Abstract
Background
Although chronic lung disease is a common cause of mortality, little is known about where individuals with chronic lung disease die.
Research Question
The aim of this study was to determine the trends and factors associated with place of death among individuals with chronic lung disease.
Study Design and Methods
This cross-sectional analysis of natural deaths was conducted by using the Centers for Disease Control and Prevention Wide-ranging OnLine Data for Epidemiologic Research from 2003 to 2017 for which COPD, interstitial lung disease (ILD), or cystic fibrosis (CF) was the underlying cause. Place of death was categorized as hospital, home, nursing facility, hospice facility, and other.
Results
From 2003 to 2017, more than 2.2. million deaths were primarily attributed to chronic lung disease (51.6% female, 92.4% white). Most were attributed to COPD (88.9%), followed by ILD (10.8.%), and CF (0.3%). Hospital and nursing facility deaths declined from 44.4% (n = 59,470) and 22.6% (n = 30,285) to 28.3% (n = 49,655) and 19.7% (n = 34,495), while home and hospice facility deaths increased from 23.3% (n = 31,296) and 0.1% (n = 192) to 34.7% (n = 60,851) and 9.0% (n = 15,861), respectively. Male sex, being married, and having some college education were associated with increased odds of home death, whereas non-white race and Hispanic ethnicity were associated with increased odds of hospital death. Compared with individuals with COPD, individuals with ILD and CF had increased odds of hospital death and reduced odds of home, nursing facility, or hospice facility death.
Interpretation
Home deaths are rising among decedents from chronic lung disease, increasing the need for quality end-of-life care in this setting. Further research should explore the end-of-life needs and preferences of these patients and their caregivers, with particular attention paid to patients with ILD and CF who continue to have high rates of hospital death.
Key Words: COPD, cystic fibrosis, home, interstitial lung disease, palliative care
Abbreviations: CF, cystic fibrosis; ICD-10, International Classification of Diseases, Tenth Revision; ILD, interstitial lung disease
FOR EDITORIAL COMMENT, SEE PAGE 449
Lung disease is responsible for significant morbidity and mortality globally, with COPD alone being the fourth leading cause of death in the United States.1 Patients with chronic progressive lung diseases such as COPD, interstitial lung disease (ILD), and cystic fibrosis (CF) tend to experience a protracted decline with frequent exacerbations and recoveries, resulting in a high physical and psychosocial symptom burden.2,3 Research indicates that breathlessness, fatigue, and anxiety occur more commonly in patients with these diagnoses than in those with advanced cancer, heart disease, or renal disease.4,5 This high symptom burden often results in acute hospitalizations given the difficulty of managing exacerbations in the home setting.
Palliative care and hospice, which have been associated with improved quality of life and increased ability to die in one’s preferred location, remain understudied and underused in patients with pulmonary disease.6, 7, 8, 9 Palliative care focuses on quality of life and symptom management of serious illness at any stage; hospice is a type of palliative care for individuals with limited life expectancy. Importantly, disparities in the provision of both of these services are well documented. For example, racial minorities are less likely to receive palliative care or use hospice than white subjects, and research suggests that older adults may be less likely to receive specialist palliative care services than younger patients.10, 11, 12 Significant geographic variation in end-of-life health-care utilization, including hospice use, among patients with COPD has also been identified.13
Location of death serves as one important metric of quality end-of-life care. Most patients wish to die at home, and dying in the hospital setting is associated with increased intensity of potentially ineffective interventions, yet some patients’ symptoms may be inadequately managed at home.14,15 Little is known, however, about place of death for patients dying of chronic lung disease and how it has changed over time. The aim of the current study therefore was to assess trends and describe factors associated with place of death among patients with chronic lung disease in the United States. We hypothesized that home deaths have increased and that disparities in location of death exist according to demographic characteristics such as age, sex, race/ethnicity, marital status, geographic region, education, and disease subtypes.
Materials and Methods
Data Source
This study used aggregated death certificate data obtained from the Centers for Disease Control and Prevention Wide-ranging OnLine Data for Epidemiologic Research database for 2003 to 2017 and individual-level data from the Mortality Multiple Cause-of-Death Public Use Record for 2006 to 2017 from the National Center for Health Statistics. These sources are based on de-identified information abstracted from death certificates, and they provide mortality data for all deaths in the United States.16,17 We included deaths occurring between 2003 and 2017 attributed to the following lung diseases using International Classification of Diseases, Tenth Revision (ICD-10), codes for the following categories: CF, COPD, and ILD.
The primary study outcome of interest was place of death. Place of death categories included hospital, home, nursing facility/long-term care, hospice facility, and other (including outpatient medical facility, ED, and dead on arrival at the hospital). Within lung disease deaths, specific diagnosis subtypes were created by using the ICD-10 codes documented as the underlying cause of death: CF, E84; COPD, J42 to J44; and ILD, J84. Centers for Disease Control and Prevention Wide-ranging OnLine Data for Epidemiologic Research lists all deaths from 1999 onward using ICD-10 codes, and we therefore did not have to convert ICD-9 codes for death prior to 2014.
Decedent demographic characteristics included age (< 64, 65-74, 75-84, and ≥ 85 years), race (white, black, Native American/Alaska Native, and Asian/Pacific Islander), ethnicity (Hispanic or non-Hispanic), sex (male or female), marital status (married or not married), and education level (some college or more, high school or less). Using the standardized National Center for Health Statistics rural-urban classification, the following categories were created: large metropolitan (population ≥ 1 million), medium metropolitan (250,000-999,999), small metropolitan (50,000-250,000), and nonmetropolitan (< 50,000).18 Geographic variables were available in aggregate only because individual-level geographic information was not publicly available.
