Abstract
Objectives:
To determine upper incisor root resorption, volume loss, and the relationship between root volume loss and tooth movement after 1 year of orthodontic treatment in patients with marginal bone loss.
Materials and Methods:
A total of 30 women (46.3 ± 5.4 years old) with moderate upper incisor bone loss who required intrusion during orthodontic treatment were recruited. Pre- and post-treatment cone beam computed tomography images were reconstructed. Upper incisors at pre- and post-treatment were superimposed; labio- and palato-apical, middle, and coronal third root volumes were assessed. Tooth movement and alveolar bone height were measured from lateral cephalometric radiographs and cone beam computed tomography. Changes in root volume/alveolar bone height were compared using paired-sample t-tests, percentage root volume loss for each tooth/segment was evaluated by one-way analysis of variance, and the relationship between percentage root loss and degree of tooth movement was assessed by linear regression.
Results:
Mean root volume significantly decreased on the labio- and palato-apical aspects of 12 and labio-apical aspects of 21 and 22 (P ≤ .024). Palato-apical segment volume loss was greater on lateral than central incisors (P ≤ .016). Two-dimensional root length and cementoenamel junction-bone crest distance did not change between T0 and T1, with no significant relationship between tooth movement amount and percentage root volume loss.
Conclusions:
Delivery of 40 g intrusive force to the four upper incisors using a T-loop and the leveling phase lead to more apical root volume loss on lateral than central incisors. There was no relationship between extent of tooth movement and upper incisor root volume loss.
Keywords: Adult treatment, CT, Root resorption, Three-dimensional
INTRODUCTION
Esthetic problems, such as tooth elongation, migration, and upper incisor spacing, lead individuals with periodontitis to seek orthodontic care.1 To correct these issues, orthodontic force combined with labial root torque is applied to induce upper incisor intrusion and palatal crown tipping.2
External root resorption is common during orthodontic treatment, especially in patients with marginal bone loss, and can be severe.3–5 Several factors have been associated with root resorption, including duration of treatment,6 type and magnitude of force,7,8 and amount of tooth movement.9 Intrusive movement has been associated with a high risk of root resorption10 due to compression of the root apex and periodontium.11 The amount of intrusion does not necessarily correlate with root resorption.12–14 However, the relationship between movement of the apex and apical root resorption was confirmed in a meta-analysis.4,15–17
Because patients with periodontitis have reduced bony support, stress distribution may vary and lead to different extents of root resorption during orthodontic treatment. The optimal force for patients with normal bone support may be too high for patients with marginal bone loss. According to Schwartz,18 forces >20 to 26 g/cm2 may cause root resorption due to periodontal ischemia. Heavy forces induce more root resorption than light forces or control treatments.10,19,20 Most previous studies were based on conventional radiography, which may over- or underestimate root resorption; three-dimensional (3D) cone beam computed tomography (CBCT) is more accurate.21
This study investigated the incidence and severity of upper incisor root resorption and volume loss and assessed the relationship between root volume loss and apical movement using CBCT in patients with marginal bone loss after 1 year of orthodontic treatment with 40 g intrusive force.
MATERIALS AND METHODS
Participants and Treatment
This study was approved by Prince of Songkla University Faculty of Dentistry ethics committee (0521.1.03/573). A total of 30 women were recruited. Inclusion criteria were (a) age 40 to 55 years, (b) 3 to 5 mm radiographic bone loss (from cementoenamel junction [CEJ] to alveolar bone), (c) maxillary incisor intrusion required, (d) nonextraction treatment, and (e) no crowding of upper anterior teeth. Exclusion criteria were (a) history of trauma or endodontic treatment on maxillary incisors, (b) receiving systemic medical treatment, or (c) poor oral hygiene.
Sample size was calculated using PS Power and Sample Size Calculation software (version 3.0.43; Vanderbilt University, Nashville, Tenn). Based on a mean ± standard deviation difference in root volume22 of 13.12 ± 25.37 mm,3 significance of 95% (α = .05), and 80% power (β = .2), the minimum sample size required for paired t-tests was 29.
All patients received periodontal treatment before orthodontic treatment. Fixed appliances were inserted within 1 month after periodontal recall. All patients had a full mouth plaque index ≤ 123 with no bleeding on probing. Periodontal maintenance with a periodontist (M.W.) was scheduled every 3 months.
Orthodontic treatment began with placement of conventional brackets (Roth system; Ormco, Orange, Calif) with 0.018-inch slots on incisors and 0.022-inch slots on canines and posterior teeth. Initial leveling and alignment were accomplished using 0.012, 0.014, 0.016, 0.016 × 0.016-inch nickel titanium and 0.016 × 0.016-inch stainless steel wires. Intrusive force (40 g)24 was applied using a 0.016 × 0.022-inch Titanium molybdenum alloy (TMA) wire with T-loops stepped gingivally between canines and lateral incisors; wires were checked/reactivated monthly. Force magnitude between upper central incisors was verified using a force gauge (Ortho Organizers, Inc., San Marcos, Calif). A typodont (Ormco) was used to verify the force at the central and lateral incisors prior to clinical application.
