Abstract
BACKGROUND AND PURPOSE: Epiphora, or tearing due to primary acquired nasolacrimal duct obstruction (PANDO), is increasingly being treated with balloon dilatation. The cause of PANDO is unknown, but a small diameter of the bony nasolacrimal canal might be one of the etiologic factors. The purpose of this study was to determine the normal distribution of diameters of the bony canal and to ascertain whether there is an association between the diameter of the bony canal and primary nasolacrimal duct obstruction.
METHODS: Using axial CT, we measured the minimum diameter of the bony nasolacrimal canal in a control group of 50 men and 50 women and in 19 patients with PANDO.
RESULTS: The mean minimum diameter in the control group was 3.5 mm, which was smaller than expected on the basis of published data. The difference between the mean minimum diameter in men (3.70 mm) and that in women (3.35 mm) was significant. The mean minimum diameter in the patient group was 3.0 mm, which was significantly smaller than that in the control group. There was, however, considerable overlap.
CONCLUSION: A small diameter of the bony canal appears to be one of the etiologic factors in PANDO.
Epiphora due to lacrimal duct obstruction is a common ophthalmologic problem, accounting for 3% of clinic ophthalmologic visits in some series (1). Obstruction of the lacrimal drainage system can be caused by congenital abnormalities or it can be acquired in the course of life. The most common congenital abnormality is a persisting membrane at the valve of Hasner, which results in complete nasolacrimal duct obstruction. Acquired obstruction of the lacrimal drainage system develops later in life and may be caused by a secondary process, related to a recognizable causative factor, or by a primary idiopathic process. Secondary acquired lacrimal duct obstruction has many different causes (2, 3). Secondary acquired lacrimal duct obstruction in the tract of the lacrimal sac and/or nasolacrimal duct is most frequently caused by facial trauma or surgery, neoplasm, sarcoidosis, or Wegener's granulomatosis. The main causes of secondary acquired obstruction of the canaliculi include infections, skin burns, drugs for glaucoma, or chemotherapeutic agents, such as fluorouracil.
Primary acquired nasolacrimal duct obstruction (PANDO) (1) develops most commonly in the tract of the lacrimal sac and duct, but it may also extend to the canaliculi. It occurs more frequently in women (50% to 83% of cases) than in men, and mostly in patients aged 40 years or older (1, 4). The process is characterized by a gradual chronic inflammation and fibrosis along the entire length of the nasolacrimal duct, leading to increasing obstruction of the drainage system, first at sites of physiological narrowing of the lacrimal drainage system, such as the valve of Rosenmüller, the junction between the lacrimal sac and duct, or the tract of the lacrimal duct. In general, stenoses occur bilaterally and tend to develop at symmetrical locations (5), with the development of stenosis on one side lagging several years behind that of stenosis on the other side, so that many patients present with one-sided epiphora. The gradual obstruction of the drainage system may be accompanied by signs and symptoms of chronic dacryocystitis, but also complicated by acute exacerbations (1). The inflammation causes reflex hypersecretion of tears, exacerbating the epiphora. PANDO can be successfully treated with dacryocystorhinostomy, a surgical procedure during which an opening is made between the lacrimal sac and the nose proximal to the obstruction of the drainage system. Today, such obstructions are increasingly being treated with balloon dacryocystoplasty, which is generally successful, depending on appropriate patient selection (6–9), or with stent placement (10).
One of the potential etiologic factors of PANDO is a relatively small diameter of the bony canal through which the nasolacrimal duct passes (1). There is a dearth of published quantitative data on the normal diameter of the bony nasolacrimal canal and no quantitative data have been published on bony nasolacrimal canal dimensions in patients with epiphora caused by obstruction of the nasolacrimal duct system. We measured the diameter of the bony canal in 24 obstructed nasolacrimal duct systems in 19 patients with epiphora due to PANDO and in a control group of 100 adults to determine the normal distribution of diameters of the bony canal in the study population and to ascertain whether there is an association between the diameter of the bony canal and primary nasolacrimal duct obstruction.
