Abstract
BACKGROUND AND PURPOSE: Few studies have examined HIV-positive patients presenting with uncomplicated headache for clinical variables that might be predictive of those patients who would most benefit from CT. Because of the value of CD4 counts in predicting the relative risk of developing opportunistic infections and neoplasms, we assessed the diagnostic yield of screening CT in HIV-positive patients presenting with headache as sorted by CD4 count.
METHODS: We reviewed CT scan results and CD4 counts in patients presenting with headache uncomplicated by altered mental status, meningeal signs, neurologic findings, or symptoms of subarachnoid hemorrhage. For analysis, scans were considered positive or negative and were grouped according to CD4 counts of less than 200 cells/μL, 200 to 499 cells/μL, and equal to or greater than 500 cells/μL. The results were then analyzed using the χ2 test.
RESULTS: One hundred seventy-eight HIV-positive patients underwent a total of 204 unen-hanced and contrast-enhanced CT examinations. One hundred twenty-eight (62.7%) of the scans were negative, and 76 (37.3%) were positive. Of the positive scans, 58 (76.3%) showed atrophy only and 18 (23.7%) showed mass lesions or white matter lesions. All cases that were positive for mass lesions or white matter lesions occurred in patients with CD4 counts less than 200 cells/μL (P = .04).
CONCLUSION: A recent CD4 count provides an important predictor variable when considering performing CT in HIV-positive patients presenting with uncomplicated headache. Performing CT of the head for patients with CD4 counts equal to or greater than 200 cells/μL is of questionable value considering the low prevalence of positive CT findings. For this select group of patients, MR imaging may be more appropriate than CT. Patients with CD4 counts less than 200 cells/μL should undergo CT because of the high prevalence of positive scans.
Headache is a common complaint of HIV-positive patients that becomes more prevalent as the disease progresses (1). The evaluation of these patients poses a challenging problem, especially in the emergency department, where headache constitutes the most commonly encountered neurologically related presentation (2). Frequently, these patients undergo urgent cranial CT to exclude pathologic abnormality. Although several studies have addressed the timing and appropriateness of CT in selected groups of patients (3–9), few studies have examined HIV-positive patients presenting with headache for clinical variables that might be predictive of those patients who would most benefit from CT (10–13). Because of the value of CD4 counts in predicting the relative risk of developing opportunistic infections and neoplasms (14), we assessed the diagnostic yield of screening CT of the head in HIV-positive patients presenting with headache as sorted by CD4 count.
Methods
From October 1990 to August 1995, 548 HIV-positive patients presenting to a large tertiary hospital underwent 794 unenhanced and contrast-enhanced cranial CT examinations. From this population, 178 patients with the chief complaint of headache underwent CT and had clinical data available for review. Excluded were patients with altered mental status, meningeal signs, neurologic findings, or complaints of “worst headache of life,” suggesting acute subarachnoid hemorrhage.
The patients' medical records, imaging request histories, and infectious disease clinic records were reviewed. Each patient's most recent CD4 count at the time of imaging and CT findings were recorded. All patients were classified using the 1993 Revised Classification System of HIV Infection from the Centers for Disease Control (14). Patients, who were reported as HIV-positive before undergoing scanning, had their HIV status confirmed from medical records and hospital infectious disease clinic records.
CT was performed using a section thickness of 10 mm. Contrast material was IV administered after an initial review of the CT scans by an attending or resident radiologist. All studies that were initially read by a radiology resident were reviewed by an attending neuroradiologist. The final report issued by the attending neuroradiologist was considered to be the authoritative interpretation.
Scans were judged as yielding either negative or positive findings. Criteria for a positive scan included either intra-axial or extra-axial intracranial findings not interpreted as chronic based on either CT appearance or persistence on previous scans and extracranial pathologic findings, such as sinusitis, that could contribute to headache. For example, by these criteria, a well-defined lucency in a vascular distribution accompanied by dilation of the adjacent ventricle or cerebrospinal fluid space would be interpreted as chronic, even in the absence of a previous CT scan. Normal scans or scans with insignificant or noncontributory findings were considered negative for the purposes of this study. Positive scans were then subgrouped into the following categories: white matter hypodensity, mass lesion, pathologic meningeal enhancement, or atrophy disproportionate with patient age.
For analysis, scan results were sorted by the patients' CD4 counts into three groups. These groups were suggested in the 1993 Revised Classification System issued by the Centers for Disease Control (14) (ie, results in patients with counts of less than 200 cells/μL, 200 to 499 cells/μL, and equal to or greater than 500 cells/μL). Using interpretation options of negative versus positive findings, scan results were then analyzed using a contingency table and the χ2 test. Values of P < .05 were considered statistically significant. This study protocol was reviewed by our institutional review board and determined to be exempt from their approval process.