CBCT and Lateral Cephalometric Analysis
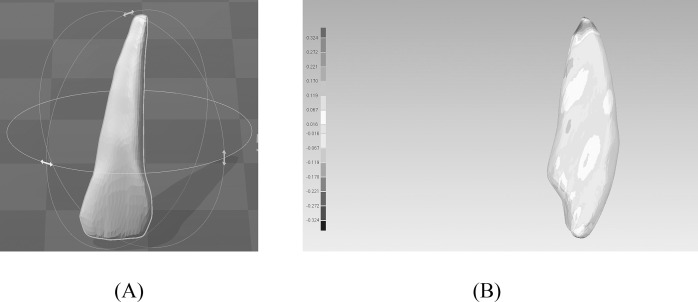
Lateral cephalograms and limited field-of-view CBCT images were taken at pretreatment (T0) and after 1 year (T1). CBCT was performed at 80 kV, 5 mA, 7.5-second exposure, 0.125 mm voxel resolution, and 80 × 40 mm field of view (Veraviewepocs J Morita MPG, Fushimi-ku, Kyoto, Japan) and reconstructed at 0.125-mm increments. Root length and 3D tooth positions (x-, y-, z-dimensions) within the dental arch were determined by fixing central points of the upper central and lateral incisors; axial slices were set perpendicular to the long axis of the root. To visualize the axial, coronal, and sagittal root planes, the first reference line was placed between the labial and palatal CEJ. A second parallel reference line was placed at the root apex (Figure 1A). Upper incisor root length was measured along the root axis perpendicular to the imaginary line between the labial and palatal CEJ and most apical part of the root (Figure 1B).25 To measure alveolar bone height, the vertical linear distance (z-dimension) between the CEJ and the upper central and lateral incisor alveolar bone crests was measured. The corresponding distances were obtained for the mesial, distal, labial and palatal bone levels (Figure 1C).25
Figure 1.
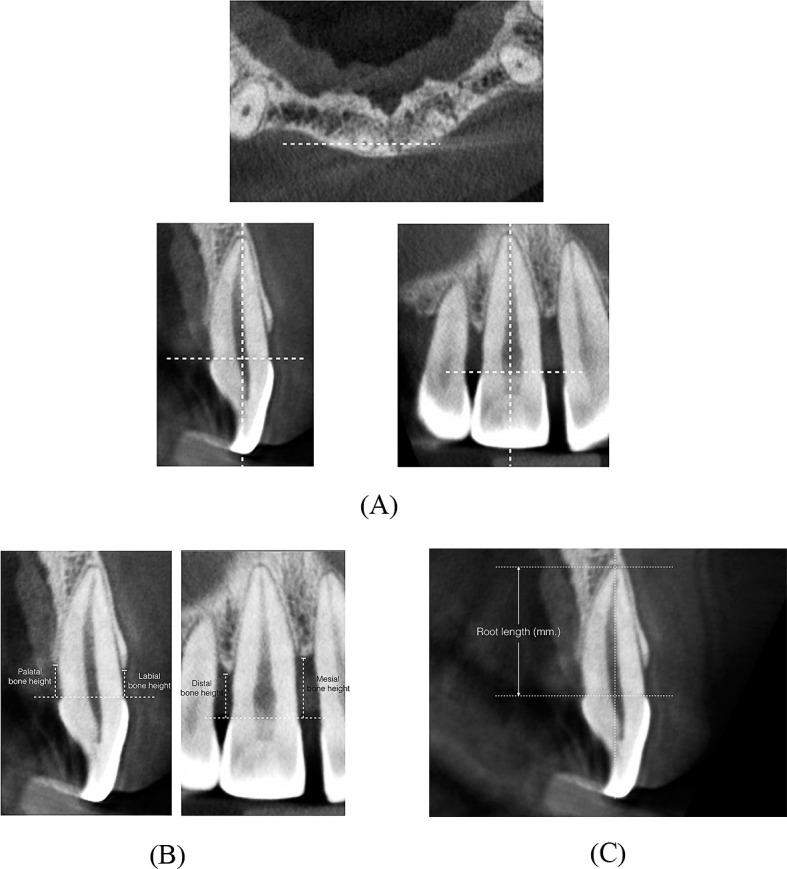
(A) Three-dimensional position of upper incisors and measurement (B) of alveolar bone crest and (C) root length on cone beam computed tomography images.
