Abstract
Purpose
This meta-analysis compared the clinical outcome of three-dimensional (3D) printing combined with open reduction and internal fixation (ORIF) to traditional ORIF in the treatment of acetabular fractures.
Methods
We searched the Cochrane Library, PubMed, Embase, VIP database, CNKI, and Wanfang database with keywords “acetabular fracture”, “3D printing”, “three-dimensional printing”, “open reduction and internal fixation”, “Acetabulum”, “Acetabula” from January 2000 to March 2020. Two reviewers independently selected articles, extracted data, assessed the quality evidence and risk bias of included trials using the Cochrane Collaboration’ s tools and/or Newcastle–Ottawa scale. When the two analysts had different opinions, they would ask the third analyst for opinion. Randomized controlled trials or retrospective comparative studies of 3D printing combined with ORIF (3D printing group) versus traditional ORIF (conventional group) in the treatment of acetabular fractures were selected. The data of operation time, intraoperative blood loss, intraoperative fluoroscopy times, incidence of complications, excellent and good rate of Matta score for reduction, and excellent and good rate of hip function score were extracted. Stata14.0 statistical software was used for data analysis.
Results
Altogether 9 articles were selected, including 5 randomized controlled trials and 4 retrospective studies. A total of 467 patients were analyzed, 250 in the conventional group, and 217 in the 3D printing group. The operation time in the 3D printing group was less than that in the conventional group and the difference was statistically significant (standardized mean difference (SMD) = −1.19, 95% CI: −1.55 to −0.82, p < 0.05). The intraoperative bleeding volume of the 3D printing group was significantly lower than that of the conventional group (SMD = −1.08, 95% CI: −1.65 to −0.51, p < 0.05). The fluoroscopy times were less in the 3D printing group than in the conventional group and the difference was statistically significant (SMD = −1.64, 95% CI: −2.35 to −0.93, p < 0.05). The total incidence of complications in the 3D printing group was significantly lower than that in the conventional group (OR = 0.43, 95% CI: 0.24–0.79, p < 0.05). There was no significant difference in the excellent and good rate of Matta score for reduction between the two groups (OR = 0.60, 95% CI: 0.34–1.06, p > 0.05). There was no significant difference in the excellent and good rate of hip function score at the end of postoperative follow-up between the two groups (OR = 0.84, 95% CI: 0.46–1.56, p > 0.05), but the follow-up time varies from 6 months to 40 months.
Conclusion
Compared with traditional ORIF, 3D printing combined with ORIF has certain advantages in terms that 3D printing not only helps surgeons to understand acetabular fractures more intuitively, but also effectively reduces operation time, intraoperative blood loss, intraoperative fluoroscopy times, and postoperative complications. However, there were no significant differences in the excellent and good rate of Matta score for reduction and the excellent and good rate of hip function score at the end of follow-up.
Keywords: Three-dimensional printing, Acetabular fractures, Open reduction and internal fixation, Meta-analysis
Introduction
Acetabular fracture is a rare injury, commonly occurred in young patients and mostly resulted from high-energy mechanism. Due to the complex anatomical structure, anatomical morphological differences between individuals, and the limitation of surgical exposure, the treatment of acetabular fracture is a challenging issue. Along with the rapid economic development in China, the incidence of acetabular fracture has increased.1 Epidemiological survey from 2003 to 2007 conducted by Prof. Zhang2 showed that adult acetabular fracture accounted for 0.86% of all adult fractures, and 20.53% of adult pelvic and acetabular fractures in the same period. The incidence of acetabular fracture is increasing rapidly, especially among the elderly, which is expected to increase significantly by 2030.3 Because acetabular fracture is an intra-articular fracture, surgery is the first consideration for its treatment, especially for young patients.4 Anatomical reduction of the acetabulum is an important factor in preventing post-traumatic osteoarthritis.
The main methods of acetabular surgery including hip arthroplasty, open reduction, and internal fixation, external fixation, and each of them has its indications, advantages and disadvantages. Traditional open reduction and internal fixation (ORIF) has always been the standard surgical method for the treatment of acetabular fracture. Use of the traditional method, surgeons can see the injured area directly, and anatomical reduction of acetabular fracture can be achieved easily, however, massive soft tissue peeling leads to long operation time, excessive blood loss and many postoperative complications.5 With the development of science and technology, three-dimensional (3D) printing is used in complex fracture gradually. In recent years, many clinicians suggest using 3D printing to treat complex fracture. In a meta-analysis, Xiong et al.6 pointed out that 3D printing assisted surgery is superior to traditional method in the treatment of traumatic orthopedic fracture, because it has shorter operation time, less intraoperative blood loss, and less intraoperative fluoroscopy. As a new technique, the clinical effect of 3D printing on acetabular fractures remains controversial. There are some clinical studies reporting the clinical effects of 3D printing combined with ORIF versus traditional ORIF in the treatment of acetabular fracture. Unfortunately, due to the small sample size, insufficient clinical evidence has been collected. This study combined the data of the clinical studies, and compared the clinical effects of 3D printing combined with ORIF versus traditional ORIF in the treatment of acetabular fracture.
Methods
Search strategy
We searched English literature in the PubMed, Embase, the Cochrane Library, with keywords: “acetabular fracture”, “3D printing”, “three-dimensional printing”, “open reduction and internal fixation”, “acetabulum”, “acetabula” from January 2000 to March 2020. And we also searched Wanfang databases, VIP databases, and CNKI database using “acetabular”, “fracture”, “3D printing” for related Chinese literature.
Inclusion and exclusion criteria of literature
Inclusion criteria: (1) the subjects were closed acetabular fractures; (2) a randomized controlled trial or retrospective comparative study of ORIF (conventional group) versus 3D printing combined with ORIF (3D printing group) in the treatment of acetabular fractures; (3) for Chinese literature, the clinical retrospective studies and randomized controlled trials published on journals listed on Peking University core periodical catalogue; and (4) literature recorded the clinical outcomes, including operation time, intraoperative blood loss, intraoperative fluoroscopy times, the incidence of complications, excellent and good rate of Matta score for reduction, excellent and good rate of hip function score.
