Abstract
Aims
We investigated the impact of actual waiting time and perceived waiting time on treatment satisfaction in patients with diabetes receiving outpatient care.
Methods
Three hundred and thirty-six outpatients diagnosed with diabetes mellitus or impaired glucose tolerance were selected and the time they spent in reception, blood collection, consultation, and accounting were recorded to measure the time they spent waiting in the hospital (actual waiting time). Simultaneously, we conducted a questionnaire survey that included questions on their perceptions of the waiting time (perceived waiting time) and satisfaction with treatment (DTSQ).
Results
No significant relationship was found between actual waiting time and DTSQ score, although associations were observed with perceived waiting time. The patients who felt the overall waiting time was long scored 23.0, those who felt it was short scored 26.0, and those who felt it was very short scored 34.0, with those who felt the waiting time was long having a significantly lower score (p = 0.004, p < 0.001, respectively) and those who felt it was short having a significantly lower score than those who felt it was very short (p = 0.008). In addition, more patients who felt the waiting time was long expressed dissatisfaction with the responses of doctors and staff than those who felt the waiting time was short.
Conclusions
These results suggest that in addition to reducing actual waiting times, shortening perceived waiting times by improving the responses of medical staff could help to increase patient satisfaction.
Keywords: Actual waiting time, Perceived waiting time, Satisfaction, Drop out, Diabetes
Introduction
The Japan Diabetes Outcome Intervention Trial-2 found that 8.25% of patients with diabetes discontinued treatment every year if no special intervention was provided [1]. It has been estimated that those who have a history of discontinuing treatment have poorer glycemic control than those with no such history [2] and are also at a higher risk of complications [3].
The study by Saisho et al. found a relationship between decreased patient satisfaction and discontinuation of treatment [4]. The diabetes treatment satisfaction questionnaire (DTSQ) was developed as a method for quantifying treatment satisfaction specific to diabetes mellitus [5], and has been used in Japan and around the world [6–8]. According to Saisho et al., the DTSQ score can be a significant predictor of intention to discontinue treatment, and those patients associated with lower DTSQ scores are at higher risk of discontinuation. In addition, the DTSQ score had a significant negative correlation with waiting time; patients who said they waited a long time for outpatient care had lower DTSQ scores. In other countries, long waiting times have been cited as a reason for lower patient satisfaction and treatment discontinuation [9–12]. Research from the United States (US) has shown that long waiting times reduce patient satisfaction and their willingness to continue hospital visits [9]. For the above reasons, the Japanese Ministry of Health, Labor and Welfare’s “Comprehensive guide to preventing the discontinuation of diabetes mellitus care” recommends creating a medical system with short waiting times [2].
However, the length of waiting times is not limited to the problem of the actual time spent waiting. Some research has argued for the need to pay attention to how the waiting time feels (perceived waiting time) along with the actual waiting time [13–20].
A study from the US reports that measures such as informing patients in advance about how long they were expected to spend at the clinic made it less likely for the patients to feel that waiting times were longer than they actually were (reduced perceived waiting time) and may have reduced the stress caused by waiting [13]. This shows that the same waiting time can be perceived in various ways and that the actual time may not match the perceived time.
Increasing patient treatment satisfaction is an effective means of reducing the discontinuation of diabetes therapy. Reducing waiting times is considered a necessary part of improving patient treatment satisfaction. There are two types of waiting time—actual waiting time and perceived waiting time—but there have been no reports on which one has a greater effect on patients' satisfaction with treatment.
In the present study, we examined how treatment satisfaction in patients with diabetes receiving outpatient care relates to waiting time from two aspects, namely actual and perceived. We also examined the factors related to perceived waiting time, with a focus on the responses of doctors and medical staff.
Materials and methods
Study population
A questionnaire was sent to 888 outpatients with diabetes or impaired glucose tolerance who visited our clinic in April 2016. We also measured time spent in clinics. Totally, 759 patients responded to the questionnaire. The subjects of the analysis were 336 patients whose actual waiting times were measured.
Questionnaire survey
We conducted a questionnaire survey about their experience in the previous visit to the clinic. The questionnaire was given to the patients by nurses or medical administrative staff, and was filled out by either the patients themselves or with assistance from staff, while waiting for outpatient consultations. The questionnaire had questions related to sex, age, frequency of visits, recent HbA1c levels, site of previous visits, feelings about waiting time (perceived waiting time), feelings about the responses of doctors and medical staff, DTSQ, history of treatment discontinuation, and intention to discontinue treatment. The DTSQ score was the sum of the responses to 6 questions that constituted primary factors indicating treatment satisfaction (Q 1, 4, 5, 6, 7, 8; minimum 0, maximum 36 points).
