Abstract
BACKGROUND AND PURPOSE: Frontal sinus entry, orbital entry, or both may occur during pterional craniotomy for microsurgical clipping of aneurysms. We sought to determine the incidence and clinical significance of these findings on postoperative CT scans.
METHODS: Eighty-two postoperative CT scans of the head obtained from 81 patients (64 women, 17 men; age range, 25–80 years) were retrospectively reviewed over a 1-year period. These scans were reviewed independently by two blinded neuroradiologists for the presence and degree of orbit and frontal sinus entry that may have occurred during craniotomy. Clinical charts, operative notes, and discussions with the patients' neurosurgeons were reviewed to determine the clinical management and significance of these findings.
RESULTS: Of the total 82 craniotomies reviewed, 77 (94%) had been performed via the pterional approach (43 right, 34 left). Twenty-three (30%) of these 77 studies revealed some evidence of penetration into the orbit or frontal sinus (orbit=65.2% [15/23]; frontal sinus=30.4% [7/23]; both=4.4% [1/23]). Only five of 16 patients with radiographic orbital penetration had evidence of involvement of intraorbital contents (ie, thickened lateral rectus, fat herniation, intraorbital air). Chart review revealed no complication or change in management. Of the seven patients with frontal sinus entry, three had mucosal exenteration and packing with antibiotic-coated gelfoam. No delayed complications (ie, persistent fever, mucocele, cerebrospinal fluid leak, air leak, or meningitis) were identified (follow-up period, 18–29 months).
CONCLUSION: Frontal sinus or orbital entry is not uncommon after pterional craniotomy, but the incidence of immediate complications is rare.
Pterional (frontotemporal) craniotomy is the most common neurosurgical approach for microsurgical clipping of intracranial aneurysms. Typically, a 5- to 7-cm bone flap centered on the pterion is elevated, providing the neurosurgeon with excellent exposure to the anterior circle of Willis. The pterion is the anatomic junction of the frontal, parietal, temporal, and greater wing of the sphenoid bones. This approach is beneficial for access to almost all aneurysms of the anterior circulation (anterior communicating artery, ophthalmic artery, anterior choroidal artery, posterior communicating artery, internal carotid artery, and middle cerebral artery bifurcation aneurysms) as well as for some basilar artery aneurysms (1–4). Adequate exposure of the aneurysms sometimes leads to purposeful or inadvertent extension of the craniotomy into the frontal sinus or orbit or both, which are regions in close proximity to the pterional bone flap.
Neuroradiologists frequently review postoperative CT scans of the head obtained from patients who have undergone microsurgical clipping via the pterional approach. The purpose of this retrospective study is to determine the incidence and significance of craniotomy entry into the orbit or frontal sinus or both.
Methods
Ninety-one patients underwent microsurgical clipping from January 1, 1997 to December 31, 1997. We retrospectively reviewed postoperative CT scans of the head obtained from 81 of the 91 patients. Ten patients were excluded because of the inability to obtain all of the radiographic and clinical information required. The population consisted of 64 women and 17 men (age range, 25–80 years). One patient had two craniotomies within the same year. Therefore, a total of 82 postoperative CT scans were reviewed. All CT scans were performed on GE HiSpeed Advantage scanners (Milwaukee, WI) using 3-mm axial scans through the posterior fossa and 10-mm axial images to the vertex of the head. The studies were evaluated in both soft-tissue and bone windows. They were independently reviewed by two neuroradiologists for presence and degree of orbit and frontal sinus involvement. If any wall of the sinus or orbit showed discontinuity through its thickness, the case was considered positive. Disagreements were decided by a consensus reading. In addition to the review of postoperative scans, the clinical charts, operative notes, and office follow-up notes were analyzed. The range of follow-up was 18 to 29 months (mean, 22 months) measured from surgical date to the most recent office visit after the date of discharge. Follow-up evaluation relied solely on office visit notes, as head imaging was not performed after the date of hospital discharge on any patient except the subject who had a second operation. The neurosurgical staff was also consulted to clarify questions regarding operative procedure and subsequent complications. We were specifically interested in the occurrence of complications such as cerebrospinal fluid rhinorrhea, excessive orbital swelling, visual compromise, extraocular palsy, air leaks, mucoceles, chronic sinusitis, or other infection.
Results
A total of 82 postoperative CT scans of the head were reviewed. Seventy-seven or 93% of the aneurysm clippings were performed via pterional approach. Forty-three pterional craniotomies were performed on the right and 34 on the left. Five of the patients who did not have a pterional craniotomy underwent either frontal- or suboccipital-approach craniotomies. By consensus of the two reviewing neuroradiologists, 23 (30%) of the 77 pterional craniotomies demonstrated radiographic penetration into the orbit or frontal sinus. Fifteen of the 23 studies showed involvement of the orbit, whereas seven showed showed some involvement of the frontal sinus. One CT scan showed involvement of both the frontal sinus and orbit. Five of the 16 patients who demonstrated penetration into the orbit showed more extensive involvement of intraorbital contents, including a thickened lateral rectus, fat herniation, or the presence of intraorbital air (Fig 1).
fig 1.
