Abstract
Backgroud
Osteoarthritis (OA) of the hip and knee is a degenerative disease with complications, including reduced range of motion and pain. Although OA of the hip and knee is common, there are few studies that investigated if patients with this condition had affected morphological truncal parameters. The objectives of this study were to compare the morphology of the spine and the pelvis of patients with hip or knee OA to that of a control group (CG) and to comment on the proposed mechanisms of these changes and the clinical effects on patients.
Methods
This study included three groups of individuals. The first group consisted of 34 patients (15 men and 19 women with a mean age of 67.62 ± 8.28 years) suffering from hip OA. The second group consisted of 45 patients (11 men and 34 women with a mean age of 72.47 ± 7.0 years) suffering from knee OA. These patients were compared with a CG, which consisted of 25 individuals (13 men and 12 women with a mean age of 69.28 ± 10.11 years). The DIERS formetric 4D analysis system was used to calculate several truncal parameters in all planes. All analyses were accomplished using the SPSS ver. 17.0, and p < 0.05 was used to determine statistical significance.
Results
Patients with hip OA presented with significantly increased values than those in the CG for sagittal imbalance, scoliosis angle, vertebral rotation, trunk torsion, and pelvic obliquity, and decreased values than those in the CG for fleche lombaire. Patients with knee OA presented with significantly increased values than those in the CG for sagittal imbalance, apical deviation, scoliosis angle, vertebral rotation, trunk torsion, and pelvic obliquity. Patients with hip or knee OA, compared to the CG, had greater forward inclination of the spine, greater scoliosis, greater vertebral rotation and trunk torsion, and greater obliquity of the pelvis at the frontal plane.
Conclusions
Patients with severe hip or knee OA could have truncal morphology alterations, in addition to reduced hip or knee range of motion and pain. These alterations could cause significant negative effects, which may then seriously affect the patients' quality of life.
Keywords: Truncal changes, Hip osteoarthritis, Knee osteoarthritis, Surface topography
The hip and knee joints are often affected by osteoarthritis (OA), which leads to significant pain and disability causing severe negative effects on patients. The incidence of radiographic hip OA in the USA was estimated to be 28% of the African-American and Caucasian-White population aged > 45 years, while 10% of these patients had symptomatic hip OA.1) A study revealed that radiographic hip OA in those aged > 50 years was 19.6%, while clinical hip OA was 4.2%. Men had a higher incidence of radiologic hip OA than did women, but men did not have a higher incidence of clinical hip OA.2)
The incidence of radiographic knee OA in the USA was estimated to be 28% of the African-American and Caucasian-White population aged > 45 years, while 16% of these patients had symptomatic knee OA.3) A study from Sweden revealed that radiographic knee OA in the population aged > 70 years was 25.4%, while clinical knee OA was 15.4%.4) It is well documented in the literature that patients with severe symptomatic hip or knee OA experience substantial pain and stiffness. These are difficult conditions for the elderly, especially because of mobility deficits, loss of independence and autonomy, and the resulting increased use of health services. However, it is not yet clear if patients with hip or knee OA have affected morphological parameters of the spine and pelvis and what the possible clinical impacts may be.
The objectives of this study were to compare the morphology of the spine and pelvis of patients with hip or knee OA with that of a control group (CG) and to comment on the proposed mechanisms of these changes and consider what the clinical effects may be on the patients.
METHODS
This study recruited three groups of individuals: patients with hip OA only, patients with knee OA only, and a third group comprising healthy individuals. The study was approved by Institutional Review Board of Athens University Medical School (IRB No. EBΔ390/9-9-14), and written informed consent was obtained from the all participating patients. Patients diagnosed as having radiographic evidence of severe unilateral hip or knee OA (Kellgren and Lawrence grade 3 or 4) were admitted to the study and assessed for inclusion. The following exclusion criteria were applied: (1) marked OA in other joints of the lower extremities, (2) arthritis secondary to other diseases, (3) neurological deficits in lower extremities, (4) history of surgical intervention in the spine or lower extremities, and (5) other diseases that would affect the alignment of the trunk. The following inclusion criteria of the CG were applied: (1) without OA in the joints of lower extremities, (2) without neurological deficits in lower extremities, (3) without history of surgical intervention in the spine or lower extremities, and (4) without other diseases that would affect the alignment of the trunk. The DIERS formetric 4D analysis system was used to calculate parameters of the trunk in all planes.
Patients with Hip OA
In total, 34 patients, 15 men and 19 women with a mean age of 67.62 ± 8.28 years (range, 47–84 years), were assessed. The mean weight of patients in this group was 82.32 ± 17.73 kg, mean height was 165.79 ± 8.80 cm, and mean body mass index (BMI) was 29.72 ± 4.31 kg/m2.
Patients with Knee OA
In total, 45 patients, 11 men and 34 women with a mean age of 72.47 ± 7.0 years (range, 5–90 years), were assessed. The mean weight of patients in this group was 79.87 ± 13.79 kg, mean height was 162.16 ± 5.89 cm, and mean BMI was 30.36 ± 4.49 kg/m2.
Control Group
This group consisted of 25 individuals, 13 men and 12 women with a mean age of 69.28 ± 10.11 years (range, 55–86 years). The mean weight of CG participants was 79.40 ± 13.08 kg, mean height was 165.04 ± 9.46 cm, and mean BMI was 29.00 ± 3.00 kg/m2.
