Abstract
BACKGROUND AND PURPOSE: When medication fails to improve symptoms of atherosclerotic stenosis of the intracranial vertebral and basilar arteries, percutaneous transluminal angioplasty (PTA) is considered. However, because investigators disagree on the usefulness of this procedure, we conducted a retrospective study to evaluate the indications, efficacy, and safety of PTA.
METHODS: Twenty patients underwent PTA of the vertebral (n = 14) or basilar (n = 6) artery, 18 for neurologic signs and symptoms of arterial stenosis that recurred or progressed despite pharmacotherapy and two prophylactically. Neurologic examinations were performed before and after the procedure and arterial patency was evaluated at follow-up by digital subtraction angiography and/or MR angiography. Imaging follow-up was available for 14 (70%) of the 20 patients, neurologic follow-up for 15 (75%).
RESULTS: The stenosis was successfully dilated in all patients, and on follow-up neuroradiologic examinations, vessel patency could be seen in 12 (86%) of 14 patients. Only one (7%) of 15 patients who returned for a follow-up neurologic examination had new symptoms (caused by occlusion of the vertebral artery 4 months after the procedure). One patient had a reversible neurologic deficit and one had hemiparesis after PTA. No patient died as a result of PTA.
CONCLUSION: In our study, PTA of intracranial vertebrobasilar arteries was associated with a low mortality and morbidity rate and with a high degree of patency. This technique may therefore be regarded as an effective means of improving the patency of stenotic arteries. In selective cases, it might be considered for use prophylactically.
Atherosclerotic stenosis of cranial vessels can damage brain tissue by causing either a thromboembolic territorial infarct or a hemodynamic infarct. Treatment of such a stenosis depends on its pathophysiological effects. If the stenosis results in thromboemboli, then antiplatelet aggregation, anticoagulant medication, or a combination of both is prescribed; the appropriate medication is still a matter of debate (1–6). If the stenosis causes hemodynamic abnormalities, the effects may be attenuated by treatment designed to improve the patient's cardiac output and raise blood pressure (7, 8), although this is a controversial procedure when used on a regular basis, since, in some patients, signs and symptoms of stenosis recur or progress despite medication.
Decreasing the risk of stroke in patients with stenosis of intracranial arteries is challenging. Endovascular procedures, such as percutaneous transluminal angioplasty (PTA), have been increasingly advocated when established treatments fail to relieve the effects of stenosis. In particular, PTA has been found to be effective and to be associated with low morbidity and mortality when used to treat atherosclerotic stenosis in the extracranial and anterior intracranial circulation (9, 10); however, in the posterior intracranial circulation, results of PTA performed to relieve stenosis have been conflicting (11–17). Because of these conflicting results, we conducted a retrospective study to evaluate the indications, efficacy, and safety of PTA in the intracranial vertebral and basilar arteries.
Patients and Methods
Patients
The findings in all patients who underwent PTA of intracranial vertebral or basilar arteries at our institution between 1997 and 1999 were analyzed retrospectively. All patients gave informed consent to the procedure.
A total of 20 patients (17 men and three women) were included in the study. Ages ranged from 41 to 77 years (mean age, 60 years), and risk factors for cerebral infarction included hypertension (n = 16), hyperlipidemia (n = 12), obesity (n = 1), diabetes mellitus (n = 2), smoking (n = 11), arterial occlusive disease (n = 1), and coronary heart disease (n = 5). All patients were being treated with anticoagulant or antiplatelet medication (Table 1). In 18 patients, the Barthel index was 100; for the remaining two, it was 50 (case 12) and 85 (case 13), respectively.
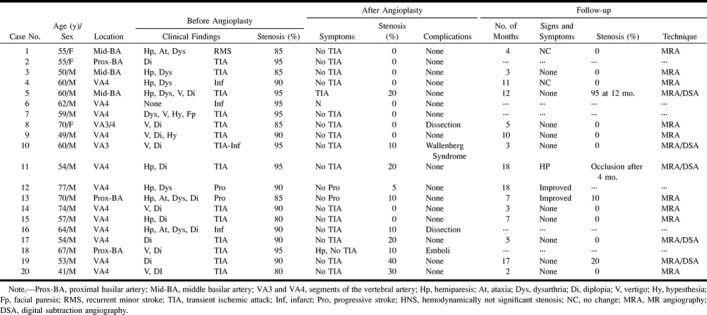
TABLE 1:
Clinical and imaging findings before and after angioplasty for intracranial artery stenosis
Indications for PTA
In general, PTA was planned to decrease the risk of new or recurrent cerebral infarction in patients with significant atherosclerotic stenosis of the intracranial vertebral or basilar arteries when 1) symptoms of stenosis recurred or progressed despite antiplatelet or anticoagulant pharmacotherapy, 2) coronary artery bypass surgery was planned, or 3) previous infarctions had occurred and collateral circulation could not be established. This spectrum of indications is represented in the following brief case descriptions.