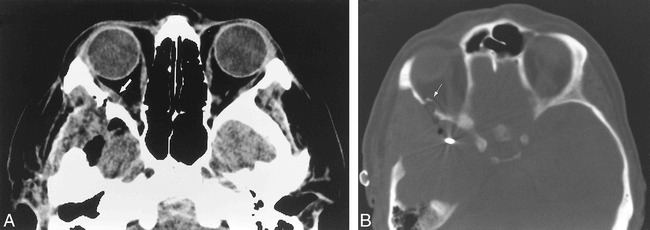
Orbital entry. A, Axial CT soft-tissue window image obtained from a 48-year-old woman with a basilar-tip aneurysm shows violation of the right lateral orbital wall (arrow).
B, The CT scan of the same patient filmed in bone windows shows displacement of the lateral orbital bone fragment (arrow), medial into the orbit.
Review of the operative notes and clinical charts revealed that one patient who demonstrated intraorbital involvement had considerable postoperative periorbital swelling, which prompted an ophthalmologic consult. The examination did not reveal any significant visual impairment or orbital injury. The periorbital swelling subsequently subsided without any sequela during the postoperative course and was normal by the time of the follow-up office visit. Orbital entry did not result in any other reported complications or change in overall postoperative management. However, three of the seven patients with frontal sinus entry did undergo mucosal exenteration and packing with antibiotic-coated gelfoam at the time of the craniotomy closure. One of these three patients also underwent placment of a vascularized pericranial graft (5). None of these patients have thus far developed complications such as mucoceles, air, or CSF leaks (6, 7).
Discussion
Frontal Sinus Entry
Neurosurgeons review preoperative CT scans to assess the osseous anatomy of patients, including the amount of pneumatization of the frontal sinus. By doing so, the neurosurgeon may be able to prepare for possible inadvertent entry into structures such as the frontal sinus. Management options for inadvertent frontal sinus entry are controversial among neurosurgeons and otorhinolarngologists. Both surgical specialties agree that if the frontal sinus is entered but the mucosa is not violated, no treatment is required. However, if the frontal sinus mucosa is violated, treatment is varied depending on the preference of the individual surgeon. During craniotomy closure, some neurosurgeons prefer total mucosal exenteration, irrigation, packing with antibiotic-soaked gelfoam, and placement of a pericranial graft over the entrance to the frontal sinus (6). Otorhinolaryngologists, on the other hand, may treat with frontal sinus cranialization or an osteoplastic frontal sinus operation with fat obliteration (8–13).
As noted previously, of the three patients treated for frontal sinus entry, two had mucosal exenteration and packing with antibiotic-soaked gelfoam, whereas the third also had pericranial graft placement (Fig 2). This last patient had postoperative fevers with positive CSF cultures for inflammation and bacteria and was treated with IV antibiotics without further complication or sequela. It is unclear whether this infection was related to the sinus entry. Frontal sinus entry with partial sinus opacification was not recognized in four patients during surgery but was seen on postoperative CT scans. Despite the lack of the usual operative precautionary treatment with antibiotic-soaked gelfoam, these patients did not develop associated complications. It is important to note, however, that our series includes a relatively short clinical follow-up period of 18 to 29 months without delayed imaging. Mucoceles or delayed CSF leaks can develop many years after surgery and long-term follow-up may be advisable in some cases (14–16).
fig 2.
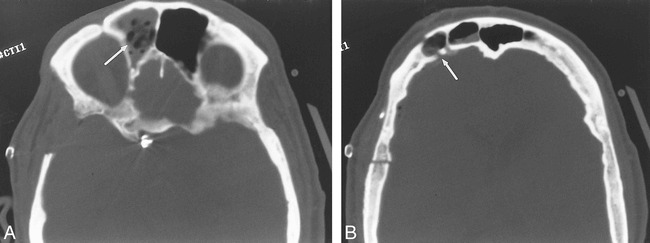
Sinus entry. A and B, These axial CT images filmed in bone windows are from a 56-year-old with an anterior communicating artery aneurysm who had extensive pneumatiztion of the frontal sinus and thick calvarium. Owing to frontal sinus entry during a right pterional craniotomy, the patient required frontal sinus mucosal exenteration with antibiotic-laden gelfoam (arrows) placed in the sinus. A pericranial graft over the entrance of the frontal sinus was also required
Orbital Entry
In our analysis of postoperative CT scans of the head obtained after pterional craniotomies, some violation of the orbital wall, especially the superolateral orbital rim, was more common than frontal sinus entry. Even though five of the 17 patients with orbital entry had radiographic evidence of extensive orbital penetration, only one patient had postoperative sequela. This patient had extensive periorbital swelling but a normal ophthalmologic examination. No treatment or intervention was required, and the swelling subsided over several days. Therefore, orbital entry usually is not a significant complication of pterional-approach craniotomies.