Results
The study population of 178 HIV-positive patients (130 male and 48 female patients) presenting with headache ranged in age from 22 to 62 years (mean age, 36.2 years). These patients underwent a total of 204 cranial CT examinations. All scanning was performed both without and with contrast enhancement. One hundred twenty-eight (62.7%) scans were interpreted as negative, whereas 76 (37.3%) were considered positive. Of the positive scans, 58 (76.3%) showed atrophy only and the remaining 18 (23.7%) showed lesions or a white matter abnormality. No cases of abnormal meningeal enhancement or significant extracranial pathologic findings, such as sinusitis, were found.
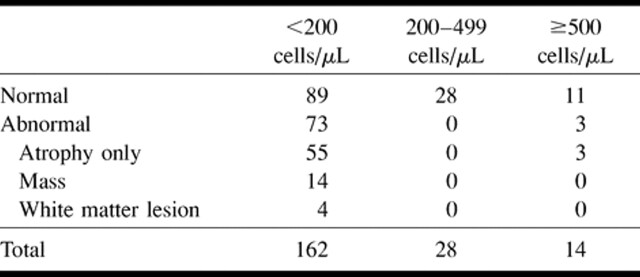
The diagnostic yield based on grouping by CD4 count is illustrated in the Table. All cases that were positive for mass lesions occurred among patients with CD4 counts less than 200 cells/μL (P = .04). Mass lesions included toxoplasmosis (13 patients) and lymphoma (one patient). The four scans showing white matter disease were obtained from patients with CD4 counts less than 200 cells/μL. Atrophy as the sole finding was also far more prevalent when the CD4 count declined to less than 200 cells/μL.
CT detectable CNS pathology based on CD4 count
Discussion
Several studies have attempted to define the prevalence of CT abnormalities in HIV-positive patients presenting with headache (10–13). Levy et al (10) characterized the imaging findings of 200 consecutive patients with AIDS with neurologic symptoms including headache and found that 40.5% of the patients had normal results of their studies, 37.5% of the patients had cerebral atrophy, and 22% of the patients had one or more focal lesions. These studies, however, failed to differentiate patients with positive neurologic signs from those with only headache.
Headache is a difficult symptom to analyze because its predictive value changes as the conditions of HIV-positive patients relapse and remit with progression and treatment of the underlying disease. Headache is usually nonspecific and may be due to a variety of causes including systemic infection, migraine, Herpes zoster, ocular pathologic abnormality, or sinusitis. Studies have even suggested that azidothymidine, the most frequently prescribed antiretroviral drug, contributes to headache in this patient group (15). Not surprisingly, the results of studies attempting to correlate headache and opportunistic pathologic abnormalities vary from 4% in outpatient volunteers to 82% of the HIV-positive population presenting to AIDS clinics (14) or emergency departments (1, 12, 13).
The revised classification system for HIV infection provides a unique opportunity to sort patients into pretest categories based on CD4 count. Reflecting the prognostic significance of the CD4 count, the Centers for Disease Control classification emphasizes both clinical (opportunistic infections and tumors) and laboratory (CD4) parameters. Under the revised system, the CD4 count plays a significant role in determining the clinical stage of HIV-positive patients.
HIV-positive patients with early disease (≥500 cells/μL) are relatively asymptomatic. Middle stage disease (200–499 cells/μL) may manifest vague symptoms, such as myalgias, headaches, arthralgias, and fatigue. Patients whose disease is in the late stage (<200 cells/μL) require extensive prophylactic therapy. Patients with early, middle, and late disease have a 5%, 20–30%, and 50–70% risk, respectively, for developing an AIDS-defining illness and dying within 18 to 24 months if they do not receive antiretroviral therapy. Patients with CD4 counts less than 50 cells/μL have a very high likelihood of dying as the result of an AIDS-related illness within 2 years (16).
For hospitals relying primarily on CT as a screening examination in the emergency department, CD4 counts provide an excellent first study before scanning. Our results clearly show that using CT in HIV-positive patients with headache, no specific neurologic signs or the worst headache of life, and CD4 counts equal to or greater than 200 cells/μL seldom yields positive findings. Seventy-six of the 204 CT scans in our study were positive. Of these 76, all except three were obtained from patients with CD4 counts less than 200 cells/μL. The three positive scans obtained from patients with CD4 counts equal to or greater than 200 cells/μL showed atrophy only. All mass lesions arose among patients with CD4 counts less than 200 cells/μL. Thirteen of the 18 positive cases were later diagnosed with toxoplasmosis. Toxoplasmosis is well known to be the most common CNS infection causing focal cerebral lesions in the HIV-positive population. One study reviewing 115 HIV-positive patients with proven toxoplasmosis revealed that 55% of these patients presented with headache. In that study, 95% of the patients had CD4 counts less than 200 cells/μL and 66% had counts less than 100 cells/μL (median CD4 count, 50 cells/μL) (17). Our findings support the necessity of brain imaging in the advanced HIV stage group having CD4 counts less than 200 cells/μL. We found no focal lesions on the CT scans of patients with CD4 counts equal to or greater than 200 cells/μL. Because of its superior sensitivity to subtle white matter and meningeal disease, MR imaging may be the preferred method for screening these selected patients.