PTA was indicated in 18 patients because symptoms of stenosis recurred or progressed despite appropriate medical therapy (warfarin: international normalized ratio [INR], 3.0–4.0; heparin: activated partial thromboplastin time [APTT], two to three times baseline). We did not administer a combination of antiplatelet and anticoagulation medication. One of the symptomatic patients, a 50-year-old man (case 3) reported recurrent sensorimotor hemiparesis of the left side, lasting each time for 10 to 15 minutes. He was admitted to the stroke unit and was treated with heparin (APTT, two to three times baseline). Although under medication, the patient experienced daily transient ischemic attacks (TIAs), beginning with perioral hypesthesia, dysarthria, and hemiparesis of the left side, which resolved when the blood pressure was raised. Neurologic examination in the interval between TIAs revealed no motor or sensory deficit. MR imaging as well as CT showed no signs of infarction or hemorrhage. Doppler sonography showed inadequate vasomotor reserve and no signals typical of emboli. Digital subtraction angiography (DSA) revealed an 85% stenosis of the basilar artery. PTA was indicated for recurrent hemodynamic TIAs despite anticoagulant medication.
Another symptomatic patient, a 70-year-old woman (case 8), reported recurrent vertigo, ataxia, and double vision over a period of 6 months. She presented after experiencing a transient dysarthria that lasted 30 minutes. Because of an earlier myocardial infarction, the patient had been on antiplatelet therapy for over 20 years. MR and CT studies showed no signs of infarction or hemorrhage. Doppler sonography and DSA revealed an 85% stenosis of the V4 segment of the left vertebral artery. The right vertebral artery was hypoplastic. PTA was recommended for recurrent TIAs despite medication.
In one of the two asymptomatic patients (case 6), MR images showed infarcts in the pons and thalamus and supratentorial white matter lesions, and angiographic studies revealed a 95% stenosis in the V4 segment of the dominant right vertebral artery and a 90% stenosis at the origin of the right vertebral artery. The left vertebral artery was hypoplastic. PTA was recommended because coronary artery bypass surgery was planned and the results of preoperative imaging studies indicated that the patient would be at high risk for cerebral infarction due to intraoperative hypotension.
The second patient without recurrent or progressive symptoms of intracranial vertebral or basilar artery stenosis (case 4) had homonymous hemianopsia as a result of previous cerebral infarction and evidence of generalized severe atherosclerosis of cerebral vessels. MR images showed a large infarct in the territory of the right middle cerebral artery and multiple white matter lesions. Intraarterial DSA showed an occlusion of the right internal carotid artery, a 30% stenosis of the left common and left internal carotid artery, a 70% stenosis of the left middle cerebral artery, a 90% stenosis of the right dominant and left hypoplastic vertebral artery (which filled mainly by the posterior inferior cerebellar artery), and two 70% stenoses of the P1 segment of the left posterior cerebral artery. As a result of these stenoses, the basilar artery was filled primarily by the right vertebral artery, and collateral circulation could not be established through the posterior communicating artery. In addition, Doppler sonography showed inadequate vasomotor reserve. PTA was recommended because the perfusion of the basilar artery was considered to be at risk and the vasomotor reserve was inadequate.
