Abstract
Canalicular adenoma (CA) is a rare, benign salivary gland tumor that has special tendency to occur in the upper lip. Buccal mucosa is the second most common site. It occurs more often in older patients with peak prevalence in the seventh decade of life. A definitive female predominance has been reported. According to the latest English published literature, 531 cases of CA have been reported. We present a case of CA of the hard palate that presented in a 29-year-old female patient. The histopathological and immunohistochemical findings showed typical features of CA and intense expression of pan-cytokeratin and S-100 protein. We also review its differential diagnosis from other salivary gland tumors.
Key Words: Adenoma, canalicular, minor salivary gland, palate
INTRODUCTION
Canalicular adenoma (CA) is an uncommon benign tumor that occurs almost exclusively in the minor salivary glands, accounting for approximately 1% of all salivary gland tumors. Because of its uniform microscopic pattern, CA has also been called as monomorphic adenoma.[1]
CA shows a striking predilection for the upper lip, with nearly 75% of cases having occurred in this location. Buccal mucosa is the second most common site.[1] Moreover, the third common location is the palate.[2,3] It occurs more often in older patients with a peak prevalence noted in the seventh decade and women are affected commonly.[4,5,6] It presents as a painless, slowly growing nonulcerative nodule usually ranging from several millimeters to 2 cm in size.[1,2] The overlying mucosa may be normal in color or bluish. In some instances, the lesion presents multifocally.[1]
Histologically, it consists of monomorphic columnar or cuboidal epithelial cells, with deeply basophilic nuclei arranged in single or bilayered cords/tubules.[1,2,3,4,5] The ductal structures in the form of long canals are called tubules. The tumor cells are supported by a loose connective tissue stroma with scattered blood vessels being surrounded by a delicate fibrous capsule. The mitotic activity is uncommon.[5,6,7] In this paper, we report one such rare case of CA of the palate. According to our information from different literature, this is the first report of CA in the palate in Iran.
CASE REPORT
A 29-year-old female patient was referred to Zanjan University of Medical Science with a chief complaint of palatal swelling and for carrying out an excisional biopsy and pathological examination of the same. Clinically, it presented as a nonulcerative exophytic soft tissue lesion measuring 3 mm × 5 mm with a covering normal mucosa in the mid-palatal area on the hard palate. (Note: Clinical picture of the lesion was not taken before the surgery, but follow-up picture was taken.) The patient was systemically healthy and was not on any medication. Differential diagnosis could be basal cell adenoma, mucocele, and pleomorphic adenoma. The lesion was excised under local anesthesia. There was no erosion of the underlying bone. The macroscopic examination showed multiple pieces of brown soft tissue approximately measuring 0.3 cm × 0.5 cm × 0.8 cm.
Microscopically, hematoxylin and eosin-stained sections revealed multiple large lobular islands of cuboidal-to-columnar epithelial cells with deep basophilic nuclei arranged in single or bilayered cords, with droplets of hyaline material being noted scattered among the epithelial cells. Parallel rows of epithelial cells with basophilic nuclei appeared to form ductal structures. Stroma was hypocellular and vascular and neither cytological pleomorphism nor mitotic figures were observed [Figures 1 and 2].
Figure 1.
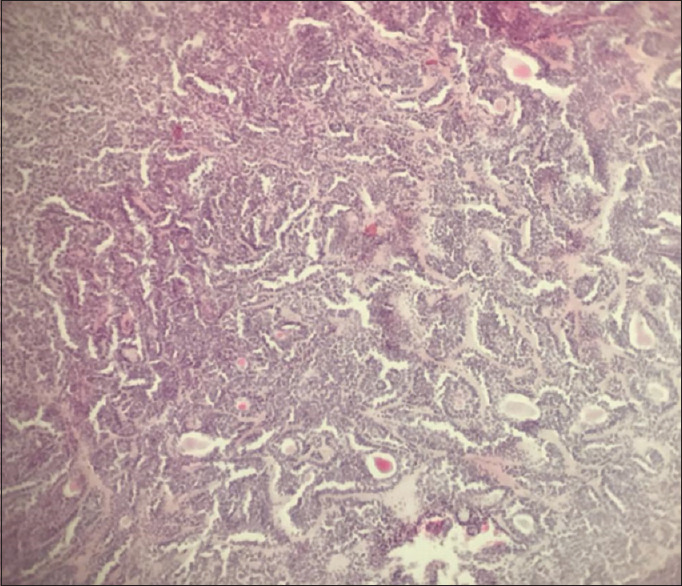
Parallel rows of epithelial cells with basophilic nuclei appeared to form ductal structures (H and E, ×40).
