Abstract
Background
The association between psychosocial stress and coronary heart disease (CHD) may be stronger in women than men and may differ across types of stressors. In this study, we assessed associations of psychosocial stressors, including job strain, stressful life events, and social strain with the incidence of CHD in women.
Methods and Results
We used longitudinal data from 80 825 WHI‐OS (Women's Health Initiative Observational Study) participants with a mean age of 63.4 years (7.3 years) at baseline. Job strain was assessed through linkage of Standard Occupational Classification codes to the Occupational Information Network. Stressful life events and social strain were assessed via validated self‐reported questionnaires. Cox proportional hazard models were used to evaluate associations of each stressor with CHD separately and jointly. A total of 3841 (4.8%) women developed CHD during an average of 14.7 years of follow‐up. After adjustment for age, other stressors, job tenure, and socioeconomic factors, high stressful life events score was associated with a 12% increased CHD risk, and high social strain was associated with a 9% increased CHD risk. Job strain was not independently associated with CHD risk, but we observed a statistically significant interaction between job strain and social strain (P=0.04), such that among women with high social strain, passive job strain was associated with a 21% increased CHD risk.
Conclusions
High stressful life events and social strain were each associated with higher CHD risk. Job strain and social strain work synergistically to increase CHD risk.
Keywords: coronary heart disease, job strain, social strain, stressful life events, women
Subject Categories: Aging, Cardiovascular Disease, Risk Factors, Women
Nonstandard Abbreviations and Acronyms
- BHAT
Beta‐Blocker Heart Attack Trial
- O*NET
Occupational Information Network
- WHI
Women's Health Initiative
- WHI‐OS
Women's Health Initiative Observational Study
Clinical Perspective
What Is New?
Job strain and social strain work synergistically to increase coronary heart disease risk.
What Are the Clinical Implications?
Prevention strategies including monitoring stress at work, decreasing workload, and promoting social networks are needed and should receive more attention in the future.
Psychosocial stress typically occurs when people have difficulty in coping with challenging environmental conditions and can lead to dysregulation of homeostasis that may result in illness. 1 Since the perception of psychosocial stress is subjective, studies of psychological stress usually focus on the occurrence of environmental events (stressors) that exceed one's coping ability. 2
Recently, several large research studies identified that psychosocial stress from different domains of life (eg, finance, work, and relationships) may play a role in the development of coronary heart disease (CHD). 3 , 4 , 5 Psychosocial stress can directly increase cardiovascular reactivity (eg, heart rate), inflammation, and produce metabolic changes, which, in turn, lead to incident CHD. 6 Additionally, psychosocial stress has well‐documented adverse effects on a range of poor health behaviors (eg, smoking, physical inactivity, and consumption of alcohol) and clinical CHD risk factors, including hypertension and diabetes mellitus, 6 , 7 that are primary contributors to the development of CHD.
Sex differences in stress levels have been documented. 8 , 9 , 10 , 11 According to a survey by the American Psychological Association, women are more likely than men to report high average stress levels and stress‐related physical and emotional symptoms (eg, fatigue and depression). 9 This finding suggests that the strength of the association between psychosocial stress and CHD may be higher in women than men. Women may be exposed to psychosocial stressors that are less common among men. 10 Low et al 11 reviewed studies on psychosocial risk and CHD in women and found that stress from relationships and family responsibilities may be more important than job stress for women's cardiovascular health. Thus, identifying which stressors are most relevant to CHD in women can provide insight into understanding sex differences in the relationship between psychosocial stress and CHD.
Most studies of psychosocial stress and CHD concentrate on the relationship between one individual source of stress, such as caregiving. 12 However, different domains of stress may act synergistically to increase the risk of CHD. 13 For example, death of a loved one can disrupt an individual's life and induce stress in other domains, like work‐related stress, enhancing CHD risk. 12 Similarly, daily life stressors and family problems may act synergistically with job stress, accelerating the development of CHD in women since they usually take more domestic and caregiving responsibilities. 13 , 14 Prior studies, which evaluated single domains of stress without considering the influence from others, may therefore have underestimated the association between stress and CHD risk.
To better characterize the associations between different domains of psychosocial stress and CHD in women, we utilized data from WHI‐OS (Women's Health Initiative Observational Study), a nationally representative cohort study of postmenopausal women in the United States. We aimed to determine the independent and synergistic effect of different stress domains, including work, stressful life events, and social relationships, on women's CHD risk.
Methods
Because of the sensitive nature of the data collected for this study, requests to access the data set from qualified researchers trained in human subject confidentiality protocols may be sent to the WHI (Women's Health Initiative) at helpdesk@whi.org.
Study Population
WHI‐OS included 93 676 postmenopausal women aged 50 to 79 years at baseline. Participants were enrolled from 1993 to 1998 at 40 geographically diverse clinical centers throughout the United States and followed until 2005. 15 Written informed consent was obtained from all women before enrollment. Women who consented to participate in the WHI Extension Study were followed for an additional 10 years from 2005 to 2015. 15 The average follow‐up for the current analysis was 14.7 years. A total of 91 627 women (97.8% of the WHI‐OS sample) responded to the occupational history questionnaire at baseline. Among those women, 80 825 women provided job title and tenure information on their most recent job, responded to life events and social strain questions, did not report a history of nonfatal myocardial infarction at baseline, and were not lost to follow‐up (Figure). A total of 8812 participants were missing information on covariates (income, smoking, drinking status, hypertension, diabetes mellitus, and high cholesterol, and depression symptoms) but were not excluded from the analysis since they account for nearly 10% of the eligible participants (see information on multiple imputation below).
