Abstract
Using six waves of data from the Panel Study of Income Dynamics (2007–2017) and the Childhood Retrospective Circumstances Study (2014) (n=3,240), this paper estimates how childhood experiences with parental mental health problems shape trajectories of children’s own distress in adulthood. Findings indicate that those who experience poor parental mental health have consistently greater distress than their non-exposed counterparts throughout adulthood. More severe and longer exposures to parental mental health problems corresponds to even greater distress in adulthood. The gender of the parent afflicted does not predict differences in adult mental health, but those individuals exposed to both maternal and paternal poor mental health have the greatest distress in adulthood. Together, results suggest that parental mental health during children’s formative years is a significant predictor of life course distress and that heterogeneity in this experience corresponds to unique mental health trajectories.
The outcomes of children who are exposed to parental mental health problems are of growing concern as recent research estimates that 18.2 percent of parents suffer from mental illness and 3.8 percent of parents suffer from serious mental illness (Stambaugh et al. 2017). Parents’ psychological problems may lead to negative parenting behaviors, lack of attention to children’s needs, or increased dysfunction within the home (Elgar et al. 2007; Wilson and Durbin 2010). As such, mothers’ and fathers’ mental health problems are key sources of stress for children and have been linked to worse mental health and more behavioral problems for children during their youth (Meadows, McLanahan, and Brooks-Gunn 2007; Schepman et al. 2011)
Life course scholars have long suggested that negative events in childhood may be associated with poor health throughout the life course (Elder 1998; Ferraro and Wilkinson 2013; Pearlin 2010). Stress process literature has likewise suggested that current stress may be fundamentally linked to experiences with past stressors (Aneshensel 2015). However, research in both of these frameworks has highlighted that the link between early life stress and later stage mental health is not deterministic and that the impact of these stressors may, in fact, wane across the life course (George 2013). Although much is known about the consequences of parental mental health problems on children during childhood, a key question remains how this childhood stressor continues to negatively impact children’s mental health as they age throughout adulthood.
The current study contributes to research on early life exposures and mental health in several ways. First, by drawing on the stress process model and the life course perspective, I conceptualize parental mental health problems as a stressor with long-term consequences for children’s distress. Second, I use a large, nationally representative panel data set that includes measurements of children’s distress as adults over six waves to construct age-based mental health trajectories. This strategy allows for a dynamic understanding of how the impact of poor parental mental health influences children’s baseline and growth of distress across adulthood. Furthermore, although research on other adverse childhood circumstances has emphasized that experiences with adversity may differ across individuals (Friedman et al. 2015; Schilling, Aseltine, and Gore 2008), few studies have questioned whether heterogeneity in the experience with parental mental problems corresponds with different long-term consequences for children once they reach adulthood. Therefore, I extend prior work that typically treats the presence of poor parental mental health dichotomously (was present/ was not present in childhood) by refining the measurement of parental mental health to include the severity of the mental health problems, the duration for which the individual was exposed to this particular stressor in childhood, and the gender of the parent with mental health problems. In doing so, this study clarifies which experiences with parental mental health are particularly harmful to children’s life course outcomes.
BACKGROUND
Linking Parental Mental Health Problems with Life Course Mental Health
Early life is a crucial period of biological, emotional, and mental development. The plasticity of this period makes individuals extremely vulnerable to the impact of stressors and has therefore been referred to as a sensitive period (McFarland 2017; Miller, Chen, and Parker 2011). Parental mental health problems may act as a stressor for children during a sensitive period because parents are central to the lives of their children and provide an essential source of social control, self-esteem, and belonging (Schepman et al. 2011; Umberson, Crosnoe, and Reczek 2010; Wilkinson and Andersson 2019). Mothers and fathers with mental health problems may display impaired parenting behaviors such as harshness or disengagement from the children’s needs (Elgar et al. 2007; Wilson and Durbin 2010). These behaviors, in turn, can lead to a range of deleterious emotions for children including, but not limited to, insecurity and distress (Cummings, Mark, Keller, and Davies 2005; Elgar et al. 2007; Noonan, Burns, and Violato 2018; Wilson and Durbin 2010). In addition to parenting behaviors, parents’ mental health could lead to other sources of stressful family dysfunction, such as increased marital conflict, parental abuse of drugs/alcohol, or parental divorce that may add to children’s distress (Avison 2010; Hanington et al. 2012; Williams and Cheadle 2016). Although research has predominantly focused on the impact of this stressor on children in early life, the consequences of parents’ psychological problems may extend past this window.
Both the stress process model and the life course perspective have highlighted that stress during a sensitive period can lead to worse health outcomes for individuals throughout their lives and into adulthood (Kuh et al. 2003; Pearlin 2010). Although literature on the long term consequences of childhood circumstances was originally developed to explain differences in adult physical health outcomes, this literature is often extended to explain disparate adult mental health outcomes (Aneshensel 2015; Avison 2010; George 2013). This research suggests that childhood misfortune may define starting points of adult mental health (Avison 2010; Pearlin 2010), as well as the growth of distress with age (Schafer and Ferraro 2013).
First, childhood stressors may have an enduring influence on mental health over the life course that remains stable across age (Schafer and Ferraro 2013; Umberson et al. 2014). Consequently, those exposed to childhood adversity may have consistently higher distress than their non-exposed counterparts throughout adulthood. Second, childhood adversity may lead to mounting distress with age (Ferraro and Shippee 2009; Umberson et al. 2014). This may be due to a compounding of depressive or anxious symptomatology throughout the life course or through the accumulation of related stressors that further worsen adult health (Ferraro and Shippee 2009; Ferraro and Wilkinson 2013; George 2013; Umberson et al. 2014). Thus, in addition to higher baseline distress, individuals exposed to childhood stressors may have increasingly worse mental health compared to their non-exposed peers with age. Finally, research suggests that childhood stressors may only be relevant for children’s health early in the life course and that the impact of childhood stressors wanes as individuals age (Oldehinkel et al. 2014; Schaan 2014; Schafer and Ferraro 2013). Therefore, individuals exposed to childhood misfortune may experience initial increases in distress, but eventually, converge to mirror the mental health of their non-exposed counterparts.
The few studies that have analyzed the long-term impact of parental mental health problems have concluded that exposure to this stressor is related to children’s poor adult mental health (Angelini et al. 2016; Goosby 2013). However, these studies have only assessed children’s adult mental health at one point in time. In doing so, they have been unable to assess how this childhood stressor shapes mental health trajectories across adulthood (Schafer and Ferraro 2013). Thus, it remains unclear whether the gap in distress between those exposed to parental mental health problems and those not exposed to this stressor remains stable, increases, or wanes across adulthood.
Heterogeneity in Parental Mental Health Problems
Of growing concern in the study of childhood adversity is how heterogeneity in these experiences corresponds to variation in both child (Strohschein and Gauthier 2018) and adult health outcomes (Friedman et al. 2015; Schilling et al. 2008). It is likewise imperative to recognize that not all experiences with parental mental health problems are comparable. The stress placed on children during the sensitive period may be a product of key characteristics of poor parental mental health. For example, the severity of maternal psychological problems calculated through the Delusions-Symptoms-States Inventory (DSSI) has been positively correlated with children’s increased depressive symptoms and behavioral problems in early life (Brennan et al. 2000; Hammen and Brennan 2003). Mars and colleagues (2012) likewise noted that severe parental depression, as measured through impairment in everyday activities and hospitalization, was predictive of children’s increased depressive symptoms. Conversely, the absence of negative emotional expressiveness (less severe presentation of mental health problems) has been found to diminish the impact that parental depression has on children in their youth (Cummings, Cheung, and Davies 2013). Thus, more severe experiences with parental mental health problems may predict even greater distress in adulthood.
