Abstract
The Go Red for Women movement was initiated by the American Heart Association (AHA) in the early 2000s to raise awareness concerning cardiovascular disease (CVD) risk in women. In 2016, the AHA funded 5 research centers across the United States to advance our knowledge of the risks and presentation of CVD that are specific to women. This report highlights the findings of the centers, showing how insufficient sleep, sedentariness, and pregnancy‐related complications may increase CVD risk in women, as well as presentation and factors associated with myocardial infarction with nonobstructive coronary arteries and heart failure with preserved ejection fraction in women. These projects were augmented by collaborative ancillary studies assessing the relationships between various lifestyle behaviors, including nightly fasting duration, mindfulness, and behavioral and anthropometric risk factors and CVD risk, as well as metabolomic profiling of heart failure with preserved ejection fraction in women. The Go Red for Women Strategically Focused Research Network enhanced the evidence base related to heart disease in women, promoting awareness of the female‐specific factors that influence CVD.
Keywords: health outcomes, heart failure, myocardial infarction, pregnancy, sedentary behavior, sleep, stress
Subject Categories: Basic Science Research, Biomarkers, Clinical Studies
Nonstandard Abbreviations and Acronyms
- AHA
American Heart Association
- cGMP
cyclic guanosine mono‐phosphate
- CUIMC
Columbia University Irving Medical Center
- GRFW
Go Red for Women
- HFpEF
heart failure with preserved ejection fraction
- HFrEF
heart failure with reduced ejection fraction
- JHU
Johns Hopkins University
- MINOCA
myocardial infarction with non‐obstructive coronary arteries
- NYU
New York University
- SFRN
Strategically Focused Research Network
- UCSD
University of California at San Diego
Cardiovascular disease (CVD) is the leading cause of death in women, 1 yet women are less likely to be diagnosed and receive preventive care and aggressive treatment compared with men. 2 Various female‐specific factors have been identified that contribute to their increased risk. 3 In spring 2016, the American Heart Association (AHA) funded 5 centers to study CVD risk in women as part of its Strategically Focused Research Network (SFRN) mechanism. The goal of this program was to yield important gains in knowledge and research capacity, including developing a new cadre of investigators focused on women's health research to energize the field. The Go Red for Women (GRFW) Network was launched, covering topics of sleep (Columbia University Irving Medical Center [CUIMC]), heart failure with preserved ejection fraction (HFpEF; Johns Hopkins University School of Medicine [JHU]), placental and maternal microvascular response to pregnancy (Magee‐Womens Research Institute and Foundation), stress and myocardial infarction (MI) with nonobstructive coronary arteries (MINOCA; New York University Langone Medical Center [NYU]), and sedentary behavior in Latinas (University of California at San Diego [UCSD]). 4 Over the 4‐year award period, collaborations were fostered, both within and among centers throughout the network, and a competitive grant mechanism was launched to further promote within‐network collaborations. These Soter Awards, granted to junior faculty and fellows, provided additional research experience and training, and expanded collaborations across the network. Herein, we summarize the findings of each center, describing the network's contributions to advancing the mission and impact of the AHA and its GRFW initiative.
Center Findings
CUIMC: Sleep and CVD Risk in Women Across the Lifespan
Insufficient sleep, a highly prevalent behavior, is associated with increased cardiovascular risk in observational studies, 5 with women experiencing greater adverse consequences for some risk factors than men. 6 , 7 , 8 However, the subjective reporting of sleep duration and possible reverse effects of CVD on sleep, limitations inherent to observational studies, preclude conclusions on causal relationships between insufficient sleep and cardiovascular risk. Moreover, the mechanisms that mediate increased cardiovascular risk in insufficient sleep are poorly understood. The overall scientific goals of this center were to (1) document patterns of sleep and potential confounders and modulators of CVD risk among a diverse group of women throughout the lifespan, and (2) assess the causal relationship between insufficient sleep and cardiometabolic risk via a rigorous clinical and translational intervention to evaluate mechanisms.
Prior research on sleep and CVD has not fully considered sex, race/ethnicity, psychosocial factors, including caregiving responsibilities, and stages of life that may differentially impact women. A 1‐year prospective study was conducted to evaluate sleep patterns and their relationship to lifestyle and psychosocial risk factors, caregiving, cardiometabolic health, and clinical outcomes among a diverse cohort of 506 women recruited from the Northern Manhattan community. Women enrolled in the study were on average 37 years old, 61% identified as a racial minority and/or of Hispanic ethnicity, and over half had overweight/obesity. Approximately 50% of women reported poor sleep quality, with 43% reporting sleeping <7 h/night, and 38% reporting some level of insomnia. Poor sleep quality and risk of obstructive sleep apnea were associated with systolic and diastolic blood pressure, respectively, after adjusting for confounders. 9 Furthermore, women reporting adequate sleep duration (≥7 h/night), good sleep quality, no insomnia or snoring, low risk for obstructive sleep apnea, and morning chronotype (preference for morning activities and morning alertness) had better overall cardiovascular health, assessed by AHA Life's Simple 7, and a greater likelihood of meeting >4 of the AHA Life's Simple 7 metrics than women reporting poor sleep. 10 These associations were stronger among postmenopausal and racial/ethnic minority women. Conversely, women with evening chronotypes (preference for evening activities and evening alertness) had greater odds of having poor cardiovascular health and adverse health behaviors after adjustment for sociodemographic factors and menopausal status. 11 High risk of obstructive sleep apnea was associated with systemic inflammation (C‐reactive protein level of ≥2 mg/L); however, this association was seen among racial/ethnic minority women, but not White women. 12 We also found evidence suggesting that poor sleep may negatively influence cardiovascular health via: (1) consumption of higher‐energy and lower‐quality diet, 13 and (2) increased psychosocial risk factors for CVD including depression, low social support, and caregiving. 14
Despite studies showing that chronic short sleep duration is associated with increased risk of CVD, 15 causal evidence relies on short intervention studies of severe sleep restriction that do not reflect conditions of habitual short sleepers, those who get <7 hours of sleep per night recommended by the Sleep Research Society and the American Academy of Sleep Medicine. 16 Particularly, some studies highlight an impact of acute sleep restriction on blood pressure 17 and insulin resistance. 18 However, whether habitual short sleep duration (<7 h/night) sustained over a longer period of time affects CVD risk is unknown. We performed a randomized controlled trial of sleep restriction in pre‐ and postmenopausal women with habitual adequate sleep, determined using 2 weeks of wrist actigraphy, to assess causality. The study included 2 phases of 6 weeks each: sleep restriction, in which sleep duration was curtailed by 1.5 hours by delaying bedtime, mimicking life‐like conditions; and adequate sleep, whereby women maintained their regular sleep schedule, as assessed during the screening period. To date, 26 premenopausal and 10 postmenopausal women with or at risk of overweight/obesity completed the study (78% retention rate). Four additional women (1 postmenopausal) are currently enrolled to achieve our final sample size of 40 women. Overall, sleep was reduced by an average of 1.3 h/night during sleep restriction relative to habitual sleep. Data from 19 premenopausal women who completed the study at the time of analysis show that average 24‐hour ambulatory diastolic blood pressure increased after 6 weeks of sleep restriction relative to adequate sleep, and in‐office systolic blood pressure also increased over time during sleep restriction relative to adequate sleep. 19 During adequate sleep, bedtime and wake‐up times were prescribed to ensure compliance with sleep duration. This resulted in an unexpected observation that women who reduced their bedtime variability, even in the absence of changes in habitual sleep duration, had reductions in adiposity compared with those who increased or did not change their bedtime variability. 20
Our clinical trial was also the basis for investigations into causal mechanisms by measuring the impact of sleep restriction on endothelial dysfunction, an early step in the development of CVD. Endothelial cells were collected before and after 6 weeks of objectively monitored mild sleep restriction or adequate sleep. Sleep restriction increased endothelial inflammation and oxidative stress, and impaired vasomotor function compared with adequate sleep duration. Remarkably, endothelial antioxidant response was completely lacking despite markedly increased endothelial oxidative stress. Using an unbiased approach of RNAseq in harvested endothelial cells and a predicted protein–protein interaction algorithm, we identified defective in cullin neddylation 1 domain containing 3, a protein that sequesters cullin‐3 to the plasma membrane and regulates nuclear factor (erythroid‐derived 2)‐like 2‐mediated antioxidant response in endothelial cells, as a novel mediator of impaired endothelial nuclear factor (erythroid‐derived 2)‐like 2‐dependent antioxidant response in insufficient sleep. Curtailing sleep by delaying bedtime reduced expression of endothelial defective in cullin neddylation 1 domain containing 3 by reducing daytime expression of its regulator serum response factor, a transcription factor that is responsive to sleep pressure and primes cortical response to sleep deprivation. Our study shows that insufficient sleep promotes endothelial oxidative stress and inflammation and impairs antioxidant response and vasomotor tone, highlighting a mechanism by which curtailing sleep leads to endothelial dysfunction and increases cardiovascular risk.
Overall, our findings provide important insight for sleep as a highly prevalent yet frequently overlooked CVD risk marker in a diverse population of women. Moreover, we have identified a novel mechanism linking insufficient sleep, a common behavior practiced by more than a third of adults, to impaired vascular health. Combined, our findings suggest that insufficient sleep increases the risk for CVD in women, and that improvements in sleep hygiene may be relevant to risk reduction efforts. Our center's outcomes support efforts to increase women's awareness of sleep as a risk factor for CVD. Particularly, sleep health, as a multidimensional lifestyle behavior that encompasses sleep duration, continuity, and timing, and that results in satisfaction with one's sleep and daytime alertness, 21 should be evaluated for risk prevention.
JHU: Role of Sex Hormones and Cyclic Guanosine Monophosphate/Protein Kinase G in Cardiac and Metabolic Disorders in Patients With Heart Failure With Preserved Ejection Fraction
Over half of all patients with heart failure have preserved ejection fraction, which is increasing in prevalence and has very few therapies. 22 Women are more often affected, and reasons for sex differences remain uncertain. 23 Progress has been limited by a lack of molecular and cellular understanding of the underlying pathophysiology. Preclinical models have focused on hypertension with hypertrophy and diastolic dysfunction, but the substrate for heart failure with preserved ejection fraction (HFpEF) has shifted to obesity and cardiometabolic diseases with their multiorgan effects. Our center aimed to elucidate novel HFpEF mechanisms examining sex differences, the role of cyclic guanosine monophosphate (cGMP)/protein kinase G signaling, 24 and myocardial pathobiology.