Exclusion criteria: (1) low quality Chinese literature (published on Chinese journals that are not listed on Peking University core periodical catalogue); (2) literature with the Newcastle-Ottawa scale (NOS) score less than 5 or the Cochrane system rated as high risk; (3) old acetabular fracture (more than 3 weeks), open fracture or bone tumor; (4) no outcome indicator or inability to provide mean value and standard deviation; and (5) single group sample size < 10.
Data extraction and literature screening
Data about general information and clinical outcomes were extracted. General information including authors’ name, publish date, study design, intervention method, case number, mean age, gender, and follow-up period. Clinical outcomes including operation time, intraoperative blood loss, intraoperative fluoroscopy times, the incidence of complications, excellent and good rate of Matta score for reduction, and excellent and good rate of hip function score.
According to the inclusion and exclusion criteria, 2 evaluators screened the literature strictly by reading the title, abstract or full text of the articles. During the data extracting process, 2 researchers double checked the data, and the third evaluator will assist in judging when there was any difference. A quality evaluator assessed the quality of the literature according to the standards for randomized controlled study in the Cochrane system. The quality of the retrospective comparative study was assessed with the NOS. The full score was 10, in which the NOS score ≤5 was classified as low-quality literature. The higher the score, the better the quality of the literature.
Statistical analysis
Data were analyzed by Stata 14.0 software. The heterogeneity of each study was tested by the I2 or p value test. It showed that there was heterogeneity between studies when I2 > 50% or p < 0.1. There was no heterogeneity and the fixed effect model was used to combine the effect. If there was heterogeneity, the random-effect model was used to combine the effect. Publication bias was judged by the symmetry of the funnel chart and the Egger test. Egger test p > 0.05 showed that there was no publication bias.
Results
Results of literature screening
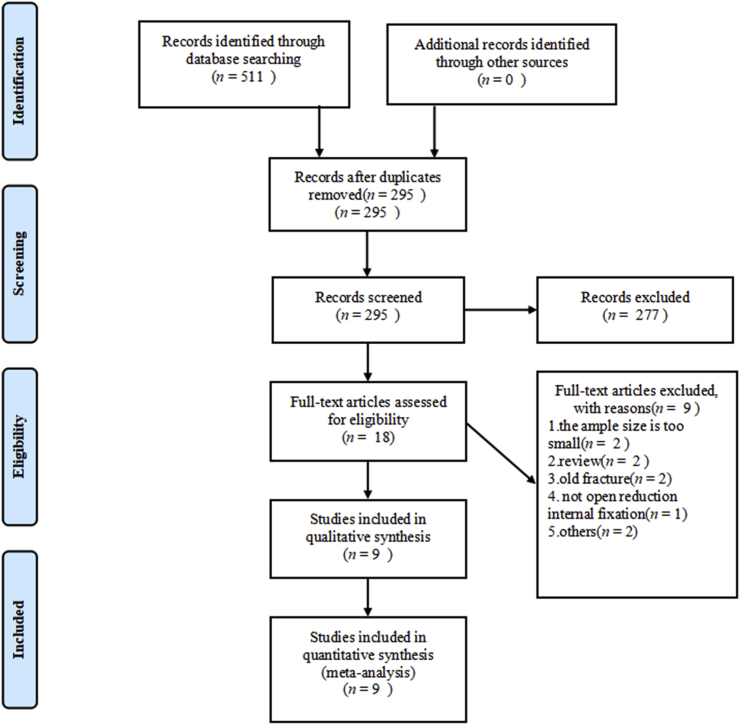
There were 182 English literature preliminarily retrieved from the international databases (PubMed 115, Embase 57, the Cochrane library 10). Among them, 49 articles were repeated, and another 123 articles were removed by reading the title or abstract. Full text of 10 English articles was read and finally 5 articles7, 8, 9, 10, 11 were included in this study. There were 329 related Chinese literature (Wanfang databases 147, VIP databases 93, CNKI 89). Among them, 167 articles were repeated and another 154 articles were removed by reading the title or abstract. Full text of 8 Chinese articles was read and finally 4 articles12, 13, 14, 15 were included in this study (Fig. 1).
Fig. 1.
Flow diagram.
General information and quality assessment of the eligible studies
All of the 9 included articles were published between 2016 and 2020, including 5 randomized controlled trials7, 8, 9, 10,15 and 4 retrospective comparative studies.11, 12, 13, 14 The general information of all the 9 articles is shown in Table 1. A total of 467 patients were analyzed, 217 in the 3D printing group and 250 in the conventional group. Risk of bias assessment of randomized controlled trials was assessed with the Cochrane system evaluation standards (Table 2). The quality of retrospective studies was assessed with the NOS score: 2 studies scored 7 points and 2 studies scored 6 points (Table 3).
Table 1.
General information of the eligible studies.
| Study (year) | Patient (n) | Age (year) | Gender (male/female) | Variables assessed | Follow-up (month) |
|---|---|---|---|---|---|
| Maini et al.7 (2018) | a, b, e | unclear | |||
| 3D printing | 10 | 37.9 | 9/1 | ||
| Conventional | 11 | 40.5 | 9/2 | ||
| Maini et al.8 (2018) | a, b, e | unclear | |||
| 3D printing | 12 | 38.2 | 11/1 | ||
| Conventional | 13 | 40.3 | 12/1 | ||
| Huang et al.9 (2020) | a, c, d, f | 40 | |||
| 3D printing | 20 | 43.4 | 12/8 | ||
| Conventional | 20 | 37.4 | 14/6 | ||
| Wan et al.10 (2019) | a, b, c, d, e, f | 6 | |||
| 3D printing | 48 | 43.4 | 34/14 | ||
| Conventional | 48 | 41.5 | 32/16 | ||
| Chen et al.11 (2019) | a, b, e, f | unclear | |||
| 3D printing | 28 | 46.1 | 18/10 | ||
| Conventional | 24 | 42.3 | 14/10 | ||
| Liu et al.12 (2017) | a, b, c, d, e, f | 15 | |||
| 3D printing | 19 | 37.6 | 12/7 | ||
| Conventional | 34 | 37.4 | 23/11 | ||
| Zhang et al.13 (2016) | a, b, c, d, e, f | 20 | |||
| 3D printing | 53 | 41.2 | 36/17 | ||
| Conventional | 68 | 42.6 | 42/26 | ||
| Wang et al.14 (2016) | a, b, c, d, e | 11 | |||
| 3D printing | 15 | 45.1 | 7/8 | ||
| Conventional | 19 | 43.7 | 11/8 | ||
| Zhang et al.15 (2020) | a, b | 12 | |||
| 3D printing | 12 | 38 | 7/5 | ||
| Conventional | 13 | 40.0 | 7/6 | ||
Variables assessed: a. operation time, b. intraoperative bleeding volume, c. intraoperative fluoroscopy times, d. total incidence of complications, e. the excellent and good rate of Matta score for reduction, f. the excellent and good rate of postoperative hip joint function.
