Abstract
BACKGROUND
Phimosis is one of the most common diseases in children. Early selection of appropriate treatment for phimosis in children is beneficial to the development of their reproductive organs and significantly improves the prognosis of phimosis in children. Although traditional circumcision is the most widely used, it has many disadvantages, including postoperative bleeding and incision infection, pain, obvious scars on the surgical incision, and unsatisfactory appearance. In addition, there is much controversy regarding treatment options and timing at home and abroad. Surgical procedures such as circumcision and cerclage for children with excessively long foreskin will greatly affect the normal life of children after the operation. Young children need general anesthesia, but this anesthesia carries a great risk.
AIM
To design a new children phimosis dilatation retractor for children phimosis.
METHODS
The children phimosis was dilated with an elastic dilation frame, in order to expand the foreskin mouth and expose the penis head, and after that, the phimosis was cured.
RESULTS
A new type of phimosis dilatation retractor was designed, which can gently dilate the prepuce at multiple angles and in multiple directions at the same time. It has obtained the national patent for clinical application.
CONCLUSION
The phimosis dilatation retractor based on the principle of elastically expanding the prepuce can achieve the purpose of expanding the phimosis. The clinical application shows that the effect of the children phimosis retractor is significant, which is worth promoting.
Keywords: Dilation, Phimosis, Retractor, Children
Core Tip: This new type of phimosis dilatation retractor can be applied to treat most cases of phimosis in children, and no general anesthetics are required. Compared to other treatments, retractor is easy to operate and inexpensive. Furthermore, good treatment effects can be achieved through gentle and continuous dilation of the foreskin. These characteristics make this retractor suitable for clinical promotion.
INTRODUCTION
Phimosis is a condition in which the foreskin cannot be pulled back from around the tip of a normal-looking penis because the foreskin mouth is too narrow. It can be categorized as born phimosis and acquired phimosis. For born phimosis, non-surgical treatments like partial cleaning and pulling back of foreskin are required and no surgeries are required. If the phimosis of some people suffer from balanoposthitis and foreskin damages, and fiber at the foreskin mouth is contracted, their phimosis will develop into the acquired type. This kind of phimosis needs to be treated by either circumcision or cerclage surgery[1]. Phimosis is one of the most common illnesses among children. Intervening children phimosis through various methods benefits the development of their reproductive organs. Now treatments for intervening children’s phimosis are all twofold, and timely selection of the right therapy method can significantly improve the prognosis of children phimosis. Traditional circumcision, though the most widely used, has many disadvantages, including bleeding and infection of incisions after the operation, pain, obvious scar on surgical incisions, unsatisfactory outlook, and so on[2,3]. For infant and toddler phimosis, there is great controversy surrounding selection and timing of treatments at home and abroad[4]. Some experts believe that only perineum hygiene is required for children within three years old, and children between three and six years old can pull back their foreskin at home by themselves. They also think that foreskin dilation treatments can be performed on children between seven and twelve years old, and circumcision and cerclage surgery for children phimosis can be performed on children over 13 years old. Surgeries like circumcision and cerclage surgeries for children phimosis can greatly affect children's normal life in the post-surgery period. General anesthesia is required for children of young ages, but this kind of anesthesia involves great risks. Besides, healing of operative incisions takes a long time[5]. Therefore, parents resort to treatments that are more suitable for treating children phimosis because post-surgery wound hurts, which is especially true in case of medicine change to the degree where children cannot bear the pain.
In this subject, a children phimosis retractor that has obtained invention and patent licensing in 2018 is invented (Patent No. ZL2017 1 0149501.X). This invention is commissioned to Guangzhou ORCL Medical Co., Ltd for production (Product name: retractor. Product Record No. Yue Sui Apparatus Record No. 20181294).
The usage report of the children phimosis retractor is reported below.
MATERIALS AND METHODS
General documentation
In this study, we selected 87 children cases seeking medical advice from the urology department in the hospital to treat phimosis from January 1, 2019 to January 31, 2019. Their ages ranged from three to eleven years old, with an average value of 7.6. In these cases, 43 cases had glans blistering and the smegma was visible in 63 cases. Pulling back the foreskin of these penises, we can see narrow foreskin mouths and none of the external urethral orifices was properly exposed.
