Abstract
The 2019 report of a randomized, placebo-controlled clinical trial demonstrating that immune therapy can delay the onset of clinical type 1 diabetes (T1D) in antibody-positive relatives by a median of 2 years stands out as a landmark in the decades-long effort to prevent T1D. With this important step achieved, it is now time to consider what is needed to bring disease-modifying therapy for prevention or delay of T1D to clinical use from this point. Long considered a chicken and egg problem (why screen for T1D risk when we have no therapy, and how can we develop therapies without more screening), we now have the opportunity to break this impasse. The purpose of this article is to place this clinical trial result in context, highlighting key foundational studies leading to this accomplishment, addressing the current gaps, and suggesting that a key next step for prevention of T1D is to screen and monitor relatives for T1D risk in the context of clinical care.
Introduction
The 2019 report of a randomized, placebo-controlled clinical trial demonstrating that immune therapy can delay the onset of clinical type 1 diabetes (T1D) in antibody-positive relatives by a median of 2 years stands out as a landmark in the decades-long effort to prevent T1D (1). The purpose of this article is to place this clinical trial result in context as seen from the perspective of one individual and to suggest a next step in T1D prevention. The first section briefly highlights foundational studies and current status of identification of individuals at risk and then emphasizes the essential role of the immune system and therefore immune therapies in impacting disease course. The second section weaves together future considerations both for identifying those at risk and for providing therapeutic options and suggests that a key next step to preventing T1D is to screen and monitor relatives for risk in the context of clinical care (Fig. 1).
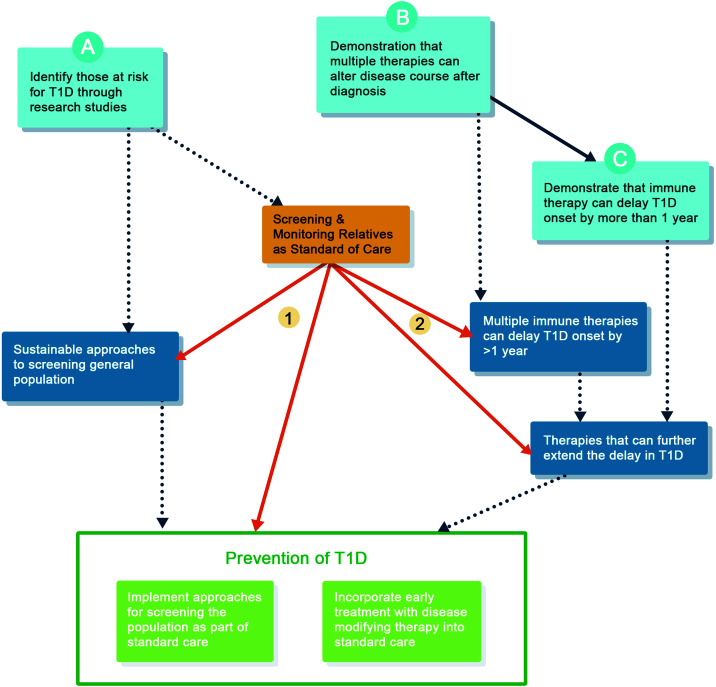
Figure 1.
Key role of screening and monitoring relatives as standard of care to achieve the goal of T1D prevention. Prevention of T1D (green) will ultimately require both implementation of screening programs for the general population and that multiple options for disease-modifying therapy be available as part of standard of clinical care. This will be achieved by building on current accomplishments and interim steps. Current accomplishments (aqua): we currently identify those at risk through research studies (A) and have demonstrated that multiple therapies alter disease course after diagnosis (B), which has led to the demonstration that one therapy can delay T1D by >1 year (C). This conceptual goal has actually been exceeded, as the TrialNet teplizumab trial reported a delay in T1D by a median of 2 years (1). Interim future steps (dark blue): sustainable approaches to screening the general population, demonstrating that multiple therapies can delay T1D, and extending the duration of therapies delaying T1D are interim steps informed by current accomplishments (dotted lines). Key step (orange): screening and monitoring relatives as standard of care is a key step, as it will accelerate (1) development and eventual implementation of general population screening and (2) trial enrollment, and therefore approval for multiple therapies, which will provide the essential justification for screening the general population.
We Can Identify Individuals at Risk for T1D
Almost 50 years have passed since the association of T1D with class II HLA DR3/4, the recognition of increased risk within families, and the first reports of autoantibodies (AAb) notably found prior to clinical diagnosis. Discovery and validation of AAb, in different populations from multiple studies (2–7), continue to refine risk prediction and have led to the conceptual breakthrough that once multiple antibodies are present, T1D almost inevitably follows. Further, when monitored with serial oral glucose tolerance tests, progression proceeds from normal to abnormal (but asymptomatic) glucose tolerance prior to meeting established criteria for T1D diagnosis. This concept has recently been codified as stages of T1D: multiple AAb+ and normal glucose tolerance as stage 1, multiple AAb+ and abnormal glucose tolerance (AGT) as stage 2, and T1D diagnosis as stage 3 (8). The predictability of T1D was initially demonstrated by longitudinal studies in family members and offered the possibility that intervention could prevent disease. While the primary outcome results of the early large, multicenter, prevention trials were negative (2–7), the rate of development of T1D was remarkably similar in multiple settings (Fig. 1, box A).