Table 2.
The quality of the retrospective control studies assessed with Newcastle–Ottawa scale.
| Study (year) | Selection | Comparability | Exposure or outcome | NOS score |
|---|---|---|---|---|
| Chen et al.11 (2019) | ★★★ | ★ | ★★ | 6 |
| Liu et al.12 (2017) | ★★★ | ★ | ★★★ | 7 |
| Zhang et al.13 (2016) | ★★★ | ★ | ★★ | 6 |
| Wang et al.14 (2016) | ★★★ | ★★ | ★★ | 7 |
Note: Newcastle–Ottawa scale (NOS). It contains 8 items, which are categorized into 3 dimensions: selection, comparability, and exposure (case-control study) or outcome (cohort study); a maximum of 4 stars could be given in “selection,” a maximum of 2 stars could be given in “comparability”, a maximum of 4 stars could be given in “exposure or outcome”. One star equated to 1 point, the full score was 10 points, and it was classified as low-quality literature when NOS score ≤5 points. The higher the score, the better the quality of the literature.
Table 3.
Risk of bias assessment of the randomized controlled trial was assessed by the Cochrane collaboration tool.
| Study (year) | Randomization | Allocation concealment | Blinding of participants | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Maini et al.7 (2018) | Low risk | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Maini et al.8 (2018) | Low risk | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Huang et al.9 (2020) | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
| Wan et al.10 (2019) | Low risk | Unclear | Unclear | Unclear | Low risk | Low risk | Low risk |
| Zhang et al.15 (2020) | Low risk | Low risk | Unclear | Unclear | Low risk | Low risk | Low risk |
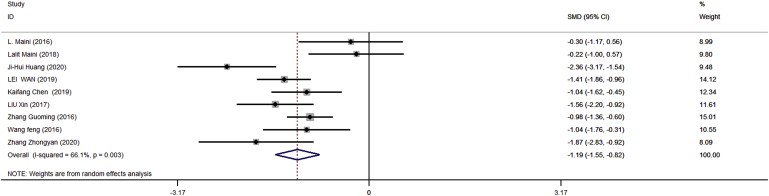
Operation time
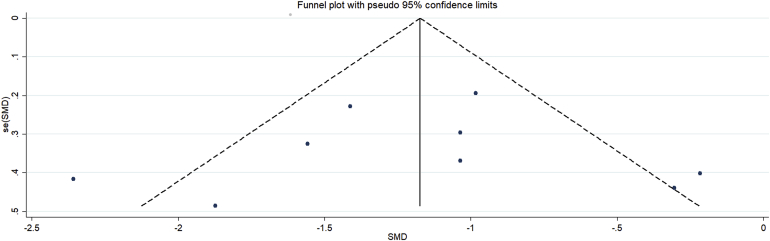
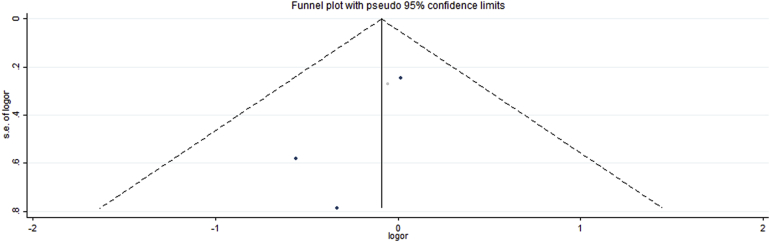
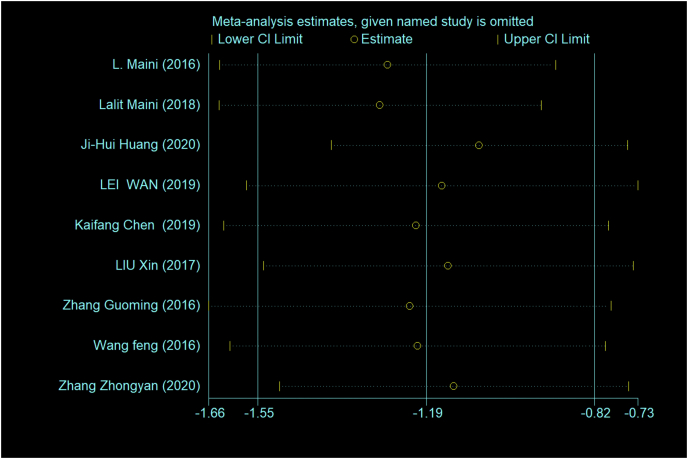
The operation time of the 467 patients in the 9 articles7, 8, 9, 10, 11, 12, 13, 14, 15 were collected and evaluated. The results of the fixed effect model showed that there was statistical heterogeneity among studies (p < 0.01, I2 = 66.1%). The random-effect model was used for analysis. The operation time in the 3D printing group was statistically significantly shorter than that in the conventional group (standardized mean difference (SMD) = −1.19, 95% CI: −1.55 to −0.82, p < 0.05) (Fig. 2). Funnel chart and Egger method were used to test the published bias of the 9 articles about the operation time of acetabular fractures in this meta-analysis (Fig. 3). The Egger test revealed no publication bias in the included studies (95% CI: −5.199 to 4.430, p = 0.837).
Fig. 2.
The operation time of the 3D group was shorter than that of the conventional group and the difference was statistically significant. (Forest plot of operation time).
Fig. 3.
Funnel plot of operation time.