Population studies assessed if the menopausal transition modulates oxidative stress and plasma cGMP associations with cardiac structure and function to potentially raise HFpEF risk in older women. Plasma cGMP levels and urinary isoprostane levels were measured in 3 community‐based cohorts: ARIC (Atherosclerosis Risk In Communities), MESA (MultiEthnic Study of Atherosclerosis), and CARDIA (Coronary Artery Risk Development In young Adults), also utilizing sex hormone and phenotypic data already collected. A more androgenic sex hormone profile was associated with a greater increase in left ventricular mass 25 and with incident cardiovascular and heart failure events in postmenopausal women. 26 This was also associated with greater subclinical atherosclerosis, 27 N‐terminal pro‐B‐type natriuretic peptide, 28 worse aortic distensibility 26 and endothelial dysfunction, 29 and lower plasma cGMP levels in women. 30 Contrary to our starting hypothesis, higher levels of cGMP were associated with increased risk for atherosclerotic CVD events. 31 However, the strength of the association with heart failure and HFpEF was attenuated after adjusting for N‐terminal pro‐B‐type natriuretic peptide, the primary upstream stimulator of cGMP measured in blood. The status of nitric oxide signaling is poorly reflected in the peripheral blood. Higher cGMP is also associated with hypertension, chronic kidney disease, metabolic risk factors, 30 and greater rise in left ventricular mass over time. 32 Although augmenting intracellular cGMP confers myocardial protection against pathological stress, here it more likely was a marker for compensatory changes, much as observed with elevated natriuretic peptides themselves. Urinary isoprostanes, a measure of oxidative stress, were associated with postmenopausal status 33 and cardiovascular risk factors. 34
Our clinical–translational research focused on myocardial biology of patients with HFpEF, with the goal of identifying biological subgroups for which to better target therapeutics. We have established an HFpEF clinic with the largest repository of right ventricular endomyocardial biopsy tissue from well‐phenotyped patients with HFpEF. In one study, biopsies from 108 patients with HFpEF were contrasted to controls and patients with heart failure with reduced ejection fraction (HFrEF). In patients with HFpEF, 93% had fibrosis, but this was mild in nearly three‐fourths, often overlapping with controls. Fibrosis was somewhat greater in HFrEF. 35 , 36 Cardiomyocyte hypertrophy was absent or mild in over half of the patients with HFpEF, and severe in only 3%. Importantly, undiagnosed cardiac amyloidosis was found in 14% of patients. Older age and renal disease were associated with greater myocardial inflammation (CD68+ cells) in HFpEF, and there were no sex differences in the histopathology.
We also determined transcriptomic signatures by RNAseq in the same 3 patient groups. 37 Agnostic clustering identified distinct separation of gene transcription between the groups, with or without adjusting for differences in major comorbidities (sex, age, diabetes mellitus, body mass index, and renal function). Gene enrichment in pathways often viewed as characteristic of HFpEF, such as fibrosis, hypertrophy, and inflammation, were similarly observed in HFrEF. The groups differed notably in oxidative phosphorylation, endoplasmic reticular stress, and autophagy pathways. Genes upregulated in HFpEF were in mitochondrial ATP synthesis and largely correlated with obesity, whereas downregulated genes enriched for protein processing, endoplasmic reticulum stress, and angiogenesis were independent of obesity and other major comorbidities. Within HFpEF, we identified transcriptomic signatures in different clinical cohorts, including one behaving more like HFrEF, with higher natriuretic peptide, right ventricular disease, pulmonary hypertension, and higher mortality. A second group had smaller hearts, less hypertrophy and natriuretic peptide elevation, and an inflammatory signature.
Another study asked whether and how the presence of morbid obesity impacts underlying right ventricular sarcomere function in HFpEF. 38 In prior data in mostly nonobese patients with HFpEF with marked hypertension and left ventricular hypertrophy, myocytes were passively stiffer but had normal calcium‐stimulated systolic contractility. We found similar properties in our patients with prominent hemodynamic stress (higher blood pressures), left ventricular hypertrophy, but less obesity. However, myocytes from very obese patients with less hemodynamic stress and hypertrophy had depressed contractility and less passive stiffening. Overall, maximal sarcomere tension (marker of contractile reserve) inversely correlated with body mass index (r=−0.69, P=2×10−8). There was no sex dependence. The data show that obesity is altering underlying myocardial behavior in HFpEF, raising questions about the best treatments. Ongoing efforts are dissecting the mechanisms and testing a potential use of sarcomere‐enhancing therapies.
We also examined body fat composition using magnetic resonance imaging HFpEF on patients (n=55), and found men had greater visceral to subcutaneous adipose tissue ratio versus women, liver fat and epicardial adipose tissue were associated with worse global well‐being score, and skeletal muscle adipose tissue was associated with diabetes mellitus, hypertension, obstructive sleep apnea, and reduced 6‐minute walk test distance. 39 Ongoing studies are examining associations with sex hormones, exercise myocardial mechanics, intracellular cGMP signaling from platelets, and physiological studies using an atrial natriuretic peptide mimetic.
In the basic science project, we developed a new preclinical mouse model of cardiometabolic syndrome combining morbid obesity with pressure‐load stress and testing the efficacy of enhancing cGMP/protein kinase G signaling to counter cardiac and metabolic abnormalities. 40 The model tested the role of female sex hormones on the efficacy of inhibiting phosphodiesterase type 9 to enhance cGMP. Phosphodiesterase type 9 inhibition reduced obesity and associated metabolic syndrome but only in ovariectomized female and male mice. All groups exhibited improved heart function and less hypertrophy from the treatment. Cardiometabolic improvement was coupled to increased lipolysis linked to augmentation of peroxisome proliferator activated receptor α regulation. Interactions between this transcription factor and estrogen may explain the sex dimorphism. Phosphodiesterase type 9 inhibitors are already in human testing for neurocognitive disease and recently heart failure, so these findings are translationally relevant.
Collectively, our center identified clinical and risk associations with cGMP as a biomarker in HFpEF, characterized its histopathological abnormalities, performed the first gene expression profiling to identify molecular signatures and potentially new therapeutic targets, determined sarcomere pathophysiology and the impact of obesity, and developed a new preclinical model and therapeutic approach for cardiometabolic syndrome, with HFpEF features, based on phosphodiesterase type 9 inhibition, revealing a potent role of sex hormone status.
Magee‐Womens Research Institute and Foundation: Women's Cardiovascular Health and Microvascular Mechanisms: Novel Insights From Pregnancy
For many years, attempts to elucidate the unique features of CVD in women have focused on the observation that CVD is more common after menopause. 41 However, data now suggest CVD risk trajectories develop earlier in women's lives, and microvascular dysfunction may be of particular importance in CVD in women. 42 , 43 , 44 , 45 Pregnancy is a complex stressor for women. Adverse pregnancy outcomes, such as preeclampsia, preterm birth, and fetal growth restriction are associated with increased risk of later life CVD. 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 Pregnancy is associated with profound physiological changes in microvascular and cardiac structure and function, and alterations in metabolism and inflammatory pathways. These and other challenges associated with pregnancy could unmask or perhaps initiate CVD. With this background, the goal of our center was to investigate pregnancy as an event that could predict women's future CVD risk and the biological mechanisms underlying this risk.
Our center proposed that women with placental evidence of maternal vascular malperfusion during pregnancy would have excess risk of cardiometabolic and microvascular disease 8 to 10 years postpartum compared with those without these lesions. A common finding in preeclampsia and other adverse pregnancy outcomes is that the maternal decidua fails to adapt, resulting in insufficient placental perfusion to support fetal growth and development. 54 This decidual vasculopathy includes suboptimal remodeling of the maternal spiral arteries into highly dilated conduits feeding the placenta and related spiral artery pathologies. Decidual vasculopathy and concomitant hypoxia/reperfusion lesions in the placenta are collectively termed maternal vascular malperfusion. 54 We studied a highly unique cohort of women 8 to 10 years after pregnancy that included placental data, and found that decidual vasculopathy or other maternal vascular malperfusion features are more likely to occur in placentas of Black compared with White women. 55 Black women in the United States are at increased risk for CVD, because they develop CVD earlier and have higher CVD mortality rates compared with White women. 56 Placental vascular malperfusion might be an early identifier of a subset of Black women at exceptionally high risk of CVD later in life. Maternal vascular malperfusion of the placenta also identifies risk of adverse outcomes in a subsequent pregnancy even when detected in placentas from women without complications, 57 and is associated with a blunted blood pressure decline from before conception to early in gestation. 58 We also have reported that 8 to 10 years after pregnancy, women with maternal vascular malperfusion have excess masked hypertension, 59 sublingual microvascular dysfunction assessed via sidestream dark‐field imaging, 60 and reduced coronary flow reserve assessed via myocardial contrast echocardiography. 61 These exciting discoveries suggest that small vessel impairments in the placenta may make women susceptible to small vessel disease later in life.
Consistent with these observations, we performed a case‐control study of women who were prospectively recruited and evaluated during late pregnancy, with a follow‐up 1 year postpartum to test the hypothesis that dysfunction of the glycocalyx lining endothelium and placental trophoblast contributes to the adverse outcomes of pregnancy and later life CVD. Although follow‐up is ongoing, current data suggest that the functional barrier properties of the sublingual microvascular glycocalyx are significantly reduced, along with evidence of impaired microvascular perfusion, at 1 year postpartum in women with prior preeclampsia compared with women who had uncomplicated pregnancies. 62 We have also observed significant differences in maternal vascular function associated with preeclampsia and placental glycocalyx abnormalities, with higher total peripheral resistance index and increased arterial stiffness using noninvasive vascular assessments at 1 year postpartum. 63
To investigate whether an adverse pregnancy outcome causes a lasting injury to the maternal vasculature, we utilized a novel model of pregnancy‐specific hypertension resulting in a preeclampsia‐like phenotype in otherwise normal mice. 64 We found that these otherwise low‐risk female mice developed pregnancy‐specific hypertension, renal dysfunction, endothelial‐dependent and endothelial‐independent vascular dysfunction, reduced placental efficiency, and fetal growth restriction. 65 Importantly, although elevated blood pressure resolved after pregnancy, these mice still exhibited vascular dysfunction postpregnancy. In addition, we observed cardiac hypertrophy in both the male and female offspring of mice that developed pregnancy‐specific hypertension. 66 These data may shed light on epidemiologic studies showing increased risk of maternal CVD later in life and also CVD among the children of women with adverse pregnancy outcomes. 67
We further addressed how pregnancy itself affects future maternal vascular health and CVD risk. Human data suggest a single uncomplicated normotensive pregnancy may be protective of future CVD, 49 yet successive uncomplicated pregnancies are associated with an increased risk of future hypertension and CVD compared with never‐pregnant women. 68 , 69 , 70 , 71 , 72 We therefore investigated changes in postpartum vascular function in low‐risk (wild‐type C57B6J) and high‐risk (apoE−/−, hypercholesterolemic) female mice following 1, 2, or 3 successive pregnancies. Multiple pregnancies had no effect on postpartum vascular function or blood pressure in low‐risk mice. In contrast, high‐risk mice with 2 or 3 pregnancies had significantly higher blood pressure and exhibited vascular dysfunction compared with similarly aged never‐pregnant high‐risk female mice. 73 These striking data indicate that pregnancy can directly affect future maternal vascular function, but the presence of underlying risk factors is an important determinant of trajectories.