Analysis
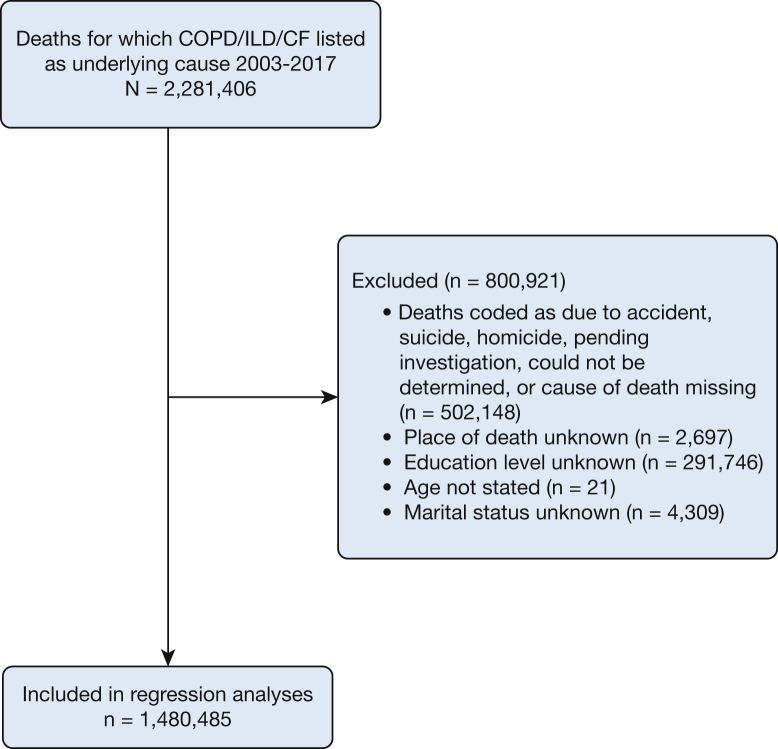
This descriptive study evaluated trends in and factors associated with place of death for 2013 to 2017. To assess the relation between patient characteristics and place, multivariable logistic regression was performed with models adjusting for decedent demographic characteristics, marital status, education, and year of death. A unique model was generated for each place of death vs all other places of death, defined as a binary indicator. The Huber-White SEs were used to estimate CIs robust to unknown correlations in the outcome. We used listwise deletion of cases with missing values (Fig 1). Deaths from 2003 to 2006 were not included in the regression analyses because a consistent code for education level was missing for these years.
Figure 1.
Participation flowchart. CF = cystic fibrosis; ILD = interstitial lung disease.
All analyses were conducted by using Stata version 16.0 (StataCorp). A two-tailed P value < .05 was considered statistically significant. ORs are presented with 95% CIs.
Results
Overall Trends
Between 2003 and 2017, more than 2.2 million deaths were primarily attributed to COPD, ILD, or CF (51.6% female, 92.4% white) (Table 1). The number of annual deaths due to these diseases increased from 134,040 in 2003 to 175,333 in 2017. The majority of these deaths were attributed to COPD (88.9%), ILD (10.8%), and CF (0.3%).
Table 1.
Place of Death of Decedents With COPD, Interstitial Lung Disease, and Cystic Fibrosis (2003-2017)
| Characteristic | Total (N = 2,279,875) | Hospital (n = 816,061 [35.8%]) | Home (n = 658,817 [28.9%]) | Nursing Home (n = 475,794 [20.9%]) | Hospice Facility (n = 119,861 [5.3%]) | Other (n = 209,342 [9.2%]) |
|---|---|---|---|---|---|---|
| Age, y | ||||||
| < 65 | 315,975 (13.9) | 128,782 (15.8) | 108,706 (16.5) | 24,706 (5.2) | 11,555 (9.6) | 42,226 (20.2) |
| 65-74 | 538,520 (23.6) | 220,417 (27.0) | 169,395 (25.7) | 69,088 (14.5) | 28,515 (23.8) | 51,105 (24.4) |
| 75-84 | 811,810 (35.6) | 300,725 (36.9) | 230,156 (34.9) | 168,943 (35.5) | 45,412 (37.9) | 66,574 (31.8) |
| ≥ 85 | 613,517 (26.9) | 166,127 (20.4) | 150,542 (22.9) | 213,050 (44.8) | 34,376 (28.7) | 49,422 (23.6) |
| Sex | ||||||
| Male | 1,103,423 (48.4) | 412,937 (50.6) | 335,696 (51.0) | 196,373 (41.3) | 55,559 (46.4) | 102,858 (49.1) |
| Female | 1,176,452 (51.6) | 403,124 (49.4) | 323,121 (49.0) | 279,421 (58.7) | 64,302 (53.7) | 106,484 (50.9) |
| Race | ||||||
| White | 2,105,853 (92.4) | 739,089 (90.6) | 616,082 (93.5) | 450,252 (94.6) | 113,662 (94.8) | 186,768 (89.2) |
| Black | 135,257 (5.9) | 58,902 (7.2) | 32,010 (4.9) | 20,307 (4.3) | 5,142 (4.3) | 18,896 (9.0) |
| Asian or Pacific Islander | 27,027 (1.2) | 13,301 (1.6) | 6,997 (1.1) | 3,558 (0.8) | 707 (0.6) | 2,464 (1.2) |
| Native American | 11,738 (0.5) | 4,769 (0.6) | 3,728 (0.6) | 1,677 (0.4) | 350 (0.3) | 1,214 (0.6) |
| Ethnicity | ||||||
| Non-Hispanic | 2,196,755 (96.4) | 778,850 (95.4) | 635,160 (96.4) | 465,195 (97.8) | 115,645 (96.5) | 201,905 (96.4) |
| Hispanic | 78,065 (3.4) | 35,244 (4.3) | 22,318 (3.4) | 9,606 (2.0) | 3,989 (3.3) | 6,908 (3.3) |
| Lung disease | ||||||
| COPD | 2,026,758 (88.9) | 693,593 (85.0) | 589,736 (89.5) | 445,991 (93.7) | 107,057 (89.3) | 190,381 (90.9) |
| Interstitial lung disease | 246,210 (10.8) | 117,552 (14.4) | 67,843 (10.3) | 29,685 (6.2) | 12,638 (10.5) | 18,492 (8.8) |
| Cystic fibrosis | 6,907 (0.3) | 4,916 (0.6) | 1,238 (0.2) | 118 (0.0) | 166 (0.1) | 469 (0.2) |
| County urbanization | ||||||
| Large central metro | 517,940 (22.7) | 201,535 (24.7) | 141,831 (21.5) | 100,411 (21.1) | 29,722 (24.8) | 44,441 (21.2) |
| Large fringe metro | 499,063 (21.9) | 177,468 (21.8) | 141,180 (21.4) | 100,306 (21.1) | 30,415 (25.4) | 49,694 (23.7) |
| Medium metro | 507,846 (22.3) | 169,328 (20.7) | 151,020 (22.9) | 106,104 (22.3) | 34,396 (28.7) | 46,998 (22.5) |
| Small metro | 257,926 (11.3) | 87,988 (10.8) | 78,785 (12.0) | 55,863 (11.7) | 12,414 (10.4) | 22,876 (10.9) |
| Micropolitan (nonmetro) | 277,653 (12.2) | 97,420 (11.9) | 82,688 (12.6) | 64,052 (13.5) | 8,321 (6.9) | 25,172 (12.0) |
| Noncore (nonmetro) | 219,447 (9.6) | 82,322 (10.1) | 63,313 (9.6) | 49,058 (10.3) | 4,593 (3.8) | 20,161 (9.6) |
Data are expressed as No. (%). Age not stated, n = 53. Ethnicity not stated, n = 5,055. Other category includes outpatient medical facility or ED, dead on arrival, other and unknown.