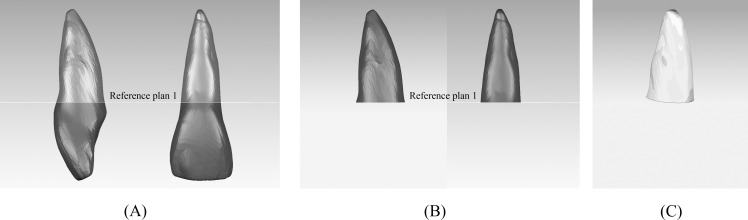
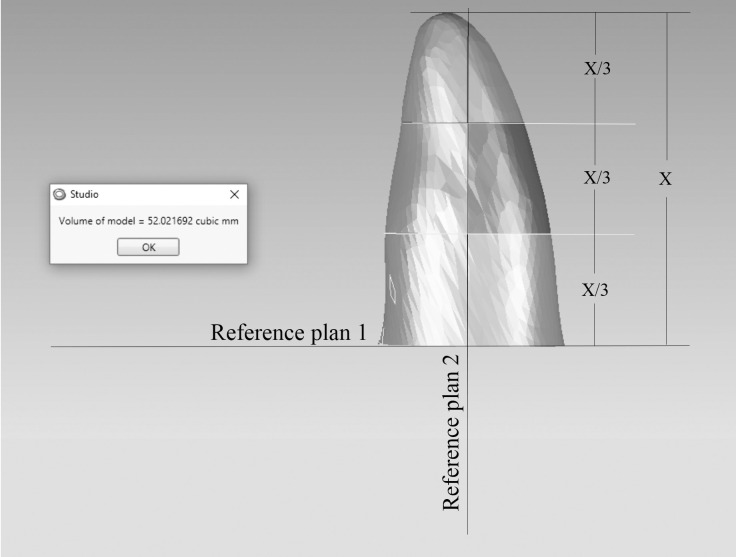
DICOM (Digital Imaging and Communications in Medicine) datasets were imported into ITK-Snap software (version 3.2, http://www.itksnap.org) to generate stereolithographic (STL) data (Figure 2A).26 The radiographer assigned a number to each STL image; the primary investigator (P.P.) was blinded to the codes. The 144 corresponding STL images for T0 and T1 were imported into Geomagic (Geomagic, Cary, N.C.) and superimposed by the best fit alignment of T0 to T1 images using an iterative closest point algorithm27 (Figure 2B). Reference plane 1 was constructed between the highest point of the labial and palatal CEJ. T0 to T1 STL images were segmented immediately below reference plane 1, and the root portion was analyzed (Figure 3). The roots were segmented into anteroposterior, labial, and palatal aspects using the mid-point between the labial and palatal CEJ and the line perpendicular to reference plane 1 as reference points (reference plane 2). In the vertical dimension, the roots were separated into cervical, middle, and coronal thirds (lengths) along reference plane 2 and three planes parallel to reference plane 1 (ie, six segments: labio- and palato-apical, middle, and coronal thirds). Root volumes were computed using Geomagic software (Figure 4). Measurements were performed twice by the same blinded investigator (in a dark room) at least 4 weeks apart and averaged. Root volume loss was determined as the difference between T0 and T1. The percentage of root volume loss22 was calculated as:
Figure 2.
(A) Stereolithography (STL) images of a three-dimensional model of the incisor. (B) Mesial color map of registered pre- and posttreatment (T0, T1) images. Colors illustrate surface match between images. Maximum linear change on palato-apical aspect of root was recorded as 0.324 mm over resorption area (a).
Figure 3.
(A) Reference plane 1 (highest point of labial to palatal cementoenamel junction [CEJ]). (B) Pre- and posttreatment (T0, T1) root portion segmented below reference plane 1. (C) Superimposed root images at T0 and T1-mesial palatal color map view.
Figure 4.
Roots were segmented into six portions (reference plane 2, mid-point between labial and palatal palatal cementoenamel junction [CEJ] to line perpendicular to reference plane 1; X, root length), and mesio-palatal aspect root volumes were computed.
Lateral cephalometric radiographs were taken at T0 and T1. The right upper central and lateral incisors were identified by comparing crown inclination with dental casts. The center of resistance of the central incisor (midpoint of root in alveolar bone) and teeth were copied from T0 to T1 images based on palatal fit and the key ridges. Tooth movement was measured as shown in Figure 5.14
Figure 5.
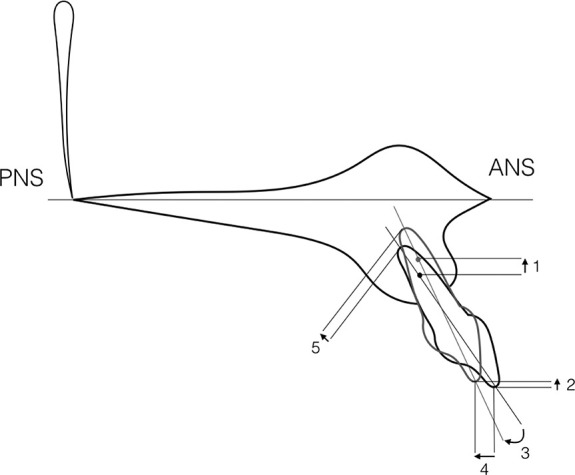
Measurement of right upper central incisor movement from lateral cephalometric superimpositions (using palatal plane as a horizontal reference). (1) Intrusion (vertical movement of center of resistance [CR]), (2) vertical change of incisal edge, (3) change in inclination, (4) anteroposterior change of incisal edge, and (5) linear movement of apex.