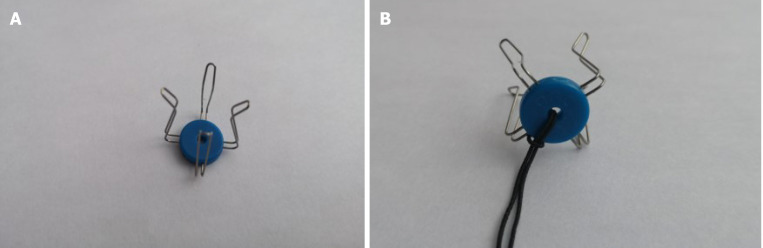
Product structure
The product structure is shown in Figure 1.
Figure 1.
Product structure. A: According to the degree of phimosis, 2-4 directions are chosen to expand; B: Silk thread pastes on the skin to prevent it from falling during activities.
Usage
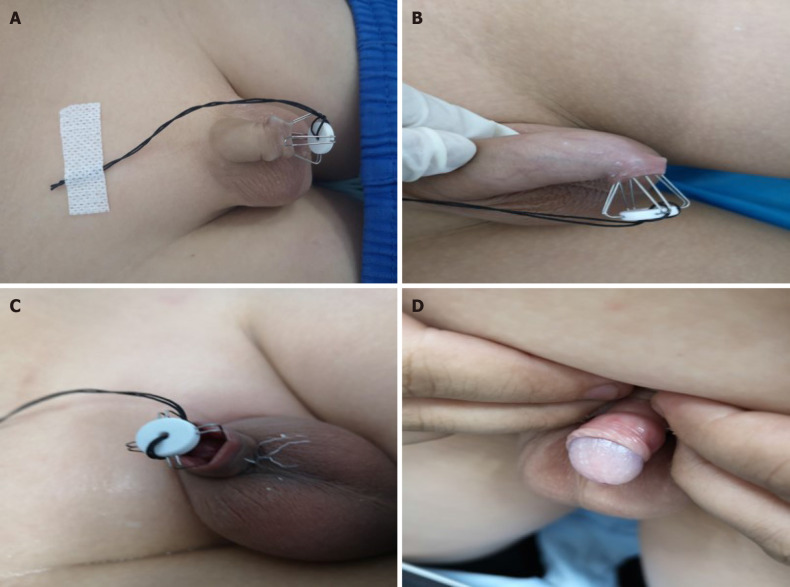
A child suffering from phimosis should be placed in the supine position. First, iodine was used to disinfect the foreskin mouth and then a small amount of lidocaine cream, a kind of skin surface anesthetic, was applied to the disinfected foreskin mouth. Second, one hand was used to pull back the foreskin so that there was tension around the foreskin mouth. Afterwards, the other hand was used to hold the retractor. Third, the two work ends were closed in the opposite direction and the retractor was put into the foreskin mouth to the point that the tips of the two work ends extended over the narrow part of the foreskin mouth. After these steps, the force applied by work ends of the retractor was diluting the foreskin and the retractor would not fall off, as certain amount of tension existed there. If the retractor was prone to fall off after being put into the foreskin mouth, three or four work ends can be selected. All work ends should extend over the narrow part of the foreskin mouth. Children suffering from phimosis should wear the retractor for at least seven to fourteen days, with 1 to 2 h each day. Besides, these children should pull back their foreskins to the point that the corona of glans penis is exposed each day. After these treatments, they should also pull back their foreskins to expose the glans, and clean and then put the penis to its original position, as shown in Figure 2.
Figure 2.
Usage. A: Expansion in two directions; B: Expansion in three directions; C: Expansion in four directions; D: Effect of dilation therapy.
RESULTS
In the 87 cases whose foreskins were dilated, three cases experienced obvious pain, two had preputial edema, and 35 had adherent prepuce 2 wk after the operation. These difficulties were overcome by performing the foreskin dilation and relaxation treatment with lidocaine cream used for superficial anesthesia. None of the cases had red and swollen foreskins or had difficulty urinating after the treatment.
Postoperative follow-up at 1 mo showed all of the 87 cases could fully expose their glans and coronas of glans penises were visible.
DISCUSSION
As the foreskin mouth is narrow, people suffering from phimosis can experience dysuria and thinning of urinary flow, expansion of the foreskin cavity, or a narrow external urethral orifice, and they may experience frequent micturition or urgent micturition if the urinary tract is infected. Usually, a large amount of smegma amassed is on the corona of glans inside the foreskin cavity. Through the foreskin, small white swellings are visible. During acute inflammation, the glans and foreskin are wet, red, and swollen, and purulent secretions are produced[6,7]. Phimosis can cause various physiological hazards to male health, including foreskin and glans inflammation, penile cancer, premature ejaculation, impotence, urinary tract infection, and so on[8]. Phimosis also affects the normal lives of those suffering from it. For men with serious phimosis, even the risk of human immunodeficiency virus infection is increased[9,10].