Actual waiting time
During the same period that the questionnaire survey was conducted, 1 out of every 2–4 appointments was selected to record the time the patients passed through reception, blood collection, consultation, and accounting to calculate actual waiting times (from reception to blood collection, blood collection to consultation, consultation to accounting, and overall from reception to accounting). The patients who were selected were those with appointments at the beginning of a 15-min appointment block.
Statistical analysis
The actual waiting times were divided into tertiles to create three groups—short waiting time, moderate waiting time, and long waiting time. Multiple comparisons were performed using the Kruskal–Wallis test to compare the actual measurements to the DTSQ primary factor scores for each group. The chi-square test was used to examine the relationship between perceived waiting time and the responses of doctors and staff. In addition, receiver operating characteristic (ROC) analysis was used to determine cutoff values for predicting perceived waiting time from actual waiting time and treatment discontinuation from the DTSQ score. All statistical tests were two sided and p values < 0.05 were considered statistically significant. Analyses were performed with IBM SPSS Statistics Base 24 (IBM Japan, Ltd.).
Ethical approval
We obtained the approval of the institutional ethics review board of TDE Healthcare Corporation TOSAKI Clinic for Diabetes and Endocrinology (approval no. 820303, approval date; March 27, 2016). Patients were notified in writing that responding to the questionnaire meant agreeing to participate in the study.
Results
Patient background
Of the 336 subjects, 214 were men (63.7%) and 122 were women (36.3%) (Table 1). The number of patients and their respective ages were 84 in their 50s (25.0%) and 92 in their 60s (27.4%).
Table 1.
Baseline characteristics
| Total n = 336 | |||
|---|---|---|---|
| Sex | Male | 214 | (63.7) |
| Female | 122 | (36.3) | |
| Age class | ≥ 10 and < 20 | 2 | (0.6) |
| ≥ 20 and < 30 | 7 | (2.1) | |
| ≥ 30 and < 40 | 31 | (9.2) | |
| ≥ 40 and < 50 | 56 | (16.7) | |
| ≥ 50 and < 60 | 84 | (25.0) | |
| ≥ 60 and < 70 | 92 | (27.4) | |
| ≥ 70 and < 80 | 51 | (15.2) | |
| ≥ 80 and < 90 | 11 | (3.3) | |
| ≥ 90 | 2 | (0.6) | |
| Hospital visit frequency | Every 2 weeks | 46 | (13.8) |
| Every month | 280 | (83.8) | |
| Every 2 months | 8 | (2.4) | |
| HbA1c | < 6.9% (< 51 mmol/mol) | 150 | (45.6) |
| ≥ 6.9 and ≤ 7.4% (≥ 51 and ≤ 57 mmol/mol) | 111 | (33.7) | |
| ≥ 7.5 and ≤ 8.4% (≥ 58 and ≤ 72 mmol/mol) | 42 | (12.8) | |
| ≥ 8.5% (≥ 73 mmol/mol) | 14 | (4.3) | |
| Missing data | 12 | (3.6) | |
| Previous site of care | Hospital | 98 | (30.2) |
| Clinic | 114 | (35.2) | |
| This hospital is first | 112 | (34.6) | |
n(%)
Actual waiting times in the three groups and DTSQ scores
The time measurements (reception to blood collection, blood collection to consultation, consultation to accounting, overall) were divided into tertiles to create three groups—a short-waiting time group, a moderate-waiting time group, and a long-waiting time group (Table 2).
Table 2.