Lastly, possible interventions were investigated. The amino acid L‐citrulline is readily converted to L‐arginine in vivo, and this activity has been identified as a target to increase nitric oxide, improve vascular function, and lower blood pressure. 74 Maternal supplementation with citrulline during pregnancy prevented maternal vascular dysfunction in our pregnancy‐specific hypertension model, improved offspring growth and maternal vascular function postpregnancy. 75 Interestingly, citrulline supplementation also significantly improved the maternal vascular glycocalyx in these mice. The importance of glycocalyx integrity on the changes in maternal vascular function following citrulline supplementation needs to be further elucidated.
Our combined human and animal model life‐course approach has supported the concept that pregnancy significantly influences later‐life CVD trajectories and provides important information about future risk. Our mouse model data suggest that a history of successive pregnancies in the presence of underlying risk factors such as hypercholesterolemia hastens CVD development. Furthermore, a transient, preeclampsia‐like phenotype in otherwise low‐risk mice results in lasting vascular dysfunction postpregnancy. Our data overall indicate that microvascular dysfunction, both maternal and placental, is important in connecting pregnancy phenotype to future CVD. Microvascular impairments in the placenta, more common in Black compared with White women, may be an early identifier of women with heightened susceptibility to peripheral and coronary microvascular disease. In addition to this early signal, animal studies suggest that L‐citrulline may act by improving nitric oxide bioavailability while preserving the vascular glycocalyx. The ability to leverage pregnancy for early detection of CVD risk and prevention could have important public health implications.
NYU: The Women's Heart Attack Research Program: Mechanisms of MINOCA, Platelet Activity, and Stress
Sex differences exist in presentation, diagnosis, and outcomes following MI. MINOCA is an example of this phenomenon, occurring in 3% to 5% of males with MI but as many as 15% of females. 76 Multiple processes may result in MINOCA, including plaque‐mediated events, coronary spasm, or even unrecognized myocarditis. Detailed understanding of pathogenetic mechanisms is lacking. 77 , 78 Fundamental questions as to why some women with nonobstructive plaque remain stable and others develop MI remain unanswered. Psychological stress is a potential contributing factor. Stress levels are higher in women than men after MI and partly explain their poorer recovery. 79 , 80 The Women's Heart Attack Research Program investigated the relationships between stress, platelet activity, and MINOCA in women with MI as compared with controls.
The 2 main scientific goals of our center were to (1) delineate mechanisms of MINOCA using multimodality imaging, comprehensive assessment of platelet biology, and measurement of perceived stress within the framework of a multicenter, diagnostic, observational cohort study; and (2) investigate the effects of a stress management intervention on stress levels, quality of life, and platelet biology among women who suffered recent MI. Additional aims were achievable because our 3 studies were combined into 1 protocol, with merged consent forms to make coenrollment simpler. All centers in the network participated in our multicenter studies.
Outcomes of MINOCA are better than in typical MI with obstructive coronary artery disease, but the 4‐year rate of major adverse cardiovascular events is ≈24%, 81 making MINOCA a problem of special importance to women and the physicians who care for them. There is uncertainty about which post‐MI treatment recommendations should apply to patients with MINOCA. Optimal treatment is likely to differ substantially by mechanism. We enrolled 145 women with MINOCA at 16 sites in North America into our multimodality imaging study. Women with MI meeting the universal definition of MI who did not have prior known obstructive coronary artery disease were enrolled before diagnostic coronary angiography. Fully eligible women, with <50% stenosis at angiography and no contraindication, underwent coronary optical coherence tomography to identify vascular causes of MINOCA, and cardiac magnetic resonance imaging to identify and characterize myocardial abnormalities in MINOCA. Images were reviewed at independent core laboratories. Results were combined to determine the underlying cause of the MI presentation. Coronary optical coherence tomography identified a culprit lesion in 46% of the cohort. Most culprit lesions (94%) represented atherosclerotic plaque disruption. 82 Cardiac magnetic resonance was abnormal in 74% of the women, most commonly demonstrating ischemic injury. Women with evidence of infarction or ischemic injury on cardiac magnetic resonance, who did not have a coronary culprit lesion on optical coherence tomography, most likely had coronary artery spasm or thromboembolism. 83 The 2 imaging tests provided independent information. Thus, identification of the underlying cause of MINOCA is feasible and has the potential to guide medical therapy for secondary prevention.
Pathological and clinical studies consistently demonstrate that platelets are major culprits in MI pathogenesis. Anuclear platelets play a major role in thrombosis, atherosclerosis, and inflammation. Platelets, which contain transcripts and the necessary molecular machinery to conduct translation, are intercellular regulators of vascular homeostasis, inflammation, and immune activity. The platelet transcriptome has been used to identify individuals with metabolic, inflammatory, and cardiovascular diseases. We investigated the mechanistic role of platelets in 141 women with different phenotypes of CVD, including MINOCA, MI with obstructive coronary artery disease, and age‐ and race‐matched women referred for cardiac catheterization and found to have nonobstructive coronary artery disease. Analysis of platelet aggregation, flow cytometry (for monocyte‐platelet aggregates, reticulated platelets, P‐selectin, and procaspase activating compound‐1 expression), and hematology analysis will determine whether women with MINOCA have a different platelet activity profile than women with MI with obstructive coronary artery disease or controls, and whether coding and noncoding RNA profiles differ by coronary artery disease status. Analysis based on the underlying cause of MINOCA as identified in the imaging study will generate new hypotheses about mechanistic pathways. Interactions between platelets and leukocytes may serve as a pathophysiologic link between inflammation and thrombosis. We found that the whole blood transcriptome signature is unique in women with MINOCA compared with both control and MI–coronary artery disease women. 84 Several novel canonical pathways (eg, estrogen receptor, mTOR, eIF2) were found to be differentially expressed in the circulating blood profile of women with MINOCA versus both controls and MI with obstructive coronary artery disease. Thus, through their genotype, phenotype, and complex network of effect, platelets may be a significant mediator of MINOCA.
In addition, it is recognized that mental stress results in elevated measures of platelet activity. 85 Acquisition of validated measures of stress and depression in our cohort will permit us to shed light on the mechanistic pathways by which stress may increase cardiovascular risk. High perceived stress is associated with adverse outcomes following MI and helps explain poorer outcomes in women than men. 79 , 86 There are sex and gender differences in the experience and effects of stress, and evidence suggests that men with heart disease benefit more than women from psychosocial interventions that have been tested. 80 , 87 We adapted a group‐based mindfulness program that targets key stress‐related risk factors in women (eg, rumination, low social support) for telephone delivery, and are conducting a multicenter randomized, controlled trial to test its effects on perceived stress over 6 months. 88 Secondary outcomes include depressive symptoms, anxiety, quality of life, and sleep, assessed by 7 days of wrist actigraphy. Women with elevated stress levels ≥2 months post‐MI were recruited from 14 sites and via self‐referral. Of 488 women evaluated at the time of MI hospitalization, more than half reported high perceived stress. Although average stress levels declined at the 2‐month follow‐up, nearly half of women reported continued or newly elevated stress. 89 Enrolled participants (n=130) were randomized to stress management or heart disease education, an active control condition also delivered by telephone. Participants (33% racial/ethnic minorities, 27% MINOCA) reported high levels of current and past life stressors and clinically significant depressive symptoms at baseline. 90 Preliminary analysis of our baseline actigraphy data shows that poor sleep is common in this sample, particularly in Black women, and is associated with higher stress and depressive symptoms. 91 Satisfaction with the stress management program was high in women of all race/ethnic groups, but minority participants found the heart disease education program more helpful than did White participants. Our study is ongoing, but results will indicate whether there is benefit of a novel telephone‐based stress management program for post‐MI women.
UCSD: Sedentary Behavior and CVD Risk in Latina Women
Hispanic/Latinos are the largest minority population in the United States and have significantly elevated cardiometabolic risk. 92 Older Hispanic/Latino adults have elevated risk for cardiometabolic disease and accumulate high amounts of sedentary time. 93 , 94 , 95 Postmenopausal women may face a higher risk for cardiometabolic health and are understudied with respect to their physical activity and sedentary behaviors. In this regard, women of Mexican descent were shown to have higher levels of sedentary time than other Latina groups living in the United States, which may predispose them to higher CVD‐associated risk. 96 Therefore, the objective of the UCSD Women's Cardiovascular Health Research Center was to conduct contemporary and innovative translational research to better understand and provide relevant information to practitioners and public health officials on the risk factors, intervention methods for, and metabolic consequences of higher levels of sedentary behavior and sitting time among Latinas.
To examine biopsychosocial and ecological correlates of Latina women's sedentary behavior, our center leveraged data from 401 Mexican‐heritage women participating in the Hispanic Community Health Study/ Study of Latinos Casitas Ancillary Study. Examples of these potential correlates include time spent sitting in transportation, leisure, and screen time. In this study, and according to objectively measured data, participants were found to sit, on average, 5.65 h/day. Of this, women were most likely to spend time using screens (3.15 h/day), as compared with leisure time sitting (eg, knitting, talking with friends) (1.77 h/day) or transportation (1.02 h/day). Examining different dimensions of sitting behavior (such as locations of sedentary time) should be considered in future research among Latina women to determine behaviors that could be targeted for intervention.
There are few community‐based randomized clinical trials designed to reduce sedentary behavior or sitting time, and none among Latinas, who are particularly at risk for cardiometabolic diseases. Therefore, our center performed a 2‐arm randomized controlled trial testing a 12‐week sitting time‐reduction intervention aimed to reduce CVD risk. A total of 254 overweight, sedentary postmenopausal Latinas in San Diego were randomized to either an intervention group coached to replace sitting time with standing bouts or a comparison group that received heart health information. The intervention, based on social‐cognitive behavior change, included culturally tailored coaching. Intervention participants received 3 in‐person health‐counseling sessions, 1 home visit, and 5 telephone calls using motivational interviewing, whereas the comparison group received an equal number of contacts to discuss topics on healthy aging. The primary outcome was change in sitting time at 12 weeks, objectively measured via thigh‐worn inclinometers (activPAL). Our intervention was successful at reducing sitting time and increasing standing time and step counts in the intervention group, compared with the control (unpublished results). Furthermore, we demonstrated the feasibility and effectiveness of implementing sitting time reduction interventions among older, predominantly Spanish‐speaking postmenopausal Latinas.
Although sedentary behavior and sitting time are associated with risk for CVD and other chronic diseases, the molecular consequences of sitting are not well characterized, and mediators of the associated risk are unknown. Prior research indicates that extended sitting reduces blood flow velocity in the lower extremities, energy expenditure, and skeletal muscle contractility, 97 , 98 which can result in changes to physiologically active circulating molecules. 79 Therefore, we sought to characterize standard and novel molecular biomarkers and transducers of sitting time–associated CVD risk using biospecimens from our randomized trial.
