Abstract
Residential area characteristics and discrimination have been associated with psychological distress. Differences in these relationships across racial groups are not well understood. We examined the relative role of perceived discrimination, neighborhood problems and neighborhood cohesion/trust in explaining differences in psychological distress (indicated by anxiety and depressive symptoms) between 224 African American and 225 White smokers (income ≤ 400% federal poverty level) in a smoking cessation intervention study. Surveys were linked to US census-tract data. We conducted random intercept Poisson multi-level regression models and examined interactions between race and neighborhood experiences. African Americans had greater risk of anxiety and depressive symptoms and greater individual and neighborhood disadvantage than Whites. Controlling for objective neighborhood characteristics, when perceived discrimination and perceived neighborhood characteristics were added to the regression models the association between anxiety symptoms and race were no longer statistically significant; the association between depressive symptoms and race decreased but remained statistically significant. Lower neighborhood social cohesion/trust and greater neighborhood problems increased depressive symptoms for African Americans, but not for Whites. Perceived discrimination and neighborhood social cohesion/trust outweighed the importance of race in explaining anxiety symptoms. These findings underscore the need for multi-level interventions addressing social and environmental contexts.
Keywords: Depressive symptoms, Anxiety symptoms, Neighborhood-socioeconomic contexts, Race, Neighborhood social cohesion
Introduction
Residential-area characteristics and racial concentration provide an environmental context that influences racial health disparities (Aneshensel and Sucoff 1996; Do et al. 2008; Bécares 2012). Exposures to persistent stressors within the broader context of social and residential disadvantage, such as experiences of discrimination or neighborhood disorder, may influence mental and physical health across lower socioeconomic status and minority groups (Everett et al. 2016; Matthews et al. 2010; Williams and Mohammed 2013). Although several studies indicate that African Americans have lower rates of major depressive and anxiety disorders (except for post-traumatic stress disorder) compared to non-Hispanic Whites (Williams et al. 2007; Himle et al. 2009), recent national surveys show that African Americans experience higher rates of psychological distress and elevated depressive symptomology compared to non-Hispanic Whites (Weissman et al. 2015; Rodriquez et al. 2018). There is a paucity of literature on how psychological distress among at-risk African Americans and Whites may be associated with supports and stressors within neighborhoods. Psychological distress warrants investigation due to potential effects on quality of life and health, with even low levels of distress symptoms associated with cardiovascular disease and all-cause mortality (Russ et al. 2012).
The Environmental Affordances model posits that social structures and social position associated with race impact physical and mental health through exposure to chronic stressors and coping-related health behaviors (Mezuk et al. 2013). Central to the Environmental Affordances model is the proposition that racial health disparities are due to differing environments and resources between African Americans and Whites. Unhealthy coping behaviors (e.g., tobacco use) are hypothesized to reduce the effect of chronic stressors on psychopathology in the short-term, but increase risk of morbidity and early mortality. Importantly, smokers are more likely to be economically disadvantaged (Jamal et al. 2016) and, as such, may be exposed to greater levels of chronic stressors than the general population. Even though smoking can be conceptualized as a coping strategy, smokers remain more likely to experience negative mental health outcomes. Data show that smokers have higher prevalence of comorbid mental health conditions (Lawrence et al. 2009), and experience elevated levels of psychological distress compared to nonsmokers (Lawrence and Williams 2016). The goal of this study is to understand the pervasive mental health risks experienced by lower income African American and White smokers including discrimination and neighborhood disadvantage. We conceptualized a link between disadvantaged neighborhood environments and psychological distress through the interplay of neighborhood stressors (e.g., neighborhood disorder) that increase individuals’ experience of stress, and neighborhood stress-buffering mechanisms that increase social support (Stockdale et al. 2007).
Neighborhood Social Cohesion and Neighborhood Problems
Neighborhood social cohesion and exposure to neighborhood problems have implications for psychological well-being. Social cohesion can be considered an aspect of social capital (Almedom 2005) that increases feelings of safety, reduces stress, facilitates integration into social networks, encourages reciprocity, and enhances the ability to access and capitalize on available social resources. Heightened levels of neighborhood social cohesion has been shown to have protective effects on mental health (Mair et al. 2008; Echeverría et al. 2008).
Neighborhood problems refers to features of neighborhoods that function as stressors (e.g., noise, litter, safety concerns) (Steptoe and Feldman 2001). Living in a neighborhood perceived as problematic has been demonstrated to increase risk of mental health problems (Matthews et al. 2010; Gary et al. 2007; Mair et al. 2009; Mair et al. 2010). Neighborhood disorder marked by weak social control (i.e., observable neighborhood problems) can produce psychological distress that is active (e.g., anxiety) or passive (e.g., depression) (Ross and Mirowsky 2009). Generalized distrust in a community is associated with reduced social support and elevated sense of threat; individuals living in disadvantaged neighborhoods are likely to have greater psychological distress through increased exposure to stressors and greater neighborhood disorder (Ross 2000).
The associations between neighborhood characteristics and mental health may vary by race. One study found that anxiety, depression, and ratings of stress increased among Whites and African Americans reporting greater neighborhood problems, however, neighborhood cohesion, defined as the ability of people to work together, only benefited Whites (Gary et al. 2007). This race-specific benefit was not observed in a multi-ethnic, population-based cohort study that found similar associations among neighborhood cohesion, neighborhood problems, and depressive symptoms in separate models reported by race (Echeverría et al. 2008). The lack of consistency in findings between these studies could be due to differences in measurement, particularly for neighborhood cohesion, or unique neighborhood contexts. In the United States, the impact of neighborhood characteristics on mental health by race warrants further study. Historical factors have led to African Americans and Whites living in neighborhoods with varying levels of racial segregation resulting in differential exposures to neighborhood-level resources and stressors (Matthews et al. 2010; Williams and Mohammed 2013). Racial residential segregation has significant socioeconomic implications for African American communities and, in turn, psychological well-being and health of African Americans.
Perceived Discrimination
Perceived discrimination (including attributions to racial and non-racial reasons) adversely impacts mental and physical health through increased stress and health-compromising behaviors (Pascoe and Smart Richman 2009). Although low SES African Americans and Whites report comparable levels of discrimination and greater discrimination than higher SES groups, a greater proportion of African American’s discriminatory experiences are attributed to race (Williams et al. 2012). Greater levels of racial discrimination are associated with more severe psychological distress among African Americans (Krieger et al. 2011). A meta-analytic review found that the effect size for the association between racial discrimination and psychological distress was lower than that for other attributions for discrimination (e.g., disability status, HIV+ status, sexual orientation, weight) (Schmitt et al. 2014). To date, much of the research on the impact of discrimination among African Americans has focused on racial discrimination; however, perceived general discrimination contributes to psychological distress in African American and Whites (Everett et al. 2016).