Statistical Analyses
Error was assessed using Dahlberg's formula, within-observer repeatability, intraclass correlation coefficients. The result of the Shapiro-Wilks test was not statistically significant.
Paired t-tests were used to compare mean root volume at T0 and T1 and one-way analysis of variance and the post-hoc Tukey's honesty least significant difference test for root volume changes and percentage root loss between all incisors and different root segments. The relationships between percentage root loss and tooth movement on lateral cephalometric radiographs were examined using linear regression. Data were analyzed using R software (The Comprehensive R Archive Network, www.r-project.org); P < .05 was considered significant.
RESULTS
A total of 30 female patients aged 46.3 ± 5.4 years (range 40–55) were assessed. Paired t-tests indicated that replicate measurements of root volume and bone height from CBCT for each patient by the same investigator were reliable. The intraclass correlation coefficient was >.90 for all measurements. Intrusive force was 53, 45.3, 45.3, and 53 g for teeth 12, 11, 21, and 22, respectively. Right upper central and lateral incisor movement between T0 and T1 is summarized in Table 1.
Table 1.
Movement of the Upper Central and Lateral Incisors Between Pre- and Posttreatment
| Parameter |
Central Incisors |
Lateral Incisors |
||
| Mean ± SDa |
Range |
Mean ± SDa |
Range |
|
| Intrusion distance, mm | 2.4 ± 0.8 | 1.5–3.5 | 2.5 ± 0.8 | 1.5–5.0 |
| Vertical change in incisal edge, mm | 1.3 ± 0.7 | 0–3.5 | 1.4 ± 0.8 | 0–4.0 |
| Inclination change, degrees | −6.4 ± 7.9 | −20.0–8.0 | −6.5 ± 8.0 | −21–9.0 |
| Anteroposterior change in incisal edge, mm | 2.3 ± 1.4 | 0.5–5.5 | 2.3 ± 1.6 | 0.5–6.0 |
| Movement of apex, mm | 2.3 ± 0.9 | 1.0–4.5 | 2.3 ± 1.0 | 1.0–4.5 |
SD indicates standard deviation.
Mean upper central and lateral incisor root volumes, percentage tooth loss, and root length (two-dimensional [2D]) at T0 and T1 were normally distributed (Table 2). Mean root volume significantly decreased on the labio- and palato-apical aspects of 12 and labio-apical aspects of 21 and 22 (P = .018, .002, .006 and .024, respectively). There was no significant difference in root length (2D) between T0 and T1.
Table 2.
Root Volume of the Upper Central and Lateral Incisors at T0 and T1a
| Tooth No. |
Time Point |
Root Volume (mm3) |
Percentage of Tooth Loss (%) | Root Length (mm) |
|||
| T0 | T1 | Sig. |
|||||
| Mean ± SD |
Sig. |
Mean ± SD |
Mean ± SD |
Mean ± SD |
|||
| 12 | |||||||
| Labial | |||||||
| Coronal | T0 | 64.57 ± 18.65 | .839 | 2.18 ± 1.37 | 12.80 ± 1.52 | 12.16 ± 1.71 | .325 |
| T1 | 63.14 ± 18.22 | ||||||
| Middle | T0 | 36.57 ± 9.86 | .618 | 5.2 ± 1.94 | |||
| T1 | 34.71 ± 9.60 | ||||||
| Apical | T0 | 15.71 ± 4.62 | .018* | 29.36 ± 7.65 | |||
| T1 | 11.36 ± 4.50 | ||||||
| Palatal | |||||||
| Coronal | T0 | 51.64 ± 10.17 | .755 | 2.48 ± 1.66 | |||
| T1 | 50.43 ± 10.17 | ||||||
| Middle | T0 | 30.07 ± 6.145 | .524 | 5.15 ± 3.12 | |||
| T1 | 28.57 ± 6.14 | ||||||