Methods
The control group consisted of 50 men and 50 women presenting with disorders of the sinuses, nose, or epipharynx at our department between December 1997 and June 1998. Patients with epiphora were not included in the control group. The mean age of the men was 48 years (range, 20–83 years) and that of the women was 47 years (range, 17–81 years). CT was performed using axial 2-mm-thick slices, photographed on bone windows, so that the bony canal was present on several consecutive slices. The smallest diameter of the bony lacrimal canal observed on any of the slices was determined, resulting in 100 minimum diameters of the bony canal in men and 100 minimum diameters in women. The diameters were measured by two of the authors using calipers on a computer screen.
The patient group consisted of 19 adults (15 women and four men with a mean age of 58 years; range, 38–87 years) with a total of 24 obstructed nasolacrimal duct systems. These subjects were selected from a group of 200 patients with epiphora due to obstruction of the lacrimal drainage system who were treated with balloon dacryocystoplasty in our department between September 1992 and July 1997. These 200 patients were selected for balloon dacryocystoplasty by a full ophthalmologic work-up and dacryocystography. Inclusion criteria for balloon dacryocystoplasty included complete or partial obstruction of the tract of the lacrimal sac, the junction between the lacrimal sac and duct, the duct, or the valve of Hasner. Exclusion criteria included active dacryocystitis, reflex hypersecretion of tears, eyelid malformation, obstruction of the canaliculi, dysfunction of the lacrimal pump mechanism, and secondary acquired nasolacrimal duct obstruction, such as posttraumatic obstruction of the bony canal, tumor, sarcoidosis, or Wegener's granulomatosis (9). Of the 200 patients treated with balloon dacryocystoplasty, 19 patients with 24 obstructed nasolacrimal duct systems (Table 1) were selected for inclusion in the present study, because in these patients the minimum diameter of the bony lacrimal canal had been determined by CT of the lacrimal drainage system on 2-mm-thick axial bone window slices before balloon dacryocystoplasty. Dacryocystoplasty was performed on the right side in nine patients, on the left side in five patients, and on both sides in five patients. Dacryocystoplasty was performed for 10 complete obstructions, requiring recanalization of the lacrimal drainage system using a guidewire, and for 14 partial obstructions. Long-term patency after dacryocystoplasty was good (ie, no epiphora or occasional epiphora requiring dabbing less than once a day) in nine nasolacrimal duct systems and poor (ie, tearing ranging from mild epiphora, requiring drying two to four times a day, to severe epiphora, with constant tear overflow) in 15.
Patient data and results of measuring the minimum diameter of the bony lacrimal canal in 24 obstructed nasolacrimal duct systems in 19 patients treated with balloon dilatation
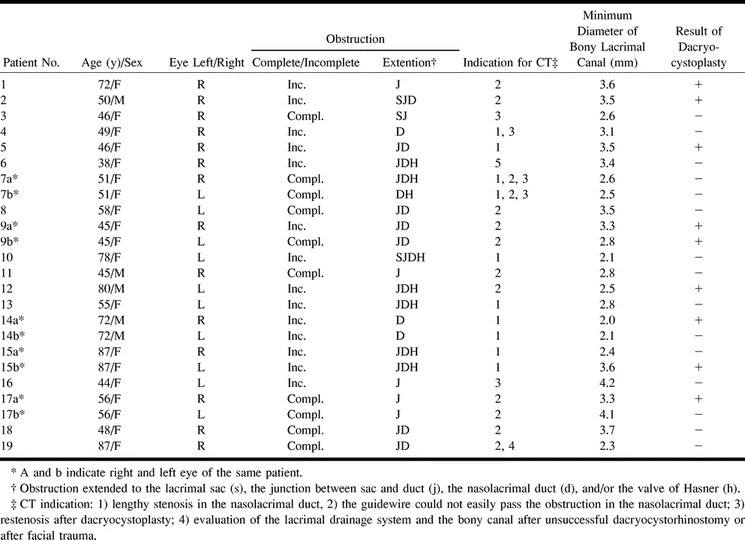
Extent of obstruction was determined by digital subtraction dacryocystography before balloon dacryocystoplasty. In the 24 obstructed nasolacrimal duct systems, we found 20 obstructions that extended to the junction between the lacrimal sac and duct, 18 that extended to the lacrimal duct, and eight that extended to the valve of Hasner (8). Proximal extension of the obstruction to the lacrimal sac was found in three cases (Table 1). Indications for CT varied (Table 1). Association between minimum diameter of the bony canal and age was determined for both the control and patient groups.
