Abstract
Summary: Primary solitary amyloidoma of the spine is a disease characterized by localized deposits of amyloid. We describe and illustrate the radiologic appearance of primary solitary amyloidoma of the spine on plain radiographs, CT scans, and MR images. The imaging findings revealed features of a nonspecific soft-tissue mass with calcifications. Epidural extension of the amyloidoma caused spinal cord compression.
Primary solitary amyloidosis or amyloidoma is a disease characterized by localized deposition of amyloid in which no plasma cell dyscrasia or abnormal serum proteins are detectable (1). Only a few cases of primary amyloidoma of the spine and only two cases involving the cervical spine have been reported (2, 3). We describe a case of a primary amyloidoma of the cervical spine that caused spinal cord compression.
Case Report
A 45-year-old woman presented with paraparesis, urinary incontinence, and a 3-month history of intermittently recurring pain in the posterior portion of the neck. Physical examination revealed tenderness over the lower cervical spine at the C7 level. Sensation was decreased to pinprick from the T8 dermatome down. Motor strength was 3/5 in the left lower extremity and 2/5 to 3/5 in the right lower extremity. Results of routine blood examination and urinalysis were normal. Bence-Jones protein was not detected in repeated urinalysis. The serum immunoelectrophoresis detected no abnormal band. A bone marrow biopsy specimen showed normal cellularity with no evidence of multiple myeloma or systemic amyloidosis. Results of a rectal biopsy were normal. Plain radiography, CT, MR imaging, and a bone scan with 99mTc-methylene diphosphonate (MDP) were performed and showed an abnormal mass involving the C7 vertebra (Fig 1A-H).
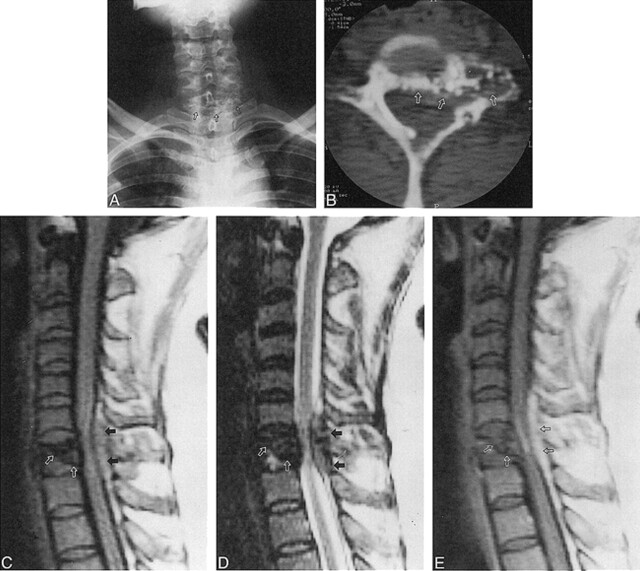
fig 1.
45-year-old woman with paraparesis, urinary incontinence, and posterior neck pain.
A, Anteroposterior radiograph of cervical spine shows osteolytic lesion with scattered calcifications (arrows) in the C7 vertebra.
B, Axial CT scan reveals osteolytic lesion with scattered calcifications involving the left lateral mass, pedicle, and anterior portion of the lamina of C7 (arrows).
C and D, Sagittal T1- (C) and T2-weighted (D) MR images show an inhomogeneous low-signal mass and a partially collapsed C7 body (white arrows), with extension to the posterior extradural space (black arrows).
E, Subtle enhancement of amyloid deposits within the partially collapsed vertebral body (white arrows) and extradural mass (black arrows) are noted on sagittal contrast-enhanced T1-weighted MR image.
A decompressive corpectomy with anterior instrumentation and fusion from C6 to T1 was performed via the anterior approach. At surgery, a friable, reddish, extradural mass was found to be compressing the dura. After the operation, the patient's paraparesis and urinary incontinence resolved completely. The biopsy specimen was positive to Congo red stain at histologic examination, with green birefringence to polarized light (Fig 1I), which is characteristic of amyloidoma. During 3 years of follow-up, the patient has reported no specific symptoms despite the presence of a residual mass at C7. A follow-up CT study after 3 years showed no growth of the residual mass (Fig 1J).
Discussion
Amyloidosis may be a systemic or localized process. It may occur spontaneously or in response to chronic disease processes. Primary amyloidosis is characterized by no detectable plasma cell dyscrasia or abnormal serum proteins; secondary amyloidosis involves systemic disease, in which the breakdown of cells is protracted (2).