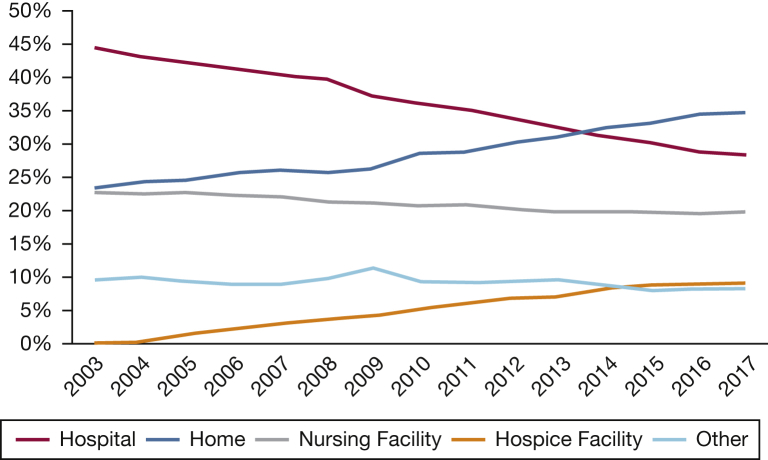
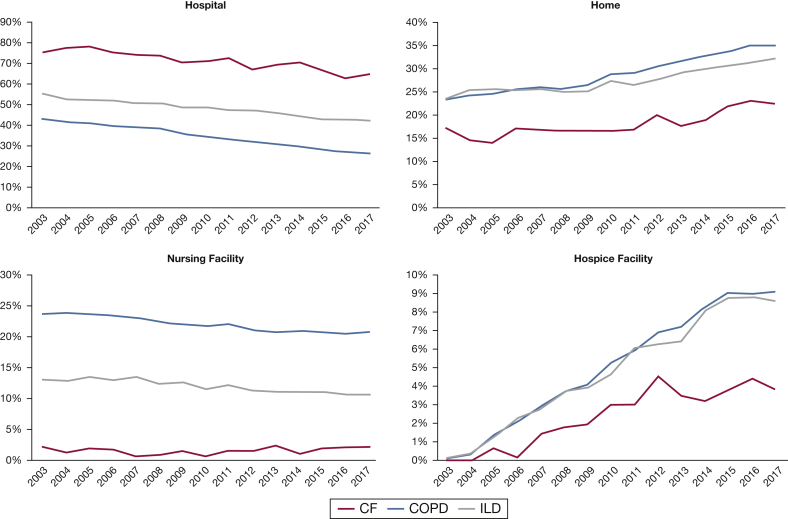
Between 2003 and 2017, home and hospice facility deaths increased while deaths in the hospital and nursing facilities decreased (Fig 2). The proportion of lung disease deaths occurring in the hospital decreased from 44.4% (n = 59,470) in 2003 to 28.3% (n = 49,655) in 2017. The proportion of deaths in nursing facilities fell slightly from 22.6% (n = 30,285) in 2003 to 19.7% (n = 34,495) in 2017. Over the same period, the proportion of deaths occurring at home increased from 23.3% (n = 31,296) to 34.7% (n = 60,851). The proportion of deaths in a hospice facility increased from 0.1% (n = 192) in 2003 to 9.1% (n = 15,861) in 2017.
Figure 2.
Trends for lung disease in places of death (2003-2017).
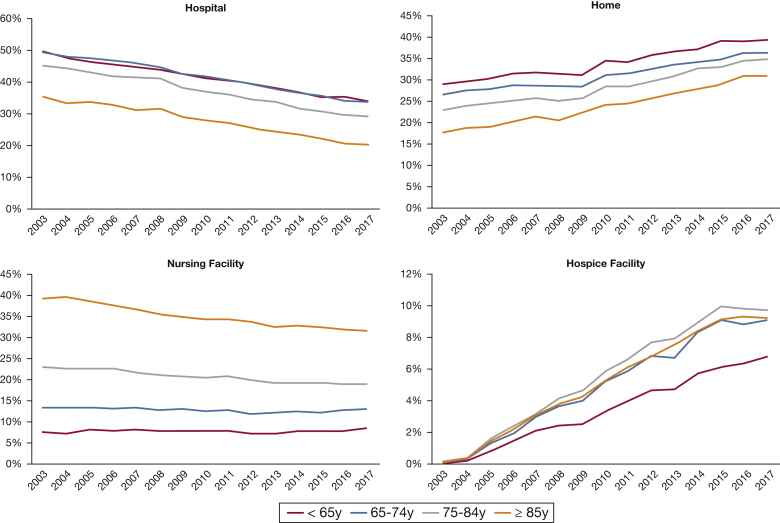
Differences According to Age
Compared with younger decedents, a lesser proportion of decedents aged ≥ 85 years died in the hospital and a greater proportion died in nursing facilities (Fig 3). The proportion of deaths occurring in nursing facilities fell over time among all age groups with the exception of those aged < 65 years. Among this youngest group, the proportion of nursing facility deaths increased from 7.5% (n = 1,306) in 2003 to 8.4% in 2017 (n = 2,085). Throughout the study period, a greater proportion of decedents aged < 65 years died at home compared with older decedents. A greater proportion of decedents between ages 75 and 84 years died in hospice facilities (37.9%) compared with decedents of all other ages (9.6% among those aged < 65 years, 23.8% among those aged 65-74 years, and 28.7% among those aged ≥ 85 years).
