Abstract
High-level toxic metal exposure has become rare in the recent years. Although, it has not known whether relatively lower exposure may adversely affect human reproductive system. Spontaneous abortion (SA) is a serious reproductive problem, which, in many cases, the cause(s) is not clearly understood. To assess the relationship between prenatal blood level of metals and SA risk, we compared blood concentration of some heavy metals in samples taken from mothers recruited in Tehran Environment and Neurodevelopmental Defects (TEND) study conducted on apparently healthy pregnant women in Tehran, Iran who subsequently experienced spontaneous abortion with mothers who their pregnancy ended to live births. During early gestation, 206 women were enrolled to the survey and followed up till fetal abortion or baby deliveries occur. Blood metal concentrations were measured using an inductively coupled plasma mass spectrometer. The mean blood levels of lead, antimony, and nickel were higher in SA than ongoing pregnancy; however, this difference was not statistically significant. When adjusted for covariates, the logistic regression analysis showed significant association between maternal age and the risk of SA in all models. Among toxic metals only antimony had a noticeable positive relation with the risk of SA (OR: 1.65, 95% CI:1.08–2.52, P value: 0.02). Pearson’s correlation coefficient showed significant (P < 0.05) positive correlations among prenatal blood metals levels, except for nickel. Although the present study failed to provide strong evidence for the effects of toxic metals on the occurrence of SA at the relatively low-levels, these metals should be avoided in women who plan pregnancy and/or during the early stages of gestation to prevent the chance of adverse effects.
Keywords: Toxic metal, Pregnancy, Spontaneous abortion, Blood, Antimony
Introduction
Toxic metals, such as lead and cadmium, are ubiquitous environmental pollutants. Human exposure commonly occurs through foods and industrial activities. Despite extensive efforts and strict regulations, clinical and subclinical poisoning of some toxic metals still occurs and continues to rise in developing nations [1]. Although high-level toxic metal exposure becoming rare in the recent years, it has not been yet known whether relatively lower concentrations may adversely affect human reproductive system. In addition, many of these metals can accumulate in some parts of human body (i.e., bones, hair, and red blood cells) [2, 3], then, release form retained organs and increase blood concentrations during highly exchangeable period, such as pregnancy [4, 5]. These elements (i.e., lead, nickel, chromium, mercury, and cadmium) in pregnant women’s blood can pass through the placenta barrier to the fetus, in different rates, and increase the risk of adverse effects, such as pregnancy induced-hypertension, premature delivery, low birth weight, fetal loss, and stillbirth [6–12].
Spontaneous abortion (SA) is a serious reproductive problem, occurring in 10–15% of pregnancies [13]. Although the cause(s) of SA has not clearly been understood, about 60% of cases are thought to result from physiological/anatomic disorders, gene anomaly, infections, hormonal disruptions, immunologic problems; or they may be related to diseases, such as diabetes mellitus and thyroid dysfunction [14, 15]. Epidemiologic studies indicate that prenatal exposure to toxic metals (lead, mercury, nickel, arsenic, chromium, antimony, bismuth, and cadmium), measured in maternal blood or placenta, can increase the probability of SA and stillbirths occurrence [1, 3, 16–21]. For instance, increased maternal blood cadmium and lead can increase the risk of miscarriage, up to 2-fold, than control group [3, 22]. In addition, SA were reported in 16% of nickel-exposed female workers compared with 9% in the construction workers [23]. Although reproductive toxicant of some toxic metals have been shown in deferent researches, the direct effects on SA risk have not been completely elucidated yet [24–26].
Consistent evidences have tended to indicate an increase SA risk at high levels of metals concentrations. However, influence of the relatively lower levels (i.e., < 5 μg/dL for lead), which frequently occurs in many industries and/or in general population, has not been elucidated yet. To assess the effects of prenatal whole blood metals on SA risk, we employed the data of a birth cohort study (Tehran Environment and Neurodevelopmental Disorder, TEND) on apparently healthy pregnant women, begun in March 2016.