The Current Study
The current study was designed to address three gaps in the existing research literature exploring the role of residential factors in explaining mental health risks. First, studies focusing on residential area and mental health have generally focused on depressive symptoms or non-specific mental illness symptoms (Arcaya et al. 2016), but anxiety-related symptoms may also be important sequelae of discriminatory experiences, particularly for African Americans (Pieterse et al. 2012). Second, while the impact of discriminatory experiences on mental health may be particularly relevant among low SES individuals, there is less research investigating their role in explaining racial differences in mental health problems after taking into account the effects of residential characteristics (English et al. 2014; Shell et al. 2013). Third, findings on racial differences in the associations of neighborhood cohesion and mental health problems has been equivocal and these studies have either focused on a single community (Gary et al. 2007) or have not explored potential race interactions (Echeverría et al. 2008).
The aim of this study was to understand the relative role of perceived discrimination and neighborhood experiences (including neighborhood problems and neighborhood cohesion/trust) in explaining racial differences in anxiety and depressive symptoms, while adjusting for objective neighborhood characteristics (including neighborhood disadvantage, racial composition, and density) among low-income African American and White smokers. We explored moderating effects of race on the associations of perceived discrimination and neighborhood experiences with mental illness symptoms to consider how the relative importance of neighborhood experiences vary by race.
Method
Study participants
Participants were African American and White smokers enrolled in a smoking cessation trial in a large, Midwestern city. The trial was a prospective cohort intervention study of varenicline for smoking cessation designed to assess potential predictors of differential quit rates among African American and White lower income smokers (Nollen et al. 2016). The design included stratified enrollment to obtain equal numbers of participants by race (224 African Americans, 225 Whites) and, within race, by age (< 40, ≥ 40) and gender. Participants were recruited through community- (e.g., radio, television, social media ads) and clinic-based efforts (e.g., provider referral) in a large Midwestern city. As a condition of eligibility, participants were recruited within a restricted income range (≤ 400% Federal Poverty Level; FPL). Because the parent trial provided varenicline, individuals were ineligible if they received medication or counseling for substance use or depression in the last year, had a history of panic or anxiety disorder, psychosis or bipolar disorder, or screened positive for possible depression at eligibility screening. Therefore, the resulting sample excluded participants with known mood and anxiety disorders. The dependent variables in this study were subclinical levels of anxiety and depressive symptoms. Eligible participants provided written informed consent. The majority (70.6%) of the sample were < 200% FPL, with African American and White households supporting 3 family members (including the participant) on a mean household income of $21,293 (SD=$15,501) and $35,806 (SD=$21,035), respectively (Nollen et al. 2016). A detailed description of the trial methods and baseline participant characteristics is published elsewhere (Nollen et al. 2016). For the current analyses, we excluded 5 participants who had missing values on addresses (e.g., post office box listed), resulting in a final sample of 444 individuals (221 African Americans, 223 Whites) from 240 unique census tracts (average of 1.9 persons per tract; range 1–13 participants).
Study procedures were approved and monitored by the Human Subjects Committee of the researchers’ institution.
Measures
Outcomes: Psychological Distress Symptoms
The dependent variables included two indicators of psychological distress: anxiety symptoms and depressive symptoms. The Generalized Anxiety Disorder 7-item (GAD-7) assessed how often participants experienced symptoms of generalized anxiety disorder (e.g., on edge, uncontrolled worry, restlessness) in the past two weeks (Spitzer et al. 2006). Response options ranged between 0 ‘not at all’ to 3 ‘nearly every day’. Scores were summed (α=0.83) and treated continuously ranging between 0–21, with higher scores indicating greater anxiety. The Patient Health Questionnaire (PHQ)-9 was used to assess the frequency of symptoms for each of the DSM-IV criteria for depression over the past 2 weeks (response options ranged from 0 ‘not at all’ to 3 ‘nearly every day’) (Kroenke et al. 2003). Depressive symptoms were included as a continuous variable (α= 0.77) ranging from 0 −27.
Perceived Discrimination and Neighborhood Experiences
Discrimination was assessed using the Everyday Discrimination Scale (Short Version), a 5-item scale assessing the frequency of experiences of discrimination (e.g., being treated with less respect, people acting as if they are afraid of you) (Sternthal et al. 2011). Frequencies of the five situations (‘never’ to ‘almost every day’) were summed to produce the continuous scale score ranging between 0–25 (α=0.76).
Perceived neighborhood experiences were conceptualized using two constructs: neighborhood problems (indicating neighborhood disorder) and social cohesion/trust. The neighborhood problems questionnaire is a 10-item measure that asked participants to identify the degree (0=not a problem; 1=some problem; 2=serious problem) to which issues such as litter, vandalism, noise, traffic, and safety are problems in their neighborhood (Steptoe and Feldman 2001). Responses were averaged to create a continuous variable ranging from 0–2. The 5-item neighborhood social cohesion/trust questionnaire assessed participant’s beliefs about their neighbors’ trustworthiness, shared values, willingness to help, close-knit connections, and ability to get along with each other (Sampson et al. 1997). Responses ranged from ‘strongly disagree’ (0) to ‘strongly agree’ (4) and were averaged to form a single scale (α=0.86) ranging between 0–4.
Sociodemographic characteristics
Demographic variables included race (non-Hispanic Black/African American or non-Hispanic White), gender (male or female), age (continuous), and, marital status. Marital status included married or living with a current partner versus not currently married (included separated, never married, divorced, or widowed).
Socioeconomic Status
Education was included as a dichotomous variable for highest level of educational attainment (high school diploma or less compared to “some college or college degree”). Poverty was dichotomized as those above or below 300% of the 2012 Federal Poverty Line based on total gross annual household income and the number of people living in the home (Department of Health and Human Services and Office of the Secretary 2012). Employment was dichotomized as either currently employed (including both part-time or full time) versus not currently employed that included unemployed, students, homemakers, and retired. Homeownership was a binary variable describing living situation (homeownership versus renting or living with friends/family) and generally serves as an intra-community factor that influences neighborhood attachment and cohesion (Delnevo et al. 2011).
Neighborhood Characteristics
Neighborhood-level characteristics were obtained using US census tract 5-year estimates (2008–2012) from the American Community Survey. Participants provided their addresses and these were linked to census tracts using ArcGIS. Census tracts are relatively permanent geographic regions which are subdivisions of counties used by the US Census Bureau for statistical reporting. These tracts usually have a population size of 1,200–8,000 people with boundaries designed to capture social and economic homogeneity that generally map to neighborhoods (Kawachi and Berkman 2003; U.S. Census Bureau 2015).
