Abstract
Suboptimal hearing aid use negatively impacts health and well-being. The aim of this study was to conduct a controlled trial of a behavior change intervention to promote hearing aid use. This study was a quasi-randomized controlled trial with two arms. A total of 160 first-time hearing aid users were recruited at their hearing aid fitting appointments. The control arm received standard care. In addition to standard care, the intervention arm received I-PLAN, which comprised (a) information about the consequences of hearing aid use/nonuse, (b) reminder prompt to use the hearing aids, and (c) an action plan. The primary outcome, measured at 6 weeks, was self-reported proportion of time the hearing aid was used in situations that caused hearing difficulty. Secondary outcomes were data-logged hearing aid use, self-reported hearing aid benefit, self-regulation, and habit formation. The results showed that the proportion of time the hearing aids were used in situations that caused hearing difficulty was similar in both groups. There were no statistically significant differences between groups in any outcome measure including data-logged hearing aid use. The relatively high levels of hearing aid use across research participants may have limited the potential for the intervention to impact on hearing aid use. Although the intervention materials proved acceptable and deliverable, future intervention trials should target suboptimal hearing aid users.
Keywords: hearing aids, intervention, audiologists, adult patients
Hearing aids are the main treatment for hearing loss (Grenness et al., 2015; Pryce et al., 2016) and are effective in improving hearing-related quality of life (Chisolm et al., 2007; Ferguson et al., 2017). However, studies report that 5% to 24% of hearing aid owners do not use their hearing aids (Aazh et al., 2015; Hartley et al., 2010; Hougaard & Ruf, 2011; Solheim & Hickson, 2017) and 40% of new adult patients use their hearing aids fewer than 4 hours per day (Aazh et al., 2015). A recent study reported that adult patients were highly motivated to use their hearing aids but had difficulty translating motivation into action (i.e., “volitional processes”; Sawyer et al., 2019). This suggests that interventions should target “volitional processes” (e.g., action planning) to increase hearing aid use among adult patients (Sawyer et al., 2019). In addition, given that little is known about what behaviors audiologists perform that may facilitate hearing aid use, studies that involve audiologists delivering interventions face-to-face are needed to provide an evidence base for clinical practice (Ismail et al., 2019).
Although various interventions have attempted to promote hearing aid use, a Cochrane systematic review found that none of the 37 trials improved hearing aid use (Barker, Mackenzie, Elliott, et al. 2016). One of the reasons is that none of the interventions were developed using behavior change theory and evidence (Armitage et al., 2017), for example, the behavior change wheel (Michie et al., 2014). The behavior change wheel is a systematic approach for designing behavior change intervention (Michie et al., 2014). It was developed based on a systematic review and a synthesis of 19 multiple frameworks of behavior change (Michie et al., 2014). Using the behavior change wheel, Barker et al. (2018) developed the “I-PLAN” intervention. The I-PLAN intervention aims to support audiologists during hearing aid fitting appointments to support adult patients in using their hearing aids. The I-PLAN comprises three components: (a) provision of information related to the benefits of using and disadvantages of not using a hearing aid, (b) provision of prompts as a reminder for hearing aid use, and (c) creation of an action plan for hearing aid use (Barker et al., 2018; see Table 1). Given previous intervention studies were focused on providing information relating to communication techniques to reduce negative impact of hearing loss and/or information concerning the management and use of hearing aids (Barker, Mackenzie, Elliott, et al., 2016), the I-PLAN intervention is a promising intervention to promote hearing aid use. The components of the I-PLAN target both motivation (via provision of information) and volitional processes (via provision of prompt and plan) of adult patients. To date, there remains a paucity of evidence on the effectiveness of the I-PLAN intervention.
Table 1.
Active Components of the I-PLAN Intervention.
| Components of the I-PLAN | Behavior Change Technique (BCT) | Definition (from BCTTv1; Michie et al., 2013) |
|---|---|---|
| Provision of information related to consequences of hearing aid use and nonuse | 5.1 Information about health consequences | Provide information (e.g., written, verbal, and visual) about health consequences of performing the behavior |
| 5.3 Information about social and environmental consequences | Provide information (e.g., written, verbal, and visual) about social and environmental consequences of performing the behavior | |
| Provision of a prompt to remind patients to use their hearing aids | 7.1 Prompts/cues | Introduce or define environmental or social stimulus with the purpose of prompting or cueing the behavior. The prompt or cue would normally occur at the time or place of performance |
| 12.5 Adding objects to the environment | Add objects to the environment in order to facilitate performance of the behavior | |
| 1.4 Action planning | Prompt detailed planning of performance of the behavior (must include one of context, frequency, duration and intensity). Context may be environmental (physical or social) or internal (physical, emotional, or cognitive) | |
| Creation of a written behavioral plan for hearing aid use | 1.1 Goal setting (behavior) | Set or agree a goal defined in terms of the behavior to be achieved |
| 1.2 Problem solving | Analyze or prompt the person to analyze factors influencing the behavior and generate or select strategies that include overcoming barriers and/or increasing facilitators | |
| 1.4 Action planning | Prompt detailed planning of performance of the behavior (must include one of context, frequency, duration and intensity). Context may be environmental (physical or social) or internal (physical, emotional, or cognitive) |
In addition to testing the I-PLAN intervention, we wanted to understand the potential mechanisms of action thereby allowing the intervention to be optimized (Bauman et al., 2002) and considered two potential avenues. First, given that the intervention is designed to enhance self-regulation (defined as “any efforts undertaken to alter one’s behavior”; Sniehotta et al., 2005; p. 245), we assessed the three action control constructs that play major roles in self-regulation: awareness of standards for action, self-monitoring, and self-regulatory effort as potential mediators of any effect (Sniehotta et al., 2006). Therefore, self-regulation can be considered as a personal process that involves monitoring, evaluating, and readjusting one’s behavior to achieve a behavior goal (e.g., using a hearing aid). Second, action plans specified in the “when-then” format (as in this study) have been shown to change behavior via habits (Armitage, 2016) and repeated successful performance of behaviors leads to habit formation (Gardner et al., 2012). Habit is “a process by which a stimulus generates an impulse to act as a result of a learned stimulus-response association” (Gardner, 2015, p. 277). The components of the I-PLAN may facilitate habit formation by providing opportunity for patients to use their hearing aids in a similar context every day, so we additionally assessed habit as a potential mediator.
