Abstract
Asthma and pulmonary tuberculosis (PTB) are disease entities with different pathogenesis. However, endobronchial tuberculosis (EBTB), a peculiar form of PTB, can mimic the symptoms of asthma. Although uncommon, the coexistence of asthma and PTB can appear. We report three cases of PTB. The first two cases with EBTB were misdiagnosed as asthma and the third case with asthma developed PTB four months after high‐dose inhaled corticosteroid (ICS) therapy. The first two cases presented with chronic cough up mucopurulent/purulent sputum and localized wheezing which revealed diagnostic clues. The third case presented with dry cough and showed a positive bronchodilator response and the right pulmonary apical fibrosis which could be associated with quiescent tuberculous infection. EBTB should be included in the differential diagnosis of asthma. Although rare, physicians should be aware that PTB can also be developed during the treatment course of asthma.
Keywords: Asthma, endobronchial tuberculosis, inhaled corticosteroid, wheezing
Endobronchial tuberculosis should be included in the differential diagnosis of asthma. Although rare, physicians should be aware that pulmonary tuberculosis can also be developed during the treatment course of asthma.
Introduction
Asthma and pulmonary tuberculosis (PTB) are common respiratory diseases in developing countries such as Vietnam. They have differences in predominant Th1 or Th2 pathogenesis and they are also considered as mutual exclusive diseases [1]. Although coexistence of them is uncommon, it can still appear [1, 2]. Moreover, endobronchial tuberculosis (EBTB), a peculiar entity of PTB causing the tuberculous infection of tracheobronchial tree, could present with clinical features (chronic cough, wheezing, and normal chest X‐ray (CXR)) mimicking asthma [3, 4]. The differential diagnosis of two conditions can be challenging for pulmonary physicians. We report three cases evaluated at the Asthma and COPD care outpatient unit (ACOCU): the first two cases with EBTB were misdiagnosed as asthma and the third case presented with the coexistence of asthma and PTB.
Case Series
Case 1
An 18‐year‐old female non‐smoker presented at ACOCU with a four‐month history of chronic cough and wheezing. She coughed up mucopurulent/yellow sputum. Her past medical history was unremarkable. Physical examination revealed bilateral wheezing but predominant over the left lung. Her CXR was normal (Fig. 1) and the result of spirometry revealed only mild restrictive pattern and a negative bronchodilator test (post‐test values of FEV1 (forced expiratory volume in 1 sec), FVC (forced vital capacity), and FEV1/FVC were 66%, 68%, and 0.87, respectively). She was diagnosed with asthma and treated with budesonide/formoterol but her condition had no improvement. Bronchoscopy showed whitish pseudo‐membrane alongside the lower third trachea to narrow the left main bronchus. Xpert MTB/RIF of bronchial lavage was positive for Mycobacterium tuberculosis sensitive with rifampicin. Diagnosis of EBTB was established and the patient showed clinical improvement on anti‐tuberculous treatment.
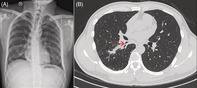
Figure 1.

Chest X‐ray showed no abnormal finding of lung fields.
Case 2
A 40‐year‐old male non‐smoker presented at ACOCU with a two‐month history of chronic cough and intermittent wheezing. His past medical history was unremarkable. Through two months, he had coughed up mucopurulent sputum and his severity of cough worsened despite using budesonide/formoterol as the asthma medication. On clinical examination, we documented monophonic wheezing predominant on the right lung. CXR was normal and spirometry showed no both obstructive and restrictive patterns (post‐test values of FEV1, FVC, and FEV1/FVC were 78%, 80%, and 0.83, respectively). Chest computed tomography (CT) scan revealed the narrowing of the right lower lobe bronchus and scattered parenchymal infiltrations (Fig. 2). Acid‐fast bacillus (AFB) smear of sputum was positive and the diagnosis of EBTB was made. Anti‐tuberculous treatment improved his condition spectacularly.
Figure 2.
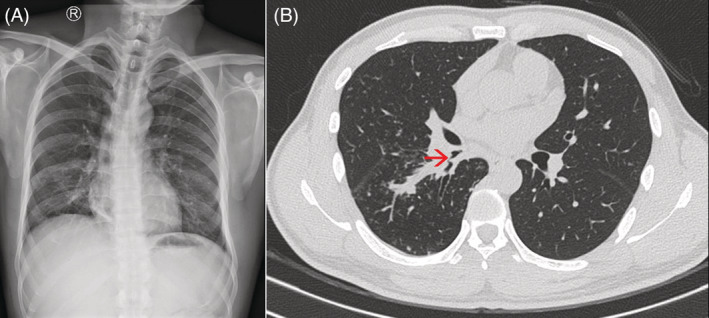
Chest X‐ray and chest computed tomography (CT) scan. (A) Chest X‐ray showed no abnormal finding of lung fields. (B) Chest CT scan showed the narrowing of the right lower lobe bronchus (red arrow).