Tract variables included measures of neighborhood socioeconomic disadvantage, percentage non-Hispanic Black or African American, and tract-density. Following the work of Turney and others (2010), we created a standardized index of neighborhood socioeconomic disadvantage comprised of the percentage of the tract on public assistance, percent with less than a high school education, percent unemployed, percent living below 100% of the federal poverty level, and percent of female headed households. We created z-scores for each variable and summed these standardized scores to create the neighborhood disadvantage index (α=0.84).
Census tract racial/ethnic composition was assessed using percent African American or Black. Census tract density (per square mile) was included in each of the models to account for neighborhood-level differences between dense urban areas and less dense suburban areas (Chaix et al. 2006). Each of the tract-level variables was centered using the sample mean.
Analyses
We conducted a series of random intercept multi-level Poisson regression models (Rabe-Hesketh and Skrondal 2012) to examine the effects of individual-level and neighborhood-level characteristics on mental health using the xtmepoisson command within Stata version 12 (StataCorp 2011). We fit a Poisson model to account for the dependent count variables allowing the predicted risk of mental illness symptoms to vary across neighborhoods. Random intercept models included level-1 individuals nested within level-2 census tracts (i.e., neighborhoods) to accommodate for over dispersion in the dependent variables and to model unobserved heterogeneity across neighborhoods, while treating the effects of individual factors as fixed. The residual error across neighborhoods was included as the level-2 residual term with a mean of zero and an unknown standard deviation (i.e., the estimated standard deviation of the intercept across neighborhoods σμ). All models used maximum likelihood estimation with adaptive Gaussian quadrature, adjusting for clustering at the tract-level, heteroscedastic error terms, and varying sample sizes by level of analysis (Rabe-Hesketh and Skrondal 2012) Likelihood ratio tests indicated the multilevel Poisson model was a better fit than the single-level Poisson model.
We estimated models to show the differences in risk of mental illness symptoms by race/ethnicity while additively adjusting for covariates. First, in Model 1 we considered how race was associated with mental illness symptoms after adjusting for sociodemographic characteristics (age, gender, marital status, household number) that could be sources of variation in mental illness symptoms (level-1) and objective neighborhood characteristics (neighborhood disadvantage, % African American, population density) which may impact mental health (level-2). Next, we added individual level SES (education level, poverty level, employment status, living situation/home ownership) (Model 2), and perceived neighborhood experiences (neighborhood problems, neighborhood social cohesion/trust) (Model 3) to the models. Finally, we tested a set of interaction terms to determine whether race moderated perceived discrimination and neighborhood experiences. We examined the same series of models for both depressive and anxiety symptoms to identify both similarities and unique associations across mental illness symptoms. Results are presented as incident rate ratios (IRR; exponentiated Poisson regression coefficients) and 95% confidence intervals (CI).
Results
Table 1 provides unadjusted sample characteristics by race. Compared to Whites, African Americans reported greater anxiety symptoms (mean = 2.98 [95% CI: 2.51–3.46] vs. 2.10[1.75–2.46], p ≤.001) and depressive symptoms (2.11 [1.66–2.55] vs. 1.25[1.01–1.49], p =0.004). Using census-tract derived data, African American participants lived in neighborhoods characterized by higher levels of neighborhood disadvantage (9.10 [8.55–9.65]) compared to Whites (mean = 5.12 [4.70–5.55]). They also tended to live in predominantly African American neighborhoods (56.3% African American [51.9–50.6]) whereas White participants lived in neighborhoods with lower proportions of African Americans (11.9% [9.8–14.0], p<0.001). There were no differences between African Americans and Whites on the number of years in their current address (mean =4.88 [4.29–5.46]).
Table 1.
Individual and Neighborhood-Level Descriptive Statistics of the Study Sample
| Overall |
White |
African American |
P- Value |
||||
|---|---|---|---|---|---|---|---|
| % or mean (95% CI) | % or mean (95% CI) | % or mean (95% CI) | |||||
| Mental Health | |||||||
| Mean anxiety symptoms (range 0 – 21) | 2.55 | (2.25–2.84) | 2.10 | (1.75 – 2.46) | 2.98 | (2.51–3.46) | <0.001 |
| Mean Depressive symptoms (range 0–27) | 1.68 | (1.43–1.94) | 1.25 | (1.01–1.49) | 2.11 | (1.66–2.55) | 0.004 |
| Sociodemographic Characteristics | |||||||
| Race (non-Hispanic white, ref) | |||||||
| Non-Hispanic African American, % | 50.23 | - | - | ||||
| Mean age (range 20–72) | 41.41 | (40.33–42.50) | 40.49 | (39.02–41.97) | 42.33 | (40.74–43.91) | 0.096 |
| Gender (male, ref) | |||||||
| Female, % | 50.00 | 49.77 | 50.23 | 0.924 | |||
| Marital Status (not married, ref) | |||||||
| Married /Living with partner, % | 50.23 | 55.73 | 42.93 | 0.008 | |||
| Mean household residents (range 1–5) | 2.71 | (2.58–2.84) | 2.83 | (2.64–3.03) | 2.59 | (2.41–2.77) | 0.074 |
| Socioeconomic Status | |||||||
| Education Level (Some college/college degree, ref) | |||||||
| No college education, % | 33.78 | 25.79 | 41.70 | <0.001 | |||
| Poverty level (<300% FPL, ref) | |||||||
| 300%+ FPL, % | 12.16 | 18.55 | 5.83 | <0.001 | |||
| Employment Status (Currently employed, ref) | |||||||
| Not currently employed, % | 50.23 | 41.05 | 66.67 | <0.001 | |||
| Living situation (rent or live with friend/family, ref) | |||||||
| Homeowner, % | 25.45 | 33.94 | 17.04 | <0.001 | |||
| Mean years at current address (range 0 – 37) | 4.88 | (4.29–5.46) | 4.93 | (4.13–5.73) | 4.82 | (3.97–5.67) | 0.851 |
| Discrimination and Neighborhood Experiences | |||||||
| Mean discrimination experiences (range 0 –25) | 5.94 | (5.48–6.40) | 5.13 | (4.58–5.68) | 6.74 | (6.03–7.46) | <0.001 |
| Mean neighborhood problems (range 0–2) | 0.45 | (0.41–0.49) | 0.36 | (0.31–0.40) | 0.55 | (0.49–0.61) | <0.001 |