Figure 1. Flowchart showing the study design: analytical population.
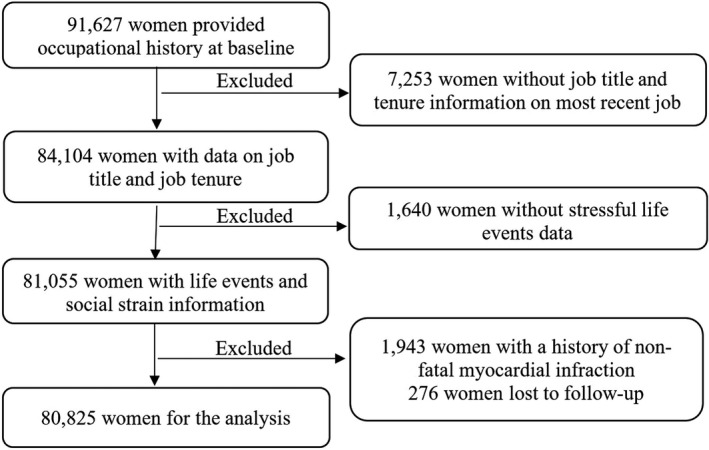
The left columns represent participants included in the analysis and the right columns indicate participants removed from the analysis.
This analysis was reviewed and approved by Drexel University's institutional review board.
Job Strain
Karasek Job Demand–Control Model is a well‐established theoretical framework 16 that has been applied to the relationship between job strain and health outcomes, including cardiovascular problems. 17 In the model, job control describes whether workers can exert their influence over tasks, while job demand describes the workload and intensity. Occupations combining high demand with low control are recognized as the most stressful jobs. 18 In WHI‐OS, women reported up to 3 paid jobs (full or part‐time) held for the longest period since age 18. Using text response of job title and industry, trained coders at the National Institute for Occupational Safety and Health assigned 6‐digit 2010 Standard Occupational Classification codes to each job. We matched the occupational codes to the Occupational Information Network (O*NET) 21.0 database to evaluate the job demand and job control for each job. Prior studies have extracted indicators from O*NET to assess job strain 19 , 20 and found a high level of consistency between the constructed O*NET psychosocial scales and scales based on self‐reported questionnaires, especially for the Job Demand–Control Model. 19 , 20 Hence, we identified O*NET indicators that have been previously used to evaluate job strain. 19 , 20
Thirteen job indicators from O*NET were used to calculate scores of job demand and job control. Job demand was calculated from the mean of 5 items: selective attention, attention to details, importance of being exact, consequence of error, and time sharing (Cronbach α=0.66). Job control was calculated from the mean of 8 items: achievement, active learning and thinking creatively, independence, impact of decision on coworkers or company results, frequency of decision‐making, freedom to make decisions, and structured work or not (Cronbach α=0.85). All O*NET job indicators were standardized by creating a Z score with the mean equal to 0 and the SD equal to 1 based on the O*NET data set. Higher scores of demand and control variables represent greater job demand or job control.
We assessed job strain based on the participant's job closest in time to study enrollment. Overall job strain was operationalized as 4 categories constructed by dichotomizing job demand and job control scores at medians and cross‐tabulating: active work (high demand and high control), high strain (high demand and low control), low strain (low demand and high control), and passive work (low demand and low control). We dichotomized job demand and job control at the median values from the entire O*NET data set, ie, across all jobs in the US workforce. We also explored individual associations of job demand and job control with CHD as continuous variables since placing the women into job strain categories may lead to exposure misclassification. 21
Stressful Life Events
Information on stressful life events was collected at baseline via a self‐administered questionnaire originally developed in the Alameda County Epidemiologic Study 22 and modified in the BHAT (Beta‐Blocker Heart Attack Trial). 23 Further changes were introduced in the WHI study to ensure relevance to older women. 24 Participants were asked about their experience with 11 major life events occurring over the previous year: spouse died, spouse with serious illness, close friend died, major problems with money, divorced/separated, close friend divorced, major conflict with children or grandchildren, lost job, physically abused, verbally abused, and pet died. For each event, women were asked to indicate whether they experienced the event (yes or no) and the extent to which the event upset them (1=did not upset me, 2=upset me moderately, and 3=upset me very much). The final score on the stressful life events scale ranged from 0 to 33, with a higher score indicating a greater number of upsetting life events. For consistency with prior studies conducted with this cohort, 25 we created 4 categories of stressful life events based on the quartile distribution of the responses: low (0), medium‐low (1 or 2), medium‐high (3 or 4), and high (≥5). We also evaluated the association between CHD and stressful life events as a continuous variable to evaluate exposure misclassification.
Social Strain
Social strain, the negative aspect of social relations, was measured at baseline by questions derived from a valid scale of negative social relationships. 26 Participants were asked about the number of people who get on their nerves, who ask too much of them, who exclude them, and who try to coerce them in their current life. For each question, a scale ranging from 1 to 5 (none to all) was used to measure the frequency of negative social relations. The final summary score of social strain ranged from 4 to 20, where a higher score indicates greater social strain. Based on prior studies conducted with this cohort, 25 we categorized social strain based on the tertile distribution of responses as low (<4), medium (5 or 6), and high (≥7). We also evaluated the association between CHD and social strain as a continuous variable to evaluate exposure misclassification.
