Abstract
Background:
The Centers for Medicare & Medicaid Services (CMS) recently instituted physician reimbursements for advance care planning (ACP) discussions with patients.
Aim:
To measure public support for similar programs.
Design:
Cross-sectional online and in-person surveys.
Setting/Participants:
English-speaking adults recruited at public parks in Philadelphia, Pennsylvania, from July to August 2013 and online through survey sampling international Web-based recruitment platform in July 2015. Participants indicated support for 6 programs designed to increase advance directive (AD) completion or ACP discussion using 5-point Likert scales. Participants also indicated how much money (US$0-US$1000) was appropriate to incentivize such behaviors, compared to smoking cessation or colonoscopy screening.
Results:
We recruited 883 participants: 503 online and 380 in-person. The status quo of no systematic approach to motivate AD completion was supported by 67.0% of participants (63.9%–70.1%). The most popular programs were paying patients to complete ADs (58.0%; 54.5%–61.2%) and requiring patients to complete ADs or declination forms for health insurance (54.1%; 50.8%–57.4%). Participants more commonly supported paying patients to complete ADs than paying physicians whose patients complete ADs (22.6%; 19.8%–25.4%) or paying physicians who document ACP discussions (19.1%; 16.5%–21.7%; both P < .001). Participants supported smaller payments for AD completion and ACP than for obtaining screening colonoscopies or stopping smoking.
Conclusions:
Americans view payments for AD completion or ACP more skeptically than for other health behaviors and prefer that such payments go to patients rather than physicians. The current CMS policy of reimbursing physicians for ACP conversations with patients was the least preferred of the programs evaluated.
Keywords: advance directive, advance care planning, incentives, end of life, public opinion, survey
Introduction
End-of-life care in the United States tends to be intensive,1–3 expensive,4 and nonresponsive to patients’ goals.5–7 To address these problems, several policies and practices have been established to motivate advance care planning (ACP), including the completion of written advance directives (ADs). Observational studies suggest that increasing rates of AD completion and ACP discussions may promote the chances that dying patients receive the care they desire.8–11 However, such behaviors remain uncommon among patients who may benefit from them, and efforts to encourage AD completion have had limited success.12
To increase the rates of ACP and completion of ADs, several US Congressmen have proposed several bipartisan bills. These include the Personalize Your Care Act of 2013,13 primarily sponsored by Representative Blumenhauer (D– Oregon); the Medicare Choices Empowerment and Protection Act,14 primarily sponsored by Senator Coburn (R – Oklahoma); and the Care Planning Act of 2015,15 primarily sponsored by Senator Warner (D – Virginia). The Coburn bill proposed an outcome-based incentive in that Medicare patients would receive financial incentives for completing an AD. The Blumenhauer and Warner bills proposed process-based incentives whereby health-care professionals would be reimbursed for documenting ACP discussions.
Although none of these bills have been passed, in November 2015, the Centers for Medicare & Medicaid Services (CMS) finalized changes to the physician fee schedule that includes new payment codes to reimburse health-care professionals for discussing ACP with patients.16 This process-based incentive targeted at health-care providers went into effect in January 2016. In this study, we examined public support for financial incentive programs like that enacted by CMS and other policies designed to encourage ACP or AD completion. Our goal was to gauge the acceptability of these policies to the public as their potential effects on patients and families remain uncertain. We explored these issues among two very different samples of Americans so as to assess the generalizability of the results.
Methods
We developed the 13-question, 10-minute survey instrument iteratively through consultation with researchers and clinicians with experience in critical care, palliative care, and medical ethics at the University of Pennsylvania. We then pilot tested a penultimate version with 22 participants during a 2-day period at a public park in Philadelphia, Pennsylvania. Survey language was modified based on participant feedback to improve clarity.
After finalizing the instrument, we recruited participants using 2 distinct strategies: distribution of in-person surveys in July and August 2013 (ie, before news of the CMS proposal), and utilization of an online survey hosted by survey sampling international (SSI) in July 2015 (ie, after news of the CMS proposal). For the in-person portion, we recruited participants from 6 public parks in Philadelphia, Pennsylvania, staggering the time and day spent at each park. Recruitment was conducted on all 7 days of the week during time blocks ranging from morning commuting hours to early evenings. For the online portion, we created a survey tool identical to the written form using Qualtrics software and employed SSI (http://www.surveysampling.com/) for survey distribution. For both surveys, we recruited English-speaking adults, age 18 or older.