| Mean neighborhood social cohesion/trust (range 0–4) | 2.39 | (2.30–2.47) | 2.54 | (2.42–2.66) | 2.24 | (2.11–2.36) | <0.001 |
| Neighborhood Characteristics (level-2)a | |||||||
| Mean neighborhood disadvantage (range 0–22) | 7.12 | (6.73–7.51) | 5.12 | (4.70–5.55) | 9.10 | (8.55–9.65) | <0.001 |
| Mean % African American (range 0–100) | 34.15 | (30.98–37.33) | 11.86 | (9.75–13.96) | 56.25 | (51.92–60.58) | <0.001 |
| Mean population density (per sq. mile) | 3,035.44 | (2857.80–3213.09) | 2,474.51 | (2223.31–2725.70) | 3,591.35 | (3360.60–3822.09) | <0.001 |
| N | 444 | 223 | 221 | ||||
Chi squares or 2-tailed t-tests for significant differences between non-Hispanic Whites and non-Hispanic African Americans
Includes 240 census tracts
Table 2 provides the Incidence Rate Ratios (IRRs) for risk of anxiety (Models 1a-3a) and depressive symptoms (Models 1b-3b) from multilevel Poisson regression models. In Model 1a race was significantly associated with anxiety symptoms such that African Americans showed a 33% increase in the incidence rate for anxiety symptoms compared to Whites (IRR = 1.33 [1.07–1.64], p<0.01) after controlling for demographic and objective neighborhood characteristics. The IRR for anxiety symptoms for African Americans decreased from 1.33 ([1.07–1.64], p <0.01; Model 1a) to 1.22 ([0.98–1.51], p<0.10; Model 2a) becoming non-significant when individual socioeconomic variables (education, income, employment, and homeownership) were included in the model. In Model 3a, discrimination, neighborhood problems, and neighborhood social cohesion/trust was added to build on Model 2a, and the association between race and anxiety remained non-significant (IRR = 1.17 [0.95–1.46]). Each one-unit increase in discrimination frequency was associated with an anxiety symptom increase by a factor of 1.06 (IRR = 1.06 [1.04–1.08], p<0.001]. Neighborhood social cohesion/trust was negatively associated with anxiety symptoms (IRR = 0.78 [0.71– 0.86], p<0.001) and the association between neighborhood problems and anxiety symptoms approached statistical significance (IRR = 1.22 [0.99–1.49]).
Table 2.
Multilevel Poisson Regression (Incident Rate Ratios; 95% C.I) Analysis of Mental Illness Symptoms on Discrimination, Neighborhood Experiences, and Neighborhood Characteristics
| Anxiety Symptoms | Depressive Symptoms | |||||
|---|---|---|---|---|---|---|
| Model 1a | Model 2a | Model 3a | Model 1b | Model 2b | Model 3b | |
| Race (non-Hispanic white, ref) | ||||||
| Non-Hispanic African American | 1.33** | 1.22† | 1.17 | 1.55*** | 1.38* | 1.41* |
| (1.07 – 1.64) | (0.98 – 1.51) | (0.95 – 1.46) | (1.20 – 2.01) | (1.06 – 1.79) | (1.08 – 1.84) | |
| Age (range 20–72) | 1.00 | 1.00 | 1.01 | |||
| (0.99 – 1.01) | (0.99 – 1.01) | (1.00 – 1.01) | 1.03*** | 1.03*** | 1.03*** | |
| Gender (male, ref) | 1.00 | 1.02 | 1.03 | (1.02 – 1.04) | (1.02 – 1.04) | (1.02 – 1.04) |
| Female | (0.86 – 1.17) | (0.87 – 1.19) | (0.88 – 1.21) | 0.83† | 0.88 | 0.91 |
| (0.69 – 1.00) | (0.73 – 1.06) | (0.75 – 1.11) | ||||
| Marital Status (not married, ref) | ||||||
| Married /Living with partner | 0.86† | 0.90 | 0.87 | 0.85 | 0.90 | 0.89 |
| (0.73 – 1.01) | (0.76 – 1.07) | (0.73 – 1.04) | (0.70 – 1.04) | (0.73 – 1.10) | (0.72 – 1.09) | |
| Household residents (range 1–5) | 1.02 | 1.01 | 1.05 | 1.16*** | 1.13*** | 1.16*** |
| (0.96 – 1.09) | (0.95 – 1.08) | (0.99 – 1.12) | (1.08 – 1.25) | (1.05 – 1.21) | (1.08 – 1.25) | |
| Education Level (Some college/college degree, ref) | ||||||
| No college education | 0.98 | 0.93 | 1.33** | 1.32** | ||
| (0.83 – 1.14) | (0.79 – 1.09) | (1.10 – 1.61) | (1.09 – 1.60) | |||
| Poverty level (<300% FPL, ref) | ||||||
| 300%+ FPL | 0.61** | 0.72* | 0.61** | 0.67* | ||
| (0.45 – 0.83) | (0.53 – 0.98) | (0.42 – 0.88) | (0.46 – 0.98) | |||
| Employment Status (Currently employed, ref) | ||||||
| Not currently employed | 1.17* | 1.13 | 0.99 | 0.96 | ||
| (1.00 – 1.38) | (0.96 – 1.33) | (0.81 – 1.19) | (0.79 – 1.17) | |||
| Living situation (rent or live with friend/family, ref) | ||||||
| Homeowner | 0.86 | 0.96 | 0.80† | 0.84 | ||
| (0.71 – 1.05) | (0.79 – 1.17) | (0.63 – 1.02) | (0.66 – 1.07) | |||
| Discrimination experiences (range 0 –25) | 1.06*** | 1.02* | ||||
| (1.04 – 1.08) | (1.01 – 1.04) | |||||
| Neighborhood problems scale (range 0–2) | 1.22† | 1.16 | ||||
| (0.99 – 1.49) | (0.91 – 1.46) | |||||
| Neighborhood social cohesion/trust (range 0–4) | 0.78*** | 0.84** | ||||
| (0.71 – 0.86) | (0.75 – 0.95) | |||||
| Neighborhood disadvantage index (range 0–22) | 1.01 | 1.01 | 0.99 | 1.02 | 1.01 | 1.00 |
| (0.97 – 1.05) | (0.96 – 1.05) | (0.95 – 1.03) | (0.97 – 1.07) | (0.96 – 1.06) | (0.95 – 1.05) | |
| % African American (range 0–100) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| (1.00 – 1.01) | (0.99 – 1.01) | (0.99 – 1.01) | (0.99 – 1.01) | (0.99 – 1.01) | (0.99 – 1.01) | |
| Population density (per sq. mile) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| (1.00 – 1.00) | (1.00 – 1.00) | (1.00 – 1.00) | (1.00 – 1.00) | (1.00 – 1.00) | (1.00 – 1.00) | |
| Constant | 1.44 | 1.46 | 1.27 | 0.19*** | 0.20*** | 0.20*** |
| (0.89 – 2.35) | (0.90 – 2.39) | (0.71 – 2.26) | (0.11 – 0.34) | (0.11 – 0.35) | (0.10 – 0.39) | |
| Level-2 residual standard deviation (σμ) | 0.84 | 0.84 | 0.80 | 0.85 | 0.86 | 0.86 |
| Log-likelihood | −1100.26 | −1063.57 | −1016.52 | −910.76 | −894.43 | −885.80 |
p<0.001
p<0.01
p<0.05
P<0.10
Similar relationships persisted in the depressive symptoms models. The incident rate ratios for African Americans indicated an elevated expected incidence rate of depressive symptoms across each of the models. Controlling for demographic, socioeconomic, perceived discrimination and neighborhood experiences, as well as neighborhood characteristics reduced the relative magnitude of race by approximately 22% (natural log [ln] (1.55)- ln (1.41))/ln(1.55)*100). Unlike the models for anxiety symptoms, the race effect was not fully explained by the inclusion of covariates and remained statistically significant, albeit diminished (IRR 1.41 [1.08–1.84], p<0.05). Compared to anxiety symptoms, Models 2b and 3b show similar results with nearly identical relationships between discrimination experiences, neighborhood problems and neighborhood social cohesion/trust with depressive symptoms.