Possible complications related to orbital entry include orbital hematomas or damage to the extraocular muscles, affecting ocular movement. As with endoscopic sinus surgery, complications of orbital hematomas can lead to optic nerve ischemia or increase in orbital pressure or both, causing injury to the nerve and visual loss. Injury to the superior ophthalmic vein or the ophthalmic artery is rare, as the muscular capsule may serve as a relative barrier to intraconal entry.
Although no major complications were identified in our series, a prospective study with longer clinical and imaging follow-up may be useful to identify a subset of patients at increased risk of developing complications. Although clinical evaluation of patients will be most accurate in assessing long-term complications, mucoceles (with an expanded sinus) and CSF leaks (intrathecal contrast dye studies showing flow into the nose) should be easily distinguishable from the effects of mucosal exenteration.
Conclusion
Frontal sinus and orbital entry of a pterional craniotomy are common but rarely cause significant complications in patients with microsurgical clipping of aneurysms.
Footnotes
Address reprint requests to David M. Yousem, MD, Professor, Department of Radiology, Director of Neuroradiology, Johns Hopkins Hospital, 600 N Wolfe Street/Houck B-112, Baltimore, MD 21287.
References
- 1.Ojemann RG, Heros RC, Crowell RM. Surgical Management of CerebrovascularDisease. 2nd ed. Baltimore: Williams and Wilkins 1988 179-180
- 2.Day JD, Levy M, Grannotta SL. Surgery of internal carotid artery aneurysms. In: The Practice of Neurosurgery Baltimore: Williams and Wilkins 1996 2034-2036
- 3.Yasargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol 1975;3:7-14 [PubMed] [Google Scholar]
- 4.Ciric IS, Rosenblatt S. Supratentorial craniotomies. In: Apuzzo MLJ, ed. Brain Surgery: Complication Avoidance and Management New York: Churchill Livingstone 1993 60-61
- 5.Al-Mefty O, Smith RR. Combined approaches in the management of brain lesions. In: Apuzzo MLJ, ed. Brain Surgery: Complication Avoidance and Management New York: Churchill Livingstone 1993 2300
- 6.Couldwell WT, Weiss MH. Cerebrospinal fluid fistulas. In: Apuzzo MLJ, ed Brain Surgery: Complication Avoidance and Management New York: Churchill Livingstone 1993 2336-2337
- 7.Schramm VL Jr, Marron JC. Sinus complications of frontal craniotomy. Laryngoscope 1979;89:1436-1445 [DOI] [PubMed] [Google Scholar]
- 8.Hardy JM, Montgomery WW. Osteoplastic frontal sinusotomy: an anlysis of 250 patients. Ann Otol Rhinol Laryngol 1976;85:523-532 [DOI] [PubMed] [Google Scholar]
- 9.Donald PJ. Frontobasal approach for trauma and tumor. Minim Invasive Neurosurg 1994;37:37-41 [DOI] [PubMed] [Google Scholar]
- 10.Wallis A, Donald PJ. Frontal sinus fractures: a review of 72 cases. Laryngoscope 1988;98:593-598 [DOI] [PubMed] [Google Scholar]
- 11.Donald PJ. Frontal sinus ablation by cranialization. Arch Otolargngol Head Neck Surg 1982;108:142-146 [DOI] [PubMed] [Google Scholar]
- 12.Donald PJ. Recent advances in paranasal sinus surgery. Head Neck Surg 1981;4:146-153 [DOI] [PubMed] [Google Scholar]
- 13.Ballenger JJ, Snow JB Jr. Otorhinolaryngology: Head and Neck Surgery. 15th ed. Baltimore: Williams and Wilkins 1996 190-191
- 14.Kuo WR, Juan KH, Tai PY, Lin IF, et al. The mucoceles or pyoceles of the paransal sinuses. Kaohsiung Journal of Medical Sciences 1993;9:578-584 [PubMed] [Google Scholar]
- 15.Abrahamson IA Jr, Baluyot ST, Tew JM Jr, Scioville G. Frontal sinus mucocele. Ann Ophthalmol 1979;11:173-178 [PubMed] [Google Scholar]
- 16.Schuller DE, Schleuning AJ. DeWesse and Saunders' Otolaryngology Head and Neck Surgery 8th ed.. St Louis: Mosby 1994 121