Participants indicated their support using a 5-point Likert scale for 6 programs to increase ACP or completion of ADs defined in the survey as “a document that allows a person to declare his or her wishes regarding medical treatment if he or she were to become unable to speak for him or herself.” These programs include 3 incentive-based programs, 2 nonincentive-based programs, and the status quo of not systematically encouraging AD completion (Figure 1). The incentive-based programs included a completion-based incentive for patients wherein patients are financially compensated for completing an AD, a completion-based incentive for physicians, wherein physicians are financially compensated when his or her patients complete ADs, and a process-based incentive for physicians wherein physicians are financially compensated for documenting discussions of AD completion with patients. The 2 nonincentive-based programs were a forced active choice program in which patients must complete either an AD or a declination form indicating they do not wish to complete an AD as a condition of health insurance coverage and an insurance requirement in which patients must complete an AD in order to receive health insurance coverage. Finally, there was the status quo option, in which patients may complete ADs whenever they choose with no systematic incentive or guidance.
Figure 1.
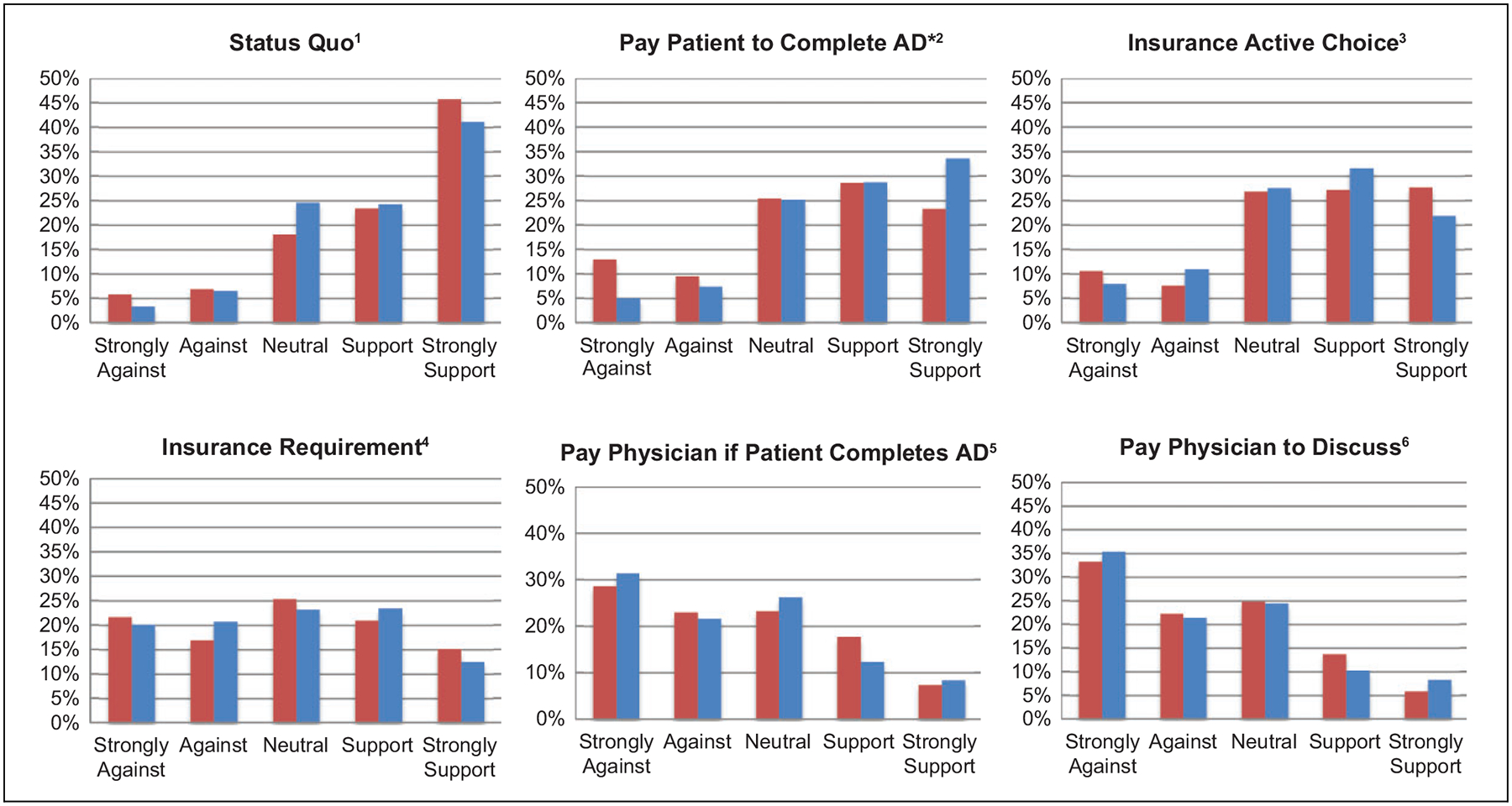
Programs, definitions, and percentage of participants that support each. AD indicates advance directive. Asterisk denotes significant differences between the in-person and online samples (P =.002). Graphs are ordered from most to least overall support across all participants, where support is defined as support or strongly support. 1 Status quo: Patients may complete ADs whenever they choose with no systematic incentive or guidance. 2 Completion-based incentive for patients: Patients are financially compensated for completing an AD. 3 Forced active choice: As a condition of health insurance converage, patients must complete either an AD or a declination form indicating they do not wish to complete an AD. 4 Insurance requirement: Patients must complete an AD in order to receive health insurance coverage. 5 Completion-based incentive for physicians: Physicians are financially compensated when his or her patients complete ADs. 6 Process-based incentive for physicians: Physicians are financially compensated for documenting discussions of AD completion with patients
We also asked participants how much money, from US$0 to US$1000, they would find appropriate to pay patients who complete ADs, pay physicians whose patients complete ADs, or pay physicians who discuss end-of-life preferences with their patients.