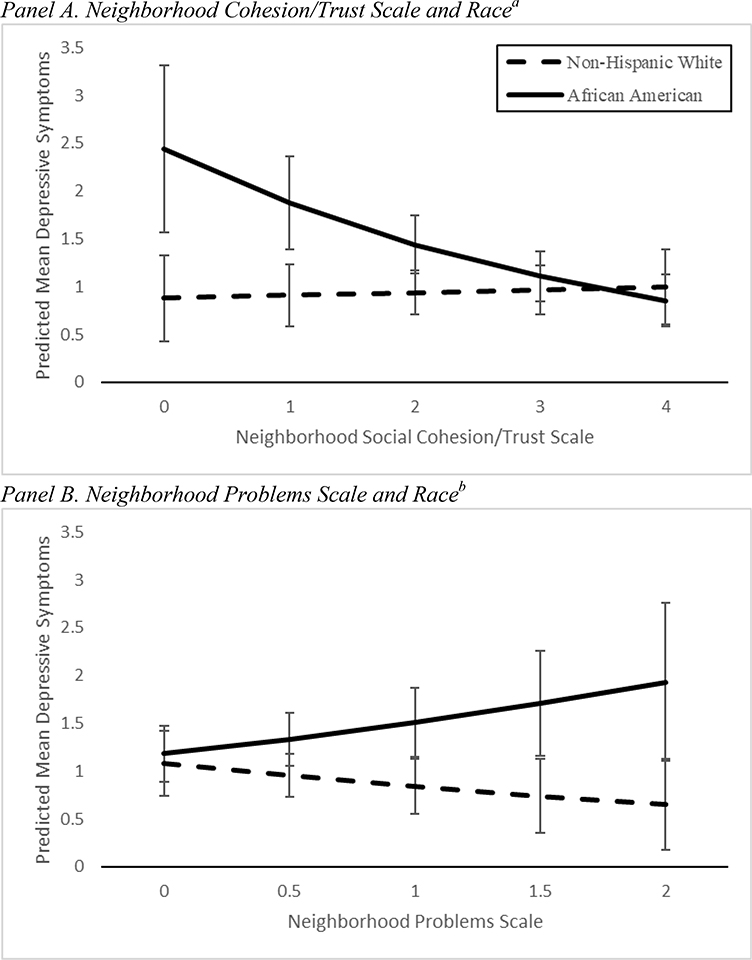
Finally, we tested for moderating interactions between race and each of the perceived stressors and neighborhood experiences. We did not find any statistically significant moderating relationships in the models for anxiety symptoms. In the case of depressive symptoms, the interaction terms with race for both neighborhood problems (IRR=1.65 [1.03–2.63], p=0.04) and neighborhood social cohesion/trust (IRR = 0.75 [0.60-.93], p=0.008) were statistically significant, while perceived discrimination was not (IRR=1.01 [0.95–1.08], p=0.73). Figure 1 illustrates these relationships by plotting the mean predicted values for the interactions based on race and scores on the problems and cohesion/trust scales, while holding all other variables at their mean values. The marginal effects (i.e., the unit increase in the probability of depressive symptoms for a change in either neighborhood problems or cohesion/trust) and confidence intervals are presented in Figure 1 (see Appendix B for model results). Marginal effects were statistically significant (p<0.01) at the lower levels of social cohesion and trust scale and when the neighborhood problems scale was between 1–1.5 as shown in Figure 1. Panel A shows that the probability of depressive symptoms generally declined with increased levels of neighborhood social cohesion, but this significantly reduced the expected means only for African Americans, whereas neighborhood social cohesion/trust did not appear to be related with depressive symptoms for Whites. Panel B indicates a similar relationship, with higher levels of neighborhood problems associated with higher predictive mean depressive symptoms, but only for African Americans.
Figure 1.
Predictive Mean Depressive Symptoms for Marginal Interaction Effects
Results of predicted margins from full multi-level Poisson models with interactions (95% C.I.)
a Main Interaction effects significant at p≤0.01 level; Marginal effects significant at p<0.001
b Main interaction significant at p<0.05; Marginal effects significant at p≤0.001
Discussion
The current study examined the relative importance of neighborhood experiences and perceived discrimination in explaining racial differences in mental health risk among low income African American and White smokers, while controlling for residential area-level characteristics. In accordance with the Environmental Affordances Model, we found that racial disparities in mental illness symptoms are due, in part, to different environments and perceptions of these environments by race (Mezuk et al. 2013). First, even though the study sample was restricted to individuals with household incomes less than 400% of the Federal Poverty Level and both groups were low income, we found that African Americans in our sample resided in more disadvantaged neighborhoods and also reported higher levels of discrimination, neighborhood problems, and lower levels of neighborhood social cohesion/trust; factors associated with mental illness symptoms. This underscores how low-income residents, but especially low income African Americans, continue to face neighborhood conditions that are systematically structured by race (Williams and Collins 2001; Do et al. 2008) with potential exposures to race-related stressors (Baumhofer et al. 2018). Findings also underscore the importance of adjusting for objective neighborhood conditions when examining mental health differences by race.