Angioplasty Technique
Before, during, and after angioplasty, patients were given heparin intravenously (APTT, two to three times baseline). All PTA procedures were performed with the patient under general anesthesia. Balloon angioplasty was performed in all cases by neuroradiologists experienced in interventional techniques, using a procedure similar to that described previously (12, 15, 17–19). In short, a 6F sheath was introduced into the femoral artery, through which a 6F guiding catheter (Cordis Envoy, Cordis Endovascular Systems, Miami Lakes, FL) was threaded so that the tip rested in the cervical portion of the vertebral artery (20). A 0.014-inch guidewire (Dasher-14, Target Therapeutics, Fremont, CA) was navigated across the stenosis to permit placement of the balloon dilatation microcatheter (Stealth, Target Therapeutics) at the site of the stenosis. The guidewire was then removed and replaced by a Stealth valve wire (Target Therapeutics). Dilatation was achieved by inflating the balloon to about 6 to 8 atm for 10 to 20 seconds. After the balloon was deflated, the result was verified and, eventually, inflation was repeated. The length of the balloon used was determined by the length and the anatomic site of the stenosis, but the balloon was always longer than the stenosis itself. The balloon was inflated to a diameter equal to or less than the diameter of the normal vessel. The sheath was removed after the procedure.
Immediately after angioplasty, each patient underwent a complete neurologic examination, after which his or her neurologic status was monitored closely for 24 hours. The Barthel index was determined before and after angioplasty. Patients in whom a good PTA result was achieved were acclimated to an antiplatelet therapy 2 weeks after the procedure; when residual stenosis remained, anticoagulant therapy was continued, with a change from heparin to warfarin (INR, 3.0–4.0).
Follow-up
Three patients (cases 2, 6, and 7) were lost to follow-up and two additional patients (cases 16 and 18) were treated recently and follow-up findings have not yet been established. In the remaining 15 cases (75%), the time between angioplasty and the last follow-up examination ranged from 2 to 18 months (mean, 8 months). All 15 patients underwent follow-up neurologic examination, 14 (70%) had follow-up MR imaging, including MR angiography, and five patients (25%) also had DSA.
Results
The percentage of stenosis of the intracranial vertebral or basilar arteries was 95% in seven patients, 90% in seven patients, 85% in four patients, and 80% in two patients. The stenosis was located in the basilar artery in six patients and in the intradural segment of the vertebral artery in 14 patients. In one patient (case 6), who underwent PTA prophylactically before coronary artery bypass surgery, stenosis in the extracranial portion of the right dominant vertebral artery was also dilated. Immediate and follow-up results of PTA in the 20 patients are summarized in Table 1.
Immediate Results of Angioplasty
Immediately after angioplasty, the vessel lumen was seen to be completely restored to normal diameter (0% stenosis) in 10 (50%) of the 20 patients or almost completely restored (up to 10% stenosis) in six (30%) of the patients (Figs 1 and 2). In four patients (20%), residual stenoses of 20% (cases 5, 11, and 17), 30% (case 20), and 40% (case 19) caused no appreciable hemodynamic alterations. A small dissection was observed angiographically in the arterial wall of one patient (case 8, Fig 3) and it was suspected at MR angiography in a second patient (case 16). In another patient (case 5), blood flow stopped after the first balloon dilatation but was restored after the second dilatation; and at the end of the procedure, no appreciable abnormality in blood flow was evident. The Barthel index of all patients but one (case 18) remained unchanged. This patient experienced a permanent neurologic deficit most probably due to emboli. His Barthel index decreased from 100 to 90. One patient (case 10) had transient (2 days) symptoms of Wallenberg syndrome.
fig 1.
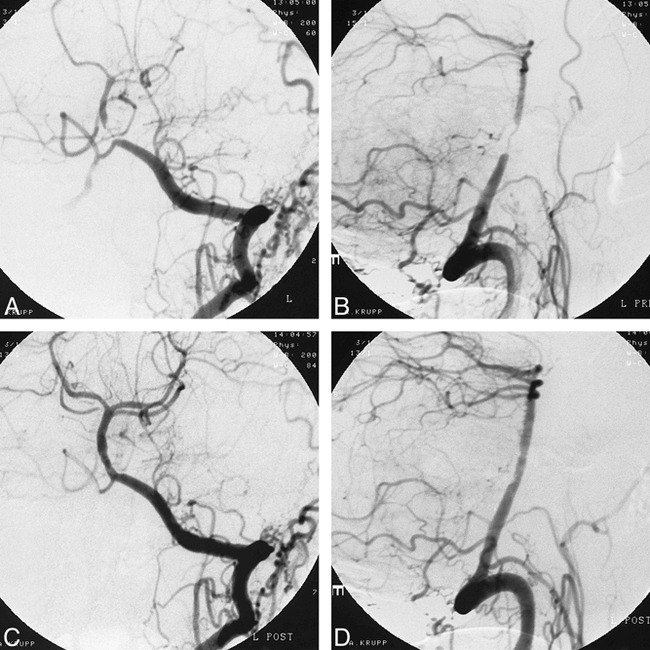
A–D, Angiographic findings in a patient (case 2) with a filiform stenosis of the proximal basilar artery before (A and B) and after (C and D) PTA. A and C, anteroposterior view; B and D, lateral view
fig 3.