In addition to severity, the duration of exposure to poor parental mental health may predict the stress placed on children. This is a particularly salient source of heterogeneity given that some psychological problems last only for a short while and may not occur again for many years, if at all (Coryell et al. 1994). Children who are exposed to poor parental mental health for most of their youth may find it particularly difficult to escape the negative consequences compared to those who only experience this stressor for a brief period (George 2014).
Finally, experiences with parental mental health may differ based on the gender of the parent afflicted. Women are generally more likely to display depressive symptoms, and mothers are expected to be more directly involved as the predominant caretaker compared to fathers (Moser and Jacob 1997; Rosenfield and Mouzon 2013). Maternal mental health problems may, therefore, cause greater stress for a child and lead to greater disruption of the childhood environment (Connell and Goodman 2002). Indeed, multiple studies have noted that poor maternal mental health is more detrimental to children’s outcomes than poor paternal mental health (Meadows et al. 2007; Noonan et al. 2018) and that maternal depression is more predictive of family stress, such as economic hardship, than paternal depression (Williams and Cheadle 2016). Consequently, maternal psychological problems may also confer the greatest long-term risk to children’s distress. However, it should be noted that many of the studies that examine the gender of the parent afflicted note that having both a mother and a father with mental health problems, as opposed to only one parent afflicted, is the most stressful circumstance for a child. These studies largely suggest that having a least one non-afflicted parent in the home may buffer the effects of parental mental health problems, no matter if the afflicted parent is the mother or the father (Kahn, Brandt, and Whitaker 2004; Meadows et al. 2007).
The Present Study
Past work has linked exposure to poor parental mental health in early life to children’s distress in adulthood. However, these studies have been unable to assess how this stressor impacts children’s mental health trajectories over multiple years of adulthood. Furthermore, little work has analyzed how heterogeneity in the experience with parental mental health problems may relate to disparate outcomes for children in adulthood. The goal of this study is to build on existing work to examine (1) how exposure to parental mental health problems during a sensitive period shapes children’s baseline and growth of distress throughout adulthood, and (2) if differences in the severity of this experience, the duration exposed to poor parental mental health, and the gender of the afflicted parent correspond to differences in adult distress trajectories.
METHODS
Data
The data for this study comes from six waves (2007–2017) of the Panel Study of Income Dynamic (PSID). The PSID is an ongoing nationally representative sample of U.S. households. The original PSID was collected annually beginning in 1968 with a sample of over 5,000 households. Since 1997, the survey has been collected biannually (McGonagle and Freedman 2015). In 2014, the PSID included a Childhood Retrospective Circumstances Study (CRCS) supplement that was given to a sample of household heads and spouses/partners from PSID families that participated in the 2013 wave. The purpose of the CRCS was to supplement information on adult respondents’ childhood experiences that were not captured in the main PSID interview (McGonagle and Freedman 2015). Thus, the CRCS is uniquely suited for answering questions on the long-term impacts of childhood experiences on adult mental health.
The present analysis focuses on adult respondents who were at least 25 years old at the 2007 wave of the PSID and no older than 65 at the 2017 wave. This age range captures individuals through early to mid-adulthood. Only the main respondent of a PSID household was asked to provide information on his/her psychological distress. Consequently, the present analysis focuses solely on respondents who participated in the CRCS and who also provided information on their psychological distress in adulthood in at least one wave (n=3,240). The total sample is mostly female (62.93 percent) and white (61.23 percent). This demographic breakdown mirrors that of the main respondents in the PSID over the waves used in analyses.
Measures
Adult Mental Health
Adult mental health is measured using the K-6 Non-Specific Psychological Distress Scale at each wave of analysis. This scale is a shortened version of the K-10 scale originally developed by Kessler and colleagues (2003) and measures how often the respondent felt nervous, hopeless, restless/fidgety, that everything was an effort, so sad that nothing could cheer him/her up, and/or worthless in the past 4 weeks. Response categories include “none,” “a little,” “some,” “most,” and “all.” Scores on each item are summed to produce a scale ranging from 0 to 24. Since the majority of respondents score very low on the K-6 scale, distress scores were logged to address skew (i.e. ln(“K-6” +1)).
Parental Mental Health Problems
Prior to answering any questions on childhood experiences with parental mental health problems, respondents were asked to identify one mother figure and one father figure with whom they spent the majority of their childhood. Although this figure was often the biological parent, this figure could also be a stepparent, an adoptive parent, another relative, or a non-relative who still took on a role as a “mother” or “father” figure. The majority of respondents (75.19 percent) indicated their father figure was their biological father and a majority (93.09 percent) indicated their mother figure was their biological mother. All questions asked about respondents’ parents during this time refer to the persons whom they indicated were their main parental figures.
The presence of parental mental health problems in childhood is indicated by the presence of anxiety and/or depression in either parental figure. Respondents were asked whether, before they were 17, their “mother/stepmother/woman who raised R” experienced “periods lasting 2 or more weeks where she was sad or depressed for most of the time.” They were also asked whether the woman who raised them, “ever had anxiety attacks where all of a sudden she felt frightened, anxious, or panicky.” The same two questions were asked about the respondent’s “father/stepfather/ man who raised R.” Parental mental health problems were coded “1” if a respondent answered yes to any of the above experiences. The PSID did not begin collecting information about respondent’s psychological distress until 2001 (and not consistently until 2007), therefore prospective information on parent’s mental health while the respondent was under the age of 17 could not be ascertained.
Severity
The severity of parental mental health problems is captured through an index of the number of additional indicators of parental mental health problems. For parental anxiety, respondents were asked whether their mother/father ever received treatment, whether their mother/father was ever hospitalized, and whether the anxiety ever interfered a lot with the mother’s/father’s life or activities. Respondents were asked the same questions about their mother’s/father’s depression. Additionally, respondents were asked if, during the time the depression was at its worst, the mother/father experienced other symptoms (such as low energy or changes in sleep). These questions yield a total of 14 possible additional indicators of poor parental mental health (3 related to the mother figure’s anxiety, 4 related to mother figure’s depression, 3 related to the father figure’s anxiety, 4 related to father figure’s depression). Those who did not indicate having any parent with mental health problems were not asked about additional indicators and were coded “0” on this index. Due to low cell counts at the highest levels of this index, responses are collapsed into an index ranging from 0 to 4 or more. Alternate forms of the severity variable were tested including a non-collapsed index and a logged version of the index. These alternate forms of the severity variable yielded substantively similar results to those presented here.