| Apical | T0 | 17.00 ± 4.47 | .002* | 34.95 ± 10.03 | |||
| T1 | 11.43 ± 4.24 | ||||||
| 11 | |||||||
| Labial | |||||||
| Coronal | T0 | 79.87 ± 20.34 | .838 | 2.05 ± 0.96 | 13.09 ± 1.46 | 12.45 ± 1.48 | .276 |
| T1 | 78.33 ± 20.35 | ||||||
| Middle | T0 | 42.80 ± 11.53 | .690 | 3.87 ± 2.27 | |||
| T1 | 41.13 ± 11.09 | ||||||
| Apical | T0 | 19.20 ± 6.74 | .106 | 23.11 ± 8.00 | |||
| T1 | 15.13 ± 6.61 | ||||||
| Palatal | |||||||
| Coronal | T0 | 74.20 ± 16.85 | .785 | 2.18 ± 1.34 | |||
| T1 | 72.53 ± 16.22 | ||||||
| Middle | T0 | 40.80 ± 8.70 | .596 | 4.57 ± 2.94 | |||
| T1 | 39.07 ± 9.01 | ||||||
| Apical | T0 | 17.60 ± 6.07 | .074 | 24.11 ± 8.25 | |||
| T1 | 13.67 ± 5.54 | ||||||
| 21 | |||||||
| Labial | |||||||
| Coronal | T0 | 73.93 ± 13.61 | .771 | 2.05 ± 1.16 | 12.71 ± 1.58 | 11.94 ± 1.65 | .236 |
| T1 | 72.47 ± 13.66 | ||||||
| Middle | T0 | 41.33 ± 9.39 | .662 | 4.00 ± 1.80 | |||
| T1 | 39.80 ± 9.64 | ||||||
| Apical | T0 | 16.60 ± 3.18 | .006* | 22.53 ± 6.95 | |||
| T1 | 13.00 ± 3.38 | ||||||
| Palatal | |||||||
| Coronal | T0 | 75.00 ± 12.87 | .723 | 2.24 ± 0.92 | |||
| T1 | 73.33 ± 12.61 | ||||||
| Middle | T0 | 43.20 ± 7.11 | .530 | 3.98 ± 2.00 | |||
| T1 | 41.53 ± 7,23 | ||||||
| Apical | T0 | 20.07 ± 6.47 | .054 | 25.43 ± 9.03 | |||
| T1 | 15.40 ± 6.23 | ||||||
| 22 | |||||||
| Labial | |||||||
| Coronal | T0 | 66.86 ± 17.40 | .838 | 2.13 ± 1.57 | 13.00 ± 1.53 | 12.33 ± 1.69 | .302 |
| T1 | 65.50 ± 17.30 | ||||||
| Middle | T0 | 36.00 ± 9.70 | .590 | 5.86 ± 2.14 | |||
| T1 | 34.00 ± 9.72 | ||||||
| Apical | T0 | 12.57 ± 4.88 | .024* | 39.23 ± 14.44 | |||
| T1 | 8.21 ± 4.78 | ||||||
| Palatal | |||||||
| Coronal | T0 | 59.07 ± 15.11 | .803 | 2.49 ± 1.40 | |||
| T1 | 57.64 ± 14.87 | ||||||
| Middle | T0 | 33.50 ± 9.70 | .584 | 6.20 ± 2.10 | |||
| T1 | 31.50 ± 9.40 | ||||||
| Apical | T0 | 19.29 ± 10.31 | .137 | 37.3 ± 17.92 | |||
| T1 | 13.43 ± 9.89 | ||||||
T0 indicates pretreatment; T1, posttreatment; SD, standard deviation; Sig., significance.
P < .05, paired t-test.
Comparing the same segments of different teeth, root volume loss on the palato-apical segment was significantly less on central than lateral incisors (11/12, P < .001; 11/22, P < .001; 21/12, P = .016; and 21/22, P = .001). The percentage of root volume loss between T0 and T1 was less on the labio-apical aspects of 11 vs 22 and 21 vs 22 (P < .001) and palato-apical aspects of 11 vs 22 and 21 vs 22 (P = .021 and .045).
There were no significant differences in root volume changes and percentage root volume loss between the left and right central and lateral incisors. Therefore, the left and right central and lateral incisor data were pooled to compare different segments of each tooth. On central incisors, root volume loss was significantly greater on the labio-apical segment than other segments, with the exception of the palato-apical segment. On lateral incisors, root volume loss was significantly greater on the palato-apical segment than other segments.
The CEJ–alveolar bone crest distance did not significantly change between T0 and T1 (Table 3).
Table 3.
