Abstract
Background and Aims:
Transcutaneous electrical nerve stimulation (TENS) is a noninvasive complementary therapy for postoperative pain management. The effect of TENS on quality of recovery (QoR) and pain treatment in the early postoperative period is not well documented. The aim of this study was to evaluate the effect of TENS on postoperative QoR and pain in patients who had undergone a total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH + BSO).
Material and Methods:
Fifty-two patients were randomized into two groups: control (sham TENS treatment) and TENS (TENS treatment). QoR, dynamic pain, and static pain were evaluated after surgery.
Results:
The QoR score was significantly higher in the TENS group as compared with that in the control group (P = 0.029). Pain scores during coughing (dynamic pain) were significantly less in TENS group compared to control group (P <0.001). However, there was no between-group difference in pain scores at rest (static pain) or total analgesic consumption (P = 0.63 or P = 0.83, respectively).
Conclusion:
TENS may be a valuable tool to improve patients' QoR and dynamic pain scores after TAH + BSO.
Keywords: Abdominal hysterectomy, postoperative pain, quality of recovery, transcutaneous electrical nerve stimulation
Introduction
Hysterectomy is a commonly performed surgical procedure worldwide.[1] Successful postoperative pain management is important in improved recovery after surgery. Laparoscopic surgery can result in reduced postoperative pain. However, an abdominal surgical approach may be used in some hysterectomies, depending on the surgeon's and the patient's specific characteristics such as uterine size, vaginal shape, and body mass index. Current postoperative pain management protocols following abdominal hysterectomies are unsatisfactory.[2,3,4] The preferred postoperative pain relief method is opioid usage.[4] However, due to opioid-related side effects, including emesis and itching, opioid use can lead to poor quality of recovery (QoR).[5] Thus, contemporary pain therapy aims to reduce opioid usage via multimodal techniques.
Transcutaneous electrical nerve stimulation (TENS) is a noninvasive effective complementary therapy technique suggested as a part of a multimodal approach in postoperative pain management.[6] Some previous studies focused on the beneficial effects of TENS on pain and bladder function recovery after an abdominal hysterectomy.[7,8] However, the effect of TENS on QoR after an abdominal hysterectomy is unknown. Therefore, we conducted this prospective, randomized, controlled study to evaluate the effects of TENS on postoperative QoR and pain in patients who had undergone a total abdominal hysterectomy with bilateral salpingo-oophorectomy (TAH + BSO).
Material and Methods
After obtaining approval from the Tokat Gaziosmanpasa University Clinical Researches Ethical Committee (IRB no: 16-KAEK-083), this prospective, randomized, double-blind, sham-controlled study compared the effect of TENS on postoperative QoR after a TAH + BSO procedure. Informed written consent was obtained from all the patients. Fifty-two female patients, aged 18–65 years with American Society of Anesthesiologist (ASA) physical status I or II who underwent elective TAH + BSO for benign gynecological diseases in Tokat Gaziosmapasa University application and research center between March 2016 and May 2017 were enrolled in the study. The study protocol was registered at www.clinicaltrials.gov (NCT03072888). Patients who had dermatological lesions affecting electrode placement, preprocedural use of opioids, steroids, or psychoactive drugs, previous TENS experience, or a body mass index of ≥40 kg/m2 were excluded from the study. Fifty subjects completed the full study protocol and were included in the analysis [Figure 1].
Figure 1.
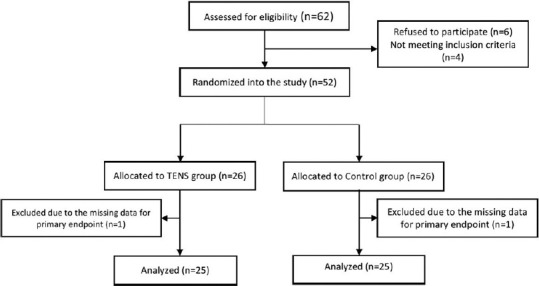
Flow diagram of the study
The patients were randomized using a computer-generated table of random numbers, into two groups; a TENS group and a control group. Randomization was done by an investigator not involved in the study. The name of the group to which the patient had been allocated was written on a piece of paper and the paper was placed inside a sealed opaque envelope. The patients, surgical team, and outcome assessor were blinded to the treatment assignment.