In parallel to studies in family members, genetic testing of those without family members with disease also proved to be a way to identify individuals who would develop AAb and thus T1D. To make an impact on incidence of disease, such studies are essential; while family members have ∼15× increased relative risk of disease, ∼80% of those with T1D have no affected relatives (9,10). Another advance in identifying at-risk individuals stemmed from the observation from Finland and elsewhere that 95% of children destined to develop T1D by puberty had AAb by age 5 years (11). Ziegler capitalized on this information and initiated a study in Bavaria, Germany, in which children, regardless of familial relationship or HLA type, are tested for AAb at routine pediatric well-child visits (12). As recently reported, 280 multiple AAb+ children have been identified and 43 have developed T1D (13). Since T1D also occurs in older children and through adulthood, additional testing will be needed over time to capture all individuals who will develop disease; yet, this limited study is a beautiful demonstration of the possibilities of this approach.
We Have Demonstrated That Multiple Immune Therapies Can Alter Disease Progression
Given that we can identify individuals destined to develop T1D, which interventions will be effective in slowing or stopping disease progression? Current evidence indicates that immune therapies are essential. The arguments that T1D is an immune-mediated disease are solid: 1) the genetics, where the class II HLA type responsible for antigen recognition is strongly associated with disease (14); 2) the presence of islet antigen–directed AAb, a fundamental component of the autoimmune response, preceding and defining disease (15); and 3) the pathology, whereby immune cell islet infiltrates have been observed in many cadaver specimens of individuals with T1D (16). Collectively, these findings indicate that the immune system plays an essential role in T1D disease progression. Note the phrasing here. The fact that the immune system plays a role in T1D disease progression does not mean that immune system dysfunction is the primary cause of the disease. Indeed, with the exception of rare syndromes of immune system failure such as immunodysregulation polyendocrinopathy enteropathy X-linked (IPEX) syndrome, which results in multiorgan autoimmunity due to a lack of regulatory T cells, it is unknown for T1D and all immune-mediated diseases whether tissue damage is a result of the immune system responding appropriately to cellular injury or foreign insults or occurs in response to the immune system de novo attacking “self.” The important message is that we can alter disease course with immune therapy even without a full understanding of the primary cause(s) of disease; altering disease course is an important and clinically relevant step on the road to prevention. Immune therapy has not yet cured any immune-mediated disease; yet, immune therapy is clinically useful in many disease settings, with significant impact on people’s lives.
Immune Therapy Can Delay Progression to Clinical T1D
In the last dozen years, seven immune therapies have shown effectiveness in preserving β-cell function in phase 2 trials in individuals recently diagnosed with clinical T1D (Table 1). Four, (anti-TNFα, anti-thymocyte globulin, abatacept, and rituximab) are clinically available and widely used in treatment of other immune-mediated diseases (Fig. 1, box B).
Table 1.
Successful fully powered trials of disease-modifying therapy in last 12 years
| Date | Drug | Mechanism of action | Administration | Population (references) |
|---|---|---|---|---|
| 2009/2019 | Teplizumab | T-cell modulation | 14-day i.v. course | N = 76 AAb+ relatives ages 8–50 years (1,38) |
| N = 83 ages 8–30 years, new onset (30) | ||||
| 2009 | Rituximab | B-cell depletion | i.v. course (1/week × 4 weeks) | N = 87 ages 8–40 years, new onset (39) |
| 2011 | Abatacept | Cosimulation blockade | Monthly i.v. infusion | N = 112 ages 6–45 years, new onset (31) |
| 2013 | Alefacept | Target CD2 memory cells | Two 12-week courses of weekly intramuscular injections | N = 49 ages 12–35 years, new onset (40) |
| 2018 | Low-dose anti-thymocyte globulin | T-cell depletion | 2 days i.v. infusion | N = 89 ages 12–45 years, new onset (41) |
| 2020 | Anti–IL-21 (+/– liraglutide) | Anti-cytokine (±GLP1 agonist) | Anti-cytokine therapy i.v. every 6 weeks; GLP-1 s.c. daily | N = 299 ages >20 years, new onset (42) |
| 2020 | Golimumab | Anti-cytokine (anti-TNFα) | s.c. injection every 2 weeks | N = 84 ages 6–21 years, new onset (43) |
It is in this context that the results of the recent Type 1 Diabetes TrialNet study testing teplizumab for prevention of T1D should be considered (1). TrialNet is a National Institutes of Health–funded international clinical trial network aiming to bring disease-modifying therapy into clinical use. This landmark trial showed that treating autoimmunity early can delay the clinical appearance of disease. With a median 2-year delay in disease progression and 25 of 44 treated individuals still without clinical disease at study end (and median delay in disease progression now extended to 3 years in posttrial follow-up), this is a tremendous advance both for T1D and other immune-mediated diseases with a long preclinical period. This delay is clinically important. Despite new technologies, anyone with T1D would agree that any time without clinical T1D, and the 24-7 emotional and fiscal burdens that it entails, is meaningful. Epidemiology data highlight reduced life expectancy with younger age of diagnosis (17), and complications are strongly related to duration of disease (18); thus, a delay in clinical diagnosis also offers the promise of long-term future benefit. In addition to at least 2 years without the direct health care costs of having T1D (estimated in 2020 as $6,288/year [19]), these potential long-term benefits on complications of disease are likely also to reduce the financial burden of the disease. With only a single 2-week course of treatment, this finding is indeed a scientific and clinical breakthrough—fulfilling the promise of decades of research (Fig. 1, box C).