The Apparatus and Studied Parameters
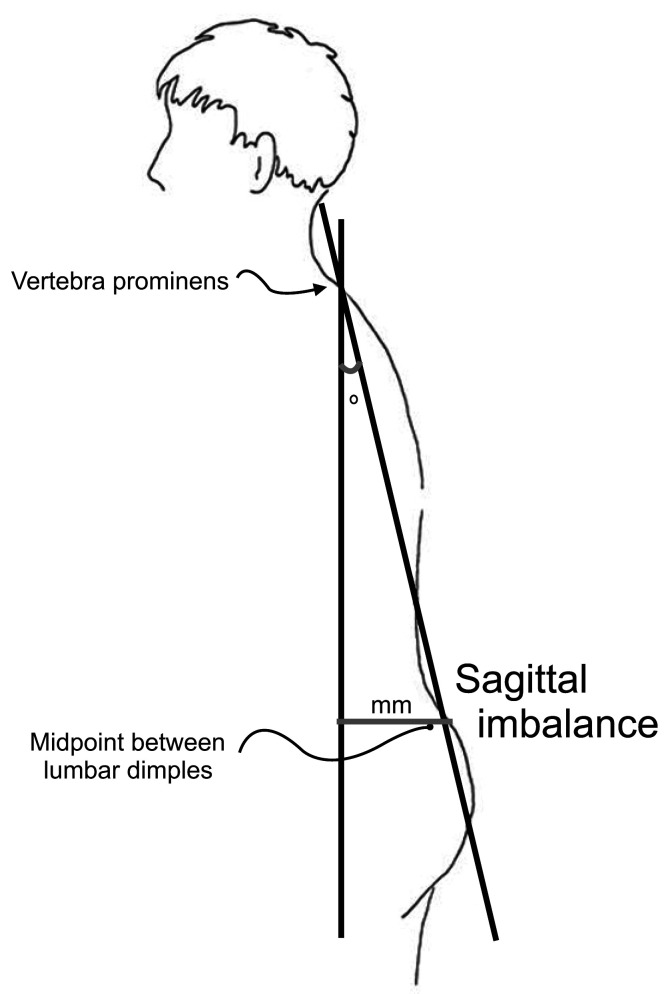
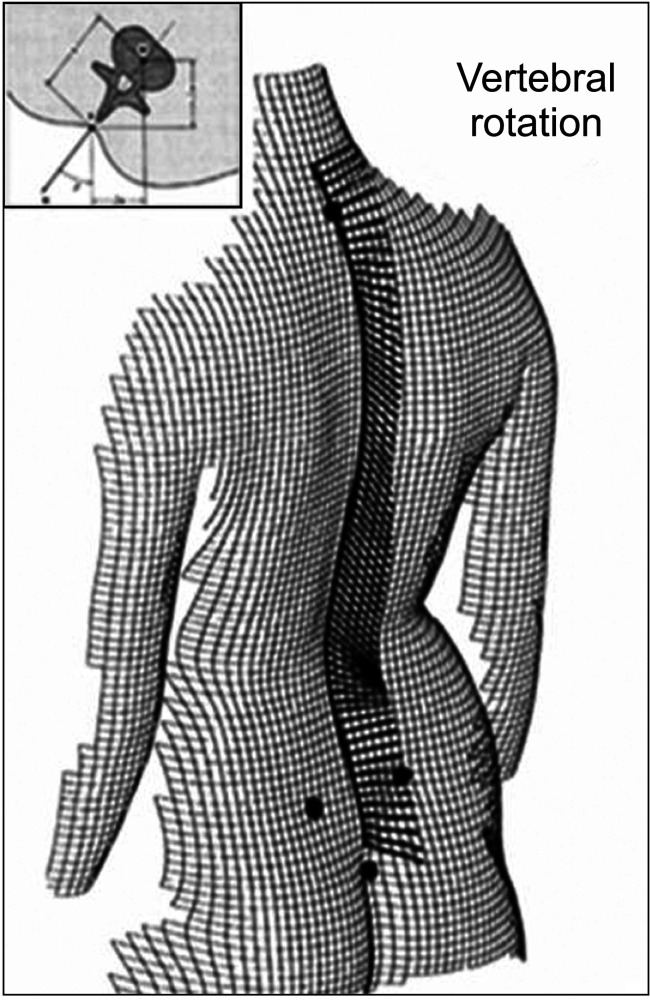
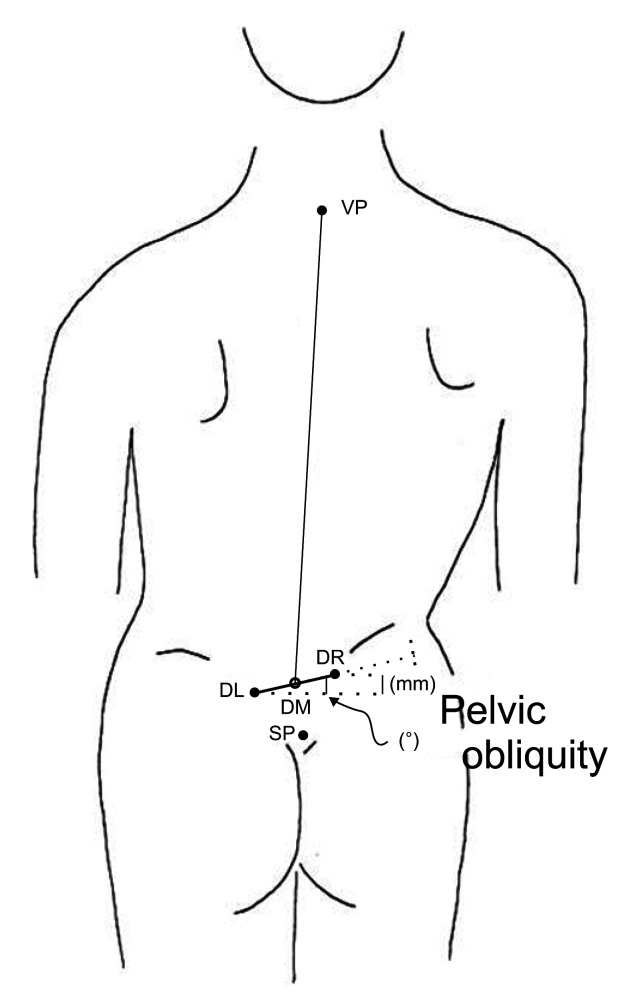
The DIERS formetric 4D analysis system was used for recording the parameters of interest. This device is a surface topography instrument that does not expose subjects to radiation.5,6) The final result is a high resolution three-dimensional back shape reconstruction. The following parameters were assessed in the spine: (1) sagittal plane: the fleche cervicale (the horizontal spatial distance from the kyphotic apex to the cervical apex), the fleche lombaire (the horizontal spatial distance from the kyphotic apex to the lordotic apex), the kyphotic angle, the lordotic angle, and the sagittal imbalance; (2) coronal plane: the coronal imbalance, the apical deviation, and the scoliosis angle; and (3) transverse plane: the vertebral rotation and the trunk torsion. The following parameters were assessed in the pelvis: (1) sagittal plane: the pelvic inclination and the pelvic torsion; (2) coronal plane: the pelvic obliquity; and (3) transverse plane: the pelvis rotation.
