Abstract
Aim
This study aimed to explore the current status of e-health literacy among Chinese older adults, and to summarize and analyze the related influencing factors.
Subject and methods
Following the PRISMA Checklist, we searched MEDLINE, CINAHL Complete (EBSCO), PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure, WanFang Data, and China Science and Technology Journal Database to identify the relevant literature published between January 2000 and December 2020. The Mixed Methods Assessment Tool (MMAT) was used to appraise the quality of the studies.
Results
Five articles were included for the systematic review. The results showed that the e-health literacy of Chinese older adults was low. Based on the social-ecological model, the influencing factors at the individual level included age, gender, educational attainment, socioeconomic status, physical and psychological conditions, frequency of internet use, and credibility perception of online health resources; at the interpersonal level, the influencing factors included marital status, being the family carer and being taught how to use internet to find health resources; at the social/community level, influencing factors included language barriers and cultural barriers.
Conclusion
Current e-health literacy among Chinese older adults is low, which is affected by a number of factors. Medical staff should provide detailed health information with guaranteed accuracy and reliability for elderly people. It is necessary to develop intervention programs tailored to varied educational needs of the elderly with different backgrounds (i.e., age, gender, educational attainment, and socioeconomic status) need to be developed in the near future. Family members are encouraged to teach older adults how to use e-health resource in appropriate ways.
Keywords: E-health literacy, Older adults, Influencing factors, Systematic review
Introduction
In the digital age, people obtain a large amount of health information from the internet, which provides new opportunities for chronic disease management, and increases the bilateral communication between medical staff and patients in a continuous and real-time manner, both within and outside the hospital (Graffigna et al. 2017). Electronic health (e-health) refers to health services and information that are disseminated or enhanced through the internet and information technologies (Azeez and der Vyver 2019). The World Health Organization (WHO) believes that improving health services through digital technology can enable more people to enjoy better health and well-being (World Health Organization 2018).
E-health literacy is the ability to seek, find, understand, and appraise health information from electronic sources, and to apply gained knowledge to address or solve a health problem (Norman and Skinner 2006). The uneven level of e-health literacy means that not everyone has the opportunity and ability to enjoy the benefits of e-health, which leads to the emergence of the digital divide. The digital divide refers to a social phenomenon caused by the lack of coordination between the speed of socioeconomic development and the public’s ability to accept new technologies and culture (Hong et al. 2017). Many studies have confirmed that older adults are one of the main populations in the digital divide, especially in the field of medicine and health (Fox and Connolly 2018; Walker et al. 2020).
There were 176.03 million older adults over the age of 65 in China by the end of 2019, accounting for 12.57% of the total population (National Bureau of Statistics of China 2020). "Netizens" aged 60 and above accounted for only 6.7% of all netizens (Center China Internet Network Information 2020). Since the outbreak of COVID-19, online medical services such as online treatment and home delivery of medicines have developed rapidly in China, and electronic devices have become the main means for people to obtain health services. However, many older adults have faced huge challenges in accessing and using e-health resources, which has had a significantly negative impact on the elderly population (Paige et al. 2018). Developing e-health literacy skills and knowledge for the elderly, and promoting healthy aging is a priority of the WHO (Zhou and Zheng 2018).
The view that the elderly are experiencing low e-health literacy is universally supported (Arcury et al. 2020; Cherid et al. 2020; Choi and DiNitto 2013a), particularly among low-income homebound older adults (Choi and DiNitto 2013a) and individuals with chronic disease (Lin et al. 2019). A number of influencing factors were found to be associated with e-health literacy among older adults, such as age, gender, education attainment, marital status, and income (Liu 2020; Zhou 2018). However, the conclusions with regard to some of the influencing factors are controversial. For example, Zibrik et al. (2015) found that gender was significantly related to e-health literacy, while Cherid et al. (2020) found that the e-health literacy level was similar in elderly men and women. At present, the impact of the influencing factors associated with e-health literacy among Chinese older adults remain unclear. The elderly are the main beneficiaries of e-health resources in the digital age. It is necessary to attach great importance to the e-health literacy status of the elderly and its influencing factors (Wang et al. 2019), effectively solve the difficulties encountered by the elderly in obtaining and using e-health resources, and help the elderly bridge the digital divide and better integrate into the digital age.
The specific objectives of the study were to improve the understanding about current status of e-health literacy among Chinese older adults, and identify the set of factors contributing to the low level of e-health literacy based on the social-ecological model, so as to provide references for improving the e-health literacy of the elderly.
Methods
Literature search strategy
A review plan was developed by the research team in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist. An online database search was conducted between Dec 10 and Dec 12, 2020. To identify relevant published articles, we used the following eight databases including MEDLINE, CINAHL Complete (EBSCO), PubMed, Embase, Cochrane Library, China National Knowledge Infrastructure (CNKI), WANFANG DATA, and China Science and Technology Journal Database (VIP). The versions used were published between January 2000 and December 2020. The following combinations of terms and truncated words were used: (e-health literacy OR electronic health literacy OR digital literacy) AND (elderly OR aged OR old* OR ageing OR senior) AND (Chinese OR China).
