The second wave of COVID-19 has affected India substantially, with the highest number of daily reported cases being slightly more than 0·4 million on May 7, 2021, and has declined since. Even though the number of new reported cases has reduced, India still contributed to approximately 45% of the new cases detected globally and nearly 34% of the deaths globally during the third week of May, 2021.1
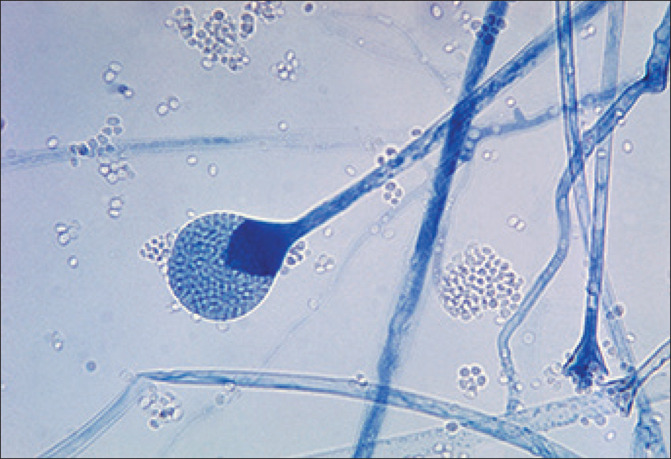
As India continues to achieve stability over the existing situation, another imminent threat has emerged as a challenge to India in the form of coronavirus disease-associated mucormycosis. Mucormycosis, caused by a group of moulds called mucormycetes, is a rare but potentially fatal infection if inadequately treated. Often referred to as the so-called black fungus, the incidence of mucormycosis has risen more rapidly during the second wave compared with the first wave of COVID-19 in India, with at least 14 872 cases as of May 28, 2021. The state of Gujarat alone contributed to the highest number of cases, with at least 3726 cases of mucormycosis in patients with active and recovered COVID-19, followed by the state of Maharashtra. Since the communication from the Health Minister of Maharashtra on May 19, 2021, there have been 90 deaths attributable to mucormycosis. Other states such as Rajasthan, Andhra Pradesh, Karnataka, Haryana, Madhya Pradesh, Uttarakhand, and Delhi have also shown a steady rise in the number of mucormycosis cases and deaths related to it; with multiple states already having declared it as an epidemic and a notifiable disease to the national health authorities.2
The Indian Council of Medical Research released guidelines for the screening, diagnosis, and management of mucormycosis in patients with COVID-19.3 The most common causes attributed to the rise of mucormycosis in COVID-19 patients are uncontrolled diabetes, the excessive use of corticosteroids for immunosuppression, and long-term stays in the intensive care unit. Even though no official figures about mucormycosis in COVID-19 cases were released by the Union Health Ministry during the first wave of COVID-19, India contributed to approximately 71% of the global cases of mucormycosis in patients with COVID-19 based on published literature from December, 2019, to the start of April, 2021.4
Various states have quickly undertaken measures to ascertain control over the situation by setting up special task forces, issuing guidelines, arranging separate wards in hospitals for the management of mucormycosis cases, and procuring the drugs required for treatment. Approximately 0·1 million vials of amphotericin B, the drug used in the medical management of mucormycosis, have already been distributed to the states from May 1, to May 14, 2021, by the Union Ministry of Health. The shortage of amphotericin B has been noticed in multiple states and measures are being undertaken for the procurement and optimal allocation of the drug by ramping up domestic production; in addition to this, different methods of importing the drug are currently being explored by the Union Ministry of Health. The Ministry also needs to step up to monitor and analyse the situation; to disseminate information, education, and communication materials for the general public; and to undertake essential measures for preventing a further rise in the number of mucormycosis cases in patients with COVID-19 and mortality.
© 2021 CDC/Dr Lucille K Georg/SPL
We declare no competing interests.
References
- 1.WHO COVID-19 Weekly Epidemiological Update. May 25, 2021. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20210525_weekly_epi_update_41.pdf?sfvrsn=d602902c_6&download=true
- 2.Singh P. Hindustan Times; May 21, 2021. Black fungus: here is a list of states with highest number of mucormycosis cases.https://www.hindustantimes.com/india-news/black-fungus-states-with-highest-number-of-mucormycosis-cases-101621559394002.html [Google Scholar]
- 3.Indian Council of Medical Research Evidence based advisory in the time of COVID-19 (screening, diagnosis & management of mucormycosis) May 9, 2021. https://www.icmr.gov.in/pdf/covid/techdoc/Mucormycosis_ADVISORY_FROM_ICMR_In_COVID19_time.pdf
- 4.John TM, Jacob CN, Kontoyiannis DP. When uncontrolled diabetes mellitus and severe COVID-19 converge: the perfect storm for mucormycosis. J Fungi. 2021;7:298. doi: 10.3390/jof7040298. [DOI] [PMC free article] [PubMed] [Google Scholar]