In the preoperative period, all the patients were informed about the use of patient-controlled analgesia (PCA) device and the visual analog scale (VAS).
Intraoperative procedure
All the surgical procedures were performed under general anesthesia according to a standardized protocol. Anesthesia was induced using propofol (1 mg/kg) and fentanyl (1 mcg/kg), and tracheal intubation was performed using rocuronium (0.6 mg/kg). Sevoflurane (1–2%) in 50% oxygen and 50% air was used for the maintenance of anesthesia. Approximately 30 min before the end of the operation, all patients received morphine (0.1 mg/kg) intravenously. At the end of the surgery, residual neuromuscular blockade was reversed using neostigmine (0.05 mg/kg) and atropine (0.02 mg/kg).
Postoperative procedure
In the recovery room, the PCA device was programmed to deliver morphine as a 0.02 mg/kg bolus dose intravenously, with a 15-min lockout interval, without a background infusion and then connected to the patients. The patients were reminded to press the PCA button when their pain score was higher than 3, as advised during the preoperative discussion. The TENS machine (CEFAR Medical AB, Malmö, Sweden) was connected to each patient via four electrodes placed approximately 1 cm from two parallel sides of the abdominal incision line. In the TENS group, the TENS machine was set at a high frequency (80 Hz) at a pulse duration of 180 MCS and applied for 30 min during seven sessions per day (postoperatively at 0, 2, 4, 6, 12, 18, and 24 h). The maximum tolerated sensory intensity was between 9 and 15 mA, which was adjusted, depending on the sensitivity of the individual patient. In the control group, no electrical stimulus was applied. In cases where the pain score exceeded 3, 1 g of paracetamol was administered intravenously.
Outcome measures
The demographic data record included age, body mass index, ASA physical status, surgery and anesthesia duration, perioperative analgesic consumption, pain scores at rest (static pain) and during coughing (dynamic pain), nausea, vomiting, and QoR scores. An investigator not involved with patient care was responsible for the perioperative data collection.
To assess QoR, the Turkish version of the QoR-40 questionnaire was administered 24 h postsurgery.[9] The QoR-40 questionnaire is a self-rated, 5-point Likert scale. It contains 40 items and 5 subscales: emotional state (9 items), physical comfort (12 items), patient support (7 items), physical independence (5 items), and pain (7 items). The total score can range from 40 to 200. A higher QoR-40 score indicates better QoR.[9]
The 10-cm VAS was used to assess pain intensity. The participants marked their pain intensity on the line at the appropriate point, with 0 denoting no pain and 10 denoting the worst possible pain. Static pain scores were evaluated at rest, and dynamic pain scores were evaluated during coughing postoperatively after 0 and 30 min and at 2, 4, 6, 12, 18, and 24 h.
Postoperative nausea and vomiting were evaluated using a 5-point Likert scale (0 = no nausea/vomiting, 1 = minimal nausea, 2 = moderate nausea, 3 = vomiting only once, and 4 = vomiting two or more times).
Sample size
The primary outcome was the QoR scores at postoperative 24 h. In a previous study, the mean and standard deviation (SD) QoR-40 scores of patients after TAH was 174.6 ± 10.0.[10] Assuming a two-sided type 1 error 0.01 (α = 0.01) and a power of 0.80 (β = 0.02), we calculated that a minimum of 23 patients per group were required to detect a 10-point improvement in QoR-40 scores. Thus, we determined that a sample size of 52 patients would be acceptable to account for the possibility of patient dropouts.
Statistical analysis
All statistical analyses were performed using SPSS software version 20.0 (SPSS Inc., Chicago, IL, USA). The one-sample Kolmogorov–Smirnov test was used to test the normality of the distribution. Descriptive data were presented as the mean ± SD for continuous variables, median (range) for ordinal variables, and number (frequencies) for categorical variables. Continuous variables were compared using an independent samples t-tests or Mann–Whitney U tests. Categorical variables were analyzed using Pearson's Chi-square or Fischer's exact tests. A repeated-measures analysis of variance was utilized to assess differences in VAS scores. A P value of <0.05 was considered statistically significant.