Aim and Hypotheses
We evaluated the effectiveness of I-PLAN (delivered face-to-face by audiologists during hearing aid fitting appointments) in promoting hearing aid use and benefit compared with standard care among first-time adult hearing aid users. We hypothesized that relative to participants who received standard care, participants who received I-PLAN would report higher hearing aid use in situations that caused hearing difficulty, greater hearing aid use measured via data-logging, greater hearing aid benefits measured by self-reported benefit on an outcome inventory, and higher self-regulation and habit formation measured by scores on self-regulation and habit formation measured by scores on self-regulation and behavioral automaticity questionnaires. We also hypothesized that self-regulation and habit formation would mediate the effect of the I-PLAN intervention on hearing aid use and benefit.
Methods
Study Design
This was a quasi-randomized study design with two arms; I-PLAN group and Standard Care group. Allocation of participants to condition was based on (a) when participants were able to attend their hearing aid fitting appointments and (b) the clinic schedules of study audiologists. Participants in the I-PLAN group received the I-PLAN intervention at the time of hearing aid fitting.
This study received National Health Service ethical approval from the North West–Greater Manchester East Research Ethics Committee and from the University of Manchester Ethics Committee (REC reference 17/NW/0406). This study was registered in the clinical trials database (ClinicalTrials.gov identifier is NCT04017416).
Setting
This study was conducted in a single-center audiology service in Manchester, United Kingdom. The study was conducted from January to December 2018.
Outcome Measures
The primary outcome, assessed 6 weeks post-intervention, was self-reported use of hearing aids in situations that caused hearing difficulty. The secondary outcomes were hearing aid use measured via data-logging, self-report of hearing aid benefit, self-regulation, and habit formation. The 6 weeks period between intervention and outcome assessments was chosen because it is a routine practice in U.K. National Health Service audiology clinics for patients to be followed up at 6 weeks after hearing aid being fitted. The outcome measures were as follows.
Hearing Aid Use in Situations That Cause Hearing Difficulty Unaided
A question adapted from the Glasgow Hearing Aid Benefit Profile (Gatehouse, 1999) was used to assess hearing aid use in difficult situations: “In a typical situation where you have hearing difficulty, what proportion of time do you wear your hearing aid?,” with five response options: never/not at all (0% of time), about one fourth of the time (25% of the time), one half of the time (50% of the time), three fourth of the time (75% of the time), or all the time (100% of the time). Proportion of time hearing aids were used in situations that caused hearing difficulty was measured because the aim of the I-PLAN intervention was to promote hearing aid use in listening situations based on individual needs (as specified in the “when-then” format). In addition, hearing aid use in the most critical listening situations based on individual needs is a good index of “optimal” hearing aid use (Laplante-lévesque et al., 2013).
Hearing Aid Use
An objective measure of hearing aid use was generated automatically by the hearing aid(s) data logging feature. Hearing aid use data were reported in terms of mean hours/day. The mean of the right and left hearing aid was used for participants with two hearing aids.
International Outcome Inventory for Hearing Aids
The International Outcome Inventory for Hearing Aids (IOI-HA) was used to capture self-reported hearing aid benefit (Cox & Alexander, 2002). The IOI-HA is widely used to measure hearing aid outcomes (Perez & Edmonds, 2012) and comprises seven questions such as hearing aid use, hearing aid benefit, residual activity limitations, satisfaction, residual participation restrictions, impact on others, and quality of life. Five response options are provided for each question with a score from 1 to 5 (total score 7–35). Higher scores indicate better outcomes.
Hearing Handicap Inventory for the Elderly–Screening version
The Hearing Handicap Inventory for the Elderly–Screening version (HHIE-S; Ventry & Weinstein, 1983) measures self-perceived hearing handicap. The HHIE-S consists of 10 questionnaires and assesses the effect of hearing loss on emotional and social domains. For example; “do you feel handicapped by a hearing problem?” (emotional domain) and “does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors?” (social domain). Response options are yes (4 points), sometimes (2 points), or no (0 points). Higher scores indicate greater perceived hearing handicap.
Self-regulation
Three components of self-regulation such as awareness of standards for action, self-monitoring, and self-regulatory effort were assessed. Self-regulation questions were adapted from a self-regulation questionnaire on physical activity by Sniehotta et al. (2006). There are six items (two items/component) with a 7 point Likert-type scale (1 strongly disagree to 7 strongly agree). All the items began with a statement “During the last six weeks, I … and followed by statements relating to self-regulation. For example; “ … often had the intention to use my hearing aid(s) on my mind” (awareness of standards) or “ … tried hard to use my hearing aid regularly” (self-regulatory effort). Higher scores indicate greater self-regulation. The scale showed good internal consistency with a Cronbach’s alpha of .77 in this study.
Self-Report Behavioral Automaticity Index
Habit formation in relation to hearing aid use was measured using the four items of the Self-Report Behavioral Automaticity Index (Gardner et al., 2012). All the questions began with a phrase “Using hearing aid(s) is something … ” “ … I do automatically,” “I do without thinking,” “ … I do without having to consciously remember to use them” and “ … I start doing before I realize I am doing it.” The four items were answered on 7 point Likert-type scale (1 strongly disagree to 7 strongly agree). Higher scores indicate stronger habit. The scale showed good internal consistency with a Cronbach’s alpha of .93 in this study.
The I-PLAN Written Materials
We developed three I-PLAN components for audiologists to use with their patients during hearing aid fitting consultations. We chose to develop written I-PLAN materials because they will (a) minimize effort needed by audiologists to remember the content of the I-PLAN, (b) maximize participant’s recall of the I-PLAN information (Reese & Hnath-Chisolm, 2005), and (c) make it possible to replicate the intervention for future research or clinical implementation. In addition, I-PLAN written materials also would serve as a checklist to monitor fidelity of the I-PLAN (Supplemental Material 2). The I-PLAN written materials were as follows.