Both surgical and nonsurgical treatments are available for treating children with phimosis. If newborns found to have phimosis during infancy and toddlerhood have no urinary difficulties and no foreskin infections, they only need to pay attention to penis hygiene, and no treatment is required. If these symptoms do occur, the foreskin can be repeatedly pulled back to dilate the foreskin mouth. By doing so, and with passage of time, most cases of phimosis in children can be cured, and only a small number of children need circumcision or cerclage surgery[11]. Although circumcision is a minor surgery, patients who receive this surgery tend to hold high expectations for it. Therefore, if there are any post-surgery complications, patients will experience both physical and psychological pain[12]. Usually, the post-surgery recovery period is long, and the foreskin after surgery is prone to edema. In addition, the operation time for traditional circumcision is long, and there is much bleeding during surgery. After circumcision, the foreskin is prone to have obvious edema. Furthermore, the length of the frenulum is difficult to control, and the frenulum after surgery tends to be shortened. When the penis becomes erect, the glans will come down[13]. Edema is a common complication after phimosis surgery. In the clinical field, although improvements in medical equipment and technology are both in progress, the mechanism of this complication has yet to be fully discovered and still cannot be eliminated[14]. Using a commercial ring stapler to perform phimosis surgery causes great pain when the staple is removed[15]. Gauze peeling off, hemostat dilation, and pneumatic dilation are the most common nonsurgical phimosis treatments. In these treatments, external force is applied to remove the adhesion and clean out the smegma. These treatments, however, can injure the foreskin and glans. After initial disinfection treatment of these wounds, patients can locally apply erythromycin eye ointment, moist exposed burn ointment, and other topical treatments that can help wounds recover, such as ointments containing epidermal growth factors. Such treatments should be performed multiple times until the wounds fully heal to avoid adhesion recurrence[16].
Professional and medical specialists working in the hospital should carry out all of the above treatments. Often, multiple rounds of treatment are needed. Some children with phimosis may have symptoms such as red and swollen foreskins or difficulty urinating. These children may be uncooperative in pulling back and cleaning the foreskin due to the fear of pain, resulting in narrowing of the previously dilated foreskin mouth. As a result, the glans penis becomes adherent to foreskin again, and the foreskin returns to their original status. Exacerbating this situation, secretions of the penis adhere to the foreskin after dilation, resulting in further narrowing of the foreskin mouth and causing dilation treatment failure[17,18]. In this study, an innovative retractor for dilating phimosis, which can continuously and gently dilate the foreskin in multiple directions and at multiple angles, is introduced. Using traditional hemostats or pneumatic dilation to dilate the foreskin mouth can either cause pain to patients or result in foreskin laceration or foreskin bleeding due to strong external forces exerted on the foreskin. In clinical operation, we found that phimosis can be categorized as that characterized by a narrow foreskin mouth and that characterized by both a narrow foreskin mouth and foreskin adhering to the glans[19]. For treating patients of the first type, the retractor is used for one to seven days until the glans can be fully exposed. For treating patients of the second type, the foreskin can still adhere to glans after the foreskin mouth is dilated, which means that more time needs to be invested in treating the phimosis[20]. It is recommended that the foreskin be pulled back while patients are in the bath so that the adhesion between the foreskin and glans can be released. When necessary, patients can go to a specialist department in a hospital to perform the foreskin dilation treatments. Since the narrow part of the foreskin mouth has been dilated, only slight pain is felt in these treatments, and the foreskin is not red and swollen. After these treatments, patients do not have urinary difficulties or experience obvious pain and discomfort during urination, which is acceptable for children.
CONCLUSION
This innovative retractor can be applied to treat most cases of phimosis in children, and no general anesthetics are required. Compared to other treatments, retractor is easy to operate and inexpensive. Furthermore, good treatment effects can be achieved through gentle and continuous dilation of the foreskin. These characteristics make this retractor suitable for clinical promotion.
ARTICLE HIGHLIGHTS
Research background
Phimosis is one of the most common diseases in children. Early selection of appropriate treatment for phimosis in children is beneficial to the development of their reproductive organs and significantly improves the prognosis of phimosis in children. Although traditional circumcision is the most widely used, it has many disadvantages, including postoperative bleeding and incision infection, pain, obvious scars on the surgical incision, and unsatisfactory appearance. In addition, there is much controversy regarding treatment options and timing at home and abroad. Surgical procedures such as circumcision and cerclage for children with excessively long foreskin will greatly affect the normal life of children after the operation. Young children need general anesthesia, but this anesthesia carries a great risk.