Analysis
An independent samples t-test and paired t-tests were used to determine differences between groups. A P value of less than .05 was considered to indicate a statistically significant difference.
Results
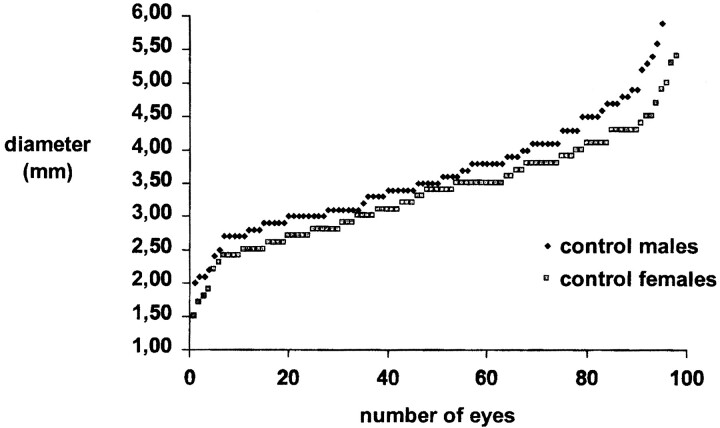
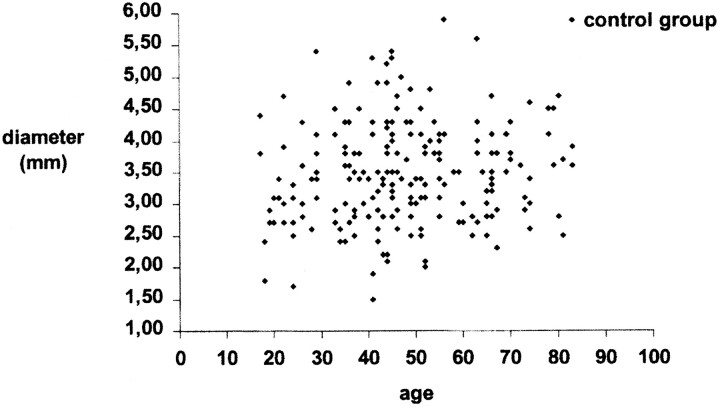
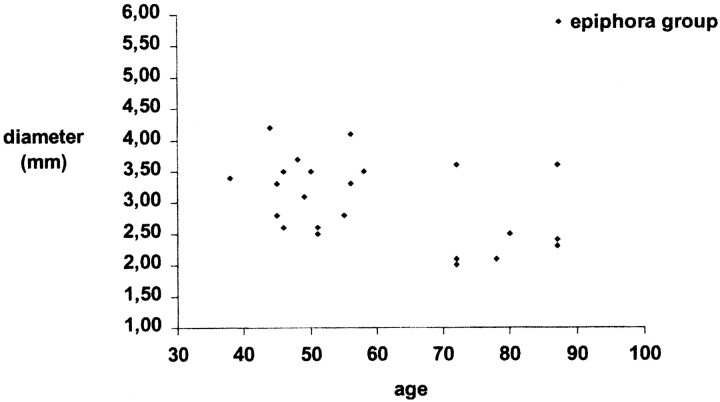
The mean minimum diameter of the bony canal in the control group was 3.5 mm (range, 1.5–6.3 mm). The mean minimum diameter of the bony canal in the 50 men was 3.7 mm (range, 2.0–6.3 mm), and in the 50 women it was 3.4 mm (range, 1.5–5.4 mm) (Fig 1). The difference between men and women in the minimum diameter of the bony canal was significant (P = .022, paired t-test). No association was found between age and diameter of the bony canal in the control group (Fig 2). In the 24 obstructed nasolacrimal duct systems in the 19 patients with epiphora treated with balloon dacryocystoplasty, the mean minimum diameter of the bony canal was 3.0 mm (range, 2.0–4.2 mm) (Table 1). The mean diameter in this group was significantly smaller than that in the control group (P = .001, paired t-test). The mean minimum diameter of the bony canal in the men with epiphora (five obstructed ducts) was 2.6 mm; among the women (19 obstructed ducts), it was 3.1 mm. In nine of the 24 obstructed nasolacrimal duct systems successfully treated with balloon dacryocystoplasty the mean minimum diameter of the bony canal was 3.1 mm, whereas it was 2.9 mm in the 15 obstructed nasolacrimal duct systems in which dacryocystoplasty was not successful. The difference was not significant (P = .4, independent samples t-test). We found an inverse association between age and diameter of the bony canal in the group with acquired obstruction of the lacrimal drainage system (ie, the older the patient, the smaller the diameter; P = .007, paired t-test) (Fig 3).