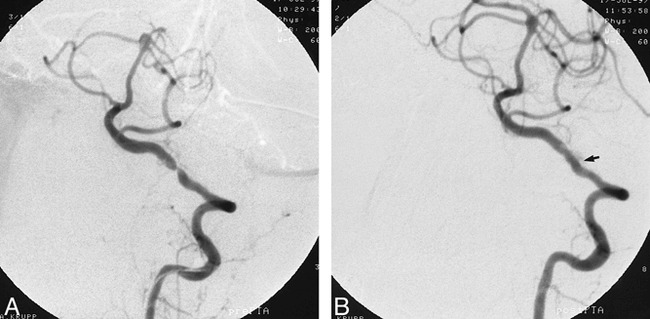
A and B, Angiographic findings in a patient (case 8) with a high-grade stenosis of the left distal vertebral artery (V4 segment). Stenosis before angioplasty (A) was completely gone immediately afterward, but a clinically asymptomatic minor dissection is evident (arrow, B)
Among the 18 patients with symptoms of stenosis, these symptoms resolved after PTA and did not recur in 17 patients (94%). In the remaining patient (case 5), symptoms (TIAs) resolved immediately after PTA and then recurred, but resolved again with warfarin therapy, which had not been effective before PTA. One of the patients (case 6) who was asymptomatic before PTA remained asymptomatic after the procedure and underwent planned bypass surgery with no neurologic sequelae. The second patient (case 4) who had no symptoms of stenosis before PTA also had no symptoms after the procedure.
Follow-up Results
Of the 14 patients who returned for follow-up neuroradiologic examinations, the patency of the treated artery remained unchanged in eight (no stenosis in seven patients and a 10% stenosis in one patient). In one patient (case 5), who had a 20% stenosis immediately after PTA, the stenosis was the same at the 2-month follow-up examination as immediately after the procedure, but at the 12-month follow-up examination the stenosis was 95%. In another patient (case 11), who had a 20% stenosis immediately after angioplasty, the vertebral artery was found to be occluded at the 4-month follow-up examination. In three patients, a 10% stenosis (case 10), 20% stenosis (case 17), and 30% stenosis (case 20) resolved completely. In the last patient, with a residual 40% stenosis (case 19), DSA 6 months after PTA showed a decrease of the stenosis to 20%. After an additional 12 months of warfarin therapy, MR angiography showed the stenosis to be unchanged at 20%, and the patient remained free of symptoms.
Of the 15 patients who underwent follow-up neurologic examinations, 10 were asymptomatic, two had improved, and two remained stable at the final examination. Specifically, the patient in whom restenosis occurred (case 5) was free of signs and symptoms of stenosis. At final follow-up, the last patient (case 11) had developed a hemiparesis associated with occlusion of the vertebral artery 4 months after angioplasty.
Discussion
Studies of the natural history of stenosis of the intracranial vertebral and basilar arteries show that this condition poses a high risk for brain stem ischemia (21). Medication is the first line of treatment, but this is problematic for patients who are already being treated medically for recurrent or progressive symptoms of stenosis. Although bypass surgery may be appropriate to treat stenotic portions of the artery in the anterior or extracranial circulation, bypass surgery for stenosis in the posterior intracranial circulation is associated with a significantly higher risk of complications (22). Our study shows that PTA is an effective and safe alternative for management of medication-refractory stenosis in the intracranial vertebrobasilar arteries.
Efficacy of Angioplasty
In our study, stenoses in the intracranial vertebrobasilar arteries were alleviated by PTA in all 20 patients (100%) and symptoms resolved after PTA in all 18 (100%) of the patients who had symptoms of stenosis before the procedure. Only one patient (5%) sustained a permanent neurologic deficit.
The affected portion of the artery was patent in 12 (86%) of our 14 patients who returned for follow-up neuroradiologic examinations between 3 and 18 months after PTA. Only one (7%) of the 15 patients who returned for follow-up neurologic evaluation had new symptoms after PTA; the other 14 patients (93%) were symptom-free or had no progression of symptoms caused by infarcts present before the procedure.