Statistical Analysis
Statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) and statistical significance was set at p < 0.05. An independent samples t-test or Mann-Whitney U-test was carried out as appropriate, based on the distribution of the data for comparisons between the CG and the OA groups. The t-test and chi-square test were used to assess homogeneity of the compared groups. Power analysis was used to determine sample size of OA patients and CG.
RESULTS
Hip OA
The demographic characteristic comparisons between the CG and the patients with hip OA are described in Table 1. No statistically significant differences were noted between the CG and patients with hip OA across demographic variables, including age (p = 0.540), sex (p = 0.605), weight (p = 0.371), height (p = 0.754), and BMI (p = 0.482).
Table 1. Homogeneity of Demographic Characteristics between the Control Group and Patients with Hip Osteoarthritis.
| Variable | Control group (n = 25) | Patient group (n = 34) | p-value |
|---|---|---|---|
| Age (yr) | 69.28 ± 10.11 | 67.62 ± 8.28 | 0.540 |
| Sex (male : female) | 13 (52) : 12 (48) | 15 (44) : 19 (56) | 0.605 |
| Weight (kg) | 79.40 ± 13.08 | 82.32 ± 17.73 | 0.371 |
| Height (cm) | 165.04 ± 9.46 | 165.79 ± 8.80 | 0.754 |
| Body mass index (kg/m2) | 29.00 ± 3.00 | 29.72 ± 4.31 | 0.482 |
| Operated leg (right : left) | - | 20 (58.8) : 14 (41.2) | - |
Values are presented as mean ± standard deviation or number (%).
Comparisons between the CG and patients with hip OA are summarized in Tables 2 and 3. Patients with hip OA presented with significantly increased values compared with those in the CG for sagittal imbalance (8.57° vs. 4.19°, p < 0.001; 65.09 vs. 32.88 mm, p = 0.001), scoliosis angle (16.50° vs. 12.96°, p = 0.025), vertebral rotation root mean square (RMS or mean value; 5.29° vs. 3.98°, p = 0.027), vertebral rotation amplitude (11.97° vs. 9.64°, p = 0.020), vertebral rotation max (9.71° vs. 7.80°, p = 0.020), trunk torsion (7.88° vs. 4.16°, p = 0.026), pelvic obliquity (4.26° vs. 0.96°, p < 0.001), and pelvic obliquity (5.91 vs. 1.34 mm, p < 0.001) and a decreased value compared with that in the CG for fleche lombaire (26.40 vs. 39.41 mm, p = 0.004) (Figs. 1, 2, 3, 4, 5, 6).
Table 2. Comparison between the Control Group and Patients with Hip Osteoarthritis.
| Variable | Control group | Patient group |
|---|---|---|
| Fleche cervicale (mm) | 79.02 ± 18.71 | 91.16 ± 29.34 |
| Fleche lombaire (mm) | 39.41 ± 11.89 | 26.40 ± 19.29 |
| Kyphotic angle (°) | 56.18 ± 9.37 | 58.40 ± 12.45 |
| Lordotic angle (°) | 42.26 ± 9.13 | 46.43 ± 11.15 |
| Sagittal imbalance (°) | 4.19 ± 2.83 | 8.57 ± 5.22 |
| Sagittal imbalance (mm) | 32.88 ± 21.42 | 65.09 ± 41.29 |
| Coronal imbalance (°) | 1.16 ± 0.69 | 1.29 ± 0.94 |
| Coronal imbalance (mm) | 8.90 ± 5.01 | 9.27 ± 6.68 |
| Apical deviation RMS (mm) | 4.94 ± 1.81 | 6.22 ± 4.00 |
| Apical deviation amplitude (mm) | 11.40 ± 3.89 | 13.71 ± 5.94 |
| Apical deviation max (mm) | 9.20 ± 3.62 | 11.00 ± 5.96 |
| Scoliosis angle (°) | 12.96 ± 4.45 | 16.50 ± 6.69 |
| Vertebral rotation RMS (°) | 3.98 ± 1.65 | 5.29 ± 2.52 |
| Vertebral rotation amplitude (°) | 9.64 ± 2.84 | 11.97 ± 4.23 |
| Vertebral rotation max (°) | 7.80 ± 2.42 | 9.71 ± 3.38 |
| Trunk torsion (°) | 4.16 ± 3.82 | 7.88 ± 7.43 |
| Pelvic inclination symmetry line (°) | 19.04 ± 8.97 | 23.00 ± 10.49 |
| Pelvic inclination dimples (°) | 17.44 ± 8.32 | 18.94 ± 7.82 |
| Pelvic torsion (°) | 2.64 ± 1.50 | 3.18 ± 1.64 |
| Pelvic obliquity (°) | 0.96 ± 1.10 | 4.26 ± 3.69 |
| Pelvic obliquity (mm) | 1.34 ± 1.68 | 5.91 ± 4.74 |
| Pelvis rotation (°) | 2.08 ± 2.48 | 3.71 ± 3.88 |
Values are presented as mean ± standard deviation.
RMS: root mean square.