Screening Relatives as Part of Standard of Care: A Key to Prevention
Goal of Screening
The primary goal of screening is to identify those at risk in order to intervene to slow or stop disease progression, as this has the greatest potential for broad benefit. Others have emphasized screening for the purpose of reducing incidence of diabetic ketoacidosis (DKA) at time of diagnosis. In the context of research studies, screening for AAb accompanied by regular oral glucose tolerance test monitoring is dramatically effective and clinically impactful; DKA incidence is reduced from ∼30% to <5% (20,21). These data highlight that in the absence of a screening and monitoring program, ∼70% of people with new-onset T1D will not have DKA at clinical presentation (20,22) and thus will not have this benefit from and monitoring for disease progression. However, all at-risk individuals could potentially benefit from delayed onset of clinical disease with disease-modifying therapy.
There is a compelling case to be made now for screening and monitoring of relatives in the context of clinical care to prevent DKA. Based on the experience from TrialNet in which first-degree relatives to age 45 years and second- and third-degree relatives to age 20 years are tested, screening 100 relatives will identify ∼3 individuals with multiple antibodies who will eventually progress to clinical T1D. Combined with regular monitoring for disease progression, at least one of these three will not develop DKA—a significant clinical benefit. Further, hypothetically, at cost of $50 per screen (100 × $50) and $500 per year for monitoring for 3 years ($500 × 3 × 3 years), the direct costs of screening and monitoring for 100 relatives will be <$10,000 to prevent at least one individual from presenting with DKA, which is much less than the cost of hospitalization due to DKA at diagnosis (23). Thus, the clinical and fiscal case for screening and monitoring relatives as part of clinical care now for the purpose of preventing DKA is clear and should be compelling for clinicians, families, and payors.
Screening and monitoring relatives now as part of clinical care for the purpose of preventing DKA have additional benefits in moving toward prevention of T1D. These include cost-effective paths for clinical trials, as well as an opportunity to test and implement best practices for screening and monitoring.
Cost-effective Paths for Clinical Trials
An interim step to delaying disease progression is to have multiple therapeutic options for patients and clinicians to select the most appropriate therapy for the individual. Bringing new therapies to market requires the involvement of industry. A major challenge for industry is uncertainty about how and when population screening approaches will be part of standard of care. Clarity is needed as to when industry will have access to an at-risk population both to conduct trials and to be assured of a market for future therapies. Screening relatives as part of clinical care for the purpose of preventing DKA is also an efficient approach to increasing the pool of individuals eligible for trials and should therefore meet industry’s needs without excessive cost (Table 2). Thus, there is no need to incur the costs and challenges of screening the general population for the purpose of rapidly enrolling trials at early stages of disease.
Table 2.
Strategies to identify individuals for clinical trials in the U.S.
| Population | Estimated N of population | Estimated average number of relatives | Estimated number to be screened annually | Estimated number with multiple AAb+ | Estimated number willing to enroll* | Theoretical number of trials with N = 300 |
|---|---|---|---|---|---|---|
| Relatives: incidence cases | 40,000 per year | 3 relatives, each age <50 years | 120,000 | 3,000 (120,000 × 2.5%) | If 20% of those eligible enroll, 600 individuals annually | 2 per year |
| Relatives: prevalence cases | 1,500,000 unique families | 2 relatives, each age <50 years | 3,000,000 | >75,000 (3,000,000 × 2.5%) | If 20% of those eligible enroll, 15,000 individuals | 50 |
| General population | 350,000,000 U.S. | N/A | 200,000,000 age <50 years | 800,000 (200,000,000 × 0.4%) | If 10% of those eligible enroll, 80,000 individuals | >260 |
Theoretical number of trials requiring 300 people that could be conducted with different approaches to screening.
*Assumes that fewer individuals without knowledge of T1D will enroll in a prevention trial in comparison with those with family members.