To provide context for interpreting these data, we also assessed how much participants would pay patients to receive screening colonoscopies when indicated and to stop smoking, as these represent other health behaviors for which incentives have been considered.17–19 Finally, we assessed participants’ proposed payments for physicians if their patients received a colonoscopy or stopped smoking. The orders in which the 6 ACP/AD programs and 7 payment amount questions were presented were each randomized to mitigate ordering effects.
We present the raw support scores for the programs graphically, and initially analyzed them using Wilcoxon sign-rank tests. We then dichotomized Likert scores as “not support” (scores of 1, 2, or 3) or “support” (scores of 4 or 5) and compared groups using McNemar’s tests. Because the results were similar, we used the binary outcome in logistic regression to identify participant characteristics that were independently associated with support for each program. We selected variables for inclusion in multivariate logistic regression based on prior hypotheses or a P < .20 in univariate analyses. Variables included due to a priori hypotheses were political ideology, religiosity, education, and income. Finally, we used Wilcoxon rank-sum tests to evaluate differences in median payments among programs. All analyses were performed using Stata 12 software (College Station, Texas).
All participants provided informed consent. In-person participants received a US$5 gift card for their participation. Online participants received the equivalent of roughly US$1 in gifts or vouchers. The institutional review board at the University of Pennsylvania approved this study. The funding organizations had no role in conducting this study.
Results
Among 553 eligible individuals that we approached for the in-person survey during 10 days in July and August 2013, 380 (68.7%) completed the questionnaires. During the online survey, among 781 individuals who started the survey during the 3 days in which it was available, 503 (64.4%) completed it.
Respondents’ characteristics are summarized in Table 1. There were several important differences between the demographics of the in-person and online samples. Members of the in-person sample were younger, had higher incomes, were more highly educated, and were more commonly nonwhite and employed full-time (all P values < .05). The online sample was more likely to identify as Christian, actively smoking, having a medical condition, and having a friend or family member with colon cancer (all P values < .05). Levels of support between the in-person and online surveys were similar for all programs to motivate AD completion or ACP except for paying patients to complete ADs, which was more popular among online participants than in-person participants (P < .002; Figure 1).
Table 1.
