Abstract
Background
Socioeconomic status is associated with differences in risk factors of cardiovascular disease and increased risks of cardiovascular disease and mortality. However, it is unclear whether an association exists between cardiovascular disease and income, a common measure of socioeconomic status, among patients with hypertension.
Methods and Results
This population‐based longitudinal study comprised 479 359 patients aged ≥19 years diagnosed with essential hypertension. Participants were categorized by income and blood pressure levels. Primary end point was all‐cause and cardiovascular mortality and secondary end points were cardiovascular events, a composite of cardiovascular death, myocardial infarction, and stroke. Low income was significantly associated with high all‐cause (hazard ratio [HR], 1.26; 95% CI, 1.23–1.29, lowest versus highest income) and cardiovascular mortality (HR, 1.31; 95% CI, 1.25–1.38) as well as cardiovascular events (HR, 1.07; 95% CI, 1.05–1.10) in patients with hypertension after adjusting for age, sex, systolic blood pressure, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and the use of aspirin or statins. In each blood pressure category, low‐income levels were associated with high all‐cause and cardiovascular mortality and cardiovascular events. The excess risks of all‐cause and cardiovascular mortality and cardiovascular events associated with uncontrolled blood pressure were more prominent in the lowest income group.
Conclusions
Low income and uncontrolled blood pressure are associated with increased all‐cause and cardiovascular mortality and cardiovascular events in patients with hypertension. These findings suggest that income is an important aspect of social determinants of health that has an impact on cardiovascular outcomes in the care of hypertension.
Keywords: blood pressure, cardiovascular diseases, health status disparities, hypertension, income, mortality
Subject Categories: Cardiovascular Disease, Hypertension, Mortality/Survival
Nonstandard Abbreviations and Acronyms
- NHIS
National Health Insurance Service
Clinical Perspective
What Is New?
Among individuals with similar blood pressure levels, low‐income levels were associated with high all‐cause mortality, cardiovascular mortality, and cardiovascular event rates.
Low income and uncontrolled blood pressure were associated with increased all‐cause mortality, cardiovascular mortality, and cardiovascular events in patients with hypertension.
What Are the Clinical Implications?
To our knowledge, this is the first study to examine the combined effects of income and blood pressure on all‐cause and cardiovascular mortality and cardiovascular events in patients with hypertension.
Income is an important aspect of social determinants of health that has an impact on cardiovascular outcomes in the care of hypertension.
Socioeconomic status (SES) is an important determinant of the likelihood that individuals and populations are exposed to environmental and other health risk factors. SES is closely related to cardiovascular disease (CVD) risk factors, morbidity, and mortality. 1 , 2 , 3 , 4 , 5 Currently, the CVD incidence is the highest among individuals with the lowest SES. Low SES is linked to the least favorable health behavioral characteristics 6 , 7 , 8 , 9 and is also associated with the worst prognosis after cardiac episodes. 6 , 7 , 8 , 9 Despite sharp declines in CVD mortality during the past 30 years, these benefits have not occurred equally across all populations in society. The most striking improvements in cardiovascular health have benefited wealthy, highly educated individuals, whereas progress among individuals with low SES has lagged, and the gap between high‐SES and low‐SES populations is widening. 10
A recent meta‐analysis demonstrated an inverse association between income as a key indicator of SES and CVD and cardiovascular‐related deaths. 11 However, few studies have focused on the relationships among income, mortality, and cardiovascular outcomes in patients with hypertension. Assessing the data from a real‐world electronic nationwide longitudinal health database would not only help better characterize the links among income, mortality, and CVD but also help guide efforts to reduce CVD burden through health service development and primary or secondary prevention. This study was conducted to evaluate the effects of income and blood pressure (BP) levels and their combined effects on mortality and cardiovascular events in more than 10 years of follow‐up in 1 554 406 Korean patients with hypertension using a large nationwide representative data set.
Methods
Data Source
This study involved the analysis of data from the National Health Insurance Service (NHIS)–National Health examinee database, which includes the data of all individuals who underwent National Health Examinations sponsored by the NHIS in South Korea. NHIS is a single insurance provider in Korea and covers 97% of the Korean population, whereas the remaining 3% are covered by the medical aid program. The NHIS claims database includes data of demographic characteristics, diagnoses, prescriptions, health screening examinations (eg, health questionnaires and laboratory tests), and death. Details on the data source have been described previously. 12 All diagnoses are recorded in the NHIS database using International Classification of Diseases, Tenth Revision (ICD‐10) codes. The study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (KBSMC 2019‐12‐022). The NHIS provided the anonymized data set to the researchers, and the requirement for informed consent was waived.
Study Population
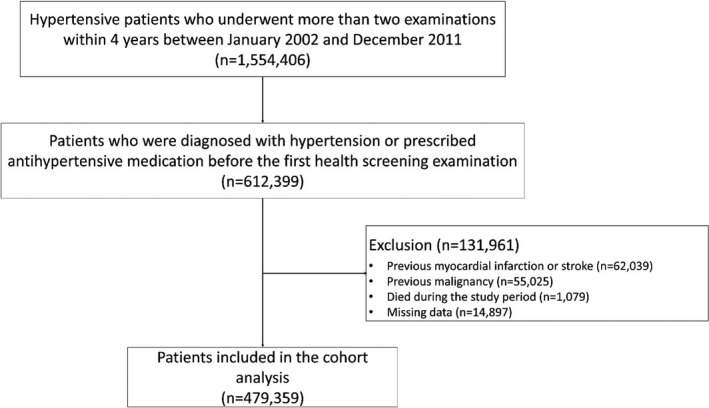
The cohort included 1 554 406 participants aged ≥19 years who underwent health screening at least twice within 4 years between 2002 and 2011. Among these participants, we included 612 399 individuals who were diagnosed with hypertension (I10–I13) or prescribed antihypertensive medication before the first health screening examination and had undergone more than 2 health examinations within 4 years between 2002 and 2011. We excluded patients with a prior diagnosis of myocardial infarction (MI; I21–I23) or stroke (I60–I64, I69) (n=62 039) and malignancy (C00–C99; n=55 025) or who died (n=1079) between the first and last health examinations. We also excluded patients with missing values in the health examination database (n=14 897). Finally, 479 359 patients were included in the main analysis. Individuals were followed up until death from any cause or the end of the study period (December 2017) or were censored for the development of MI or stroke (Figure 1).
Figure 1. Flowchart of the study population.
Sociodemographic Information
As a proxy for income, we used insurance premiums, as determined by government assessments of salary and assets. Because health insurance contributions in South Korea are imposed proportionally based on monthly salary, this measure could reflect income level. Household insurance premiums were initially categorized into 20 levels and grouped into quartiles among all households in Korea for the index year (Table S1). People with very low incomes or special care needs are covered by the medical aid program. Medical aid beneficiaries do not pay insurance premiums; their economic statuses are heterogeneous and are not included in income quartiles, and the number of medical aid beneficiaries among the screened people was very small (0.10%), thus we also excluded these participants.