Table 3. Comparison between the Control Group and Patients with Hip Osteoarthritis.
| Variable | Mean | 95% CI | p-value |
|---|---|---|---|
| Fleche cervicale (mm) | –12.15 | –25.55 to 1.26 | 0.075 |
| Fleche lombaire (mm) | 13.01 | 4.26 to 21.76 | 0.004 |
| Kyphotic angle (°) | –2.22 | –8.16 to 3.72 | 0.458 |
| Lordotic angle (°) | –4.18 | –9.64 to 1.28 | 0.131 |
| Sagittal imbalance (°) | –4.38 | –6.68 to –2.07 | < 0.001 |
| Sagittal imbalance (mm) | –32.21 | –50.34 to –14.09 | 0.001 |
| Coronal imbalance (°) | –0.13 | –0.58 to 0.31 | 0.548 |
| Coronal imbalance (mm) | –0.37 | –3.55 to 2.81 | 0.816 |
| Apical deviation RMS (mm) | –1.28 | –3.00 to 0.44 | 0.141 |
| Apical deviation amplitude (mm) | –2.31 | –5.04 to 0.42 | 0.096 |
| Apical deviation max (mm) | –1.80 | –4.50 to 0.90 | 0.186 |
| Scoliosis angle (°) | –3.54 | –6.63 to –0.45 | 0.025 |
| Vertebral rotation RMS (°) | –1.32 | –2.48 to –0.16 | 0.027 |
| Vertebral rotation amplitude (°) | –2.33 | –4.29 to –0.37 | 0.020 |
| Vertebral rotation max (°) | –1.91 | –3.49 to –0.32 | 0.020 |
| Trunk torsion (°) | –3.72 | –6.98 to –0.47 | 0.026 |
| Pelvic inclination symmetry line (°) | –3.96 | –9.17 to 1.25 | 0.134 |
| Pelvic inclination dimples (°) | –1.50 | –5.74 to 2.74 | 0.481 |
| Pelvic torsion (°) | –0.54 | –1.37 to 0.30 | 0.203 |
| Pelvic obliquity (°) | –3.30 | –4.83 to –1.78 | < 0.001 |
| Pelvic obliquity (mm) | –4.57 | –6.56 to –2.58 | < 0.001 |
| Pelvis rotation (°) | –1.63 | –3.40 to 0.15 | 0.072 |
CI: confidence interval, RMS: root mean square.
Fig. 1. Illustration of fleche cervicale and fleche lombaire. With permission of manual of DIERS.7).
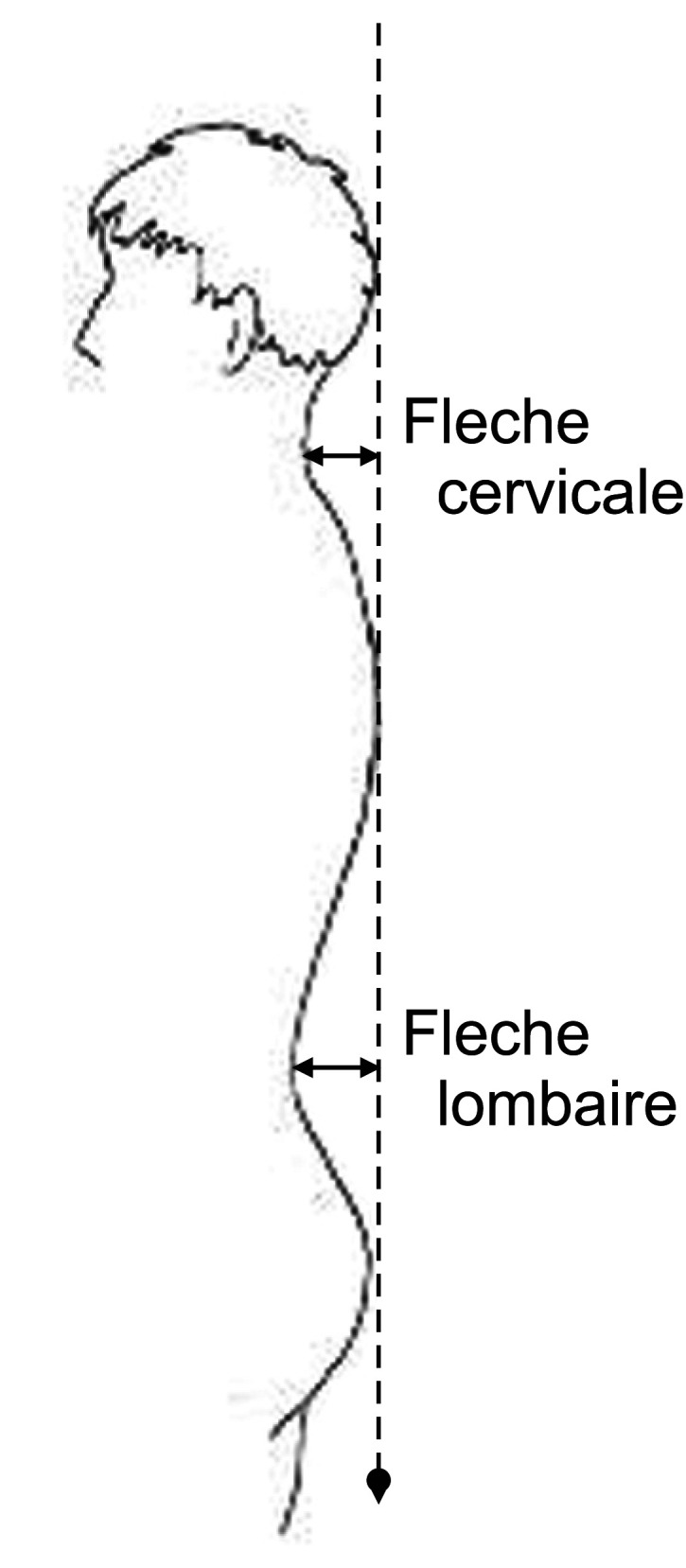
Fig. 2. Illustration of sagittal imbalance. With permission of manual of DIERS.7).
Fig. 3. Illustration of apical deviation. VP: vertebra prominens, RMS: root mean square, amp: amplitude. With permission of manual of DIERS.7).
