Introduction
Embolization of lesions fed by branches of the external carotid artery (ECA) has become a common and accepted practice to provide primary or adjunctive therapy of lesions fed by this arterial territory. Primary therapy is intended to effect a resolution of the problem via ECA embolization alone. Adjunctive therapy is usually performed before surgery to reduce blood loss, facilitate lesion removal, and reduce surgical risk (1).
The following guidelines are intended for use in quality improvement programs to evaluate ECA embolizations. Assessment guidelines include indications for embolization, success rates for achieving embolization goals, and complication rates.
Discussion
ECA embolization may be defined as endovascular occlusion of branches of the ECA in an attempt to terminate or reduce blood flow to a lesion in the head, neck, or skull base region. The procedure is usually performed in conjunction with diagnostic angiography and most often is completed in one session.
The embolic materials most commonly used in this arterial distribution are particulate materials (ie, polyvinyl alcohol sponge particles; Gelfoam sponge or powder; Avitene; Embospheres; pushable, fibered or nonfibered coils; electronically detachable, mechanically detachable, or injectable coils) (2, 3). Liquid agents include acrylic adhesives and sclerosants such as absolute alcohol and hypertonic glucose. The choice of the embolic agent is made on the basis of the intended goal of embolization (preoperative versus primary therapy), the inclusion of normal tissue in the embolic field, and the level of performance necessary. All liquid agents and small particles (smaller than approximately 200 µ) penetrate deeply into small normal vessels and may create severe ischemia, resulting in undesirable side effects such as skin necrosis and cranial nerve palsy. These unfavorable effects may be reduced by careful evaluation of superselective angiograms and provocative pharmacologic testing before embolization (4).
Indications
The common indications for ECA embolization are the primary treatment of a disease process affecting the vascular territory of the ECA (eg, epistaxis, arteriovenous fistula [AVF]) or the adjunctive reduction of blood flow to a lesion preoperatively. Preoperative embolizations may be indicated to control surgically inaccessible arterial feeders, reduce surgical blood loss, shorten the surgical procedure time, and increase the probability of total lesion resection. ECA embolization is typically considered appropriate in cases of hypervascular tumors, hemorrhage, and vascular malformations.
Hypervascular tumors (5–16) include juvenile nasopharyngeal angiofibromas, paragangliomas, meningiomas, neurogenic tumors, benign or metastatic bone tumors, and hemangiomas. Control of hemorrhage is sometimes needed in association with epistaxis (idiopathic or traumatic) (17–20), penetrating trauma, exsanguination from tumor, and postoperative complications (eg, pseudoaneurysms). Vascular malformations (21–25) include AVMs, fistulae, and dural AVF.
Threshold: 100%
When ECA embolization is performed for lesions without an established indication, a review should be conducted.
Efficacy
The indications of efficacy are technical and clinical success. Technical success is defined as occlusion of the targeted vessels. Clinical success may include improvement or alleviation of symptoms associated with the lesion or appropriate preparation of a lesion for surgical resection.
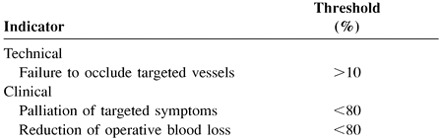 |
Safety
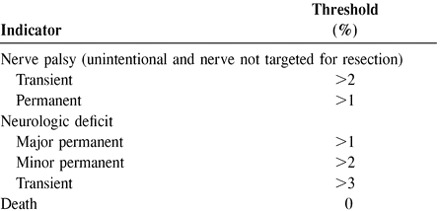
Undesirable outcomes or effects are known to occur in association with embolization. These include clinical and technical complications, and each can be categorized as severe or minor and as permanent or transient.
Threshold:
When complication thresholds are exceeded, a review should be conducted.