Screening relatives is the shortest and most cost-effective path to enrolling trials. However, this approach does leave uncertainty for industry. If the studies are conducted primarily in at-risk relatives, will the regulatory drug “label” be limited to use in relatives? There is a clear rationale that therapies applied to relatives are equally applicable to those from the general population at similar risk. The literature suggests that the risk for disease progression in multiple antibody-positive individuals is not different among those with and without a family history (24). This evidence supports the decision in TrialNet to enroll both relatives and nonrelatives in prevention trials. In the Fr1da Insulin Intervention study (25), a proportion of children identified in general population screening will be relatives of those with T1D. Collectively, these data could help determine whether response to therapy differs among multiple AAb+ individuals from the general population and those with relatives. Supportive evidence about effectiveness of therapy in at-risk general population and relatives could also come from studies of the same therapy in “new-onset” disease. Since most individuals in new onset trials do not have a relative with disease, demonstration of effectiveness in preserving β-cell function after diagnosis could indicate that the drug is effective in the general population. Combined with recent work illustrating that the rate of fall in insulin secretion in relatives is the same before and after clinical diagnosis (26), results primarily in multiple AAb+ relatives are therefore likely applicable to those from the general population at similar risk. As population screening becomes available, a commitment by industry to do additional trials in the at-risk general population could also be part of the conversation with regulators.
Developing Best Practices for Incorporating Screening Into Clinical Care
Research efforts for screening relatives largely occur through designated centers with expertise in explaining the purpose and results of testing. In the U.S. and Canada, these include (among others) clinical sites participating in TrialNet. TrialNet has recently developed online consent systems along with home or local laboratory testing. In 2020, 65% of individuals screened used this online process. Individuals found to have antibodies are notified by research teams, who explain screening results and outline next steps for monitoring for disease progression and participation in clinical trials. To move screening to routine care, we must address a significant knowledge gap of health care providers. Knowledge about risk among family members and the facts of disease progression are not widely known by both endocrinologists and primary care clinicians, reflecting a profound failure to translate information known for decades to clinical practice. Focusing first on screening relatives, and thus including clinicians caring for people with T1D, provides a platform to aggressively address this gap while evaluating the most effective approaches to education and translation of evidence into clinical practice. Physicians must be comfortable explaining test results (or referring to others for this expertise) before they will incorporate routine screening, psychosocial support, and the essential piece of monitoring into clinical practice. At the same time, the case for insurers and health care systems for screening relatives is stronger, as there is greater potential benefit to the individual; screening relatives is more efficient than screening the general population, leading to less overall screening costs to the system. Once insurers and health systems agree to screen, support, and monitor relatives, the foundation is set for screening the general population.
Expanding Screening to General Population as Part of Clinical Care
Since most people who develop T1D do not have a relative with disease and many do not have known high risk genes, reaching the ultimate goal of preventing or delaying the onset of T1D will eventually require identification of those at risk from the general population (that is, those without genetic risk or family members with T1D). However, moving screening to standard of care in the general population is potentially a more challenging problem at the current time, since 1) the relative risk is 15-fold less than among relatives and thus the individual’s potential benefit is low, 2) the aggregate costs to health systems for screening is high, and 3) many individuals and their physicians may lack existing knowledge about T1D and disease progression. Since the incidence of T1D among those without relatives is 0.3%, the positive predictive value (PPV) of a positive antibody test even with a highly sensitive assay is low. This low PPV could potentially be mitigated by a two-stage screening approach (13), yet the stress for those with a false positive test as well as the additional effort and costs needs to be fully considered (27). Further, the PPV for antibody testing among older individuals in the general population is unknown. Screening the general population first for genetic risk (28), followed by testing for autoantibodies, improves the PPV of a positive antibody test, but like for screening relatives, this approach will miss a considerable number of individuals destined to develop T1D. Work remains to be done to determine what combination and frequency of AAb and genetic screening would be optimal to increase the PPV and negative predictive value and identify those who will and will not develop T1D into adulthood. The considerations above, in addition to the markedly increased direct costs for the large number of people needing to be screened and monitored to identify the few that would benefit, highlight that the case for screening the general population for the purpose of preventing DKA is not compelling at this time.
While getting individuals, physicians, payors, and those setting clinical practice guidelines to incorporate screening relatives as part of routine care will require addressing many of the same hurdles, these challenges are more easily surmountable for this population (Table 3). Importantly, successfully overcoming challenges for implementing routine screening of relatives can accelerate subsequent implementation of routine screening in the general population (29). This includes evaluation of strategies for when (which ages), how often, and what methods for screening and monitoring are “optimal” for identification of both children and adults destined to develop T1D. Moreover, incorporating screening of relatives in clinical practice will accelerate availability of more therapies, as the pool of at-risk individuals would easily be sufficient for conducting multiple clinical trials (Table 2). Thus, continued development of sustainable approaches for screening the general population should continue in parallel with efforts to screen relatives as part of standard of care.
Table 3.