Three actual waiting time groups and diabetes treatment satisfaction questionnaire primary factor scores
| Total | Short group | Moderate group | Long group | p value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Reception to blood collection | No. of patients | 334 | (100.0) | 116 | (34.6) | 113 | (33.7) | 106 | (31.6) | |
| Time measurement (min) | 10.0 | (6.0, 14.0) | 5.0 | (4.0, 7.0)b, c | 10.0 | (8.0, 11.0)a, c | 15.5 | (14.0, 21.0)a, b | < 0.001 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 26.5 | (21.0, 30.0) | 25.0 | (19.5, 30.5) | 25.0 | (21.0, 30.3) | 0.667 | |
| Blood collection to consultation | No. of patients | 334 | (100.0) | 124 | (37.1) | 112 | (33.5) | 98 | (29.3) | |
| Time measurement (min) | 12.0 | (9.0, 19.0) | 7.5 | (6.0, 9.0) b, c | 13.0 | (12.0, 15.0) a, c | 24.0 | (19.0, 32.0) a, b | < 0.001 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 27.0 | (21.0, 32.0) | 24.5 | (19.3, 30.0) | 25.5 | (21.0, 30.0) | 0.285 | |
| Consultation to accounting | No. of patients | 335 | (100.0) | 145 | (43.3) | 109 | (32.5) | 81 | (24.2) | |
| Time measurement (min) | 5.0 | (3.0, 7.0) | 3.0 | (2.0, 4.0) b, c | 6.0 | (5.0, 7.0) a, c | 11.0 | (9.0, 13.5) a, b | < 0.001 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 25.0 | (21.0, 32.0) | 26.0 | (21.0, 30.0) | 26.0 | (19.5, 30.0) | 0.470 | |
| Overall (reception to accounting) | No. of patients | 336 | (100.0) | 117 | (34.8) | 114 | (33.9) | 105 | (31.3) | |
| Time measurement (min) | 44.0 | (35.0, 56.0) | 32.0 | (27.0, 36.0) b, c | 44.5 | (42.0, 48.0) a, c | 66.0 | (57.0, 77.0) a, b | < 0.001 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 27.0 | (21.0, 32.0) | 24.0 | (20.0, 29.3) | 26.0 | (20.0, 31.0) | 0.133 | |
No. of patients: n(%), Time measurement / DTSQ primary factors: median (25th percentile, 75th percentile), p value: intergroup comparison (Kruskal–Wallis test)
ap < 0.001, vs. short group, bp < 0.001, vs. moderate group, cp < 0.001, vs. long group (Bonferroni method)
The time measurements from reception to blood collection, blood collection to consultation, consultation to accounting, and overall (reception to accounting) were divided into tertiles to create three groups—a short waiting time, moderate waiting time, and long waiting time group
On comparing the DTSQ scores, there were no significant differences between the three groups in any of the actual waiting times (reception to blood collection, blood collection to consultation, consultation to accounting, overall).
Four perceived waiting time groups and actual waiting time
Table 3 compares perceived waiting times to the actual waiting times. The actual waiting time of those who answered the perceived waiting from reception to blood collection room time “long” was significantly longer than those who answered “very short” and “short” (p = 0.003, p = 0.026, respectively). No significant relationships were observed between perceived waiting time and actual waiting time from blood collection to consultation, consultation to accounting, or overall.
Table 3.
Actual times of the 4 perceived waiting time groups and diabetes treatment satisfaction questionnaire primary factor scores
| Total | Very short | Short | Long | Very long | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reception to blood collection | No. of patients | 327 | (100.0) | 27 | (8.3) | 245 | (74.9) | 54 | (16.5) | 1 | (0.3) | |
| Time measurement (min) | 10.0 | (6.0, 14.0) | 8.0 | (5.0, 10.0)c | 9.0 | (6.0, 14.0) c | 12.0 | (8.8, 15.0) a, b | 6.0 | (6.0, 6.0) | 0.002 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 30.0 | (23.0, 33.0)‡ | 26.0 | (20.3, 30.0) | 25.0 | (19.0, 29.3) * | 34.0 | (34.0, 34.0) | 0.030 | |
| Blood collection to consultation | No. of patients | 325 | (100.0) | 10 | (3.1) | 119 | (58.5) | 98 | (36.6) | 6 | (1.8) | |
| Time measurement (min) | 12.0 | (9.0, 19.0) | 10.5 | (7.8, 15.0) | 13.0 | (8.3, 19.0) | 25.5 | (9.0, 19.0) | 20.5 | (8.8, 42.8) | 0.293 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 33.0 | (23.5, 36.0)‡ | 23.0 | (22.0, 32.0)‡ | 24.0 | (18.3, 28.0)*, † | 21.5 | (16.0, 31.0) | < 0.001 | |