Although the CRCS did not provide a formal scale of severity, this index mirrors other studies of parental mental health problems that take into account the degree to which the psychological problems interfered with everyday living, symptomatology, and if the parent was hospitalized (Hammen and Brennan 2003; Mars et al. 2012). Additionally, one could argue that receiving help for a mental health problem is a signal of help-seeking rather than the severity of the illness. In ancillary analyses (not shown) a separate index of severity was tested that did not include help-seeking behaviors. These results mirror those of the full index. Furthermore, the reliability, as measured through the Cronbach’s alpha, of the scale without the inclusion of help-seeking was lower than the scale that included these indicators (.73 and .79, respectively).
Duration
Duration of parental mental health problems is measured by the question, “was this during all, most, some, or only a little of your childhood, before you were age 17.” Response categories include “0=none,” “1=a little,” “2=some,” “3=most,” and “4=all.” This question was asked for both depression and anxiety and for both the mother and father figure. For each parental mental health indicator, respondents were coded “0” if they previously indicated no experience with this particular parental mental health problem. The four separate duration items (i.e. maternal depression, paternal depression, maternal anxiety, paternal anxiety) that each range from 0–4 are summed to create an index of overall duration ranging from 0 to 16. Due to low cell counts at high levels of duration, responses are collapsed into an index ranging from 0 to 5 or more. Alternate forms of the duration variable (keeping the duration variable in its original scale and logging the variable) yielded similar results to those presented here.
Gender of Parent with Mental Health Problems
Gender of the parent with mental health problems is measured by a categorical indicator for whether the respondent has no parents with mental health problems in childhood, only their mother had mental health problems, only their father had mental health problems, or both parents had mental health problems. This measurement captures the gender of the parent afflicted as well as the number of parental figures afflicted.
Childhood Circumstances
I control for several childhood circumstances that may confound the relationship between parental mental health problems and children’s distress in adulthood. Ideally, childhood circumstances could be captured using previous waves of the PSID from when respondents were under the age of 17. However, of the respondents in my sample about a quarter (n=763) did not have any prospective information on their childhood and those captured for the entire length of their childhood were much younger compared to the rest of the sample. To retain the individuals with little to no prospective data and to keep the age range proposed, I use retrospective information gathered in the CRCS to measure childhood circumstances.
A dichotomous indicator is included for whether the respondent indicated that their mother figure and father figure were both biological parents. I include two measures of childhood socioeconomic status. To ensure that these measures capture the same time frame as the parental mental health questions (before the respondent was age 17) I use questions that were asked in the CRCS. The first is measured with the question, “Before age 17, compared to the average family at the time, how was the financial situation of the family that you lived with?” Responses range from 1–5 with 1 indicating that the respondent’s family was “a lot better off than the average family” and 5 indicating that the respondent’s family was, “a lot worse off than the average family.” An additional measure capturing whether the respondent’s family ever received welfare was based on the question “was there ever a period of 3 months or more when your family was on welfare or received food stamps” when the respondent was 0–5 years old, 6–12 years old, or 13–16 years old. Respondents were coded “0” if they responded no to each period and “1” if they said yes to any period. To account for the potential effect of the respondent’s mental health on their parent’s mental health, I include a self-reported measure of mental health problems in childhood. Respondents are coded as “1” if they indicated experiencing depression, anxiety, or panic attacks before they were 17 years old, and “0” if they did not experience any of these mental health problems in childhood.
Covariates
Gender and race of the respondent are included as dummy variables with gender coded as “male” (ref.) and “female,” and race coded as “white” (ref.) and “non-white.” Birth cohort is included as a time-invariant continuous variable centered on mean birth year.
Analytic Approach
I use age-based latent growth curve models (LGCM) to assess the relationship between parental mental health problems and children’s distress in adulthood. LGCM estimate an underlying average trajectory of a variable of interest over time as defined by latent intercept and slope parameters, as well as individual variation in these intercept and slope parameters (Muthén 2004). Although the PSID is organized by wave, I assign age as the time metric as it is more salient for distress trajectories (Adkins et al. 2009; Lynch and Taylor 2016). The subsequent LGCM captures within-individual change in distress with age, as well as between-person differences in baseline and growth of distress with age. I first estimate an unconditional model of logged distress as a linear function of age. Age is centered on the youngest age in the sample (age 25) to aid in model interpretation. A comparison of Bayesian Information Criteria (BIC) statistics suggested that a linear trajectory provided the best fit for the data as opposed to an intercept-only model or a quadratic model (see Appendix A).
I then regress time-invariant variables, such as the presence of parental mental health problems in childhood, on the latent intercept and slope parameters to account for between-person differences in trajectories of distress. First, I evaluate the impact of having any parent with mental health problems on children’s baseline level and growth in distress in adulthood including only demographic controls. I then estimate a full model that includes additional childhood circumstances. Next, I estimate the independent effects of the severity of the parental mental health problems, duration of exposure, and the gender of the parent with the mental health problems on distress trajectories in adulthood including all covariates.
All descriptive statistics were computed using STATA version 15.1 and LGCM were estimated using MPlus 8.2. All models are estimated using Full-Information Maximum Likelihood (FIML) to account for missing data and attrition (Allison 2002). Seventy-six percent of respondents had distress scores at every wave included in these analyses, but 774 respondents were missing a distress score from at least one wave. I conducted supplementary analyses that only included respondents with three or more measurements of distress (n=3,043) (Curran, Obeidat, and Losardo 2010). Compared to those with less than three measures of distress, there was a higher proportion of female and non-white among those with three or more measurements of distress. I compared the results from these models against those that used the entire sample and did not reach substantively different conclusions. As results did not differ, I chose to retain my sample size and conduct analyses on the full sample.
RESULTS
Descriptive Statistics
Table 1 presents descriptive statistics stratified by the presence of any parental mental health problems in the respondent’s childhood. Approximately 21.30 percent of respondents were exposed to some type of parental mental health problems in childhood. Of those 21.30 percent, a majority indicated that only their mother figure suffered from mental health problems (72.62 percent) as opposed to only their father figure (13.10 percent) or both parental figures (14.29 percent). Additionally, among those who reported experiencing some type of parental mental health problem, the severity index (ranging from 0–4+ additional indicators) averaged at 1.85 and the duration index (ranging from 0–5+) averaged at 2.60. Although the present analyses do not examine severity and duration separately by gender of the parent afflicted, it should be noted that maternal mental health problems were generally reported as more severe and of longer duration than paternal mental health problems.
Table 1.