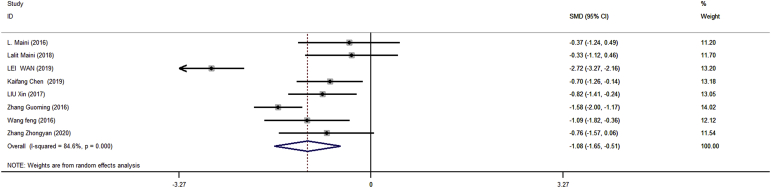
Intraoperative bleeding volume
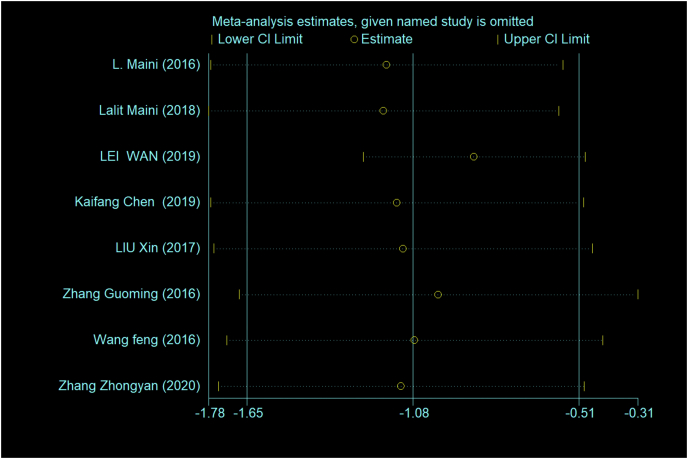
Eight articles7,8,10, 11, 12, 13, 14, 15 covering 407 patients reported the intraoperative blood loss. Data were combined and evaluated. The results of the fixed effect model showed that there was statistical heterogeneity among studies (p < 0.01, I2 = 84.6%). The random-effect model was used for analysis. The amount of intraoperative bleeding in the 3D printing group was significantly less than that in the conventional group (SMD = −1.08, 95% CI: −1.65 to −0.51, p < 0.05) (Fig. 4). Funnel chart and Egger method were used to test the publication bias of the 8 articles on intraoperative blood loss of acetabular fractures in this meta-analysis (Fig. 5). The Egger test revealed no publication bias in the included studies (95% CI: −2.975 to 13.584, p = 0.168).
Fig. 4.
The amount of intraoperative blood loss in the 3D group was less than that in the conventional group and the difference was statistically significant. (Forest plot of intraoperative blood loss).
Fig. 5.
Funnel plot of intraoperative blood loss.
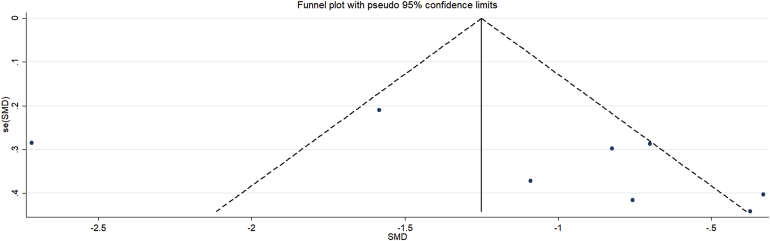
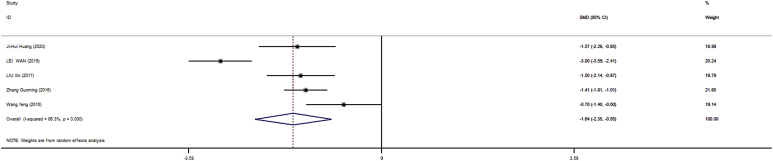
Intraoperative fluoroscopy times
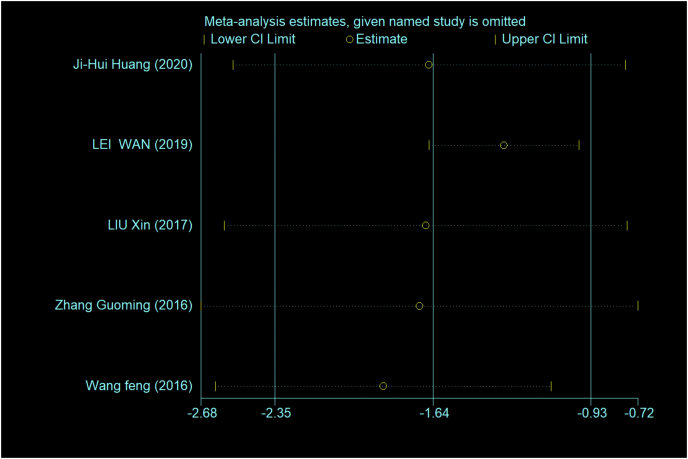
The intraoperative fluoroscopy times of 344 patients in the 5 articles9,10,12, 13, 14 were combined and evaluated. The results of the fixed effect model show that there was statistical heterogeneity among studies (p < 0.01, I2 = 86.3%). The random-effect model was used for analysis. The frequency of fluoroscopy in the 3D printing group was significantly lower than that in the conventional group (SMD = −1.64, 95% CI: −2.35 to −0.93, p < 0.05) (Fig. 6). Funnel chart and Egger method were used to test the published bias of 5 articles on fluoroscopy times of acetabular fractures in this meta-analysis (Fig. 7). The Egger test revealed no publication bias in the included studies (95% CI: −19.76 to 19.44, p = 0.981).
Fig. 6.
The times of fluoroscopy in the 3D group were less than that in the conventional group and the difference was statistically significant. (Forest plot of intraoperative fluoroscopy times).
Fig. 7.
Funnel plot of intraoperative fluoroscopy times.