Information on Consequences of Using and Not Using a Hearing Aid
We reviewed the literature (e.g., Scarinci et al., 2008; Vas et al., 2017) in order to identify commonly reported consequences of using/not using a hearing aid. To determine which consequences would be included in the I-PLAN written materials, we consulted public involvement representatives. The representatives consisted of three adult patients with hearing loss aged between 50 and 70 years, two significant others and two audiologists. All participants were asked to rank lists of consequences of hearing aid use/nonuse in order of importance (1 = most important and 5 = least important). Based on the Modified Borda Count method, each participant’s preferred options were assigned weights (1 = 5 points; 5 = 1 point). Then, the scores were added and averaged to identify the top three preferred options across participants. The top three positive and negative consequences were included in the I-PLAN written material (Behavior change Technique [BCT]: 5.3; Information about social and environmental consequences; Michie et al., 2013).
A Prompt for Hearing Aid Use
In standard care, a hearing aid box is provided free to the patients for safekeeping of hearing aid when not in use (BCT: 12.5; Adding objects to the environment; Michie et al., 2013). For example, “these two boxes here are to store each of your hearing aids in.” In the I-PLAN intervention, the hearing aid box would be explicity identified to patients by audiologists as a physical prompt to remind patients to use their hearing aid (BCT: 7.1; prompts/cues; Michie et al., 2013).
A Written Action Plan for Hearing Aid Use
In standard care, patients are advised to use their hearing aids (e.g., to use the hearing aid all the time; BCT: 1.1; Goal setting [behavior]; Michie et al., 2013). In the I-PLAN intervention, audiologists were asked to collaborate with their patients to produce a specific plan on “where” and “when” to use their hearing aids (BCT: 1.4; Action planning; Michie et al., 2013). The instruction was adapted from “volitional help sheets,” used previously to promote smoking cessation (Armitage, 2008), physical activity (Armitage & Arden, 2010) and to reduce alcohol intake (Armitage & Arden, 2012). In this study, we did not operationalize “problem solving” (BCT: 1.2; Michie et al., 2013), because we judged that first-time hearing aid users may have difficulty identifying barriers to using hearing aids as they have not yet had any experience with hearing aids. The I-PLAN intervention written materials are in Table 2.
Table 2:
The Details of the I-PLAN Intervention Written Materials.
| Components of the I-PLAN | Behavior Change Technique (BCT) | Written Materials of I-PLAN |
|---|---|---|
| Provision of information related to consequences of hearing aid use and nonuse | 5.3 Information about social and environmental consequences |
Hearing aid use will improve: • your ability to hear others • your social interactions • the lives of those around you by making it easier for them to communicate with you. Not using a hearing aid will: • reduce your ability to hear your family and friends • lead you to withdraw from social activities • cause stress and increase burden on those around you by making it harder for them to communicate with you. |
| Provision of a prompt to remind patients to use their hearing aids | 7.1 Prompts/cues |
My hearing aid reminder Please use your hearing aid box as a reminder to wear your hearing aid(s). For example, you could put your hearing aid box next to the bathroom mirror last thing at night to remind you to wear your hearing aid(s) in the morning. |
| Creation of a written behavioral plan for hearing aid use | 1.4 Action planning |
My hearing aid(s)
Please plan where and when to wear your hearing aid(s). You can choose any place and time but please write your plan in as much detail as possible. Please write your plan in the space provided. Example: “When I have finished brushing my teeth in the morning, then I will wear my hearing aid(s)” Please write your plan in the space provided in the format in the example. When I……………., then I will wear my hearing aid(s). Use the space below if you want to write more than one plan. |
Participants
The sample size calculation using G-power software (Faul et al., 2007) suggested that 128 adult patients (64 participants per group) would provide 80% statistical power to detect a significant difference on the proportion of time hearing aids were used (the primary outcome measure) between the groups with a medium-sized effect of Cohen’s f squared (f 2 = 0.0625) using a multivariate analysis of variance (MANOVA; α = .05). However, to allow for attrition, we aimed to recruit 80 participants in each group (n = 160 participants).
Adult patients who were scheduled for initial hearing aid fitting appointments were invited to participate in this study. Adults were eligible if they (a) had no previous personal experience of using a hearing aid, (ii) were aged 18 years old or above, (iii) attended initial hearing aid fitting appointment with study audiologists, (iv) were native English speakers or had good understanding of English, and (v) had sufficient mental capacity to provide informed consent based-on-audiologist’s opinion were eligible to take part in this study. The exclusion criteria were (a) inability to complete the questionnaires due to age-related problems (e.g., dementia) based-on-audiologist’s opinion and (b) presence of medical contraindications for hearing aids as described by the British Academy of Audiology (2007).
For each patient, an invitation letter, participant information sheet, consent form, and baseline questionnaire were posted at least 2 days prior to their hearing aid fitting appointment. If patients decided to take part in the study, they were asked to sign the consent form, complete the questionnaire at home and return the completed documents to their audiologist at the hearing aid fitting appointment.
Neither the study audiologists nor the authors had any role in allocation of participants to the two groups. Participants scheduling was carried out by clinical administrative staff. Allocation of participants to the study audiologists in both groups was designed to be as close as possible to the clinic procedures to minimize the demands on the participating audiological clinic. Participants were blinded to group allocation as they did not know which audiologists were delivering the I-PLAN or Standard Care when they attended their hearing aid fitting appointments. It was not possible to blind study audiologists to group allocation.
Study Audiologists
Four of seven audiologists (n = 4) in the participating U.K. National Health Service audiology clinic volunteered to help in this study. Audiologists who volunteered to help but were not interested in delivering the I-PLAN were assigned to the Standard Care group (n = 2). Audiologists who were interested in delivering the I-PLAN intervention were allocated to the I-PLAN group and attended the I-PLAN training session (n = 2). All four study audiologists were working full-time with adult patients in the audiology department (Table 3).
Table 3.
Characteristics of Study Audiologists.
| Characteristic |
I-PLAN |
SC |
||
|---|---|---|---|---|
| Audiologist 1 | Audiologist 2 | Audiologist 3 | Audiologist 4 | |
| Age (years) | 27 | 25 | 48 | 23 |
| Working experience (years) | 3.0 | 3.5 | 24 | 0.3 |
Note. SC = standard care.