Restenosis rates in studies reported in the literature range from 0% to 25% after angioplasty of a vessel in the posterior circulation and as high as 36% after angioplasty of a vessel in the anterior circulation (15, 18). Our restenosis and occlusion rate of 14% compares well with these results. The importance of following up patients with residual stenosis is emphasized by our observation that among our five patients with 20% to 40% stenosis after PTA, the vessel occluded in one and restenosed in another (40%) (Table 1). Patients with residual stenosis should therefore be followed up noninvasively by MR angiography, which Mori et al (18) suggest be performed every 3 months.
Overall, the efficacy of PTA in our series compares favorably with results reported in the literature (Table 2), indicating that PTA is effective in both the short and longer term in patients with recurrent or progressive neurologic signs and symptoms of stenosis of intracranial vertebrobasilar arteries.
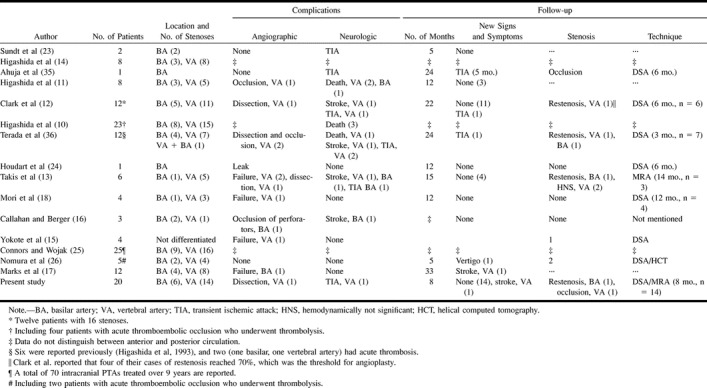
TABLE 2:
Literature review of angioplasty for atherosclerotic intracranial vertebrobasilar stenosis
Safety of Angioplasty
We found no associated mortality with the use of PTA, although one patient (5%) suffered a permanent neurologic deficit and another (5%) sustained a reversible ischemic deficit. The first reported intracranial angioplasty (of a basilar artery) was performed through surgical exposure of the extracranial vertebral artery at the base of the skull and involved resection of the arch of the atlas (23). With the development of new technology, the invasiveness of this procedure was reduced considerably, although it was still associated with a mortality rate of 37.5% (20) (Table 2). Further technological improvements resulted in a decisive decrease in mortality (10, 12, 13, 15–18, 24–26) (Table 2).
The rate of permanent neurologic deficits in larger series reported to date has ranged from 0% (17) to 33% (13) (Table 2). Our study of 20 patients represents one of the largest reported series of patients undergoing angioplasty for chronic atherosclerotic stenosis in the posterior circulation accompanied by a very low rate (5%) of permanent neurologic complications. In terms of mortality and morbidity, therefore, our results compare favorably with those reported by other investigators (Table 2).
Recently, several reports have been published concerning the successful deployment of stents for atherosclerotic disease in the intracranial internal carotid artery or in the intradural vertebral artery (27–31). Although the role, safety, and efficacy of intracranial stent placement have yet to be evaluated, the availability of this technique will make it an important adjunct in the treatment of intracranial atherosclerotic stenosis (31). In particular, the possibility of treating PTA-related dissections (although asymptomatic in our series) might prove to be significant in further reducing the morbidity of this procedure (32).
Indications for Angioplasty
The medical treatment of symptomatic intracranial stenosis has not been established definitively. Although antiplatelet therapy offers only moderate protection (5), it is often regarded as the first treatment choice. Warfarin has been shown to be significantly more effective than aspirin (4); however, in one study, it was found to be associated with a significantly higher rate of intracerebral bleeding (2). A recent analysis revealed that patients with cerebral ischemia from presumed arterial origin treated with anticoagulation had a 19-fold higher risk of intracranial hemorrhage than did treated patients with atrial fibrillation (33). Although patients with acute stroke seemed to benefit from a combined antiplatelet and anticoagulation regimen (34), a combination of low-intensity, fixed-dose warfarin and aspirin was inferior to an adjusted dose of warfarin in patients with atrial fibrillation (1). An ongoing study comparing the efficacy of low-dose anticoagulation plus acetylsalicylic acid/dipyridamole therapy with acetylsalicylic acid therapy alone might help improve the therapeutic outlook for patients with cerebral ischemia of arterial origin (3).