fig 1.
Graph shows the normal distribution of minimum diameters of the bony lacrimal canal (in mm) for the 50 men and 50 women (200 eyes) in the control group
fig 2.
Scatterplot shows the minimum diameter of the bony lacrimal canal versus age in the 100 subjects (200 ducts) in the control group. No correlation was found
fig 3.
Scatterplot shows the minimum diameter of the bony lacrimal canal of 24 obstructed lacrimal duct systems versus age in the 19 patients with PANDO. A negative correlation was found between age and diameter
Discussion
Some authors (1, 11) have suggested that PANDO is associated with a number of etiologic factors that reinforce one another in a vicious circle: inflammation, obstruction, and stasis. Inflammation leads to vascular congestion and edema, which cause obstruction of the drainage of tear fluid. Stasis of cellular debris and mucus in the lacrimal sac and the nasolacrimal duct can cause an increase in infection-induced changes in the walls of the lacrimal drainage system. This cycle induces gradual fibrosis and atrophy of the lacrimal drainage system. It is unclear what mechanism triggers this phenomenon. No specific bacterial cause has been established (1). Some authors think that hormone-related effects on the mucosa of the lacrimal drainage system are involved in the origin of PANDO (12). Others have suggested that the diameter of the bony canal may be a contributory factor (1, 7, 12), based on the assumption that in a narrow bony canal the circular effects may lead more easily to obstruction of the lacrimal drainage system.