Two hearing aid fitting consultations each were video recorded for all four study audiologists prior to the commencement of the study in order to (a) establish that usual clinical practice was different to the I-PLAN intervention and (b) provide a baseline description of clinical interactions of the study audiologists. Videos were independently reviewed by the first (Ismail) and one co-author (Dawes). Both of the authors recorded the audiologists’ clinical practice in a checklist form (Supplemental Material 1) that was developed based on the description and examples of U.K. audiologists’ practice observed in Barker, Mackenzie, and de Lusignan's (2016) study. The form was completed independently by the authors. Analysis of the video-recorded clinical consultations confirmed that the clinical practice of all study audiologists also was similar to that observed in Barker, Mackenzie, and de Lusignan’s description of the clinical practice of U.K. audiologists (see Supplemental Material 1). Clinical practice of the study audiologists did not differ between the audiologists who would later deliver the I-PLAN intervention versus those who would deliver standard care only. Comparability of I-PLAN and standard care audiologists prior to training was confirmed by showing no differences in the clinical and demographic characteristics and hearing aid use (data-logged hours of hearing aid use) of patients seen by each study audiologist in the 3 months before the study commenced (Supplemental Material 3).
I-PLAN Training
At the commencement of the study, two audiologists attended an I-PLAN training session with the first author (Ismail). The I-PLAN training session included an explanation of the development and components of the I-PLAN. Training also included a practical session using the I-PLAN where audiologists delivered the I-PLAN on each other via a role play exercise. The training lasted for about 1 hr. Following the training session, the two I-PLAN audiologists practiced delivering the I-PLAN to three first-time hearing aid patients each (n = 6, in total).
Fidelity to the I-PLAN Intervention
Three months after the study had commenced, hearing aid fitting consultations were video recorded for all study audiologists. In the I-PLAN group, four audiologist–patient consultations selected at random (n = 4; 2 patients/audiologist) were video recorded to monitor fidelity of delivery of the I-PLAN intervention by the study audiologists. The audiologists’ verbal statements were independently checked by the first (Ismail) and one co-author (Dawes) using a checklist for the content of the I-PLAN (Supplemental Material 2). In the Standard Care group, two audiologist–patient consultations were also selected at random (n = 2; 1 patient/audiologist) and video recorded to monitor the consistency of the behavior of standard care audiologists during the research study. Videos of the clinical consultations of audiologists at 3 months after the I-PLAN audiologists received I-PLAN training showed that the I-PLAN audiologists delivered the I-PLAN components as prescribed in the I-PLAN written materials (Supplemental Material 2). The clinical interactions of the standard care audiologists 3 months after the commencement of the study were consistent with observations of clinical interactions before the commencement of the study.
Hearing Aid Fitting Appointment
Standard Care Group
Audiologists in the Standard Care group were instructed to manage the participants in the same way as they would do in their routine clinics. All the procedures conducted in the routine clinical practice were in accordance with national practice guidelines and were typical of National Healthcare Services audiology departments across the United Kingdom. Specifically, standard care fitting appointments involved (a) programming of hearing aid(s); (b) performing real ear measurement ; (c) advising patients on realistic expectations (e.g., hearing aid does not restore normal hearing), communication tactics, and habituation to a hearing aid; (d) providing demonstration and instruction to operate a hearing aid; (e) explanation on services provided (access battery and repair service); (f) providing patients with batteries, hearing aid box, and written information about specific hearing aid fitting; (g) explanation about what to expect at the follow-up appointment; and (h) booking for hearing aid follow-up appointment in 6 weeks’ time. The hearing aid fitting consultation lasted up to 45 min.
I-PLAN Group
Participants in the I-PLAN group received a consultation from one of the two study audiologists trained to deliver I-PLAN. The study audiologists were instructed to deliver the I-PLAN by integrating the I-PLAN into their routine hearing aid fitting consultation. At the end of the consultation, participants were given their I-PLAN cards to take with them.
Follow-Up Appointment
All participants across the groups received a 6-week face-to-face hearing aid follow-up appointment per usual clinical care. Approximately 2 days before the 6 weeks follow-up appointment, a questionnaire was posted to the participants. Participants were asked to bring the completed questionnaire with them to the appointment. At the follow-up appointment, the audiologist discussed the particular difficulties participants were having with their hearing aid(s) and provided further education, practice, advice, and hearing-aid adjustment as required. Data on hearing aid usage (averaged across the whole 6 weeks) were downloaded from the hearing aids. When participants did not attend their follow-up appointment, they were sent a postage-paid addressed envelope and were asked to return the questionnaire to the researcher.
Statistical Analysis
Descriptive statistics were used to summarize the characteristics of participants. Potential differences in baseline variables were assessed using a MANOVA and chi-square. To investigate the effectiveness of the I-PLAN intervention on the outcome measures, a MANOVA was performed. All the analyses were performed using SPSS software version 21.0.
Results
Recruitment and Retention
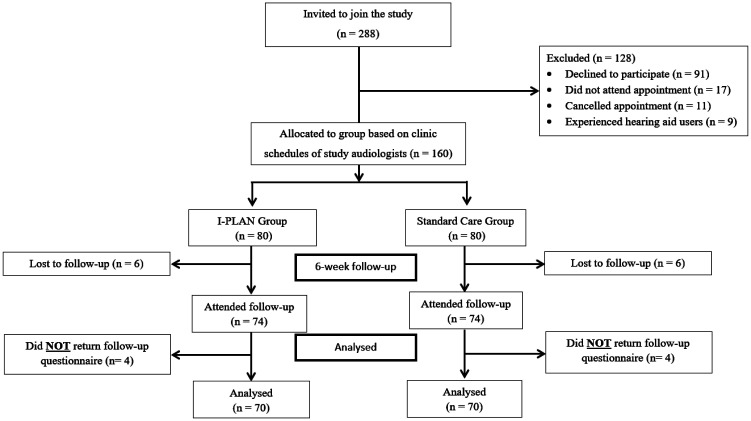
Flow of study participants for this study is illustrated in Figure 1. Prior to a hearing aid fitting appointment, 288 patients were invited to participate in the study by email. At the hearing aid fitting appointment, 160 (55.5%) agreed to participate in this study and were allocated to the I-PLAN group (n = 80) or Standard Care group (n = 80). In addition, 12 participants (7.5%; 6 from each group) did not attend (DNA) the 6-week hearing aid follow-up.
Figure 1.
Study Flow Diagram for the Main Analysis (n = 140).
Of 148 participants who attended the follow-up appointments, 8 participants (5.4%; 4 from each group) did not return their follow-up questionnaire. Six additional follow-up questionnaires were received from participants who did not attend their follow-up appointment (five participants from the I-PLAN group and one participant from the Standard Care group). Therefore, a total of 146 follow-up questionnaires were received from participants of this study.