In previous reports, patients selected for angioplasty had to meet two criteria: they had to have recurrent or progressive neurologic symptoms despite appropriate medical therapy and these symptoms had to be related to an atherosclerotic stenosis of at least 60% to 70% (10–13, 15, 17, 18, 23, 35, 36). Although 18 of our patients met these criteria, we believed that PTA was indicated in two additional patients with asymptomatic stenosis in intracranial vertebrobasilar arteries.
The first patient with asymptomatic stenosis in whom we performed PTA had previously suffered an infarction in the territory of the basilar artery and was scheduled to undergo coronary artery bypass surgery. Although he was neurologically stable, stenosis in the intracranial or extracranial circulation in combination with intraoperative hypotension presented an important risk for stroke. Therefore, when the results of routine preoperative Doppler sonography and DSA showed stenosis of the vertebral artery, we decided that, considering the low morbidity of PTA in our series, the risk of angioplasty in this case was outweighed by the risk of stroke from bypass surgery without angioplasty. Angioplasty was thus performed prophylactically in this patient. In the second patient in our series who underwent PTA prophylactically for asymptomatic stenosis in the vertebrobasilar circulation, the basilar artery was filled by a single vertebral artery with a high-grade stenosis. Because this patient's anterior circulation had no vasomotor reserve and because the anterior circulation could not fill the posterior circulation, no collateral circulation could be produced to compensate for basilar artery insufficiency. Angioplasty was therefore performed as prophylaxis against stroke in this patient as well. In both of these patients with asymptomatic stenosis of the intracranial vertebrobasilar circulation, prophylactic PTA seemed justified because of the high risk of stroke and the low rate of complications of PTA in our series and in those reported by others (12).
Conclusion
PTA of the posterior intracranial circulation can be performed with a low complication rate and a high patency rate. The results in our series are in line with those of the recent literature. Taken together, they help establish this method as an additional treatment option for patients with intracranial atherosclerotic stenosis. Nevertheless, precise indications must still be determined and can only be assessed in a prospective study. The treatment of asymptomatic patients goes beyond the current indications and could be regarded as an option in individual and complex cases. Currently, though, PTA cannot generally be considered as a viable treatment choice in asymptomatic patients with intracranial vertebrobasilar stenoses.
fig 2.
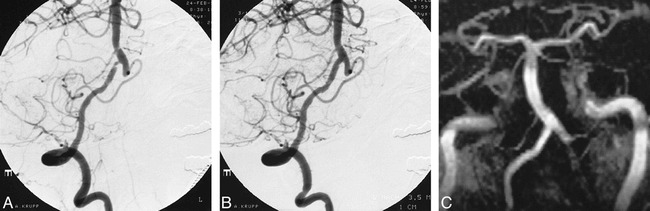
A–C, Angiographic findings in a patient (case 9) with a high-grade stenosis of the distal vertebral artery (V4 segment). Stenosis evident before PTA (A) was completely resolved immediately afterward (B); follow-up MR angiogram (C) showed no restenosis
Acknowledgments
We thank U. D. Schmid, Neurosurgical Unit, Klinik Im Park, CH-8027 Zürich, Switzerland, G. Hamann, Department of Neurology, and H. Brückmann, Department of Neuroradiology, Klinikum Grosshadern, Ludwig-Maximilians-Universität, Munich, for revising the manuscript. We thank Diana Bosse Mathis for editing the manuscript.
Footnotes
Presented at the annual meeting of the American Society of Neuroradiology, San Diego, May 1999.
Address reprint requests to Priv.-Doz. Dr. med. Tarek A. Yousry, Department of Neuroradiology, Klinikum Grosshadern, Marchioninistr. 15, D-81377 Munich, Germany.