Covariates
Age, race/ethnicity (White, Black, Hispanic, American Indian/Alaska Native, Asian/Pacific Islander, or other), education (less than high school completed, high school diploma/general equivalency diploma, some college, or college or more completed), family income (<$35 000, $35 000–$49 999, $50 000–$74 999, and >$75 000), and job tenure were included as potential confounders of associations between stress and CHD. Baseline smoking status (none, former, and current smoker), alcohol use (number of alcohol servings per week), physical activity (metabolic equivalent hours per week), body mass index (kg/m2), depressive symptoms, hypertension, total cholesterol, and diabetes mellitus were considered as potential mediators of the associations between stress and CHD. Depressive symptoms were measured by the Burnham Instrument, which included 6 items from the Center of Epidemiology Studies Depression Scale and 2 items from the National Institute of Mental Health's Diagnostic Interview Schedule. 27 The score of depressive symptoms ranged from 0 to 0.99, with higher scores indicating greater depressive symptomatology. 27
Outcome Variable
CHD in this study was defined as the occurrence of first myocardial infarction (diagnosed based on cardiac pain, cardiac enzyme and troponin levels, and ECG findings) or death from CHD. 28 Women reported treatment or hospitalization for cardiovascular‐related situations or diseases annually. A local physician adjudicator verified all self‐reported events through a review of medical records and death certificates. Locally verified events were reviewed by central cardiovascular adjudicators. While 70% of self‐reported myocardial infarctions were verified by a local adjudicator, the agreement between central reviews with local adjudication was 87% for myocardial infarctions. 28 Follow‐up continued from the point at which women entered the study until death, diagnosis of CHD, or end of follow‐up.
Statistical Analysis
Characteristics of all covariates were summarized (means, SDs, and percentages) by CHD status. We performed multiple imputation with Markov chain Monte Carlo method to predict the values for missing data on the 10% of patients with missing information. We used all available covariates believed to be associated with the missingness mechanism and created 5 regression‐based imputations. 29 Cox proportional hazard models were used to estimate the hazard ratio (HR) and 95% CIs describing the relationships between covariates and incidence of CHD. Time in the proportional hazard models was the follow‐up years. We tested the proportional hazard assumption by evaluating the interaction between time and all variables. No violations of the assumption were identified. To evaluate the associations between each stress domain and CHD risk, we established 4 models: model 1 estimated age‐adjusted associations; model 2 controlled for age and other stress domains; model 3 additionally adjusted for race/ethnicity, education, family income, and job tenure; and model 4 adjusted for covariates in model 3 plus depression symptoms, alcohol use, cigarette smoking, leisure‐time physical activity, body mass index, hypertension, diabetes mellitus, and high cholesterol. For the main effects, P<0.05 was considered statistically significant.
Multiplicative interactions among stress domains were tested by creating 2‐way interaction terms for each combination of stress domains. We added each interaction term separately into a Cox proportional model that included the main effects. Only interaction terms with P<0.1 were considered statistically significant and retained. We examined the impact of the multiplicative interaction between stress domains in 3 models: model 1 included the main effects of 3 stress domains, the possible interaction terms between stress domains, and age. Model 2 included variables in model 1 plus potential confounders: race/ethnicity, education, family income, and job tenure; and model 3 additionally adjusted for potential mediators: depressive symptoms, alcohol use, cigarette smoking, leisure‐time physical activity, body mass index, hypertension, diabetes mellitus, and high cholesterol.
Almost half of the women in this study were retired at baseline, and the association between job strain and CHD risk may be attenuated after retirement. 30 Hence, we conducted a sensitivity analysis to examine whether the association differed by women's work status (working versus retired). To evaluate bias associated with the imputation of missing data, we repeated the analysis among women with complete data only.
All analysis was performed using SAS version 9.4 (SAS Insitute Inc.).
Results
The mean age of the population was 63 years (SD=7.3) at baseline. In general, women who developed CHD during follow‐up had lower educational attainment and family income. They were also more likely to be current smokers and have hypertension, diabetes mellitus, and high cholesterol levels compared with women without CHD (Table 1).
Table 1.
Characteristics by CHD Status in WHI‐OS, 1993 to 2013
| Characteristics | CHD | Total | |
|---|---|---|---|
| Yes (n=3841) | No (n=76 984) | N=80 825 | |
| Mean (SD)/% | Mean (SD)/% | Mean (SD)/% | |
| Age, y | 67.9 (6.6) | 63.2 (7.3) | 63.4 (7.3) |
| Race/ethnicity | |||
| White* | 87 | 85.4 | 85.4 |
| Black | 7.8 | 6.9 | 7 |
| Hispanic/Latino | 1.5 | 3 | 2.9 |
| American Indian or Alaskan Native | 0.4 | 0.4 | 0.4 |
| Asian or Pacific Islander | 1.9 | 3 | 2.9 |
| Other | 0.9 | 1.1 | 1.1 |
| Missing | 0.5 | 0.2 | 0.3 |
| Education | |||
| High school diploma or less than high school | 24.1 | 19.3 | 19.5 |
| More than high school diploma | 75.2 | 80 | 79.8 |
| Missing | 0.7 | 0.7 | 0.7 |
| Income | |||
| <$35 000 | 48 | 34.1 | 34.8 |
| $35 000–$49 999 | 19.6 | 19.1 | 19.1 |
| $50 000–$74 999 | 15 | 19.7 | 19.5 |
| ≥$75 000 | 10.2 | 20.3 | 19.8 |
| Missing | 7.1 | 6.8 | 6.8 |
| Retirement status | 68.2 | 50.2 | 51 |
| Job demand | −0.1 (0.8) | −0.1 (0.8) | −0.1 (0.9) |
| Job control | 0.1 (0.9) | 0.2 (0.9) | 0.2 (0.9) |
| Job strain | |||
| Low strain | 22.3 | 24.2 | 24.0 |
| Active | 27.7 | 31.5 | 31.3 |
| Passive | 24.3 | 20.9 | 21.1 |
| High strain | 25.7 | 23.4 | 23.6 |
| Stressful life events | 3.3 (3.2) | 3.20 (3.1) | 3.2 (3.1) |
| Social strain | 6.4 (2.5) | 6.4 (2.5) | 6.4 (2.5) |
| Smoking | |||
| None | 45 | 50.5 | 50.2 |
| Former | 44.7 | 42.5 | 42.6 |
| Current | 8.8 | 5.9 | 6.1 |
| Missing | 1.5 | 1.1 | 1.1 |
| Alcohol consumption, servings per wk | 2.3 (5.0) | 2.6 (5.3) | 2.6 (5.3) |
| Depression symptoms | 0.04 (0.13) | 0.04 (0.13) | 0.04 (0.13) |
| BMI † | 28.1 (6.2) | 27.1 (5.8) | 27.1 (5.8) |
| LTPA ‡ | 11.9 (13.1) | 13.8 (14.4) | 13.8 (14.3) |
| Diabetes mellitus (treated) | 10.7 | 3.2 | 3.6 |
| Hypertension (treated) | 40.4 | 23.2 | 24 |
| High cholesterol | 20.1 | 13.5 | 13.8 |
BMI indicates body mass index; CHD, coronary heart disease; LTPA, leisure‐time physical activity; and WHI‐OS, Women's Health Initiative Observational Study.