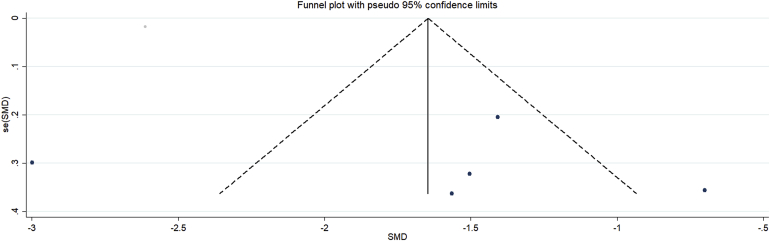
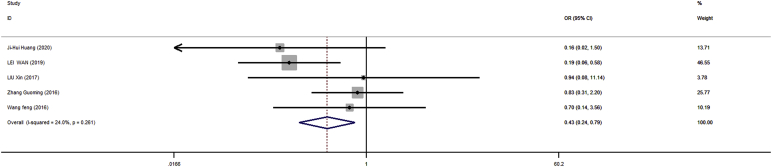
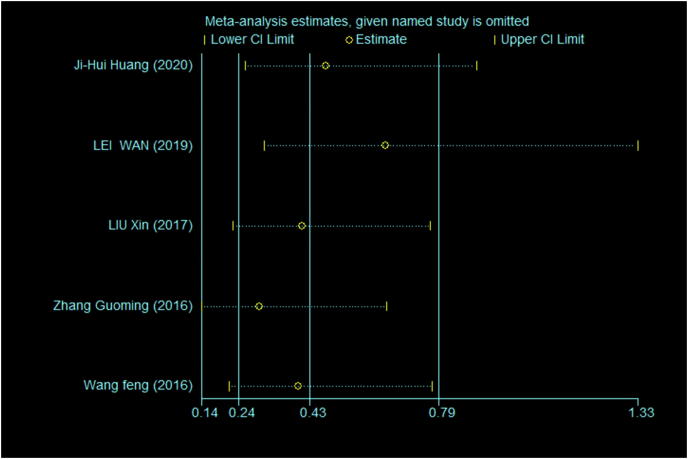
Total incidence of complications
The incidence of complications of 344 patients in the 5 articles9,10,12, 13, 14 were evaluated. The results of the fixed effect model showed that the heterogeneity among the studies was low (p = 0.261, I2 = 24%). The incidence of complications in the 3D printing group was significantly lower than that in the conventional group (OR = 0.43, 95% CI: 0.24 to 0.79, p < 0.05) (Fig. 8). Funnel chart and Egger method were used to test the publication bias of 5 articles (Fig. 9). The Egger test revealed no publication bias in the included studies (95% CI: −5.105 to 4.525, p = 0.860).
Fig. 8.
The incidence of complications in the 3D printing group was less than that in the conventional group and the difference was statistically significant. (Forest plot of the total rate of postoperative complications).
Fig. 9.
Funnel plot of the total incidence of postoperative complications.
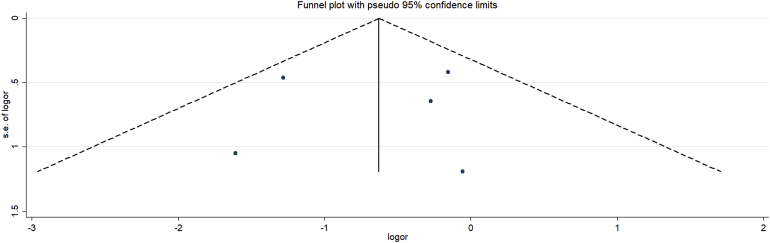
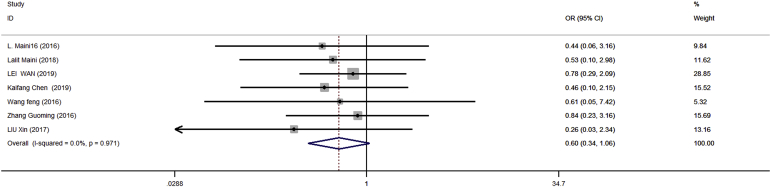
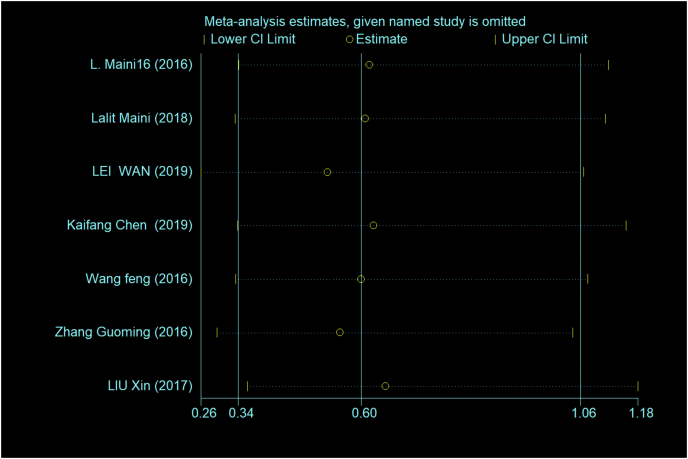
The excellent and good rate of Matta score for reduction
The excellent and good rate of Matta score for reduction of 390 patients from the 7 articles7, 8, 9, 10,12, 13, 14 were evaluated. The results of the fixed effect model showed that the statistical heterogeneity among the studies was low (p = 0.971, I2 = 0). There was no significant difference in the excellent and good rate of Matta score for reduction between the 3D printing group and the conventional group (OR = 0.60, 95% CI: 0.34 to 1.06, p > 0.05) (Fig. 10). Funnel chart and Egger method were used to test the publication bias of 5 articles on Matta score for reduction of acetabular fractures in this meta-analysis (Fig. 11). The Egger test revealed no publication bias in the included studies (95% CI: −2.20 to 0.04, p = 0.057).
Fig. 10.
There was no significant difference in postoperative reduction quality between the 3D printing group and the conventional group. (Forest plot of the excellent and good rate of Matta score for reduction).
Fig. 11.
Funnel plot of the excellent and good rate of Matta score for reduction.