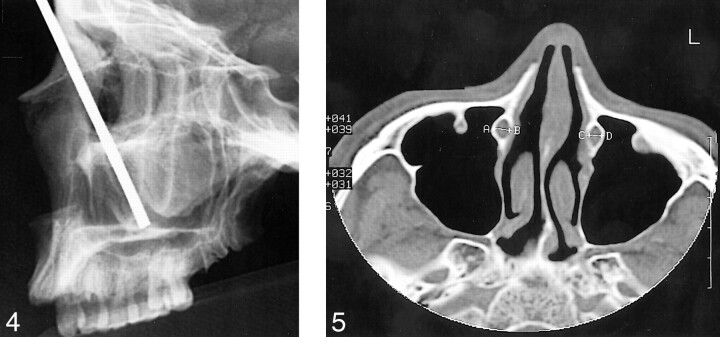
The smallest diameter of the bony canal appears to be the most relevant measure for ascertaining the origin of an obstruction of the lacrimal drainage system due to swelling of the mucosa or for choosing a balloon diameter for performing dacryocystoplasty. Errors may occur in the measurement of the smallest diameter of the bony canal on axial CT scans if the shape of the canal and the angle at which the canal and the axial plane meet are not considered. The bony lacrimal canal runs from the fossa lacrimalis in the medial corner of the eye through the maxillary bone into the nose, where it ends underneath the inferior turbinate. The high, mediodorsal part of the wall of the bony canal is formed by the lacrimal bone. The shape of the bony lacrimal canal varies from round to oval. A line through the largest diameter of an oval bony canal runs from front to back or diverges to the medial line to an imaginary point in front of the nose. The diameter of the bony canal is not the same at all levels. The smallest diameter is generally found halfway through the canal (12). The left and right bony canal usually run parallel to each other and slope at a posterior angle (15° to 25°) downward in the bony wall between the maxillary sinus and the nose (13). Figure 4 shows a lateral view of a skull with a metal bar in the bony lacrimal canal. In this case, the bony canal is at a 22.5° angle to a perpendicular line to the floor of the nose. The plane used in axial CT runs more or less parallel to the floor of the nose. When measuring the diameter of the bony canal on axial CT scans, measurement errors will occur if the anteroposterior diameter is used, because it is precisely in this direction that the projected diameter is enlarged due to the backward slope of the bony canal relative to the axial plane. The shape and slope of the bony canal allow reliable measurement of the diameter transversely, or almost transversely, provided the head is carefully positioned for CT (Fig 5).
fig 4.
Lateral skull radiograph. A metal bar in the bony lacrimal canal indicates the angle of the canal and the axial plane, which runs more or less parallel to the nasal floor. The metal bar is resting on the nasal floor.
fig 5. Axial CT scan, 2-mm-thick, of an adult male from the control group shows the bony lacrimal canals. The minimum diameter is 4.5 mm on the right side (A–B) and 3.6 mm on the left side (C–D)
Few data on the normal diameter of the bony canal have been reported in the literature. The transverse diameter is approximately 4.6 mm, according to Duke-Elder (13), who refers to anatomic observations from the early 20th century, or approximately 4.8 mm, according to Steinkogler (4), who performed measurements in epoxy resin casts of macerated skulls. The anteroposterior diameter is said to approximate 6.8 mm (4). It is striking that the mean minimum diameter of the bony canal in our control group was considerably smaller: 3.5 mm as compared with the diameters of 4.6 to 4.8 mm reported in the literature. This may be explained by the great variety of measurement methods used and possibly by a wide range in normal diameters (1.5 to 6.3 mm in our control group).
The minimum diameters of the bony canal in the men (3.70 mm) and that in the women (3.35 mm) in our group differed significantly (P = .022, paired t-test), confirming the findings of other investigators (1, 12), although they did not explicitly report the size of the diameters in women and men. The difference between men and women may be attributable to the wider midfacial structures in men as compared with that in women. In adult males, the mean intercanthal width is 33.3 mm; whereas in females it is 31.8 mm (14). It is possible that the greater prevalence of PANDO in women is due, at least in part, to the smaller diameter of the bony canal.
Groessl et al (12) analyzed the diameters of the bony canal in a group of 71 adults, although they did not mention whether this group included patients with epiphora due to an obstruction of the lacrimal drainage system. They found a positive association between the diameter of the bony canal and age in the group they studied. The older the adult, the wider the bony canal, with the association being less strong in women. These authors suggested that this observation may explain part of the difference between men and women in susceptibility to PANDO. They argued that osteoporosis, which increases with age, may account for the increased width of the bony canal, although they failed to support this assertion by densitometry or by examining whether osteoporosis does indeed cause a widening of the bony canal. In our control group, however, no association was found between age and minimum diameter of the bony canal (Fig 2). Given the well-known positive association between age and PANDO, this finding appears to be more plausible than a widening of the bony canal with increasing age. The difference between our findings and that of Groessl et al (12) may be attributed to the difference in the measurement method used. Groessl et al used the anteroposterior diameter, which cannot be reliably measured on axial CT scans. In our patient group, we found an inverse association between the patient's age and the diameter of the bony canal: the older the patient, the narrower the canal. Although this finding is consistent with an increase in lacrimal obstruction with age, it does not explain it unequivocally, as some form of selection bias cannot be ruled out.