| Consultation to accounting | No. of patients | 324 | (100.0) | 21 | (6.5) | 252 | (77.8) | 50 | (15.4) | 1 | (0.3) | |
| Time measurement (min) | 5.0 | (3.0, 7.0) | 6.0 | (2.5, 7.5) | 5.0 | (3.0, 7.0) | 6.0 | (3.0, 7.0) | 11.0 | (11.0, 11.0) | 0.389 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 31.5 | (26.8, 35.3)†, ‡ | 26.0 | (21.0, 30.0)*, ‡ | 23.0 | (17.0, 26.0) *, † | 34.0 | (34.0, 34.0) | < 0.001 | |
| Overall | No. of patients | 310 | (100.0) | 12 | (3.9) | 203 | (60.4) | 91 | (27.1) | 4 | (1.3) | |
| Time measurement (min) | 44.0 | (35.0, 56.0) | 41.5 | (31.3, 62.0) | 43.0 | (34.0, 52.0) | 47.0 | (39.0, 64.0) | 44.0 | (34.8, 51.8) | 0.050 | |
| DTSQ primary factors (points) | 26.0 | (20.0, 30.0) | 34.0 | (30.0, 36.0) †, ‡ | 26.0 | (21.0, 31.0)*, ‡ | 23.0 | (18.0, 29.0) *, † | 21.5 | (14.0, 31.3) | < 0.001 | |
No. of patients: n (%), Time measurement / DTSQ primary factors: median (25%tile, 75%tile), p value: intergroup comparison (Kruskal–Wallis test)
ap < 0.05, vs very short; bp < 0.05, vs short; cp < 0.05, vs long (Bonferroni method)
*p < 0.05, vs very short; †p < 0.05, vs short; ‡p < 0.05, vs long (Bonferroni method)
An ROC analysis was used to examine predicting perceived waiting time from the overall actual waiting time (reception to accounting). The perceived waiting times were divided into two groups: those who said the overall waiting time was “very long” or “long” and those who said it was “very short” or “short”. The analysis showed that overall actual waiting time was a significant predictor of perceived waiting time (area under the curve 0.594, p = 0.009) with an optimum cutoff value of 57.5 (sensitivity 34.8%, specificity 83.7%). This suggests that an overall actual waiting time longer than 57.5 min is a factor in making patients perceive the overall waiting time as long. In this study, 78 of the 336 subjects (23.2%) had actual waiting times of at least 57.5 min (Fig. 1).
Fig. 1.
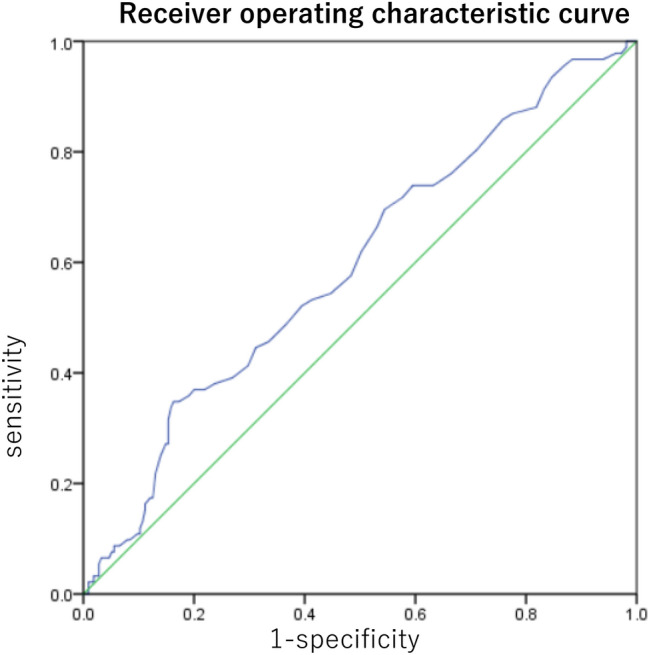
Results of receiver operating characteristic (ROC) analysis of actual waiting time to predict perceived waiting time. The area under the ROC curve was 0.594 (p = 0.009). The best cutoff value was 57.5 (34.8% sensitivity and 83.7% specificity).
Perceived waiting time and DTSQ score
We examined the relationship between perceived waiting time and DTSQ score (Table 3). The DTSQ scores of those who felt the waiting time was long from reception to blood collection, blood collection to consultation, consultation to accounting, or overall time were significantly lower than those who did not. The patients who felt the overall waiting time was long scored 23.0, those who felt it was short scored 26.0, and those who felt it was very short scored 34.0, with those who felt the waiting time was long having a significantly lower score (p = 0.004, p < 0.001, respectively) and those who felt it was short having a significantly lower score than those who felt it was very short (p = 0.008).
Perceived waiting time and the responses of doctors and staff
We examined the relationship between perceived waiting time and the responses of doctors and staff (Table 4). Perceived waiting times were divided into two groups: patients who answered “very long” or “long” in the long group, and those who answered “very short” or “short” in the short group. In addition, answers to 4 items related to the responses of doctors and medical staff—“Test results and treatment plans are explained in easy-to-understand language”, “Things like specific pointers for daily life are explained”, “My concerns and questions are addressed in an easy-to-understand manner”, and, “They are easy to talk to about anything”—were separated into a “yes” group and “no” group based on the median of the distribution of responses (5: almost always, 4, 3, 2, 1: never). The chi-square test was used to examine the two perceived waiting time groups and the two doctor and medical staff response groups. Significantly more people who answered “no” to all 4 doctor and staff response items felt the overall waiting time was long.