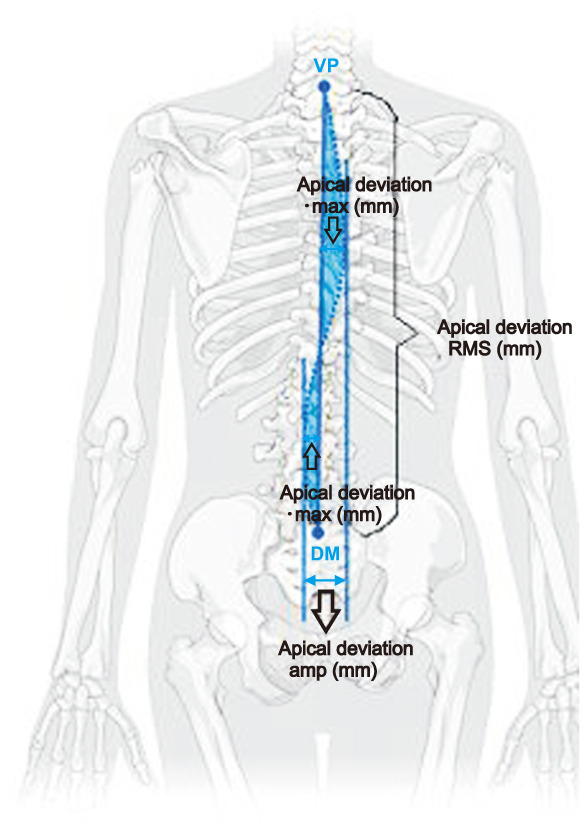
Fig. 4. Illustration of the scoliosis angle. With permission of manual of DIERS.7).
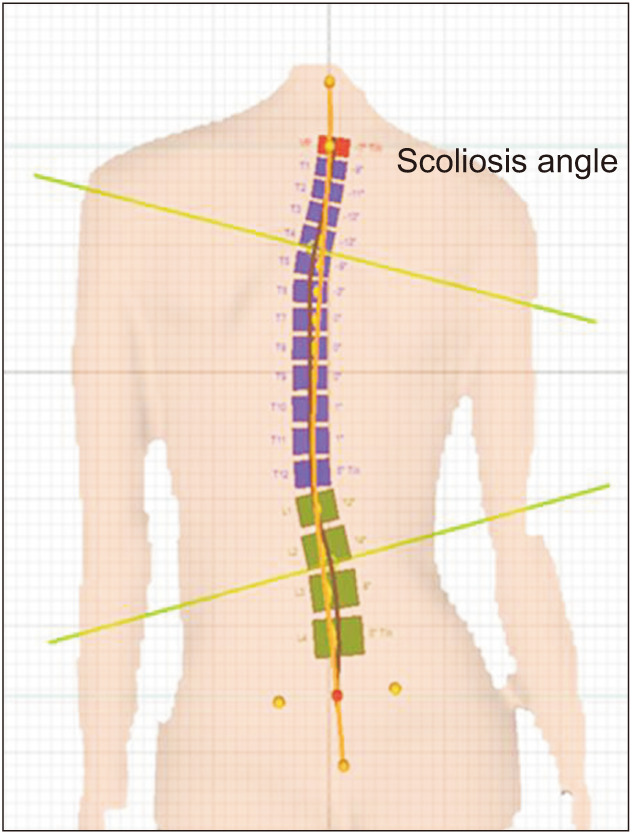
Fig. 5. Illustration of vertebral rotation. With permission of manual of DIERS.7).
In other words, the patients with hip OA, when compared to the CG, had a greater forward inclination of the spine, increased scoliosis, more vertebral rotation and trunk torsion, and greater obliquity of the pelvis in the frontal plane.
Knee OA
The demographic characteristic comparisons between the CG and the patients with knee OA are described in Table 4. No statistically significant differences were noted between the CG and patients with knee OA for all demographic variables, including age (p = 0.175), weight (p = 0.891), height (p = 0.176), and BMI (p = 0.136), except sex (p = 0.034, there were more women than men in the patients with knee OA).
Table 4. Homogeneity of Demographic Characteristics between the Control Group and Patients with Knee Osteoarthritis.
| Variable | Control group (n = 25) | Patient group (n = 45) | p-value |
|---|---|---|---|
| Age (yr) | 69.28 ± 10.11 | 72.47 ± 7.00 | 0.175 |
| Sex (male : female) | 13 (52) : 12 (48) | 11 (24.4) : 34 (75.6) | 0.034 |
| Weight (kg) | 79.40 ± 13.08 | 79.87 ± 13.79 | 0.891 |
| Height (cm) | 165.04 ± 9.46 | 162.16 ± 5.89 | 0.176 |
| Body mass index (kg/m2) | 29.00 ± 3.00 | 30.36 ± 4.49 | 0.136 |
| Operated leg (right : left) | - | 20 (44.4) : 25 (55.6) | - |
Values are presented as mean ± standard deviation or number (%).
Comparisons between the CG and the patients with knee OA are summarized in Tables 5 and 6. Patients with knee OA presented with significantly increased values compared with those in the CG for sagittal imbalance (6.89° vs. 4.19°, p = 0.012; 50.50 vs. 32.88 mm, p = 0.026), apical deviation RMS (7.03° vs. 4.94°, p = 0.014), apical deviation max (12.02 vs. 9.20 mm, p = 0.037), scoliosis angle (17.62° vs. 12.96°, p = 0.002), vertebral rotation amplitude (12.22° vs. 9.64°, p = 0.031), trunk torsion (6.96° vs. 4.16°, p = 0.044), pelvic obliquity (3.27° vs. 0.96°, p < 0.001), and pelvic obliquity (4.63 vs. 1.34 mm, p < 0.001) (Figs. 1, 2, 3, 4, 5, 6).
Table 5. Comparison between the Control Group and Patients with Knee Osteoarthritis.