Does not include Hispanic origin.
Weight (kg)/height (m)2.
Total energy expended from recreational physical activity (metabolic equivalent hours per week).
After adjustment for age and other stress domains, high job strain, high stressful life events scores, and high social strain were significantly associated with higher risk of CHD (Table 2, model 2). One‐SD increase in job control was associated with a 14% decrease in the risk of CHD (HR, 0.86; 95% CI, 0.81– 0.90) after adjustment for age, job demand, stressful life events, and social strain. Compared with low job strain, high job strain and passive work were associated with a 13% and 24% increased risk of CHD, respectively (HR, 1.13 [95% CI, 1.03–1.24] and HR, 1.24 [95% CI, 1.13–1.36]). Job demand was not associated with CHD risk. High stressful life event scores were associated with a 20% increased risk of CHD (HR, 1.20; 95% CI, 1.09–1.31), compared with low stressful life events scores. Compared with low social strain, high social strain was associated with a 12% increased risk of CHD (HR, 1.12; 95% CI, 1.04–1.22).
Table 2.
HRs for the Associations of Job Strain, Stressful Life Events, and Social Strain Categories With Incident CHD in WHI‐OS, 1993 to 2013 (N=80 825)
| Stress Domains | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Job strain | ||||
| Low strain | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Active | 0.96 (0.88–1.05) | 0.96 (0.88–1.06) | 0.96 (0.87–1.05) | 0.93 (0.88–1.02) |
| Passive | 1.25 (1.14–1.38) | 1.24 (1.13–1.36) | 1.01 (0.91–1.12) | 1.00 (0.90–1.11) |
| High strain | 1.13 (1.03–1.24) | 1.13 (1.03–1.24) | 1.00 (0.91–1.11) | 1.01 (0.91–1.11) |
| Stressful life event | ||||
| Low | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Medium‐low | 0.99 (0.91–1.09) | 0.98 (0.90–1.08) | 0.97 (0.89–1.07) | 0.95 (0.87–1.04) |
| Medium‐high | 1.13 (1.03–1.24) | 1.10 (1.00–1.21) | 1.10 (0.98–1.18) | 1.04 (0.94–1.14) |
| High | 1.25 (1.14–1.37) | 1.20 (1.09–1.31) | 1.12 (1.02–1.23) | 1.02 (0.93–1.12) |
| Social strain | ||||
| Low | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| Medium | 1.04 (0.96–1.12) | 1.02 (0.94–1.11) | 1.03 (0.95–1.11) | 0.99 (0.91–1.07) |
| High | 1.18 (1.09–1.27) | 1.12 (1.04–1.22) | 1.09 (1.01–1.18) | 1.00 (0.92–1.08) |
| Job demand* | 0.92 (0.86–0.97) | 0.97 (0.92–1.04) | 0.98 (0.92–1.04) | 0.96 (0.91–1.02) |
| Job control* | 0.84 (0.80–0.89) | 0.86 (0.81–0.90) | 0.98 (0.92–1.05) | 0.97 (0.92–1.03) |
| Stressful life events* | 1.04 (1.03–1.05) | 1.03 (1.02–1.04) | 1.02 (1.01–1.03) | 1.01 (0.99–1.02) |
| Social strain* | 1.05 (1.03–1.06) | 1.03 (1.02–1.05) | 1.03 (1.01–1.04) | 1.01 (0.99–1.03) |
Mode 1: age. Model 2: age and other domains of stress. Model 3: age, race/ethnicity, income, education, job tenure, and other domains of stress. Model 4: age, race/ethnicity, income, education, job tenure, depression symptoms, smoking, alcohol, leisure‐time physical activity, body mass index, hypertension, cholesterol, diabetes mellitus, and other domains of stress. CHD indicates coronary heart disease; HR, hazard ratio; and WHI‐OS, Women's Health Initiative Observational Study.
Model adjusted for continuous stressor instead of categorical stressor.