Methods
Study participants
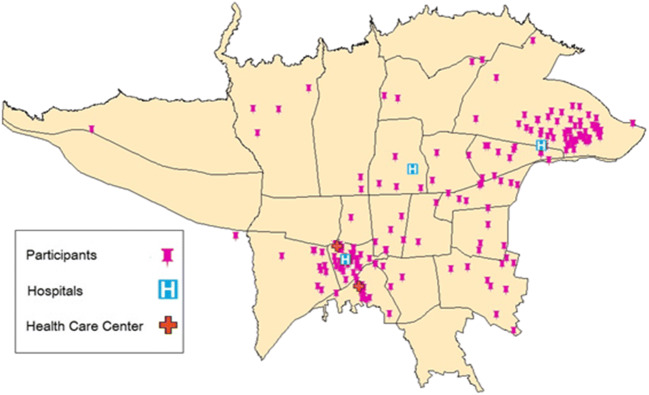
The present study was conducted in Tehran, the capital of Iran, with the population of more than 8.7 million (according to 2016 national census). The city is divided into 22 administrative districts with an area of 613 km2 [27]. Tehran has a significant variation of environmental exposures, socioeconomic conditions, and health care services availability. We recruited pregnant women who administered for prenatal care to three teaching hospitals and two healthcare centers of Tehran University of Medical Sciences (TUMS), located in different areas of the city. Figure 1 shows the location of the research sites and participants’ inhabitance. The survey data gathering and sample collection were conducted from March 2016 to October 2017.
Fig. 1.
Location of the research sites and participants residency places in Tehran map
The survey inclusion criteria were: (1) Iranian nationality; (2) Tehran city inhabitant; (3) gestational age 10 to16 weeks at the time of sampling; and (4) deciding to give birth at one of our research hospitals. The study participants did not have known chronic conditions, such as cancer, diabetes, hypertension at the time or survey recruitment. The TUMS Ethical Committees reviewed and approved the study design, procedures, and informed consent format (permission No: IR.TUMS.REC.1394.1180). All participants received verbal explanation of the purpose and procedures of the study. If they had agreed to participate to the survey, signed the informed consent in purely voluntary situation.
Of 838 pregnant women referred for prenatal care during the study recruitment period, about 25% (n = 206) women had gestational age between 10 and 16 week (confirmed by ultrasound imaging report), and agreed to participate to the survey. Blood sampling requirement was one of the main causes of women declined participation in the study. After blood sample collection in the first trimester of pregnancy, the study participants were followed till abortion or baby delivery.
Data gathering
We developed a structured questionnaire to gather participants’ information, through a face-to-face interview by trained research staffs, for socio-demographic characteristics, life style/habits, medical/pregnancy histories (if any), and occupational/environmental exposures. The pregnant women were followed and classified as SA, if fetal demise occurred before 20thweeks of gestation. In case of the study participants did not give delivery in the research hospitals, we gathered the pregnancy outcomes information using a telephone call. The women’s height was measured to the nearest centimeter using a rigid stadiometer, which was rigorously checked for accuracy. Using a standard balance beam scale, which was calibrated every day, maternal weight (kg) was measured. Body mass index (BMI) was calculated as the weight (kg) divided by square of the height (m2). Gestational age (the age of a pregnancy) is described how far along the pregnancy, measured in weeks, from the first day of the woman’s last menstrual period (LMP) to the current date, which was confirmed by ultrasound.
Collection and analysis of blood samples
Venous blood samples were collected at the early gestation from the cubital vein by vacuum tubes (Venoject VP-H070K, Terumo, Tokyo, Japan) in the morning, when the participants were overnight fasting. Using a cool box with the cold chain condition, collected blood were transferred to the TUMS Central Laboratory Complex and stored in the deep-freezer (−80 °C) before sending to Japan for blood metal measurement. We have measured concentration of many toxic metals for the current study. However, some of them were at undetectable levels (up to 80% of samples, i.e., cobalt) or need different measurement methods or devices (i.e., mercury). Thus, only data for lead, cadmium, antimony, and nickel were used for statistical analysis. For whole blood metals measurement, the blood samples (0.1 ml) were put into a perfluoroalkoxyteflon bottle, then 0.4 ml of concentrated nitric acid (Ultrapure Grade, Tama Chemicals Co., Kawasaki, Japan) was added and the samples left overnight. The sample mixture was digested with 0.2 ml hydrogen peroxide (Ultrapure Grade, Tama Chemicals Co., Kawasaki, Japan) in a microwave oven (MLS-1200 MEGA, Milestone S.R.L., Bergamo, Italy) in five steps with power set at 250, 0, 250, 400 and 600 W for 5, 1, 5, 5, and 5 min, respectively; the volume of the digested sample was then adjusted to 1.0 ml with ultrapure water. After dilution with 0.5% nitric acid, the metal concentrations were measured using an inductively coupled plasma mass spectrometer (ICP-MS, Eran DRC-II, PerkinElmer, Waltham, MA, USA) using an external multi-element standard solution (XSTC-13SPEX CertiPrep. Inc., Metuchen, NJ, USA). The blood metal measurements were repeated three times and the average was used for subsequent analysis. For instrument calibration throughout the measurements, at least 10% of the analyses were the external standard, and 5% were blank (pure water).