Participant Demographics.
| Number (%) | ||||
|---|---|---|---|---|
| Overall (n = 883) | In-person (n = 380) | Online (n = 503) | P Value | |
| Age | ||||
| 18–34 | 379 (42.9) | 204 (53.7) | 175 (34.8) | <.001 |
| 35–54 | 313 (35.4) | 116 (30.5) | 197 (39.2) | |
| 55 and older | 191 (21.6) | 60 (15.8) | 131 (26.0) | |
| Missing | 0 | 0 | 0 | |
| Gender | ||||
| Male | 447 (50.7) | 186 (49.2) | 261 (51.9) | .43 |
| Female | 434 (49.3) | 192 (50.8) | 242 (48.1) | |
| Missing | 2 | 2 | 0 | |
| Race | ||||
| White | 536 (61.7) | 175 (47.6) | 361 (71.8) | <.001 |
| Black | 216 (24.9) | 132 (35.9) | 84 (16.7) | |
| Asian | 58 (6.7) | 27 (7.3) | 31 | |
| Other | 61 (7.0) | 34 (9.2) | 27 | |
| Missing | 12 | 12 | 0 | |
| Education | ||||
| High school or less | 220 (24.9) | 101 (26.6) | 119 (22.6) | <.001 |
| College | 470 (53.2) | 159 (41.8) | 311 (61.8) | |
| Graduate School | 193 (21.9) | 120 (31.6) | 73 (14.5) | |
| Missing | 0 | 0 | 0 | |
| Full-time employment | ||||
| Yes | 441 (50.5) | 203 (54.7) | 238 (47.3) | .031 |
| No | 433 (49.5) | 168 (45.3) | 265 (52.7) | |
| Missing | 9 | 9 | 0 | |
| Household income | ||||
| $60,000 or less | 410 (47.6) | 133 (37.1) | 277 (55.1) | .021 |
| More than $60,000 | 452 (52.4) | 226 (63.0) | 226 (44.9) | |
| Missing | 21 | 21 | 0 | |
| Political ideology | ||||
| Liberal | 302 (34.5) | 145 (38.9) | 157 (31.2) | .055 |
| Moderate | 386 (44.1) | 156 (41.8) | 230 (45.7) | |
| Conservative | 188 (21.5) | 72 (19.3) | 116 (23.1) | |
| Missing | 7 | 7 | 0 | |
| Religion | ||||
| Catholic | 201 (23.5) | 72 (20.4) | 129 (25.7) | <.001 |
| Protestant | 125 (14.6) | 41 (11.6) | 84 (16.7) | |
| Other Christian | 244 (28.5) | 100 (28.3) | 144 (28.6) | |
| Jewish | 39 (4.6) | 23 (6.5) | 16 (3.2) | |
| Other faiths | 85 (9.9) | 54(15.3) | 31 (6.2) | |
| Unaffiliated | 162 (18.9) | 63 (17.9) | 99 (19.7) | |
| Missing | 27 | 27 | 0 | |
| Importance of religion in daily life | ||||
| Unimportant | 249 (28.5) | 119 (32.0) | 130 (25.8) | .115 |
| Neutral | 170 (19.4) | 72 (19.4) | 98 (19.5) | |
| Important | 456 (52.1) | 181 (48.7) | 275 (54.7) | |
| Missing | 8 | 8 | 0 | |
| Experience with AD | ||||
| Yes | 506 (59.6) | 210 (60.7) | 296 (58.8) | .60 |
| No | 343 (40.4) | 136 (39.3) | 207 (41.2) | |
| Missing | 34 | 34 | 0 | |
| Has a chronic medical condition | ||||
| Yes | 192 (21.8) | 53 (14.0) | 139 (27.6) | <.001 |
| No | 689 (78.2) | 325 (86.0) | 364 (72.4) | |
| Missing | 2 | 2 | 0 | |
| Smoker | ||||
| Yes | 211 (23.9) | 68 (17.9) | 143 (28.4) | <.001 |
| No | 672 (76.1) | 312 (82.1) | 360 (71.6) | |
| Missing | 0 | 0 | 0 | |
| Friends/family with lung cancer | ||||
| Yes | 299 (34.1) | 120 (32.2) | 179 (35.6) | .29 |
| No | 577 (65.9) | 253 (67.8) | 324 (64.4) | |
| Missing | 7 | 7 | 0 | |
| Friends/family with colon cancer | ||||
| Yes | 224 (25.4) | 78 (20.6) | 146 (29.0) | .004 |
| No | 658 (74.6) | 301 (79.4) | 357 (71.0) | |
| Missing | 1 | 1 | 0 | |
Abbreviations: AD, advance directive.