Table 4.
Two perceived waiting time groups and responses of doctors and staff
| Total | Short | Long | p value | |||||
|---|---|---|---|---|---|---|---|---|
| a. Easy-to-understand explanations |
Yes No |
136 168 |
(100.0) (100.0) |
109 105 |
(80.1) (62.5) |
27 63 |
(19.9) (37.5) |
0.001 |
| b. Specific pointers for daily life |
Yes No |
120 184 |
(100.0) (100.0) |
95 119 |
(79.2) (64.7) |
25 65 |
(20.8) (35.3) |
0.007 |
| c. Responds to doubts, questions in an easy-to-understand manner |
Yes No |
140 164 |
(100.0) (100.0) |
111 103 |
(79.3) (62.8) |
29 61 |
(20.7) (37.2) |
0.002 |
| d. Easy to talk to |
Yes No |
146 158 |
(100.0) (100.0) |
116 98 |
(79.5) (62.0) |
30 60 |
(20.5) (38.0) |
0.001 |
n(%), χ2 test
Responses to 4 items for “How do you feel about the responses of doctors and staff?” (“Test results and treatment plans are explained in easy-to-understand language”, “Things like specific pointers for daily life are explained”, “My concerns and questions are addressed in an easy-to-understand manner”, and “They are easy to talk to about anything”) were separated into a “Yes” group and “No” group based on the median of the distribution of responses (5: almost always, 4, 3, 2, 1: never)
Responses to “How do you feel about the waiting time (overall)?” were divided into 2 groups: patients who answered “very long” or “long” in the long group and those who answered “very short” or “short” in the short group
Presence or absence of intention to discontinue treatment and DTSQ score, actual waiting time, perceived waiting time
To the question, “I’ve thought about discontinuing treatment since I started coming to this hospital”, only 6.3% patients said “yes”.
We examined the relationship between DTSQ scores and intentions to discontinue treatment. The DTSQ score of those who expressed an intention to discontinue treatment was significantly lower than those who did not (p < 0.001). Receiver operating characteristic curve analysis revealed the DTSQ score as a significant predictor of the presence of intention to drop out (area under the curve = 0.808, p < 0.001), with an optimal cut-off of 22.5 (sensitivity 68.8%, specificity 80.0%). (Fig. 2).
Fig. 2.
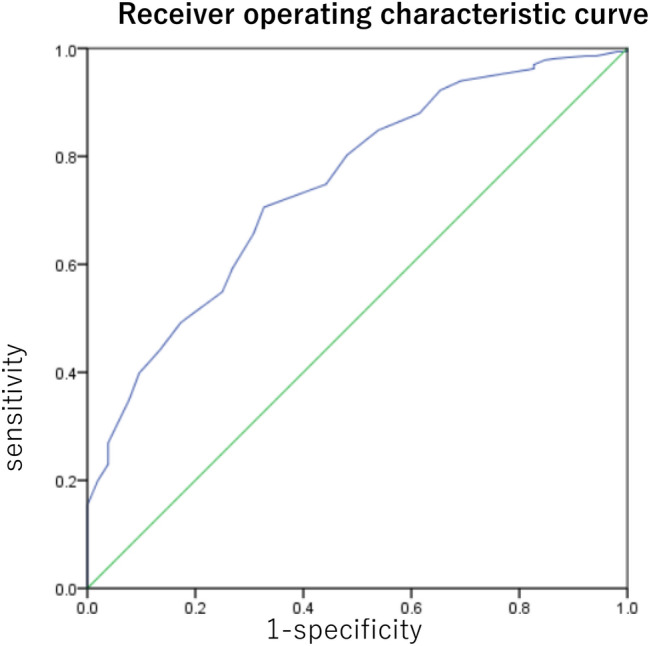
Results of receiver operating characteristic (ROC) analysis of satisfaction with treatment questionnaire (DTSQ) primary factor scores to predict intention to discontinue treatment. The area under the ROC curve was 0.808 (p < 0.001). The best cutoff value was 22.5 (68.8% sensitivity and 80.0% specificity).
With regards to treatment discontinuation intention and actual waiting time, the median actual waiting time of those who had an intention to discontinue treatment was 45.5 min; whereas, the median time of those with no intention was 44.0 min, which is not a significant difference (p = 0.597).