 |
References
- 1.Macpherson P, The value of pre-operative embolisation of meningioma estimated subjectively and objectively. Neuroradiology 1991;33:334-337 [DOI] [PubMed] [Google Scholar]
- 2.Dion JE, Principles and methodology. In: Viñuela F, Halbach VV, Dion JE, eds. Interventional Neuroradiology. New York: Raven Press. 1992:11–15
- 3.Lasjaunias P, Berenstein A, Technical aspects of surgical neuroradiology. In Surgical Neuroradiology vol 1: Berlin: Springer-Verlag 1987;1-56 [Google Scholar]
- 4.Horton JA, Kerber CW, Lidocaine injection into external branches: provocative test to preserve cranial nerve function in therapeutic embolization. AJNR Am J Neuroradiol 1986;7:105-108 [PMC free article] [PubMed] [Google Scholar]
- 5.Standard SC, Ahuja A, Livingston K, Guterman LR, Hopkins LN, Endovascular embolization and surgical excision for the treatment of cerebellar and brain stem hemangioblastomas. Surg Neurol 1994;41:405-410 [DOI] [PubMed] [Google Scholar]
- 6.Radkowski D, McGill T, Healy GB, Ohlms L, Jones DT, Angiofibroma: changes in staging and treatment. Arch Otolaryngol Head Neck Surg 1996;122:122-129 [DOI] [PubMed] [Google Scholar]
- 7.Deschler DG, Kaplan MJ, Boles R, Treatment of large juvenile nasopharyngeal angiofibroma. Otolaryngol Head Neck Surg 1992;106:278-284 [DOI] [PubMed] [Google Scholar]
- 8.Bishop GB Jr, Urist MM, Gammal T, Peters GE, Maddox WA, Paragangliomas of the neck. Arch Surg 1992;127:1441-1445 [DOI] [PubMed] [Google Scholar]
- 9.Wiet RJ, Harvey SA, O'Connor CA, Recent advances in surgery of the temporal bone and skull base. Southern Med J 1993;86:5-12 [DOI] [PubMed] [Google Scholar]
- 10.Wax MK, Briant TD, Carotid body tumors: a review. J Otolaryngol 1992;21:277-285 [PubMed] [Google Scholar]
- 11.Abramowitz J, Dion JE, Jensen ME, Angiographic diagnosis and management of head and neck schwannomas. AJNR Am J Neuroradiol 1991;12:977-984 [PMC free article] [PubMed] [Google Scholar]
- 12.Manelfe C, Lasjaunias P, Ruscalleda J, Preoperative embolization of intracranial meningiomas. AJNR Am J Neuroradiol 1986;7:963-972 [PMC free article] [PubMed] [Google Scholar]
- 13.Richter HP, Schachenmayr W, Preoperative embolization of intracranial meningiomas. Neurosurgery 1983;13:261-268 [DOI] [PubMed] [Google Scholar]
- 14.Hieshima GB, Everhart FR, Mehringer CM, Preoperative embolization of hemangiomas. Surg Neurol 1980;14:119-127 [PubMed] [Google Scholar]
- 15.Ahuja A, Gibbons KJ, Endovascular therapy of central nervous system tumors. Neurosurg Clin N Am 1994;5:541-554 [PubMed] [Google Scholar]
- 16.Platzbecker H, Kohler K, Embolization in the head and neck region. Acta Radiol Suppl 1991;377:25-26 [PubMed] [Google Scholar]
- 17.Davis KR, Embolization of epistaxis and juvenile nasopharyngeal angiofibromas. AJR Am J Roentgenol 1987;148:209-218 [DOI] [PubMed] [Google Scholar]
- 18.Vitek J, Idiopathic intractable epistaxis: endovascular therapy. Radiology 1991;181:113-116 [DOI] [PubMed] [Google Scholar]
- 19.Sokoloff J, Wickbom I, McDonald D, Brahme F, Goergen TC, Goldberger LE, Therapeutic percutaneous embolization in intractable epistaxis. Radiology 1974;111:285-287 [DOI] [PubMed] [Google Scholar]
- 20.Hicks JN, Vitek G, Transarterial embolization to control posterior epistaxis. Laryngoscope 1989;99:1027-1029 [DOI] [PubMed] [Google Scholar]
- 21.Komiyama M, Khosla VK, Yamamoto Y, Tazaki H, Toyota N, Embolization in high-flow arteriovenous malformations of the face. Ann Plast Surg 1992;28:575-583 [PubMed] [Google Scholar]
- 22.Stal S, Hamilton S, Spira M, Hemangiomas, lymphangiomas, and vascular malformations of the head and neck. Otolaryngol Clin North Am 1986;19:769-796 [PubMed] [Google Scholar]
- 23.Mulliken JB, Glowacki J, Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-422 [DOI] [PubMed] [Google Scholar]
- 24.Lasjaunias P, Berenstein A, Craniofacial vascular lesions: general. In: Surgical Neuroangiography vol 2: Berlin: Springer-Verlag 1987;317-340 [Google Scholar]
- 25.Berenstein A, Scott J, Choi IS, Persky M, Percutaneous embolization of arteriovenous fistulas of the external carotid artery. AJNR Am J Neuroradiol 1986;7:937-942 [PMC free article] [PubMed] [Google Scholar]