Patterns of relative support across the 6 programs for ACP discussions or AD completion were similar in the 2 samples (Figure 1). In both samples, the most commonly supported option was the status quo of not systematically encouraging AD completion or ACP (67.0%). Support for this status quo of not intervening was greater than for any of the 3 incentive programs examined (all P values < .001; Figure 1). Of the 290 participants who did not support the status quo, 197 (68.0%) did support 1 or more of the active interventions to increase ACP or AD completion. Only 93 individuals (10.5%) declined support for all options to motivate ACP or AD completion.
Among the incentive programs, support was substantially greater for paying patients to complete ADs (58.0%) than for either physician-directed incentive program (both Ps < .001). Support was also marginally but significantly greater for paying physicians when patients completed ADs (22.6%) than for paying physicians who document discussions about ACP (19.1%; P < .001). When asked how much money was appropriate to incentivize physician and patient behavior, the median proposed payments followed a similar pattern: US$100 (interquartile range [IQR]: 0–250) for paying patients to complete ADs, US$15 (IQR: 0–100) for paying physicians whose patients complete ADs, and US$5 (IQR: 0–100) for paying physicians who document ACP discussions. This same pattern was observed in both samples analyzed separately. Further, in both samples, the amounts supported for AD completion or ACP conversations were less than the amounts supported to reimburse patients or physicians for colonoscopy completion or smoking cessation (Figure 2).
Figure 2.
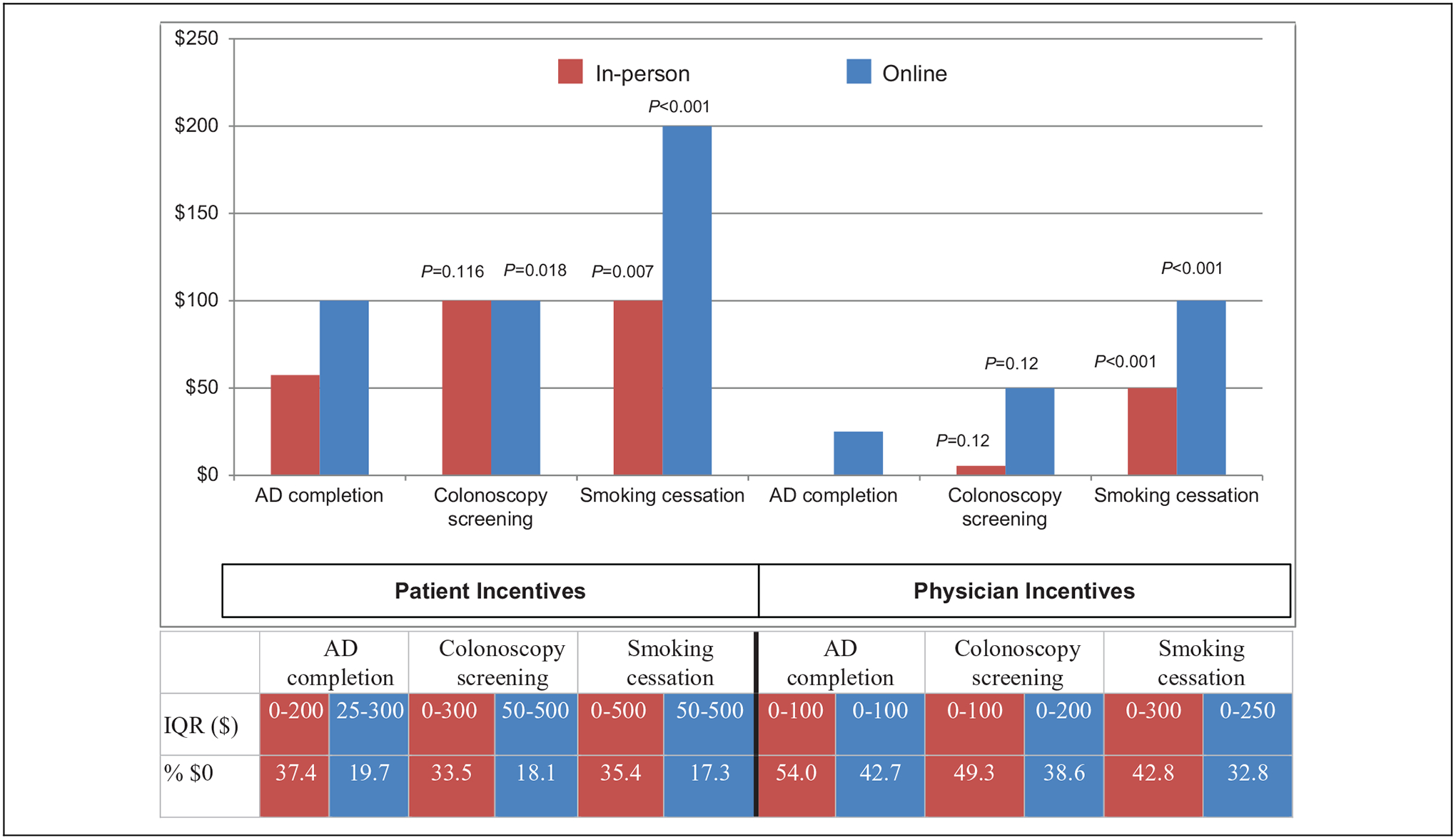
Median values, interquartile ranges, and percentage of participants selecting US$0 for financial incentives for different health behaviors. AD indicates advance directive, IQR, interquartile range; % $0, percentage of participants stating US$0 for the incentive. P values above each bar reflect Wilcoxon rank-sum comparisons of supported payments for colonoscopy screening and smoking cessation, respectively, versus AD completion for the in-person (red) and online (blue) samples.
In multivariable analyses, older participants were less likely to support completion-based incentives for patients and completion- or process-based incentives for physicians (Table 2). Participants without chronic medical conditions and blacks were more likely than participants with medical conditions and whites, respectively, to support both types of physician-targeted incentives (all P values < .05). Smokers were more likely to support all 3 incentive programs. Other participant characteristics, including gender, education, employment status, personal or family experience with an AD, importance of religion, and political ideology, were largely unrelated to support for these 3 incentive programs.
Table 2.
Logistic Regression of Relationship Between Participant Characteristics and Support for AD Completion Incentives.a
| Completion-Based Incentive for Patients | Completion-Based Incentive for Physicians | Process-Based Incentive for Physicians | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Gender | * | |||||
| Male | Reference | Reference | ||||
| Female | 0.74 (0.55–1.01) | .056 | 0.81 (0.60–1.09) | .161 | ||