Descriptive Statistics by Wave and Presence of Parental Mental Health Problems in Childhood. Panel Study of Income Dynamics (2007–2017) and Childhood Retrospective Circumstances Study (2014) (N=3,240).
| Any Parent with Mental Health Problems | No Parent with Mental Health Problems | ||||
|---|---|---|---|---|---|
| Variable | N=690 | N= 2,414 | |||
| Mean or % | SD | Mean or % | SD | ||
| K-6 Psychological Distress | |||||
| 2007 | 4.56 | 4.80 | 3.12 | 3.76 | *** |
| 2009 | 4.59 | 4.56 | 3.05 | 3.59 | *** |
| 2011 | 4.59 | 4.63 | 2.88 | 3.60 | *** |
| 2013 | 4.59 | 4.68 | 2.83 | 3.67 | *** |
| 2015 | 4.58 | 4.82 | 2.62 | 3.57 | *** |
| 2017 | 4.35 | 4.44 | 2.71 | 3.55 | *** |
| Characteristics of Parental Mental Health Problems | |||||
| Severity (0–4+) | 1.85 | 1.43 | -- | -- | |
| Duration (0–5+) | 2.60 | 1.39 | -- | -- | |
| Gender of parent with mental health problems | |||||
| None | -- | -- | |||
| Mother Only | 72.62% | -- | |||
| Father Only | 13.10% | -- | |||
| Both | 14.29% | -- | |||
| Childhood Circumstancesa | |||||
| Childhood Mental Health Problem | 39.23% | 7.77% | *** | ||
| Family Well off Financially in Childhood (1–5) b | 3.16 | 0.95 | 2.75 | 0.88 | *** |
| Family Received Welfare | 33.43% | 20.91% | |||
| Two Biological Parents | 72.17% | 74.11% | |||
| Demographic Characteristics | |||||
| Age (in 2007) | 38.17 | 9.67 | 39.81 | 9.28 | *** |
| Birth Year | 1968.19 | 9.70 | 1966.56 | 9.28 | *** |
| White | 74.67% | 58.53% | *** | ||
| Male | 31.01% | 38.48% | *** | ||
Note: Final column indicates a significant difference in either mean or proportion of variable of interested across presence of parental mental health problems in childhood
Childhood Characteristics indicate experiences before R was 17 years old
Family Well off in Childhood indicates how well off R reported R’s family was financially compared to the average family during R’s childhood (1=a lot better off, 5= a lot worse off)
p<.05
p<.01
p<.001
There were notable differences between those who experienced any parental mental health problems in childhood and those that did not. Those exposed to poor parental mental health had higher distress scores in each wave compared to those that did not. Additionally, over a third of those who experienced some type of parental mental health problem also reported suffering from mental health problems themselves in childhood as compared to the 7.77 percent among those who did not experience parental mental health problems.
Trajectories of Distress
Tables 2 and 3 present results of growth models predicting the effect of parental mental health problems in childhood on baseline and growth of distress in adulthood. Since the outcome variable is logged, coefficients are interpreted as an average of (eB-1)*100 percentage change in K-6 score intercept or growth for every one-unit increase in x. Additionally, as age is centered on the youngest age in the sample, the intercept coefficient reflects predicted distress at 25 years old.
Table 2.
Growth Model Predicting K-6 Psychological Distress by Any Parental Mental Health Problems. Panel Study of Income Dynamics (2007–2017) and Childhood Retrospective Circumstances Study (2014) (N=3,240).
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| Variable | Beta | SE | Beta | SE | Beta | SE |
| Intercept | 1.300 | 0.022 *** | 1.432 | 0.048 *** | 1.441 | 0.087 *** |
| Any Parental Mental Health Problem | 0.276 | 0.051 *** | 0.137 | 0.054 * | ||
| Birthyear | −0.003 | 0.003 | −0.006 | 0.003 * | ||
| White | −0.205 | 0.046 *** | −0.143 | 0.049 ** | ||
| Male | −0.062 | 0.044 | −0.029 | 0.043 | ||
| Childhood Mental Health Problem | 0.361 | 0.058 *** | ||||
| Family Well off Financially in Childhooda | −0.011 | 0.024 | ||||
| Family Received Welfare | 0.175 | 0.057 ** | ||||
| Two Biological Parents | −0.125 | 0.051 * | ||||
| Age (Slope) | −0.012 | 0.001 *** | −0.021 | 0.002 *** | −0.020 | 0.004 *** |
| Any Parental Mental Health Problem | 0.005 | 0.002 * | 0.004 | 0.003 | ||
| Birthyear | 0.000 | 0.000 | 0.000 | 0.000 | ||
| White | 0.009 | 0.002 *** | 0.006 | 0.002 ** | ||
| Male | −0.001 | 0.002 | −0.001 | 0.002 | ||
| Childhood Mental Health Problem | 0.007 | 0.003 * | ||||
| Family Well off Financially in Childhood a | 0.000 | 0.001 | ||||
| Family Received Welfare | −0.003 | 0.003 | ||||
| Two Biological Parents | 0.002 | 0.002 | ||||
| BIC | 38005.699 | 73902.107 | 90544.698 | |||
Notes: Birth year is mean-centered
SE=Standard Error
Family Well off Financially in Childhood indicates how well off R reported R’s family was financially compared to the average family during R’s childhood (1=a lot better off, 5= a lot worse off)
p<.05
p<.01
p<.001
Table 3.
Growth Model Predicting K-6 Psychological Distress by Characteristics of Parental Mental Health Problems. Panel Study of Income Dynamics (2007–2017) and Childhood Retrospective Circumstances Study (2014) (N=3,240).
| Severity | Duration | Gender of Parent with Mental Health Problems | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| Variable | Beta | SE | Beta | SE | Beta | SE |
| Intercept | 1.445 | 0.087 *** | 1.448 | 0.087 *** | 1.436 | 0.087*** |
| Severity (0–4+) | 0.060 | 0.021 ** | ||||
| Duration (0–5+) | 0.056 | 0.019 ** | ||||
| Gender of parent with mental health problems | ||||||
| None (ref.) | ||||||
| Mother Only | 0.153 | 0.059 ** | ||||
| Father Only | 0.274 | 0.111 * | ||||
| Both Mother and Father | 0.006 | 0.122 | ||||
| Age (Slope) | −0.020 | 0.004 *** | −0.020 | 0.004 *** | −0.019 | 0.004 *** |
| Severity (0–4+) | 0.000 | 0.001 | ||||
| Duration (0–5+) | 0.001 | 0.001 | ||||
| Gender of parent with mental health problems | ||||||
| None (ref.) | ||||||
| Mother Only | 0.002 | 0.003 | ||||
| Father Only | −0.003 | 0.005 | ||||
| Both Mother and Father | 0.017 | 0.006 ** | ||||
| BIC | 96045.721 | 97031.469 | 85481.080 | |||
Notes: All Models control for the full set of covariates
SE=Standard Error
p<.05
p<.01
p<.001
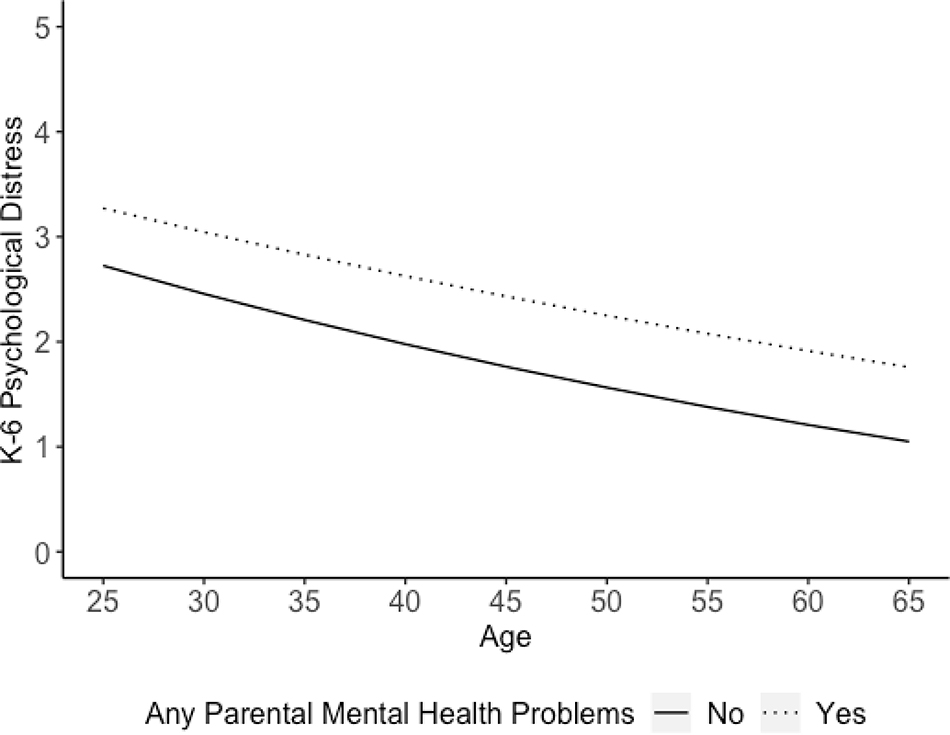
Consistent with life course research on distress trajectories (Clarke et al. 2011), results from the unconditional growth model (Table 2 Model 1) indicate that the average trajectory of distress for this sample is low and decreasing across age. The average K-6 score at age 25 is approximately 3 (out of 24) and every year of age corresponds to an average of 1.19 percent (B =−0.012, p<.001) decrease in distress. Models 2 and 3 in Table 2 assess the relationship between having any parent with mental health problems and adult distress. In the model controlling only for demographic characteristics (Model 2), having any parent with mental health problems corresponds to an increase in intercept and a slower decrease in distress with age. When controlling for childhood circumstances the effect of this stressor on the growth of distress is entirely attenuated, however having a parent with mental health problems is still associated with an average of 14.68 percent (B =.137, p<.01) higher distress at age 25 compared to those who have not experienced this stressor (Model 3). Results from the full model are presented in Figure 1 in the standard (not-logged) K-6 scale holding all other covariates at their mean values. As seen in this figure, those who were exposed to poor parental mental health as a child have consistently higher distress across adulthood compared to those who were not exposed to this stressor. As evident by the non-significant effect of parental mental health problems on the slope of distress, these individuals do not converge to the distress levels of their non-exposed peers with age, but they also do not become increasingly worse off with age.