| Variable | Control group | Patient group |
|---|---|---|
| Fleche cervicale (mm) | 79.02 ± 18.71 | 83.50 ± 24.56 |
| Fleche lombaire (mm) | 39.41 ± 11.89 | 32.35 ± 18.12 |
| Kyphotic angle (°) | 56.18 ± 9.37 | 61.12 ± 13.20 |
| Lordotic angle (°) | 42.26 ± 9.13 | 48.42 ± 16.30 |
| Sagittal imbalance (°) | 4.19 ± 2.83 | 6.89 ± 4.75 |
| Sagittal imbalance (mm) | 32.88 ± 21.42 | 50.50 ± 35.27 |
| Coronal imbalance (°) | 1.16 ± 0.69 | 1.24 ± 1.15 |
| Coronal imbalance (mm) | 8.90 ± 5.01 | 9.05 ± 7.70 |
| Apical deviation RMS (mm) | 4.94 ± 1.81 | 7.03 ± 3.91 |
| Apical deviation amplitude (mm) | 11.40 ± 3.89 | 14.04 ± 6.13 |
| Apical deviation max (mm) | 9.20 ± 3.62 | 12.02 ± 6.07 |
| Scoliosis angle (°) | 12.96 ± 4.45 | 17.62 ± 6.34 |
| Vertebral rotation RMS (°) | 3.98 ± 1.65 | 4.94 ± 2.59 |
| Vertebral rotation amplitude (°) | 9.64 ± 2.84 | 12.22 ± 5.44 |
| Vertebral rotation max (°) | 7.80 ± 2.42 | 9.27 ± 4.22 |
| Trunk torsion (°) | 4.16 ± 3.82 | 6.96 ± 6.18 |
| Pelvic inclination symmetry line (°) | 19.04 ± 8.97 | 24.84 ± 16.59 |
| Pelvic inclination dimples (°) | 17.44 ± 8.32 | 20.29 ± 12.19 |
| Pelvic torsion (°) | 2.64 ± 1.50 | 2.64 ± 2.24 |
| Pelvic obliquity (°) | 0.96 ± 1.10 | 3.27 ± 2.71 |
| Pelvic obliquity (mm) | 1.34 ± 1.68 | 4.63 ± 3.77 |
| Pelvis rotation (°) | 2.08 ± 2.48 | 3.04 ± 4.29 |
Values are presented as mean ± standard deviation.
RMS: root mean square.
Table 6. Comparison between the Control Group and Patients with Knee Osteoarthritis.
| Variable | Mean | 95% CI | p-value |
|---|---|---|---|
| Fleche cervicale (mm) | –4.48 | –15.77 to 6.80 | 0.430 |
| Fleche lombaire (mm) | 7.06 | –1.01 to 15.12 | 0.085 |
| Kyphotic angle (°) | –4.94 | –10.91 to 1.02 | 0.103 |
| Lordotic angle (°) | –6.17 | –13.23 to 0.90 | 0.086 |
| Sagittal imbalance (°) | –2.70 | –4.78 to –0.62 | 0.012 |
| Sagittal imbalance (mm) | –17.62 | –33.09 to –2.14 | 0.026 |
| Coronal imbalance (°) | –0.08 | –0.59 to 0.42 | 0.739 |
| Coronal imbalance (mm) | –0.15 | –3.57 to 3.27 | 0.930 |
| Apical deviation RMS (mm) | –2.09 | –3.74 to –0.43 | 0.014 |
| Apical deviation amplitude (mm) | –2.64 | –5.36 to 0.07 | 0.056 |
| Apical deviation max (mm) | –2.82 | –5.48 to –0.17 | 0.037 |
| Scoliosis angle (°) | –4.66 | –7.52 to –1.80 | 0.002 |
| Vertebral rotation RMS (°) | –0.96 | –2.10 to 0.19 | 0.109 |
| Vertebral rotation amplitude (°) | –2.58 | –4.91 to –0.25 | 0.031 |
| Vertebral rotation max (°) | –1.47 | –3.30 to 0.37 | 0.115 |
| Trunk torsion (°) | –2.80 | –5.51 to –0.08 | 0.044 |
| Pelvic inclination symmetry line (°) | –5.80 | –12.96 to 1.35 | 0.110 |
| Pelvic inclination dimples (°) | –2.85 | –8.31 to 2.62 | 0.302 |
| Pelvic torsion (°) | 0.00 | –1.00 to 0.99 | 0.993 |
| Pelvic obliquity (°) | –2.31 | –3.44 to –1.17 | < 0.001 |
| Pelvic obliquity (mm) | –3.28 | –4.87 to –1.69 | < 0.001 |
| Pelvis rotation (°) | –0.96 | –2.83 to 0.90 | 0.306 |
CI: confidence interval, RMS: root mean square.
Fig. 6. Illustration of pelvic obliquity. VP: vertebra prominens, DR: dimple right, DL: dimple left, DM: dimple middle, SP: sacrum point. With permission of manual of DIERS.7).
In other words, the patients with knee OA, when compared to the CG, had a greater forward inclination of the spine, increased scoliosis and apical deviation, more vertebral rotation and trunk torsion, and greater obliquity of the pelvis in the frontal plane.
DISCUSSION
Hip OA
There are several studies on truncal changes in patients with severe hip OA. Weng et al.8) described that digital lateral radiographs of patients with hip OA, compared to those of asymptomatic controls, showed (1) more forward inclination of the spine in the sagittal plane, (2) greater incidence of unbalanced spinal-pelvic alignment, and (3) more anteversion of the pelvis in the sagittal plane. The compensatory mechanisms for the flexed hip joint with OA were femoral retroversion and forward inclination of the spine and pelvis. The study by Bendaya et al.9) in patients with hip OA showed that the sacral slope was higher in comparison to that of their CG, indicating that there was a greater anterior pelvic tilt in the sagittal plane. The study by Raphael et al.10) showed that patients with hip OA showed no differences in pelvic incidence when compared to the pelvic incidence in a healthy participant sample. Radcliff et al.11) showed that patients with hip OA had a higher sacral slope than a group of patients with symptomatic degenerative disease of the lumbar spine. Yoshimoto et al.12) showed that patients with hip OA had increased values for pelvic incidence, lordotic angle of the spine, pelvic obliquity in the frontal plane, and anterior pelvic tilt when compared to those of patients with low back pain. The finding of Weng et al.8) of forward inclination of the spine and the finding of Yoshimoto et al.12) of increased pelvic obliquity in the frontal plane coincide with the results of this study.
An explanation of the changes in the spine and pelvis in patients with hip OA, as revealed in this study, will follow. It is known that the hip with OA is initially flexed due to pain, osteophytes, and contracture of the articular capsule. Flexion may also occur due to subluxation of the femoral head from the acetabulum in OA. The first compensatory mechanism is anterior pelvic inclination in the sagittal plane in order to reduce pain and improve coverage of the femoral head. The second compensatory mechanism is the increased lordotic angle of the spine so that the “C7 plumb line” remains over the sacral endplate and normal balance of the human body is preserved.8,12,13) However, in elderly patients with hip OA and a stiff spine, this mechanism is not sufficient, resulting in forward inclination of the spine and sagittal imbalance.8) In this study, the finding of forward inclination of the spine and statistically insignificantly increased lordotic angle of the spine and the anterior pelvic tilt are justified when considered in light of this context.