Figure 3.
Trends according to age in places of death (2003-2017).
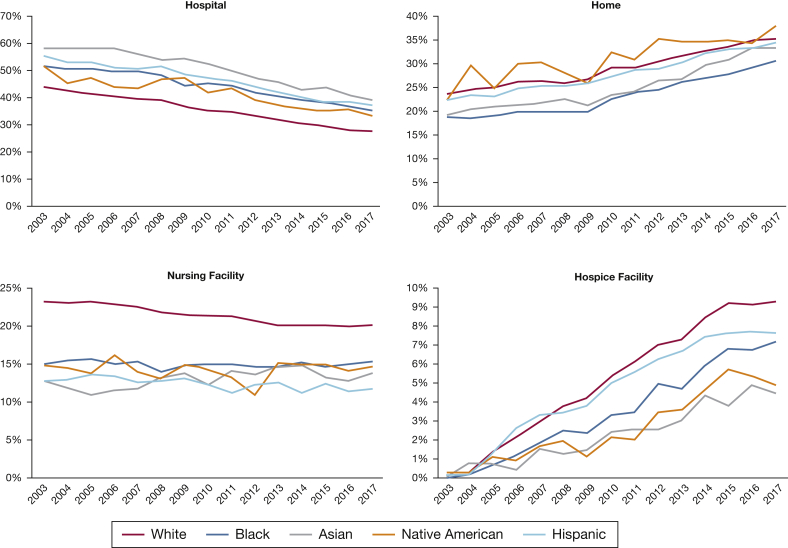
Differences According to Ethnicity and Race
Among both Hispanic and non-Hispanic subjects, home and hospice facility deaths increased while hospital and nursing facility deaths decreased. However, differences between these groups were noted (Fig 4). Throughout the study, a greater percentage of Hispanic vs non-Hispanic subjects died in the hospital, whereas a greater percentage of non-Hispanic vs Hispanic subjects died at home, in nursing facilities, and in hospice facilities. The difference in hospital, home, and nursing facility deaths between Hispanic and non-Hispanic subjects decreased, from 11.3% to 8.9%, 1.2% to 0.3%, and 10.1% to 8.3%, respectively.
Figure 4.
Trends according to race and ethnicity in places of death (2003-2017).
Compared with black decedents, a greater percentage of white decedents died at home, in nursing facilities, and hospice facilities, whereas a smaller percentage died in the hospital (Fig 4). The difference between black and white subjects in home deaths decreased from 5.0% to 4.4% over the study period, whereas the difference in hospital deaths between black and white subjects was virtually unchanged, decreasing slightly from 7.8% to 7.7% between 2003 and 2017. Increases in home deaths were seen among decedents from all racial groups, with Native American subjects having the greatest percentage of home deaths in 2017 (37.8%) followed by white subjects (35.0%). In 2017, a smaller percentage of white decedents died in the hospital (27.6%) relative to non-white subjects (Native American subjects, 33.0%; black subjects, 35.3%; Asian subjects, 39.0%). Hospice facility deaths increased for all racial groups, with a greater percentage occurring among white decedents (9.3%), followed by black subjects (7.2%), Native American subjects (4.9%), and Asian subjects (4.5%). The percentage of nursing facility deaths increased slightly among black and Asian decedents.
Geographic Differences
The greatest proportion of home deaths in 2017 occurred in nonmetropolitan areas (36.2%) and the least in large metropolitan areas (33.0%) (e-Fig 1). Large metropolitan areas (29.9%) had the greatest proportion of hospital deaths, and medium metropolitan areas had the smallest (26.5%). Nonmetropolitan areas had the greatest (22.6%) proportion of nursing facility deaths, and large metropolitan areas had the lowest (18.3%). Medium metropolitan areas had the greatest proportion of hospice facility deaths (10.4%), and nonmetropolitan had the smallest (5.2%).
Compared with other parts of the country, a greater percentage of decedents in the West census region died at home (38.9% in 2017) (e-Fig 2). The Northeast had the smallest percentage of home deaths in the country, with only 29.1% in 2017. Compared with other regions, a greater percentage of decedents in the Northeast (32.6%) died in the hospital in 2017. The greatest reduction in hospital deaths occurred in the South (42.0% change), followed by the Midwest (33.6% change) and the Northeast (32.8% change). From 2003 to 2017, the West experienced the smallest decline in hospital deaths (28.8% change). Throughout the study period, the greatest percentage of nursing facility deaths occurred in the Midwest relative to other regions. In 2017, the South experienced the greatest percentage of hospice facility deaths (12.0%), whereas the West had the smallest percentage (6.0%) compared with other regions.
Differences According to Lung Disease Type
The pattern of increasing home and hospice deaths as well as decreasing hospital and nursing facility deaths was consistent across all lung disease subgroups, although the magnitude of these changes differed (Fig 5). The greatest increases in home deaths occurred among deaths due to COPD, increasing by > 50% over the study period to reach 35.1% in 2017. In 2017, 32.2% of decedents with ILD and 22.4% of those with CF died at home. The proportion of patients dying in the hospital was reduced over the period in all lung disease groups. The greatest reduction in hospital deaths occurred among COPD (38.6% change), followed by ILD (23.1% change) and CF (14.8%). The lowest rate was observed among deaths due to COPD disorders in 2017 at 26.5%. Rates of hospice facility deaths increased the most among COPD and ILD, reaching 9.1% and 8.6%, respectively, in 2017. Only 3.9% of CF deaths in 2017 occurred in a hospice facility.