References
- 1. Stroke Prevention in Atrial Fibrillation Investigators. Adjusted-dose warfarin versus low-intensity, fixed dose warfarin plus aspirin for high-risk patients with atrial fibrillation: stroke prevention in atrial fibrillation III randomised clinical trial. Lancet 1996;348:633-638 [PubMed] [Google Scholar]
- 2. The Stroke Prevention in Reversible Ischemia Trial (SPIRIT) Study Group. A randomized trial of anticoagulants versus aspirin after cerebral ischemia of presumed arterial origin. Ann Neurol 1997;42:857-865 [DOI] [PubMed] [Google Scholar]
- 3.Gorter JW, De Schryver EL, Algra A. Secondary prevention after ischemic cerebral infarct, the ESPRIT study: low dose anticoagulation, combined therapy with acetylsalicylic acid/dipyridamole or monotherapy with acetylsalicylic acid? Nervenarzt 1999;70:368-370 [DOI] [PubMed] [Google Scholar]
- 4.Chimowitz MI, Kokkinos J, Strong J, et al. The warfarin-aspirin symptomatic intracranial disease study. Neurology 1995;45:1488-1493 [DOI] [PubMed] [Google Scholar]
- 5.Algra A, van Gijn J. Aspirin at any dose above 30 mg offers only modest protection after cerebral ischemia. J Neurol Neurosurg Psychiatry 1996;60:197-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. The Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Study Group. Prognosis of patients with symptomatic vertebral or basilar artery stenosis. Stroke 1998;29:1389-1392 [DOI] [PubMed] [Google Scholar]
- 7.Kwiatkowski TG, Libman RB. Emergency strategies. In: Welch KMA, Caplan LR, Reis DJ, Siesjö BK, Weir B, eds. Primer on Cerebrovascular Diseases. San Diego: Academic Press 1997;671-675
- 8.Helgason CM. Mechanisms of antiplatelet agents and the prevention of stroke. In: Welch KMA, Caplan LR, Reis DJ, Siesjö BK, Weir B, eds. Primer on Cerebrovascular Diseases. San Diego: Academic Press 1997;712-716
- 9.Brückmann H, Ringelstein EB, H. B Zeumer H. Percutaneous transluminal angioplasty of the vertebral artery: a therapeutic alternative to operative reconstruction of proximal vertebral artery stenoses. J Neurol 1986;233:336-339 [DOI] [PubMed] [Google Scholar]
- 10.Higashida RT, Tsai FY, Halbach VV, Dowd CF, Hieshima GB. Transluminal angioplasty, thrombolysis, and stenting for extracranial and intracranial cerebral vascular disease. J Intervent Cardiol 1996;9:245-255 [Google Scholar]
- 11.Higashida RT, Tsai FY, Halbach VV, et al. Transluminal angioplasty for atherosclerotic disease of the vertebral and basilar arteries. J Neurosurg 1993;78:192-198 [DOI] [PubMed] [Google Scholar]
- 12.Clark WM, Barnwell SL, Nesbit G, O'Neill OR, Wynn ML, Coull BM. Safety and efficacy of percutaneous transluminal angioplasty for intracranial atherosclerotic stenosis. Stroke 1995;26:1200-1204 [DOI] [PubMed] [Google Scholar]
- 13.Takis C, Kwan ES, Pessin MS, Jacobs DH, Caplan LR. Intracranial angioplasty: experience and complications. AJNR Am J Neuroradiol 1997;18:1661-1668 [PMC free article] [PubMed] [Google Scholar]
- 14.Higashida RT, Hieshima GB, Halbach VV. Advances in the treatment of complex cerebrovascular disorders by interventional neurovascular techniques. Circulation 1991;83: (Suppl I) 196-206 [PubMed] [Google Scholar]
- 15.Yokote H, Terada T, Ryujin K, et al. Percutaneous transluminal angioplasty for intracranial arteriosclerotic lesions. Neuroradiology 1998;40:590-596 [DOI] [PubMed] [Google Scholar]
- 16.Callahan ASI, Berger BL. Balloon angioplasty of intracranial arteries for stroke prevention. J Neuroimaging 1997;7:232-235 [DOI] [PubMed] [Google Scholar]
- 17.Marks MP, Marcellus M, Norbash AM, Steinberg GK, Tong D, Albers GW. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke 1999;30:1065-1069 [DOI] [PubMed] [Google Scholar]
- 18.Mori T, Mori K, Fukuoka M, Arisawa M, Honda S. Percutaneous transluminal cerebral angioplasty: serial angiographic follow-up after successful dilatation. Neuroradiology 1997;39:111-116 [DOI] [PubMed] [Google Scholar]