Case 3
A 20‐year‐old female patient visited ACOCU with the chief complaint of dry cough for six months. She had intermittent breathlessness with severe emotional distress. Her past medical history revealed atopic eczema and allergic rhino‐sinusitis. Physical examination had no abnormal signs. Her CXR at the first visit showed small fibrosis at the right lung apex and the result of spirometry showed a positive bronchodilator test (% change of FEV1 was 12% and 250 mL). Post‐test values of FEV1, FVC, and FEV1/FVC were 86%, 80%, and 0.93, respectively. She had been diagnosed with asthma and treated with budesonide/formoterol (800 μg budesonide per day). Although her cough improved initially, it worsened with yellow sputum after four months. The second CXR revealed typical finding of post‐primary tuberculosis at the apical zone of the right lung (Fig. 3). Sputum smears for AFB were positive and anti‐tuberculous treatment was initiated. Her condition was improved with both asthma and anti‐tuberculous treatment.
Figure 3.
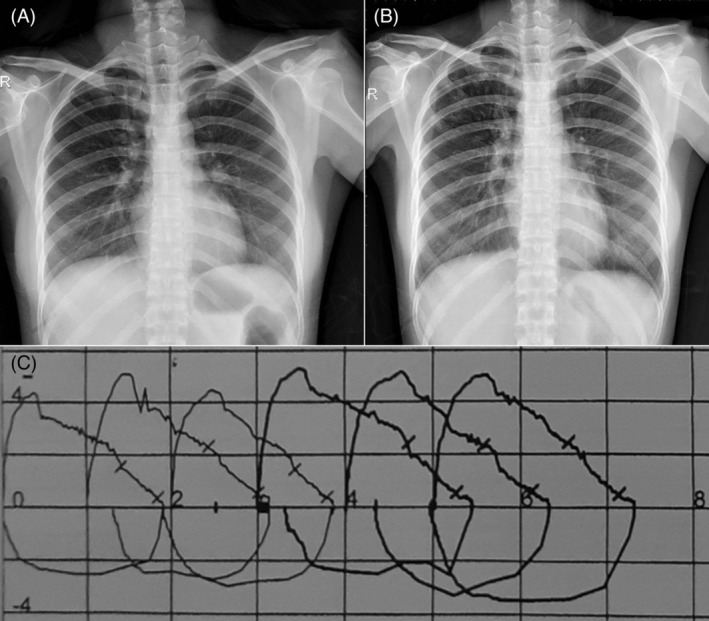
Two chest X‐rays and the flow–volume curve of spirometry. (A) Chest X‐ray (CXR) at the first visit revealed the right apical fibrosis. (B) Second CXR after more than four months of the first one revealed the right apical infiltration. (C) The flow–volume curve showed a positive bronchodilator test with bold curve representing post‐test spirometry.
Discussion
Chronic cough and wheezing are two symptoms appearing in both asthma and PTB. Wheezing in PTB patients is usually locally monophonic and can be caused by intraluminal obstruction due to secretions or the proliferative tubercular lesion on the bronchial wall, stricture in healed tubercular focus, or extra‐luminal obstruction associated with lymph node enlargement. Moreover, 10–20% of EBTB patients present with normal CXR [5, 6, 7]. Therefore, differentiation between asthma and EBTB is necessary, especially in the area with the high prevalence of PTB. Previously published cases showed that EBTB with normal CXR could simulate asthma [3, 4] similar to our first two cases. It is essential to raise awareness of EBTB among patients diagnosed with asthma. Our case series emphasized several suspecting features including chronic cough up of mucopurulent/purulent sputum and local wheezing that were not controlled by the conventional asthma treatment. Prolonged cough with “barking” or “hacking” characteristics was the diagnostic clue of EBTB [8, 9], especially in patients non‐responsive to antibiotic treatment. Mucopurulent/purulent sputum among asthma patients is associated with neutrophilia and possible bacterial infection [10] which our case series suggested as a feature suspecting tuberculous infection.
Although uncommon, coexistence of asthma and PTB could appear similar to our third case [1, 2, 11]. Two conditions are considered mutually exclusive diseases because of the opposite immune mechanism associated with Th1/Th2 predominant pathogenesis [1]. Corticosteroid could affect lymphocyte function and immunologically mediated processes to impair cell‐mediated immunity and antibody production. In turn, it results in the development of tuberculosis not only with the systemic corticosteroid therapy, but also with inhaled corticosteroid (ICS) usage among patients with respiratory disease [12, 13]. Whether the use of ICS in asthma patients cause flare‐up of tuberculous lesion has still been debate [13, 14]. Our asthma case showed the apical small fibrosis on CXR which could be suitable for quiescent tuberculous infection, and a smear‐positive PTB was established after more than four months of treatment with high‐dose ICS. The development of PTB should be considered during the treatment course of asthma.