Quality control and detection limits
We analyzed the quality control materials Seronorm Trace Elements Whole Blood control in three levels (Sero, Billingstad, Norway). The limit of detection (LOD) and the limit of quantification (LOQ) were the concentration equivalent to the signal of each element, which was equal to 3 and 10 times the standard deviation of 10 repeated measurements of the blank signal.
Data analysis
Using the Student t-test, we examined differences in continuous variables between women with SA and ongoing pregnancies. For nominal variable comparison between the two groups we employed Chi-square test and Fischer exact test, when applicable. Pearson correlation coefficient was used to study relationships among the blood metal levels and gestational age at the time of delivery. To examine whether prenatal blood metal exposure is independently associated with the risk of SA (as a dependent variable: SA = 1 and non-abortion = 0), we performed multiple logistic regression analysis, estimating odds ratios (OR) and 95% confidence intervals (CI), using the enter method. The model was adjusted for potential sources of confounders, including maternal age, parity, and a history of previous abortion. Then, we added each metal to the model separately. P-values less than 0.05 were considered to be statistically significant. The Statistical Package for Social Sciences software (SPSS Inc. Chicago, Illinois, USA) was utilized for all statistical analyses.
Results
Of the 206 recruited participants, two twin pregnancies were excluded. Thirty-eight women’s data was excluded due to technical problems of metal measurement and loss to follow-up. Thus, 166 participants’ data was included in the statistical analysis (25 abortions and 141 ongoing pregnancies). Pregnant women’s characteristics and blood metal levels showed in the Table 1.
Table 1.
Prenatal metal levels and women characteristics in all participants (n = 166)
| Continues variable | mean ± SD | Range |
| Blood concentration of (μg/L) | ||
| Lead | 49.6 ± 66.77 | 5.17–709.82 |
| Cadmium | 0.51 ± 0.52 | 0–3.76 |
| Antimony | 2.79 ± 1.60 | 0.50–11.38 |
| Nickel | 96.57 ± 220.65 | 1.27–2418.48 |
| Age (y) | 31.9 ± 6.0 | 19–47 |
| Weight (kg) | 66.3 ± 13.3 | 44–170 |
| Height (cm) | 161.2 ± 11.3 | 120–179 |
| Body mass index (kg/m2) | 26.2 ± 5.2 | 17.2–62.1 |
| Red blood cell count (Million) | 4.26 ± 0.42 | 2.96–5.24 |
| Categorical variables | Frequency | % |
| Primipara | 85 | 51 |
| Previous abortion | 38 | 23 |
We compared participants’ characteristics and the blood metal levels between SA women and ongoing pregnancy groups. Except for cadmium, all metal levels were higher in SA than ongoing pregnancy (10.5 μg/L for lead, 0.22 μg/L for antimony, and 40.1 μg/L for nickel), although, these concentration differences were not statistically significant (Table 2). Women with SA were significantly older than control group (36.1 ± 6.4 vs 31.5 ± 5.8 years, p < 0.05). Maternal anthropometrics characteristics (weight, height, and BMI) were not significantly different between SA and ongoing pregnancy groups (not shown data). Primipara was more frequent in ongoing pregnancies than SA (56% vs 29%, respectively, p < 0.05) (Table 2).
Table 2.
Compression continues and categorical variables between spontaneous abortion and ongoing pregnancy groups
|
Spontaneous abortion n = 25 |
Ongoing pregnancy n = 141 |
p value | |
| Continues variable a | (mean ± SD) | (mean ± SD) | |
| Blood concentration of (μg/L) | |||
| Lead | 55.43 ± 54.3 | 44.97 ± 45.6 | 0.307 |
| Cadmium | 0.51 ± 0.5 | 0.51 ± 0.5 | 0.957 |
| Antimony | 2.89 ± 1.4 | 2.67 ± 1.6 | 0.529 |
| Nickel | 131.45 ± 156.8 | 91.32 ± 241.2 | 0.485 |
| Age (y) | 36.1 ± 6.4 | 31.5 ± 5.8 | 0.001 |
| Weight (kg) | 69.4 ± 10.3 | 66.1 ± 14.3 | 0.321 |
| Height (cm) | 160.1 ± 11.3 | 161.3 ± 5.7 | 0.466 |
| Body mass index (kg/m2) | 27.7 ± 5.9 | 26.1 ± 5.3 | 0.241 |
| Red blood cell count (Million) | 4.31 ± 0.35 | 4.25 ± 0.42 | 0.594 |
| Categorical variables b | Frequency (%) | frequency (%) | |
| Primipara | 7 (29) | 79 (56) | 0.047 |
| Previous abortion | 8 (33) | 29 (21) | 0.180 |
NS none significant
aStudent t-test
bChi-square test
Pearson’s correlation coefficient showed significant positive correlations among prenatal blood metals levels, except for nickel (Table 3). There was not a significant correlation between gestational age at the time of delivery with metal levels, in all subjects or separately for cases and controls (not shown data).