Bone Height of the Upper Central and Lateral Incisors at T0 and T1
| Tooth No. |
Mean ± SD |
t |
Sig. (2-tailed) |
Mean Difference |
SE Difference |
| 12 | |||||
| Mesial | |||||
| T0 | 4.76 ± 0.85 | −0.513 | .61 | −0.19 | 0.37 |
| T1 | 4.94 ± 1.08 | ||||
| Distal | |||||
| T0 | 3.86 ± 0.89 | −0.910 | .37 | −0.37 | 0.41 |
| T1 | 4.23 ± 1.24 | ||||
| Labial | |||||
| T0 | 3.44 ± 1.23 | 0.293 | .77 | 0.11 | 0.37 |
| T1 | 3.33 ± 0.62 | ||||
| Palatal | |||||
| T0 | 3.51 ± 2.79 | 0.058 | .95 | 0.05 | 0.90 |
| T1 | 3.46 ± 1.87 | ||||
| 11 | |||||
| Mesial | |||||
| T0 | 3.82 ± 1.22 | −0.521 | .61 | −0.19 | 0.37 |
| T1 | 4.01 ± 0.73 | ||||
| Distal | |||||
| T0 | 3.95 ± 0.96 | −0.443 | .66 | −0.15 | 0.34 |
| T1 | 4.10 ± 0.93 | ||||
| Labial | |||||
| T0 | 3.24 ± 1.04 | 0.116 | .91 | 0.05 | 0.41 |
| T1 | 3.20 ± 1.20 | ||||
| Palatal | |||||
| T0 | 3.04 ± 0.90 | −1.525 | .14 | −1.06 | 0.70 |
| T1 | 4.10 ± 2.55 | ||||
| 21 | |||||
| Mesial | |||||
| T0 | 3.93 ± 1.37 | −0.530 | .60 | −0.22 | 0.42 |
| T1 | 4.15 ± 0.84 | ||||
| Distal | |||||
| T0 | 3.08 ± 0.94 | −0.004 | 1.00 | 0.00 | 0.31 |
| T1 | 3.08 ± 0.77 | ||||
| Labial | |||||
| T0 | 3.10 ± 0.92 | −0.840 | .41 | −0.29 | 0.35 |
| T1 | 3.40 ± 0.99 | ||||
| Palatal | |||||
| T0 | 3.36 ± 1.75 | −1.663 | .11 | −1.44 | 0.86 |
| T1 | 4.80 ± 2.85 | ||||
| 22 | |||||
| Mesial | |||||
| T0 | 4.11 ± 2.62 | −0.174 | .86 | −0.14 | 0.83 |
| T1 | 4.25 ± 1.66 | ||||
| Distal | |||||
| T0 | 4.26 ± 2.36 | 0.555 | .58 | 0.43 | 0.78 |
| T1 | 3.82 ± 1.70 | ||||
| Labial | |||||
| T0 | 3.46 ± 1.22 | 0.082 | .94 | 0.03 | 0.39 |
| T1 | 3.42 ± 0.81 | ||||
| Palatal | |||||
| T0 | 3.36 ± 2.06 | −0.012 | .99 | −0.01 | 0.67 |
| T1 | 3.37 ± 1.41 | ||||
T0 indicates pretreatment; T1, posttreatment; SD, standard deviation; Sig., significance; SE, standard error.
Regression analysis revealed no significant linear relationship between any tooth movement parameter and percentage root volume loss.
DISCUSSION
Central and lateral incisor root volumes and root length were measured in adult females after 1 year of orthodontic treatment. The literature indicates gender and age may affect root resorption, with nonsignificant findings reported. However, adult female patientss were selected for this study to reduce confounding factors.28 Previous studies of root resorption during application of intrusion mechanics have assessed heterogeneous cohorts that included children, adolescents, and adults.12–14 However, growing patients may have a higher rate of alveolar bone remodeling. Previous studies employed convention periapical films, which can be unreliable.15,29 This is the first 3D assessment of root volume loss after orthodontic treatment in adult patients. Root volume decreased on the apical aspect, especially the palato-apical segments of the lateral incisors, whereas 2D imaging indicated no significant change in root length.
In this study, a continuous archwire was used for incisor intrusion that may also therefore result in extrusion of the posterior teeth. The extent of upper central and lateral incisor root resorption (0.64–0.77 mm) was lower than the values of 1.36 ± 1.46 mm,4 1.84 mm,13 0.76 ± 0.64,30 and 1 to 3 mm24 reported by studies that used segmented techniques. The patients in this study had marginal alveolar bone loss and were treated carefully using light intrusive force (40 g), which may lead to less resorption than higher forces. Although 10 g of intrusive force/tooth was recommended for patients with marginal bone loss by Melsen et al.,24 they used different mechanics and force magnitude varied from 10 to 20 g/tooth depending on periodontal support (but not specifically related to periodontal support). In the current study, an attempt was made to control the magnitude of force applied to the upper incisors, although the magnitude of torque from the prescription bracket depended on initial upper incisor inclination. However, no relationship was observed between the change in inclination and root resorption. In future studies, initial inclination should be controlled to reduce its influence as a confounder.