Second, African Americans smokers had greater risk of anxiety and depressive symptoms compared to Whites, even after accounting for individual and neighborhood SES, neighborhood racial composition, and density. These racial differences are consistent with the findings for depressive symptoms from a smoking cessation clinical trial with a multi-ethic sample (Webb Hooper et al. 2014). Consistent with other studies, we found that race had a stronger association with depressive symptoms than with anxiety symptoms (Everett et al. 2016). Anxiety, as assessed in this study, focused on generalized anxiety symptoms marked by worry and nervousness (Spitzer et al. 2006) and depressive symptoms focused on depressed mood and anhedonia (Kroenke et al. 2003). Differences between African Americans and Whites on anxiety symptoms in the sample were explained by living at less than 300% poverty level and being unemployed. In contrast, adjusting for perceived discrimination and neighborhood experiences indicated a slight suppressor effect for the association between race and depressive symptoms, increasing the relative importance of race on depressive symptoms by approximately 7%. This means that even if discrimination and perceived neighborhood experiences were potentially equalized, African Americans would remain at a higher risk of depressive symptoms. While this may be due to factors not measured in this study (e.g., additional stressors), it may also be due, in part, to the relative importance of neighborhood social cohesion/trust for depressive symptoms among African Americans observed in this study. We found that African Americans had higher levels of depressive symptoms than Whites when they perceived lower neighborhood social cohesion and similar reports of depressive symptoms when they perceived higher neighborhood social cohesion.
Third, our findings showed how both neighborhood problems and neighborhood social cohesion/trust moderated the relationship between race and depressive symptoms, but not anxiety symptoms. African Americans reporting low levels of neighborhood social cohesion/trust had significantly greater risk of depressive symptoms than Whites, but this differential risk decreased with higher levels of cohesion emphasizing the potential role of efforts to build neighborhood cohesion. Similarly, we found that reports of higher numbers of neighborhood problems resulted in marked increases in the risk of depressive symptoms for African Americans. At higher levels of neighborhood social cohesion/trust and lower levels of neighborhood problems, the racial disparity between African American and White smokers at risk for depressive symptoms became negligible. Again, these factors represent modifiable targets for intervention. Thus, African Americans may be more heavily impacted by intangible neighborhood social supports and environmental stressors than Whites, suggesting the relative importance of community public health investment in disadvantaged neighborhoods with particular attention to social cohesion and reduction of visible disorder. This finding contradicts some previous research suggesting that social cohesion/trust primarily benefits Whites (Gary et al. 2007) and that the associations between perceived neighborhood characteristics and depressive symptoms were no different between races (Echeverría et al. 2008). These previous studies stratified all analyses by race, whereas, the current study adjusted for objective neighborhood factors and tested moderation effects allowing us to further identify specific relationships that differed by race. Taken together, these results continue to highlight how both perceived and objective neighborhood factors may have different implications for mental health outcomes (Williams et al. 1997).
Limitations
Neighborhood-level SES and mental illness symptoms showed statistically significant bivariate associations (see supplemental table online), but, similar to findings from a large, national survey, these became non-significant within the multilevel framework (Moore et al. 2016). However, each neighborhood represented in this study had an average of two participants which potentially led to reduced neighborhood-level variance and biased estimates of the level-2 standard errors that made it challenging to present meaningful random effects (Maas and Hox 2005). Consistent with many studies that use U.S. Census tract data, we are unable to determine whether this geography appropriately and accurately represents a meaningful neighborhood among our sample. In part the lack of findings at the tract-level may have to do with perceptions of space and contextual influences on health outcomes that vary across studies (Diez-Roux 1998; Cummins 2007). The lack of consistency with some other studies may be in part due to either mis-specified spatial schemes (i.e., modifiable areal unit problem) or obscured contextual effects (i.e., Uncertain Geographic Context Problem). Our data limit us on the inclusion of other indicators of residential space to address these potential measurement issues (Wong 2004; Openshow 1979; Kwan 2012). Future explorations with larger sample sizes and more geographic heterogeneity would benefit from the inclusion of more dynamic and subjective neighborhood measures to provide more precise estimates (Lee et al. 2008) and to assess effects across various measures of context (Shi 2009).
Future studies would need to include more populated neighborhoods to consider how neighborhood experiences (e.g., problems, social cohesion/trust, discrimination) vary across different types of neighborhoods (i.e., random slope models). Another limitation of this study is that we excluded individuals with reported past mental illness. The parent study excluded smokers who had been treated for depression in the past year (11.5% of 1537 screened) and who had a history of anxiety or bipolar disorders (8.5%) because these were contraindicated for varenicline use (Nollen et al. 2016). Yet, this also serves as a potential strength as these findings demonstrate how perceptions of neighborhood factors related to subclinical and undiagnosed mental health problems. Finally, the recruitment of the sample from one region in the Midwest may not capture geographic variations of a large, nationally representative sample. However, this also enabled us to describe the effects of race, SES, and residential area characteristics on psychological distress within a well-defined but heterogeneous geographic area.
Conclusions
The focus of this paper was on understanding contextual factors associated with mental health among a sample of lower income African American and White smokers. Lower income smokers are at greater risk than the general population for continued smoking (Reid et al. 2010) and, in turn, the development of tobacco-related disease. Smoking rates are higher among persons with mental health disorders with lower rates of decline in smoking prevalence than in the general population (Cook et al. 2014). This study highlights the pervasive mental health risks experienced by lower income smokers, including discrimination, lack of neighborhood social cohesion, and neighborhood problems. Within our sample, African Americans had greater anxiety and depressive symptoms, experienced more discrimination, lower social cohesion/trust, and more neighborhood problems than Whites. These findings highlight the powerful influence of neighborhood experiences in which African Americans continue to be disadvantaged, and underscore the need to develop and evaluate public health interventions that address social and environmental contexts (Cooper et al. 2015). Place-based policies have the potential to address mental health needs through housing conditions, mental health services, or health behaviors (Turney et al. 2013). Interventions to promote mental health and reduce unhealthy coping behaviors, such as smoking, among lower income communities may do well to target strengthening positive social ties, community participation, and reducing exposure to neighborhood-specific problems (e.g., crime, disorder), particularly for African Americans (e.g., Hull et al. 2008). This may be possible through mobilizing social media linkages and capacity-building among existing neighborhood organizations. Efforts to reduce observable signs of disorder (e.g. litter, noise) and improve neighborhood aesthetics (Henderson et al. 2016) may also be appropriate targets.
Supplementary Material
ACKNOWLEDGEMENTS
The clinical trials registration number for the parent study is NCT01836276. This work was supported by the National Institute on Drug Abuse (R01-DA031815 to NLN) and by a Diversity Supplement (R01 DA031815-S1; TSS). Pfizer Global Pharmaceuticals provided the medication for the parent study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Conflict of Interest: This work was supported by the NIH, National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health. The study sponsor had no role in study design; collection, analysis, or interpretation of data; writing the report; or the decision to submit the report for publication. None of the authors have institutional or corporate affiliations that conflict with this study, and no financial disclosures were reported by the authors of this paper.