Table 3.
Pearson’s correlation coefficient (r) among blood metal concentrations
| Lead | Cadmium | Antimony | Nickel | ||
|---|---|---|---|---|---|
| Lead | r | 1 | |||
| p value | |||||
| Cadmium | r | .249 | 1 | ||
| p value | < 0.01 | ||||
| Antimony | r | .316 | .405 | 1 | |
| p value | < 0.01 | < 0.01 | |||
| Nickel | r | .027 | .034 | .114 | 1 |
| p value | .743 | .683 | .165 | ||
Multiple logistic regression models, when adjusted for confounders and blood metals, showed a significant association between maternal age and the risk of SA in all models (Table 4). Among toxic metals only antimony had a noticeable positive association with increased risk of SA, when adjusted for confounders (OR: 1.65, 95% CI: 1.08–2.52, p value: 0.020).
Table 4.
Possible risk factors for spontaneous abortion: results of logistic regression analysis
| Selected variable | Odds ratio | 95% Confidence interval | p value | |
|---|---|---|---|---|
| Model 1a | Age | 1.194 | 1.052–1.354 | 0.006 |
| Model 1 + lead | Age | 1.212 | 1.059–1.389 | 0.005 |
| Pb | 1.008 | 0.998–1.019 | 0.130 | |
| Model 1 + cadmium | Age | 1.217 | 1.061–1.396 | 0.005 |
| Cd | 1.690 | 0.595–4.797 | 0.325 | |
| Model 1 + antimony | Age | 1.254 | 1.078–1.459 | 0.003 |
| Sb | 1.652 | 1.081–2.525 | 0.020 | |
| Model 1 + nickel | Age | 1.166 | 1.003–1.354 | 0.045 |
| Ni | 1.005 | 1.000–1.011 | 0.044 |
aVariables were selected by forward stepwise method: spontaneous abortion (=1) and non-abortion (= 0) as dependent variable; maternal age, primipara, and previous abortion as independent variables
Although, there is an air pollution variation and industrial activities throughout the city, the present study failed to find a significant difference in the risk of SA, maternal blood metals levels, and other characteristics in the study’s participants among the city regions (not shown data).
Discussion
The rate of SA (15%) in the present TEND cohort study was close to Nybo Andersen et al. (2000) study in Denmark [13]. The results of univariate analysis revealed higher concentrations of measured toxic metals (lead, antimony, and nickel) in women with SA than ongoing pregnancies (not at the statistically significant level). The multiple variable analysis models showed higher maternal age, in all model, correlated with SA risk. This analysis showed that only antimony had a noticeable correlation with increase the risk of SA.
Consistent with the present study, our previous study results showed no significant statistically relationship between blood lead level and the risk of SA at relatively low levels (<5 μg/dL) [28]. Similarly, two other studies have failed to demonstrate significant difference between prenatal blood lead concentrations [29] or lead level in fetal tissue content [30] in aborting pregnancies and non-aborting pregnancies. Although there are several studies reported inducing risk of SA by increasing prenatal blood lead exposure [3, 18, 31–33], almost all of these studies showed higher concentrations of blood lead than the current study. Thus, as we expected, relationship between lead and the risk of abortion might be dose dependent and detectable at higher level of exposure.
The present study did not find a significant relationship between cadmium and the risk of SA. Similarly, a study observed no evidence of relationship between cadmium exposure and pregnancy loss [19]. On the other hand, cadmium is known as an important toxic metal for human reproductive system that may induce the risk of miscarriage at the average concentration of 2.73 μg/L [3]. However, this level is several times higher than obtained in the present study. Therefore, cadmium, like lead, might induce adverse pregnancy outcomes at relatively higher concentrations.