In preparation for this, we initially studied associations of daily sitting time and mean sitting bout duration with cardiometabolic risk biomarkers using archival data and plasma samples among 518 postmenopausal women with overweight/obesity. 99 Sitting behaviors were determined objectively. In this sample, Hispanic women had shorter total sitting time (by 50.5 min/d) and mean sitting bout duration (by 3.6 min/bout), compared with non‐Hispanic women. Sitting time measures in the overall cohort were significantly associated with cardiometabolic disease risk factors, including greater body mass index, waist circumference, fasting blood glucose, insulin, and insulin resistance. The detrimental association between sitting bout duration and fasting blood glucose appeared to be greater in Hispanic women than in non‐Hispanic women (P interaction=0.03). 100
As endothelial dysfunction is associated with prolonged sitting, 97 , 98 , 101 we then profiled endothelial cell‐derived, CVD‐associated microRNAs contained in circulating CD144+ extracellular vesicles from women in the cohort described above. Plasma samples from select individuals in this cohort were used. Interrupted sitter and super sitter subgroups were defined by low moderate‐to‐vigorous physical activity and 2 extreme quartiles of mean sitting bout length (mean [SD] 25.5 [3.2] versus 65.0 [24.3] minutes, respectively, P<0.01). Levels of let‐7d‐5p, microRNA‐133b, and microRNA‐142‐3p were significantly greater in super sitters versus interrupted sitters. Pathway analyses suggest that these microRNAs mediate negative effects of prolonged sitting by targeting adrenergic signaling in cardiomyocytes, adherens junction, branched chain amino acid metabolism, and mucin type O‐glycan pathways. Analyses of other biomarkers associated with sitting time and sitting time change are ongoing.
In summary, the UCSD Women's Cardiovascular Health Research Center successfully designed and implemented a multidisciplinary and multilevel research program targeting an understudied minority population. Preliminary findings indicate that women of Mexican descent spend a significant amount of time engag ed in sedentary behavior, most of which is viewing a screen of some type, that the amount of time spent sitting can be reduced significantly by employing a behavioral intervention, and that accumulated sitting time is associated with certain cardiometabolic risk biomarkers. Therefore, reductions in sitting time may be particularly advantageous for Latinas, who are at high risk of CVD.
Findings From Soter Awards
CUIMC‐UCSD: Nightly Fasting and Eating Patterns and Cardiometabolic Risk in Hispanic/Latina Women
Alignment of eating patterns with endogenous circadian rhythms may play a role in CVD risk. Experimental studies demonstrate that time‐restricted feeding regimens that prolong nightly fasting duration and align eating patterns with 24‐hour light/dark cycles are associated with lower cardiometabolic risk. 102 , 103 Observational US studies are limited 104 , 105 , 106 due to the lack of time‐stamped diet data in most cohorts, which rely primarily on food frequency questionnaires for dietary assessment. To add to the knowledge from observational studies, we conducted a collaborative study to investigate nightly fasting duration and meal timing patterns, assessed using two 24‐hour recalls, in relation to cardiometabolic risk factors among ≈12 000 Hispanic/Latino adults, aged 18 to 76 years and free of cancer and diabetes mellitus at baseline, from the Hispanic Community Health Study/Study of Latinos. Given that eating patterns are dynamic and 2 nonconsecutive days may be insufficient to capture habitual eating patterns and assess weekday/weekend differences, we also conducted a prospective study nested within the CUIMC GRFW cohort. Dietary data were collected over 7 consecutive days using an electronic food record at baseline and 1‐year follow‐up in a subset of 116 women (mean age, 33 years; 45% Hispanic).
Contrary to our hypothesis but consistent with emerging observational data, 107 we found that a longer habitual nightly fasting duration was associated with higher adiposity and blood pressure in both cohorts. 108 On the other hand, as initially hypothesized, earlier timing and lower proportion of daily energy intake consumed at evening meals were associated with better cardiometabolic health. A greater proportion of daily energy intake consumed after 6 pm was associated with higher fasting glucose, insulin, and insulin resistance in the Hispanic Community Health Study/Study of Latinos. 109 Nighttime eaters who consumed ≥30% versus <30% of their daily energy intake after 6 pm, had greater odds of hypertension and prediabetes mellitus, with stronger associations among women.
In the GRFW cohort, an increase in percentage of daily calories consumed after 8 pm predicted higher adiposity. 108 Furthermore, later timing of the first eating occasion was related to poorer cardiovascular health and elevated blood pressure and fasting glucose. Eating jet lag, defined as the difference in mealtimes on work versus free days, was also related to cardiometabolic risk. 110 A greater difference between timing of the first eating occasion and nightly fasting duration on weekdays versus weekends was associated with higher body mass index, waist circumference, and blood pressure. Higher day‐to‐day variability in eating timing and nightly fasting duration was also related to poorer glycemic control and higher blood pressure. Overall, our findings suggest that earlier timing of the first eating occasion, reducing nighttime eating, and stabilizing eating timing patterns across days and between weekdays and weekends, may represent a novel lifestyle strategy for CVD prevention efforts in women. Findings warrant confirmation in multiethnic population‐based cohorts over longer follow‐up and testing of causality in sufficiently powered randomized controlled trials.
JHU‐UCSD: Integrating Metabolomics Into Deep Phenotyping of Heart Failure With Preserved Ejection Fraction
HFpEF, constituting half of heart failure today, is more common in women than men, and is associated with numerous comorbidities including hypertension, diabetes mellitus, and obesity. Though the clinical syndrome is often similar to HFrEF, and morbidity and mortality outcomes remain similar between the 2 types of heart failure, there remain no specific therapies for HFpEF with proven survival benefit. 111 The overall aim of this collaborative project was to investigate metabolomic signatures in myocardial tissue and serum from patients with HFpEF to better understand the underlying mechanisms of this syndrome. Our goal was to determine if patients with HFpEF have distinctive metabolomic profiles when compared with patients with HFrEF or controls, what features are shared, and what are characteristic of HFpEF. Secondly, we had speculated that patients with HFpEF with severe obesity will have a metabolomic signature that differentiates these patients from those with less severe obesity. We looked at subgroups within HFpEF to identify if there is a metabolism defect that can potentially help develop more precision‐guided therapeutics.
The results of the analysis yielded some surprising findings. Although there are many differences between HFpEF and controls, or HFrEF and controls, we found less disparity between the 2 forms of heart failure, as well as between preidentified subgroups within HFpEF. As of this writing, these results were just released, so the analysis is just beginning, and there will likely be far more detailed insights derived from the assay. However, the robustness of the profiles and consistency between patients is promising, and this work will undoubtedly advance the field of HFpEF research to better illuminate the underlying metabolic defects that are involved. Bioinformatic analyses to correlate deep clinical phenotyping features with these metabolomic signatures is ongoing.
NYU‐UCSD: Evaluating a Mindfulness‐Based Intervention for Diverse Prehypertensive Women
Hypertension is a major modifiable risk factor for CVD. 112 Interventions that target prehypertension can prevent or delay progression to hypertension and thereby reduce CVD risk. 113 Mindfulness‐based interventions reduce blood pressure, but applications to women of different racial and ethnic groups are unknown. 114 , 115 The aims of this study were to adapt the telephone‐based mindfulness intervention developed at the NYU GRFW center for the Latina population, and to evaluate its feasibility, acceptability, and effects in diverse women with prehypertension.
We conducted focus groups with 64 Spanish‐speaking Latina participants recruited from a large federally‐qualified health center in the United States–Mexico border region of San Diego, California and from NYU Langone and Bellevue Hospital in New York City. 116 Women were generally middle‐aged, native Spanish speakers, born outside the United States, primarily from Mexico in San Diego, and from the Dominican Republic, Ecuador, and Puerto Rico in New York City. The majority of participants at both sites expressed interest in learning stress management skills, though more women in New York City than San Diego indicated they would likely participate in a phone‐based program with other Latina women. Participant feedback informed modifications to the program materials and study protocols.
We then conducted a 2‐site pilot randomized controlled trial in which 84 women with prehypertension (n=47 in San Diego; n=37 in New York City) were randomized to the mindfulness program or usual care. Outcomes included feasibility (session completion, retention rates), acceptability (satisfaction ratings), and 3‐month changes in blood pressure, perceived stress, and depressive symptoms. Women at the 2 sites had a similar average age and baseline blood pressure. The San Diego sample was primarily foreign born and 97% primarily Spanish speaking, whereas the New York City sample was racially and ethnically diverse. Session completion was good, and satisfaction ratings and retention rates were high at both sites. Follow‐up data collection was recently completed. Preliminary analyses do not indicate intervention effects on systolic blood pressure, but women assigned to the mindfulness program showed greater reductions in perceived stress and depressive symptoms than those assigned to usual care.
Overall, results support the feasibility and acceptability of telephone‐based mindfulness training in diverse women with prehypertension, and preliminary findings for stress and depressive symptoms suggest this may be a promising strategy. Investigating the role of cultural factors and diversity within the Latina population may inform improvements to enhance engagement and efficacy of the intervention.
NYU‐UCSD: Correlates of Behavioral and Anthropometric Risk Factors for Cardiovascular Disease in Asian American Women: A Collaborative Training Proposal
Physical inactivity, sedentary behavior, and short sleep duration are recognized as independent CVD risk factors. 117 These behaviors are interrelated and proportionally allocated in each 24‐hour period, 118 but little is known about their unique and combined impact on CVD risk, particularly using objective measures. Asian American women are less likely to engage in optimal levels of physical activity or to have adequate sleep duration compared with Asian American men, 119 which may contribute to CVD disparities. The immigration experience disrupts family and social networks, causes financial hardships, and increases exposure to discrimination, 120 all of which may interfere with health‐promoting behaviors. 121 , 122 Identifying determinants of lifestyle behaviors in Asian immigrant women would inform the development of tailored behavioral interventions that can reduce CVD risk in this understudied group. In this study, we investigated 24‐hour activity patterns in healthy Asian American women and examined correlates of physical activity, sedentary behavior, and sleep. Middle‐aged normotensive women from 4 Asian subgroups (Chinese, Korean, Bengali, Filipino) were recruited from ethnic faith‐ and community‐based organizations in New York City. Participants completed self‐report questionnaires and 7 days of wrist and hip actigraphy to measure sleep duration, moderate–vigorous physical activity, light physical activity, and sedentary behavior. The sample of 75 women with valid data showed suboptimal levels of physical activity and sleep. 123 As expected, more moderate–vigorous physical activity and longer sleep duration were significantly associated with lower body mass index. Using isotemporal substitution models, we found that replacing 30 minutes of sedentary behavior or light physical activity with moderate–vigorous physical activity or sleep was associated with significant reductions in body mass index and waist circumference. 124 We also found acculturation and discrimination were associated with less physical activity and poorer sleep. 98 More frequent everyday discrimination was associated with shorter sleep duration and poorer sleep quality. These findings suggest that culturally tailored strategies to improve lifestyle behaviors may reduce CVD risk in Asian American immigrant women. We are also applying these methods to the actigraphy data collected in our stress management trial. 125 Findings will advance our understanding of correlates of physical activity in post‐MI women and of the potential impact of stress management on physical activity patterns.