BP Measurement
BP was measured using either sphygmomanometers or oscillometric devices after 3 to 5 minutes of rest at health examination centers or clinics. BP was measured at least twice at 1‐minute to 2‐minute intervals by qualified medical personnel using an appropriately sized cuff. The protocol for BP measurement is described elsewhere. 13 Baseline BP was defined as the mean values of 2 BP measurements during different health screenings, which we assumed to be representative of the overall BP levels. The study participants were categorized into the following 4 groups according to BP: <130/80, 130 to 139/80 to 89, 140 to 149/90 to 99, ≥150/100 mm Hg.
Follow‐Up and Outcome Measurement
Follow‐up data obtained for up to 16 years (until 2018) were analyzed. Median follow‐up was 9.2 years (interquartile range, 7.0–11.0). The primary end points were all‐cause and cardiovascular mortality during the study period. The secondary end points were cardiovascular events: a composite of cardiovascular death, MI, and stroke. All deaths and their causes were retrieved from the mortality records of the National Statistical Office of Korea. Cardiovascular death was defined as death attributed to CVD (I00–I99) by certificate. MI was defined as hospitalization with ICD‐10 codes I21–I23 as a primary or secondary diagnosis. Stroke was defined by discharge diagnosis (ICD‐10 codes I60–I69) among patients who had been hospitalized. 14
Statistical Analysis
Data are reported as mean±SD or median (interquartile range) for continuous variables and as number (percentage) for categorical variables. The incidence rates were estimated as the total number of outcomes during the follow‐up period divided by 100 000 person‐years. Cox proportional hazards regression models were used to estimate the effects of income and BP level at baseline on the risk of all‐cause and cardiovascular mortality and cardiovascular events with adjustment for covariates, such as age, sex, BP, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and aspirin or statin use. Covariates were carefully selected that were known to affect the outcomes. 15 , 16 We evaluated between‐group differences in risk by income/BP strata by visual inspection of the overlapping of the 95% CI. Subgroup analyses by antihypertensive medication use and sex were also performed. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC) and R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline Characteristics
A total of 479 359 individuals diagnosed with hypertension and with available BP values were followed for 4 415 708 person‐years. The baseline characteristics by income level are summarized in Table 1. Their median age was 60 years (interquartile range, 51–68 years), and 57% were women. The age was relatively higher in individuals with the highest income, and women were more prevalent in the lowest income group. BP, alcohol consumption, and body mass index were comparable across income levels. The proportions of current smokers were low in the highest income groups. Individuals with low incomes were less physically active and more likely to have diabetes mellitus and dyslipidemia, whereas individuals with the highest income were more likely to take aspirin, statins, or antihypertensive medications. These patterns were observed regardless of sex, except for a high diabetes mellitus prevalence in women with high incomes (Table S2).
Table 1.
Baseline Characteristics of the Study Population According to Income Level
| Income | P Value | ||||
|---|---|---|---|---|---|
| Quartile 1, Highest | Quartile 2 | Quartile 3 | Quartile 4, Lowest | ||
| Number of patients | 163 347 (34.0) | 119 253 (24.9) | 92 393 (19.3) | 104 366 (21.8) | <0.0001 |
| Age, y | 62 (52–70) | 59 (50–66) | 58 (50–66) | 58 (50–66) | <0.0001 |
| Sex | <0.0001 | ||||
| Male | 71 570 (43.8) | 54 005 (45.3) | 41 624 (45.0) | 41 176 (39.4) | |
| Female | 91 777 (56.2) | 65 248 (54.7) | 50 769 (55.0) | 63 190 (60.6) | |
| Blood pressure, mm Hg | <0.0001 | ||||
| Systolic blood pressure | 132.4±12.6 | 132.8±12.9 | 132.8±13.2 | 133.1±13.1 | |
| Diastolic blood pressure | 81.0±7.9 | 81.6±8.1 | 81.8±8.2 | 81.7±8.1 | |
| Smoking | <0.0001 | ||||
| Never | 118 278 (72.4) | 82 998 (69.6) | 62 740 (67.9) | 75 603 (72.4) | |
| Past | 26 193 (16.0) | 17 656 (14.8) | 13 077 (14.2) | 12 809 (12.3) | |
| Current | 18 876 (11.6) | 18 599 (15.6) | 16 576 (17.9) | 15 954 (15.3) | |
| Physical activity, times/wk | <0.0001 | ||||
| 0 | 84 219 (51.5) | 64 876 (54.4) | 51 456 (55.7) | 59 099 (56.6) | |
| 1–2 | 23 893 (14.6) | 17 548 (14.7) | 13 882 (15.0) | 14 669 (14.0) | |
| 3–4 | 20 510 (12.6) | 13 967 (11.7) | 10 224 (11.1) | 11 335 (10.9) | |
| 5–6 | 14 698 (9.0) | 9695 (8.1) | 7112 (7.7) | 8108 (7.8) | |
| 7 | 20 027 (12.3) | 13 167 (11.1) | 9719 (10.5) | 11 155 (10.7) | |
| Alcohol consumption, times/wk | <0.0001 | ||||
| 0 | 111 261 (68.1) | 77 812 (65.2) | 58 754 (63.6) | 69 909 (67.0) | |
| <1 | 18 814 (11.5) | 14 681 (12.3) | 12 032 (13.0) | 12 924 (12.4) | |
| 1–2 | 21 690 (13.3) | 17 351 (14.6) | 14 280 (15.5) | 14 282 (13.7) | |
| 3–4 | 6274 (3.8) | 5030 (4.2) | 3926 (4.2) | 3855 (3.7) | |
| ≥5 | 5308 (3.3) | 4379 (3.7) | 3401 (3.7) | 3396 (3.2) | |
| Body mass index, kg/m2 | 24.8±3.2 | 25.0±3.3 | 24.9±3.4 | 24.8±3.4 | <0.0001 |
| <18.5 | 2636 (1.6) | 2004 (1.7) | 1686 (1.8) | 1973 (1.9) | |
| 18.5–22.9 | 42 312 (25.9) | 30 221 (25.3) | 24 308 (26.3) | 28 254 (27.1) | |
| 23.0–24.9 | 42 874 (26.3) | 30 032 (25.2) | 22 698 (24.6) | 26 168 (25.1) | |
| ≥25.0 | 75 525 (46.2) | 56 996 (47.8) | 43 701 (47.3) | 47 971 (45.9) | |
| Fasting serum glucose, mg/dL | 105.0±28.4 | 105.5±30.5 | 105.6±31.3 | 105.8±32.3 | 0.735 |
| <100.0 | 87 854 (53.8) | 64 184 (53.8) | 49 984 (54.1) | 56 659 (54.3) | |
| 100.0–125.9 | 54 380 (33.3) | 39 166 (32.8) | 30 021 (32.5) | 33 568 (32.2) | |
| ≥126.0 | 21 113 (12.9) | 15 903 (13.4) | 12 388 (13.4) | 14 139 (13.5) | |
| Total cholesterol, mg/dL | 196.3±41.1 | 197.5±42.9 | 197.3±40.3 | 197.7±41.0 | <0.0001 |
| <200.0 | 91 720 (56.2) | 65 845 (55.2) | 51 318 (55.5) | 57 409 (55.0) | |
| 200.0–239.9 | 51 169 (31.3) | 37 458 (31.4) | 28 508 (30.9) | 32 793 (31.4) | |
| ≥240.0 | 20 458 (12.5) | 15 950 (13.4) | 12 567 (13.6) | 14 164 (13.6) | |
| Diabetes mellitus | 18 849 (11.5) | 13 397 (11.2) | 10 007 (10.8) | 11 165 (10.7) | <0.0001 |
| Aspirin | 43 983 (26.9) | 29 557 (24.8) | 21 574 (23.4) | 25 329 (24.3) | <0.0001 |
| Statin | 23 293 (14.3) | 15 657 (13.1) | 11 175 (12.1) | 13 034 (12.5) | <0.0001 |
| Antihypertensive medication | 82 321 (50.4) | 58 175 (48.8) | 44 535 (48.2) | 52 561 (50.4) | 0.017 |
Data are expressed as mean±SD, median (interquartile range), or number (percentage).