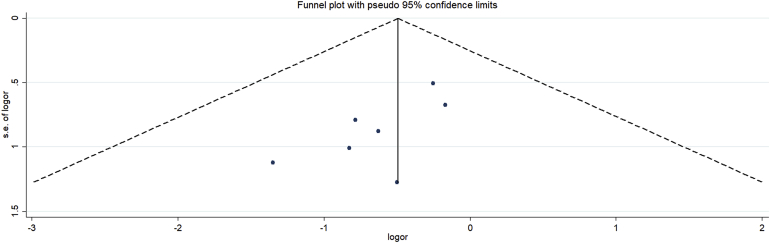
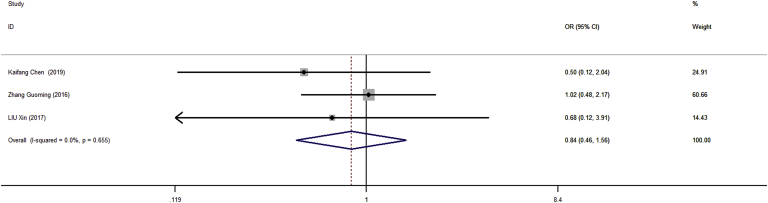
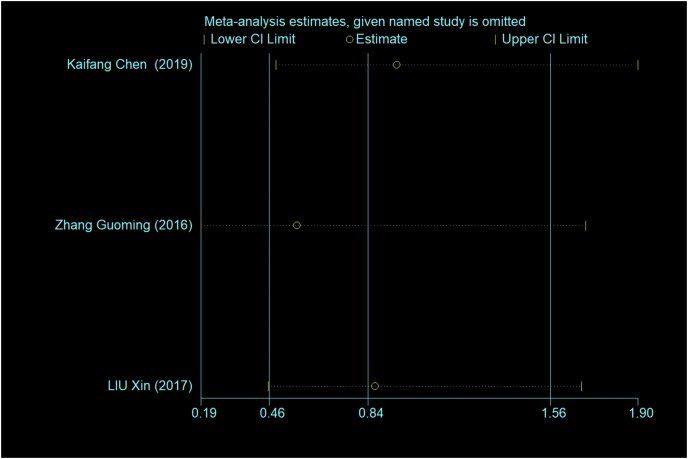
The excellent and good rate of postoperative hip joint function
The hip joint function of 226 patients from the 3 articles11, 12, 13 was assessed according to the modified Merle d’Aubigne & Postel score. The results of fixed effect model showed that the statistical heterogeneity among the studies was low (p = 0.65, I2 = 0). There was no significant difference in excellent and good rate of postoperative hip function scores between 3D printing group and conventional group. (OR = 0.84, 95% CI: 0.46 to 1.56, p > 0.05) (Fig. 12). Funnel chart and Egger method were used to test the publication bias of 5 articles about the excellent and good rate of postoperative hip function score of acetabular fracture in this meta-analysis (Fig. 13). The Egger test revealed no publication bias in the included studies (95% CI: −11.24 to 8.68, p = 0.35).
Fig. 12.
There was no significant difference in the excellent and good rate of postoperative hip joint scores between the 3D printing group and the conventional group. (Forest plot of hip joint function score).
Fig. 13.
Funnel plot of hip joint function score.
Sensitivity analysis
To verify the robustness of our results, sensitivity analysis was applied. The results suggested that the findings of this meta-analysis were relatively robust for all the 5 variables of operation time, intraoperative blood loss, intraoperative fluoroscopy times, total incidence of complications, excellent and good rate of Matta score for reduction, and excellent and good rate of hip function score (see in Appendix 1).
Discussion
Acetabular fracture is generally caused by high energy. The acetabulum is the largest movable joint and load-bearing joint of the human body with a deep concave hemispherical shape and a radius of about 1.8 cm. It is composed of anterior and posterior columns intersecting and camber 60°. There are rich muscles, nerves, and blood vessels around the acetabulum. The anatomical structure of the acetabulum is complex and it is easy to cause more bleeding after an injury. The operation of acetabular fracture has always been very challenging.16
The classification by Judet and Letournel of acetabular fractures based on double column support was described for the first time in an article published in the 1960s.17 However, in the classification of Judet and Letournel, the scope of the anterior wall and posterior wall of the acetabulum is unclear. It cannot be applied to atypical acetabular fracture, which may adversely affect its clinical application.18 Butler et al.19 believed that the Judet and Letournel classification system is still the gold standard for acetabular fracture. In a survey of 1266 patients with unilateral acetabular fractures from 1991 to 2006, ORIF was the main surgical method for acetabular fracture; although the frequency of surgical intervention increased, the quality of reduction did not improve over time.20 Boudissa et al.21 investigated 414 patients with acetabular fracture, but only 156 relatively young patients were treated with ORIF, and the most common complications of them were nerve injury, hemorrhagic shock, and deep venous thrombosis. Tannast et al.22 pointed out that 79% of patients with displaced acetabular fractures were able to avoid subsequent total hip arthroplasty within 20 years after ORIF. The preoperative planning of ORIF of acetabular fractures is essential. However, the preoperative planning based on the experience of clinicians and plain films or CT images have some limitations. Mishra et al.23 pointed out that 3D printing is very beneficial for complex orthopedic trauma, with better reduction, better implantation of the plate, and shorter operation time.
3D printing technology was first introduced by the engineering department and gradually applied to the medical field. 3D printing technique can directly display the shape of fracture and the spatial relationship between adjacent anatomical structures. It plays a important guiding role in the diagnosis, classification, and surgical treatment of complex fractures. Clinicians can simulate the operation before the operation and pre-bend the steel plate, which can shorten the curve of training young doctors.24 In recent years, many doctors have pointed out that 3D printing combined with ORIF can get better clinical results. A large number of clinical studies on 3D printing combined with ORIF in the treatment of acetabular fractures have been published,7, 8, 9, 10, 11, 12, 13, 14, 15 but their sample sizes were small. Therefore, we conducted a meta-analysis and combined the cases in the previous studies. With enlarged sample size, the conclusions of this study were much more objective and reliable, which provide some clinical guidance for the treatment of acetabular fractures.
The operation time and intraoperative blood loss were closely associated with the risk of operation and postoperative infection. In this meta-analysis, the operation time and intraoperative blood loss in the 3D printing group were significantly less than those in the conventional group. Because of the complexity of acetabular anatomy, simple two-dimensional images are difficult to reflect it directly. The surgeons in the conventional group only can choose appropriate plates and screws after the soft-tissue peeled and make final decision according to the situation during the operation. At the same time, they have to consider whether the bone implant was needed or not. On the other hand, the surgeons in the 3D printing group can perform pre-operation on the model, which can shorten the time of selecting plates and screws. The time of operation is related to the amount of intraoperative blood loss. The type of fracture also has effect on the results. Hsu et al.25 pointed out that in the 3D printing group the amount of bleeding in patients with acetabular fractures involving the anterior column was significantly less than that in the conventional group. However, the blood loss of patients with the posterior acetabular wall or posterior column fracture in the 3D printing group was not different from that in the conventional group. In this meta-analysis, the fluoroscopy times of 3D printing group was significantly less than that of the conventional group, which reduced radiation exposure to patients and health care workers. The results showed that the operation in the 3D printing group was smoother than that in the conventional group.