Gaps in transitioning research to clinical care
| Science alone is insufficient. Gaps to be addressed in transitioning research to clinical care for T1D prevention |
|---|
| Challenges applicable to screening and monitoring both relatives and the general population. Efforts in relatives can inform work in the general population |
| • Routine clinical laboratory processes for assays validated to predict risk |
| • Linking screening with follow-up monitoring and social/emotional support within clinical practice |
| • Education about risk: clinicians, insurers, health systems, families, screened individuals |
| • Determine the “optimal” ages, frequency, and methods for screening and monitoring for disease progression for children and adults |
| • Address costs |
| Challenges applicable to any immune therapy approved for T1D prevention |
| • Endocrinologists trained in use of immune therapy or use of expert centers, referrals to nonendocrinology colleagues |
| • Education about risks/benefits of therapy: individuals at risk, primary care clinicians, insurers |
| • Address costs |
Interim Steps to Prevention: Therapies
With capitalizing on our ability to identify those at risk for disease and the identification of multiple immune agents that impact disease course after diagnosis, additional steps are readily apparent on the path to clinical use of therapy to slow or stop T1D. As illustrated (Fig. 1), these include demonstrating that multiple therapies can delay clinical T1D and, separately, that therapy can increase the duration of disease delay. Notably absent from this illustration is an explicit step for a short-term therapy that indefinitely stops disease progression—this ultimate aim of achieving immune tolerance will trump existing therapy. However, it is likely to come after other approaches are clinically available.
Next Steps for Teplizumab
The demonstration that teplizumab can delay progression to clinical onset raises scientific and clinically relevant questions. What is the duration of the therapeutic effect? Will repeat treatment keep clinical disease safely at bay indefinitely? What accounts for the degree of effect in an individual? Can an individual’s response to therapy be predicted?
In a broader sense, these trial results raise the question of whether delay of the disease depends on when in disease course the drug is given. Previous studies with teplizumab have demonstrated that it can preserve β-cell function when administered shortly after diagnosis (30). In the recent trial, the drug was given at stage 2 disease to participants with multiple antibodies and AGT (1). Within 2 years, 50% of the placebo group progressed to clinical T1D; thus, the TrialNet prevention trial demonstrated efficacy in altering disease course during a time of rapid progression. Whether teplizumab would be effective at earlier stages of disease is unknown, but answering this question will provide essential information for design of future studies.
Moving Other Disease-Modifying Therapies to Prevention
Demonstrating that any or all of these other agents are effective in delaying progression to clinical disease opens a broader path for future clinical options for patients. Indeed, abatacept (CTLA4-Ig) may be the first agent tested in all three stages of disease. The new onset trial demonstrated efficacy in preserving β-cell function (31), recruitment is complete on the abatacept prevention trial in those with stage 1 T1D (multiple AAb+ and normal glucose tolerance) with outcome data expected in 2021 (32), and a trial of abatacept in combination with rituximab in stage 2 T1D (multiple AAb+ and AGT) had been launched but is currently on hold due to the uncertain impact of the coronavirus disease 2019 (COVID-19) pandemic on risk of study participation (33). Comparing clinical results and immune response from the same drug at different stages of disease is likely to provide important insights as to when to treat.
The framework described above is, first, to demonstrate effectiveness in disease modification in new-onset disease and then test for prevention at earlier disease stages. This is a product of the time in which such studies were designed. The first immune therapy trials were conducted before the inevitability of disease progression in multiple AAb+ individuals was fully known, and there was understandable reluctance to test therapies in an at-risk population including otherwise “healthy” children without strong evidence supporting “prospect of benefit” and understanding of potential harm. However, newer immunotherapeutics with better safety profiles are routinely used in children with other autoimmune diseases and it is now clear that multiple AAb+ individuals have the initial stages of a disease leading to clinical T1D. Therefore, it is not unreasonable to propose that standard dosing regimens of immune therapies in clinical use in other immune-mediated diseases could be tested directly in earlier stages of T1D without doing studies in new onset populations. This approach could both shorten the time to evaluate the spectrum of therapies in early disease and guard against a more significant problem, namely, that therapies may be effective only if given earlier. Placing the hurdle of a “positive” new onset trial before testing in prevention may lead to discarding otherwise promising “standard” approaches. For example, the anti-IL1 therapies anakinra and canakinumab were ineffective in new-onset disease (34). The hurdle of now testing these therapies, which have a reasonable safety profile, in earlier disease is significant despite emerging data suggesting a role for the innate immune system long before clinical diagnosis. This approach is not without precedent; given reasonable scientific rationale and reasonable safety profiles, nicotinamide (3), parenteral insulin (2), oral and nasal insulin (4–6), and hydroxychloroquine (35) were all brought to trial in prevention without positive fully powered trials in new-onset disease.
Keeping Success From Creating a Roadblock for Choice
The impressive results from the TrialNet teplizumab prevention study take us to a new era. Yet, teplizumab does not cure T1D. The TrialNet prevention study was small, involving only 76 individuals. As with all therapies, not everyone responds to the drug; while 16 of 32 placebo-treated individuals developed T1D within 2 years of randomization, 11 of the 44 treated with teplizumab also progressed to clinical T1D during this time period. Moreover, even when it is clinically available, not everyone will want to take this drug, which carries the burden of 12–14 sequential days of i.v. infusion.