Figure 5.
Trends according to lung disease subtype in places of death (2003-2017). See Figure 1 legend for expansion of abbreviations.
Logistic Regression Results
Of all deaths between 2003 and 2017, a total of 1,480,485 met our inclusion criteria for the regression analysis. After adjusting for covariates, lung disease type is the one of the most influential factors in place of death. Decedent age, sex, race, ethnicity, marital status, and education level were also significantly associated with location of death (Table 2).
Table 2.
Multivariable Logistic Regression: Decedent Characteristics and Place of Death, 2006-2017 (N = 1,480,485)
| Characteristic | Hospital vs All Other Places | Home vs All Other Places | Nursing Facility vs All Other Places | Hospice Facility vs All Other Places |
|---|---|---|---|---|
| Age, y | ||||
| < 65 | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| 65-74 | 1.06 (1.03-1.09)a | 0.812 (0.803-0.821)a | 1.77 (1.73-1.80)a | 1.46 (1.41-1.50)a |
| 75-84 | 0.879 (0.847-0.913)a | 0.708 (0.684-0.732)a | 3.07 (2.97-3.18)a | 1.64 (1.58-1.71)a |
| ≥ 85 | 0.575 (0.546-0.606)a | 0.578 (0.550-0.608)a | 5.89 (5.62-6.17)a | 1.53 (1.48-1.57)a |
| Sex | ||||
| Female | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Male | 1.03 (1.02-1.04)a | 1.09 (1.08-1.10)a | 0.916 (0.909-0.922)a | 0.904 (0.890-0.918)a |
| Race | ||||
| White | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Black | 1.44 (1.42-1.46)a | 0.724 (0.705-0.744)a | 0.713 (0.685-0.741)a | 0.763 (0.730-0.797)a |
| Native American | 1.24 (1.19-1.29)a | 1.04 (0.989-1.09) | 0.779 (0.726-0.835)a | 0.508 (0.452-0.572)a |
| Asian | 1.63 (1.55-1.71)a | 0.887 (0.842-0.934)b | 0.508 (0.474-0.546)a | 0.592 (0.523-0.670)a |
| Ethnicity | ||||
| Non-Hispanic | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Hispanic | 1.41 (1.37-1.45)a | 0.979 (0.955-1.00) | 0.500 (0.483-0.517)a | 1.05 (1.00-1.09)c |
| Marital status | ||||
| Married | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Not married | 1.21 (1.20-1.23)a | 1.26 (1.24-1.28) | 0.504 (0.489-0.518)a | 1.08 (1.06-1.10)a |
| Education | ||||
| High school or less | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Some college or more | 0.976 (0.969-0.984)a | 1.03 (1.01-1.04)a | 0.903 (0.892-0.915)a | 1.19 (1.16-1.22)a |
| Lung disease | ||||
| COPD | 1 [Ref] | 1 [Ref] | 1 [Ref] | 1 [Ref] |
| Interstitial lung disease | 1.78 (1.70-1.87)a | 0.844 (0.822-0.866)a | 0.537 (0.523-0.552)a | 0.946 (0.921-0.971)a |
| Cystic fibrosis | 4.22 (3.98-4.48)a | 0.407 (0.386-0.431)a | 0.166 (0.126-0.219)a | 0.635 (0.549-0.736)a |
Data are expressed as OR (95% CI). In addition to adjusting for all variables in the table, the models adjusted for year of death.
P < .001.
P < .01.
P < .05.
Odds of hospital and home deaths declined with age while odds of nursing facility and hospice facility deaths increased with age. Decedents aged ≥ 85 years had the greatest odds of nursing facility death relative to younger decedents. Odds of hospice facility death were the greatest among decedents aged ≥ 65 years relative to decedents aged < 65 years. Relative to female decedents, male decedents had increased odds of home death and reduced odds of nursing facility or hospice facility death.
Relative to nonmarried decedents, married decedents had almost 50% lower odds of nursing facility death and increased odds of hospital, home, or hospice facility death. Relative to decedents with less than high school education, decedents with some college education had lower odds of hospital or nursing facility death and increased odds of home and hospice facility death.
Non-white decedents had increased odds of hospital death and reduced rates of nursing and hospice facility death relative to white decedents. For example, black and Asian decedents had 47% and 62% greater odds, respectively, of a hospital death compared with white decedents and reduced odds of home death, nursing facility death, and hospice facility death.
Decedents of Hispanic ethnicity had nearly 40% higher odds of hospital death, greater odds of hospice facility death, and reduced odds of death at home or nursing facility than non-Hispanic subjects.
Discussion
This analysis found that, from 2003 to 2017, the proportion of lung disease deaths occurring in the hospital declined while the proportion occurring at home increased. This move toward deinstitutionalized deaths is also evident in the reduction of deaths occurring in nursing facilities, although there was an increase in the proportion of those dying in hospice facilities. Although home surpassed the hospital as the most common place of death for this population in 2014, this trend was largely driven by deaths caused by COPD. The hospital remains the most common location of death for decedents from ILD or CF. We also found disparities in location of death according to age, race, Hispanic ethnicity, sex, marital status, education level, urban-rural status, and census region. These findings highlight the complex factors that influence where patients with lung disease die yet also offer implications for how to improve end-of-life care for this population.