References
- Almedom AM (2005). Social capital and mental health: An interdisciplinary review of primary evidence. Social Science and Medicine, 61(5), 943–964, doi: 10.1016/j.socscimed.2004.12.025. [DOI] [PubMed] [Google Scholar]
- Aneshensel CS, & Sucoff CA (1996). The Neighborhood Context of Adolescent Mental Health. Journal of Health and Social Behavior, 37(4), 293–310, doi: 10.2307/2137258. [DOI] [PubMed] [Google Scholar]
- Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, & Subramanian SV (2016). Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Social Science and Medicine, 168(Supplement C), 16–29, doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumhofer NK, Panapasa SV, Cook EF, & Williams DR (2018). Association of cultural affinity and island food consumption in the Pacific Islander health study. Ethnicity and Health, 1–17, doi: 10.1080/13557858.2018.1547815. [DOI] [PubMed] [Google Scholar]
- Bécares L (2012). Ethnic Density Effects on Physical Morbidity, Mortality, and Health Behaviors: A Systematic Review of the Literature. American Journal of Public Health, 102(12), e33–e66, doi: 10.2105/AJPH.2012.300832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B, Rosvall M, Lynch J, & Merlo J (2006). Disentangling contextual effects on cause-specific mortality in a longitudinal 23-year follow-up study: impact of population density or socioeconomic environment? International Journal of Epidemiology, 35(3), 633–643, doi: 10.1093/ije/dyl009. [DOI] [PubMed] [Google Scholar]
- Cook B, Wayne G, Kafali E, Liu Z, Shu C, & Flores M (2014). Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA, 311(2), 172–182, doi: 10.1001/jama.2013.284985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Ortega AN, Ammerman AS, Buchwald D, Paskett ED, Powell LH, et al. (2015). Calling for a Bold New Vision of Health Disparities Intervention Research. American Journal of Public Health, 105(S3), S374–S376, doi: 10.2105/AJPH.2014.302386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummins S (2007). Commentary: investigating neighbourhood effects on health—avoiding the ‘local trap’. International Journal of Epidemiology, 36(2), 355–357. [DOI] [PubMed] [Google Scholar]
- Delnevo CD, Gundersen DA, Hrywna M, Echeverria SE, & Steinberg MB (2011). Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. American Journal of Preventive Medicine, 41(4), 357–365, doi: 10.1016/j.amepre.2011.06.039. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services, & Office of the Secretary (2012). Annual Update of the HHS Poverty Guidelines, 42. U.S.C. 9902 (2). Federal Register, 77(17), 4034–4035. [Google Scholar]
- Diez-Roux AV (1998). Bringing context back into epidemiology: variables and fallacies in multilevel analysis. American Journal of Public Health, 88(2), 216–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do DP, Finch BK, Basurto-Davila R, Bird C, Escarce J, & Lurie N (2008). Does place explain racial health disparities? Quantifying the contribution of residential context to the Black/white health gap in the United States. Social Science and Medicine, 67(8), 1258–1268, doi: 10.1016/j.socscimed.2008.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Echeverría S, Diez-Roux AV, Shea S, Borrell LN, & Jackson S (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health & place, 14(4), 853–865. [DOI] [PubMed] [Google Scholar]
- English D, Lambert SF, Evans MK, & Zonderman AB (2014). Neighborhood racial composition, racial discrimination, and depressive symptoms in African Americans. American Journal of Community Psychology, 54(3–4), 219–228, doi: 10.1007/s10464-014-9666-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett BG, Saint Onge JM, & Mollborn S (2016). Effects of Minority Status and Perceived Discrimination on Mental Health. Population Research and Policy Review, 35(4), 445–469, doi: 10.1007/s11113-016-9391-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gary TL, Stark SA, & LaVeist TA (2007). Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health Place, 13(2), 569–575, doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Henderson H, Child S, Moore S, Moore JB, & Kaczynski AT (2016). The Influence of Neighborhood Aesthetics, Safety, and Social Cohesion on Perceived Stress in Disadvantaged Communities. American Journal of Community Psychology, 58(1–2), 80–88, doi: 10.1002/ajcp.12081. [DOI] [PubMed] [Google Scholar]
- Himle JA, Baser RE, Taylor RJ, Campbell RD, & Jackson JS (2009). Anxiety disorders among African Americans, blacks of Caribbean descent, and non-Hispanic whites in the United States. Journal of Anxiety Disorders, 23(5), 578–590, doi: 10.1016/j.janxdis.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull P, Kilbourne B, Reece M, & Husaini B (2008). Community involvement and adolescent mental health: Moderating effects of race/ethnicity and neighborhood disadvantage. Journal of Community Psychology, 36(4), 534–551. [Google Scholar]
- Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, & Graffunder CM (2016). Current Cigarette Smoking Among Adults — United States, 2005–2015. MMWR: Morbidity and Mortality Weekly Report, 65(44), 1205–1211, doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- Kawachi I, & Berkman LF (Eds.). (2003). Neighborhoods and Health (First Edition ed., Medicine). New York, NY: Oxford University Press. [Google Scholar]
- Krieger N, Kosheleva A, Waterman PD, Chen JT, & Koenen K (2011). Racial Discrimination, Psychological Distress, and Self-Rated Health Among US-Born and Foreign-Born Black Americans. American Journal of Public Health, 101(9), 1704–1713, doi: 10.2105/ajph.2011.300168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care, 41(11), 1284–1292, doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- Kwan M-P (2012). The uncertain geographic context problem. Annals of the Association of American Geographers, 102(5), 958–968. [Google Scholar]
- Lawrence D, Mitrou F, & Zubrick SR (2009). Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health, 9, 285, doi: 10.1186/1471-2458-9-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence D, & Williams JM (2016). Trends in Smoking Rates by Level of Psychological Distress—Time Series Analysis of US National Health Interview Survey Data 1997–2014. Nicotine & tobacco research, 18(6), 1463–1470, doi: 10.1093/ntr/ntv272. [DOI] [PubMed] [Google Scholar]
- Lee BA, Reardon SF, Firebaugh G, Farrell CR, Matthews SA, & O’Sullivan D (2008). Beyond the census tract: Patterns and determinants of racial segregation at multiple geographic scales. American Sociological Review, 73(5), 766–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maas CJM, & Hox JJ (2005). Sufficient Sample Sizes for Multilevel Modeling. Methodology: European Journal of Research Methods for the Behavioral and Social Sciences, 1(3), 86–92, doi: 10.1027/1614-2241.1.3.86. [DOI] [Google Scholar]
- Mair C, Diez Roux AV, Osypuk TL, Rapp SR, Seeman T, & Watson KE (2010). Is neighborhood racial/ethnic composition associated with depressive symptoms? The multi-ethnic study of atherosclerosis. Social Science and Medicine, 71(3), 541–550, doi: 10.1016/j.socscimed.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair C, Roux AVD, & Galea S (2008). Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. Journal of Epidemiology and Community Health (1979-), 62(11), 940–946. [DOI] [PubMed] [Google Scholar]