In this meta-analysis, the patients in the 3D printing group had fewer complications than that in the conventional group, but only 5 articles mentioned complications. Among the articles included in this study, the most common complications were nerve injury and infection. There were 8 cases in the 3D printing group and 16 in the conventional group sustained nerve injury. There were 4 cases in the 3D printing group and 15 in the conventional group had infection. The controversy about the incidence of complications has been existing for a long time. Huang et al.9 and Wang et al.14 considered that there was no significant difference in complications between the 3D printing group and the conventional group. The causes of complications are various, which are related to the type of injury, the degree of bone and soft tissue injury, age, body weight, smoking and the experience of orthopedic clinicians. Among them, the potential modifiable risk factors are smoking and obesity. Better understanding of risk factors is beneficial to fewer complications.26
The quality of reduction was evaluated with the Matta score.27 The displacement of the fracture <1 mm was an excellent (anatomical) reduction, 1–3 mm was a good (satisfactory) reduction, and >3 mm was a poor reduction. Seven articles in this meta-analysis used the Matta score to evaluate the quality of reduction, the result showed there was no difference between the two groups. Xiong et al.6 pointed out that there was no significant difference in anatomical reduction between the 3D printing group and the conventional group. In a comparative study of 16 patients with acetabular fracture and dislocation, Li et al.28 pointed out that the operation time and complications in the 3D printing group were less than those in the conventional group. However, there was no significant difference in the quality of postoperative reduction. In a meta-analysis of 3D printing combined with ORIF versus traditional ORIF in the treatment of tibial plateau fractures, Xie et al.29 pointed out that there was no significant difference in functional evaluation at the end of postoperative follow-up between the two groups.
In some of the articles included in this study, hip joint function was assessed according to the modified Merle d ’Aubigne & Postel score, i.e. 18 points representing an excellent hip joint function, 15–17 points a good function, 13–14 points an acceptable function, and <13 points poor function. Only 3 articles used the modified Merle d ’Aubigne & Postel score to evaluate the hip joint function. Our results showed that there was no difference between the two groups. The main purpose of application of 3D printing technology in the treatment of acetabular fractures are reducing operation time, intraoperative blood loss and postoperative complications. unfortunately, it is difficult to improve the quality of reduction and hip function.
Compared with traditional surgery, 3D printing technique combined with ORIF can improve the efficiency and safety of orthopedic surgery. In addition to treating patients, 3D technology may play an important role in education and training in orthopedics and trauma surgeries in the future.30 The doctor can better explain the disease to patients and their families. It is helpful to the diagnosis and classification of fractures.31 Before the operation, we can simulate the surgical approach, pre-bend the steel plate, and discuss the surgical plan on the 3D model. For complicated fractures, its advantages are more visible. However, there were some shortcomings of 3D printing technique. Xiong et al.6 pointed out that the hospitalization time of 3D printing was significantly longer than that of the conventional group, which would increase the economic burden of patients. 3D printing can only reflect the structure of bone tissue, but cannot reveal the soft tissue structures such as blood vessels, nerves, and so on.32 Meanwhile, the reduction of the fracture depends on the experience and technique of the surgeon. The accuracy of 3D printing also needs to be improved.
Some limitations were existing in this study. Among the 9 articles, there were only 4 retrospective studies, which reduced the robustness of its conclusion. The heterogeneity of the operation time, intraoperative bleeding volume, and intraoperative fluoroscopy times may be related to surgeons’ skill and fracture type. The sample size in the report is relatively small; the complexity of acetabular fractures is various; surgeons’ skill levels are different and the follow-up time varies at the end of the period. Those will also reduce the robustness of the conclusion. It is still necessary to further absorb foreign high-quality literature for study. A large sample size randomized controlled clinical trial should be conducted in order to draw a more reliable outcome.
3D printing combined with ORIF has certain advantages over traditional ORIF. 3D printing can help surgeons understand acetabular fractures more intuitively and effectively reduce operation time, intraoperative blood loss, fluoroscopy times and postoperative complications. However, there was no significant difference on the excellent and good rate of Matta score for reduction and the excellent and good rate of hip function score. 3D printing combined with ORIF is still a good choice for the treatment of acetabular fractures.
Funding
Nil.
Ethical statement
Not applicable.
Declaration of competing interest
All authors declare no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cjtee.2021.02.007.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Fig S1.
Fig S2.
Fig S3.
Fig S4.
Fig S5.
Fig S6.