In the clinical field, although improvements in medical equipment and technology are in progress, the mechanism of this complication has not been fully discovered and it still cannot be eliminated
In this study, an innovative retractor for phimosis expansion was introduced, which can continuously and gently expand the foreskin in multiple directions and at multiple angles, and relieve the patient's pain.
Research motivation
To design a retractor that can effectively expand the foreskin and reduce patient complications.
Research objectives
To design and manufacture a new type of retractor to verify its effectiveness.
Research methods
A total of 87 children with phimosis were selected. A new type of retractor was designed and manufactured. The children phimosis was dilated with an elastic dilation frame, in order to expand the foreskin mouth and expose the penis head, and after that, the phimosis was cured.
Research results
Complications occurred in a small number of children 2 wk after surgery. These difficulties were overcome by performing the foreskin dilation and relaxation treatment with lidocaine cream used for superficial anesthesia. None of the cases had red and swollen foreskins or had difficulty urinating after the treatment. One month after the operation, all patients can fully reveal the glans.
Research conclusions
The phimosis dilatation retractor based on the principle of elastically expanding the prepuce can achieve the purpose of expanding the phimosis. The clinical application shows that the effect of the children phimosis retractor is significant, which is worth promoting.
Research perspectives
The characteristics mentioned above make this innovative retractor suitable for clinical promotion.
Footnotes
Institutional review board statement: The study was reviewed and approved by the Ethics Committee of Longgang Central Hospital.
Informed consent statement: All study participants or their legal guardian provided informed written consent for personal and medical data collection prior to study enrolment.
Conflict-of-interest statement: The authors declare that they have no conflict of interest to disclose.
Manuscript source: Unsolicited manuscript
Peer-review started: December 29, 2020
First decision: January 17, 2021
Article in press: March 20, 2021
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Martelotto S S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Liu JH
Contributor Information
You-Wei Yue, Department of Urology, Longgang Central Hospital, Shenzhen 518116, Guangdong Province, China.
Yi-Wen Chen, Department of Urology, Longgang Central Hospital, Shenzhen 518116, Guangdong Province, China.
Li-Ping Deng, Department of Endocrinology, Longgang Central Hospital, Shenzhen 518116, Guangdong Province, China.
Han-Liang Zhu, Department of Urology, Longgang Central Hospital, Shenzhen 518116, Guangdong Province, China.
Jian-Hua Feng, Department of Urology, Longgang Central Hospital, Shenzhen 518116, Guangdong Province, China. 1053259373@qq.com.
Data sharing statement
No additional data are available.
References
- 1.Ribilotta A, Sergio M, Scarponi D. Parental stress in the relationship with children affected by chronic hematological disease. Minerva Pediatr. 2020 doi: 10.23736/S2724-5276.20.05912-5. [DOI] [PubMed] [Google Scholar]
- 2.Yang Z, Liu F, Cui L, Liu H, Zuo J, Liu L, Li S. Comparison of the effects of reconstruction of the lateral ankle ligaments using peroneus longus and peroneus brevis tendon graft. Medicine (Baltimore) 2020;99:e22912. doi: 10.1097/MD.0000000000022912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghidini F, Virgone C, Pulvirenti R, Trovalusci E, Gamba P. Could a careful clinical examination distinguish physiologic phimosis from balanitis xerotica obliterans in children? Eur J Pediatr. 2021;180:591–595. doi: 10.1007/s00431-020-03881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaufman MR, Smelyanskaya M, Van Lith LM, Mallalieu EC, Waxman A, Hatzhold K, Marcell AV, Kasedde S, Lija G, Hasen N, Ncube G, Samuelson JL, Bonnecwe C, Seifert-Ahanda K, Njeuhmeli E, Tobian AA. Adolescent Sexual and Reproductive Health Services and Implications for the Provision of Voluntary Medical Male Circumcision: Results of a Systematic Literature Review. PLoS One. 2016;11:e0149892. doi: 10.1371/journal.pone.0149892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stangl FP, Thalmann GN. [Urologic Emergencies: Paraphimosis] Ther Umsch. 2020;77:223–225. doi: 10.1024/0040-5930/a001182. [DOI] [PubMed] [Google Scholar]