- Mair C, Roux AVD, Shen M, Shea S, Seeman T, Echeverria S, et al. (2009). Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the multiethnic study of atherosclerosis. Annals of Epidemiology, 19(1), 49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC, & Taylor SE (2010). Are psychosocial factors mediators of socioeconomic status and health connections? A progress report and blueprint for the future. Annals of the New York Academy of Sciences, 1186, 146–173, doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Abdou CM, Hudson D, Kershaw KN, Rafferty JA, Lee H, et al. (2013). “White Box” Epidemiology and the Social Neuroscience of Health Behaviors: The Environmental Affordances Model. Soc Ment Health, 3(2), doi: 10.1177/2156869313480892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KA, Hirsch JA, August C, Mair C, Sanchez BN, & Roux AVD (2016). Neighborhood Social Resources and Depressive Symptoms: Longitudinal Results from the Multi-Ethnic Study of Atherosclerosis. [journal article]. Journal of Urban Health, 93(3), 572–588, doi: 10.1007/s11524-016-0042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nollen NL, Cox LS, Yu Q, Ellerbeck EF, Scheuermann TS, Benowitz NL, et al. (2016). A clinical trial to examine disparities in quitting between African-American and White adult smokers: Design, accrual, and baseline characteristics. Contemporary Clinical Trials, 47, 12–21, doi: 10.1016/j.cct.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Openshow S (1979). A million or so correlation coefficients, three experiments on the modifiable areal unit problem. Statistical applications in the spatial science, 127–144. [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: a meta-analytic review. Psychological Bulletin, 135(4), 531–554, doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse AL, Todd NR, Neville HA, & Carter RT (2012). Perceived racism and mental health among Black American adults: A meta-analytic review. Journal of Counseling Psychology, 59(1), 1–9, doi: 10.1037/a0026208. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, & Skrondal A (2012). Multilevel and Longitudinal Modeling Using Stata (Third Edition ed.). College Station, TX: Stata Press. [Google Scholar]
- Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M, & Collaboration, o. b. o. t. I. (2010). Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: Findings from the International Tobacco Control Four Country Survey. Nicotine & tobacco research, 12(suppl_1), S20–S33, doi: 10.1093/ntr/ntq051 %J Nicotine & Tobacco Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriquez EJ, Livaudais-Toman J, Gregorich SE, Jackson JS, Napoles AM, & Perez-Stable EJ (2018). Relationships between allostatic load, unhealthy behaviors, and depressive disorder in U.S. adults, 2005–2012 NHANES. Preventive Medicine, 110, 9–15, doi: 10.1016/j.ypmed.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross CE (2000). Neighborhood Disadvantage and Adult Depression. Journal of Health and Social Behavior, 41(2), 177–187, doi: 10.2307/2676304. [DOI] [Google Scholar]
- Ross CE, & Mirowsky J (2009). Neighborhood Disorder, Subjective Alienation, and Distress∗. Journal of Health and Social Behavior, 50(1), 49–64. [DOI] [PubMed] [Google Scholar]
- Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, & Batty GD (2012). Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ : British Medical Journal, 345, doi: 10.1136/bmj.e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, & Earls F (1997). Neighborhoods and violent crime: a multilevel study of collective efficacy. Science, 277(5328), 918–924. [DOI] [PubMed] [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, & Garcia A (2014). The Consequences of Perceived Discrimination for Psychological Well-Being: A Meta-Analytic Review. Psychological Bulletin, 140(4), 921–948, doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- Shell AM, Peek MK, & Eschbach K (2013). Neighborhood Hispanic composition and depressive symptoms among Mexican-descent residents of Texas City, Texas. Social Science and Medicine, 99, 56–63, doi: 10.1016/j.socscimed.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi W (2009). Principles of modeling uncertainties in spatial data and spatial analyses: CRC press. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Lowe B (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097, doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- StataCorp (2011). Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. [Google Scholar]
- Steptoe A, & Feldman PJ (2001). Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine, 23(3), 177–185. [DOI] [PubMed] [Google Scholar]
- Sternthal MJ, Slopen N, & Williams DR (2011). Racial Disparities in Health. Du Bois Review: Social Science Research on Race, 8(01), 95–113, doi:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockdale SE, Wells KB, Tang L, Belin TR, Zhang L, & Sherbourne CD (2007). The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Social Science and Medicine, 65(9), 1867–1881, doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turney K, & Harknett K (2010). Neighborhood Disadvantage, Residential Stability, and Perceptions of Instrumental Support among New Mothers. J Fam Issues, 31(4), 499–524, doi:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turney K, Kissane R, & Edin K (2013). After moving to opportunity: how moving to a low-poverty neighborhood improves mental health among African American women. Society and Mental Health, 3(1), 1–21. [Google Scholar]
- U.S. Census Bureau (2015). Geographic Terms and Concepts Census Tract. https://www.census.gov/geo/reference/gtc/gtc_ct.html. Accessed July 19 2016.
- Webb Hooper M, Baker EA, & McNutt MD (2014). Racial/Ethnic differences among smokers: revisited and expanded to help seekers. Nicotine Tob Res, 16(5), 621–625, doi: 10.1093/ntr/ntt206. [DOI] [PubMed] [Google Scholar]
- Weissman J, Pratt LA, Miller EA, & Parker JD (2015). Serious Psychological Distress Among Adults, United States, 2009–2013: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- Williams DR, & Collins C (2001). Racial Residential Segregation: A Fundamental Cause of Racial Disparities in Health. Public Health Reports, 116(5), 404–416, doi:doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry, 64(3), 305–315, doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams DR, John DA, Oyserman D, Sonnega J, Mohammed SA, & Jackson JS (2012). Research on Discrimination and Health: An Exploratory Study of Unresolved Conceptual and Measurement Issues. American Journal of Public Health, 102(5), 975–978, doi: 10.2105/AJPH.2012.300702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2013). Racism and Health I: Pathways and Scientific Evidence. The American behavioral scientist, 57(8), 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. Journal of Health Psychology, 2, 335–351, doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wong DW (2004). Comparing Traditional and Spatial Segregation Measures: A Spatial Scale Perspective. Urban Geography, 25(1), 66–82. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.