For perceived waiting time, about half of patients who expressed an intention to discontinue treatment felt the waiting time was long; whereas, among patients with no intention to discontinue treatment, less than 30% of these patients felt the waiting time was long (p = 0.066).
Discussion
In this study, we examined waiting time, which is considered a reason for treatment discontinuation and investigated how actual and perceived waiting times are related to patient treatment satisfaction. We also examined the factors related to perceived waiting time, with a focus on the responses of doctors and medical staff. The results showed no significant association between actual waiting time and the DTSQ score, but patients with long perceived waiting times showed significantly lower DTSQ scores. In addition, many of the patients who expressed dissatisfaction in all doctor and staff response items had long perceived waiting times. Perceived waiting time is related to treatment satisfaction, and thus, along with reducing actual waiting times, it is important to improve the responses of the medical staff so patients do not perceive the waiting to be are long. Our results suggest that this may reduce treatment discontinuation rates.
Shortening actual waiting times for outpatients has become a concern worldwide [21, 22]. An outpatient diabetes clinic in Singapore introduced an initiative to shorten the time patients spend at the clinic. Yet, this did not result in a significant change, with time spent in the clinic going from 108.2 to 106.6 min, showing that other improvements are needed [21]. At a clinic in the US, the Plan-Do-Study-Act cycle was used to reduce the time spent at the hospital, which, over a year, succeeded in reducing waiting time from 71 to 60 min and improved treatment satisfaction among patients [22].
A questionnaire survey on outpatient waiting time in Japan found that the mean acceptable time from reception to accounting was 68 min, although only 38% of patients (38/101) spent 68 min or less [23]. In the present study, the mean waiting time was 47.7 min, and 85.1% (286/336) of the patients spent 68 min or less.
One of the possible reasons for the absence of an association between actual waiting time and DTSQ score in the present study is that patient treatment satisfaction had been maintained by already shortening actual waiting times to some degree. The actual waiting time in the subjects of this study is shorter than that in the previous study, and even the actual waiting time of “long group” divided by the tertile is about 66 min, which was considered to be within the allowable range in the previous study. Since there was no major problem in the actual waiting time itself, it is possible that there was no relationship between actual waiting time and diabetes treatment satisfaction. In our study, the cutoff value for perceiving overall waiting time (reception to accounting) as short was 57 min or less, with about 3/4 of the patients falling within this range. When shortening actual waiting times, it is best to first aim to reduce waiting time to less than 57 min.
A significant relationship between perceived and actual waiting times was only observed for reception to blood collection, with no other periods showing significant associations. Many previous studies treated waiting time as the actual time measurement, and Japanese guidelines recommend medical institutions to shorten actual waiting times. However, the results of our study suggest that some patients will perceive waiting times to be long even if the actual time is reduced. When investigating patient waiting times, it is necessary to understand the perceptual aspects of how patients feel about waiting times, in addition to performing actual measurements.
In addition, while there was no association between actual waiting time and DTSQ score, all aspects of perceived waiting time were associated with the DTSQ score. As mentioned above, after shortening actual waiting times to under 57 min, it is considered important to try to reduce perceived waiting times (i.e., not making patients feel they are waiting for a long time). In the present study, patients who felt the overall waiting time was short had positive impressions of the responses of doctors and medical staff. A report by Saisho et al. found that DTSQ scores had strong positive correlations with the level of satisfaction with care provided by doctors and the overall level of outpatient care [4]. Along with shortening actual waiting times, improving the responses of doctors and staff may help shorten perceived waiting times, and eventually increase patients' satisfaction with treatment.
Previous research has shown that patients with high treatment satisfactions are at low risk of discontinuing treatment. In the present study, the cut-off DTSQ primary factor score for intention to discontinue treatment was 22.5 points, which is consistent with a report on 139 cases described by Saisho et al. [4]. It is notable that our study, with its large subject population of 336 patients, obtained similar results. The results of the present study support the possibility that treatment discontinuation could be reduced by increasing satisfaction with treatment.
This study had several limitations. First, patients underwent different examinations on the days in question. Patients who underwent examinations or received dietary guidance between blood collection and the consultation needed time to go through these procedures. As their waiting times may have been shorter if these were omitted, it is possible for this to have impacted their perceptions of waiting time. Second, because this study's data were from a cross-sectional survey, the causal relationship between waiting time and treatment satisfaction is unclear. Therefore, it cannot be denied that those who are originally satisfied with the treatment may feel that the waiting time is short. Moreover, the patients who said they intended to discontinue treatment may be different from those who actually discontinue treatment. That being said, patients who said they intended to discontinue treatment were more likely to have a history of discontinuing treatment. In the future, detailed examination by longitudinal survey will be required. Third, the actual waiting time is short as a whole in this study; so, there is a possibility that few subjects of this study considered the actual waiting time itself as a problem. However, it is interesting that there was a difference in diabetes treatment satisfaction depending on perceived waiting time.