Figure 2.
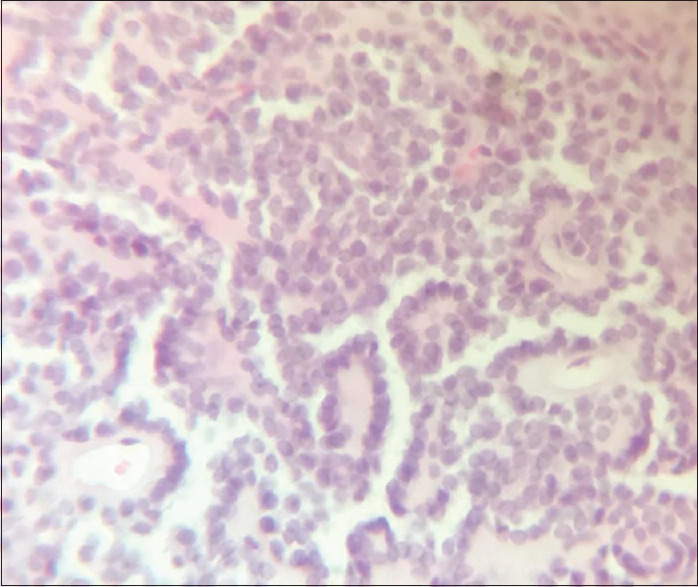
Single or bilayered cords of uniform cuboidal epithelial cells which enclose ductal structures in the form of long canals (H and E, ×100).
Immunohistochemically, most of the glandular epithelial cells stained positive for S-100 and pan-cytokeratin. The S-100 protein staining was localized to outer portions of the canals [Figure 3]. Intense expression of pan-cytokeratin by tumor cells was also noted. According to Machado de Sousa et al., solid areas of basal cell adenoma did not stain for cytokeratins,[8] so definite diagnosis of CA was confirmed. In our case, the lesion was surgically excised, and there have been no recurrences even after 6-month follow-up [Figure 4].
Figure 3.
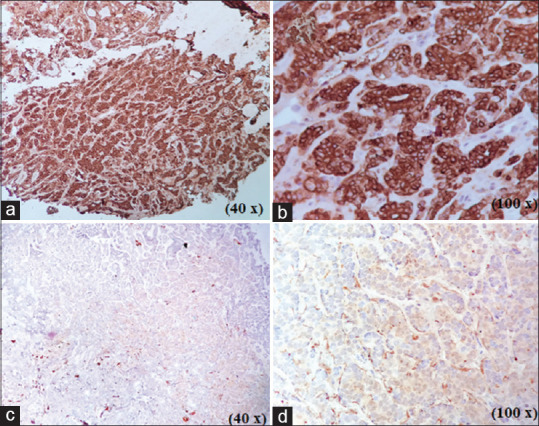
(a and b) Intense expression of pan-cytokeratin by tumor cells. The staining was cytoplasmic (×40 and × 100). (c and d) Canalicular adenoma stained with S-100 protein. Staining was localized to outer portions of canals (×40 and × 100).
Figure 4.

Clinical view about 6 months later with no report of recurrence or any evidence of new lesion.
DISCUSSION
In 1953, Bhaskar and Weinmann described CA for the first time.[9] Rauch et al. in 1970 stated that benign tumors of the salivary glands could be divided into two categories: monomorphic adenomas and pleomorphic adenomas.[10] In 1972, the World Health Organization classified monomorphic adenomas further to include CA and basal cell adenoma.[11] In 1984, Gardner and Daley announced that CA and basal cell adenoma were two distinct lesions in terms of clinical presentation and histopathological and histochemical findings.[12] In 2006, Liess et al. further divided monomorphic adenoma into three categories: canalicular, basal cell, and trabeculotubular types.[13] Hence, multiple instances of origin and classification have been cited in different articles.