Results
Fifty-two patients were randomized in the study and 50 patients completed the study protocol. The flow diagram of the study is shown in Figure 1.
There were no statistically significant between-group differences in demographic and surgical characteristics [Table 1].
Table 1.
Demographic and perioperative characteristics
| Characteristics | Control | TENS | P |
|---|---|---|---|
| Patients (n) | 25 | 25 | - |
| Age (years) | 54 (33) | 49 (23) | 0.07 |
| Body mass index | 25.8±1.8 | 25.2±2.3 | 0.38 |
| ASA status (I/II) | 11/14 | 10/15 | 0.72 |
| Duration of operation (min) | 100 (40) | 100 (30) | 0.97 |
Data are presented as mean±SD, median (range) or number. TENS: transcutaneous electrical nerve stimulation, ASA: the American Society of Anesthesiologists
Global QoR-40 scores in the TENS group were significantly higher than those in the control group (P = 0.029) [Table 2]. Among the QoR-40 subscale scores, only physical independence and pain scores were significantly different in the two groups (P = 0.017, P = 0.001 respectively) [Table 2].
Table 2.
Quality of recovery scores
| Control | TENS | P | |
|---|---|---|---|
| Physical independence | 22 (7) | 22 (8) | 0.953 |
| Physical comfort | 50 (13) | 54 (17) | 0.020 |
| Pain | 32 (7) | 34 (6) | 0.001 |
| Support | 35 (1) | 35 (1) | 1 |
| Emotional status | 45 (2) | 45 (2) | 0.350 |
| Global QoR-40 score | 186 (22) | 188 (22) | 0.029 |
Data are presented as median (range), QoR: quality of recovery
There was a significant between-group difference in pain scores during coughing (P <0.001) [Figure 2]. The TENS treatment reduced pain scores during coughing at 0 and 30 min and 2, 4, 6, 12, 18, and 24 h after surgery. However, there was no between-group difference in pain scores at rest, total morphine consumption, or nausea and vomiting scores [Figure 3 and Table 3]. Four patients in the TENS group and six patients in the control group required additional analgesics (paracetamol). However, there was no between-group difference in additional analgesic consumption (P = 0.48).
Figure 2.
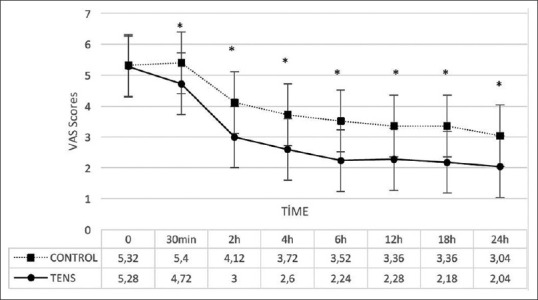
Changes in dynamic pain scores. Data are presented as mean and SD. The difference in scores between the two groups was statistically significant using repeated measures ANalysis Of VAriance (ANOVA) test (P <0.001). Posthoc test showed that visual analog scale (VAS) scores during coughing were statistically different at each time points except at 0 h. * = P < 0.05
Figure 3.
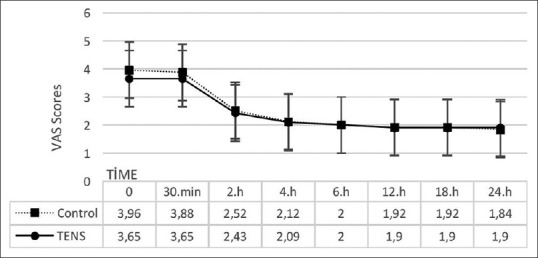
Changes in the Static Pain Scores. Data are presented as mean and SD. There is no statistical difference in the static pain scores using repeated measures ANOVA test (P = 0.451)
Table 3.