Mortality and Cardiovascular Events According to Income
Table 2 shows the mortality and cardiovascular event rates according to income level. In 4 415 708 person‐years, 47 860 deaths were observed. The all‐cause and cardiovascular mortality increased gradually with decreasing income. Compared with the highest income group (quartile 1), the lowest group (quartile 4) showed a 26% higher risk of all‐cause and 31% higher cardiovascular mortality after adjusting for sex, age, body mass index, smoking, physical activity, comorbidity, and aspirin or statin use. Cardiovascular events showed a similar trend, with the lowest income group showing a 7% higher risk compared with that in the highest income group. The risk of MI and stroke were also high in individuals with low incomes; however, the differences in the risk of these events were not prominent across income levels because the absolute event rates were low. Subgroup analyses by sex also revealed similar results (Table 2).
Table 2.
Incidence of Mortality and Cardiovascular Events According to Income Level in All Patients With Hypertension
| Income | ||||
|---|---|---|---|---|
| Quartile 1, Highest | Quartile 2 | Quartile 3 | Quartile 4, Lowest | |
| Total | ||||
| All‐cause mortality | ||||
| Events | 17 076 | 11 010 | 8812 | 10 962 |
| Person‐years | 1 518 195 | 1 097 667 | 840 612 | 959 235 |
| Incidence (events/100 000 person‐years) | 1125 | 1003 | 1048 | 1143 |
| Adjusted HR (95% CI) | Reference | 1.12 (1.09–1.15) | 1.22 (1.19–1.25) | 1.26 (1.23–1.29) |
| Cardiovascular mortality | ||||
| Events | 4301 | 2715 | 2209 | 2862 |
| Person‐years | 1 518 195 | 1 097 667 | 840 612 | 959 235 |
| Incidence (events/100 000 person‐years) | 283 | 247 | 263 | 298 |
| Adjusted HR (95% CI) | Reference | 1.12 (1.06–1.17) | 1.24 (1.17–1.30) | 1.31 (1.25–1.38) |
| MI | ||||
| Events | 3288 | 2319 | 1669 | 2048 |
| Person‐years | 1 569 652 | 1 131 642 | 869 919 | 997 053 |
| Incidence (events/100 000 person‐years) | 209 | 205 | 192 | 205 |
| Adjusted HR (95% CI) | Reference | 1.06 (1.01–1.12) | 1.02 (0.96–1.08) | 1.07 (1.01–1.13) |
| Stroke | ||||
| Events | 14 885 | 9764 | 7396 | 8729 |
| Person‐years | 1 497 688 | 1 086 012 | 833 855 | 954 467 |
| Incidence (events/100 000 person‐years) | 994 | 899 | 887 | 915 |
| Adjusted HR (95% CI) | Reference | 1.02 (1.00–1.05) | 1.05 (1.02–1.07) | 1.04 (1.01–1.06) |
| Cardiovascular events | ||||
| Events | 20 041 | 13 262 | 10 042 | 12 056 |
| Person‐years | 1 470 019 | 1 067 675 | 819 874 | 936 690 |
| Incidence (events/100 000 person‐years) | 1363 | 1242 | 1225 | 1287 |
| Adjusted HR (95% CI) | Reference | 1.04 (1.02–1.06) | 1.06 (1.03–1.09) | 1.07 (1.05–1.10) |
| Men | ||||
| All‐cause mortality | ||||
| Events | 9174 | 6268 | 5061 | 6085 |
| Person‐years | 687 336 | 506 781 | 378 642 | 374 375 |
| Incidence (events/100 000 person‐years) | 1335 | 1237 | 1337 | 1625 |
| Adjusted HR (95% CI) | Reference | 1.13 (1.09–1.17) | 1.25 (1.21–1.29) | 1.28 (1.24–1.32) |
| Cardiovascular mortality | ||||
| Events | 2066 | 1394 | 1129 | 1411 |
| Person‐years | 687 336 | 506 781 | 378 642 | 374 375 |
| Incidence (events/100 000 person‐years) | 301 | 275 | 298 | 377 |
| Adjusted HR (95% CI) | Reference | 1.13 (1.05–1.21) | 1.25 (1.16–1.35) | 1.32 (1.23–1.42) |
| MI | ||||
| Events | 1847 | 1351 | 973 | 1121 |
| Person‐years | 715 961 | 527 122 | 396 386 | 396 348 |
| Incidence (events/100 000 person‐years) | 258 | 256 | 245 | 283 |
| Adjusted HR (95% CI) | Reference | 1.06 (0.99–1.14) | 1.02 (0.94–1.10) | 1.07 (1.00–1.16) |
| Stroke | ||||
| Events | 6711 | 4583 | 3409 | 3958 |
| Person‐years | 684 862 | 506 801 | 380 780 | 377 989 |
| Incidence (events/100 000 person‐years) | 980 | 904 | 895 | 1047 |
| Adjusted HR (95% CI) | Reference | 1.04 (1.00–1.08) | 1.03 (0.99–1.08) | 1.05 (1.01–1.10) |
| Cardiovascular events | ||||
| Events | 9483 | 6545 | 4910 | 5758 |
| Person‐years | 669 098 | 496 195 | 372 566 | 368 083 |
| Incidence (events/100 000 person‐years) | 1417 | 1319 | 1318 | 1564 |
| Adjusted HR (95% CI) | Reference | 1.04 (1.01–1.08) | 1.05 (1.01–1.09) | 1.09 (1.05–1.12) |
| Women | ||||
| All‐cause mortality | ||||
| Events | 7902 | 4742 | 3751 | 4877 |
| Person‐years | 830 859 | 590 886 | 461 969 | 584 860 |
| Incidence (events/100 000 person‐years) | 951 | 803 | 812 | 834 |
| Adjusted HR (95% CI) | Reference | 1.10 (1.06–1.14) | 1.17 (1.13–1.22) | 1.21 (1.17–1.26) |
| Cardiovascular mortality | ||||
| Events | 2235 | 1321 | 1080 | 1451 |
| Person‐years | 830 859 | 590 886 | 461 969 | 584 860 |
| Incidence (events/100 000 person‐years) | 269 | 224 | 234 | 248 |
| Adjusted HR (95% CI) | Reference | 1.10 (1.02–1.17) | 1.20 (1.12–1.29) | 1.28 (1.20–1.37) |
| MI | ||||
| Events | 1441 | 968 | 696 | 927 |
| Person‐years | 853 692 | 604 520 | 473 533 | 600 705 |
| Incidence (events/100 000 person‐years) | 169 | 160 | 147 | 154 |
| Adjusted HR (95% CI) | Reference | 1.07 (0.99–1.16) | 1.03 (0.94–1.13) | 1.11 (1.02–1.21) |
| Stroke | ||||
| Events | 8174 | 5181 | 3987 | 4771 |
| Person‐years | 812 826 | 579 211 | 453 075 | 576 478 |
| Incidence (events/100 000 person‐years) | 1006 | 894 | 880 | 828 |
| Adjusted HR (95% CI) | Reference | 1.01 (0.98–1.05) | 1.05 (1.01–1.09) | 1.02 (0.98–1.06) |
| Cardiovascular events | ||||
| Events | 10 558 | 6717 | 5132 | 6298 |
| Person‐years | 800 921 | 571 480 | 447 308 | 568 607 |
| Incidence (events/100 000 person‐years) | 1318 | 1175 | 1147 | 1108 |
| Adjusted HR (95% CI) | Reference | 1.03 (1.00–1.07) | 1.07 (1.03–1.10) | 1.06 (1.03–1.10) |
HR was adjusted for age, sex, blood pressure level, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and aspirin or statin use. HR indicates hazard ratio; and MI, myocardial infarction.