Over time, the greatest change in place of death was the increase in hospice facility deaths. Although the overall numbers are small, this growth speaks to the increased use of hospice by patients with lung disease.13,19 Among chronic lung disease diagnoses, COPD comprises the greatest proportion of hospice facility deaths, indicating a need to ensure that patients with other lung disease subtypes have access to and are offered hospice. We also found geographic differences in hospice facility deaths, with fewer occurring in rural areas and in the West and Northeast. Although geographic disparities in hospice use among patients with COPD have been previously documented, these findings suggest that access to inpatient hospice may be inequitable and that these gaps should be explored further.13 Because patients receiving care in inpatient hospices are typically experiencing severe symptom burden, the increase in hospice facility deaths is in line with the challenging end-of-life experience for patients with chronic lung disease.4,20,21
A home death will not be appropriate or possible for all individuals. However, because most people with lung disease prefer to die at home, the marked increase in the proportion of home deaths is encouraging.14 Even so, it is important to note that preferred place of death may change with disease progression or if the necessary support to remain at home is lacking.22,23 Because lung disease deaths occur more frequently at home, unpaid caregivers, typically relatives, will be responsible for more and more patient care, making the need for caregiver support more critical. This may explain our finding that married decedents have increased odds of home death relative to nonmarried decedents. Similarly, the increased odds of home death among decedents with greater education, often a proxy for socioeconomic status, may reflect greater financial resources to support a home death.
We also found significant racial differences in place of death, with most non-white decedents experiencing greater odds of hospital deaths and lower odds of home, nursing facility, or hospice facility death. These findings are similar to other research on location of death among other disease groups and are unsurprising given the well-documented underuse of hospice use, advance care planning, and greater preference for aggressive end-of-life care among racial and ethnic minorities.24, 25, 26, 27, 28, 29, 30 These findings reinforce the need to explore culturally tailored strategies for improving the quality of care for these patients.31
The continuously high rate of hospital death among these patients, particularly those with ILD and CF, suggests that more research and clinical interventions are needed to improve end-of-life care in lung disease. A study of all natural deaths in the United States found that a greater proportion of decedents from pulmonary disease die in the hospital than individuals dying of cancer, cardiovascular disease, cerebrovascular disease, or dementia; however, hospital deaths are dropping among all disease groups.32 However, even among lung disease diagnoses, there are striking differences in place of death. Compared with decedents from COPD, a greater proportion of decedents from ILD and CF died in the hospital, and a smaller proportion died at home. The majority of patients with chronic lung disease have COPD; it is therefore understandable that this diagnosis has been the focus on end-of-life research on lung disease. However, the end-of-life experiences of individuals with other lung diseases deserve greater attention.
Patients with chronic lung disease are likely to experience hospitalizations, particularly ICU admissions, at the end of life, which may be both burdensome to the patient and costly to the health-care system.33 These patients often receive life-prolonging interventions in the last 24 h of life.34, 35, 36, 37 Rather than simply responding to acute exacerbations, care for patients with lung disease should follow a previously developed plan for managing their disease and symptoms.33,38 Incorporating palliative care early in the disease course may improve the quality of life and symptom burden of these patients. A study of patients with idiopathic pulmonary fibrosis found that palliative care use was associated with increased likelihood of home or hospice death.39 However, only a minority of patients with chronic lung disease receive formal palliative care referrals, and many of these referrals are only following ICU admission or prior to initiation of hospice.40 In a study of patients with COPD and their caregivers, fewer than one-third of respondents had heard of palliative care.41 After receiving education about palliative care, all respondents voiced belief that palliative care should be integrated earlier in the COPD disease course. Qualitative interviews with patients with end-stage ILD and their caregivers have revealed that most lacked prognostic understanding of their disease and did not engage in end-of-life discussions or planning with each other or with their clinicians.42 Increased palliative care use, advance directive completion, and improved patient-clinician communication may assist patients in understanding the progressive and terminal nature of their disease and improve their end-of-life experience.43,44 A randomized controlled trial of a community-based palliative care intervention has shown promise for improving symptoms and quality of life among patients with ILD, and other innovative care models should be explored.45 Despite such efforts, hospice use among this population is likely to remain low because the current model of hospice, which requires a life expectancy ≤ 6 months and the ceasing of disease-directed therapies, may not fit the disease course and needs of patients with lung disease. In addition, the cost of some symptom-directed treatments exceeds Medicare’s hospice per diem and may be an additional barrier to hospice use for some individuals. Services such as high-flow oxygen can be challenging to provide in home settings and may not be available through all hospices. New models of hospice care for patients with lung disease should be considered.
We believe this study is the first to examine location of death among individuals in the United States with lung disease using national data, but there are several limitations. Although this dataset offers a more complete picture of place of death trends than other sources, errors in death certificate documentation have been documented.46 It is also possible that cause of death documentation may reflect misdiagnosis, not uncommon in patients with asthma and COPD.47,48 In addition, this dataset did not permit determination of hospice use in home or nursing facility settings. Furthermore, our focus on underlying cause of death may have resulted in an undercount of deaths to which chronic lung disease contributed. Finally, we lacked information on individual preferences, which prohibited determination of concordance between preferred and actual place of death.
Conclusions
Given the significant burden of chronic lung disease, attention to the end-of-life needs of this population will grow in importance.49 As more patients with chronic lung die at home, the need to understand their experiences will become more urgent. The substantial physical and existential suffering accompanying these diseases and the impact on caregivers make both palliative care and hospice essential components of care for these patients and an issue of health-care equity.8,50,51 Research should continue to explore barriers to palliative care and hospice for patients with lung disease, and the factors contributing to disparities in place of death should be examined.
Acknowledgments
Author contributions: S. H. C. and H. J. W. take responsibility for (are the guarantors of) the content of the manuscript, including the data and analysis. S. H. C. and H. J. W. contributed to the study concept and design. S. H. C. conducted the statistical analysis. All authors contributed to interpretation of data and writing of the manuscript, and all authors read and approved the final version.
Financial/nonfinancial disclosures: None declared.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Additional information: The e-Figures can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: Dr Kavalieratos receives research funding from the National Institutes of Health [grant K01HL133466] and the Cystic Fibrosis Foundation.