Some authors have suggested that a narrow bony lacrimal canal predisposes one to lacrimal obstruction, whereas others have been unable to confirm the relationship between diameter of the bony canal and lacrimal obstruction (1, 4). The mean minimum diameter of the bony canal in our patients with epiphora (3.0 mm) was significantly smaller than that in the control subjects (3.5 mm) (P = .001, paired t-test). However, our group of patients with epiphora was small and heterogeneous and may not be representative of the entire group of 200 patients who underwent balloon dacryocystoplasty. Nonetheless, the diameters we found are clearly suggestive of a relationship between a narrower bony canal and obstruction of the lacrimal drainage system.
In contrast to the control group, the patient group did not show any difference between men and women in the minimum diameter of the bony canal. Although the patient group may have been too small and heterogeneous to draw any conclusions, it is interesting that this finding is not incompatible with the more frequent occurrence of lacrimal duct obstruction in women as compared with men, because the men in the control group had a larger mean diameter of the bony canal than did the women.
Although the mean diameter of the bony canal in the epiphora group (3.0 mm) was significantly smaller than that in the control group (3.5 mm), it should be noted that the range of diameters found in the control group (1.5–6.3 mm) shows complete overlap with the range found in the epiphora group (2.0–4.2 mm). This overlap indicates that a relatively small minimum diameter of the bony canal is not the sole etiologic factor in PANDO.
The relationship between the origin of obstruction of the lacrimal drainage system and the diameter of the bony canal and the fact that this diameter does not change as a result of balloon dacryocystoplasty suggests that a smaller diameter of the bony canal has a negative effect on long-term patency of the nasolacrimal duct system after balloon dacryocystoplasty. This is consistent with the findings that restenosis after balloon dacryocystoplasty occurs frequently in patients with posttraumatic strictures with bony narrowing and in those with long-distance rigid occlusion of the nasolacrimal duct system involving a relatively narrow bony canal (7, 15). Further research is needed to ascertain whether a minimum threshold value of the diameter of the bony canal can be determined below which balloon dacryocystoplasty as a treatment for lacrimal obstruction is contraindicated, rendering surgical dacryocystorhinostomy the preferred treatment. We recommend that CT be used more often in selecting patients for balloon dacryocystoplasty, such as in cases of restenosis after balloon dacryocystoplasty. Routine CT of the bony canal before balloon dacryocystoplasty does not appear to be indicated, given the high success rate of the treatment and that a comparison of patients with good versus poor patency after balloon dacryocystoplasty did not reveal any significant difference between the diameters of the bony canal in the two groups.
Conclusion
Our study produced the following results: 1) the diameter of the bony canal differed significantly between the patient group (3.0 mm) and the control group (3.5 mm) (P = .001); 2) the mean minimum diameter of the bony nasolacrimal canal in our control group (3.5 mm) was smaller than that reported in the literature; 3) in the control group, the mean minimum diameter of the bony canal in men (3.70 mm) differed significantly from that in women (3.35 mm) (P = .022); 4) no relationship between age and minimum diameter of the bony canal was observed in the control group; 5) no significant difference between men and women with respect to the minimum diameter of the bony canal was found in the patient group; 6) a significant relationship (P = .007) was found between minimum diameter of the bony canal and age in the patient group: the older the patient, the narrower the canal, although there was no conclusive explanation for this finding; and 7) the diameters of the bony canal in the control group overlapped with those in the patient group, suggesting that a small diameter of the bony canal is not the only etiologic factor in obstruction of the lacrimal drainage system.