Key is to assure that other drugs will eventually be available for clinicians and individuals to choose from, and this will require additional clinical trials. How might clinical approval of teplizumab in prevention impact the ability of other therapies to be studied or approved? If teplizumab is approved, it is possible that individuals would be less willing to enroll in a trial at all—and instead would opt for treatment as part of clinical care. They may also be less willing to receive a placebo. Future trials may wish (or be required) to involve teplizumab as an active comparator. These studies would likely be designed as noninferiority studies (36), aimed to demonstrate that the new drug is not substantially worse than teplizumab, and will require larger numbers of participants than placebo-controlled studies. For example, with a noninferiority margin of 1.5 (indicating that the new therapy would be considered noninferior if the outcome is 1.5 times worse than teplizumab), a trial with 80% power and α of 0.050 would require >350 participants. Such challenges are not new to medicine, but the success of the teplizumab prevention trial makes these challenges new to T1D prevention—a challenge that could be addressed through rapidly bringing screening and monitoring of relatives to clinical care and thus increasing the pool of potentially eligible individuals for trials. Cooperative approaches across industry and academia and consideration of innovative study designs with shared placebo groups will be needed until identifying those at risk becomes standard of care.
On a Slower Road to Clinical Application
The above discussion focuses on therapies with a potentially straightforward road to clinical use: single broad immunosuppression drugs demonstrated to slow disease progression in a population of individuals at risk for T1D. Pursuing this path can accelerate progress on more difficult, likely slower routes to clinical translation; these include combination in lieu of single agents, cellular therapy, antigen and nonimmune therapies as compared with broad immune suppression, β-cell directed therapies, and personalized approaches.
Conclusion
The field is poised to deliver on the promise of delaying or preventing T1D and incorporating population-wide screening and early treatment into standard of care having met many, but not all, of the Wilson-Jungner criteria for screening proposed in 1968 (37). Screening and monitoring relatives as standard of care for the purpose of preventing DKA constitute a key next step, and using existing immune therapies can accelerate clinical trials and lead to shorter paths for prevention (Table 4). At these early stages of transitioning from research to clinical care, public/private cooperation is essential to earn and sustain the trust of clinicians and those living with and at risk for T1D. Together, we can transparently describe the path to prevention recognizing the tremendous progress made as well as the distance yet to travel.
Table 4.
Key messages
| • The premise underlying this article is that to prevent or delay the onset of T1D we will eventually need to incorporate screening for T1D risk in those with and without family members who have T1D and we will need to have effective therapies with a reasonable safety profile to use in clinical care. |
| • The rationale for incorporating screening programs in those without family members as part of clinical care at this time is weak. Without therapies, the only clinical benefit that is possible from screening and monitoring is reduction of DKA at time of diagnosis. The low prevalence of T1D in the general population means that even a very highly sensitive screening test will have a low PPV. The costs of screening will be high in aggregate and the benefit to an individual low. The potential “harm” of this approach is both the significant costs of screening and monitoring and the psychological stress on the individual/family, particularly if there is a lack of knowledge among clinicians for how to provide interpretation and support. |
| • In contrast, reducing DKA through screening and monitoring programs among those with a relative with T1D is a reasonable and achievable goal at this time. Since there are fewer relatives to screen, the aggregate costs to the health care system are less. With a 1 in 20 risk for T1D, the predictive value of a positive test is much higher and thus the potential benefit to the individual is higher. Screening and monitoring of relatives as standard of care would reduce DKA at diagnosis dramatically in relatives at risk for disease. |
| • At the same time, additional benefits will accrue through this effort to bring screening and monitoring relatives to clinical care. These include creating a competitive marketplace to develop and implement better (easier and cheaper) screening and monitoring approaches and providing “real-world” evidence of the processes, costs, benefits, and harms of screening that will be needed to expand from testing relatives to testing the general population as part of clinical care. |
| • Critically, screening relatives as part of clinical care will address the concern of industry about the feasibility of developing therapies to prevent or delay T1D. The number of individuals who will be identified through widespread screening of relatives will be sufficient for conducting multiple clinical trials. Positive results in such trials will eventually lead to a clinical indication of such therapies in prevention and thus provide the essential piece to someday justify screening the population without relatives with T1D as part of clinical care. |
Article Information
Acknowledgments. The author is grateful for members of Benaroya Research Institute (BRI) faculty, Cate Speake and Tee Bahnson for critical review and suggestions for the manuscript, Anna Bjork for assistance with figures, and Anne Hocking, Colin O’Rourke, and Alyssa Ylescupidez for editing (all at BRI). The author also acknowledges that the concepts presented herein have evolved over many years through conversations with academic colleagues, members of nonprofit advocacy groups, and industry.
Funding. Support for this work was from Benaroya Research Institute Member working fund.
Duality of Interest. C.J.G. consulted with VielaBio this past year, received in-kind support for ongoing research studies from Bristol-Myers Squibb and Janssen, and has been a site principal investigator for clinical trials by Pfizer, Provention Bio, and ActoBio. No other potential conflicts of interest relevant to this article were reported.
All of the opinions expressed are entirely those of the author.