Figure 1.
Predicted K-6 Scores by Presence of Parental Mental Health Problems in Childhood. Panel Study of Income Dynamics (2007–2017) and Childhood Retrospective Circumstances Study (2014) (N=3,240).
Note: Predicted Scores are calculated from Table 2 Model 3 holding all other covariates at their grand mean value.
Results from Table 2, Model 3 also indicate that having experienced childhood mental health problems is a significant predictor of increased baseline distress and a slower decline of distress with age. Although temporal order of parents’ and children’s mental health problems cannot be determined, it may be that the effect of parental mental health problems on children’s distress in adulthood is in part explained by the children’s initial increase in distress in early life (Cummings et al. 2013; Meadows et al. 2007).
Trajectories of Distress by Variations in Parental Mental Health Problems
Table 3 shows the independent impacts of various characteristics of parental mental health problems on distress in adulthood controlling for demographic and childhood characteristics. Results from Model 1 indicate that every increase in the severity scale measuring additional indicators of parental mental health problems is associated with an average of 6.18 percent (B =.060, p<.01) increase in baseline distress with no impact on the growth of distress with age. Similarly, every increase on the duration scale (Model 2) is associated with an average of 5.76 percent (B=.056, p<.001) higher baseline distress, with no impact on the growth of distress with age. These results suggest that those who experience more severe or longer durations of poor parental mental health have even greater adult distress at age 25 and that this increase in distress remains mostly stable with age.
As the severity and duration measures are somewhat driven by the number of parents with mental health problems, in alternate analyses (available upon request) I examined whether maximum severity (measured as the maximum severity score between the maternal and paternal indices) and maximum duration (taken as the maximum duration of the four possible parental mental health statuses) operated similarly to the summative scales. Rather than capturing overall exposure, the maximum measures capture whether more severe or longer cases of parental mental health problems are detrimental to adult mental health regardless of the number of parents who had mental health problems. The maximum measures of severity and duration were likewise related to increased baseline distress in adulthood, with no subsequent effect on the slope of distress with age.
In Model 3, I examine how the gender of the afflicted parent may shape adult distress. Results from this model reveal that both mothers’ and fathers’ mental health problems in childhood are associated with increased distress at age 25 and that this increase remains stable across age. Ancillary analyses (not shown) that compare solely maternal mental health problems with paternal mental health problems indicate that the impact on baseline distress does not differ by the gender of the afflicted parent.
This model also indicates that having both a mother and father with mental health problems compared to no parents corresponds to an average 1.71 (B =.017, p<.01) percent increase in distress with every year of age. Those with no experience with poor parental mental health follow a trajectory of declining distress with age, but those exposed to both maternal and paternal mental health problems have almost no decline of distress with age. Accordingly, the gap in distress between these groups grows across adulthood.
Although previous research has suggested that the transmission of mental health problems from parent to child is not entirely based in genetics (McAdams et al. 2015; Silberg, Maes, and Eaves 2010; Tully, Iacono, and McGue 2008), I conducted a supplementary analysis on those with non-biological parents. I treated those who indicated they had either a biological mother, biological father, or some other relative as their mother or father figure as having a biological parent. Those who indicated all of their parents were adoptive, step, or non-relative were coded as having non-biological parents (n=57). Fit statistics for this subgroup suggested that an intercept-only model fit the data better than a linear growth model (see Appendix B). In the intercept-only model (see Appendix C), having any parent with mental health problems is a significant predictor of increased distress among those with non-biological parents. However, this effect is attenuated when controlling for the respondent’s own mental health problems in childhood. Thus, similar to results for the entire sample, part of the long-term effect of parental mental health problems operates through an increase in one’s own mental health problems in childhood. Although the current analysis is unable to include specific genetic data, these results lend support to the argument that poor parental mental health is a significant stressor with long-term consequences for children’s distress, regardless of biological ties.
DISCUSSION
Research within the stress process and life course literature has reinforced that stress in childhood, and particularly stress associated with parental mental health, is often a precursor for poor outcomes in adulthood (Angelini et al. 2016; Goosby 2013). While studies have established a relationship between parental mental health problems and distress in adulthood, few have questioned how this stressor shapes mental health across multiple years of adulthood. Thus, existing cross-sectional studies have not investigated whether the gap in distress between those exposed to this childhood stressor and those not exposed remains stable, increases, or decreases across adulthood (Ferraro and Wilkinson 2013; Schafer and Ferraro 2013).
Results from this study indicate that controlling for potential childhood confounders, any experience with parental mental health problems has an enduring impact on children’s distress. Those who are exposed to this childhood stressor remain at a consistently higher level of distress compared to their non-exposed counterparts, and this gap is stable across adulthood. In other words, these children never escape the stress accrued during this childhood experience, even as they enter new stages of the life course. However, this stressor does not pose additional threats to mental health above this baseline increase (Schafer and Ferraro 2013).