All associations were attenuated after adjustment for race/ethnicity, education, family income, and job tenure (model 3). Job control and job strain were no longer significantly related to CHD risk (job control HR, 0.98 [95% CI, 0.92–1.05]; high job strain HR, 1.00 [95% CI, 0.91–1.11]). However, the associations between high stressful life event scores and high social strain with greater CHD risk remained statistically significant (high stressful life event HR, 1.12 [95% CI, 1.02–1.23]; high social strain HR, 1.09 [95% CI, 1.01–1.18]). As expected, additionally adjusting for potential mediators further attenuated the associations (model 4). Findings for models with continuous measures of stressful life event and social strain were similar to the findings from the categorical measures (Table 2).
We did not find a significant interaction between job strain and stressful life events (P=0.20) or stressful life events and social strain (P=0.66). However, we observed a significant interaction between job strain and social strain with CHD risk (P=0.04) such that the estimated impact of job strain on CHD risk was increased for women also reporting high social strain (Table 3). In the absence of social strain, job strain was not associated with CHD risk in women. Among women with high social strain, CHD risk was 25% higher for women with high job strain and 50% higher for passive jobs compared with women with low job strain after adjustment for age and stressful life event scores (HR, 1.25 [95% CI, 1.07–1.46]; HR, 1.50 [95% CI, 1.30–1.74], respectively). Controlling for race/ethnicity, family income, job tenure, and stressful life events score attenuated the associations, but passive jobs remained significantly associated with a 21% higher risk of CHD for women with high social strain (HR, 1.21; 95% CI, 1.03–1.41). In order to better understand the unexpected association with job strain, we evaluated the characteristics of participants by levels of job strain. Women who worked in passive jobs had lower education and income compared with women in active or high‐strain jobs (Table S1). Additionally, women with passive jobs were more likely to have diabetes mellitus, hypertension, and high cholesterol (Table S1).
Table 3.
HRs for Associations of Job Strain With Incident CHD by Social Strain in WHI‐OS, 1993 to 2013 (N=80 825)
| Social Strain | Job Strain | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Low | Low | Reference | Reference | Reference |
| Active | 0.92 (0.79–1.08) | 0.91 (0.78–1.06) | 0.88 (0.75–1.03) | |
| Passive | 1.03 (0.87–1.21) | 0.85 (0.71–1.00) | 0.86 (0.72–1.02) | |
| High | 0.96 (0.82–1.13) | 0.85 (0.72–1.01) | 0.86 (0.73–1.01) | |
| Medium | Low | Reference | Reference | Reference |
| Active | 0.95 (0.81–1.12) | 0.93 (0.80–1.10) | 0.90 (0.77–1.06) | |
| Passive | 1.16 (0.97–1.14) | 0.96 (0.81–1.15) | 0.92 (0.77–1.10) | |
| High | 1.19 (1.01–1.40) | 1.05 (0.89–1.23) | 1.02 (0.87–1.21) | |
| High | Low | Reference | Reference | Reference |
| Active | 1.02 (0.88–1.19) | 1.02 (0.87–1.19) | 1.00 (0.86–1.16) | |
| Passive | 1.50 (1.30–1.74) | 1.21 (1.03–1.41) | 1.20 (1.03–1.40) | |
| High | 1.25 (1.07–1.46) | 1.13 (0.97–1.32) | 1.14 (0.97–1.33) |
Model 1: age and life stress. Model 2: age, race/ethnicity, income, education, job tenure, and other domains of stress. Model 3: age, race/ethnicity, income, education, job tenure, depression symptoms, smoking, alcohol, leisure‐time physical activity, body mass index, hypertension, cholesterol, diabetes mellitus, and other domains of stress. CHD indicates coronary heart disease; HR, hazard ratio; and WHI‐OS, Women's Health Initiative Observational Study.
Compared with participants with missing data, those with complete data were more likely to be White and in the higher education categories (Table S2). We observed no significant changes in associations when we restricted the analysis to women with complete information (Table S3). After stratifying on working status, the patterns of associations for job strain, stressful life event scores, and social strain of CHD were similar in the sample of women who were currently working and the full sample (Table S4). However, the magnitude of the association was stronger for women who were currently working.
Discussion
In this large sample of postmenopausal women, we found that stressful life events and social strain were each associated with increased risk of CHD. The association between job strain and CHD risk was fully attenuated after adjustment for socioeconomic status. Job strain interacted with social strain in relation to CHD risk. The estimated impact of job strain on CHD risk was increased for women also reporting high social strain.