Clinical and Demographic Characteristics of Participants
Table 4 shows the characteristics of the participants recruited to the study and allocated to the I-PLAN group and Standard Care group at the hearing aid fitting appointment. Consistent with the sampling frame, all participants recruited to this study were first-time hearing aid users. The mean age of all participants was 72 years (SD = 10.7, range 41–91 years). Approximately half (52%) were males. All the participants across the groups were fitted with behind-the-ear hearing aid(s). In addition, 62% (99 out of 160) of the participants were fitted bilaterally. The mean score of the self-perceived hearing handicap based on the HHIE-S (unaided) questionnaire was 20.5 (SD = 9.6) which indicates a mild-moderate hearing handicap.
Table 4.
Clinical and Demographic Characteristics of Participants Recruited to This Study and Allocated to the I-PLAN or Standard Care (SC) Group at the Hearing-Aid Fitting Appointment.
| Characteristic |
I-PLAN (n = 80) |
SC (n = 80) |
||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Age (years) | 73.7 | 9.4 | 70.4 | 11.7 |
| Age range (years) | 41–91 | 42–91 | ||
| Hearing loss (dBHL)a | 34.7 | 11.9 | 33.6 | 13.4 |
| HHIE-S (unaided) | 21.6 | 9.5 | 19.4 | 9.6 |
| Gender | N | % | N | % |
| Male | 41 | 51.2 | 42 | 52.5 |
| Female | 39 | 48.8 | 38 | 47.5 |
| Fitted ear | ||||
| Unilateral | 32 | 40.0 | 29 | 36.3 |
| Bilateral | 48 | 60.0 | 51 | 63.7 |
Note. HHIE-S = Hearing Handicap Inventory for the Elderly–Screening version.
aAverage of hearing thresholds at .5, 1, 2, and 4 kHz in the better ear.
At the hearing aid fitting appointment, based on MANOVA, there was a significant difference between I-PLAN group and Standard Care group in baseline characteristics, F(3, 156) = 2.81; p = .04; Pillai’s trace V = 0.05; Partial η2 = 0.05. Decomposition of this effect using univariate analyses of variance showed there was a borderline significant difference in age, F(1, 158) = 3.69; p = .06, between the two groups. The mean age was higher for I-PLAN by 3 years. Given how close the two groups are in age, this seems surprising and likely due to the high number of participants. There were no significant differences in pure tone average, F(1, 158) = 0.34; p = .56, and HHIE-S (unaided; F1, 158 = 2.21; p = 0.14, between the two groups. There were no significant differences between I-PLAN and Standard Care groups in gender, χ2(1) = 0.03; p = .87, and fitted ear, χ2(1) = 0.24; p = .63, based on Chi-Square tests.
There was also no significant difference in baseline characteristics between those who did and did not attend the 6-week follow-up appointment (Supplemental Material 4).
Hearing Aid Use
Self-Reported Hearing Aid Use in Situations That Caused Hearing Difficulty Unaided
Out of 146 participants who returned their follow-up questionnaire, the mean proportion of time the hearing aids were used in situations that caused hearing difficulty unaided was 81.0% (SD = 25.9) of the time for the I-PLAN group (n = 75) and 79.6% (SD = 29.4) of the time for the Standard Care group (n = 71). Four participants (2.7%) reported that they used their hearing aids “never/not at all of the time” in situations where they had hearing difficulty. All of these participants were in the Standard Care group. Across both groups, 11 participants (7.5%) reported using their hearing aids for “one fourth of the time,” 19 (13%) for “one half of the time,” 28 (19.2%) for “three fourth of the time,” and 84 (57.5%) for “all the time.” Figure 2 shows the frequency of self-reported hearing aid use for the I-PLAN and Standard Care groups.
Figure 2.
The Frequency of Hearing Aid Use Measured via Self-Reported Hearing Aid Use in Situations That Caused Hearing Difficulty Unaided for the I-PLAN and Standard Care Groups.
Objective Hearing Aid Use Measured Via Data Logging
Overall, average hearing aid use as measured via data logging by all participants (n = 148) at the 6-week follow-up appointment was 9.3 (SD = 5.2) hours per day. Mean hearing aid use in the I-PLAN group (n = 74) was 9.7 (SD = 4.9) hours per day. Mean hearing aid use in the Standard Care group (n = 74) was 8.8 (SD = 5.6) hours per day. Figure 3 shows the distribution of hearing aid use for the I-PLAN and Standard Care groups. Among participants who attended the 6-week follow-up appointment but did not return the follow-up questionnaire (n = 8), the mean hearing aid use was 6.5 (SD = 5.0) hours per day.
Figure 3.
The Distribution of Hearing Aid Use Measured Via Data-Logging (Hours Per Day) According to Groups. The middle line in the boxplot represents the median.
Out of 148 participants, 16.9% (25 out of 148) used their hearing aid fewer than 4 hours per day (“non-regular hearing aid use,” according to criteria used by Aazh et al., 2015). Of the 25 participants, 15 (20.3%) of the participants were in the Standard Care group (n = 74) and 10 (13.5%) were in the I-PLAN group (n = 74).
Effects of the I-PLAN Intervention
As shown in Table 5, the I-PLAN intervention had no impact on hearing aid use (proportion of time of hearing aid use or data-logging, benefit [IOI-HA or HHIE-S (aided)]) and potential mediators (self-regulation or habit formation). There was no significant effect between the I-PLAN and Standard Care groups for any of the measures, F(6, 133) = 0.46; p = .83; Pillai’s trace V = 0.02 Partial η2 = 0.02.
Table 5.