The Global Initiative for Asthma guideline 2020 emphasized the re‐assessment during management of asthma patients which is useful to make the correct final diagnosis and detect factors associated with uncontrolled asthma [15]. PTB, particularly EBTB, should be noticed in this situation. Bronchoscopy in the first case and chest CT scan in the second case showed the role in diagnosing EBTB which was documented previously [6]. The main mission of an ACOCU is the management of asthmatic and chronic obstructive pulmonary disease patients. Therefore, differential diagnosis of asthma and EBTB would be difficult to achieve in a simple ACOCUs where only CXR and spirometry are available.
In conclusion, misdiagnosis of EBTB as asthma is not uncommon, especially in EBTB patients with normal CXR. Diagnostic clues including cough up of mucopurulent/purulent sputum, locally monophonic wheezing, and non‐responsiveness with conventional asthma treatment should be noticed. Moreover, although coexistence of asthma and PTB is uncommon, physicians should be aware that PTB can also be developed during the treatment course of asthma.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this manuscript and accompanying images.
Author Contribution Statement
Conceptualization: Lam Nguyen‐Ho, Au Nguyen‐Tiet, Chang Yoon‐Seok. Data curation: Lam Nguyen‐Ho, Au Nguyen‐Tiet. Writing ‐ original draft preparation: Lam Nguyen‐Ho, Au Nguyen‐Tiet. Writing ‐ review and editing: Au Nguyen‐Tiet, Chang Yoon‐Seok. Approval of final manuscript: all authors.
Nguyen‐Ho, L , Nguyen‐Tiet, A , Chang, Y‐S . (2021) Asthma and pulmonary tuberculosis: misdiagnosis or coexistence. Respirology Case Reports, 9(7), e00797. 10.1002/rcr2.797
Associate Editor: Semra Bilaceroglu
References
- 1. Bragina EY, Tiys ES, Freidin MB, et al. 2014. Insights into pathophysiology of dystropy through the analysis of gene networks: an example of bronchial asthma and tuberculosis. Immunogenetics 66:457–465. [DOI] [PubMed] [Google Scholar]
- 2. Thakur R, and Verma PK. 2018. Incidence of tuberculosis among patients of bronchial asthma receiving treatment with metered dose corticosteroid by inhalation. J. Evid. Based Med. Healthc. 5:2760–2764. [Google Scholar]
- 3. Lee YH, and Sin‐Fai‐Lam KN. 2004. Endobronchial tuberculosis simulating bronchial asthma. Singapore Med. J. 45:390–392. [PubMed] [Google Scholar]
- 4. Baris SA, Onyilmaz T, Basyigit I, et al. 2015. Endobronchial tuberculosis mimicking asthma. Tuberc. Res. Treat. 2015:781842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nguyen‐Ho L, Tran‐Van N, Le‐Thuong V, et al. 2019. Hilar asymmetry in endobronchial tuberculosis patients: an often‐overlooked clue. Int. J. Infect. Dis. 80:80–83. [DOI] [PubMed] [Google Scholar]
- 6. Shahzad T, and Irfan M. 2016. Endobronchial tuberculosis – a review. J. Thorac. Dis. 8:3797–3802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nguyen‐Ho L, Tran‐Van N, and Le‐Thuong V. 2021. Central versus peripheral lesion on chest X‐ray: a case series of 31 endobronchial tuberculosis patients with negative sputum smears. Int. J. Mycobacteriol. 10:89–92. [DOI] [PubMed] [Google Scholar]
- 8. Nguyen‐Ho L. 2017. Comment on: approaching chronic cough. Singapore Med. J. 58:573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jolobe OMP. 2015. The index of suspicion for endobronchial tuberculosis when the chest X‐ray is normal. Q. J. Med. 108:265–266. [DOI] [PubMed] [Google Scholar]
- 10. Berlyne GS, Efthimiadis A, Hussack P, et al. 1999. Sputum in asthma: color versus cell counts. J. Allergy Clin. Immunol. 104:182–183. [DOI] [PubMed] [Google Scholar]
- 11. Tocker AM, and Davidson AG. 1994. The relationship of bronchial asthma (and hay fever) to pulmonary tuberculosis. J. Allergy 15:108–119. [Google Scholar]
- 12. Brassard P, Suissa S, Kezouh A, et al. 2011. Inhaled corticosteroids and risk of tuberculosis in patients with respiratory diseases. Am. J. Respir. Crit. Care Med. 183:675–678. [DOI] [PubMed] [Google Scholar]
- 13. Brode SK, Campitelli MA, Kwong JC, et al. 2017. The risk of mycobacterial infections associated with inhaled corticosteroid use. Eur. Respir. J. 50:1700037. [DOI] [PubMed] [Google Scholar]
- 14. Lee CH, Kim K, Hyun MK, et al. 2013. Use of inhaled corticosteroids and the risk of tuberculosis. Thorax 68:1105–1113. [DOI] [PubMed] [Google Scholar]
- 15. Global Initiative for Asthma . Global strategy for asthma management and prevention 2020. www.ginasthma.org. (accessed 4 Jun 2020).