In addition to establishing the long-term impact of parental mental health problems, this study sought to unpack how heterogeneity in the experience with this childhood stressor corresponds to varied adult mental health outcomes. Specifically, this study aimed to uncover the independent effects of severity, duration, and gender of the afflicted parent. Increases in the severity or the duration exposed to this stressor correspond to even greater distress in adulthood. Thus, the presentation of parental mental health problems does predict the degree to which children end up more distressed than those who did not experience this stressor. Contrary to past work that suggests maternal mental health is more impactful than paternal mental health (Meadows et al. 2007; Noonan et al. 2018), results from the current study indicate that the impact of maternal and paternal mental health problems was largely the same. In fact, consistent with some past work (e.g. Kahn et al., 2004) the presence of both maternal and paternal mental health problems was the most problematic for children’s adult distress. Those individuals exposed to both maternal and paternal poor mental health remained at a consistent level of distress throughout adulthood, while all others experienced the normative decline of distress associated with aging (Clarke et al. 2011). Even though only a small number of respondents reported both maternal and paternal mental health problems, this finding highlights how difficult it may be for these individuals to escape the negative impacts of dual exposure to mental health problems.
Taken together, these findings underscore the importance of acknowledging that not all experiences with childhood adversity, and particularly parental mental health problems, look alike. Variation in the experience with this stressor corresponds with diverse outcomes in adulthood. Studies that dichotomize childhood adversity rather than test specific characteristics of the stressor may underestimate the impact it has on children who are exposed to the most severe cases or who are exposed for longer periods of early life. This study focused on analyzing characteristics of parental mental health problems, but the concepts of heterogeneity can, and should, be applied to other childhood stressors to identify those individuals at risk for the greatest distress once they reach adulthood.
The primary limitation of this study is that analyses rely on respondents’ retrospective reports of their childhood experiences. Some respondents may over or underestimate their mother’s and father’s symptomology, the severity of these mental health problems, or the duration for which these symptoms occurred. Individuals who experience parental mental health problems at extremely young ages may have difficulty understanding the event or be vulnerable to infantile amnesia (Brewin, Andrews, and Gotlib 1993; Hardt and Rutter 2004) wherein events that occur before age three are difficult to recall. Finally, those who are currently experiencing mental health problems may be more likely to recall past negative events than those with more positive affect, especially when memories are self-referential (Hardt and Rutter 2004; Schraedley, Turner, and Gotlib 2002). Since there is no prospective data on parental mental health when respondents were children, it is not possible to corroborate the retrospective reports. That being said, recent research suggests that respondents are more likely to underreport instead of over-report negative childhood events, which would lead to conservative estimates (Hardt and Rutter 2004). Qualitative studies have highlighted that even young children have a generally sophisticated understanding of their parents’ mental health (Mordoch and Hall 2008; Simpson-Adkins and Daiches 2018). And research has argued that retrospective reports of childhood circumstances, and particularly parental psychopathology (Schraedley et al. 2002), are not likely to be significantly altered by current mood statuses (Brewin et al. 1993). Brewin and colleagues (1993) also note that those with depressed affect tend to place blame on internal factors rather than external, making it unlikely that they would blame external childhood circumstances if those experiences did not occur. Nevertheless, results presented here should be interpreted with the understanding that no formal test of validity and reliability can be assessed with this data.
Another limitation is the inability to measure the timing of parental mental health problems. A more complete history of parents’ psychological problems would be necessary to explore whether individuals are sensitive to the timing of exposure to this stressor. Furthermore, as the CRCS does not ask individuals about more severe mental health diagnoses, a thorough investigation of how different types/more severe types of parental mental health problems influence children’s life course mental health cannot be conducted. It should also be noted that due to the lack of complete prospective data on the respondents in this sample, a more complete measure of family structure in childhood could not be obtained. The mother/father figures identified in the CRCS are the parental figures who were most present in the respondent’s childhood, however, there may be other adults in the child’s life the child sought out to buffer the effects of adversity (Kysar-Moon 2019) or who could also suffer from mental health problems.
Despite these limitations, this work sets the foundation for several future studies on parental mental health and children’s outcomes in adulthood. In particular, future work should focus on the many circumstances, both in childhood and adulthood, that may link poor parental mental health to children’s adult distress. This study provided preliminary evidence that the impact of parental mental health on children’s mental health in adulthood may operate through children’s initial increased distress in childhood. However, this study does not formally test how adulthood statuses, such as marital status, parenthood, or economic attainment, may likewise act as crucial links connecting parental mental health to offspring’s adult distress. Future work should also focus on the psychosocial resources that may buffer the impact of this stressor (Aneshensel and Avison 2015). For example, there is a body of literature that suggests that parental warmth in childhood is protective for children throughout the life course (Chen, Kubzansky, and VanderWeele 2019; Wilkinson and Andersson 2019). Parents who experience psychological problems may be able to offset the negative long-term impacts through positive relationships with their children. A thorough examination of mediators and psychosocial buffers would be especially relevant for informing interventions to address negative impacts on life course mental health.
In sum, although previous research has established a relationship between parental mental health and children’s outcomes in adulthood, this study was one of the first to comment on how this experience shapes trajectories of mental health throughout early to mid-adulthood. Moreover, this study furthered the understanding of parental mental health problems by exploring crucial sources of heterogeneity in this experience. The results presented here reinforce the persistent nature of stress associated with parent’s mental health and underline that children with more intense exposure to this stressor are at an even greater risk of heightened distress throughout adulthood.
Supplementary Material
Acknowledgments
The collection of data used in this study was partly supported by the National Institutes of Health under grant number R01 HD069609 and R01 AG040213, and the National Science Foundation under award numbers SES 1157698 and 1623684.
Footnotes
Some of the data used in this analysis are derived from Restricted Data Files of the Panel Study of Income Dynamics, obtained under special contractual arrangements designed to protect the anonymity of respondents. These data are not available from the author. Persons interested in obtaining PSID Restricted Data Files should contact PSIDHelp@umich.edu.