We further tested whether the associations between income and mortality/cardiovascular events differed by antihypertensive medication use (Table 3). Similar to the main results, mortality and cardiovascular events increased gradually with decreasing income, regardless of antihypertensive medication use; however, the differences in the risk of all‐cause and cardiovascular mortality and cardiovascular events across income levels were more prominent in those who were not taking antihypertensive medications.
Table 3.
Mortality and Cardiovascular Events for Individuals According to Income and Antihypertensive Medication Use
| With Antihypertensive Medications | Without Antihypertensive Medications | |||||||
|---|---|---|---|---|---|---|---|---|
| Income Quartile 1, Highest | Income Quartile 2 | Income Quartile 3 | Income Quartile 4, Lowest | Income Quartile 1, Highest | Income Quartile 2 | Income Quartile 3 | Income Quartile 4, Lowest | |
| Total | ||||||||
| All‐cause mortality | ||||||||
| Events | 9071 | 5610 | 4304 | 5575 | 8005 | 5400 | 4508 | 5387 |
| Person‐years | 737 894 | 517 603 | 394 595 | 469 564 | 780 300 | 580 063 | 446 017 | 489 671 |
| Incidence (events/100 000 person‐years) | 1229 | 1084 | 1091 | 1187 | 1026 | 931 | 1011 | 1100 |
| Adjusted HR (95% CI) | Reference | 1.11 (1.07–1.15) | 1.16 (1.12–1.21) | 1.23 (1.19–1.27) | Reference | 1.13 (1.09–1.17) | 1.28 (1.24–1.33) | 1.29 (1.24–1.33) |
| Cardiovascular mortality | ||||||||
| Events | 2318 | 1438 | 1111 | 1476 | 1983 | 1277 | 1098 | 1386 |
| Person‐years | 737 894 | 517 603 | 394 595 | 469 564 | 780 300 | 580 063 | 446 017 | 489 671 |
| Incidence (events/100 000 person‐years) | 314 | 278 | 282 | 314 | 254 | 220 | 246 | 283 |
| Adjusted HR (95% CI) | Reference | 1.13 (1.06–1.21) | 1.19 (1.11–1.28) | 1.29 (1.21–1.38) | Reference | 1.10 (1.03–1.18) | 1.28 (1.19–1.38) | 1.32 (1.24–1.42) |
| MI | ||||||||
| Events | 1700 | 1144 | 812 | 1050 | 1588 | 1175 | 857 | 998 |
| Person‐years | 764 454 | 534 408 | 408 125 | 487 831 | 805 198 | 597 234 | 461 793 | 509 221 |
| Incidence (events/100 000 person‐years) | 222 | 214 | 199 | 215 | 197 | 197 | 186 | 196 |
| Adjusted HR (95% CI) | Reference | 1.03 (0.95–1.11) | 0.97 (0.89–1.06) | 1.04 (0.97–1.13) | Reference | 1.10 (1.02–1.19) | 1.07 (0.98–1.16) | 1.10 (1.01–1.19) |
| Stroke | ||||||||
| Events | 7637 | 4801 | 3629 | 4401 | 7248 | 4963 | 3767 | 4328 |
| Person‐years | 728 920 | 512 856 | 390 932 | 467 584 | 768 768 | 573 156 | 442 922 | 486 883 |
| Incidence (events/100 000 person‐years) | 1048 | 936 | 928 | 941 | 943 | 866 | 850 | 889 |
| Adjusted HR (95% CI) | Reference | 1.00 (0.96–1.04) | 1.02 (0.98–1.07) | 1.02 (0.98–1.06) | Reference | 1.05 (1.01–1.09) | 1.07 (1.02–1.11) | 1.05 (1.01–1.09) |
| Cardiovascular events | ||||||||
| Events | 10 402 | 6587 | 4964 | 6130 | 9639 | 6675 | 5078 | 5926 |
| Person‐years | 714 809 | 504 078 | 384 173 | 458 767 | 755 209 | 563 597 | 435 701 | 477 923 |
| Incidence (events/100 000 person‐years) | 1455 | 1307 | 1292 | 1336 | 1276 | 1184 | 1165 | 1240 |
| Adjusted HR (95% CI) | Reference | 1.01 (0.98–1.04) | 1.03 (1.00–1.07) | 1.05 (1.01–1.08) | Reference | 1.07 (1.03–1.10) | 1.09 (1.05–1.12) | 1.09 (1.06–1.13) |
| Men | ||||||||
| All‐cause mortality | ||||||||
| Events | 4728 | 3070 | 2389 | 3081 | 4446 | 3198 | 2672 | 3004 |
| Person‐years | 323 302 | 231 076 | 176 407 | 188 700 | 364 034 | 275 705 | 202 234 | 185 674 |
| Incidence (events/100 000 person‐years) | 1462 | 1329 | 1354 | 1633 | 1221 | 1160 | 1321 | 1618 |
| Adjusted HR (95% CI) | Reference | 1.10 (1.05–1.15) | 1.17 (1.11–1.23) | 1.24 (1.18–1.29) | Reference | 1.16 (1.11–1.22) | 1.33 (1.27–1.39) | 1.32 (1.26–1.39) |
| Cardiovascular mortality | ||||||||
| Events | 1075 | 692 | 547 | 713 | 991 | 702 | 582 | 698 |
| Person‐years | 323 302 | 231 076 | 176 407 | 188 700 | 364 034 | 275 705 | 202 234 | 185 674 |
| Incidence (events/100 000 person‐years) | 333 | 299 | 310 | 378 | 272 | 255 | 288 | 376 |
| Adjusted HR (95% CI) | Reference | 1.09 (0.99–1.20) | 1.18 (1.07–1.31) | 1.26 (1.14–1.38) | Reference | 1.17 (1.06–1.29) | 1.31 (1.18–1.46) | 1.37 (1.25–1.52) |
| MI | ||||||||
| Events | 906 | 682 | 469 | 590 | 941 | 669 | 504 | 531 |
| Person‐years | 337 547 | 240 418 | 184 241 | 199 014 | 378 413 | 286 704 | 212 145 | 197 334 |
| Incidence (events/100 000 person‐years) | 268 | 284 | 255 | 296 | 249 | 233 | 238 | 269 |
| Adjusted HR (95% CI) | Reference | 1.09 (0.99–1.21) | 0.98 (0.88–1.10) | 1.08 (0.98–1.20) | Reference | 1.03 (0.93–1.14) | 1.05 (0.94–1.17) | 1.06 (0.95–1.18) |
| Stroke | ||||||||
| Events | 3346 | 2171 | 1645 | 2029 | 3365 | 2412 | 1764 | 1929 |
| Person‐years | 322 408 | 231 559 | 176 907 | 190 155 | 362 453 | 275 242 | 203 872 | 187 834 |
| Incidence (events/100 000 person‐years) | 1038 | 938 | 930 | 1067 | 928 | 876 | 865 | 1027 |