- 6.Agwu NP, Muhammad AS, Abdullahi AA, Bashir B, Legbo JN, Mungadi IA. Pattern and outcome of management of Fournier's gangrene in a resource-constraint setting. Urol Ann. 2020;12:248–253. doi: 10.4103/UA.UA_62_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan P. A prospective study comparing modified foreskin reconstruction vs circumcision with tubularized incised plate urethroplasty for distal and mid penile hypospadias. J Pediatr Urol 2020; 16: 674.e1-674. :e7. doi: 10.1016/j.jpurol.2020.07.040. [DOI] [PubMed] [Google Scholar]
- 8.Ali A, Derar D, Al-Sobyil FA, Zeitoun MM, Hassanein KMA, Al-Howas A. Phimosis in male dromedary camels: Clinical findings and changes in the hemogram, nitric oxide metabolites, and testosterone concentrations. Theriogenology. 2016;85:1576–1581. doi: 10.1016/j.theriogenology.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Joseph Davey DL, Wall KM, Kilembe W, Naw HK, Brill I, Vwalika B, Chomba E, Mulenga J, Tichacek A, Javanbakt M, Gorbach PM, Allen SA. HIV Incidence and Predictors of HIV Acquisition From an Outside Partner in Serodiscordant Couples in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2017;76:123–131. doi: 10.1097/QAI.0000000000001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akyüz O, Çam K. The Management of Phimosis Seen after Circumcision with Thermocautery. Urol J. 2020;17:50–54. doi: 10.22037/uj.v0i0.5138. [DOI] [PubMed] [Google Scholar]
- 11.Balaji DR, Reddy G, Babu R, Paramaswamy B, Ramasundaram M, Agarwal P, Joseph LD, D'Cruze L, Sundaram S. Androgen Receptor Expression in Hypospadias. J Indian Assoc Pediatr Surg. 2020;25:6–9. doi: 10.4103/jiaps.JIAPS_166_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lourenção PLTA, Queiroz DS, de-Oliveira WE Junior, Comes GT, Marques RG, Jozala DR, Ortolan EVP. Observation time and spontaneous resolution of primary phimosis in children. Rev Col Bras Cir. 2017;44:505–510. doi: 10.1590/0100-69912017005013. [DOI] [PubMed] [Google Scholar]
- 13.Kjellgard C, Westphal S, Flisberg A. [Intoxication with prilocaine/lidocaine can cause serious methemoglobinemia] Lakartidningen. 2019;116 [PubMed] [Google Scholar]
- 14.Jing P, Zou J, Zhao D, Yang J, Feng S, Wang C. [Clinical study of concealed penis correction surgery based on principle of midline symmetry] Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:505–508. doi: 10.7507/1002-1892.201909106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan F, Pan L, Zhang A, Liu Y, Zhang F, Dai Y. Circumcision with a novel disposable device in Chinese children: a randomized controlled trial. Int J Urol. 2013;20:220–226. doi: 10.1111/j.1442-2042.2012.03132.x. [DOI] [PubMed] [Google Scholar]
- 16.Jiang ZL, Sun CW, Sun J, Shi GF, Li H. Subcutaneous tissue-sparing dorsal slit with new marking technique: A novel circumcision method. Medicine (Baltimore) 2019;98:e15322. doi: 10.1097/MD.0000000000015322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russo T, Currò M, Barbera A, Caccamo D, Antonuccio P, Arena S, Montalto AS, Parisi S, Marseglia L, Gitto E, Ientile R, Impellizzeri P, Romeo C. Expression of Transglutaminase in Foreskin of Children with Balanitis Xerotica Obliterans. Int J Mol Sci. 2016;17 doi: 10.3390/ijms17091551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang H, Huang Z, Zhou J, Zhang X, Liang C. Clinical Outcomes And Risk Factors In Patients Circumcised By Chinese Shang Ring: A Prospective Study Based On Age And Types Of Penile Disease. Ther Clin Risk Manag. 2019;15:1233–1241. doi: 10.2147/TCRM.S215471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barone MA, Li PS, Lee RK, Ouma D, Oundo M, Barasa M, Oketch J, Otiende P, Nyangweso N, Maina M, Kiswi N, Chirchir B, Goldstein M, Awori QD. Simplifying the ShangRing technique for circumcision in boys and men: use of the no-flip technique with randomization to removal at 7 days vs spontaneous detachment. Asian J Androl. 2019;21:324–331. doi: 10.4103/aja.aja_91_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tewari S, Lubna N, Shah R, Al-Rikabi ABH, Shah K, Sheth J, Sheth F. Molecular characterization and evaluation of complex rearrangements in a case of ring chromosome 15. Mol Cytogenet. 2017;10:38. doi: 10.1186/s13039-017-0339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data are available.