REFERENCES
- Adkins Daniel E., Wang Victor, Dupre Matthew E., van den Oord Edwin J. C. G., and Elder Glen H. Jr. 2009. “Structure and Stress: Trajectories of Depressive Symptoms across Adolescence and Young Adulthood.” Social Forces 88(1):31–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison Paul. 2002. Missing Data. 2455 Teller Road, Thousand Oaks California 91320 United States of America: SAGE Publications, Inc. [Google Scholar]
- Aneshensel Carol S. 2015. “Sociological Inquiry into Mental Health: The Legacy of Leonard I. Pearlin.” Journal of Health and Social Behavior 56(2):166–78. [DOI] [PubMed] [Google Scholar]
- Aneshensel Carol S. and Avison William R. 2015. “The Stress Process: An Appreciation of Leonard I. Pearlin.” Society and Mental Health 5(2):67–85. [Google Scholar]
- Angelini Viola, Klijs Bart, Smidt Nynke, and Mierau Jochen O. 2016. “Associations between Childhood Parental Mental Health Difficulties and Depressive Symptoms in Late Adulthood: The Influence of Life-Course Socioeconomic, Health and Lifestyle Factors.” PLoS One; San Francisco 11(12):e0167703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avison William R. 2010. “Incorporating Children’s Lives into a Life Course Perspective on Stress and Mental Health.” Journal of Health and Social Behavior; Washington 51(4):361–75. [DOI] [PubMed] [Google Scholar]
- Brennan Patricia A., Hammen Constance, Andersen Margaret J., Bor William, Najman Jake M., and Williams Gail M. 2000. “Chronicity, Severity, and Timing of Maternal Depressive Symptoms: Relationships with Child Outcomes at Age 5.” Developmental Psychology 36(6):759–66. [DOI] [PubMed] [Google Scholar]
- Brewin Chris R., Andrews Bernice, and Gotlib Ian H. 1993. “Psychopathology and Early Experience: A Reappraisal of Retrospective Reports.” Psychological Bulletin 113(1):82–98. [DOI] [PubMed] [Google Scholar]
- Chen Ying, Kubzansky Laura D., and VanderWeele Tyler J. 2019. “Parental Warmth and Flourishing in Mid-Life.” Social Science & Medicine 220:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke Philippa, Marshall Victor, House James, and Lantz Paula. 2011. “The Social Structuring of Mental Health over the Adult Life Course: Advancing Theory in the Sociology of Aging.” Social Forces; a Scientific Medium of Social Study and Interpretation 89(4):1287–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell Arin M. and Goodman Sherryl H. 2002. “The Association between Psychopathology in Fathers versus Mothers and Children’s Internalizing and Externalizing Behavior Problems: A Meta-Analysis.” Psychological Bulletin 128(5):746–73. [DOI] [PubMed] [Google Scholar]
- Coryell William, Winokur George, Maser Jack D., Akiskal Hagop S., Keller Martin B., and Endicott Jean. 1994. “Recurrently Situational (Reactive) Depression: A Study of Course, Phenomenology and Familial Psychopathology.” Journal of Affective Disorders 31(3):203–10. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Cheung Rebecca Y. M., and Davies Patrick T. 2013. “Prospective Relations Between Parental Depression, Negative Expressiveness, Emotional Insecurity, and Children’s Internalizing Symptoms.” Child Psychiatry and Human Development; New York 44(6):698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings EM, Keller Peggy S., and Davies Patrick T. 2005. “Towards a Family Process Model of Maternal and Paternal Depressive Symptoms: Exploring Multiple Relations with Child and Family Functioning.” Journal of Child Psychology and Psychiatry 46(5):479–89. [DOI] [PubMed] [Google Scholar]
- Curran Patrick J., Obeidat Khawla, and Losardo Diane. 2010. “Twelve Frequently Asked Questions About Growth Curve Modeling.” Journal of Cognition and Development: Official Journal of the Cognitive Development Society 11 (2):121–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder Glen H. 1998. “The Life Course as Developmental Theory.” Child Development 69(1):1–12. [PubMed] [Google Scholar]
- Elgar Frank J., Mills Rosemary S. L., McGrath Patrick J., Waschbusch Daniel A., and Brownridge Douglas A. 2007. “Maternal and Paternal Depressive Symptoms and Child Maladjustment: The Mediating Role of Parental Behavior.” Journal of Abnormal Child Psychology 35(6):943–55. [DOI] [PubMed] [Google Scholar]
- Ferraro Kenneth F. and Shippee Tetyana Pylypiv. 2009. “Aging and Cumulative Inequality: How Does Inequality Get Under the Skin?” The Gerontologist 49(3):333–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro Kenneth F. and Wilkinson Lindsay R. 2013. “Age, Aging, and Mental Health.” Pp. 183–203 in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Phelan JC, and Bierman A Dordrecht: Springer Netherlands. [Google Scholar]
- Friedman Esther M., Jennifer Karas Montez Connor McDevitt Sheehan, Guenewald Tara L., and Seeman Teresa E. 2015. “Childhood Adversities and Adult Cardiometabolic Health: Does the Quantity, Timing, and Type of Adversity Matter?” Journal of Aging and Health 27(8):1311–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George Linda K. 2013. “Life-Course Perspectives on Mental Health.” Pp. 585–602 in Handbook of the Sociology of Mental Health, Handbooks of Sociology and Social Research, edited by Aneshensel CS, Phelan JC, and Bierman A Dordrecht: Springer Netherlands. [Google Scholar]
- George Linda K. 2014. “Taking Time Seriously: A Call to Action in Mental Health Research.” Journal of Health and Social Behavior 55(3):251–64. [DOI] [PubMed] [Google Scholar]
- Goosby Bridget J. 2013. “Early Life Course Pathways of Adult Depression and Chronic Pain.” Journal of Health and Social Behavior; Washington 54(1):75–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen Constance and Brennan Patricia A. 2003. “Severity, Chronicity, and Timing of Maternal Depression and Risk for Adolescent Offspring Diagnoses in a Community Sample.” Archives of General Psychiatry 60(3):253–58. [DOI] [PubMed] [Google Scholar]
- Hanington L, Heron J, Stein A, and Ramchandani P 2012. “Parental Depression and Child Outcomes – Is Marital Conflict the Missing Link?” Child: Care, Health and Development 38(4):520–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt Jochen and Rutter Michael. 2004. “Validity of Adult Retrospective Reports of Adverse Childhood Experiences: Review of the Evidence.” Journal of Child Psychology and Psychiatry 45(2):260–73. [DOI] [PubMed] [Google Scholar]
- Kahn Robert S., Brandt Dominique, and Whitaker Robert C. 2004. “Combined Effect of Mothers’ and Fathers’ Mental Health Symptoms on Children’s Behavioral and Emotional Well-Being.” Archives of Pediatrics & Adolescent Medicine 158(8):721–29. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., Barker Peggy R., Colpe Lisa J., Epstein Joan F., Gfroerer Joseph C., Hiripi Eva, Howes Mary J., Normand Sharon-Lise T., Manderscheid Ronald W., Walters Ellen E., and Zaslavsky Alan M. 2003. “Screening for Serious Mental Illness in the General Population.” Archives of General Psychiatry 60(2):184–89. [DOI] [PubMed] [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, and Power C 2003. “Life Course Epidemiology.” Journal of Epidemiology and Community Health; London 57(10):778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kysar-Moon Ashleigh. 2019. “Childhood Adversity and Internalizing Problems: Evidence of a Race Mental Health Paradox.” Society and Mental Health 215686931984332. [Google Scholar]
- Lynch Scott M. and Taylor Miles G. 2016. “Chapter 2 - Trajectory Models for Aging Research.” Pp. 23–51 in Handbook of Aging and the Social Sciences (Eighth Edition), edited by George LK and Ferraro KF San Diego: Academic Press. [Google Scholar]