Outcome Measures for the I-PLAN and Standard Care (SC) Groups 6-Week Follow-Up Appointment.
| Outcome measures |
I-PLAN (n = 70)a |
SC (n = 70)a |
Mean difference (95% CI) | d | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Proportion of time (%) | 81.4 | 25.4 | 80.0 | 29.4 | 1.4 [−7.8, 10.6] | 0.1 |
| Data logging (hours/day) | 9.8 | 5.0 | 9.1 | 5.5 | 0.7 [−1.1, 2.4] | 0.1 |
| IOI-HA | 28.5 | 4.0 | 28.3 | 4.3 | 0.2 [−1.2, 1.6] | 0.0 |
| HHIE-S (aided) | 14.6 | 9.4 | 12.6 | 9.2 | 1.9 [−1.2, 5.1] | 0.2 |
| Self-regulation | 5.1 | 0.9 | 5.0 | 1.1 | 0.2 [−0.2, 0.5] | 0.1 |
| SRBAI | 4.6 | 1.5 | 4.6 | 1.5 | 0.1 [−0.4, 0.5] | 0.0 |
Note. HHIE-S =Hearing Handicap Inventory for the Elderly–Screening version; IOI-HA = International Outcome Inventory for Hearing Aids; SRBAI = Self-Report Behavioral Automaticity Index
aThe reported mean and standard deviations values are “raw” and not adjusted for baseline characteristics. The analyses were based on data obtained in participants who attended the 6 weeks follow-up appointment and returned the follow-up questionnaire (I-PLAN, n = 70 and Standard Care, n = 70).
Note: Second analysis for self-reported outcomes was also conducted. The analysis was based on data obtained in participants who returned their follow-up questionnaire (I-PLAN, n = 75 and Standard Care, n = 71). The results remained nonsignificant.
Discussion
This study investigated face-to-face delivery of the I-PLAN to promote hearing aid use and benefit among adult first-time hearing aid users. There was no significant difference between the I-PLAN and Standard Care groups on hearing aid use measured by self-reported proportion of time hearing aids used in situations that caused hearing difficulty or data-logged hearing aid use, hearing aid benefit, IOI-HA, HHIE-S (aided), or potential mediators’ self-regulation and habit formation.
While the I-PLAN did not increase hearing aid use or benefit, it may be premature to conclude that the I-PLAN is ineffective in promoting hearing aid use. Average hearing aid use as shown by data logging by the participants in this study at the 6-week follow-up appointment was high (Mean148 = 9.3 hours; SD = 5.2). There may therefore be limited potential to increase hearing aid use among the first-time hearing aid users in this study. As participants were required to give informed written consent to participate, the sample recruited to the study may have been biased in favor of those who were motivated to help with hearing research, and so may also be more likely to use their hearing aid(s) than those who declined to participate. It may be desirable to target those at high risk of not using or under using their hearing aids for interventions to promote hearing aid use, rather than delivering interventions to those who use hearing aids regularly.
In addition, 16.9% (25 out of 148) of participants were nonregular hearing aid users (hearing aid use fewer than 4 hours per day; Aazh et al., 2015); much lower than the 40% non-regular users reported by Aazh et al. (2015) in a sample of new hearing aid users from another U.K. National Health Service audiology clinic. Hearing aid use may be different in different clinical samples. The clinic that hosted our study draws on a fairly affluent and well-educated population of patients, and hearing aid use rates may be above average in this study sample. There were no significant differences between non-regular and regular hearing aid users in other baseline characteristics in this study, but previous studies showed that adult patients who had a lower income (Lupsakko et al., 2005) and who did not perceive a need for a hearing aid (Lupsakko et al., 2005; Solheim et al., 2018) were more likely not to use or under use their hearing aids. Other factors that might predict low hearing aid use, for example, personality traits and coping strategies (Cox et al., 2005) or postmotivational variables (e.g., action planning; Sawyer et al., 2019). Combinations of demographic and/or psychological variables could be used to identify those who are likely not to use hearing aids and may benefit from interventions to promote hearing aid use.
It is possible that the behavior change techniques in the I-PLAN might interact with each other to reduce effectiveness (Michie et al., 2018). The I-PLAN intervention involved a combination of several behavior change techniques and it was not possible to disentangle the independent contributions of individual behavior change techniques in the I-PLAN. Factorial study designs could isolate and investigate how individual behavior change techniques relate to hearing aid use. Alternatively, there were dozens of potential behavior change techniques that were not incorporated in I-PLAN that could be tested in the future. In addition, given that participants may have received information concerning the consequences of using and not using a hearing aid at the hearing aid fitting appointment as part of standard care (e.g., Barker Mackenzie, & de Lusignan, 2016), it is also possible that some of the behavior change techniques specified in the I-PLAN, for example, the information about social and environmental consequences (BCT: 5.3; Michie et al., 2013) were also delivered by study audiologists in the Standard Care group. However, based on our video observations of clinical interactions in the Standard Care group, none of the information about social and environmental consequences as stated in the I-PLAN materials was delivered by the study audiologists. The video observations of the study audiologists were also in line with a systematic review which concluded that audiologists typically focus on provision of information concerning technical aspects of hearing aids during hearing aid consultations (Ismail et al., 2019).
The effectiveness of the I-PLAN may also depend how behavior change techniques are delivered (Michie et al., 2018). Although the style of delivery of the behavior change techniques was beyond the scope of this study, it is possible that individual consultation styles of audiologists could add noise to the outcome data. For example, audiologists with better communication skills may promote better patient adherence to the audiologist’s recommendations (see Zolnierek & DiMatteo, 2009). But as there was no difference in participant outcomes between study audiologists at the 6-week outcome assessment, it is unlikely that differences in interaction styles between audiologists had an appreciable impact on patient outcomes. Studies could investigate different modes of delivery of the I-PLAN components. For example, I-PLAN components could be provided in a written format without audiologists’ involvement, which may be easily implemented in the clinical routine. The I-PLAN components also could be provided on-line in video format (e.g., Ferguson et al., 2016). In addition, studies should ideally measure longer term outcomes than the 6-week follow-up in this study. Hearing aid use declines over longer durations (e.g., Humes et al., 2002) and useful interventions should support hearing aid use in the long term.
Limitations of the Study
First, there may have been contamination of the intervention across I-PLAN and standard care study audiologists given they were working in the same clinic. However, based on our video recordings, the clinical interactions of the standard care audiologists were consistent between observations prior to commencement of the study and 3 months after the commencement. A cluster randomized design using different clinical sites would eliminate the possibility of contamination in future studies. Second, participants were not randomized to group. In this study, randomization was not feasible. The procedures of this study were designed to be as close to routine clinic procedure in order to avoid additional burden on the clinic that was hosting the study. Third, the “standard care” at the host audiology clinic was comprehensive and included real ear verification and counseling. There may have been little scope to improve on this high standard of care and limiting the benefits of the I-PLAN.