Supplementary Data
References
- 1.National Center for Health Statistics Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- 2.Stapleton R.D., Curtis J.R. End-of-life considerations in older patients who have lung disease. Clin Chest Med. 2007;28(4):801–811, vii. doi: 10.1016/j.ccm.2007.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourke S.J., Peel E.T. Palliative care of chronic progressive lung disease. Clin Med (Lond) 2014;14(1):79–82. doi: 10.7861/clinmedicine.14-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solano J.P., Gomes B., Higginson I.J. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31(1):58–69. doi: 10.1016/j.jpainsymman.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 5.Ahmadi Z., Wysham N.G., Lundstrom S., Janson C., Currow D.C., Ekstrom M. End-of-life care in oxygen-dependent ILD compared with lung cancer: a national population-based study. Thorax. 2016;71(6):510–516. doi: 10.1136/thoraxjnl-2015-207439. [DOI] [PubMed] [Google Scholar]
- 6.Bell C.L., Somogyi-Zalud E., Masaki K.H. Factors associated with congruence between preferred and actual place of death. J Pain Symptom Manage. 2010;39(3):591–604. doi: 10.1016/j.jpainsymman.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kavalieratos D., Corbelli J., Zhang D. Association between palliative care and patient and caregiver outcomes: a systematic review and meta-analysis. JAMA. 2016;316(20):2104–2114. doi: 10.1001/jama.2016.16840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown C.E., Jecker N.S., Curtis J.R. Inadequate palliative care in chronic lung disease. An issue of health care inequality. Ann Am Thorac Soc. 2016;13(3):311–316. doi: 10.1513/AnnalsATS.201510-666PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beernaert K., Cohen J., Deliens L. Referral to palliative care in COPD and other chronic diseases: a population-based study. Respir Med. 2013;107(11):1731–1739. doi: 10.1016/j.rmed.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Burt J., Raine R. The effect of age on referral to and use of specialist palliative care services in adult cancer patients: a systematic review. Age Ageing. 2006;35(5):469–476. doi: 10.1093/ageing/afl001. [DOI] [PubMed] [Google Scholar]
- 11.Rush B., Hertz P., Bond A., McDermid R.C., Celi L.A. Use of palliative care in patients with end-stage COPD and receiving home oxygen: national trends and barriers to care in the United States. Chest. 2017;151(1):41–46. doi: 10.1016/j.chest.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson K.S. Racial and ethnic disparities in palliative care. J Palliat Med. 2013;16(11):1329–1334. doi: 10.1089/jpm.2013.9468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Iyer AS, Goodrich CA, Dransfield MT, et al. End-of-life spending and healthcare utilization among older adults with chronic obstructive pulmonary disease [published online ahead of print December 27, 2019]. Am J Med. 10.1016/j.amjmed.2019.11.024. [DOI] [PMC free article] [PubMed]
- 14.Skorstengaard M.H., Neergaard M.A., Andreassen P. Preferred place of care and death in terminally ill patients with lung and heart disease compared to cancer patients. J Palliat Med. 2017;20(11):1217–1224. doi: 10.1089/jpm.2017.0082. [DOI] [PubMed] [Google Scholar]
- 15.Higginson I.J., Sen-Gupta G.J. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3(3):287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Health Statistics 2017 . National Center for Health Statistics; , Hyattsville, MD: 2017. Data File Documentations. Mortality Multiple Cause-of-Death Public Use Record, 2003-2017. [Google Scholar]
- 17.Centers for Disease Control and Prevention CDC WONDER. https://wonder.cdc.gov
- 18.Ingram D.D., Franco S.J. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;166:1–73. [PubMed] [Google Scholar]
- 19.National Hopsice and Palliative Care Organization . National Hopsice and Palliative Care Organization; Alexandria, VA: 2019. NHPCO Facts and Figures. [Google Scholar]
- 20.Center for Medicare & Medicaid Services. Medicare Benefit Policy Manual. Chapter 9 - Coverage of Hospice Services Under Hospital Insurance. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/bp102c09.pdf. Accessed November 12, 2019.
- 21.Warraich H.J., Xu H., DeVore A.D. Trends in hospice discharge and relative outcomes among Medicare patients in the Get With The Guidelines-Heart Failure Registry. JAMA Cardiol. 2018;3(10):917–926. doi: 10.1001/jamacardio.2018.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gomes B., Calanzani N., Gysels M., Hall S., Higginson I.J. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliat Care. 2013;12:7. doi: 10.1186/1472-684X-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turner V., Flemming K. Socioeconomic factors affecting access to preferred place of death: a qualitative evidence synthesis. Palliat Med. 2019;33(6):607–617. doi: 10.1177/0269216319835146. [DOI] [PubMed] [Google Scholar]
- 24.Cross S.H., Kaufman B.G., Taylor D.H., Jr., Kamal A.H., Warraich H.J. Trends and factors associated with place of death for individuals with dementia in the United States. J Am Geriatr Soc. 2020;68(2):250–255. doi: 10.1111/jgs.16200. [DOI] [PubMed] [Google Scholar]
- 25.Cross S.H., Kaufman B.G., Mentz R.J., Kamal A.H., Taylor D.H., Jr., Warraich H.J. Trends in place of death for individuals with cardiovascular disease in the United States. J Am Coll Cardiol. 2019;74(15):1943–1946. doi: 10.1016/j.jacc.2019.08.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cross S.H., Kaufman B.G., Warraich H.J. Trends in location of death for individuals with cerebrovascular disease in the United States. JAMA Neurol. 2019;76(11):1399–1401. doi: 10.1001/jamaneurol.2019.2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chino F., Kamal A.H., Leblanc T.W., Zafar S.Y., Suneja G., Chino J.P. Place of death for patients with cancer in the United States, 1999 through 2015: racial, age, and geographic disparities. Cancer. 2018;124(22):4408–4419. doi: 10.1002/cncr.31737. [DOI] [PubMed] [Google Scholar]