Primary localized amyloid deposits in bone are unusual and any bone may be involved. Skeletal amyloid deposits often have an associated soft-tissue mass that may contain variable amounts of calcification (4). The lesions grow slowly and can produce significant local destruction of bone and soft tissue. It is this tumor-like appearance and behavior that make the diagnosis difficult to establish on imaging studies (5). Primary amyloidoma involving the spine is extremely rare, and only two cases of involvement of the cervical spine have been reported. Previous reports have described various radiologic findings of spinal amyloid lesions, such as vertebral body fractures and collapse, osteopenia, and lytic lesions. The MR signal characteristics are similar to those of primary amyloid lesions in the nasopharynx and sternum (2, 3, 6, 7) and include low-to-intermediate signal on T1-weighted images, intermediate-to-high signal on T2-weighted images, and variable enhancement on contrast-enhanced T1-weighted images.
In our case, the amyloid tumor arose in the cervical spine. The spinal amyloid deposits appeared as low signal on both T1- and T2-weighted MR images. The exact mechanism for signal hypointensity on both sequences is not entirely clear, although areas of punctate calcification within the amyloid deposit may cause signal loss on both T1- and T2-weighted images. The extradural extension of the amyloid deposits showed prominent enhancement on contrast-enhanced T1-weighted studies, possibly related to reactive inflammatory changes (3). On the basis of the plain radiographic, CT, and MR findings, the differential diagnosis included chondrosarcoma, osteogenic sarcoma, and a calcified metastatic tumor, such as mucinous adenocarcinoma of the colon. Despite its rarity and nonspecific radiologic findings, primary spinal amyloidoma should be included in the differential diagnosis of an osteolytic and calcified mass of the spine.
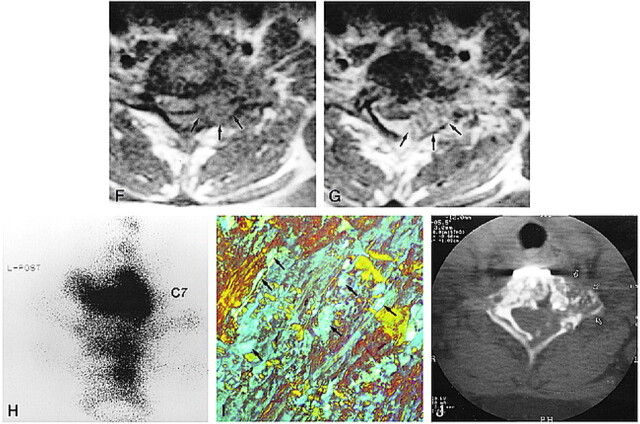
fig 1.
Continued.
F and G, Axial T1-weighted MR images show the extradural mass encircling the anterior and lateral aspect of the dural sac (arrows, F). After contrast administration (G), the enhancing mass partially compresses the spinal cord (arrows).
H, Posterior pinhole bone scintigram of cervicothoracic junction obtained with 99mTc-MDP shows increased radioactivity in C7. Minimally increased radioactivity is also noted in T1 and T2 vertebral bodies.
I, Biopsy specimen viewed with polarized light is positive for Congo red stain, showing a characteristic green or apple-green birefringence (arrows) (original magnification ×80).
J, At 3-year follow-up, CT scan shows no growth of the residual mass in C7 vertebra (arrows). The metallic instrument for fixation is noted in the anterior aspect of C7.
Footnotes
Address reprint requests to Young Ha Park, MD, Department of Radiology, St. Vincent's Hospital, The Catholic University of Korea, 93 Chi-dong, Paldal-ku, Suwon, Kyunggi-do, 442–723, Korea.
References
- 1.Bauer WH, Kuzma JF. Solitary “tumors” of atypical amyloid (paramyloid). Am J Clin Pathol 1949;19:1097-1112 [DOI] [PubMed] [Google Scholar]
- 2.Dickmam CA, Sonntag VK, Johnson P, Medina M. Amyloidoma of the cervical spine: a case report. Neurosurgery 1988;22:419-422 [DOI] [PubMed] [Google Scholar]
- 3.Meyers SP, Mullins KJ, Kazee AM. Unifocal primary amyloidoma of the spine causing compression of the cervical spinal cord: MR findings. J Comput Assist Tomogr 1996;20:592-593 [DOI] [PubMed] [Google Scholar]
- 4.Schindel S. Amyloid tumor of the larynx (case report with E.M.). Ann Otolarngol 1972;81:438-444 [DOI] [PubMed] [Google Scholar]
- 5.Pawar S, Kay C, Anderson H. Primary amyloidoma of the spine. J Comput Assist Tomogr 1982;6:1175-1177 [DOI] [PubMed] [Google Scholar]
- 6.Hegarty JL, Rao VM. Amyloidoma of the nasopharynx: CT and MR findings. AJNR Am J Neuroradiol 1993;14:215-218 [PMC free article] [PubMed] [Google Scholar]
- 7.Urban BA, Fishman EK, Humphrey RL. Primary amyloidosis of the sternum: imaging findings. Clin Imaging 1994;18:75-78 [DOI] [PubMed] [Google Scholar]