| Age | ||||||
| 18–34 | Reference | Reference | Reference | |||
| 35–54 | 0.45 (0.30–0.68) | <.001 | 0.40 (0.28–0.58) | <.001 | 0.46 (0.32–0.65) | <.001 |
| 55 and older | 0.27 (0.17–0.43) | <.001 | 0.30 (0.20–0.46) | <.001 | 0.35 (0.23–0.53) | <.001 |
| Race | * | |||||
| White | Reference | Reference | ||||
| Black | 1.96 (1.31–2.92) | .001 | 2.06 (1.38–3.09) | <.001 | ||
| Other | 1.44 (0.90–2.31) | .128 | 1.42 (0.90–2.24) | .129 | ||
| Full-time employment | * | * | ||||
| Yes | Reference | |||||
| No | 1.53 (1.07–2.18) | .020 | ||||
| Education | ||||||
| High school or less | Reference | Reference | Reference | |||
| College | 1.13 (0.74–1.73) | .57 | 0.87 (0.59–1.28) | .48 | 1.06 (0.73–1.55) | .76 |
| Beyond college | 0.82 (0.49–1.37) | .45 | 0.53 (0.32–0.86) | .011 | 0.83 (0.51–1.34) | .44 |
| Political ideology | ||||||
| Moderate | Reference | Reference | Reference | |||
| Liberal | 1.60 (1.08–2.37) | .020 | 1.31 (0.92–1.87) | .137 | 1.30 (0.91–1.85) | .144 |
| Conservative | 1.46 (0.95–2.26) | .086 | 1.46 (0.99–2.14) | .056 | 1.49 (1.01–2.18) | .042 |
| Importance of religion | ||||||
| Neutral | Reference | Reference | Reference | |||
| Unimportant | 1.51 (0.94–2.43) | .085 | 0.92 (0.59–1.43) | .70 | 1.00 (0.64–1.55) | .99 |
| Important | 1.48 (0.98–2.25) | .065 | 1.09 (0.73–1.64) | .68 | 1.08 (0.72–1.61) | .72 |
| Annual Income | ||||||
| More than US$60,000 | Reference | Reference | Reference | |||
| $60,000 or less | 1.09 (0.76–1.57) | .64 | 0.81 (0.58–1.13) | .21 | 0.85 (0.62–1.18) | .34 |
| Experience with ADs | * | |||||
| Yes | Reference | Reference | ||||
| No | 1.07 (0.78–1.46) | .69 | 1.12 (0.82–1.53) | .46 | ||
| Smoker | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 2.10(1.33–3.31) | .001 | 1.85 (1.26–2.69) | .002 | 1.69 (0.38–0.82) | .002 |
| Has a medical condition | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 0.86 (0.55–1.34) | .51 | 0.68 (0.46–1.00) | .049 | 0.56 (0.39–0.82) | .009 |
| Site | ||||||
| Online | Reference | Reference | Reference | |||
| In-person | 0.35 (0.25–0.51) | <.001 | 0.55 (0.39–0.78) | .001 | 0.49 (0.35–0.70) | <.001 |
Abbreviations: AD, advance directive; CI, confidence interval; OR, odds ratio.
Variables insignificant in univariate analyses (P > .2) were omitted in multivariate analysis and are denoted as “*.”
Discussion
This study of 2 distinct and demographically heterogeneous samples yields several important findings regarding how the American public views programs designed to promote ACP, including the completion of ADs. First, we found that nearly one-third of the public explicitly does not support the status quo policy of not systematically encouraging more Americans to engage in ACP or complete ADs. Further, we found that 90% of Americans do support 1 or more programs designed to increase the rates of these behaviors.
However, views on the optimal ways to intervene are mixed. More than half of participants in this study supported using financial incentives to motivate patients to complete ADs, as previously proposed in the Coburn bill. Similar support was noted for a forced active choice intervention in which patients would be required to complete either an AD or a form declining AD completion as a condition of health insurance. By contrast, less than a quarter of Americans support paying physicians when their patients complete ADs, and even fewer support paying physicians to discuss ACP with patients—the program CMS implemented in January 2016.