Although, prenatal blood nickel was higher in SA group than non-SA, the correlation was not at significant level and was not confirmed in multivariate analysis in the present study. Similarly, Rzymski, et al. (2018) study filed to demonstrate a significant correlation between nickel exposure and miscarriage risk [3]. However, another study on pregnant women who was occupationally exposure to nickel at early stage of pregnancy has reported increased the risk of SA [34]. On the other word, the findings of present study and the previous ones do not exclude the possibility of the risk of nickel for adverse pregnancy outcomes, especially at the relatively higher dose.
Among other measured metals just antimony had a noticeable correlation with the risk of SA in the logistic regression analyses. A study has reported increasing risk of abortion by using antimony compound (sodium antimony gluconate for Kala azar treatment) during early to mid-pregnancy [26]. In addition, Wang et al. study (2020) has reported two-times higher serum antimony in women who had SA than non-pregnant and non-SA women [21]. As there is not many reports in the literature about this toxic metal and pregnancy loss, the effect of antimony on abortion and it’s probably mechanism should be investigated more in future studies.
In short, the pathophysiology and molecular mechanisms of the effect of prenatal metal exposure on SA risk has not been clearly understood. The effects may be direct on the specific reproductive target organs. For example, nickel, cobalt, and cadmium may cause reduction in the trophoblast area and disturb aggregation of mononuclear trophoblastic cells to multinucleated cells [35]. In addition, toxic metals can indirectly induce pregnancy adverse effects through mechanisms such as disruption of reproductive hormones pathways [36]. We know that the balance of these hormones is important for abiding pregnancy, from the implantation of the blastocyst to the onset of parturition. Animal studies have shown that different concentrations of metals can disrupt signals within and between the hypothalamus and pituitary gland and can induce hypothalamic pituitary axis imbalances [37, 38] Several previous studies have reported estrogen and progesterone secretion rate influenced by metal exposure [38, 39]. Similarly, toxic metals might also facilitate SA by other mechanisms, such as producing reactive oxygen species in relatively higher blood concentrations to damage target organs [40, 41].
The univariate analysis showed that women in SA group were on average 6 years older than pregnancy group. Although, it may simply relate to repeated abortions in SA group, some of previous studies have reported increasing risk of miscarriage with increased maternal age, especially after age of 30–35 year [23, 42, 43]. Similarly, a case-control study reported maternal age as an important factor contributing to abortion [35]. Thus, higher maternal age may be an independent risk factor for the occurrence SA. In addition, primipara women had lower frequency of SA. This difference may be induced by higher previous abortion (i.e., recurrent abortion) in SA group than in ongoing pregnancy group (33% vs 21%, respectively).
Although, we did not investigate the source of toxic metals exposure in this study, exposure by air pollutants, contaminated foods and using contaminated skin care products could be the probable source of their exposure, as none of the participants had known occupationally exposure to metals. Our study results revealed a positive significant correlation between prenatal blood metal levels, except for nickel. This may be due to common source of exposure to toxic metal in the present study participants. Many of these metals are used as a complex (alloy) in the related industries. On the other hand, these metals may have synergistic effect in absorption and/or distribution in organs [34, 44].
To promote a better understanding of heavy metals effects on SA risk, although the current survey collected prenatal blood samples as early as possible (gestational age 10 to 16 weeks), our survey failed to include earlier abortions. As, the probability of SA decreases sharply after the 10th week of gestation, the findings should be considered for the relation between exposure to heavy metals and relatively late abortion. Finally, the current study results were limited by lack of comprehensive information on some potential confounders, such as reproductive hormonal imbalance, and genetic factors.
Conclusion
The present study’s participants were apparently healthy pregnant woman. We found non-significant higher concentrations of heavy metals (lead, antimony, and nickel) in whole blood sample sat the early pregnancy in SA group than non-abortion women. Although the present study filed to find evidences to prove the effects of toxic metals on the occurrence of SA at the relatively low-level blood toxic metals, these metals should be avoided in women who plan pregnancy and/or during the early stages of gestation to decrease the probable risk of pregnancy adverse effects due to the effects might be at subclinical levels and difficult to detect.
Acknowledgments
This research project was financially supported by Institute for Environmental Research, Tehran University of Medical Sciences, Iran by (Grant No. 25759-46-02-94), and Iran National Sciences Foundation (INFS) by (Grant No.93050433) and a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant No. 15H05288). The authors acknowledge all participants and administrations of hospitals and health care centers for their cooperation.