Prior prospective studies of the association between job strain and CHD risk among women yielded mixed results. 31 , 32 , 33 , 34 Job strain (high demand and low control) was not associated with the risk of CHD during 4 years of follow‐up among 35 038 US female nurses aged 46 to 71 years in the Nurses' Health Study (relative risk, 0.71; 95% CI, 0.42–1.19). 31 Similarly, compared with high job strain (high demand and low control), low job strain (low demand and high control) was not significantly associated with decreased risk of CHD after controlling for age and traditional CHD risk factors (relative risk, 1.63; 95% CI, 0.57–4.67) in the Framingham Offspring Study (n=1328; age range, 18–77 years) over a 10‐year follow‐up period. 32 Additionally, the Women's Lifestyle and Health Cohort Study (n=49 259 women; age range, 30–50 years) found no association between self‐reported high job strain (high demands and low control) and the incidence of CHD during 11 years of follow‐up (HR, 1.0; 95% CI, 0.5–1.9). 33 In contrast, a collaborative meta‐analysis of longitudinal studies evaluating job strain among 97 117 female employees in 8 European countries using the Job Content Questionnaire found that women with high job strain (high demand and low control) experienced 46% greater risk of CHD (HR, 1.46; 95% CI, 1.07–1.99) compared with women with lower job strain (including all other combinations of demands and control) after adjusting for age. 34
We observed no independent association between job strain and CHD risk after controlling for age, other domains of stress, job tenure, and socioeconomic indicators. Inconsistent findings for job strain in prior research may be partially explained by differences in measurement of job strain, population age, and consideration of confounders. Some studies combined low, passive, and active job strain into 1 group, which may ignore the potential impact of the passive or active work on CHD risk. Advanced age may attenuate the association between job strain and cardiovascular disease, as retirement is more common in older age groups. 30 Moreover, most studies considered adjustment for traditional CHD factors while few studies adjusted for the impact of emotional disorders such as depression, which is related to both psychosocial stress and CHD. 35
Results from our study suggest a strong interaction between job strain and social strain. Stressful life events and social isolation have been consistently and positively related to CHD in prior research. 10 , 14 , 25 , 36 A previous study utilizing WHI data found that stressful life events and social strain were associated with a higher incidence of CHD. 25 However, this study did not consider the interdependent effects of multiple stress domains, including job strain, or evaluate the interaction between stress domains. Few studies have examined the interactions among different stress domains and the impact on CHD among women. 14 , 37 In the Stockholm Female Coronary Risk Study of 287 (131 cases and 156 controls) women aged 30 to 65 years, exposure to stress from work and family was associated with the highest risk and the worst CHD prognosis. 14 This is consistent with our finding that the association between job strain and CHD risk was higher among women also reporting high social strain. In our study, passive work was associated with the highest risk of CHD among women with high social strain. Similar to prior research, 38 women in our study population who worked in passive jobs were more likely to be in lower socioeconomic status categories (eg, less than high school education and lowest income group) and have higher prevalence of diabetes mellitus, hypertension, and high cholesterol. Low socioeconomic status is correlated with increased risk of cardiovascular disease. 6 , 7 The residual confounding by socioeconomic status in combination with a large burden of CHD risk factors may partially explain the increased CHD risk for passive work in our population.
The prolonged effects of stress are directly related to endothelial damage. 7 When women are exposed to stressful situations over time, a series of cardiovascular reactions are elicited (eg, increased blood pressure, autonomic activity, and inflammation), which, in turn, may lead to endothelial damage and accelerate the atherosclerotic process. 7 Additionally, stress may decrease a person's cognitive abilities, leading to difficulties in learning new things and being active in social relationships. 39 Alternatively, people with harmonious social relationships may be more confident in their ability to control their environment, which may help them reduce the perception of threats and act as an important resource in handling adverse situations, eg, at work, and therefore relieve the potential negative health impact of stress. 39
This study has several strengths. First, the use of 3 previously validated stress measures allowed us to examine the unique impact of different stress domains and their potential interaction on the development of CHD in women. Second, we included job tenure in the models of job strain and CHD since recent evidence suggests that cumulative job strain may be a stronger predictor of CHD. 12 This study measured job strain by linking women's reports of occupation to standard occupational information data sets, which reduces the bias of self‐reported occupational exposure based on present health status and participants' attitude. The use of a standard occupational informational data set may, however, underestimate variability in exposure within the same occupation.
Our study also has several limitations. First, our results may reflect the “healthy worker” bias. 40 People who are able to meet the high demands of working for a long period may have better physical health. However, after stratifying on working status, we observed similar associations for people who were still working at baseline to the overall cohort, suggesting that the healthy worker bias was relatively modest. Although we were able to adjust for many confounders in multivariable models, residual confounding may still exist. Working hours (eg, shift work) and social support are associated with CHD 41 , 42 and were not considered in this study, which, in turn, may bias our effect estimates. In this study, we focused on the impact of stress from the most recent/current job. People may take different jobs during their life. Ignoring the change of job strain over the life course will likely lead to an underestimation of the associations. Based on the traditional job strain definition, we used median cut points for job demand and control, which may misclassify workers regarding their exposure to job strain and result in biased estimated associations. 21 However, we observed similar patterns of associations with CHD for continuous stressors, including continuous job control and job demand, suggesting that the effect of misclassification in our measure of job strain was small. Notably, the Cronbach α for job demand in our study was not high. Job demand consists of both quantitative demands (work overload) and qualitative demands (intellectual and emotional demand). 43 For women, qualitative demand is more important than quantitative demands. 43 However, our objective measurement of job demand based on previous studies may not adequately capture the qualitative demands and thus only partially measured job demand for women. Sex‐specific measurement of job demand is needed in the future.
Conclusions
Stressful life events and social strain were each associated with increased risk of CHD among women. For job strain, the increased CHD risk was confounded by socioeconomic factors. Exposure to job strain and social strain interacted synergistically, resulting in a higher risk of CHD than expected from exposure to either stressor alone. Our findings support the public health concern about the harmful impact of stress on well‐being and, in particular, on cardiovascular risk. Addressing stress may have an important role in the prevention of CHD in women, especially for women who experience stress at work in addition to social stress. Although a variety of interventions directed at stressors such as special education programs and cognitive‐behavioral therapy have been developed, these interventions have primarily focused on secondary prevention. 44 Primary prevention strategies including monitoring stress at work, decreasing workload, and promoting social networks are needed and should receive more attention in the future. Because sex and socioeconomic status may influence people's ability to manage stress, research is necessary to identify subgroups of people who may be more likely to benefit from the implementation of preventive interventions.
Sources of Funding
The WHI program is funded by the National Heart, Lung, and Blood Institute; National Institutes of Health; and the US Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C.
Disclosures
None.
Supporting information
Tables S1–S4
(J Am Heart Assoc. 2021;10:e017780. DOI: 10.1161/JAHA.120.017780.)