Several participant characteristics were associated with support for programs that incentivize AD completion or ACP. Importantly, older participants and those who said they had a chronic medical illness were less likely to support any of the incentive programs. This could reflect greater leeriness of government intervention among people likely to be targeted by programs to motivate ACP. Alternatively, these findings could be attributable to such patients’ needs being met by the current system in which the government does not actively promote ACP, making such persons less interested in change.
We also found that smokers more uniformly supported incentive programs for ACP. Although this could reflect smokers’ recognition of the importance of planning for future ill health, given their current behaviors, another possibility is that the high levels of present bias that characterize most smokers20 make them particularly interested in incentive programs. Indeed, financial incentives have proven to be highly motivating among smokers in helping them to quit.17,19 Further research is needed to better understand these relationships.
Finally, we found that incentives for ACP and AD completion were generally less popular than incentives for screening colonoscopy or smoking cessation. Like screening colonoscopy, engaging in ACP or completing ADs often reflects a one-time commitment (at least, once within a substantial period of time). And like smoking cessation, ACP requires an unpleasant upfront activity (ie, contemplating one’s mortality) in exchange for future benefits (ie, providing guidance to clinicians and family members regarding how one wishes to be treated). Given these similarities, our findings likely reflect genuinely lower support for incentivizing ACP or AD completion, perhaps because failures to be screened or to stop smoking are more readily recognized as threats to future health and well-being.
These findings should be interpreted in the context of the study’s limitations. First, public support is not the only criterion upon which to evaluate the prudence of public policy. The CMS policy to reimburse physicians for engaging their patients in ACP discussions may prove to be wise even if it is never well liked. However, the fact that this policy was less well accepted than all other policies we evaluated suggests potential barriers that may need to be overcome to promote successful implementation.
Second, like all survey studies, it is difficult to gauge the generalizability of the findings because it is rarely possible to prove that the views of survey respondents reflect the views of nonrespondents. Some reassurance is provided by the fact that the demographic characteristics of the online respondents almost precisely mirror the characteristics of the most recent US census. More importantly, we found nearly identical results in 2 separate populations with objectively different measured demographics (and hence, presumably different unmeasured characteristics). Such replication of results among objectively different populations suggests that the results may generalize to at least a substantial fraction of Americans.