Funding
This research project was financially supported by Institute for Environmental Research, Tehran University of Medical Sciences, Iran by (Grant No. 25759-46-02-94), and Iran National Sciences Foundation (INFS) by (Grant No.93050433) and a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (Grant No. 15H05288).
Compliance with ethical standards
Conflict of interest
The authors declare that there are no conflicts of interest in this study.
Ethical approval
The TUMS Ethical Committees reviewed and approved the study design, procedures, and informed consent format (permission No:IR.TUMS.REC.1394.1180).
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohsen Vigeh, Email: vigeh@sina.tums.ac.ir.
Masud Yunesian, Email: yunesian@tums.ac.ir.
References
- 1.Amadi CN, Igweze ZN, Orisakwe OE. Heavy metals in miscarriages and stillbirths in developing nations. Middle East Fertil Soc J. 2017;22(2):91–100. [Google Scholar]
- 2.Wang Z, Yu X, Geng M, Wang Z, Wang Q, Zeng X. Accumulation of heavy metal in scalp hair of people exposed in Beijing sewage discharge channel sewage irrigation area in Tianjin, China. Environ Sci Pollut Res Int. 2017;24(15):13741–13748. doi: 10.1007/s11356-017-8884-x. [DOI] [PubMed] [Google Scholar]
- 3.Omeljaniuk WJ, et al. Cadmium and Lead in women who miscarried. Clin Lab. 2018;64(1):59–67. doi: 10.7754/Clin.Lab.2017.170611. [DOI] [PubMed] [Google Scholar]
- 4.Johnson MA. High calcium intake blunts pregnancy-induced increases in maternal blood lead. Nutr Rev. 2001;59(5):152–156. doi: 10.1111/j.1753-4887.2001.tb07004.x. [DOI] [PubMed] [Google Scholar]
- 5.Rothenberg SJ, Kondrashov V, Manalo M, Manton WI, Khan F, Todd AC, Johnson C. Seasonal variation in bone lead contribution to blood lead during pregnancy. Environ Res. 2001;85(3):191–194. doi: 10.1006/enrs.2000.4238. [DOI] [PubMed] [Google Scholar]
- 6.Nishioka E, Yokoyama K, Matsukawa T, Vigeh M, Hirayama S, Ueno T, Miida T, Makino S, Takeda S. Evidence that birth weight is decreased by maternal lead levels below 5mug/dl in male newborns. Reprod Toxicol. 2014;47:21–26. doi: 10.1016/j.reprotox.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Vigeh M, Yokoyama K, Shinohara A, Afshinrokh M, Yunesian M. Early pregnancy blood lead levels and the risk of premature rupture of the membranes. Reprod Toxicol. 2010;30(3):477–480. doi: 10.1016/j.reprotox.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Vigeh M, Yokoyama K, Seyedaghamiri Z, Shinohara A, Matsukawa T, Chiba M, Yunesian M. Blood lead at currently acceptable levels may cause preterm labour. Occup Environ Med. 2011;68(3):231–234. doi: 10.1136/oem.2009.050419. [DOI] [PubMed] [Google Scholar]
- 9.Lead poisoning in pregnant women who used Ayurvedic medications from India--New York City, 2011-2012. MMWR Morb Mortal Wkly Rep. 2012;61(33):641–6. [PubMed]
- 10.Hafez AS, Fahim HI, Badawy HA. Socioenvironmental predictors of abortion and stillbirths in an industrial community in Egypt. J Egypt Public Health Assoc. 2001;76(1–2):1–16. [PubMed] [Google Scholar]
- 11.Ikeh-Tawari EP, Anetor JI, Charles-Davies MA. Cadmium level in pregnancy, influence on neonatal birth weight and possible amelioration by some essential trace elements. Toxicol Int. 2013;20(1):108–112. doi: 10.4103/0971-6580.111558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henríquez-Hernández LA, Luzardo OP, Boada LD, González-Antuña A, Domínguez-Bencomo AI, Zumbado M, Burillo-Putze G. Assessment of 22 inorganic elements in human amniotic fluid: a cross-sectional study conducted in Canary Islands (Spain) Int J Environ Health Res. 2019;29(2):130–139. doi: 10.1080/09603123.2018.1516284. [DOI] [PubMed] [Google Scholar]
- 13.Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ. 2000;320(7251):1708–1712. doi: 10.1136/bmj.320.7251.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weselak M, Arbuckle TE, Walker MC, Krewski D. The influence of the environment and other exogenous agents on spontaneous abortion risk. J Toxicol Environ Health B Crit Rev. 2008;11(3–4):221–241. doi: 10.1080/10937400701873530. [DOI] [PubMed] [Google Scholar]