Faculty and Fellow Outcomes
The SFRN structure is meant to foster cross‐disciplinary interactions and promote the development of leaders in women's health research. Throughout the network, research principal investigators have been successful in obtaining additional independent and collaborative funding from the AHA as well as the National Institutes of Health. Of note, the CUIMC team established a sleep center of excellence to promote sleep and circadian rhythms education and research across the institution. Investigators obtained new R01 Research Grants, an AHA collaborative grant with JHU, and a Research Goes Red grant. The JHU center was renewed to study cardiac sarcomere dysfunction in HFpEF, and JHU received 3 additional SFRN grants from the AHA, namely in obesity, health technologies, and innovation, and cardiometabolic health/diabetes networks. The Magee‐Womens Research Institute and Foundation (MWRIF) center was renewed to study the effects of perinatal stress‐related mood disorders on cardiovascular health, and the NYU center was renewed with expanded aims addressing sex as a biological variable affecting MI pathogenesis, platelet activity, and signaling pathways, and the perception and impact of stress. AHA also funded a diabetes SFRN grant to NYU. UCSD obtained a P01 grant from the National Institutes of Health to study cardiometabolic health effects of interrupting sitting among postmenopausal women.
In addition, each center within the network trained 3 postdoctoral fellows in multidisciplinary research related to CVD in women, and provided mentorship to graduate students and other non–SFRN‐named fellows (Table). Network fellows were highly successful in obtaining pilot awards, career development grants (K99/R00, K01, K23), and faculty positions at academic institutions across the United States.
Table 1.
Educational Contributions of the Go Red for Women Network
| Network Outcomes | No. |
|---|---|
| Fellows trained | 20 |
| Other nonfellow trainees | 25 |
| Graduate students | 19 |
| Medical fellows | 6 |
| Publications | 121 |
| Original | 84 |
| Reviews | 37 |
| Abstracts | 145 |
| Grants | 14 |
| Pilot research | 6 |
| Career development | 9 |
The intent of the GRFW network was to accelerate the generation of important, novel ideas and yield important gains in knowledge and research capacity. From their close collaboration and harmonization of various research methods, including questionnaires and tools to assess pregnancy history, stress, sleep, and sharing of novel research methods, research programs were enhanced and additional grant funding secured (Figure). Overall, our network successfully trained the next cadre of scientists and propelled the careers of academic leaders in the field of women's cardiovascular health, in addition to enhancing the evidence base and awareness related to heart disease in women. The findings generated by the network, and the new investigators trained in multidisciplinary research, will further promote awareness in both the public and medical field, of the female‐specific factors that influence CVD.
Figure 1. Collaboration and training outcomes of the Go Red for Women network.
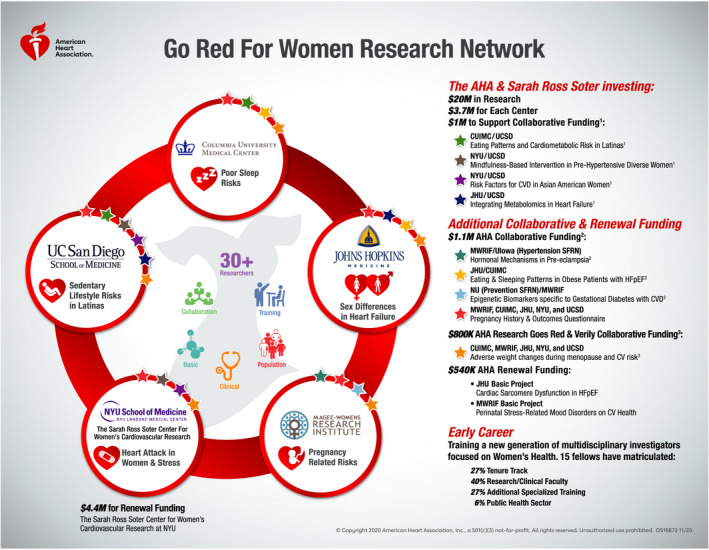
Stars represent additional ancillary collaborative awards between centers. 1Sarah Ross Soter provided $1 million to support collaborative awards (Soter awards) between Columbia University Irving Medical Center (CUIMC) and University of California at San Diego (UCSD), New York University (NYU) and UCSD (2 awards), and Johns Hopkins University (JHU) and UCSD. 2Additional collaborative awards was funded by the American Heart Association (AHA) to support internetwork collaborations between the Magee‐Womens Research Institute and Foundation (MWRIF) and University of Iowa [UIowa], JHU and CUIMC, Northwestern University (NU) and MWRIF, and MWRIF, CUIMC, JHU, NYU, and UCSD. 3AHA and Verily collaborative funding was provided to all 5 centers within the Go Red for Women network. CVD, cardiovascular disease. ©Copyright 2020 American Heart Association, Inc. Reproduced with permission.
Sources of Funding
This work was funded by AHA 16SFRN27950012 (St‐Onge), AHA 16SFRN27960002 and 16SFRN29940002 (Allison), AHA 16SFRN27960011 and AHA 811531 (Aggarwal), AHA 16SFRN28739992 (Berger), AHA 16SFRN27940007 (Castenada, Talavera), AHA 16SFRN28930000 (Catov), AHA 16SFRN27810006 (Hochman), AHA 16SFRN27810001 and AHA 16SFRN28340000 (Hubel), AHA 16SFRN29050000 and NIH R01HL106041 (Jelic), AHA 16SFRN2862000 (Kass), AHA 16SFRN27880000‐1 and NIH K99HL148511 (Makarem), AHA 16SFRN27880000 (Mosca), 16SFRN27870000 (Ouyang), AHA 16SFRN27810006 (Park), 16SFRN28680004 (Post), AHA 16SFRN27860002 (Powers), AHA 16SFRN28730004 (Reynolds), AHA 16SFRN28420000 (Sears), AHA 16SFRN28780016 and NIH R01HL107577, R01HL127028, R01HL140731, and R01HL149423 (Shah), AHA 16SFRN28850003 (Spruill).
Disclosures
Dr Kass is coinventor on a submitted patent on the use of PDE9A inhibitors to treat obesity and related cardiometabolic disorders (Patent Cooperation Treaty submitted, patent pending). Dr Reynolds reports in‐kind support from Abbott Vascular and Siemens related to this publication and in‐kind support from BioTelemetry for an unrelated project. Dr Shah reports receiving grant funding from the, Actelion, AstraZeneca, Corvia, Novartis, and Pfizer; and consulting fees from Abbott, Actelion, Amgen, Aria CV, AstraZeneca, Axon Therapies, Bayer, Boehringer‐Ingelheim, Boston Scientific, Bristol Myers Squibb, Coridea, Cyclerion, Cytokinetics, Edwards, Eisai, Imara, Ionis, Ironwood, Lilly, Merck, MyoKardia, Novartis, Novo Nordisk, Pfizer, Regeneron, Sanofi, Shifamed, and United Therapeutics. The remaining authors have no disclosures to report.
(J Am Heart Assoc. 2021;10:e019519. DOI: 10.1161/JAHA.120.019519.)
For Sources of Funding and Disclosures, see page 12.
REFERENCES
- 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245.DOI: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118:1273–1293.DOI: 10.1161/CIRCRESAHA.116.307547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Agarwala A, Michos ED, Samad Z, Ballantyne CM, Virani SS. The use of sex‐specific factors in the assessment of women's cardiovascular risk. Circulation. 2020;141:592–599.DOI: 10.1161/CIRCULATIONAHA.119.043429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mosca L, Ouyang P, Hubel CA, Reynolds HR, Allison MA. Go red for women Strategically Focused Research Network centers. Circulation. 2017;135:609–611.DOI: 10.1161/CIRCULATIONAHA.116.025955. [DOI] [PubMed] [Google Scholar]
- 5. Ford ES. Habitual sleep duration and predicted 10‐year cardiovascular risk using the pooled cohort risk equations among US adults. J Am Heart Assoc. 2014;3:e001454. DOI: 10.1161/JAHA.114.001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang Y, Mei H, Jiang YR, Sun WQ, Song YJ, Liu SJ, Jiang F. Relationship between duration of sleep and hypertension in adults: a meta‐analysis. J Clin Sleep Med. 2015;11:1047–1056.DOI: 10.5664/jcsm.5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Domínguez F, Fuster V, Fernández‐Alvira JM, Fernández‐Friera L, López‐Melgar B, Blanco‐Rojo R, Fernández‐Ortiz A, García‐Pavía P, Sanz J, Mendiguren JM, et al. Association of sleep duration and quality with subclinical atherosclerosis. J Am Coll Cardiol. 2019;73:134–144.DOI: 10.1016/j.jacc.2018.10.060. [DOI] [PubMed] [Google Scholar]
- 8. Meisinger C, Heier M, Lowel H, Schneider A, Doring A. Sleep duration and sleep complaints and risk of myocardial infarction in middle‐aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30:1121–1127.DOI: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aggarwal B, Makarem N, Shah R, Emin M, Wei Y, St‐Onge MP, Jelic S. Effects of inadequate sleep on blood pressure and endothelial inflammation in women: findings from the American Heart Association Go Red for Women Strategically Focused Research Network. J Am Heart Assoc. 2018;7:e008590. DOI: 10.1161/JAHA.118.008590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Makarem N, St‐Onge MP, Liao M, Lloyd‐Jones DM, Aggarwal B. Association of sleep characteristics with cardiovascular health among women and differences by race/ethnicity and menopausal status: findings from the American Heart Association Go Red for Women Strategically Focused Research Network. Sleep Health. 2019;5:501–508.DOI: 10.1016/j.sleh.2019.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Makarem N, Paul J, Giardina EV, Liao M, Aggarwal B. Evening chronotype is associated with poor cardiovascular health and adverse health behaviors in a diverse population of women. Chronobiol Int. 2020;37:673–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zuraikat FM, Makarem N, Liao M, St‐Onge MP, Aggarwal B. Measures of poor sleep quality are associated with higher energy intake and poor diet quality in a diverse sample of women from the Go Red for Women Strategically Focused Research Network. J Am Heart Assoc. 2020;9:e014587. DOI: 10.1161/JAHA.119.014587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mayat Z, Giardina EV, Liao M, Aggarwal B. Associations of inflammation, physical activity, and sleep in a diverse population of women. J Womens Health (Larchmt). 2020;29:1007–1016.DOI: 10.1089/jwh.2019.7663. [DOI] [PubMed] [Google Scholar]