According to Neville et al., 2015, the term “monomorphic adenoma” should be avoided and each tumor in the category of monomorphic adenoma should be referred to by its specific name.[1]
CA is a rare, benign minor salivary gland tumor that shows a striking predilection for the upper lip, with nearly 75% of cases having been reported in this location. The buccal mucosa is the second most common site.[1] Based on the systematic review published in 2017, CA was found mostly in the upper lip (55%) and buccal mucosa (23.4%); hard palate was the third most common location (14%).[3] In our case, it was reported in the hard palate which is an uncommon site. According to the latest published English literature, 531 cases of CA have been reported so far.[2,3,14] Out of which, 52 cases were reported in the hard palate (14.5%),[3] four cases were reported in the parotid gland (1.1%), and one was reported in the lacrimal gland.[15] According to our knowledge from different literature, there are some reports in Turkey,[16,17] and in Iran, there was only one case report of parotid gland.[18] CA was frequently diagnosed in the seventh decade of life, and it occurred most often in women (64%).[3] Our patient was a 29-year-old female. Clinically, CA presents as a painless, nonulcerative single nodular lesion (46.5%) or as a submucosal swelling (8.8%), mass (3.8%), multiple nodules (1.3%), and bilateral nodules (0.6%). The tumors tend to be solitary but sometimes can be found as multiple tumors (10%).[3,15,19] Our case presented as a solitary nodule.
Clinically, CA of the minor glands can be misdiagnosed as basal cell adenoma/mucocele/pleomorphic adenoma. If it presents in the parotid gland, Warthin's tumor and adenoid cystic carcinoma should be differentiated from CA.[19]
The histopathological findings of our case showed typical CA characteristics, such as single or bilayered strands of cuboidal-to-columnar cells with deeply basophilic nuclei enclosing ductal spaces/tubules. Droplets of hyaline material were noted scattered among the epithelial cells. Stroma was hypocellular and vascular, and neither cytological pleomorphism nor mitotic figures were observed. Histologically, owing to the basaloid nature of tumor cells, CA needs to be differentiated from other salivary gland tumors, such as basal cell adenoma, adenoid cystic carcinoma, and low-grade adenocarcinoma. Thus, immunohistochemical examination can prove useful in confirming the diagnosis.[20] Many a reported cases of CA have shown strong and diffuse reaction to pan-cytokeratin and S-100 protein.[21,22,23] Our immunohistochemical findings too reconfirmed the diffuse positivity for S-100 protein and pan-cytokeratin.
The treatment of CA is surgical excision and enucleation. Recurrences are uncommon and have only been reported in 5% of patients treated by surgical excision. These cases probably must have recurred owing to the multifocal nature of CA.[1,3,19] Werder et al. recommended regular clinical follow-up of CA after the surgical removal.[24]
CONCLUSION
CA is an uncommon, benign, slow-growing minor salivary gland tumor. There have been no reported cases of metastasis, malignant changes, or tumor-related death. Treatment is best achieved by complete surgical removal, and the prognosis is excellent.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- 1.Neville BW, Damm DD, Allen CM, Chi AC. Oral and Maxillofacial Pathology. 4th edition. Missouri: WB saunders, Elsevier Health Sciences; 2016. [Google Scholar]
- 2.Thompson LD, Bauer JL, Chiosea S, McHugh JB, Seethala RR, Miettinen M, et al. Canalicular adenoma: A clinicopathologic and immunohistochemical analysis of 67 cases with a review of the literature. Head Neck Pathol. 2015;9:181–95. doi: 10.1007/s12105-014-0560-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peraza AJ, Wright J, Gómez R. Canalicular adenoma: A systematic review. J Craniomaxillofac Surg. 2017;45:1754–8. doi: 10.1016/j.jcms.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 4.Rousseau A, Mock D, Dover DG, Jordan RC. Multiple canalicular adenomas: A case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:346–50. doi: 10.1016/s1079-2104(99)70221-0. [DOI] [PubMed] [Google Scholar]