Conclusion
Our results suggest that in addition to shortening actual waiting times, improving the responses of medical staff to shorten perceived waiting times could lead to higher patient satisfaction and fewer patients that discontinue treatment. Going forward, a prospective study with patients undergoing set examinations on the day should be conducted and it should be confirmed whether subjects actually discontinue treatment after the survey.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by ST-S and TT. The first draft of the manuscript was written by ST-S and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Compliance with ethical standards
Conflict of interest
Shiori Toga-Sato declares no conflicts of interest associated with this manuscript. Takahiro Tosaki received lecture fees from Eli Lilly, Astellas, AstraZeneca, Mitsubishi Tanabe, MSD and Takeda, and research funding from Mitsubishi Tanabe, Daiichi Sankyo and Takeda. Masaki Kondo received research funding from Johnson & Johnson, Daiichi Sankyo, Eli Lilly, Kyowa Hakko Kirin, Taisho Toyama, MSD, Mitsubishi Tanabe, Sanofi, Takeda, Japan Tobacco, Novo Nordisk and Ono. Shin Tsunekawa received research funding from Johnson & Johnson, Daiichi Sankyo, Eli Lilly, Kyowa Hakko Kirin, Taisho Toyama, MSD, Mitsubishi Tanabe, Sanofi, Takeda, Japan Tobacco, Novo Nordisk and Ono. Yoshiro Kato received research funding from Johnson & Johnson, Daiichi Sankyo, Eli Lilly, Kyowa Hakko Kirin, Taisho Toyama, MSD, Mitsubishi Tanabe, Sanofi, Takeda, Japan Tobacco, Novo Nordisk and Ono. Jiro Nakamura received lecture fees from Kyowa Hakko Kirin, Ono, Pfizer, Eli Lilly, Novartis, Sanofi, MSD, Taisho Toyama, Mitsubishi Tanabe, Astellas and Shionogi, and research funding from Johnson & Johnson, Daiichi Sankyo, Eli Lilly, Kyowa Hakko Kirin, Taisho Toyama, MSD, Mitsubishi Tanabe, Sanofi, Takeda, Japan Tobacco, Novo Nordisk and Ono. Hideki Kamiya received lecture fees from Eli Lilly, Ono, Novartis, Astellas, MSD, Takeda, AstraZeneca, Boehringer Ingelheim, Sanofi and Novo Nordisk, and research funding from Johnson & Johnson, Daiichi Sankyo, Eli Lilly, Kyowa Hakko Kirin, Taisho Toyama, MSD, Mitsubishi Tanabe, Sanofi, Takeda, Japan Tobacco, Novo Nordisk and Ono.
Footnotes
The original online version of this article was revised due to table 2 and 3 was published incorrectly and corrected in this version.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/27/2021
A Correction to this paper has been published: 10.1007/s13340-021-00491-9
References
- 1.Health, Labour and Welfare Ministry. Japanese Practice Guidance to improve Patients’ Adherence to Appointments for Diabetes Care. http://human-data.or.jp/wp/wp-content/uploads/2018/07/dm_jushinchudan_guide43_e.pdf; 2014. Accessed on 13 Oct 2020.