- 14. Aggarwal B, Makarem N, Liao M, Mayat Z, Byun S, Giardina EG. Psychosocial factors are strongly associated with sleep disturbances and evening chronotype among diverse women: evidence from the AHA Go Red for Women Strategically Focused Research Network. Circulation. 2019;139:AP281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. St‐Onge MP, Grandner MA, Brown D, Conroy MB, Jean‐Louis G, Coons M, Bhatt DL; American Heart Association Obesity BCD, Nutrition Committees of the Council on L, Cardiometabolic H, Council on Cardiovascular Disease in the Y, Council on Clinical C and Stroke C . Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. 2016;134:e367–e386.DOI: 10.1161/CIR.0000000000000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38:843–844.DOI: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang H, Haack M, Gautam S, Meier‐Ewert HK, Mullington JM. Repetitive exposure to shortened sleep leads to blunted sleep‐associated blood pressure dipping. J Hypertens. 2017;35:1187–1194.DOI: 10.1097/HJH.0000000000001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buxton OM, Pavlova M, Reid EW, Wang W, Simonson DC, Adler GK. Sleep restriction for 1 week reduces insulin sensitivity in healthy men. Diabetes. 2010;59:2126–2133.DOI: 10.2337/db09-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. St‐Onge MP, Campbell A, Aggarwal B, Taylor JL, Spruill TM, RoyChoudhury A. Mild sleep restriction increases 24‐hour ambulatory blood pressure in premenopausal women with no indication of mediation by psychological effects. Am Heart J. 2020;223:12–22.DOI: 10.1016/j.ahj.2020.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. St‐Onge MP, Campbell A, Zuraikat F, Cheng B, Shah R, Berger JS, Sampogna RV, Jelic S. Impact of change in bedtime variability on body composition and inflammation: secondary findings from the Go Red for Women Strategically Focused Research Network. Int J Obes (Lond). 2020;44:1803–1806.DOI: 10.1038/s41366-020-0555-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17.DOI: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shah SJ, Borlaug BA, Kitzman DW, McCulloch AD, Blaxall BC, Agarwal R, Chirinos JA, Collins S, Deo RC, Gladwin MT, et al. Research priorities for heart failure with preserved ejection fraction: National Heart, Lung, and Blood Institute Working Group Summary. Circulation. 2020;141:1001–1026.DOI: 10.1161/CIRCULATIONAHA.119.041886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Beale AL, Meyer P, Marwick TH, Lam CSP, Kaye DM. Sex differences in cardiovascular pathophysiology: why women are overrepresented in heart failure with preserved ejection fraction. Circulation. 2018;138:198–205.DOI: 10.1161/CIRCULATIONAHA.118.034271. [DOI] [PubMed] [Google Scholar]
- 24. Dunkerly‐Eyring B, Kass DA. Myocardial phosphodiesterases and their role in cGMP regulation. J Cardiovasc Pharmacol. 2020;75:483–493.DOI: 10.1097/FJC.0000000000000773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Subramanya V, Zhao DI, Ouyang P, Lima JA, Vaidya D, Ndumele CE, Bluemke DA, Shah SJ, Guallar E, Nwabuo CC, et al. Sex hormone levels and change in left ventricular structure among men and post‐menopausal women: the Multi‐Ethnic Study of Atherosclerosis (MESA). Maturitas. 2018;108:37–44.DOI: 10.1016/j.maturitas.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Subramanya V, Ambale‐Venkatesh B, Ohyama Y, Zhao DI, Nwabuo CC, Post WS, Guallar E, Ouyang P, Shah SJ, Allison MA, et al. Relation of sex hormone levels with prevalent and 10‐year change in aortic distensibility assessed by MRI: the Multi‐Ethnic Study of Atherosclerosis. Am J Hypertens. 2018;31:774–783.DOI: 10.1093/ajh/hpy024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Subramanya V, Zhao D, Ouyang P, Ying W, Vaidya D, Ndumele CE, Heckbert SR, Budoff MJ, Post WS, Michos ED. Association of endogenous sex hormone levels with coronary artery calcium progression among post‐menopausal women in the Multi‐Ethnic Study of Atherosclerosis (MESA). J Cardiovasc Comput Tomogr. 2019;13:41–47.DOI: 10.1016/j.jcct.2018.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ying W, Zhao DI, Ouyang P, Subramanya V, Vaidya D, Ndumele CE, Sharma K, Shah SJ, Heckbert SR, Lima JA, et al. Sex hormones and change in N‐terminal pro‐B‐type natriuretic peptide levels: the Multi‐Ethnic Study of Atherosclerosis. J Clin Endocrinol Metab. 2018;103:4304–4314.DOI: 10.1210/jc.2018-01437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mathews L, Subramanya V, Zhao DI, Ouyang P, Vaidya D, Guallar E, Yeboah J, Herrington D, Hays AG, Budoff MJ, et al. Endogenous sex hormones and endothelial function in postmenopausal women and men: the Multi‐Ethnic Study of Atherosclerosis. J Womens Health (Larchmt). 2019;28:900–909.DOI: 10.1089/jwh.2018.7441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ying W, Zhao DI, Ouyang P, Subramanya V, Vaidya D, Ndumele CE, Guallar E, Sharma K, Shah SJ, Kass DA, et al. associations between the cyclic guanosine monophosphate pathway and cardiovascular risk factors: MESA. J Am Heart Assoc. 2019;8:e013149. DOI: 10.1161/JAHA.119.013149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhao DI, Guallar E, Vaidya D, Ndumele CE, Ouyang P, Post WS, Lima JA, Ying W, Kass DA, Hoogeveen RC, et al. Cyclic guanosine monophosphate and risk of incident heart failure and other cardiovascular events: the ARIC study. J Am Heart Assoc. 2020;9:e013966. DOI: 10.1161/JAHA.119.013966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Subramanya V, Ying W, Zhao D, Vaidya D, Ndumele CE, Lima JA, Ouyang P, Hoogeveen RC, Shah SJ, Heckbert SR, et al. Abstract 12012: lower circulating levels of cyclic guanosine monophosphate are associated with greater concentric left ventricular remodeling in the Multi‐Ethnic Study of Atherosclerosis. Circulation. 2018;138:A12012–A12012. [Google Scholar]
- 33. Heravi A, Michos ED, Zhao D, Ambale‐Venkatesh B, De Vasconcellos HD , Lloyd‐Jones D, Schreiner P, Reis J, Lewis CE, Sidney S, et al. Associations between urinary isoprostane levels and menopausal status in the Coronary Artery Risk Development In Young Adults (CARDIA) Study. Circulation. 2019;140:A13792. [Google Scholar]
- 34. Heravi A, Michos ED, Zhao D, Ambale‐Venkatesh B, De Vasconcellos HD , Lloyd‐Jones D, Schreiner P, Reis J, Lewis CE, Sidney S, et al. Post. characterization of urinary isoprostanes vs. cardiovascular risk factors in the Coronary Artery Risk Development Young Adults (CARDIA) cohort. Circulation. 2019;140 (abstract). [Google Scholar]
- 35. Hahn VS, Yanek LR, Vaishnav J, Ying W, Vaidya D, Lee YZJ, Riley SJ, Subramanya V, Brown EE, Hopkins CD, et al. Endomyocardial biopsy characterization of heart failure with preserved ejection fraction and prevalence of cardiac amyloidosis. JACC Heart Fail. 2020;8:712–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hahn VS, Yanek LR, Vaishnav J, Ying W, Vaidya DM, Lee YZJ, Riley SJ, Subramanya V, Brown EE, Hopkins CD, et al. endomyocardial biopsy characterization of heart failure with preserved ejection fraction and prevalence of cardiac amyloidosis. JACC Heart Fail. 2020;8:712–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hahn VS, Knutsdottir H, Luo X, Bedi K, Margulies KB, Haldar SM, Stolina M, Yin J, Khakoo AY, Vaishnav J, et al. Myocardial gene expression signatures in human heart failure with preserved ejection fraction. Circulation. 2020. Oct 29 [epub ahead of print]. DOI: 10.1161/CIRCULATIONAHA.120.050498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Aslam MI, Hahn VS, Jani V, Hsu S, Sharma K, Kass DA. Reduced right ventricular sarcomere contractility in HFpEF with severe obesity. Circulation. 2020. Dec 20 [epub ahead of print]. DOI: 10.1161/CIRCULATIONAHA.120.052414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ying W, Sharma K, Subramanya V, Dvorak SJ, Bach ME, Soleimanifard S, Vaidya D, Michos ED, Shah SJ, Hays A. Visceral adiposity is increased in patients with heart failure with preserved ejection fraction. Circulation. 2018;138:A15394–A15394 (abstract). [Google Scholar]
- 40. Mishra S, Zhu G, Rodriguez S, Wong W. Cardiometabolic profile in female mice independent of estrogen status. Circ Res. 2019;125:A18(abstract). [Google Scholar]
- 41. Eaker ED, Chesebro JH, Sacks FM, Wenger NK, Whisnant JP, Winston M. Cardiovascular disease in women. Circulation. 1993;88:1999–2009.DOI: 10.1161/01.CIR.88.4.1999. [DOI] [PubMed] [Google Scholar]
- 42. Anderson GL, Limacher M, Assaf AR, Bassford T, Beres ford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. [see comment]. JAMA. 2004;291:1701–1712. [DOI] [PubMed] [Google Scholar]
- 43. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. [see comment]. JAMA. 2002;288:321–333. [DOI] [PubMed] [Google Scholar]
- 44. Alexandersen P, Karsdal MA, Christiansen C. Long‐term prevention with hormone‐replacement therapy after the menopause: which women should be targeted? Womens Health. 2009;5:637–647.DOI: 10.2217/WHE.09.52. [DOI] [PubMed] [Google Scholar]
- 45. Mosca L, Manson JE, Sutherland SE, Langer RD, Manolio T, Barrett‐Connor E. Cardiovascular disease in women: a statement for healthcare professionals from the American Heart Association. Writing Group. Circulation. 1997;96:2468–2482.DOI: 10.1161/01.CIR.96.7.2468. [DOI] [PubMed] [Google Scholar]
- 46. Irgens HU, Reisaeter L, Irgens LM, Lie RT. Long term mortality of mothers and fathers after pre‐eclampsia: population based cohort study. BMJ. 2001;323:1213–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Freibert SM, Mannino DM, Bush H, Crofford LJ. The association of adverse pregnancy events and cardiovascular disease in women 50 years of age and older. J Womens Health (Larchmt). 2011;20:287–293.DOI: 10.1089/jwh.2010.2097. [DOI] [PubMed] [Google Scholar]
- 48. Germain AM, Romanik MC, Guerra I, Solari S, Reyes MS, Johnson RJ, Price K, Karumanchi SA, Valdes G. Endothelial dysfunction: a link among preeclampsia, recurrent pregnancy loss, and future cardiovascular events? [see comment]. Hypertension. 2007;49:90–95.DOI: 10.1161/01.HYP.0000251522.18094.d4. [DOI] [PubMed] [Google Scholar]
