, et al Current applications of robotics in spine surgery: a systematic review of the literature. Neuro-surgical Focus. 2017;42(5):E2. doi: 10.3171/2017.2.FOCUS16544. [DOI] [PubMed] [Google Scholar]
- 12.Schröder ML, Staartjes VE Revisions for screw malposition and clinical outcomes after robot-guided lumbar fusion for spondylolisthesis. Neurosurgical Focus. 2017;42(5):E12. doi: 10.3171/2017.3.FOCUS16534. [DOI] [PubMed] [Google Scholar]
- 13.Molliqaj G, Schatlo B, Alaid A, et al Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus. 2017;42(5):E14. doi: 10.3171/2017.3.FOCUS179. [DOI] [PubMed] [Google Scholar]
- 14.Yu L, Chen X, Margalit A, et al Robot-assisted vs freehand pedicle screw fixation in spine surgery-a systematic review and a meta analysis of comparative studies . Int J Med Robot. 2018;14(3):e1892. doi: 10.1002/rcs.1892. [DOI] [PubMed] [Google Scholar]
- 15.Keric N, Eum DJ, Afghanyar F, et al Evaluation of surgical strategy of conventional vs percutaneous robot-assisted spinal transpedicular instrumentation in spondylodiscitis . J Robot Surg. 2017;11(1):17–25. doi: 10.1007/s11701-016-0597-5. [DOI] [PubMed] [Google Scholar]
- 16.Kim HJ, Jung WI, Chang BS, et al A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery . Int J Med Robot. 2017;13(3) doi: 10.1002/rcs.1779. [DOI] [PubMed] [Google Scholar]
- 17.Archavlis E, Amr N, Kantelhardt SR, et al Rates of upper facet joint violation in minimally invasive percutaneous and open instrumentation: a comparative cohort study of different insertion techniques. J Neurol Surg A Cent Eur Neurosurg. 2018;79(1):1–8. doi: 10.1055/s-0037-1603631. [DOI] [PubMed] [Google Scholar]
- 18.Teles AR, Paci M, Gutman G, et al Anatomical and technical factors associated with superior facet joint violation in lumbar fusion. J Neurosurg Spine. 2018;28(2):173–180. doi: 10.3171/2017.6.SPINE17130. [DOI] [PubMed] [Google Scholar]
- 19.Schatlo B, Molliqaj G, Cuvinciuc V, et al Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine. 2014;20(6):636–643. doi: 10.3171/2014.3.SPINE13714. [DOI] [PubMed] [Google Scholar]
- 20.Takahashi J, Hirabayashi H, Hashidate H, et al Accuracy of multilevel registration in image-guided pedicle screw insertion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35(3):347–352. doi: 10.1097/BRS.0b013e3181b77f0a. [DOI] [PubMed] [Google Scholar]
- 21.Roser F, Tatagiba M, Maier G Spinal robotics: current applications and future perspectives. Neurosurgery. 2013;72(Suppl 1):12–18. doi: 10.1227/NEU.0b013e318270d02c. [DOI] [PubMed] [Google Scholar]
- 22.Solomiichuk V, Fleischhammer J, Molliqaj G, et al Robotic versus fluoroscopy-guided pedicle screw insertion for metastatic spinal disease: a matched-cohort comparison. Neurosurg Focus. 2017;42(5):E13. doi: 10.3171/2017.3.FOCUS1710. [DOI] [PubMed] [Google Scholar]
- 23.Park SM, Kim HJ, Lee SY, et al Radiographic and clinical outcomes of Robot-Assisted posterior pedicle screw fixation: Two-Year results from a randomized controlled trial. Yonsei Med J. 2018;59(3):438–444. doi: 10.3349/ymj.2018.59.3.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsai TH, Tzou RD, Su YF, et al Pedicle screw placement accuracy of bone-mounted miniature robot system. Medicine. 2017;96(3):e5835. doi: 10.1097/MD.0000000000005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han X, Tian W, Liu Y, et al Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. 2019:1–8. doi: 10.3171/2018.10.SPINE18487. [DOI] [PubMed] [Google Scholar]