| Adjusted HR (95% CI) | Reference | 0.99 (0.94–1.04) | 1.00 (0.94–1.06) | 1.04 (0.98–1.10) | Reference | 1.09 (1.03–1.14) | 1.06 (1.00–1.13) | 1.07 (1.01–1.13) |
| Cardiovascular events | ||||||||
| Events | 4760 | 3166 | 2384 | 2975 | 4723 | 3379 | 2526 | 2783 |
| Person‐years | 314 792 | 226 436 | 173 000 | 185 150 | 354 305 | 269 758 | 199 566 | 182 933 |
| Incidence (events/100 000 person‐years) | 1512 | 1398 | 1378 | 1607 | 1333 | 1253 | 1266 | 1521 |
| Adjusted HR (95% CI) | Reference | 1.01 (0.96–1.05) | 1.02 (0.97–1.07) | 1.07 (1.02–1.12) | Reference | 1.08 (1.03–1.13) | 1.09 (1.03–1.14) | 1.10 (1.05–1.15) |
| Women | ||||||||
| All‐cause mortality | ||||||||
| Events | 4343 | 2540 | 1915 | 2494 | 3559 | 2202 | 1836 | 2383 |
| Person‐years | 414 593 | 286 528 | 218 187 | 280 864 | 416 266 | 304 358 | 243 782 | 303 996 |
| Incidence (events/100 000 person‐years) | 1048 | 886 | 878 | 888 | 855 | 723 | 753 | 784 |
| Adjusted HR (95% CI) | Reference | 1.11 (1.06–1.17) | 1.14 (1.08–1.20) | 1.21 (1.15–1.27) | Reference | 1.08 (1.03–1.14) | 1.21 (1.15–1.28) | 1.22 (1.16–1.29) |
| Cardiovascular mortality | ||||||||
| Events | 1243 | 746 | 564 | 763 | 992 | 575 | 516 | 688 |
| Person‐years | 414 593 | 286 528 | 218 187 | 280 864 | 416 266 | 304 358 | 243 782 | 303 996 |
| Incidence (events/100 000 person‐years) | 300 | 260 | 258 | 272 | 238 | 189 | 212 | 226 |
| Adjusted HR (95% CI) | Reference | 1.16 (1.06–1.27) | 1.18 (1.06–1.30) | 1.30 (1.19–1.42) | Reference | 1.03 (0.93–1.14) | 1.24 (1.11–1.38) | 1.25 (1.14–1.38) |
| MI | ||||||||
| Events | 794 | 462 | 343 | 460 | 647 | 506 | 353 | 467 |
| Person‐years | 426 907 | 293 990 | 223 885 | 288 818 | 426 784 | 310 530 | 249 648 | 311 887 |
| Incidence (events/100 000 person‐years) | 186 | 157 | 153 | 159 | 152 | 163 | 141 | 150 |
| Adjusted HR (95% CI) | Reference | 0.95 (0.85–1.07) | 0.96 (0.85–1.10) | 1.04 (0.93–1.17) | Reference | 1.21 (1.07–1.36) | 1.10 (0.97–1.26) | 1.18 (1.05–1.34) |
| Stroke | ||||||||
| Events | 4291 | 2630 | 1984 | 2372 | 3883 | 2551 | 2003 | 2399 |
| Person‐years | 406 511 | 281 297 | 214 025 | 277 429 | 406 314 | 297 914 | 239 050 | 299 049 |
| Incidence (events/100 000 person‐years) | 1056 | 935 | 927 | 855 | 956 | 856 | 838 | 802 |
| Adjusted HR (95% CI) | Reference | 1.01 (0.96–1.06) | 1.04 (0.98–1.10) | 1.00 (0.95–1.05) | Reference | 1.02 (0.97–1.07) | 1.06 (1.01–1.12) | 1.03 (0.98–1.09) |
| Cardiovascular events | ||||||||
| Events | 5642 | 3421 | 2580 | 3155 | 4916 | 3296 | 2552 | 3143 |
| Person‐years | 400 017 | 277 642 | 211 173 | 273 617 | 400 904 | 293 838 | 236 135 | 294 990 |
| Incidence (events/100 000 person‐years) | 1410 | 1232 | 1222 | 1153 | 1226 | 1122 | 1081 | 1065 |
| Adjusted HR (95% CI) | Reference | 1.02 (0.97–1.06) | 1.05 (1.00–1.10) | 1.03 (0.99–1.08) | Reference | 1.05 (1.01–1.10) | 1.09 (1.04–1.14) | 1.09 (1.04–1.14) |
HR was adjusted for age, sex, levels of blood pressure, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and aspirin or statin use. HR indicates hazard ratio; and MI, myocardial infarction.
Mortality and Cardiovascular Events According to Income and BP Levels
The effects of each level of income and BP on mortality and cardiovascular events were determined by comparison to the lowest BP (<130/80 mm Hg) and highest income group. Among individuals with similar BP levels, we observed that low income levels were associated with the risk of high all‐cause and cardiovascular mortality and cardiovascular events (Figure 2, Figure S1A). However, in the highest BP (≥150/100 mm Hg) categories, the risk gradient was slightly attenuated in the lowest 2 income groups (quartiles 3 and 4), suggesting that high BP itself is a powerful risk factor. Of note, individuals with the highest income with a BP of 140 to 149/90 to 99 mm Hg had low all‐cause mortality (hazard ratio [HR], 1.03; 95% CI, 0.99–1.08) than those with the lowest income with a BP of <130/80 mm Hg (HR, 1.20; 95% CI, 1.14–1.26). In addition, we explored the risk stratified primarily by income and then by BP for each income level (Figure 3, Figure S1B). Among individuals with similar income levels, we observed that high BP was associated with the risk of high all‐cause and cardiovascular mortality and cardiovascular events. Even in the highest income group, the all‐cause (HR, 1.30; 95% CI, 1.24–1.37) and cardiovascular mortality (HR, 1.38; 95% CI, 1.26–1.52) increase significantly in the individuals with highest BP (≥150/100 mm Hg). Interestingly, J‐shaped associations between BP and all‐cause mortality as well as cardiovascular mortality were observed in the group with the highest income, with those with a BP of 130 to 139/80 to 89 mm Hg showing a lower risk compared with that in those with a BP of <130/80 mm Hg. Collectively, low income and high BP were associated with a high risk of mortality and cardiovascular events.