Total morphine consumption and the nausea-vomiting scores of the patients
| Control | TENS | P | |
|---|---|---|---|
| Total morphine consumption | 26.6±3 | 26.3±2.8 | 0.769 |
| Nausea and vomiting score | 0 (3) | 0 (3) | 1.0 |
Data are presented as mean±SD or median (range)
Discussion
The findings of this study indicated that TENS treatment improved the QoR scores of patients following TAH + BSO under general anesthesia. Moreover, TENS had a positive effect on dynamic pain scores. However, TENS did not affect static pain scores or total analgesic consumption.
Improving patient care is a primary goal for health care providers. Despite advances in medical facilities in recent years, multiple complications may occur during the perioperative term and lead to patient dissatisfaction. Postoperative pain is an important source of patient postoperative dissatisfaction.[11] TENS is administered using an easy-to-handle device that delivers low-voltage electrical currents through the skin via electrodes to reduce pain.[6] This non-pharmacological pain management technique has attracted research attention due to its low cost and absence of undesirable effects. Although several studies have evaluated the effectiveness of TENS for pain management, to the best of our knowledge, there are no studies on the effect of TENS on the QoR.[6,12]
QoR in the early period following anesthesia is an easy and reliable outcome to measure the postoperative health quality. QoR is multidimensional and can be affected by many variables such as pain, emotional status, physical comfort, and independence.[13] In the present study, the patients' QoR scores improved in the TENS group. Among the QoR-40 subscales; there was a statistically significant between-group difference in physical independence and pain scores. Wu et al. reported that pain during activity had a higher correlation coefficient with the QoR score than pain at rest. In the present study, dynamic pain decreased in the TENS group, and this may have improved the patients' movement.[14] Therefore, treating postoperative dynamic pain with TENS may have helped the patients have greater physical independence and improved QoR.
As pain is patient-specific, assessing the success of postoperative pain therapy is difficult. The VAS and other numeric rating scales are reliable tools for assessing acute pain.[15] However, if a pain assessment includes only the period at rest, the effect of particular therapy methods may be unclear, as systemic opioids are generally sufficient to combat pain at rest. The data from Niemi et al.'s study documented that dynamic, cough-provoked pain was a more sensitive outcome measure of postoperative pain relief than pain at rest.[16] Thus, in the present study, we assessed pain at rest and during coughing. TENS reduced only dynamic pain scores. In another study, Rakel et al. investigated the effectiveness of TENS on pain after abdominal surgery and reported that it was effective in reducing pain only during movement, similar to our results.[17] These results may be attributed to the nature of pain after abdominal surgery. Pain after an abdominal hysterectomy arises from cutaneous, deep somatic, or visceral structures due to tissue damage.[18] Although characterizing the source of pain is difficult, sharp and sudden pain is related to the abdominal wall and mediated by Aδ fibers. In contrast, burning pain is mediated by C-fibers and thought to originate from deeper structures.[19] Postsurgical pain at rest is usually moderate. However, pain during various activities such as coughing and turning may be severe due to reactivation of Aδ fibers.[19,20] Moreover, Aδ fiber-mediated pain exhibits a decreased response to opioids.[21] Previous pharmacological and physiological studies demonstrated that TENS reduced primary mechanical hyperalgesia by stimulating Aα, Aβ, and Aδ fibers.[22,23,24] In the present study, we did not evaluate this relationship. Nevertheless, the effect of TENS on Aδ fibers may explain the analgesic effect of TENS during coughing, but not at rest.
In the present study, in relation to analgesic consumption, the amount of opioid drug usage was similar in the two groups, although the patients in the control group had high pain scores during movement. This discrepancy may have resulted from patients' avoidance of movement and demanding opioids according to their pain at rest. Another study that evaluated the effect of TENS on pain management after knee arthroplasty based on the cumulative morphine dose used via PCA found no significant reduction in the dose after TENS.[25] The authors concluded that there was no utility for TENS in the postoperative management of pain after knee arthroplasty.[25] However, they did not present data on pain scores due to missing data points or paradoxical reporting.[25] In another study, Rakel et al. reported similar results to those found in the present study. In their study, although TENS did not reduce postoperative opioid consumption after total knee arthroplasty, it reduced pain scores during activity. They concluded that TENS was a useful analgesic method after a total knee arthroplasty as compared with pharmacological analgesia alone.[12] Similarly, our study demonstrated that TENS treatment was a useful complementary analgesic method after TAH + BSO.