The findings of greater scoliosis of the spine and greater obliquity of the pelvis in the frontal plane in the patients with hip OA could be explained by the occurrence of hip flexion and the coxa valga or, more typically, coxa vara deformity of the hip with OA. These maladaptations cause functional leg length inequality that may result in greater pelvic obliquity and functional scoliosis in the frontal plane as a compensatory mechanism, as revealed in this study and other orthopedic studies.14,15,16)
The findings of greater vertebral rotation and trunk torsion in patients with hip OA are, to our knowledge, published here for the first time. A mechanism to explain these findings may be that the deficiency of complete internal and external rotation of the hip can cause changes in the trunk in the transverse plane. In this study, we found a similar finding of greater pelvic rotation in patients with hip OA, although not statistically significant, when compared to that in the CG.
It should be added that a general proposed mechanism for truncal changes in patients with hip OA is the limitation of motion at the hip joint. In severe OA, the hip joint can be observed in a flexed, externally rotated, and adducted position. It is worth noting that patients with hip OA often have balance disorders, gait abnormalities, and decreased strength of muscles controlling the knee.17,18) Consequently, the abnormal new position and kinematics of the affected hip can cause an unbalanced upright posture with effects on the morphology of the spine and the pelvis in all three planes of motion.
Knee OA
There are several studies on truncal changes in patients with severe knee OA. Wang et al.19) described that patients with knee OA had greater forward inclination of the spine, while the hip and knee joints were more flexed than in the CG. Global imbalance was also observed at a higher rate than in the CG. Patients with knee flexion < 10° were characterized by decreased lumbar lordosis and forward inclination of the spine, and when knee flexion was increased, > 10° knee flexion patients had greater forward inclination of the spine and pelvis than the CG. Thus, the progressive compensatory mechanisms have been identified depending on the severity of knee OA in elderly patients. The study by Tauchi et al.20) showed a strong correlation between progressive knee OA and increases in the spinal inclination angle. Lee et al.21) attempted to simulate progressive knee OA and the compaction effects among young patients by positioning them with a specialized femoral splint at 0°, 15°, and 30°. Radiologic examinations were performed on these patients and the results were decreased lumbar lordosis, greater anterior inclination of the spine, and no changes to the pelvis. The study by Murata et al.22) revealed that patients with a 5° reduction in knee extension, simulating knee OA, had reduced lumbar lordosis. The finding of forward inclination of the spine in this study coincides with the findings of Wang et al.,19) Tauchi et al.,20) and Lee et al.21)
An explanation of the changes in the spine and pelvis in patients with knee OA, as revealed in this study, will follow. It is known that the knee with OA is initially flexed due to pain, osteophytes, and contracture of articular capsule. The compensatory mechanism is hip flexion and anterior pelvic inclination in the sagittal plane in order to keep normal sagittal balance. In this study, the finding of forward inclination of the spine was justified when considered in light of the above context. Furthermore, in this study, an anterior pelvic tilt was also observed, which, albeit not statistically significant, contributed to confirming the aforementioned sequence of compensatory mechanisms.
The findings of greater scoliosis, apical deviation of the spine, and greater obliquity of the pelvis could be explained by contracture and varus-valgus deformity of the osteoarthritic knee. These cause functional leg length inequality that may result in truncal changes at the frontal plane as a compensatory mechanism, as revealed from this study and other orthopedic studies.14,15,16)
The findings of greater vertebral rotation and trunk torsion in patients with knee OA are, to our knowledge, published here for first time. The deformity of the osteoarthritic knee joint results in gait differences and hip muscle weakness. Therefore, patients with knee OA have maladaptive kinematic forces and load during posture and gait, resulting in morphological changes not only in the lower extremities but also in the trunk in the sagittal, frontal, and transverse planes.
Clinical Effects
The clinical effects of sagittal imbalance in patients with hip or knee OA can be very significant. Spinal malalignment and the compensatory mechanisms might result in greater muscular effort and energy expenditure in maintaining upright posture and finally extreme muscular demand, fatigue, significant pain, and disability.23) Several studies have described the relationship between spinal imbalance and greater pain, worsening functionality, and decreased satisfaction as measured by the health-related quality of life, Oswestry Disability Index, Scoliosis Research Society, 12-item short form Survey scores.24,25) One more clinical effect of sagittal imbalance is the downward direction of the gaze that could result in greater risk of falls and possible fractures.
In the frontal plane, patients with hip or knee OA had greater scoliosis that could be an aesthetic problem, as well as a cause of functional impairments, such as pain from excessive loading of the zygapophyseal joints and degeneration of the intervertebral discs from asymmetrical loading. The neurologic symptoms could manifest as numbness, loss of sensation, and muscle weakness, especially in the legs.26,27)
Concerning the greater pelvic obliquity in the frontal plane in the patients with hip or knee OA, this finding mainly indicates functional leg length discrepancy. As such, patients with hip or knee OA could have various orthopedic pathologies related to leg length discrepancy, including OA of the lumbar spinal joints, low back pain, knee pain, lower extremity stress fractures, and standing posture, postural balance, gait, and running impairments.28,29) The clinical effects of greater vertebral rotation and trunk torsion in patients with hip or knee OA could manifest as spinal deformation and reduced spinal mobility. The greater vertebral rotation may also cause spinal OA, arthritis of the zygapophyseal joints, and narrowing of the intervertebral foramina. These may then result in pain, tenderness, and neurological symptoms.
There are some limitations to this study. The first is that measurements using the DIERS formetric 4D analysis system were done by one examiner and intraobsever or interobserver reliability could not be calculated. However, measurements from the DIERS formetric 4D analysis system are highly reproducible and comparable to radiography. The second is that the clinical effects were not evaluated for the patients with hip or knee OA of this study. The third is that the number of patients was limited. However, there were statistically significant findings in this study.