Conclusion
This was a controlled trial of the I-PLAN intervention to promote hearing aid use and benefit among first-time adult hearing aid users. There were no statistically significant differences in any outcome measure. The I-PLAN intervention might be effective in promoting hearing aid use among patients with lower levels of hearing aid use than was the case for this study sample, where average hearing aid use was high. Interventions to promote hearing aid use should seek to identify and target those who are at risk of not using their hearing aid.
Supplemental Material
Supplemental material, sj-pdf-1-tia-10.1177_2331216520969472 for A Quasi-Randomized Controlled Trial of the I-PLAN Intervention to Promote Hearing Aid Use Among First-Time Adult Hearing Aid Users by Afzarini H. Ismail, Kevin J. Munro, Christopher J. Armitage, Antonia Marsden and Piers D. Dawes in Trends in Hearing
Acknowledgments
The authors would like to thank the audiology team at Central Manchester University Hospitals NHS Foundation Trust for their help in recruiting participants. The authors also would like to thank Prof. Harvey Dillon for his constructive feedback on an early version of this manuscript and Dr. Fiona Barker for her advice and support for this study.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Ministry of Higher Education Malaysia, International Islamic University Malaysia, NIHR Manchester Biomedical Research Centre and the NIHR Greater Manchester Patient Safety Translational Research Centre. Mrs. Ismail was funded by the Ministry of Higher Education Malaysia and the International Islamic University Malaysia.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs
Afzarini H. Ismail https://orcid.org/0000-0002-0126-7386
Kevin J. Munro https://orcid.org/0000-0001-6543-9098
References
- Aazh H., Prasher D., Nanchahal K., Moore B. C. J. (2015). Hearing-aid use and its determinants in the UK National Health Service: A cross-sectional study at the Royal Surrey County Hospital. International Journal of Audiology, 54(3), 152–161. 10.3109/14992027.2014.967367 [DOI] [PubMed] [Google Scholar]
- Armitage C. J. (2008). A volitional help sheet to encourage smoking cessation: A randomized exploratory trial. Health Psychology, 27(5), 557–566. 10.1037/0278-6133.27.5.557 [DOI] [PubMed] [Google Scholar]
- Armitage C. J. (2016). Evidence that implementation intentions can overcome the effects of smoking habits. Health Psychology, 35(9), 935–943. 10.1037/hea0000344 [DOI] [PubMed] [Google Scholar]
- Armitage C. J., Arden M. A. (2010). A volitional help sheet to increase physical activity in people with low socioeconomic status: A randomised exploratory trial. Psychology and Health, 25(10), 1129–1145. 10.1080/08870440903121638 [DOI] [PubMed] [Google Scholar]
- Armitage C. J., Arden M. A. (2012). A volitional help sheet to reduce alcohol consumption in the general population: A field experiment. Prevention Science, 13(6), 635–643. 10.1007/s11121-012-0291-4 [DOI] [PubMed] [Google Scholar]
- Armitage C. J., Lees D., Lewis K., Munro K. J. (2017). Preliminary support for a brief psychological intervention to improve first-time hearing aid use among adults. British Journal of Health Psychology, 22(4), 686–700. 10.1111/bjhp.12244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Academy of Audiology. (2007). Guidance on the use of real ear measurement to verify the fitting of digital signal processing hearing aids. British Society of Audiology, (July), 1–20. https://doi.org/http://www.thebsa.org.uk/wp-content/uploads/2014/04/REM.pdf
- Barker F., de Lusignan S., Cooke D. (2018). Improving collaborative behaviour planning in adult auditory rehabilitation: Development of the I-PLAN intervention using the behaviour change wheel. Annals of Behavioral Medicine, 56, 489–500. 10.1007/s12160-016-9843-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker F., Mackenzie E., de Lusignan S. (2016). Current process in hearing-aid fitting appointments: An analysis of audiologists’ use of behaviour change techniques using the behaviour change technique taxonomy (v1). International Journal of Audiology, 55(11), 643–652. 10.1080/14992027.2016.1197425 [DOI] [PubMed] [Google Scholar]
- Barker F., Mackenzie E., Elliott L., Jones S., & de Lusignan S. (2016). Interventions to improve hearing aid use in adult auditory rehabilitation. Cochrane Database of Systematic Reviews, 8, CD010342. 10.1002/14651858.CD010342.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman A. E., Sallis J. F., Dzewaltowski D. A., Owen N. (2002). Toward a better understanding of the influences on physical activity: The role of determinants, correlates, causal variables, mediators, moderators, and confounders. American Journal of Preventive Medicine, 23(2 Suppl), 5–14. 10.1016/S0749-3797(02)00469-5 [DOI] [PubMed] [Google Scholar]
- Chisolm T. H., Johnson C. E., Danhauer J. L., Portz L. J. P., Abrams H. B., Lesner S., McCarthy P. A., Newman C. W. (2007). A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology Task Force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology, 18(2), 151–183. 10.3766/jaaa.18.2.7 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C. (2002). The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric properties of the English version. International Journal of Audiology, 41(1), 30–35. 10.3109/14992020209101309 [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Gray G. A. (2005). Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear and Hearing, 26(1), 12–26. doi: 10.1097/00003446-200502000-00002. [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.G., Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behaviour Research Methods, 39(2), 175–191. 10.1088/1755-1315/148/1/012022 [DOI] [PubMed] [Google Scholar]