The present study has some limitations. First, the sample size was relatively small. Second, although the TENS machine was similarly placed to patients in both groups, the patients in the control group did not receive any electrical stimulus. Thus, it is possible that the patients could have deduced the group allocation. And, we did not evaluate the awareness of the patients regarding whether real or sham TENS therapy was applied during the study.
Conclusion
TENS may be a valuable tool to improve the patient's QoR and dynamic pain scores after TAH + BSO.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
All of the authors declare no conflict of interest.
Acknowledgements
The abstract of this study was presented in ARUD 2017 Balkan States Anesthesia Days – IV, 2017, Sarajevo, Bosnia, and Herzegovina.
References
- 1.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–5. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 2.Wijk L, Franzen K, Ljungqvist O, Nilsson K. Implementing a structured enhanced recovery after surgery (ERAS) protocol reduces length of stay after abdominal hysterectomy. Acta Obstet Gynecol Scand. 2014;93:749–56. doi: 10.1111/aogs.12423. [DOI] [PubMed] [Google Scholar]
- 3.Gharaei H, Imani F, Almasi F, Solimani M. The effect of ultrasound-guided TAPB on pain management after total abdominal hysterectomy. Korean J Pain. 2013;26:374–8. doi: 10.3344/kjp.2013.26.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azari L, Santoso JT, Osborne SE. Optimal pain management in total abdominal hysterectomy. Obstet Gynecol Surv. 2013;68:215–27. doi: 10.1097/OGX.0b013e31827f5119. [DOI] [PubMed] [Google Scholar]
- 5.De Oliveira GS, Jr, Milad MP, Fitzgerald P, Rahmani R, McCarthy RJ. Transversus abdominis plane infiltration and quality of recovery after laparoscopic hysterectomy: A randomized controlled trial. Obstet Gynecol. 2011;118:1230–7. doi: 10.1097/AOG.0b013e318236f67f. [DOI] [PubMed] [Google Scholar]
- 6.Johnson MI. Transcutaneous electrical nerve stimulation (TENS) as an adjunct for pain management in perioperative settings: A critical review. Expert Rev Neurother. 2017;17:1013–27. doi: 10.1080/14737175.2017.1364158. [DOI] [PubMed] [Google Scholar]
- 7.Sun XL, Wang HB, Wang ZQ, Cao TT, Yang X, Han JS, et al. Effect of transcutaneous electrical stimulation treatment on lower urinary tract symptoms after class III radical hysterectomy in cervical cancer patients: Study protocol for a multicentre, randomized controlled trial. BMC Cancer. 2017;17:1–7. doi: 10.1186/s12885-017-3387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh M, Khan RM, Bano S, Huda W, Hakim S, Grover N. Non-pharmacological relief of acute pain following total abdominal hysterectomy. Can J Anesth. 2002;49:530–1. doi: 10.1007/BF03017944. [DOI] [PubMed] [Google Scholar]
- 9.Karaman S, Arici S, Dogru S, Karaman T, Tapar H, Kaya Z, et al. Validation of the Turkish version of the quality of recovery-40 questionnaire. Health Qual Life Outcomes. 2014;12:1–6. doi: 10.1186/1477-7525-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karaman T, Ozsoy AZ, Karaman S, Dogru S, Tapar H, Sahin A, et al. The effects of transversus abdominis plane block on analgesic and anesthetic consumption during total abdominal hysterectomy: A randomized controlled study. Rev Bras Anestesiol. 2018;68:285–91. doi: 10.1016/j.bjane.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gebremedhn EG, Chekol WB, Amberbir WD, Flatie TD. Patient satisfaction with anaesthesia services and associated factors at the University of Gondar Hospital, 2013: A cross-sectional study. BMC Res Notes. 