The symptoms of hip or knee OA include pain, stiffness, tenderness and loss of flexibility. In this study, patients with severe hip or knee OA were also found to have truncal morphological alterations that could result in significant negative effects. Nevertheless, it is unclear whether a causal relationship exists between spine alignment and hip or knee OA. Further studies on truncal changes in patients after total hip or knee arthroplasty will be valuable and such studies are already in progress in our team.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of hip symptoms and radiographic and symptomatic hip osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2009;36(4):809–815. doi: 10.3899/jrheum.080677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66(11):3013–3017. doi: 10.1002/art.38795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34(1):172–180. [PubMed] [Google Scholar]
- 4.Turkiewicz A, Gerhardsson de Verdier M, Engstrom G, et al. Prevalence of knee pain and knee OA in southern Sweden and the proportion that seeks medical care. Rheumatology (Oxford) 2015;54(5):827–835. doi: 10.1093/rheumatology/keu409. [DOI] [PubMed] [Google Scholar]
- 5.Drerup B, Hierholzer E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin Biomech (Bristol, Avon) 1994;9(1):28–36. doi: 10.1016/0268-0033(94)90055-8. [DOI] [PubMed] [Google Scholar]
- 6.Degenhardt B, Starks Z, Bhatia S, Franklin GA. Appraisal of the DIERS method for calculating postural measurements: an observational study. Scoliosis Spinal Disord. 2017;12:28. doi: 10.1186/s13013-017-0134-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hubner J. Manual of DIERS formetric III 4D. 3rd ed. Schlangenbad: DIERS International; 2010. [Google Scholar]
- 8.Weng WJ, Wang WJ, Wu MD, Xu ZH, Xu LL, Qiu Y. Characteristics of sagittal spine-pelvis-leg alignment in patients with severe hip osteoarthritis. Eur Spine J. 2015;24(6):1228–1236. doi: 10.1007/s00586-014-3700-5. [DOI] [PubMed] [Google Scholar]
- 9.Bendaya S, Lazennec JY, Anglin C, et al. Healthy vs. osteoarthritic hips: a comparison of hip, pelvis and femoral parameters and relationships using the EOS® system. Clin Biomech (Bristol, Avon) 2015;30(2):195–204. doi: 10.1016/j.clinbiomech.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Raphael IJ, Rasouli MR, Kepler CK, Restrepo S, Albert TJ, Radcliff KE. Pelvic incidence in patients with hip osteoarthritis. Arch Bone Jt Surg. 2016;4(2):132–136. [PMC free article] [PubMed] [Google Scholar]
- 11.Radcliff KE, Orozco F, Molby N, et al. Change in spinal alignment after total hip arthroplasty. Orthop Surg. 2013;5(4):261–265. doi: 10.1111/os.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yoshimoto H, Sato S, Masuda T, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 2005;30(14):1650–1657. doi: 10.1097/01.brs.0000169446.69758.fa. [DOI] [PubMed] [Google Scholar]
- 13.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976) 1983;8(3):316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Murray KJ, Azari MF. Leg length discrepancy and osteoarthritis in the knee, hip and lumbar spine. J Can Chiropr Assoc. 2015;59(3):226–237. [PMC free article] [PubMed] [Google Scholar]
- 15.Raczkowski JW, Daniszewska B, Zolynski K. Functional scoliosis caused by leg length discrepancy. Arch Med Sci. 2010;6(3):393–398. doi: 10.5114/aoms.2010.14262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Young RS, Andrew PD, Cummings GS. Effect of simulating leg length inequality on pelvic torsion and trunk mobility. Gait Posture. 2000;11(3):217–223. doi: 10.1016/s0966-6362(00)00048-5. [DOI] [PubMed] [Google Scholar]
- 17.Rasch A, Dalen N, Berg HE. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop. 2010;81(2):183–188. doi: 10.3109/17453671003793204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Majewski M, Bischoff-Ferrari HA, Gruneberg C, Dick W, Allum JH. Improvements in balance after total hip replacement. J Bone Joint Surg Br. 2005;87(10):1337–1343. doi: 10.1302/0301-620X.87B10.16605. [DOI] [PubMed] [Google Scholar]
- 19.Wang WJ, Liu F, Zhu YW, Sun MH, Qiu Y, Weng WJ. Sagittal alignment of the spine-pelvis-lower extremity axis in patients with severe knee osteoarthritis: a radiographic study. Bone Joint Res. 2016;5(5):198–205. doi: 10.1302/2046-3758.55.2000538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tauchi R, Imagama S, Muramoto A, Tsuboi M, Ishiguro N, Hasegawa Y. Influence of spinal imbalance on knee osteoarthritis in community-living elderly adults. Nagoya J Med Sci. 2015;77(3):329–337. [PMC free article] [PubMed] [Google Scholar]
- 21.Lee CS, Park SJ, Chung SS, Lee KH. The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. 2013;22(5):1059–1065. doi: 10.1007/s00586-013-2661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murata Y, Takahashi K, Yamagata M, Hanaoka E, Moriya H. The knee-spine syndrome: association between lumbar lordosis and extension of the knee. J Bone Joint Surg Br. 2003;85(1):95–99. doi: 10.1302/0301-620x.85b1.13389. [DOI] [PubMed] [Google Scholar]
- 23.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35(25):2224–2231. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 24.Hasegawa K, Okamoto M, Hatsushikano S, Shimoda H, Ono M, Watanabe K. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur Spine J. 2016;25(11):3675–3686. doi: 10.1007/s00586-016-4702-2. [DOI] [PubMed] [Google Scholar]
- 25.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 2005;30(18):2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]
- 26.Wong E, Altaf F, Oh LJ, Gray RJ. Adult degenerative lumbar scoliosis. Orthopedics. 2017;40(6):e930–e939. doi: 10.3928/01477447-20170606-02. [DOI] [PubMed] [Google Scholar]
- 27.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 28.Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003;33(5):221–234. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 29.Gurney B. Leg length discrepancy. Gait Posture. 2002;15(2):195–206. doi: 10.1016/s0966-6362(01)00148-5. [DOI] [PubMed] [Google Scholar]