- Mars Becky, Collishaw Stephan, Smith Daniel, Thapar Ajay, Potter Robert, Sellers Ruth, Harold Gordon T., Craddock Nicholas, Rice Frances, and Thapar Anita. 2012. “Offspring of Parents with Recurrent Depression: Which Features of Parent Depression Index Risk for Offspring Psychopathology?” Journal of Affective Disorders 136(1–2):44–53. [DOI] [PubMed] [Google Scholar]
- McAdams TA, Rijsdijk FV, Neiderhiser JM, Narusyte J, Shaw DS, Natsuaki MN, Spotts EL, Ganiban JM, David Reiss LD, Leve P. Lichtenstein, and Eley TC 2015. “The Relationship between Parental Depressive Symptoms and Offspring Psychopathology: Evidence from a Children-of-Twins Study and an Adoption Study.” Psychological Medicine; Cambridge 45(12):2583–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland Michael J. 2017. “Poverty and Problem Behaviors across the Early Life Course: The Role of Sensitive Period Exposure.” Population Research and Policy Review 36(5):739–60. [Google Scholar]
- McGonagle Katherine and Freedman Vicki A. 2015. “The Panel Study of Income Dynamics’ Childhood Retrospective Circumstances Study (PSID-CRCS) User Guide: Final Release 1.” Institute for Social Research, University of Michigan. [Google Scholar]
- Meadows Sarah O., McLanahan Sara S., and Jeanne Brooks-Gunn. 2007. “Parental Depression and Anxiety and Early Childhood Behavior Problems Across Family Types.” Journal of Marriage and Family; Minneapolis 69(5):1162–77. [Google Scholar]
- Miller Gregory E., Chen Edith, and Parker Karen J. 2011. “Psychological Stress in Childhood and Susceptibility to the Chronic Diseases of Aging: Moving toward a Model of Behavioral and Biological Mechanisms.” Psychological Bulletin 137(6):959–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mordoch Elaine and Hall Wendy A. 2008. “Children’s Perceptions of Living With a Parent With a Mental Illness: Finding the Rhythm and Maintaining the Frame.” Qualitative Health Research 18(8):1127–44. [DOI] [PubMed] [Google Scholar]
- Moser Richard and Jacob Theodore. 1997. “Parent-Child Interactions and Child Outcomes as Related to Gender of Alcoholic Parent.” Journal of Substance Abuse 9:189–208. [DOI] [PubMed] [Google Scholar]
- Muthén Bengt. 2004. “Latent Variable Analysis: Growth Mixture Modeling and Related Techniques for Longitudinal Data.” Pp. 346–69 in The SAGE Handbook of Quantitative Methodology for the Social Sciences. 2455 Teller Road, Thousand Oaks California: 91320 United States of America: SAGE Publications, Inc. [Google Scholar]
- Noonan Katharine, Burns Richéal, and Violato Mara. 2018. “Family Income, Maternal Psychological Distress and Child Socio-Emotional Behaviour: Longitudinal Findings from the UK Millennium Cohort Study.” SSM - Population Health 4:280–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldehinkel Albertine J., Ormel Johan, Verhulst Frank C., and Nederhof Esther. 2014. “Childhood Adversities and Adolescent Depression: A Matter of Both Risk and Resilience.” Development and Psychopathology; Cambridge 26(4pt1):1067–75. [DOI] [PubMed] [Google Scholar]
- Panel Study of Income Dynamics, public use dataset. Produced and distributed by the Survey Research Center, Institute for Social Research, University of Michigan, Ann Arbor, MI: 2017. [Google Scholar]
- Panel Study of Income Dynamics, restricted use data. Produced and distributed by the Survey Research Center, Institute for Social Research, University of Michigan, Ann Arbor, MI: 2017. [Google Scholar]
- Pearlin Leonard I. 2010. “The Life Course and the Stress Process: Some Conceptual Comparisons.” The Journals of Gerontology: Series B 65B(2):207–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield Sarah and Mouzon Dawne. 2013. “Gender and Mental Health.” Pp. 277–96 in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Phelan JC, and Bierman A Dordrecht: Springer Netherlands. [Google Scholar]
- Schaan Barbara. 2014. “The Interaction of Family Background and Personal Education on Depressive Symptoms in Later Life.” Social Science & Medicine 102:94–102. [DOI] [PubMed] [Google Scholar]
- Schafer Markus H. and Ferraro Kenneth F. 2013. “Childhood Misfortune and Adult Health: Enduring and Cascadic Effects on Somatic and Psychological Symptoms?” Journal of Aging and Health 25(1):3–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schepman Karen, Collishaw Stephan, Gardner Frances, Maughan Barbara, Scott Jacqueline, and Pickles Andrew. 2011. “Do Changes in Parent Mental Health Explain Trends in Youth Emotional Problems?” Social Science & Medicine 73(2):293–300. [DOI] [PubMed] [Google Scholar]
- Schilling Elizabeth A., Aseltine Robert H., and Gore Susan. 2008. “The Impact of Cumulative Childhood Adversity on Young Adult Mental Health: Measures, Models, and Interpretations.” Social Science & Medicine 66(5):1140–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schraedley Pamela K., Jay Turner R, and Gotlib Ian H. 2002. “Stability of Retrospective Reports in Depression: Traumatic Events, Past Depressive Episodes, and Parental Psychopathology.” Journal of Health and Social Behavior; Washington 43(3):307–16. [PubMed] [Google Scholar]
- Silberg Judy, Maes Hermine, and Eaves Lindon J. 2010. “Genetic and Environmental Influences on the Transmission of Parental Depression to Children’s Depression and Conduct Disturbance: An Extended Children of Twins Study.” The Journal of Child Psychology and Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson-Adkins Graham John and Daiches Anna. 2018. “How Do Children Make Sense of Their Parent’s Mental Health Difficulties: A Meta-Synthesis.” Journal of Child and Family Studies 27(9):2705–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stambaugh Leyla F., Valerie Forman-Hoffman Jason Williams, Pemberton Michael R., Ringeisen Heather, Hedden Sarra L., and Bose Jonaki. 2017. “Prevalence of Serious Mental Illness among Parents in the United States: Results from the National Survey of Drug Use and Health, 2008–2014.” Annals of Epidemiology 27(3):222–24. [DOI] [PubMed] [Google Scholar]
- Strohschein Lisa and Gauthier Anne H. 2018. “Poverty Dynamics, Parenting, and Child Mental Health in Canada.” Society and Mental Health 8(3):231–47. [Google Scholar]
- Tully Erin C., Iacono William G., and Matt McGue. 2008. “An Adoption Study of Parental Depression as an Environmental Liability for Adolescent Depression and Childhood Disruptive Disorders.” The American Journal of Psychiatry; Washington 165(9):1148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Crosnoe Robert, and Reczek Corinne. 2010. “Social Relationships and Health Behavior Across the Life Course.” Annual Review of Sociology 36:139–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Thomas Patricia A., Liu Hui, and Thomeer Mieke Beth. 2014. “Race, Gender, and Chains of Disadvantage: Childhood Adversity, Social Relationships, and Health.” Journal of Health & Social Behavior 55(1):20–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson Renae and Andersson Matthew A. 2019. “Adolescent Socioeconomic Status and Parent-Child Emotional Bonds: Reexamining Gender Differences in Mental Well-Being during Young Adulthood.” Society and Mental Health 9(1):95–110. [Google Scholar]
- Williams Deadric T. and Cheadle Jacob E. 2016. “Economic Hardship, Parents’ Depression, and Relationship Distress among Couples With Young Children.” Society and Mental Health 6(2):73–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson Sylia and Durbin C. Emily. 2010. “Effects of Paternal Depression on Fathers’ Parenting Behaviors: A Meta-Analytic Review.” Clinical Psychology Review 30(2):167–80. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.