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.017780
For Sources of Funding and Disclosures, see page 9.
See Editorial by Tracy and Volgman
References
- 1. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY: Springer; 1984. [Google Scholar]
- 2. Cohen S, Denise JD, Gregory EM. Psychological stress and disease. JAMA. 2007;298:1685–1687. DOI: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 3. Lagraauw HM, Kuiper J, Bot I. Acute and chronic psychological stress as risk factors for cardiovascular disease: insights gained from epidemiological, clinical and experimental studies. Brain Behav Immun. 2015;50:18–30. DOI: 10.1016/j.bbi.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 4. Kivimäki M, Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol. 2018;15:215. DOI: 10.1038/nrcardio.2017.189. [DOI] [PubMed] [Google Scholar]
- 5. Rosengren A, Hawken S, Ôunpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthi‐amorn C, Sato H, Yusuf S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:953–962. [DOI] [PubMed] [Google Scholar]
- 6. Hjemdahl P, Rosengren A, Steptoe A, eds. Stress and cardiovascular disease. London, England: Springer Science & Business Media; 2012. [Google Scholar]
- 7. Merz CN, Dwyer J, Nordstrom CK, Walton KG, Salerno JW, Schneider RH. Psychosocial stress and cardiovascular disease: pathophysiological links. Behav Med. 2002;27:141–147. DOI: 10.1080/08964280209596039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. O’Neil A, Scovelle AJ, Milner AJ, Kavanagh A. Gender/sex as a social determinant of cardiovascular risk. Circulation. 2018;37:854–864. DOI: 10.1161/CIRCULATIONAHA.117.028595. [DOI] [PubMed] [Google Scholar]
- 9. American Psychological Association . Stress in America: the impact of discrimination. Stress in America™ Survey. 2016.
- 10. Terrill AL, Garofalo JP, Soliday E, Craft R. Multiple roles and stress burden in women: a conceptual model of heart disease risk. J Appl Biobehav Res. 2012;17:4–22. DOI: 10.1111/j.1751-9861.2011.00071.x. [DOI] [Google Scholar]
- 11. Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: current research and future directions. Psychosom Med. 2010;72:842. DOI: 10.1097/PSY.0b013e3181f6934f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Albert MA, Durazo EM, Slopen N, Zaslavsky AM, Buring JE, Silva T, Chasman D, Williams DR. Cumulative psychological stress and cardiovascular disease risk in middle aged and older women: rationale, design, and baseline characteristics. Am Heart J. 2017;192:1–12. DOI: 10.1016/j.ahj.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leineweber C, Baltzer M, Hanson LL, Westerlund H. Work–family conflict and health in Swedish working women and men: a 2‐year prospective analysis (the SLOSH study). Eur J Public Health. 2013;23:710–716. DOI: 10.1093/eurpub/cks064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang HX, Leineweber C, Kirkeeide R, Svane B, Schenck‐Gustafsson K, Theorell T, Orth‐Gomér K. Psychosocial stress and atherosclerosis: family and work stress accelerate progression of coronary disease in women. The Stockholm Female Coronary Angiography Study. J Intern Med. 2007;261:245–254. DOI: 10.1111/j.1365-2796.2006.01759.x. [DOI] [PubMed] [Google Scholar]
- 15. Hays J, Hunt JR, Hubbell FA, Anderson GL, Limacher M, Allen C, Rossouw JE. The Women's Health Initiative recruitment methods and results. Ann Epidemiol. 2003;13:S18–S77. DOI: 10.1016/S1047-2797(03)00042-5. [DOI] [PubMed] [Google Scholar]
- 16. Karasek RA Jr. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q. 1979;285–308. DOI: 10.2307/2392498. [DOI] [Google Scholar]
- 17. Bosma H, Peter R, Siegrist J, Marmot M. Two alternative job stress models and the risk of coronary heart disease. Am J Public Health. 1998;88:68–74. DOI: 10.2105/AJPH.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cifuentes M, Boyer J, Lombardi DA, Punnett L. Use of O* NET as a job exposure matrix: a literature review. Am J Ind Med. 2010;53:898–914. DOI: 10.1002/ajim.20846. [DOI] [PubMed] [Google Scholar]
- 19. Cifuentes M, Boyer J, Gore R, d'Errico A, Tessler J, Scollin P, Lerner D, Kriebel D, Punnett L, Slatin C. Inter‐method agreement between O* NET and survey measures of psychosocial exposure among healthcare industry employees. Am J Ind Med. 2007;50:545–553. DOI: 10.1002/ajim.20480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Meyer JD, Cifuentes M, Warren N. Association of self‐rated physical health and incident hypertension with O* NET factors: validation using a representative national survey. J Occup Environ Med. 2011;53:139–145. DOI: 10.1097/JOM.0b013e318203f220. [DOI] [PubMed] [Google Scholar]
- 21. Burr H, Formazin M, Pohrt A. Methodological and conceptual issues regarding occupational psychosocial coronary heart disease epidemiology. Scand J Work Environ Health. 2016;42:251–255. [DOI] [PubMed] [Google Scholar]
- 22. Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine‐year follow‐up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. [DOI] [PubMed] [Google Scholar]
- 23. Ruberman W, Weinblatt E, Goldberg JD, Chaudhary BS. Psychosocial influences on mortality after myocardial infarction. N Engl J Med. 1984;311:552–559. [DOI] [PubMed] [Google Scholar]