Although several studies have suggested management strategies for HIV-positive patients presenting with headache, no studies have isolated headache as a possible predictor of disease. We observed this measure to be a powerful tool for outcome analysis in this patient population. Tso et al (2) found that, without the CD4 count for prevalence discrimination, CT prompted by complaints of headache had a statistically significant negative association with CNS lesions.
Many HIV-positive patients require lumbar puncture during their initial evaluation in the emergency department. Tso et al (2) also addressed the continuing debate regarding whether scanning is required before lumbar puncture. Baker et al (18) questioned the ability of CT to be predictive of increased intracranial pressure. Although CT may effectively screen for significant risk of herniation or disastrous neurologic consequence, the cost-effectiveness of using CT to reassure physicians further is especially doubtful within the equal to or greater than 200 CD4 count subgroup, according to our results.
Limiting CT scanning in HIV-positive patients presenting with uncomplicated headache and CD4 counts equal to or greater than 200 cells/μL may substantially reduce the number of CT examinations performed. Moreover, the CD4 count result may appropriately suggest the use of MR imaging as the initial imaging method rather than CT. One of our institutions charges $124 for a CD4 count, as compared with charges of $790, $992, and $2559 for unenhanced CT, contrast-enhanced CT, and contrast-enhanced MR imaging, respectively. The cost-effectiveness of this strategy, weighed against potential savings in imaging, is promising, especially because many clinicians are inclined to order MR imaging in the face of negative CT results.
Our data were collected before the era of highly active antiretroviral therapy. Currently, clinicians are debating whether patients should be evaluated based on their lowest attained CD4 count or their most recent CD4 count. Official recommendations for prophylaxis for opportunistic infections are still based on the nadir CD4 count; however, many clinicians are discontinuing prophylaxis for Pneumocystis carinii pneumonia when CD4 counts rise above 200 to 300 cells/μL based on very preliminary data (19). Several studies have shown a dramatic decline in all opportunistic diseases, including cerebral toxoplasmosis and CNS lymphoma. Thus, the risk to the HIV patient for developing intracranial disease is much lower once some degree of immune reconstitution has occurred with combination antiretroviral therapy (20).
Based on our results, we suggest considering the following management plan. All HIV-positive patients presenting with headache without neurologic signs should have recent CD4 counts reviewed or ordered immediately. Patients with headaches uncomplicated by focal findings and CD4 counts equal to or greater than 200 cells/μL should be managed clinically without requisite brain imaging. A patient who has a CD4 counts less than 200 cells/μL should be imaged urgently to exclude a lesion. Patients with CD4 counts equal to or greater than 200 cells/μL, and in whom a lesion is strongly suspected, may benefit from MR imaging without preliminary CT scanning.
Our study is limited in several ways. First, data from the medical records of many study participants were incomplete. In addition, the study population was largely unique to an inner city HIV-positive population. The imaging protocols reviewed often failed to completely evaluate the paranasal sinuses and orbits compared with dedicated high-resolution examinations. Although no significant extracranial pathologic abnormality was identified, detailed views may have revealed disease in many of these patients. Our hospitals tend to rely on CT as the initial screening examination in the emergency department. Because of its superior sensitivity to white matter and meningeal disease, MR imaging may have revealed significant pathologic changes among patients with CD4 counts equal to or greater than 200 cell/μL. Before the results from this study can be generalized to other HIV-positive populations, our conclusions must be further tested with both CT and MR imaging.
Conclusion
Our results suggest that a recent CD4 count provides an important predictor variable when considering performing CT of the head in HIV-positive patients presenting with headache without altered mental status, meningeal signs, or neurologic findings. Performing CT of the head among patients with CD4 counts equal to or greater than 200 cells/μL is of questionable value considering the low prevalence of positive CT findings. For this select group of patients, MR imaging may be more appropriate than CT. Patients with CD4 counts less than 200 cells/μL should undergo CT or MR imaging of the head because of the high prevalence of positive findings.
Footnotes
Presented at the Annual Meeting of the American Society of Neuroradiology, Toronto, Canada, May 15–22, 1997.