2015;8:1–9. doi: 10.1186/s13104-015-1332-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rakel BA, Zimmerman MB, Geasland K, Embree J, Clark CR, Noiseux NO, et al. Transcutaneous electrical nerve stimulation for the control of pain during rehabilitation after total knee arthroplasty: A randomized, blinded, placebo-controlled trial. Pain. 2014;155:2599–611. doi: 10.1016/j.pain.2014.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myles PS, Weitkamp B, Jones K, Melick J, Hensen S. Validity and reliability of a postoperative quality of recovery score: The QoR-40. Br J Anaesth. 2000;84:11–5. doi: 10.1093/oxfordjournals.bja.a013366. [DOI] [PubMed] [Google Scholar]
- 14.Wu CL, Rowlingson AJ, Partin AW, Kalish MA, Courpas GE, Walsh PC, et al. Correlation of postoperative pain to quality of recovery in the immediate postoperative period. Reg Anesth Pain Med. 2005;30:516–22. doi: 10.1016/j.rapm.2005.07.190. [DOI] [PubMed] [Google Scholar]
- 15.Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 16.Niemi G, Breivik H. The minimally effective concentration of adrenaline in a low-concentration thoracic epidural analgesic infusion of bupivacaine, fentanyl and adrenaline after major surgery. A randomized, double-blind, dose-finding study. Acta Anaesthesiol Scand. 2003;47:439–50. doi: 10.1034/j.1399-6576.2003.00077.x. [DOI] [PubMed] [Google Scholar]
- 17.Rakel B, Frantz R. Effectiveness of transcutaneous electrical nerve stimulation on postoperative pain with movement. J Pain. 2003;4:455–64. doi: 10.1067/s1526-5900(03)00780-6. [DOI] [PubMed] [Google Scholar]
- 18.Leung CC, Chan YM, Ngai SW, Ng K-J, Tsui SL. Effect of pre-incision skin infiltration on post-hysterectomy pain--a double-blind randomized controlled trial. Anaesth Intensive Care. 2000;28:510–6. doi: 10.1177/0310057X0002800504. [DOI] [PubMed] [Google Scholar]
- 19.Brennan TJ. Pathophysiology of postoperative pain. Pain. 2011;152:S33–40. doi: 10.1016/j.pain.2010.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pirec V, Laurito CE, Lu Y, Yeomans DC. The combined effects of N-type calcium channel blockers and morphine on A-delta versus C fiber mediated nociception. Anesth Analg. 2001;92:239–43. doi: 10.1097/00000539-200101000-00046. [DOI] [PubMed] [Google Scholar]
- 21.Yeomans DC, Cooper BY, Vierck CJ., Jr Effects of systemic morphine on responses of primates to first or second pain sensations. Pain. 1996;66:253–63. doi: 10.1016/0304-3959(96)03082-5. [DOI] [PubMed] [Google Scholar]
- 22.Gopalkrishnan P, Sluka KA. Effect of varying frequency, intensity, and pulse duration of transcutaneous electrical nerve stimulation on primary hyperalgesia in inflamed rats. Arch Phys Med Rehabil. 2000;81:984–90. doi: 10.1053/apmr.2000.5576. [DOI] [PubMed] [Google Scholar]
- 23.Radhakrishnan R, Sluka KA. Deep tissue afferents, but not cutaneous afferents, mediate transcutaneous electrical nerve stimulation-induced antihyperalgesic. J Pain. 2000;81:984–90. doi: 10.1016/j.jpain.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Levin MF, Hui-Chan CW. Conventional and acupuncture-like transcutaneous electrical nerve stimulation excite similar afferent fibers. Arch Phys Med Rehabil. 1993;74:54–60. [PubMed] [Google Scholar]
- 25.Breit R, Van der Wall H. Transcutaneous electrical nerve stimulation for postoperative pain relief after total knee arthroplasty. J Arthroplasty. 2004;19:45–8. doi: 10.1016/s0883-5403(03)00458-3. [DOI] [PubMed] [Google Scholar]