References
- 1. Herold KC, Bundy BN, Long SA, et al.; Type 1 Diabetes TrialNet Study Group. An anti-CD3 antibody, teplizumab, in relatives at risk for type 1 diabetes. N Engl J Med 2019;381:603–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diabetes Prevention Trial--Type 1 Diabetes Study Group. Effects of insulin in relatives of patients with type 1 diabetes mellitus. N Engl J Med 2002;346:1685–1691 [DOI] [PubMed] [Google Scholar]
- 3. Gale EA, Bingley PJ, Emmett CL; European Nicotinamide Diabetes Intervention Trial (ENDIT) Group. European Nicotinamide Diabetes Intervention Trial (ENDIT): a randomised controlled trial of intervention before the onset of type 1 diabetes. Lancet 2004;363:925–931 [DOI] [PubMed] [Google Scholar]
- 4.The Diabetes Prevention Trial-Type 1 Study Group. Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial–Type 1. Diabetes Care 2005;28:1068–1076 [DOI] [PubMed] [Google Scholar]
- 5. Näntö-Salonen K, Kupila A, Simell S, et al. Nasal insulin to prevent type 1 diabetes in children with HLA genotypes and autoantibodies conferring increased risk of disease: a double-blind, randomised controlled trial. Lancet 2008;372:1746–1755 [DOI] [PubMed] [Google Scholar]
- 6. Krischer JP, Schatz DA, Bundy B, Skyler JS; Writing Committee for the Type 1 Diabetes TrialNet Oral Insulin Study Group. Effect of oral insulin on prevention of diabetes in relatives of patients with type 1 diabetes: a randomized clinical trial. JAMA 2017;318:1891–1902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Knip M, Akerblom HK, Al Taji E, et al.; Writing Group for the TRIGR Study Group. Effect of hydrolyzed infant formula vs conventional formula on risk of type 1 diabetes: the TRIGR randomized clinical trial. JAMA 2018;319:38–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care 2015;38:1964–1974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dahlquist G, Blom L, Holmgren G, et al. The epidemiology of diabetes in Swedish children 0-14 years--a six-year prospective study. Diabetologia 1985;28:802–808 [DOI] [PubMed] [Google Scholar]
- 10. Allen C, Palta M, D’Alessio DJ.. Risk of diabetes in siblings and other relatives of IDDM subjects. Diabetes 1991;40:831–836 [DOI] [PubMed] [Google Scholar]
- 11. Parikka V, Näntö-Salonen K, Saarinen M, et al. Early seroconversion and rapidly increasing autoantibody concentrations predict prepubertal manifestation of type 1 diabetes in children at genetic risk. Diabetologia 2012;55:1926–1936 [DOI] [PubMed] [Google Scholar]
- 12. Raab J, Haupt F, Scholz M, et al.; Fr1da Study Group. Capillary blood islet autoantibody screening for identifying pre-type 1 diabetes in the general population: design and initial results of the Fr1da study. BMJ Open 2016;6:e011144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ziegler AG, Kick K, Bonifacio E, et al.; Fr1da Study Group. Yield of a public health screening of children for islet autoantibodies in Bavaria, Germany. JAMA 2020;323:339–351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Concannon P, Rich SS, Nepom GT.. Genetics of type 1A diabetes. N Engl J Med 2009;360:1646–1654 [DOI] [PubMed] [Google Scholar]
- 15. Skyler JS, Bakris GL, Bonifacio E, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes 2017;66:241–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Campbell-Thompson M, Fu A, Kaddis JS, et al. Insulitis and β-cell mass in the natural history of type 1 diabetes. Diabetes 2016;65:719–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rawshani A, Sattar N, Franzén S, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet 2018;392:477–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group; Nathan DM, Zinman B, Cleary PA, et al. Modern-day clinical course of type 1 diabetes mellitus after 30 years’ duration: the diabetes control and complications trial/epidemiology of diabetes interventions and complications and Pittsburgh epidemiology of diabetes complications experience (1983-2005). Arch Intern Med 2009;169:1307–1316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tao B, Pietropaolo M, Atkinson M, Schatz D, Taylor D.. Estimating the cost of type 1 diabetes in the U.S.: a propensity score matching method. PLoS One 2010;5:e11501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Winkler C, Schober E, Ziegler AG, Holl RW.. Markedly reduced rate of diabetic ketoacidosis at onset of type 1 diabetes in relatives screened for islet autoantibodies. Pediatr Diabetes 2012;13:308–313 [DOI] [PubMed] [Google Scholar]
- 21. Triolo TM, Chase HP, Barker JM; DPT-1 Study Group. Diabetic subjects diagnosed through the Diabetes Prevention Trial–Type 1 (DPT-1) are often asymptomatic with normal A1C at diabetes onset. Diabetes Care 2009;32:769–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rewers A, Klingensmith G, Davis C, et al. Presence of diabetic ketoacidosis at diagnosis of diabetes mellitus in youth: the Search for Diabetes in Youth Study. Pediatrics 2008;121:e1258–e1266 [DOI] [PubMed] [Google Scholar]