- 28.Wicher C.P., Meeker M.A. What influences African American end-of-life preferences? J Health Care Poor Underserved. 2012;23(1):28–58. doi: 10.1353/hpu.2012.0027. [DOI] [PubMed] [Google Scholar]
- 29.Greiner K.A., Perera S., Ahluwalia J.S. Hospice usage by minorities in the last year of life: results from the National Mortality Followback Survey. J Am Geriatr Soc. 2003;51(7):970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 30.Welch L.C., Teno J.M., Mor V. End-of-life care in black and white: race matters for medical care of dying patients and their families. J Am Geriatr Soc. 2005;53(7):1145–1153. doi: 10.1111/j.1532-5415.2005.53357.x. [DOI] [PubMed] [Google Scholar]
- 31.Ejem D.B., Barrett N., Rhodes R.L. Reducing disparities in the quality of palliative care for older African Americans through Improved advance care planning: study design and protocol. J Palliat Med. 2019;22(suppl 1):90–100. doi: 10.1089/jpm.2019.0146. [DOI] [PubMed] [Google Scholar]
- 32.Cross S.H., Warraich H.J. Changes in place of death in the United States. N Engl J Med. 2019;381(24):2639–2670. doi: 10.1056/NEJMc1911892. [DOI] [PubMed] [Google Scholar]
- 33.Au D.H., Udris E.M., Fihn S.D., McDonell M.B., Curtis J.R. Differences in health care utilization at the end of life among patients with chronic obstructive pulmonary disease and patients with lung cancer. Arch Intern Med. 2006;166(3):326–331. doi: 10.1001/archinte.166.3.326. [DOI] [PubMed] [Google Scholar]
- 34.Philip J.A., Gold M., Sutherland S. End-of-life care in adults with cystic fibrosis. J Palliat Med. 2008;11(2):198–203. doi: 10.1089/jpm.2007.0106. [DOI] [PubMed] [Google Scholar]
- 35.Rajala K., Lehto J.T., Saarinen M., Sutinen E., Saarto T., Myllarniemi M. End-of-life care of patients with idiopathic pulmonary fibrosis. BMC Palliat Care. 2016;15(1):85. doi: 10.1186/s12904-016-0158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Claessens M.T., Lynn J., Zhong Z. Dying with lung cancer or chronic obstructive pulmonary disease: insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48(suppl 1):S146–S153. doi: 10.1111/j.1532-5415.2000.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 37.Chen E, Homa K, Goggin J, et al. End-of-life practice patterns at U.S. adult cystic fibrosis care centers: a national retrospective chart review. J Cyst Fibros. 2018:17(4):548-554. [DOI] [PubMed]
- 38.Curtis J.R. Palliative and end-of-life care for patients with severe COPD. Eur Respir J. 2008;32(3):796–803. doi: 10.1183/09031936.00126107. [DOI] [PubMed] [Google Scholar]
- 39.Zou R.H., Nouraie M., Chen X. Assessing patterns of palliative care referral and location of death in patients with idiopathic pulmonary fibrosis: a sixteen-year single-center retrospective cohort study. J Palliat Med. 2019;22(5):538–544. doi: 10.1089/jpm.2018.0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindell K.O., Liang Z., Hoffman L.A. Palliative care and location of death in decedents with idiopathic pulmonary fibrosis. Chest. 2015;147(2):423–429. doi: 10.1378/chest.14-1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iyer A.S., Dionne-Odom J.N., Ford S.M. A formative evaluation of patient and family caregiver perspectives on early palliative care in chronic obstructive pulmonary disease across disease severity. Ann Am Thorac Soc. 2019;16(8):1024–1033. doi: 10.1513/AnnalsATS.201902-112OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bajwah S., Koffman J., Higginson I.J. 'I wish I knew more...' the end-of-life planning and information needs for end-stage fibrotic interstitial lung disease: views of patients, carers and health professionals. BMJ Support Palliat Care. 2013;3(1):84–90. doi: 10.1136/bmjspcare-2012-000263. [DOI] [PubMed] [Google Scholar]
- 43.Patel K., Janssen D.J., Curtis J.R. Advance care planning in COPD. Respirology. 2012;17(1):72–78. doi: 10.1111/j.1440-1843.2011.02087.x. [DOI] [PubMed] [Google Scholar]
- 44.Narsavage G.L., Chen Y.J., Korn B., Elk R. The potential of palliative care for patients with respiratory diseases. Breathe (Sheff) 2017;13(4):278–289. doi: 10.1183/20734735.014217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bajwah S., Ross J.R., Wells A.U. Palliative care for patients with advanced fibrotic lung disease: a randomised controlled phase II and feasibility trial of a community case conference intervention. Thorax. 2015;70(9):830–839. doi: 10.1136/thoraxjnl-2014-206583. [DOI] [PubMed] [Google Scholar]
- 46.Drummond M.B., Wise R.A., John M., Zvarich M.T., McGarvey L.P. Accuracy of death certificates in COPD: analysis from the TORCH trial. COPD. 2010;7(3):179–185. doi: 10.3109/15412555.2010.481695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tinkelman D.G., Price D.B., Nordyke R.J., Halbert R.J. Misdiagnosis of COPD and asthma in primary care patients 40 years of age and over. J Asthma. 2006;43(1):75–80. doi: 10.1080/02770900500448738. [DOI] [PubMed] [Google Scholar]
- 48.Heffler E., Crimi C., Mancuso S. Misdiagnosis of asthma and COPD and underuse of spirometry in primary care unselected patients. Respir Med. 2018;142:48–52. doi: 10.1016/j.rmed.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 49.Dwyer-Lindgren L., Bertozzi-Villa A., Stubbs R.W. Trends and patterns of differences in chronic respiratory disease mortality among US counties, 1980-2014. JAMA. 2017;318(12):1136–1149. doi: 10.1001/jama.2017.11747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trandel E.T., Pilewski J.M., Dellon E.P. Symptom burden and unmet existential needs in adults with cystic fibrosis. West J Nurs Res. 2019;41(10):1448–1464. doi: 10.1177/0193945919852585. [DOI] [PubMed] [Google Scholar]
- 51.Bajwah S., Higginson I.J., Ross J.R. The palliative care needs for fibrotic interstitial lung disease: a qualitative study of patients, informal caregivers and health professionals. Palliat Med. 2013;27(9):869–876. doi: 10.1177/0269216313497226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.