- 24. Matthews KA, Shumaker SA, Bowen DJ, Langer RD, Hunt JR, Kaplan RM, Klesges RC, Ritenbaugh C. Women's Health Initiative. Why now? What is it? What's new? Am Psychol. 1997;52:101–116. [DOI] [PubMed] [Google Scholar]
- 25. Kershaw KN, Brenes GA, Charles LE, Coday M, Daviglus ML, Denburg NL, Kroenke CH, Safford MM, Savla T, Tindle HA, et al. Associations of stressful life events and social strain with incident cardiovascular disease in the Women's Health Initiative. J Am Heart Assoc. 2014;3:e000687. DOI: 10.1161/JAHA.113.000687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aneshensel CS. Social stress: theory and research. Ann Rev Sociol. 1992;18:15–38. [Google Scholar]
- 27. Burnam MA, Wells KB, Leake B, Landsverk J. Development of a brief screening instrument for detecting depressive disorders. Med Care. 1988;26:775–789. [DOI] [PubMed] [Google Scholar]
- 28. Curb JD, Mctiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx‐Burns L, Pastore L, Criqui M, et al. Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol. 2003;13:S122–S128. [DOI] [PubMed] [Google Scholar]
- 29. Schafer JL. Analysis of Incomplete Multivariate Data. New York, NY: Chapman and Hall/CRC; 1997. [Google Scholar]
- 30. Kivimäki M, Theorell T, Westerlund H, Vahtera J, Alfredsson L. Job strain and ischaemic disease: does the inclusion of older employees in the cohort dilute the association? The WOLF Stockholm Study. J Epidemiol Community Health. 2008;62:372–374. [DOI] [PubMed] [Google Scholar]
- 31. Lee S, Colditz G, Berkman L, Kawachi I. A prospective study of job strain and coronary heart disease in US women. Int J Epidemiol. 2002;31:1147–1153. DOI: 10.1093/ije/31.6.1147. [DOI] [PubMed] [Google Scholar]
- 32. Eaker ED, Sullivan LM, Kelly‐Hayes M, D’Agostino RB Sr, Benjamin EJ. Does job strain increase the risk for coronary heart disease or death in men and women? The Framingham Offspring Study. Am J Epidemiol. 2004;159:950–958. DOI: 10.1093/aje/kwh127. [DOI] [PubMed] [Google Scholar]
- 33. Kuper H, Adami HO, Theorell T, Weiderpass E. Psychosocial determinants of coronary heart disease in middle‐aged women: a prospective study in Sweden. Am J Epidemiol. 2006;164:349–357. DOI: 10.1093/aje/kwj212. [DOI] [PubMed] [Google Scholar]
- 34. Kivimäki M, Nyberg ST, Batty GD, Fransson EI, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta‐analysis of individual participant data. Lancet. 2012;380:1491–1497. DOI: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Antonogeorgos G, Panagiotakos DB, Pitsavos C, Papageorgiou C, Chrysohoou C, Papadimitriou GN, Stefanadis C. Understanding the role of depression and anxiety on cardiovascular disease risk, using structural equation modeling; the mediating effect of the Mediterranean diet and physical activity: the ATTICA study. Ann Epidemiol. 2012;22:630–637. DOI: 10.1016/j.annepidem.2012.06.103. [DOI] [PubMed] [Google Scholar]
- 36. Orth‐Gomér K, Schneiderman N, Vaccarino V, Deter HC, eds. Psychosocial Stress and Cardiovascular Disease in Women. Switzerland: Springer International Publishing; 2015. [Google Scholar]
- 37. Orth‐Gomér K, Leineweber C. Multiple stressors and coronary disease in women: the Stockholm Female Coronary Risk Study. Biol Psychol. 2005;69:57–66. DOI: 10.1016/j.biopsycho.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 38. von Bonsdorff MB, Seitsamo J, von Bonsdorff ME, Ilmarinen J, Nygård CH, Rantanen T. Job strain among blue‐collar and white‐collar employees as a determinant of total mortality: a 28‐year population‐based follow‐up. BMJ Open. 2012;2:e000860. DOI: 10.1136/bmjopen-2012-000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vezina M, Derriennic F, Monfort C. The impact of job strain on social isolation: a longitudinal analysis of French workers. Soc Sci Med. 2004;59:29–38. DOI: 10.1016/j.socscimed.2003.09.033. [DOI] [PubMed] [Google Scholar]
- 40. Clays E, Casini A, Van Herck K, De Bacquer D, Kittel F, De Backer G, Holtermann A. Do psychosocial job resources buffer the relation between physical work demands and coronary heart disease? A prospective study among men. Int Arch Occup Environ Health. 2016;89:1299–1307. DOI: 10.1007/s00420-016-1165-z. [DOI] [PubMed] [Google Scholar]
- 41. Hammar N, Alfredsson L, Johnson JV. Job strain, social support at work, and incidence of myocardial infarction. Occup Environ Med. 1998;55:548–553. DOI: 10.1136/oem.55.8.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kivimäki M, Jokela M, Nyberg ST, Singh‐Manoux A, Fransson EI, Alfredsson L, Bjorner JB, Borritz M, Burr H, Casini A, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta‐analysis of published and unpublished data for 603 838 individuals. Lancet. 2015;386:1739–1746. [DOI] [PubMed] [Google Scholar]
- 43. Rivera‐Torres P, Araque‐Padilla RA, Montero‐Simó MJ. Job stress across gender: the importance of emotional and intellectual demands and social support in women. Int J Environ Res Public Health. 2013;10:375–389. DOI: 10.3390/ijerph10010375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Giga SI, Cooper CL, Faragher B. The development of a framework for a comprehensive approach to stress management interventions at work. Int J Stress Manag. 2003;10:280. DOI: 10.1037/1072-5245.10.4.280. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S4