- 23. Desai D, Mehta D, Mathias P, Menon G, Schubart UK.. Health care utilization and burden of diabetic ketoacidosis in the U.S. over the past decade: a nationwide analysis. Diabetes Care 2018;41:1631–1638 [DOI] [PubMed] [Google Scholar]
- 24. Krischer JP, Liu X, Lernmark Å, et al.; TEDDY Study Group. The influence of type 1 diabetes genetic susceptibility regions, age, sex, and family history on the progression from multiple autoantibodies to type 1 diabetes: a TEDDY study report. Diabetes 2017;66:3122–3129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Technische Universität München. Fr1da Insulin Intervention. ClinicalTrials.gov. NLM Identifier: NCT02620072. Accessed 1 February 2021. Available from https://clinicaltrials.gov/ct2/show/NCT02620072
- 26. Bogun MM, Bundy BN, Goland RS, Greenbaum CJ.. C-peptide levels in subjects followed longitudinally before and after type 1 diabetes diagnosis in TrialNet. Diabetes Care 2020;43:1836–1842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health 2017;5:307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ziegler AG, Danne T, Dunger DB, et al. Primary prevention of beta-cell autoimmunity and type 1 diabetes - the Global Platform for the Prevention of Autoimmune Diabetes (GPPAD) perspectives. Mol Metab 2016;5:255–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dunne JL, Koralova A, Sutphin J, et al. Parent and pediatrician preferences for type 1 diabetes screening in the U.S. Diabetes Care 2021;44:332–339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Herold KC, Gitelman SE, Ehlers MR, et al.; AbATE Study Team. Teplizumab (anti-CD3 mAb) treatment preserves C-peptide responses in patients with new-onset type 1 diabetes in a randomized controlled trial: metabolic and immunologic features at baseline identify a subgroup of responders. Diabetes 2013;62:3766–3774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Orban T, Bundy B, Becker DJ, et al.; Type 1 Diabetes TrialNet Abatacept Study Group. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet 2011;378:412–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Institute of Diabetes and Digestive and Kidney Diseases. CTLA4-Ig (Abatacept) for Prevention of Abnormal Glucose Tolerance and Diabetes in Relatives At-Risk for Type 1. ClinicalTrials.gov. NLM Identifier: NCT01773707. Accessed 1 February 2021. Available from https://www.clinicaltrials.gov/ct2/show/NCT01773707
- 33.National Institute of Diabetes and Digestive and Kidney Diseases. Rituximab and Abatacept for Prevention or Reversal of Type 1 Diabetes (TN25). ClinicalTrials.gov. NLM Identifier: NCT03929601. Accessed 1 February 2021. Available from https://clinicaltrials.gov/ct2/show/NCT03929601
- 34. Moran A, Bundy B, Becker DJ, et al.; Type 1 Diabetes TrialNet Canakinumab Study Group; AIDA Study Group. Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet 2013;381:1905–1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Institute of Diabetes and Digestive and Kidney Diseases. Hydroxychloroquine in Individuals At-Tisk for Type 1 Diabetes Mellitus (TN-22). ClinicalTrials.gov. NLM Identifier: NCT03428945. Accessed 1 February 2021. Available from https://clinicaltrials.gov/ct2/show/NCT03428945
- 36. Mauri L, D’Agostino RB Sr.. Challenges in the design and interpretation of noninferiority trials. N Engl J Med 2017;377:1357–1367 [DOI] [PubMed] [Google Scholar]
- 37. Wilson JMG, Jungner G.. Principles and Practices of Screening for Disease. Geneva, World Health Org., 1968. [Google Scholar]
- 38. Herold KC, Gitelman S, Greenbaum C, et al.; Immune Tolerance Network ITN007AI Study Group. Treatment of patients with new onset type 1 diabetes with a single course of anti-CD3 mAb teplizumab preserves insulin production for up to 5 years. Clin Immunol 2009;132:166–173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pescovitz MD, Greenbaum CJ, Krause-Steinrauf H, et al.; Type 1 Diabetes TrialNet Anti-CD20 Study Group. Rituximab, B-lymphocyte depletion, and preservation of beta-cell function. N Engl J Med 2009;361:2143–2152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rigby MR, DiMeglio LA, Rendell MS, et al.; T1DAL Study Team. Targeting of memory T cells with alefacept in new-onset type 1 diabetes (T1DAL study): 12 month results of a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Diabetes Endocrinol 2013;1:284–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Haller MJ, Schatz DA, Skyler JS, et al.; Type 1 Diabetes TrialNet ATG-GCSF Study Group. Low-dose anti-thymocyte globulin (ATG) preserves β-cell function and improves HbA1c in new-onset type 1 diabetes. Diabetes Care 2018;41:1917–1925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Von Herrath MG, Bain SC, Bode BW, et al. Efficacy and safety of anti-interleukin (IL)-21 in combination with liraglutide in adults recently diagnosed with type 1 diabetes. Diabetes 2020;69(Suppl. 1):278-OR
- 43. Quattrin T, Haller MJ, Steck AK, et al.; T1GER Study Investigators. Golimumab and beta-cell function in youth with new-onset type 1 diabetes. N Engl J Med 2020;383:2007–2017 [DOI] [PubMed] [Google Scholar]