References
- 1.Mauffrey C., Hao J., Cuellar D.O., 3rd The epidemiology and injury patterns of acetabular fractures: are the USA and China comparable? Clin Orthop Relat Res. 2014;472:3332–3337. doi: 10.1007/s11999-014-3462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y.Z. Thieme; New York, NY: 2012. Clinical Epidemiology of Orthopedic Trauma. [Google Scholar]
- 3.Melhem E., Riouallon G., Habboubi K. Epidemiology of pelvic and acetabular fractures in France. Orthop Traumatol Surg Res. 2020;106:831–839. doi: 10.1016/j.otsr.2019.11.019. [DOI] [PubMed] [Google Scholar]
- 4.Kelly J., Ladurner A., Rickman M. Surgical management of acetabular fractures - a contemporary literature review. Injury. 2020 Oct;51(10):2267–2277. doi: 10.1016/j.injury.2020.06.016. [DOI] [PubMed] [Google Scholar]
- 5.Zhang R., Yin Y., Li S. Fixation of displaced acetabular fractures with an anatomic quadrilateral surface plate through the stoppa approach. Orthopedics. 2019;42:e180–e186. doi: 10.3928/01477447-20181227-03. [DOI] [PubMed] [Google Scholar]
- 6.Xiong L., Li X., Li H. The efficacy of 3d printing-assisted surgery for traumatic fracture: a meta-analysis. Postgrad Med. 2019;95:414–419. doi: 10.1136/postgradmedj-2019-136482. [DOI] [PubMed] [Google Scholar]
- 7.Maini L., Sharma A., Jha S. Three-dimensional printing and patient-specific pre-contoured plate: future of acetabulum fracture fixation? Eur J Trauma Emerg Surg. 2018;44:215–224. doi: 10.1007/s00068-016-0738-6. [DOI] [PubMed] [Google Scholar]
- 8.Maini L., Verma T., Sharma A. Evaluation of accuracy of virtual surgical planning for patient-specific pre-contoured plate in acetabular fracture fixation. Arch Orthop Trauma Surg. 2018;138:495–504. doi: 10.1007/s00402-018-2868-2. [DOI] [PubMed] [Google Scholar]
- 9.Huang J.H., Liao H., Tan X.Y. Surgical treatment for both-column acetabular fractures using pre-operative virtual simulation and three-dimensional printing techniques. Chin Med J (Engl). 2020;133:395–401. doi: 10.1097/CM9.0000000000000649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wan L., Zhang X., Zhang S. Clinical feasibility and application value of computer virtual reduction combined with 3d printing technique in complex acetabular fractures. Exp Ther Med. 2019;17:3630–3636. doi: 10.3892/etm.2019.7344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen K., Yang F., Yao S. Application of computer-assisted virtual surgical procedures and three-dimensional Printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019;105:877–884. doi: 10.1016/j.otsr.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Liu X., Zeng C.J., Lu J.S. Application of 3D Printing and computer-assisted surgical simulation in preoperative planning for acetabular fracture. Nan Fang Yi Ke Da Xue Xue Bao. 2017;37:378–382. doi: 10.3969/j.issn.1673-4254.2017.03.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang G.M., Zhou D.S., He Y. 3D printing used in treatment of complex acetabular fractures. China J Orthop Traumatol. 2016;18:306–311. doi: 10.3760/cma.j.issn.1671-7600.2016.04.006. [DOI] [Google Scholar]
- 14.Wang F., Wang G.D., Xie C. Application of 3D printing technology in treatment of acetabular posterior wall fractures. China J Orthop Traumatol. 2016;18:120–125. doi: 10.3760/cma.j.issn.1671-7600.2016.02.006. [DOI] [Google Scholar]
- 15.Zhang Z.Y., Qi T.N., Mu H.Z. Efficacy of 3D Printing technology-assisted virtual surgical planning in acetabular fracture fixation. Chin J Tissue Eng Res. 2020;24:2405–2409. doi: 10.3969/j.issn.2095-4344.2570. [DOI] [Google Scholar]
- 16.Sautet P., Giorgi H., Chabrand P. Is anatomic acetabular orientation related to pelvic morphology? Ct analysis of 150 healthy pelvises. Orthop Traumatol Surg Res. 2018;104:347–351. doi: 10.1016/j.otsr.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Judet R., Judet J., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 18.Zhang R., Yin Y., Li A. Three-column classification for acetabular fractures: introduction and reproducibility assessment. J Bone Joint Surg Am. 2019;101:2015–2025. doi: 10.2106/JBJS.19.00284. [DOI] [PubMed] [Google Scholar]
- 19.Butler B.A., Lawton C.D., Hashmi S.Z. The relevance of the judet and letournel acetabular fracture classification system in the modern era: a review. J Orthop Trauma. 2019;33(Suppl 2):S3–S7. doi: 10.1097/BOT.0000000000001401. [DOI] [PubMed] [Google Scholar]
- 20.Ochs B.G., Marintschev I., Hoyer H. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German pelvic multicentre study group (dao/dgu) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Boudissa M., Francony F., Kerschbaumer G. Epidemiology and treatment of acetabular fractures in a level-1 trauma centre: retrospective study of 414 patients over 10 years. Orthop Traumatol Surg Res. 2017;103:335–339. doi: 10.1016/j.otsr.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Tannast M., Najibi S., Matta J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012;94:1559–1567. doi: 10.2106/JBJS.K.00444. [DOI] [PubMed] [Google Scholar]
- 23.Mishra A., Verma T., Vaish A. Virtual preoperative planning and 3d Printing are valuable for the management of complex orthopaedic trauma. Chin J Traumatol. 2019;22:350–355. doi: 10.1016/j.cjtee.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomazevic M., Kristan A., Kamath A.F. 3D printing of implants for patient-specific acetabular fracture fixation: an experimental study. Eur J Trauma Emerg Surg. 2019 doi: 10.1007/s00068-019-01241-y. [DOI] [PubMed] [Google Scholar]
- 25.Hsu C.L., Chou Y.C., Li Y.T. Pre-operative virtual simulation and three-dimensional printing techniques for the surgical management of acetabular fractures. Int Orthop. 2019;43:1969–1976. doi: 10.1007/s00264-018-4111-8. [DOI] [PubMed] [Google Scholar]
- 26.Kusnezov N., Bader J., Blair J.A. Predictors of inpatient mortality and systemic complications in acetabular fractures requiring operative treatment. Orthopedics. 2017;40:e223–e228. doi: 10.3928/01477447-20161202-03. [DOI] [PubMed] [Google Scholar]
- 27.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 28.Li Y.T., Hung C.C., Chou Y.C. Surgical treatment for posterior dislocation of hip combined with acetabular fractures using preoperative virtual simulation and three-dimensional Printing model-assisted precontoured plate fixation techniques. BioMed Res Int. 2019;2019:3971571. doi: 10.1155/2019/3971571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xie L., Chen C., Zhang Y. Three-dimensional Printing assisted orif versus conventional orif for tibial plateau fractures: a systematic review and meta-analysis. Int J Surg. 2018;57:35–44. doi: 10.1016/j.ijsu.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 30.Weidert S., Andress S., Suero E. 3d printing in orthopedic and trauma surgery education and training : possibilities and fields of application. Unfallchirurg. 2019;122:444–451. doi: 10.1007/s00113-019-0650-8. [DOI] [PubMed] [Google Scholar]
- 31.Lim P.K., Stephenson G.S., Keown T.W. Use of 3d printed models in resident education for the classification of acetabulum fractures. J Surg Educ. 2018;75:1679–1684. doi: 10.1016/j.jsurg.2018.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lou Y., Cai L., Wang C. Comparison of traditional surgery and surgery assisted by three dimensional printing technology in the treatment of tibial plateau fractures. Int Orthop. 2017;41:1875–1880. doi: 10.1007/s00264-017-3445-y. [DOI] [PubMed] [Google Scholar]