No significant differences between any incisors were observed in the 2D analysis. However, 3D analysis revealed a significant difference in percentage root volume loss between the apical aspects of the central and lateral incisors, confirming that 2D analysis underestimates root resorption. Upper incisor intrusion is a common treatment for excessive overbite correction, especially in patients with periodontitis and pathologic upper incisor migration. The application of 40 g intrusive force to the four upper incisors using a T-loop led to greater root resorption on the lateral incisors in this study. A finite element model of the maxillary anterior teeth after orthodontic intrusion showed that stress was concentrated on the palato-apical region and distributed to the lateral incisors if the point of force application moved distally.31 In the current study, the typodont showed more force was distributed to the lateral than central incisors. Accordingly, the lateral incisors exhibited more apical root resorption than the central incisors. Application of intrusive force distal to the lateral incisor brackets, as recommended by Saga et al.,31 should be further investigated.
The root volume loss on the coronal segment (about 2%–3%) in this study was the result of root planing processes. Previously, a periodontal treatment method with hand curettes or piezoelectric ultrasonic scalers showed coronal cementum loss.32
The changes in upper incisor movement were not significantly related to root resorption. To minimize confounding factors, several factors previously shown to be associated with root resorption33 were controlled, including age (40–55 years), gender (female), duration of treatment (1 year), nonextraction treatment plan, intrusion mechanics, force magnitude, and initial alveolar bone support.
Potential limitations of this study should be considered. Segmentation and 3D registration were limited by the difficulty of defining the borders between the root surface, cementum, and alveolar bone. However, the highest precision technique available was used.26 No control group was available, although the purpose of this study was to assess whether root resorption correlated with tooth movement in patients with compromised periodontium. This study may not reflect the extent of root resorption during the entire treatment process; longitudinal observations that extend beyond debanding are required.
CONCLUSIONS
Significant volume loss in the apical third of the upper incisor root is common after 1 year of orthodontic treatment in patients with moderate bone loss.
Delivery of 40 g intrusive force to the four upper incisors using a continuous T-loop and the leveling phase lead to more apical root volume loss on the lateral than central incisors.
No relationship was observed between tooth movement and upper incisor root volume loss.
ACKNOWLEDGMENTS
We thank Prince of Songkla University Graduate School and Faculty of Dentistry for grant support. We acknowledge Ms. Vipavee Puttaravuttiporn for statistical advice.
REFERENCES
- 1.Abass SK, Hartsfield JK. Orthodontics and external apical root resorption. Semin Orthod. 2007;13:246–256. [Google Scholar]
- 2.Melsen B. Adult Orthodontics. Hoboken, NJ: Wiley; 2012. pp. 209–214. [Google Scholar]
- 3.Castro IO, Alencar AH, Valladares-Neto J, Estrela C. Apical root resorption due to orthodontic treatment detected by cone beam computed tomography. Angle Orthod. 2012;83:196–203. doi: 10.2319/032112-240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baumrind S, Korn EL, Boyd RL. Apical root resorption in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;110:311–320. doi: 10.1016/s0889-5406(96)80016-3. [DOI] [PubMed] [Google Scholar]
- 5.Topkara A, Karaman AI, Kau CH. Apical root resorption caused by orthodontic forces: A brief review and a long-term observation. Eur J Dent. 2012;6:445–453. [PMC free article] [PubMed] [Google Scholar]
- 6.Segal GR, Schiffman PH, Tuncay OC. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 7.Chan E, Darendeliler MA. Physical properties of root cementum: Part 5. Volumetric analysis of root resorption craters after application of light and heavy orthodontic forces. Am J Orthod Dentofacial Orthop. 2005;127:186–195. doi: 10.1016/j.ajodo.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 8.Acar A, Canyürek Ü, Kocaaga M, Erverdi N. Continuous vs. discontinuous force application and root resorption. Angle Orthod. 1999;69:159–163. doi: 10.1043/0003-3219(1999)069<0159:CVDFAA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Kaley J, Phillips C. Factors related to root resorption in edgewise practice. Angle Orthod. 1991;61:125–132. doi: 10.1043/0003-3219(1991)061<0125:FRTRRI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Harris DA, Jones AS, Darendeliler MA. Physical properties of root cementum: part 8. Volumetric analysis of root resorption craters after application of controlled intrusive light and heavy orthodontic forces: a microcomputed tomography scan study. Am J Orthod Dentofacial Orthop. 2006;130:639–647. doi: 10.1016/j.ajodo.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 11.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–146. doi: 10.1016/S0889-5406(05)81763-9. [DOI] [PubMed] [Google Scholar]