- Ferguson M., Brandreth M., Brassington W., Leighton P., Wharrad H. (2016). A randomized controlled trial to evaluate the benefits of a multimedia educational program for first-time hearing aid users. Ear and Hearing, 37(2), 123–136. 10.1097/AUD.0000000000000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson M., Kitterick P., Chong L., Barker F., Hoare D. (2017). Hearing aids for mild to moderate hearing loss in adults (Review) . Cochrane Database of Systematic Review, 9. 10.1002/14651858.CD012023.pub2.www.cochranelibrary.com [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B. (2015). A review and analysis of the use of ‘habit’ in understanding, predicting and influencing health-related behaviour. Health Psychology Review, 9(3), 277–295. 10.1080/17437199.2013.876238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner B., Abraham C., Lally P., de Bruijin G.-J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. International Journal of Behavioral Nutrition and Physical Activity, 9, 102. 10.1186/1479-5868-9-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatehouse S. (1999). Glasgow Hearing Aid Benefit Profile: Derivation and validation of a client-centered outcome measure for hearing aid services. Journal of the American Academy of Audiology, 10, 80–103. [Google Scholar]
- Grenness C., Hickson L., Laplante-Lévesque A., Meyer C., Davidson B. (2015). The nature of communication throughout diagnosis and management planning in initial audiologic rehabilitation consultations. Journal of the American Academy of Audiology, 26(1), 36–50. 10.3766/jaaa.26.1.5 [DOI] [PubMed] [Google Scholar]
- Hartley D., Rochtchina E., Newall P., Golding M., Mitchell P. (2010). Use of hearing aids and assistive listening devices in an older Australian population. Journal of the American Academy of Audiology, 21(10), 642–653. 10.3766/jaaa.21.10.4 [DOI] [PubMed] [Google Scholar]
- Hougaard S., Ruf S. (2011). EuroTrak 1: A consumer survey about hearing aids in Germany, France, and the UK. Hearing Review, 18, 12–28. [Google Scholar]
- Humes L. E., Wilson D. L., Barlow N. N., Garner C. B., Amos N. (2002). Longitudinal changes in hearing aid satisfaction and usage in the elderly over a period of one or two years after hearing aid delivery. Ear and Hearing, 23(5), 428–438. 10.1097/01.AUD.0000034780.45231.4B [DOI] [PubMed] [Google Scholar]
- Ismail A. H., Munro K. J., Armitage C. J., Dawes P. D. (2019). What do hearing healthcare professionals do to promote hearing aid use and benefit among adults? A systematic review. International Journal of Audiology, 58(2), 63–76. 10.1080/14992027.2018.1531154 [DOI] [PubMed] [Google Scholar]
- Laplante-lévesque A., Jensen L. D., Dawes P., Nielsen C. (2013). Optimal hearing aid use: Focus groups with hearing aid clients and audiologists. Ear and Hearing, 34, 193–202. doi: 10.1097/AUD.0b013e31826a8ecd. [DOI] [PubMed] [Google Scholar]
- Lupsakko T. A., Kautiainen H. J., Sulkava R. (2005). The non-use of hearing aids in people aged 75 years and over in the city of Kuopio in Finland. European Archives of Oto-Rhino-Laryngology, 262(3), 165–169. 10.1007/s00405-004-0789-x [DOI] [PubMed] [Google Scholar]
- Michie S., Atkins L., West R. (2014). The behaviour change wheel: A guide to designing interventions. Silverback. [Google Scholar]
- Michie S., Richardson M., Johnston M., Abraham C., Francis J., Hardeman W., Eccles, M. P., Cane, J., & Wood C. E. (2013). The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine, 46(1), 81–95. 10.1007/s12160-013-9486-6 [DOI] [PubMed] [Google Scholar]
- Michie S., West R., Sheals K., Godinho C. A. (2018). Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Translational Behavioral Medicine, 8(2), 212–224. 10.1093/tbm/ibx019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez E., Edmonds B. A. (2012). A systematic review of studies measuring and reporting hearing aid usage in older adults since 1999: A descriptive summary of measurement tools. PLoS One, 7(3), 1–8. 10.1371/journal.pone.0031831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pryce H., Hall A., Laplante-Lévesque A., Clark E. (2016). A qualitative investigation of decision making during help-seeking for adult hearing loss. International Journal of Audiology, 55(11), 658–665. 10.1080/14992027.2016.1202455 [DOI] [PubMed] [Google Scholar]
- Reese J. L., Hnath-Chisolm T. (2005). Recognition of hearing aid orientation content by first-time users. American Journal of Audiology, 14(1), 94–104. 10.1044/1059-0889(2005/009) [DOI] [PubMed] [Google Scholar]
- Sawyer C. S., Munro K. J., Dawes P., O’Driscoll M. P., Armitage C. J. (2019). Beyond motivation: Identifying targets for intervention to increase hearing aid use in adults. International Journal of Audiology, 58(1), 53–58. 10.1080/14992027.2018.1534007 [DOI] [PubMed] [Google Scholar]
- Scarinci N., Worrall L., Hickson L. (2008). The effect of hearing impairment in older people on the spouse. International Journal of Audiology, 47(3), 141–151. 10.1080/14992020701689696 [DOI] [PubMed] [Google Scholar]
- Sniehotta F. F., Nagy G., Scholz U., Schwarzer R. (2006). The role of action control in implementing intentions during the first weeks of behaviour change. British Journal of Social Psychology, 45(1), 87–106. 10.1348/014466605X62460 [DOI] [PubMed] [Google Scholar]
- Sniehotta F. F., Scholz U., Schwarzer R., Fuhrmann B., Kiwus U., Völler H. (2005). Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine, 12(4), 244–255. [DOI] [PubMed] [Google Scholar]
- Solheim J., Gay C., Hickson L. (2018). Older adults’ experiences and issues with hearing aids in the first six months after hearing aid fitting. International Journal of Audiology, 57(1), 31–39. 10.1080/14992027.2017.1380849 [DOI] [PubMed] [Google Scholar]
- Solheim J., Hickson L. (2017). Hearing aid use in the elderly as measured by datalogging and self-report. International Journal of Audiology, 56(7), 472–479. 10.1080/14992027.2017.1303201 [DOI] [PubMed] [Google Scholar]
- Vas V., Akeroyd M. A., Hall D. A. (2017). A data-driven synthesis of research evidence for domains of hearing loss, as reported by adults with hearing loss and their communication partners. Trends in Hearing, 21, 1–25. 10.1177/2331216517734088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventry I. M., Weinstein B. E. (1983). Identification of elderly people with hearing problems. ASHA, 25(7), 37–42. [PubMed] [Google Scholar]
- Zolnierek K. B. P., DiMatteo R. P. (2009). Physician communication and patient adherence to treatment. Medical Care, 47(8), 826–834. 10.1097/MLR.0b013e31819a5acc [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-tia-10.1177_2331216520969472 for A Quasi-Randomized Controlled Trial of the I-PLAN Intervention to Promote Hearing Aid Use Among First-Time Adult Hearing Aid Users by Afzarini H. Ismail, Kevin J. Munro, Christopher J. Armitage, Antonia Marsden and Piers D. Dawes in Trends in Hearing