- 15.Taskinen HK. Effects of parental occupational exposures on spontaneous abortion and congenital malformation. Scand J Work Environ Health. 1990;16(5):297–314. doi: 10.5271/sjweh.1779. [DOI] [PubMed] [Google Scholar]
- 16.Mohammadyan M, Moosazadeh M, Borji A, Khanjani N, Rahimi Moghadam S. Investigation of occupational exposure to lead and its relation with blood lead levels in electrical solderers. Environ Monit Assess. 2019;191(3):126. doi: 10.1007/s10661-019-7258-x. [DOI] [PubMed] [Google Scholar]
- 17.Anttila A, Sallmen M. Effects of parental occupational exposure to lead and other metals on spontaneous abortion. J Occup Environ Med. 1995;37(8):915–921. doi: 10.1097/00043764-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Hertz-Picciotto I. The evidence that lead increases the risk for spontaneous abortion. Am J Ind Med. 2000;38(3):300–309. doi: 10.1002/1097-0274(200009)38:3<300::aid-ajim9>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 19.Buck Louis GM, Smarr MM, Sundaram R, Steuerwald AJ, Sapra KJ, Lu Z, Parsons PJ. Low-level environmental metals and metalloids and incident pregnancy loss. Reprod Toxicol. 2017;69:68–74. doi: 10.1016/j.reprotox.2017.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McDermott S, Salzberg DC, Anderson AP, Shaw T, Lead J. Systematic review of chromium and nickel exposure during pregnancy and impact on child outcomes. J Toxicol Environ Health Part A. 2015;78(21–22):1348–1368. doi: 10.1080/15287394.2015.1090939. [DOI] [PubMed] [Google Scholar]
- 21.Wang R, Zhang L, Chen Y, Zhang S, Zhuang T, Wang L, Xu M, Zhang N, Liu S. Elevated non-essential metals and the disordered metabolism of essential metals are associated to abnormal pregnancy with spontaneous abortion. Environ Int. 2020;144:106061. doi: 10.1016/j.envint.2020.106061. [DOI] [PubMed] [Google Scholar]
- 22.Rzymski P, Niedzielski P, Poniedziałek B, Tomczyk K, Rzymski P. Identification of toxic metals in human embryonic tissues. Arch Med Sci. 2018;14(2):415–421. doi: 10.5114/aoms.2015.53915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeng LX, Yan H, Chen ZJ. Study on the current status and risk factors of spontaneous abortion of women at reproductive age in rural areas of Xianyang district, Shaanxi province. Zhonghua Liu Xing Bing Xue Za Zhi. 2007;28(1):19–23. [PubMed] [Google Scholar]
- 24.Vigeh M, Yokoyama K, Ramezanzadeh F, Dahaghin M, Sakai T, Morita Y, Kitamura F, Sato H, Kobayashi Y. Lead and other trace metals in preeclampsia: a case-control study in Tehran, Iran. Environ Res. 2006;100(2):268–275. doi: 10.1016/j.envres.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Zhang G, Wang X, Zhang X, Li Q, Xu S, Huang L, Zhang Y, Lin L, Gao D, Wu M, Sun G, Song Y, Zhong C, Yang X, Hao L, Yang H, Yang L, Yang N. Antimony in urine during early pregnancy correlates with increased risk of gestational diabetes mellitus: a prospective cohort study. Environ Int. 2019;123:164–170. doi: 10.1016/j.envint.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 26.Miah MT, Ayaz FM, Maniruzzaman M, Ahasan MN, Bari S, Mawla SM, Mahbub MS, Khan AI. Kala azar in Pregnancy. Mymensingh Med J. 2010;19(4):529–532. [PubMed] [Google Scholar]
- 27.Amini H, Schindler C, Hosseini V, Yunesian M, Künzli N. Land use regression models for Alkylbenzenes in a middle eastern megacity: Tehran study of exposure prediction for environmental Health Research (Tehran SEPEHR) Environ Sci Technol. 2017;51(15):8481–8490. doi: 10.1021/acs.est.7b02238. [DOI] [PubMed] [Google Scholar]
- 28.Vigeh M, Yokoyama K, Kitamura F, Afshinrokh M, Beygi A, Niroomanesh S. Early pregnancy blood lead and spontaneous abortion. Women Health. 2010;50(8):756–766. doi: 10.1080/03630242.2010.532760. [DOI] [PubMed] [Google Scholar]
- 29.Faikoglu R, et al. Significance of maternal plasma lead level in early pregnancy loss. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2006;41(3):501–506. doi: 10.1080/10934520500428435. [DOI] [PubMed] [Google Scholar]