- 5.Queiroz LM, da Silveira EJ, Silva Arruda Mde L, Ramos CC. A rare salivary gland neoplasm: Multiple canalicular adenoma; A case report. Auris Nasus Larynx. 2004;31:189–93. doi: 10.1016/j.anl.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 6.Suarez P, Hammond HL, Luna MA, Stimson PG. Palatal canalicular adenoma: Report of 12 cases and review of the literature. Ann Diagn Pathol. 1998;2:224–8. doi: 10.1016/s1092-9134(98)80011-7. [DOI] [PubMed] [Google Scholar]
- 7.Nelson JF, Jacoway JR. Monomorphic adenoma (canalicular type). Report of 29 cases. Cancer. 1973;31:1511–3. doi: 10.1002/1097-0142(197306)31:6<1511::aid-cncr2820310630>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 8.Machado de Sousa SO, Soares de Araújo N, Corrêa L, Pires Soubhia AM, Cavalcanti de Araújo V. Immunohistochemical aspects of basal cell adenoma and canalicular adenoma of salivary glands. Oral Oncol. 2001;37:365–8. doi: 10.1016/s1368-8375(00)00086-5. [DOI] [PubMed] [Google Scholar]
- 9.Bhaskar SN, Weinmann JP. Tumors of the minor salivary glands; a study of twenty-three cases. Oral Surg Oral Med Oral Pathol. 1955;8:1278–97. doi: 10.1016/0030-4220(55)90433-3. [DOI] [PubMed] [Google Scholar]
- 10.Samar ME, Avila RE, Fonseca IB, Anderson W, Fonseca GM, Cantín M. Multifocal canalicular adenoma of the minor labial salivary glands. Int J Clin Exp Pathol. 2014;7:8205–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Thackray AC, Sobin LH. Histological Typing of Salivary Gland Tumours. Geneva: World Health Organization; 1972. [Google Scholar]
- 12.Daley TD, Gardner DG, Smout MS. Canalicular adenoma: Not a basal cell adenoma. Oral Surg Oral Med Oral Pathol. 1984;57:181–8. doi: 10.1016/0030-4220(84)90209-3. [DOI] [PubMed] [Google Scholar]
- 13.Liess BD, Lane RV, Frazier S, Zitsch RP., 3rd Bilateral canalicular adenoma of the parotid gland. Arch Otolaryngol Head Neck Surg. 2006;132:339–41. doi: 10.1001/archotol.132.3.339. [DOI] [PubMed] [Google Scholar]
- 14.Ray M, Sathe P, Ghodke R, Suryavanshi M. Canalicular adenoma arising from the nasal septum in a child: First case report. Indian J Pathol Microbiol. 2018;61:632–4. doi: 10.4103/IJPM.IJPM_137_18. [DOI] [PubMed] [Google Scholar]
- 15.Levin F, Mirani N, Liegner JT, Langer PD. Canalicular adenoma of the lacrimal gland. Investig Ophthalmol Visual Sci. 2007;48:3590. [Google Scholar]
- 16.Yüce S, Uysal IÖ, Dogan M, Ersin T, Müderris S. Canalicular adenoma of the palate. J Craniofac Surg. 2012;23:e396–8. doi: 10.1097/SCS.0b013e31825ab388. [DOI] [PubMed] [Google Scholar]
- 17.Dayisoylu EH, Pampu AA, Mungan S, Taskesen F. Intra-mandibular canalicular adenoma: Report of a rare case. J Pak Med Assoc. 2012;62:1239–41. [PubMed] [Google Scholar]
- 18.Ansari MH. Salivary gland tumors in an Iranian population: A retrospective study of 130 cases. J Oral Maxillofac Surg. 2007;65:2187–94. doi: 10.1016/j.joms.2006.11.025. [DOI] [PubMed] [Google Scholar]
- 19.Kim D, Paeng J, Lee S, Choi S. Canalicular adenoma of the parotid gland: A rare case report and review of literature. J Clin Case Rep. 2017;7(11):1041. [Google Scholar]
- 20.Matsuzaka K, Murakami S, Shimono M, Inoue T. Canalicular adenoma arising in the upper lip: Review of the pathological findings. Bull Tokyo Dent Coll. 2004;45:229–33. doi: 10.2209/tdcpublication.45.229. [DOI] [PubMed] [Google Scholar]
- 21.Pereira MC, Pereira AA, Hanemann JA. Immunohistochemical profile of canalicular adenoma of the upper lip: A case report. Med Oral Patol Oral Cir Bucal. 2007;12:E1–3. [PubMed] [Google Scholar]
- 22.Stramandinoli-Zanicotti RT, Cesa TS, Jean Della Giustina DD, Bahr JA, Schussel JL, Sassi LM. Canalicular adenoma of the minor salivary gland in the upper lip: Case report. J Oral Diagn. 2016;1:1. [Google Scholar]
- 23.Oliveira-Santos C, Freitas-Faria P, Damante JH, Consolaro A. Asymptomatic nodules of the upper lip: Report of a canalicular adenoma with immunoprofile presentation. Gerodontology. 2012;29:e1121–4. doi: 10.1111/j.1741-2358.2010.00388.x. [DOI] [PubMed] [Google Scholar]
- 24.Werder P, Altermatt HJ, Zbären P, Bornstein MM. Canalicular adenoma of a minor salivary gland on the palate: A case presentation. Quintessence Int. 2009;40:623–6. [PubMed] [Google Scholar]