Figure 2. Mortality and cardiovascular events rates for 16 groups, stratified primarily by BP and then by income for each BP level.
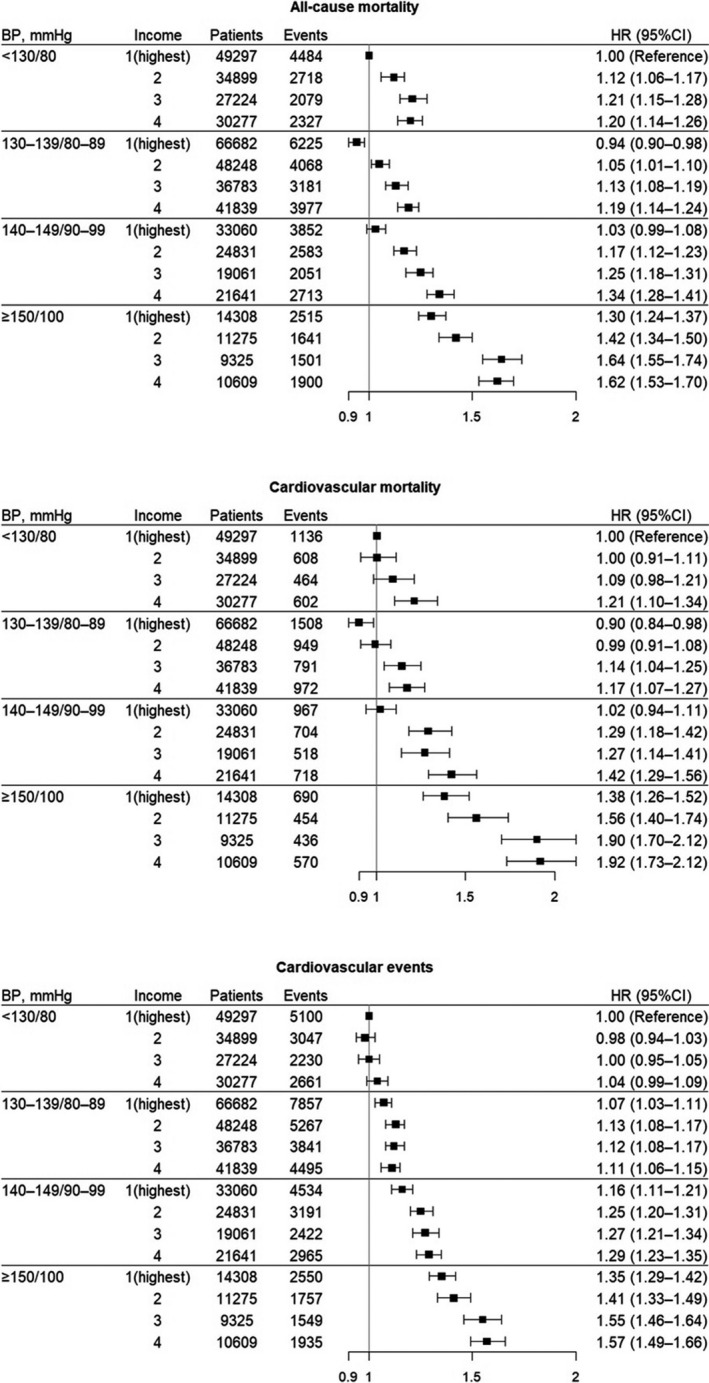
A Cox proportional hazard regression model adjusted for age, sex, BP, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and aspirin or statin use. The x axis refers to HR (95% CI), and HR itself (not log [HR]) was plotted. BP indicates blood pressure; and HR, hazard ratio.
Figure 3. Mortality and cardiovascular events rates for 16 groups, stratified primarily by income and then by BP for each income level.
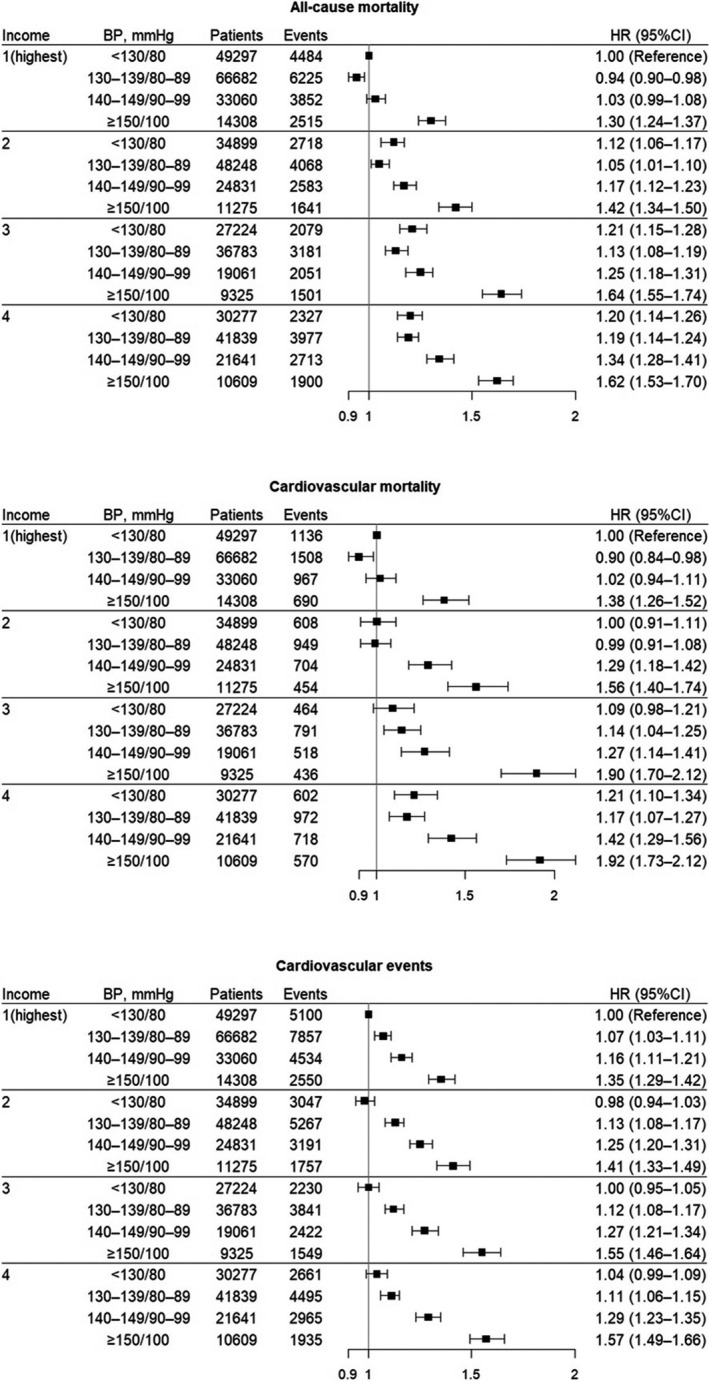
A Cox proportional hazard regression model adjusted for age, sex, BP, body mass index, smoking status, alcohol consumption, physical activity, fasting glucose, total cholesterol, and aspirin or statin use. The x axis refers to HR (95% CI), and HR itself (not log [HR]) was plotted. BP indicates blood pressure; and HR, hazard ratio.