- 30.Borella P, Picco P, Masellis G. Lead content in abortion material from urban women in early pregnancy. Int Arch Occup Environ Health. 1986;57(2):93–99. doi: 10.1007/BF00381376. [DOI] [PubMed] [Google Scholar]
- 31.Tabacova S, Balabaeva L. Environmental pollutants in relation to complications of pregnancy. Environ Health Perspect. 1993;101(Suppl 2):27–31. doi: 10.1289/ehp.93101s227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellinger DC. Teratogen update: lead and pregnancy. Birth Defects Res A Clin Mol Teratol. 2005;73(6):409–420. doi: 10.1002/bdra.20127. [DOI] [PubMed] [Google Scholar]
- 33.Borja-Aburto VH, Hertz-Picciotto I, Lopez MR, Farias P, Rios C, Blanco J. Blood lead levels measured prospectively and risk of spontaneous abortion. Am J Epidemiol. 1999;150(6):590–597. doi: 10.1093/oxfordjournals.aje.a010057. [DOI] [PubMed] [Google Scholar]
- 34.Kim SH, Chun J, Ko KH, Sung TJ. Effect of antenatal azithromycin for Ureaplasma spp. on neonatal outcome at </=30 weeks' gestational age. Pediatr Int. 2019;61(1):58–62. doi: 10.1111/ped.13738. [DOI] [PubMed] [Google Scholar]
- 35.Zhao R, Wu Y, Zhao F, Lv Y, Huang D, Wei J, Ruan C, Huang M, Deng J, Huang D, Qiu X. The risk of missed abortion associated with the levels of tobacco, heavy metals and phthalate in hair of pregnant woman: a case control study in Chinese women. Medicine (Baltimore) 2017;96(51):e9388. doi: 10.1097/MD.0000000000009388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen C, Wang N, Zhai H, Nie X, Sun H, Han B, Li Q, Chen Y, Cheng J, Xia F, Zhao L, Zheng Y, Shen Z, Lu Y. Associations of blood lead levels with reproductive hormone levels in men and postmenopausal women: results from the SPECT-China study. Sci Rep. 2016;6:37809. doi: 10.1038/srep37809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sokol RZ, Wang S, Wan YJY, Stanczyk FZ, Gentzschein E, Chapin RE. Long-term, low-dose lead exposure alters the gonadotropin-releasing hormone system in the male rat. Environ Health Perspect. 2002;110(9):871–874. doi: 10.1289/ehp.02110871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee TW, Kim DH, Ryu JY. The effects of exposure to lead, cadmium and mercury on follicle-stimulating hormone levels in men and postmenopausal women: data from the second Korean National Environmental Health Survey (2012-2014) Ann Occup Environ Med. 2019;31:e21. doi: 10.35371/aoem.2019.31.e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gallagher CM, Moonga BS, Kovach JS. Cadmium, follicle-stimulating hormone, and effects on bone in women age 42-60 years, NHANES III. Environ Res. 2010;110(1):105–111. doi: 10.1016/j.envres.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 40.Wakeel A, Xu M, Gan Y. Chromium-induced reactive oxygen species accumulation by altering the enzymatic antioxidant system and associated cytotoxic, genotoxic, ultrastructural, and photosynthetic changes in plants. Int J Mol Sci. 2020;21(3):728. doi: 10.3390/ijms21030728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaziri ND, Khan M. Interplay of reactive oxygen species and nitric oxide in the pathogenesis of experimental lead-induced hypertension. Clin Exp Pharmacol Physiol. 2007;34(9):920–925. doi: 10.1111/j.1440-1681.2007.04644.x. [DOI] [PubMed] [Google Scholar]
- 42.Magnus MC, et al. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019;364:l869. doi: 10.1136/bmj.l869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.de la Rochebrochard E, Thonneau P. Paternal age and maternal age are risk factors for miscarriage; results of a multicentre European study. Hum Reprod. 2002;17(6):1649–1656. doi: 10.1093/humrep/17.6.1649. [DOI] [PubMed] [Google Scholar]
- 44.Rakhra G, Masih D, Vats A, Vijay A, Ashraf MZ, Singh SN. Study of metal-metal interactions and their biomarkers using an intestinal human cell line. Biol Trace Elem Res. 2020;195(1):95–104. [DOI] [PubMed]