Address reprint requests to F. J. Wippold II, MD, Mallinckrodt Institute of Radiology, Washington University Medical Center, 510 South Kingshighway Boulevard, St. Louis, MO 63110.
References
- 1.Holloway RG, Kieburtz KD. Headache and the human immunodeficiency virus type I infection. Headache 1995;35:245-255 [DOI] [PubMed] [Google Scholar]
- 2.Tso EL, Todd WC, Groleau GA, Hooper FJ. Cranial computed tomography in the emergency department evaluation of HIV-infected patients with neurologic complaints. Ann Emerg Med 1993;22:1169-1176 [DOI] [PubMed] [Google Scholar]
- 3.Reinus WR, Erickson KK, Wippold FJ II. Unenhanced emergency cranial CT: optimizing patient selection with univariate and multivariate analysis. Radiology 1993;186:763-768 [DOI] [PubMed] [Google Scholar]
- 4.Reinus WR, Wippold FJ II, Erickson KK. Practical selection criteria for unenhanced cranial CT in patients with acute headache. Emerg Radiol 1994;1:81-84 [Google Scholar]
- 5.Reinus WR, Wippold FJ II, Erickson KK. Seizure patient selection for emergency computed tomography. Ann Emerg Med 1993;22:1298-1303 [DOI] [PubMed] [Google Scholar]
- 6.Mills ML, Russo LS, Ross BA. High yield criteria for urgent cranial computed tomography scans. Ann Emerg Med 1986;15:1167-1172 [DOI] [PubMed] [Google Scholar]
- 7.Grosskreutz SR, Osborn RE, Sanchez RM. Computed tomography of the brain in the evaluation of the headache patient. Mil Med 1991;156:137-140 [PubMed] [Google Scholar]
- 8.Sexton CC, Caples C. Emergency CT of the head: indications and utilization. Md Med J 1987;36:493-495 [PubMed] [Google Scholar]
- 9.Larson EB, Omenn GS, Lewis H. Diagnostic evaluation of headache: impact of computerized tomography and cost-effectiveness. JAMA 1980;243:359-362 [PubMed] [Google Scholar]
- 10.Levy RM, Rosenbloom S, Perrett R. Neuroradiologic findings in AIDS: a review of 200 cases. AJR Am J Roentgenol 1986;147:977-983 [DOI] [PubMed] [Google Scholar]
- 11.Goldstein J. Headache and acquired immunodeficiency syndrome. Neurol Clin 1990; 8:947-961 [PubMed] [Google Scholar]
- 12.Lipton RB, Feraru ER, Weiss G, et al. Headache in HIV-1 related disorders. Headache 1991;31:518-522 [DOI] [PubMed] [Google Scholar]
- 13.Singer EJ, Zorilla C, Fahy-Chandon B, Chi S, Syndulko K, Tourteliotte WW. Painful symptoms reported by ambulatory HIV-infected men in a longitudinal study. Pain 1993;54:15-19 [DOI] [PubMed] [Google Scholar]
- 14. Centers for Disease Control. 1993 Revised classification system for HIV infection and expanded surveillance case definition for AIDS among adolescents and adults. MMWR Morbid Mortal Wkly Rep CDC Surveill Summ RR-17 1992;41:1-5 [PubMed] [Google Scholar]
- 15.Richman DD, Fischl MA, Grieco MH, et al. The toxicity of azidothymidine (AZT) in the treatment of patients with AIDS and AIDS-related complex: a double-blind, placebo-controlled trial. N Engl J Med 1987;317:192-197 [DOI] [PubMed] [Google Scholar]
- 16.Broder S, Merigan TC, Bolognesi D. Textbook of AIDS Medicine. Baltimore: Williams & Wilkins; 1994:45-52 [Google Scholar]
- 17.Porter SB, Sande MA. Toxoplasmosis of the central nervous system in the acquired immunodeficiency syndrome. N Engl J Med 1992;327:1643-1648 [DOI] [PubMed] [Google Scholar]
- 18.Baker ND, Kharazi H, Laurent L, Walker AT, et al. The efficacy of routine head computed tomography (CT scan) prior to lumbar puncture in the emergency department. J Emerg Med 1994;12:597-601 [DOI] [PubMed] [Google Scholar]
- 19.Furrer H, Egger M, Opravil M, et al. Discontinuation of primary prophylaxis against Pneumocystis carinii pneumonia in HIV-1-infected adults treated with combination antiretroviral therapy: Swiss HIV cohort study. N Engl J Med 1999;340:1301-1306 [DOI] [PubMed] [Google Scholar]
- 20.Palella FJ, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med 1998;338:853-860 [DOI] [PubMed] [Google Scholar]