- 49. Jacobs MB, Kritz‐Silverstein D, Wingard DL, Barrett‐Connor E. The association of reproductive history with all‐cause and cardiovascular mortality in older women: the Rancho Bernardo Study. Fertil Steril. 2012;97:118–124.DOI: 10.1016/j.fertnstert.2011.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lykke JA, Langhoff‐Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944–951.DOI: 10.1161/HYPERTENSIONAHA.109.130765. [DOI] [PubMed] [Google Scholar]
- 51. Magnussen EB, Vatten LJ, Smith GD, Romundstad PR. Hypertensive disorders in pregnancy and subsequently measured cardiovascular risk factors. Obstet Gynecol. 2009;114:961–970.DOI: 10.1097/AOG.0b013e3181bb0dfc. [DOI] [PubMed] [Google Scholar]
- 52. Romundstad PR, Magnussen EB, Smith GD, Vatten LJ. Hypertension in pregnancy and later cardiovascular risk: common antecedents? Circulation. 2010;122:579–584.DOI: 10.1161/CIRCULATIONAHA.110.943407. [DOI] [PubMed] [Google Scholar]
- 53. Smith GN, Walker MC, Liu A, Wen SW, Swansburg M, Ramshaw H, White RR, Roddy M, Hladunewich M; Pre‐Eclampsia New Emerging T . A history of preeclampsia identifies women who have underlying cardiovascular risk factors. Am J Obstet Gynecol. 2009;200:58.e1–58.e8.DOI: 10.1016/j.ajog.2008.06.035. [DOI] [PubMed] [Google Scholar]
- 54. Parks WT. Placental hypoxia: the lesions of maternal malperfusion. Semin Perinatol. 2015;39:9–19.DOI: 10.1053/j.semperi.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 55. Assibey‐Mensah V, Parks WT, Gernand AD, Catov JM. Race and risk of maternal vascular malperfusion lesions in the placenta. Placenta. 2018;69:102–108.DOI: 10.1016/j.placenta.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 56. Kalinowski J, Taylor JY, Spruill TM. Why are young black women at high risk for cardiovascular disease? Circulation. 2019;139:1003–1004.DOI: 10.1161/CIRCULATIONAHA.118.037689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hauspurg A, Redman EK, Assibey‐Mensah V, Tony Parks W, Jeyabalan A, Roberts JM, Catov JM. Placental findings in non‐hypertensive term pregnancies and association with future adverse pregnancy outcomes: a cohort study. Placenta. 2018;74:14–19.DOI: 10.1016/j.placenta.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 58. Atlass J, Menke M, Parks WT, Catov JM. Pre‐conception blood pressure and evidence of placental malperfusion. BMC Pregnancy Childbirth. 2020;20:25. DOI: 10.1186/s12884-019-2699-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Catov J, Assibey‐Mensah V, Muldoon MF, Sun B, Parks WT. Maternal vascular lesions in the placenta may identify women susceptible to masked hypertension a decade after delivery. Circulation. 2019;139:AMP65. [Google Scholar]
- 60. Hauspurg A, Brands J, Gandley RE, Parks W, Hubel C, Catov JM. Evidence of impaired microvascular function a decade after delivery in women with placental malperfusion lesions. Circulation. 2020;141:AMP61. [Google Scholar]
- 61. Countouris ME, Catov Janet M, de Jong N, Brands J, Chen X, Berlacher K, Villanueva FS. Hypertensive disorders of pregnancy and placental maternal vascular malperfusion lesions are associated with abnormal coronary microvascular function 8 to 10 years after delivery. J Am Coll Cardiol. 2020;75:1660. [Google Scholar]
- 62. Gandley R, Brands J, Jeyabalan A, Hauspurg A, McGonigal S, Hubel C. Reduced barrier function of the microvascular endothelial glycocalyx in women with a history of preeclampsia, one year after delivery. Pregnancy Hypertens. 2018;13:S99. [Google Scholar]
- 63. Hauspurg A, Brands J, Gandley RE, Redman EK, Simhan HN, Jeyabalan A, Hubel CA. Increased peripheral vascular resistance and arterial stiffness one year after preeclampsia. Am J Obstet Gynecol. 2019;220:S287–S288. [Google Scholar]
- 64. Singh J, Ahmed A, Girardi G. Role of complement component C1q in the onset of preeclampsia in mice. Hypertension. 2011;58:716–724.DOI: 10.1161/HYPERTENSIONAHA.111.175919. [DOI] [PubMed] [Google Scholar]
- 65. Sutton EF, Gemmel M, Brands J, Gallaher MJ, Powers RW. Paternal deficiency of complement component C1q leads to a preeclampsia‐like pregnancy in wild‐type female mice and vascular adaptations postpartum. Am J Physiol Regul Integr Comp Physiol. 2020;318:R1047–R1057.DOI: 10.1152/ajpregu.00353.2019. [DOI] [PubMed] [Google Scholar]
- 66. Sutton EF, Gemmel M, Gallaher MJ, Powers R. Early vascular dysfunction in mouse offspring exposed to a preeclampsia‐like intrauterine environment. Reprod Sci. 2019;26:A62–A390. [Google Scholar]
- 67. Cunningham MW Jr, LaMarca B. Risk of cardiovascular disease, end‐stage renal disease, and stroke in postpartum women and their fetuses after a hypertensive pregnancy. Am J Physiol Regul Integr Comp Physiol. 2018;315:R521–R528.DOI: 10.1152/ajpregu.00218.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Catov JM, Newman AB, Sutton‐Tyrrell K, Harris TB, Tylavsky F, Visser M, Ayonayon HN, Ness RB. Parity and cardiovascular disease risk among older women: how do pregnancy complications mediate the association? Ann Epidemiol. 2008;18:873–879.DOI: 10.1016/j.annepidem.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Lawlor DA, Emberson JR, Ebrahim S, Whincup PH, Wannamethee SG, Walker M, Smith GD. Is the association between parity and coronary heart disease due to biological effects of pregnancy or adverse lifestyle risk factors associated with child‐rearing? Findings from the British Women's Heart and Health Study and the British Regional Heart Study. Circulation. 2003;107:1260–1264.DOI: 10.1161/01.CIR.0000053441.43495.1A. [DOI] [PubMed] [Google Scholar]
- 70. Humphries KH, Westendorp ICD, Bots ML, Spinelli JJ, Carere RG, Hofman A, Witteman JCM. Parity and carotid artery atherosclerosis in elderly women. Stroke. 2001;32:2259–2264.DOI: 10.1161/hs1001.097224. [DOI] [PubMed] [Google Scholar]
- 71. Palmer JR, Rosenberg L, Shapiro S. Reproductive factors and risk of myocardial infarction. Am J Epidemiol. 1992;136:408–416. 10.1093/oxfordjournals.aje.a116513 [DOI] [PubMed] [Google Scholar]
- 72. Ness RB, Harris T, Cobb J, Flegal KM, Kelsey JL, Balanger A, Stunkard AJ, D'Agostino RB. Number of pregnancies and the subsequent risk of cardiovascular disease. N Engl J Med. 1993;328:1528–1533.DOI: 10.1056/NEJM199305273282104. [DOI] [PubMed] [Google Scholar]
- 73. Brands J, Gallaher MJ, Powers RW. Multiple prior pregnancy significantly impairs maternal vascular function postpartum. Reprod Sci. 2018;25:A55–A324. [Google Scholar]
- 74. Koeners MP, van Faassen EE, Wesseling S, de Sain‐van der Velden M, Koomans HA, Braam B, Joles JA. Maternal supplementation with citrulline increases renal nitric oxide in young spontaneously hypertensive rats and has long‐term antihypertensive effects. Hypertension. 2007;50:1077–1084.DOI: 10.1161/HYPERTENSIONAHA.107.095794. [DOI] [PubMed] [Google Scholar]
- 75. Gemmel M, Sutton E, Brands J, Burnette L, Gallaher MJ, Powers RW. L‐citrulline supplementation during pregnancy improves perinatal and postpartum maternal vascular function in a mouse model of preeclampsia. Am J Physiol Regul Integr Comp Physiol. 2020;(in revision). [DOI] [PubMed] [Google Scholar]
- 76. Smilowitz NR, Mahajan AM, Roe MT, Hellkamp AS, Chiswell K, Gulati M, Reynolds HR. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION Registry‐GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry‐Get With the Guidelines). Circ Cardiovasc Qual Outcomes. 2017;10:e003443. DOI: 10.1161/CIRCOUTCOMES.116.003443. [DOI] [PubMed] [Google Scholar]
- 77. Tamis‐Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, Lerman A, Cushman M, Kumbhani DJ, Arslanian‐Engoren C, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139:e891–e908.DOI: 10.1161/CIR.0000000000000670. [DOI] [PubMed] [Google Scholar]
- 78. Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, et al. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol. 1995;26:1235–1241.DOI: 10.1016/0735-1097(95)00327-4. [DOI] [PubMed] [Google Scholar]
- 79. Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D’Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, et al. Sex differences in perceived stress and early recovery in young and middle‐aged patients with acute myocardial infarction. Circulation. 2015;131:614–623.DOI: 10.1161/CIRCULATIONAHA.114.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Xu X, Bao H, Strait KM, Edmondson DE, Davidson KW, Beltrame JF, Bueno H, Lin H, Dreyer RP, Brush JE, et al. Perceived stress after acute myocardial infarction: a comparison between young and middle‐aged women versus men. Psychosom Med. 2017;79:50–58.DOI: 10.1097/PSY.0000000000000429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, Nordenskjold A, Gard A, Jernberg T. Medical therapy for secondary prevention and long‐term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation. 2017;135:1481–1489.DOI: 10.1161/CIRCULATIONAHA.116.026336. [DOI] [PubMed] [Google Scholar]
- 82. Reynolds HR, Maehara A, Kwong RY, Sedlak T, Saw J, Smilowitz NR, Mahmud E, Wei J, Marzo K, Matsumura M, et al. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of MINOCA in women. Circulation. 2020. Nov 14 [epub ahead of print]. DOI: 10.1161/CIRCULATIONAHA.120.052008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Reynolds HR, Maehara A, Kwong R, Sedlak T, Saw J, Smilowitz N, Mahmud E, Wei J, Marzo K, Matsumura M, et al. Coronary OCT and cardiac MRI to determine underlying causes of MINOCA in women. Abstract Presented at American Heart Scientific Session Nov 2020. Paper presented at: AHA Scientifc Sessions 2020; 2020; Virtual Conference.