Third, the absolute levels of support we identified for intervention programs may underestimate true support because, in an effort to avoid influencing judgments, we chose not to provide participants with information regarding the utility of ACP. Such promotion of the rationale for incentive programs would likely accompany any real legislation, such that actual support for such programs may indeed prove to be greater. Nonetheless, because these nuances of how questions were posed applied to all programs, our estimates of the public’s relative support for different programs should be accurate.
In summary, this study suggests general support for efforts to engage patients in ACP, including AD completion, but varying levels of support for different ways to achieve this goal. Paying patients for AD completion or requiring them to make an active choice to complete an AD are more broadly supported than the other options we evaluated. And incentives to physicians, including the CMS policy to pay physicians for having and documenting ACP discussions, were infrequently supported. By identifying programs with greater potential for public support, these results suggest which programs might most fruitfully be tested in randomized trials among carefully selected patients to evaluate the programs’ impacts on the quality and costs of care.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Doris Duke Charitable Foundation (Dr. Auriemma), a University of Pennsylvania Center for Health Incentives and Behavioral Economics Patient Engagement and Community Outreach pilot grant (Dr. Auriemma and Dr. Halpern), and a grant from the Otto Haas Charitable Trust (Dr. Halpern). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Dr. Auriemma had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Preliminary results from this study were presented in abstract format at the Academy Health Annual Research Meeting in San Diego in May 2014.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. [DOI] [PubMed] [Google Scholar]
- 2.Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Aff. 2012;31(6): 1277–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378(9800):1408–1413. [DOI] [PubMed] [Google Scholar]
- 4.Hoover DR, Crystal S, Kumar R, Sambamoorthi U, Cantor JC. Medical expenditures during the last year of life: findings from the 1992–1996 Medicare Current Beneficiary Survey. Health Serv Res. 2002;37(6):1625–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Field MJ, Cassel CK, eds. Approaching Death: Improving Care at the End of Life. Washington, D.C.: National Academy Press; 1997. [PubMed] [Google Scholar]
- 6.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14): 1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. [DOI] [PubMed] [Google Scholar]
- 8.Silveira MJ, Kim SY, Langa KM. Advance directives and out-comes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Degenholtz HB, Rhee Y, Arnold RM. Brief communication: the relationship between having a living will and dying in place. Ann Intern Med. 2004;141(2):113–117. [DOI] [PubMed] [Google Scholar]
- 10.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc. 2007;55(2):189–194. [DOI] [PubMed] [Google Scholar]
- 11.Nicholas LH, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. 2011;306(13): 1447–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramsaroop SD, Reid MC, Adelman RD. Completing an advance directive in the primary care setting: what do we need for success? J Am Geriatr Soc. 2007;55(2):277–283. [DOI] [PubMed] [Google Scholar]
- 13.Personalize Your Care Act, H.R. 1173, 113th Cong., 1st Sess 2013.
- 14.Medicare Choices Empowerment and Protection Act, S. 2240, 113th Cong., 2nd Sess 2014.
- 15.Care Planning Act, S. 1549, 114th Cong., 1st Sess. 2015.
- 16.Centers for Medicare & Medicaid Services (US). Revisions to payment policies under the physician fee schedule and other revisions to Part B for CY 2016. Proposed Rule. Fed Regist. 2015; 80(220):41686–4966. [PubMed] [Google Scholar]
- 17.Madison KM, Volpp KG, Halpern SD. The law, policy, and ethics of employers’ use of financial incentives to improve health. J Law Med Ethics. 2011;39(3):450–468. [DOI] [PubMed] [Google Scholar]
- 18.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Eng J Med. 2009;360(7):699–709. [DOI] [PubMed] [Google Scholar]
- 19.Halpern SD, French B, Small DS, et al. Randomized trial of four financial-incentive programs for smoking cessation. N Engl J Med. 2015;372(22):2108–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mitchell SH. Measures of impulsivity in cigarette smokers and non-smokers. Psychopharmacology. 1999;146(4):455–464. [DOI] [PubMed] [Google Scholar]