- 2.Tanaka M, Ito H, Nemoto A, Ikeda N, Omoto T, Shinozaki M, et al. Relationship between the history of intermittent treatment for type 2 diabetes mellitus and the risk of diabetic vascular complications. J Jpn Diab Soc. 2019;58(2):100–108. [Google Scholar]
- 3.Okudaira M, Uchigata Y, Okada T, Iwarmoto Y. Influence of health checkup and previous intermittent treatment on diabetic complications. J Jpn Diab Soc. 2003;46(10):781–785. [Google Scholar]
- 4.Saisho Y, Itoh H. Relationship between treatment satisfaction and intention to drop out in outpatients with type 2 diabetes. J Japan Diab Soc. 2012;55(10):768–773. [Google Scholar]
- 5.Bradley C. The diabetes treatment satisfaction questionnaire: DTSQ. In: Bradley C, editor. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. Chur: Harwood Academic Publishers; 1994. pp. 111–132. [Google Scholar]
- 6.Home PD, Lindholm A, Riis A. Insulin aspart vs human insulin in the management of long-term blood glucose control in Type 1 diabetes mellitus: a randomized controlled trial. Diabet Med. 2000;17:762–770. doi: 10.1046/j.1464-5491.2000.00380.x. [DOI] [PubMed] [Google Scholar]
- 7.Ashwell SG, Bradley C, Stephens JW, Witthaus E. Treatment satisfaction and quality of life with insulin glargine plus insulin lispro compared with NPH insulin plus unmodified human insulin in individuals with type 1 diabetes. Diabetes Care. 2008;31:1112–1117. doi: 10.2337/dc07-1183. [DOI] [PubMed] [Google Scholar]
- 8.Best JH, Boye KS, Rubin RR, Cao D, Kim TH, Peyrot M. Improved treatment satisfaction and weight related quality of life with exenatide once weekly or twice daily. Diabet Med. 2009;26:722–728. doi: 10.1111/j.1464-5491.2009.02752.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camacho F, Anderson R, Safrit A, Jones AS, Hoffmann P. The relationship between patient’s perceived waiting time and office based practice satisfaction. N C Med J. 2006;67(6):409–413. [PubMed] [Google Scholar]
- 10.Rayson RS, Mas’uud IS, Thiru T, Lian LL, Yu HK. Factors affecting follow-up non-attendance in patients with Type 2 diabetes mellitus and hypertension: a systematic review. Singap Med J. 2019;60:216–223. doi: 10.11622/smedj.2019042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Archibald LK, Gill GV. Diabetic clinic defaulters—who are they and why do they default? Pract Diabetes Int. 1992;9:13–14. doi: 10.1002/pdi.1960090104. [DOI] [Google Scholar]
- 12.Hammersley MS, Holland MR, Walford S, Thorn PA. What happens to defaulters from a diabetic clinic? Br Med J. 1985;291:1330–1332. doi: 10.1136/bmj.291.6505.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holly C, Robert AW, Sarah N, Thomas PG, Bich ND. The psychology of the wait time experience—what clinics can do to manage the waiting experience for patients: a longitudinal, qualitative study. BMC Health Serv Res. 2019;19(1):459. doi: 10.1186/s12913-019-4301-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhenzhen X, Calvin O. Associations between waiting times, service times, and patient satisfaction in an endocrinology outpatient department: a time study and questionnaire survey. Inquiry. 2017;54:1–10. doi: 10.1177/0046958017739527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Locke R, Stefano M, Koster A, Taylor B, Greenspan J. Optimizing patient/caregiver satisfaction through quality of communication in the pediatric emergency department. Pediatr Emerg Care. 2011;27(11):1016–1021. doi: 10.1097/PEC.0b013e318235be06. [DOI] [PubMed] [Google Scholar]
- 16.Boudreaux ED, Friedman J, Chansky ME, Baumann BM. Emergency department patient satisfaction: examining the role of acuity. Acad Emerg Med. 2004;11(2):162–168. doi: 10.1111/j.1553-2712.2004.tb01428.x. [DOI] [PubMed] [Google Scholar]
- 17.Mowen JC, Licata JW, McPhail J. Waiting in the emergency room: how to improve patient satisfaction. J Health Care Mark. 1993;13(2):26–33. [PubMed] [Google Scholar]
- 18.Taylor S. Waiting for service: the relationship between delays and evaluations of service. J Market. 1994;58:56–69. doi: 10.1177/002224299405800205. [DOI] [Google Scholar]
- 19.Thompson DA, Yarnold PR, Williams DR, Adams SL. Effects of actual waiting time, perceived waiting time, information delivery, and expressive quality on patient satisfaction in the emergency department. Ann Emerg Med. 1996;28(6):657–665. doi: 10.1016/s0196-0644(96)70090-2. [DOI] [PubMed] [Google Scholar]
- 20.Levesque J, Bogoch ER, Cooney B, Johnston B, Wright JG. Improving patient satisfaction with time spent in an orthopedic outpatient clinic. Can J Surg. 2000;43(6):431–436. [PMC free article] [PubMed] [Google Scholar]
- 21.Emily TLH. Improving waiting time and operational clinic flow in a tertiary diabetes center. BMJ Qual Improv Rep. 2014;2(2):u201918.w1006. doi: 10.1136/bmjquality.u201918.w1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jehni R, Melody P, Yara M, Carol JP. Losing the wait: improving patient cycle time in primary care. BMJ Open Qual. 2020;9:e000910. doi: 10.1136/bmjoq-2019-000910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tokunaga M, Watanabe S, Nakane N. Survey on outpatients' waiting time and satisfaction level. J Jpn Soc Health Care Manag. 2006;7(2):324–328. [Google Scholar]