- 84. Barrett TJ, Lee AH, Smilowitz NR, Hausvater A, Fishman GI, Hochman JS, Reynolds HR, Berger JS. Whole‐blood transcriptome profiling identifies women with myocardial infarction with nonobstructive coronary artery disease. Circ Genom Precis Med. 2018;11:e002387. DOI: 10.1161/CIRCGEN.118.002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wallen NH, Held C, Rehnqvist N, Hjemdahl P. Effects of mental and physical stress on platelet function in patients with stable angina pectoris and healthy controls. Eur Heart J. 1997;18:807–815.DOI: 10.1093/oxfordjournals.eurheartj.a015346. [DOI] [PubMed] [Google Scholar]
- 86. Arnold SV, Smolderen KG, Buchanan DM, Li Y, Spertus JA. Perceived stress in myocardial infarction: long‐term mortality and health status outcomes. J Am Coll Cardiol. 2012;60:1756–1763.DOI: 10.1016/j.jacc.2012.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Linden W, Phillips MJ, Leclerc J. Psychological treatment of cardiac patients: a meta‐analysis. Eur Heart J. 2007;28:2972–2984.DOI: 10.1093/eurheartj/ehm504. [DOI] [PubMed] [Google Scholar]
- 88. Spruill TM, Reynolds HR, Dickson VV, Shallcross AJ, Visvanathan PD, Park C, Kalinowski J, Zhong H, Berger JS, Hochman JS, et al. Telephone‐based mindfulness training to reduce stress in women with myocardial infarction: rationale and design of a multicenter randomized controlled trial. Am Heart J. 2018;202:61–67.DOI: 10.1016/j.ahj.2018.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kalinowski J, Park C, Hausvater A, Smilowitz NR, Pacheco C, Herscovici R, Wei J, Toma C, Mehta L, Dickson VV, et al. Predictors of perceived stress in women after acute recovery from myocardial infarction. Circulation. 2018;138:A15115. [Google Scholar]
- 90. Sperber SH, Duberstein ZT, Kalinowski J, Reynolds HR, Berger JS, Spruill TM. Psychosocial risk factors for depression in women with myocardial infarction: mindfulness and rumination. Circulation. 2020;142:A16569. [Google Scholar]
- 91. Park C, Duberstein Z, Rutigliano M, Kalinowski J, Blanc J, Shallcross AJ, Park K, Toma C, Suppogu N, Mehta LS, et al. Psychological and demographic correlates of objectively measured sleep duration and quality in women with myocardial infarction. Circulation. 2019;140:A12980. [Google Scholar]
- 92. Daviglus ML, Pirzada A, Durazo‐Arvizu R, Chen J, Allison M, Avilés‐Santa L, Cai J, González HM, Kaplan RC, Schneiderman N, et al. Prevalence of low cardiovascular risk profile among diverse Hispanic/Latino adults in the United States by age, sex, and level of acculturation: the Hispanic Community Health Study/Study of Latinos. J Am Heart Assoc. 2016;5:e003929. DOI: 10.1161/JAHA.116.003929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Daviglus M, Talavera GA, Avilés‐Santa ML, Allison MA, Cai J, Criqui M, Gellman M, Giachello AL, Gouskova N, Kaplan RC, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308:1775–1784.DOI: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Heiss G, Snyder ML, Teng Y, Schneiderman N, Llabre MM, Cowie C, Carnethon M, Kaplan R, Giachello A, Gallo L, et al. Prevalence of metabolic syndrome among Hispanics/Latinos of diverse background: the Hispanic Community Health Study/Study of Latinos. Diabetes Care. 2014;37:2391–2399.DOI: 10.2337/dc13-2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Merchant G, Buelna C, Castañeda SF, Arredondo EM, Marshall SJ, Strizich G, Sotres‐Alvarez D, Chambers EC, McMurray RG, Evenson KR, et al. Accelerometer‐measured sedentary time among Hispanic adults: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med Rep. 2015;2:845–853.DOI: 10.1016/j.pmedr.2015.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Qi Q, Strizich G, Merchant G, Sotres‐Alvarez D, Buelna C, Castañeda SF, Gallo LC, Cai J, Gellman MD, Isasi CR, et al. Objectively measured sedentary time and cardiometabolic biomarkers in US Hispanic/Latino adults: the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Circulation. 2015;132:1560–1569.DOI: 10.1161/CIRCULATIONAHA.115.016938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Thosar SS, Bielko SL, Mather KJ, Johnston JD, Wallace JP. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc. 2015;47:843–849.DOI: 10.1249/MSS.0000000000000479. [DOI] [PubMed] [Google Scholar]
- 98. Walsh LK, Restaino RM, Martinez‐Lemus LA, Padilla J. Prolonged leg bending impairs endothelial function in the popliteal artery. Physiol Rep. 2017;5:e13478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Chang YJ, Bellettiere J, Godbole S, Keshavarz S, Maestas JP, Unkart JT, Ervin D, Allison MA, Rock CL, Patterson RE, et al. Total sitting time and sitting pattern in postmenopausal women differ by hispanic ethnicity and are associated with cardiometabolic risk biomarkers. J Am Heart Assoc. 2020;9:e013403. DOI: 10.1161/JAHA.119.013403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio‐metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Kerr J, Crist K, Vital DG, Dillon L, Aden SA, Trivedi M, Castellanos LR, Godbole S, Li H, Allison MA, et al. Acute glucoregulatory and vascular outcomes of three strategies for interrupting prolonged sitting time in postmenopausal women: a pilot, laboratory‐based, randomized, controlled, 4‐condition, 4‐period crossover trial. PLoS One. 2017;12:e0188544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Patterson RE, Sears DD. Metabolic effects of intermittent fasting. Annu Rev Nutr. 2017;37:371–393. [DOI] [PubMed] [Google Scholar]
- 103. St‐Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris‐Etherton P, Varady K; American Heart Association Obesity Committee of the Council on L, Cardiometabolic H, Council on Cardiovascular Disease in the Y, Council on Clinical C and Stroke C . Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Marinac CR, Sears DD, Natarajan L, Gallo LC, Breen CI, Patterson RE. Frequency and circadian timing of eating may influence biomarkers of inflammation and insulin resistance associated with breast cancer risk. PLoS One. 2015;10:e0136240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Marinac CR, Natarajan L, Sears DD, Gallo LC, Hartman SJ, Arredondo E, Patterson RE. Prolonged nightly fasting and breast cancer risk: findings from NHANES (2009–2010). Cancer Epidemiol Biomarkers Prev. 2015;24:783–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Marinac CR, Nelson SH, Breen CI, Hartman SJ, Natarajan L, Pierce JP, Flatt SW, Sears DD, Patterson RE. Prolonged nightly fasting and breast cancer prognosis. JAMA Oncol. 2016;2:1049–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Ha K, Song Y. Associations of meal timing and frequency with obesity and metabolic syndrome among Korean adults. Nutrients. 2019;11:2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Makarem N, Sears DD, St‐Onge MP, Zuraikat FM, Gallo LC, Talavera GA, Castaneda SF, Lai Y, Mi J, Aggarwal B. Habitual nightly fasting duration, eating timing, and eating frequency are associated with cardiometabolic risk in women. Nutrients. 2020;12:3043. DOI: 10.3390/nu12103043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Makarem N, Aggarwal B, Sears DD, St‐Onge M‐P, Castaneda SF, Talavera GA, Marinac CR, Patterson R, Sotres‐Alvarez D, Garcia M, et al. Circadian timing of food intake is associated wth cardiometabolic risk in US Hispanic/Latinos: results from the Hispanic Community Health Study/Study of Latinos. Circulation. 2018;138:A11503. [Google Scholar]
- 110. Makarem N, Sears DD, St‐Onge M‐P, Zuraikat F, Talavera GA, Castaneda SF, Xi H, Aggarwal B. Social jet lag in eating patterns as a marker of meal timing variability is associated with elevated cardiometabolic risk in the AHA Go Red for Women Strategically Focused Research Network. Circulation. 2020;142:A13175. [Google Scholar]
- 111. Sharma K, Kass DA. Heart failure with preserved ejection fraction: mechanisms, clinical features, and therapies. Circ Res. 2014;115:79–96.DOI: 10.1161/CIRCRESAHA.115.302922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–e483. [DOI] [PubMed] [Google Scholar]
- 113. Egan BM, Stevens‐Fabry S. Prehypertension—prevalence, health risks, and management strategies. Nat Rev Cardiol. 2015;12:289–300.DOI: 10.1038/nrcardio.2015.17. [DOI] [PubMed] [Google Scholar]
- 114. Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, Stein K, Dickens C. Effectiveness of mindfulness‐based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta‐analysis of randomised controlled trials. J Psychosom Res. 2014;76:341–351.DOI: 10.1016/j.jpsychores.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 115. Scott‐Sheldon LAJ, Gathright EC, Donahue ML, Balletto B, Feulner MM, DeCosta J, Cruess DG, Wing RR, Carey MP, Salmoirago‐Blotcher E. Mindfulness‐based interventions for adults with cardiovascular disease: a systematic review and meta‐analysis. Ann Behav Med. 2020;54:67–73.DOI: 10.1093/abm/kaz020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Kalinowski J, Spruill TM, Allison M, Bearse A, Rutigliano M, Payano L, Diaz L, Gallo LC, Talavera GA, Castaneda SF. Partnership to adapt a telephone‐based mindfulness program for diverse primary care Latina patients. Ann Behav Med. 2020;54:S228. [Google Scholar]
- 117. U.S. Department of Health and Human Services . Physical Activity Guidelines for Americans. 2nd ed. Washington, DC: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 118. Rosenberger ME, Fulton JE, Buman MP, Troiano RP, Grandner MA, Buchner DM, Haskell WL. The 24‐hour activity cycle: a new paradigm for physical activity. Med Sci Sports Exerc. 2019;51:454–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Chu AHY, Bernard JY, Koh D, Muller‐Riemenschneider F. Accelerometer profile of physical activity and sedentary behavior in a multi‐ethnic urban Asian population. Res Q Exerc Sport. 2020;1–8. [DOI] [PubMed] [Google Scholar]
- 120. Noh S, Kim AH, Noh MS. Korean Immigrants in Canada: Perspectives on Migration, Integration, and the Family. Toronto, Ontario: University of Toronto Press; 2012. [Google Scholar]
- 121. Park C, Nam S, Redeker NS, Shebl FM, Dixon J, Jung TH, Whittemore R. The effects of acculturation and environment on lifestyle behaviors in Korean immigrants: the mediating role of acculturative stress and body image discrepancy. Ethn Health. 2019;1–17. [DOI] [PubMed] [Google Scholar]
- 122. Park C, Spruill TM, Butler MJ, Kwon SC, Redeker NS, Gharzeddine R, Whittemore R. Gender differences in acculturative stress and habitual sleep duration in Korean American immigrants. J Immigr Minor Health. 2020;22:736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Park C, Larsen B, Kwon S, Xia Y, Dickson V, Spruill T. Acculturation and 24‐hour behaviors in Asian American women. Med Sci Sports Exerc. 2020;52:1018. [Google Scholar]
- 124. Park C, Larsen B, Xia Y, Kwon S, Dickson V, Reynolds HR, Spruill TM. Effects of reallocating time in different physical activity intensities and sleep on cardiovascular disease risk factors in Asian American women: a cross sectional modeling study. Circulation. 2020;142:A14772. [Google Scholar]
- 125. Park C, Larsen BA, Xia Y, Reynolds HR, Spruill TM. Variation in 24‐hour physical activity patterns by demographic and psychological factors in women with myocardial infarction. Circ Cardiovasc Qual Outcomes. 2020;13:A289. [Google Scholar]