- 12.Dermaut L, De Munck A. Apical root resorption of upper incisors caused by intrusive tooth movement: a radiographic study. Am J Orthod Dentofacial Orthop. 1986;90:321–326. doi: 10.1016/0889-5406(86)90088-0. [DOI] [PubMed] [Google Scholar]
- 13.McFadden WM, Engstrom C, Engstrom H, Anholm JM. A study of the relationship between incisor intrusion and root shortening. Am J Orthod Dentofacial Orthop. 1989;96:390–396. doi: 10.1016/0889-5406(89)90323-5. [DOI] [PubMed] [Google Scholar]
- 14.Costopoulos G, Nanda R. An evaluation of root resorption incident to orthodontic intrusion. Am J Orthod Dentofacial Orthop. 1996;109:543–548. doi: 10.1016/s0889-5406(96)70140-3. [DOI] [PubMed] [Google Scholar]
- 15.Parker RJ, Harris EF. Directions of orthodontic tooth movements associated with external apical root resorption of the maxillary central incisor. Am J Orthod Dentofacial Orthop. 1998;114:677–683. doi: 10.1016/s0889-5406(98)70200-8. [DOI] [PubMed] [Google Scholar]
- 16.Martins DR, Tibola D, Janson G, Maria FRT. Effects of intrusion combined with anterior retraction on apical root resorption. Eur J Orthod. 2011;34:170–175. doi: 10.1093/ejo/cjq178. [DOI] [PubMed] [Google Scholar]
- 17.Segal G, Schiffman P, Tuncay O. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz AM. Tissue changes incidental to orthodontic tooth movement. Int J Orthod Oral Surg Radiogr. 1932;18:331–352. [Google Scholar]
- 19.Chan EKM, Darendeliler MA. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7:64–70. doi: 10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 20.Chan E, Darendeliler MA. Physical properties of root cementum: part 7. Extent of root resorption under areas of compression and tension. Am J Orthod Dentofacial Orthop. 2006;129:504–510. doi: 10.1016/j.ajodo.2004.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Dudic A, Giannopoulou C, Martinez M, Montet X, Kiliaridis S. Diagnostic accuracy of digitized periapical radiographs validated against micro-computed tomography scanning in evaluating orthodontically induced apical root resorption. Eur J Oral Sci. 2008;116:467–472. doi: 10.1111/j.1600-0722.2008.00559.x. [DOI] [PubMed] [Google Scholar]
- 22.Baysal A, Karadede I, Hekimoglu S, et al. Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2011;82:488–494. doi: 10.2319/060411-367.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Quigley GA, Hein JW. Comparative cleansing efficiency of manual and power brushing. J Am Dent Assoc. 1962;65:26–29. doi: 10.14219/jada.archive.1962.0184. [DOI] [PubMed] [Google Scholar]
- 24.Melsen B, Agerbæk N, Markenstam G. Intrusion of incisors in adult patients with marginal bone loss. Am J Orthod Dentofacial Orthop. 1989;96:232–241. doi: 10.1016/0889-5406(89)90460-5. [DOI] [PubMed] [Google Scholar]
- 25.Fleiner J, Hannig C, Schulze D, Stricker A, Jacobs R. Digital method for quantification of circumferential periodontal bone level using cone beam CT. Clin Oral Investig. 2013;17:389–396. doi: 10.1007/s00784-012-0715-3. [DOI] [PubMed] [Google Scholar]
- 26.Forst D, Nijjar S, Flores-Mir C, Carey J, Secanell M, Lagravere M. Comparison of in vivo 3D cone-beam computed tomography tooth volume measurement protocols. Prog Orthod. 2014;15:69. doi: 10.1186/s40510-014-0069-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Akyalcin S, Alexander S, Silva R, English J. Evaluation of three-dimensional root surface changes and resorption following rapid maxillary expansion: a cone beam computed tomography investigation. Orthod Craniofac Res. 2015;18:117–126. doi: 10.1111/ocr.12069. [DOI] [PubMed] [Google Scholar]
- 28.Linge L, Linge BO. Patients characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;96:35–43. doi: 10.1016/S0889-5406(05)81678-6. [DOI] [PubMed] [Google Scholar]
- 29.Cardaropoli D, Re S, Corrente G, Abundo R. Intrusion of migrated incisors with infrabony defects in adult periodontal patients. Am J Orthod Dentofacial Orthop. 2001;120:671–675. doi: 10.1067/mod.2001.119385. [DOI] [PubMed] [Google Scholar]
- 30.de Almeida MR, Marçal ASB, Fernandes TMF, Vasconcelos JB, de Almeida RR, Nanda R. A comparative study of the effect of the intrusion arch and straight wire mechanics on incisor root resorption: A randomized, controlled trial. Angle Orthod. 2017;88:20–26. doi: 10.2319/06417-424R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saga AY, Maruo H, Argenta MA, Maruo IT, Tanaka OM. Orthodontic intrusion of maxillary incisors: a 3D finite element method study. Dental Press J Orthod. 2016;21:75–82. doi: 10.1590/2177-6709.21.1.075-082.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bozbay E, Dominici F, Gokbuget AY, et al. Preservation of root cementum: a comparative evaluation of power-driven versus hand instruments. Int J Dent Hyg. 2016;16:202–209. doi: 10.1111/idh.12249. [DOI] [PubMed] [Google Scholar]
- 33.Weltman B, Vig KW, Fields HW, Shanker S, Kaizar EE. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]