- 19.Higashida RT, Tsai FY, Halbach VV, Barnwell SL, Dowd CF, Hieshima GB. Interventional neurovascular techniques in the treatment of stroke: state-of-the-art therapy. J Intern Med 1995;237:105-115 [DOI] [PubMed] [Google Scholar]
- 20.Higashida RT, Tsai FY, Halbach VV, Dowd CF, Hieshima GB. Cerebral percutaneous transluminal angioplasty. Heart Dis Stroke 1993;2:497-502 [PubMed] [Google Scholar]
- 21.Akins PT, K PT, Cross DT, Moran CJ. Natural history of stenosis from intracranial atherosclerosis by serial angiography. Stroke 1998;29:433-438 [DOI] [PubMed] [Google Scholar]
- 22.Hopkins LN, Budny JL. Complications of intracranial bypass for vertebrobasilar insufficiency. J Neurosurg 1989;70:207-211 [DOI] [PubMed] [Google Scholar]
- 23.Sundt TM, Smith HC, Campbell JK, Vliestra RE, Cucchiera RF, Stanson AW. Transluminal angioplasty for basilar artery stenosis. Mayo Clin Proc 1980;55:673-680 [PubMed] [Google Scholar]
- 24.Houdart E, Ricolfi F, Brugières P, Antoine JC, Gaston A. Percutaneous transluminal angioplasty of atherosclerotic basilar artery stenosis. Neuroradiology 1996;38:383-385 [DOI] [PubMed] [Google Scholar]
- 25.Connors III JJ, Wojak JC. Percutaneous transluminal angioplasty for intracranial atherosclerotic lesions: evolution of technique and short-term results. J Neurosurg 1999;91:415-423 [DOI] [PubMed] [Google Scholar]
- 26.Nomura M, Hashimoto N, Nishi S, Akiyama Y. Percutaneous transluminal angioplasty for intracranial vertebral and/or basilar artery stenosis. Clin Radiol 1999;54:521-527 [DOI] [PubMed] [Google Scholar]
- 27.Morris PP, Martin EM, Regan J, Braden G. Intracranial deployment of coronary stents for symptomatic atherosclerotic disease. AJNR Am J Neuroradiol 1999;20:1688-1694 [PMC free article] [PubMed] [Google Scholar]
- 28.Feldman RL, Trigg L, Gaudier J, Galat J. Use of coronary Palmaz-Schatz stent in the percutaneous treatment of an intracranial carotid artery stenosis. Cathet Cardiovasc Diagn 1996;84:883-887 [DOI] [PubMed] [Google Scholar]
- 29.Al-Mubarak N, Gomez CR, Vitek JJ, Roubin GS. Stenting of symptomatic stenosis of the intracranial internal carotid artery. AJNR Am J Neuroradiol 1998;19:1949-1951 [PMC free article] [PubMed] [Google Scholar]
- 30.Mori T, Kazita K, Mori K. Cerebral angiography and stenting for intracranial vertebral atherosclerotic stenosis. AJNR Am J Neuroradiol 1999;20:787-789 [PMC free article] [PubMed] [Google Scholar]
- 31.Gomez CR, Misra VK, W LM, et al. Elective stenting of symptomatic basilar artery stenosis. Stroke 2000;31:95-99 [DOI] [PubMed] [Google Scholar]
- 32.Malek AM, Higashida RT, Halbach VV, Phatouros CC, Meyers PM, Dowd CF. Tandem intracranial stent deployment for treatment of an iatrogenic, flow-limiting, basilar artery dissection: technical case report. Neurosurgery 1999;45:919-924 [DOI] [PubMed] [Google Scholar]
- 33.Gorter JW, for the Stroke Prevention in Reversible Ischemia Trial (SPIRIT) and European Atrial Fibrillation Trial (EAFT) Study Groups. Major bleeding during anticoagulation after cerebral ischemia: pattern and risk factors. Neurology 1999;53:1319-1327 [DOI] [PubMed] [Google Scholar]
- 34. International Stroke Trial Collaborative Group. The international stroke trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischemic stroke. Lancet 1997;349:1569-1581 [PubMed] [Google Scholar]
- 35.Ahuja A, Guterman LR, Hopkins LN. Angioplasty for basilar artery atherosclerosis. J Neurosurg 1992;77:941-944 [DOI] [PubMed] [Google Scholar]
- 36.Terada T, Higashida RT, Halbach VV, et al. Transluminal angioplasty for arteriosclerotic disease of the distal vertebral and basilar arteries. J Neurol Neurosurg Psychiatry 1996;60:377-381 [DOI] [PMC free article] [PubMed] [Google Scholar]