Acknowledgments
We thank Mereke Gorsira for correcting the manuscript and Ad J. Petersen and Johan Strikwerda for their help with the photographs.
Footnotes
Address reprint requests to Alfred G. Janssen, MD, Department of Diagnostic and Interventional Radiology, De Tjongerschans Hospital, Thialfweg 44, 8441 PW Heerenveen, the Netherlands.
References
- 1.Linberg JV, Mc Cormick SA. Primary acquired nasolacrimal duct obstruction: a clinicopathologic report and biopsy technique. Ophthalmology 1986;93:1055-1063 [DOI] [PubMed] [Google Scholar]
- 2.Bartley GB. Acquired Lacrimal Drainage Obstruction: An Etiologic Classification System, Case Reports and a Review of the Literature, 3: Ophthalmic Plastic and Reconstructive Surgery.. New York: Raven Press; 1993;9:12–13 [PubMed]
- 3.Hurwitz JJ. Diseases of the sac and duct. In: Hurwitz JJ, ed. The Lacrimal System. Philadelphia: Lippincott-Raven; 1996:117–122
- 4.Steinkogler FJ. The postsaccal, idiopathic dacryostenosis: experimental and clinical aspects. Doc Ophthalmol 1986;63:269. [DOI] [PubMed] [Google Scholar]
- 5.Janssen AG. Imaging and interventional procedures for the lacrimal duct system. In: Mukherji SK, Castelijns JA, eds. Modern Head and Neck Imaging. Berlin: Springer; 1999:214
- 6.Janssen AG, Mansour Kh, Krabbe GJ, Van der Veen S, Helder AH. Dacryocystoplasty: treatment of epiphora by means of balloon dilation of the obstructed nasolacrimal duct system. Radiology 1994;193:453-456 [DOI] [PubMed] [Google Scholar]
- 7.Berkefeld J, Kirchner J, Müller HM, Fries U, Kollath J. Balloon dacryocystoplasty: indications and contraindications. Radiology 1997;205:785-790 [DOI] [PubMed] [Google Scholar]
- 8.Ilgit ET, Yüksel D, Ünal M, Akpek S, Isik S, Hasnreisoglu E. Transluminal balloon dilatation of the lacrimal drainage system for the treatment of epiphora. AJR Am J Roentgenol 1995;165:1517-1524 [DOI] [PubMed] [Google Scholar]
- 9.Janssen AG, Mansour Kh, Bos JJ. Obstructed nasolacrimal duct system in epiphora: long-term results of dacryocystoplasty by means of balloon dilation. Radiology 1997;205:791-796 [DOI] [PubMed] [Google Scholar]
- 10.Song HY, Jin YJ, Kim JH, Suh SW, Yoon HK, Kang SG, Sung KB. Nonsurgical placement of a nasolacrimal polyurethane stent: long-tern effectiveness. Radiology 1996;200:759-763 [DOI] [PubMed] [Google Scholar]
- 11.Duke-Elder S, ed. Textbook of Ophthalmology, 5: The Ocular Adnexa.. London: Kimpton; 1952:5302
- 12.Groessl SA, Sires BS, Lemke BN. An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol 1997;115:71-74 [DOI] [PubMed] [Google Scholar]
- 13.Duke-Elder S, ed. Textbook of Ophthalmology, 1: The Development, Form and Function of the Visual Apparatus.. London: Kimpton; 1946:235
- 14.Farkas LG. Anthropometry of the Head and Face.. 2nd ed. New York: Raven; 1994:272
- 15.Janssen AG. Imaging and interventional procedures for the lacrimal duct system. In: Mukherji SK, Castelijns JA, eds. Modern Head and Neck Imaging. Berlin: Springer; 1999:221