Discussion
The main findings of this nationwide study were as follows: (1) patients with hypertension with low incomes were not only likely to have unhealthy behaviors but also had high risks of all‐cause and cardiovascular mortality and cardiovascular events, (2) low income and high BP had significant effects on all‐cause and cardiovascular mortality risks and cardiovascular events, and (3) the lowest income group had significantly more mortality and cardiovascular events compared with those in other income groups, regardless of BP. The excess risks of mortality and cardiovascular events associated with BP were more prominent in the lowest income group.
Previous studies have assessed the effects of SES on CVD and cardiovascular risk factors. 1 , 6 , 7 , 17 , 18 , 19 , 20 , 21 SES is strongly inversely associated with cardiovascular risk factors and CVD in high‐income and middle‐income countries. In high‐income countries, low income is associated with a high prevalence of cardiovascular risk factors, such as smoking, hypertension, obesity, a sedentary lifestyle, diabetes mellitus, and an unhealthy diet as well as high CVD incidence and mortality. 19 A recent meta‐analysis revealed increased pooled risk ratios for low‐income versus high‐income groups for coronary artery disease, cardiovascular events, stroke, and cardiovascular‐related deaths. 11 In another meta‐analysis, Backholer et al also reported increased pooled relative risks in low‐income versus high‐income groups for coronary heart disease, stroke, and all CVDs, with no evidence of the differential effect of income by sex. 22 However, few studies have assessed whether income as an indicator of SES affects mortality and cardiovascular outcomes in patients with hypertension. Using a nationwide population‐based database, our study demonstrated income‐related excess risks in terms of all‐cause mortality, cardiovascular mortality, MI, and stroke among patients with hypertension. These findings were observed regardless of antihypertensive medication use or sex. Our study also revealed even greater combined effects of BP and income on mortality and cardiovascular events. In our study, both uncontrolled BP and low income were associated with a significantly increased risk of all‐cause and cardiovascular mortality and cardiovascular events, with synergistic increases in the risks of mortality and cardiovascular events if both conditions were present.
Several interrelated pathways may explain how income level affects the relationship between hypertension and mortality or cardiovascular events. First, patients with high SES tend to have a high awareness of hypertension prevention and control and better accessibility and adherence to medical treatment. We also observed that a high income was associated with a high rate of administration of antihypertensive medications, aspirin, or statins; their preventive effect against cardiovascular events may have contributed to the inverse association between SES and mortality or cardiovascular events. However, income‐related adverse outcomes remained robust in the group without antihypertensive medication use, suggesting an independent role of income level as a potent risk factor. Second, the mechanisms driving socioeconomic inequalities in CVD are affected by multiple factors, such as the approachability, acceptability, availability, and affordability of medical services. 23 A recent systematic review showed an association between low SES and reduced access to coronary procedures and secondary prevention, which may explain the high risk of CVD death among disadvantaged groups. 24 We observed that the differences in cardiovascular mortality among income levels were obvious compared with those in MI or stroke. Further research is needed to evaluate disparities in access to medical care, including approachability, availability, accommodation, affordability, and acceptability according to income levels. 23 Third, patients with low SES are more likely to have unhealthy lifestyle behaviors and comorbid conditions, which lead to increased mortality. 25 The current study showed that individuals with the highest income were more physically active and less likely to have diabetes mellitus and dyslipidemia. Moreover, the proportion of current smokers was low in the highest income groups. Collectively, the mechanism by which low SES contributes to adverse outcomes is complicated by a variety of health behavioral factors, comorbid conditions, and out‐of‐disease factors intertwined with each other, which warrants further study.
This study has several strengths. Clinically, it is the largest study to demonstrate the effect of income on mortality and cardiovascular outcomes in patients with hypertension. Our study focused on income as a proxy for SES. Despite the relevance of income as a measure of socioeconomic factors, the income‐related issue has received less attention than other SES measures or conventional cardiovascular risk factors in most epidemiologic studies, partly because it is sensitive information. To our knowledge, this is the first study to examine the combined effects of income and BP on mortality and cardiovascular events in patients with hypertension. Moreover, we analyzed a large sample of Korean adults, which allowed for comparisons of 16 groups based on income and BP and analyses of all‐cause and cardiovascular mortality risks and cardiovascular events. From a research perspective, our study provided evidence to support the associations among income, mortality, and cardiovascular events in patients with hypertension.
This study has several limitations. First, its retrospective design limited the investigation of causal relationships. Second, income level, which was used as a proxy for SES, was assessed based on total household income unadjusted for the number of household members because of the lack of information regarding the number of household members, which might not assess accurate income level. Furthermore, SES is a complex factor comprising several dimensions (income, education, employment status, occupational position, and neighborhood socioeconomic characteristics). Thus, our use of a single indicator of SES might have underestimated its full effect on mortality and cardiovascular events. Third, this study included patients with hypertension who had undergone at least 2 health check‐ups to assess the association between mean BP outcomes in these patients; however, these may not be representative of the entire hypertensive population. This cohort tended to include more individuals with health concerns and high SES. 26 Fourth, because this study used ICD‐10 diagnosis codes rather than adjudicated events, we cannot rule out diagnostic inaccuracies for nonfatal cardiovascular events. Fifth, we only included cardiovascular death and a new diagnosis of MI and stroke as cardiovascular events because these are major events that can be used to evaluate the long‐term prognosis of patients with hypertension and can be clearly identified by the ICD code from the NHIS data. However, misclassifying or underestimating a diagnosis based on the ICD code was still a possibility. Finally, this study was based on Korean adults under universal health insurance and should be interpreted with caution when applied to different populations or different healthcare systems.
Perspectives
Income is significantly associated with the risk of all‐cause mortality, cardiovascular mortality, and cardiovascular events among patients with hypertension. The risks of mortality and cardiovascular events are high in those with low incomes and high BP. These findings suggest that income is an important aspect of social determinants of health that has an impact on cardiovascular outcomes in the care of hypertension.
Sources of Funding
None.
Disclosures
None.
Supporting information
Tables S1–S2
Figure S1
Acknowledgments
This study used National Health Insurance Service data (NHIS‐2020‐4‐125) from the Korean National Health Insurance Service. The authors thank the Korean Society of Hypertension for statistical assistance in this study.
(J Am Heart Assoc. 2021;10:e018446. DOI: 10.1161/JAHA.120.018446.)
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.120.018446
For Sources of Funding and Disclosures, see page 14.
Contributor Information
Myeong‐Chan Cho, Email: mccho@cbnu.ac.kr.
Ki‐Chul Sung, Email: kcmd.sung@samsung.com.
REFERENCES
- 1. Schultz WM, Kelli HM, Lisko JC, Varghese T, Shen J, Sandesara P, Quyyumi AA, Taylor HA, Gulati M, Harold JG, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137:2166–2178. DOI: 10.1161/CIRCULATIONAHA.117.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Luepker RV, Rosamond WD, Murphy R, Sprafka JM, Folsom AR, McGovern PG, Blackburn H. Socioeconomic status and coronary heart disease risk factor trends. The Minnesota Heart Survey. Circulation. 1993;88:2172–2179. DOI: 10.1161/01.CIR.88.5.2172. [DOI] [PubMed] [Google Scholar]
- 3. Wang J‐Y, Wang C‐Y, Juang S‐Y, Huang K‐Y, Chou P, Chen C‐W, Lee C‐C. Low socioeconomic status increases short‐term mortality of acute myocardial infarction despite universal health coverage. Int J Cardiol. 2014;172:82–87. DOI: 10.1016/j.ijcard.2013.12.082. [DOI] [PubMed] [Google Scholar]
- 4. Walsemann KM, Goosby BJ, Farr D. Life course SES and cardiovascular risk: heterogeneity across race/ethnicity and gender. Soc Sci Med. 2016;152:147–155. DOI: 10.1016/j.socscimed.2016.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Stringhini S, Carmeli C, Jokela M, Avendaño M, Muennig P, Guida F, Ricceri F, d'Errico A, Barros H, Bochud M. Socioeconomic status and the 25× 25 risk factors as determinants of premature mortality: a multicohort study and meta‐analysis of 1· 7 million men and women. Lancet. 2017;389:1229–1237. DOI: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marmot MG, Shipley MJ, Rose G. Inequalities in death–specific explanations of a general pattern? Lancet. 1984;1:1003–1006. DOI: 10.1016/S0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 7. Marmot MG, Smith GD, Stansfeld S, Patel C, North F, Head J, White I, Brunner E, Feeney A. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337:1387–1393. DOI: 10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- 8. Myers V, Drory Y, Goldbourt U, Gerber Y. Multilevel socioeconomic status and incidence of frailty post myocardial infarction. Int J Cardiol. 2014;170:338–343. DOI: 10.1016/j.ijcard.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 9. Bergström G, Redfors B, Angerås O, Dworeck C, Shao Y, Haraldsson I, Petursson P, Milicic D, Wedel H, Albertsson P, et al. Low socioeconomic status of a patient's residential area is associated with worse prognosis after acute myocardial infarction in Sweden. Int J Cardiol. 2015;182:141–147. DOI: 10.1016/j.ijcard.2014.12.060. [DOI] [PubMed] [Google Scholar]
- 10. Lenfant C. Conference on socioeconomic status and cardiovascular health and disease. Circulation. 1996;94:2041–2044. DOI: 10.1161/01.CIR.94.9.2041. [DOI] [PubMed] [Google Scholar]
- 11. Khaing W, Vallibhakara SA, Attia J, McEvoy M, Thakkinstian A. Effects of education and income on cardiovascular outcomes: a systematic review and meta‐analysis. Eur J Prev Cardiol. 2017;24:1032–1042. DOI: 10.1177/2047487317705916. [DOI] [PubMed] [Google Scholar]
- 12. Seong SC, Kim Y‐Y, Park SK, Khang YH, Kim HC, Park JH, Kang H‐J, Do C‐H, Song J‐S, Lee E‐J, et al. Cohort profile: the National Health Insurance Service‐National Health Screening Cohort (NHIS‐HEALS) in Korea. BMJ Open. 2017;7:e016640. DOI: 10.1136/bmjopen-2017-016640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee CJ, Hwang J, Lee YH, Oh J, Lee SH, Kang SM, Choi D, Kim HC, Park S. Blood pressure level associated with lowest cardiovascular event in hypertensive diabetic patients. J Hypertens. 2018;36:2434–2443. DOI: 10.1097/HJH.0000000000001842. [DOI] [PubMed] [Google Scholar]
- 14. Park TH, Choi JC. Validation of stroke and thrombolytic therapy in Korean National Health Insurance claim data. J Clin Neurol. 2016;12:42–48. DOI: 10.3988/jcn.2016.12.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jung M‐H, Yi S‐W, An SJ, Yi J‐J. Age‐specific associations between systolic blood pressure and cardiovascular mortality. Heart. 2019;105:1070–1077. DOI: 10.1136/heartjnl-2019-314697. [DOI] [PubMed] [Google Scholar]
- 16. D’Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care. Circulation. 2008;117:743–753. DOI: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 17. Nordahl H, Osler M, Frederiksen BL, Andersen I, Prescott E, Overvad K, Diderichsen F, Rod NH. Combined effects of socioeconomic position, smoking, and hypertension on risk of ischemic and hemorrhagic stroke. Stroke. 2014;45:2582–2587. DOI: 10.1161/STROKEAHA.114.005252. [DOI] [PubMed] [Google Scholar]
- 18. Marshall IJ, Wang Y, Crichton S, McKevitt C, Rudd AG, Wolfe CD. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015;14:1206–1218. DOI: 10.1016/S1474-4422(15)00200-8. [DOI] [PubMed] [Google Scholar]
- 19. de Mestral C, Stringhini S. Socioeconomic status and cardiovascular disease: an update. Curr Cardiol Rep. 2017;19:115. DOI: 10.1007/s11886-017-0917-z. [DOI] [PubMed] [Google Scholar]
- 20. Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta‐analysis. J Hypertens. 2015;33:221–229. DOI: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 21. Bray BD, Paley L, Hoffman A, James M, Gompertz P, Wolfe CDA, Hemingway H, Rudd AG. Socioeconomic disparities in first stroke incidence, quality of care, and survival: a nationwide registry‐based cohort study of 44 million adults in England. Lancet Public Health. 2018;3:e185–e193. DOI: 10.1016/S2468-2667(18)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Backholer K, Peters SA, Bots SH, Peeters A, Huxley RR, Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta‐analysis. J Epidemiol Community Health. 2017;71:550–557. DOI: 10.1136/jech-2016-207890. [DOI] [PubMed] [Google Scholar]
- 23. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz‐Flores S, Davey‐Smith G, Dennison‐Himmelfarb CR, Lauer MS, Lockwood DW, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. DOI: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 24. Schröder SL, Richter M, Schröder J, Frantz S, Fink A. Socioeconomic inequalities in access to treatment for coronary heart disease: a systematic review. Int J Cardiol. 2016;219:70–78. DOI: 10.1016/j.ijcard.2016.05.066. [DOI] [PubMed] [Google Scholar]
- 25. Kollia N, Panagiotakos DB, Georgousopoulou E, Chrysohoou C, Tousoulis D, Stefanadis C, Papageorgiou C, Pitsavos C. Exploring the association between low socioeconomic status and cardiovascular disease risk in healthy Greeks, in the years of financial crisis (2002–2012): the ATTICA study. Int J Cardiol. 2016;223:758–763. DOI: 10.1016/j.ijcard.2016.08.294. [DOI] [PubMed] [Google Scholar]
- 26. Suh Y, Lee CJ, Cho D‐K, Cho Y‐H, Shin D‐H, Ahn C‐M, Kim J‐S, Kim B‐K, Ko Y‐G, Choi D, et al. Impact of National Health Checkup Service on hard atherosclerotic cardiovascular disease events and all‐cause mortality in the general population. Am J Cardiol. 2017;120:1804–1812. DOI: 10.1016/j.amjcard.2017.07.093. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2
Figure S1