Study selection criteria
To be selected for the review, articles needed to meet the following inclusion criteria: (a) focusing on e-health literacy, (b) targeting Chinese older adults aged 60 years and above, (c) exploring influencing factors of e-health literacy, (d) published in English or Chinese between January 2000 and December 2019. The articles were excluded if they were only about modifying related assessment tools.
Literature screening
All references retrieved from the databases were added to reference management software (EndNote X9). Exclusion of duplicates was finished automatically by this software. Two reviewers screened the titles and abstracts of the references for relevance, and identified whether they should be included for further review. Then the full texts were retrieved from the university online library and examined to determine if each study met our inclusion criteria and could be included in the review. The reference lists of included articles were also screened manually to identify additional publications. The screening procedure was conducted independently by two researchers. In case of disagreement in the above procedure, a third researcher would be contacted to resolve the conflict.
Quality appraisal
Two reviewers conducted the quality appraisal of the selected articles independently, utilising the Mixed Methods Appraisal Tool (MMAT) (Hong et al. 2018). The MMAT was developed at McGill University (a checklist and a tutorial), and can be used to appraise the methodological quality of qualitative, quantitative, and mixed-methods studies. The reliability and efficiency of MMAT for systematic mixed-studies review are promising (Pace et al. 2012). The included studies’ scores range from one to five by summing the total number of “yes” items, and are categorized into high (score of four or above), moderate (score of three) and poor (score of two or below) methodological quality based on their scores (Shrestha and Fick 2020). In case of disagreement in the assessments, a third researcher would be contacted to resolve the conflict.
Data extraction and analysis
The characteristics of the included studies were extracted, including author, year, sample, e-health literacy status, influencing factors, and conclusions. Descriptive and narrative syntheses were used to analyze the extracted data. The social-ecological model, as one of the most accepted explanations regarding the influence of personal characteristics and social environments on human development, was adopted to classify the associated influencing factors into individual, interpersonal, and social/community levels (Bronfenbrenner 2005). Due to the small number of studies included, we did not conduct a meta-analysis.
Results
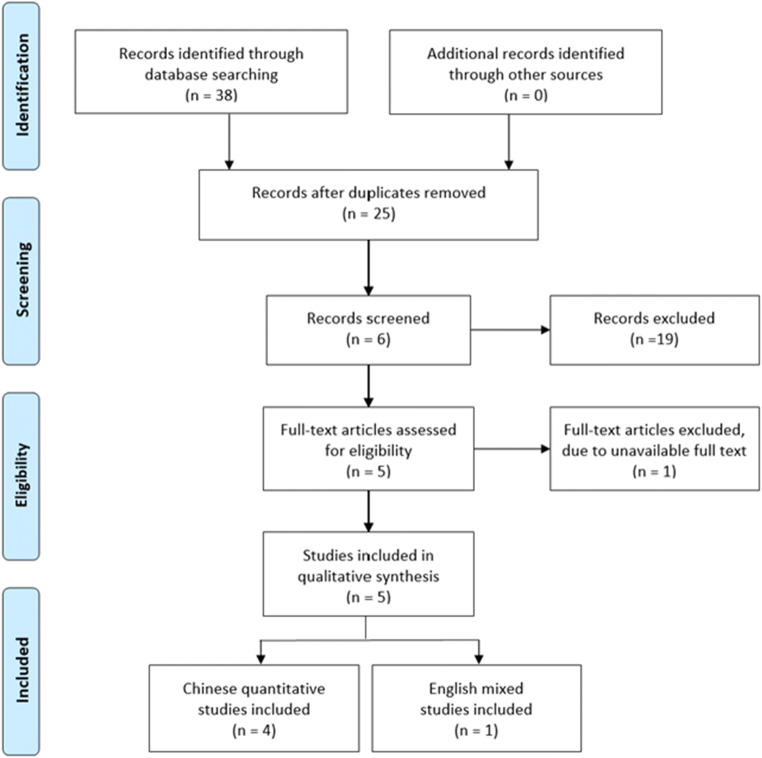
There were 38 records initially identified through database searching. After the removal of duplicates, 25 abstracts were reviewed, and six of them were included for further review. A total of five articles were included in the final synthesis, with one excluded due to full text being unavailable. Figure 1 shows the selection and reviewing process of the literature.
Fig. 1.
PRISMA flow diagram of the study selection process
The characteristics and quality of the included studies
Four of the included studies (Li et al. 2019; Liu et al. 2020; Zang et al. 2017; Zhou and Zheng 2018) were conducted in China. All of them were cross-sectional studies exploring the status quo and influencing factors of e-health literacy among Chinese older adults. Another one was conducted in British Columbia, and was a mixed study about e-health literacy among Chinese older adults living in British Columbia (Zibrik et al. 2015). Table 1 shows the characteristics of the studies. Quality appraisal results from the MMAT showed that the overall average quality of included studies was four, with scores ranging from three to five. Table 2 shows the individual quality appraisal details.
Table 1.
E-health literacy studies among Chinese people included in analysis
| First author | Sample | E-health literacy status among the Chinese elderly | Influencing factors | Conclusions |
|---|---|---|---|---|
| Ge Zang 2017 | 256 elderly hemodialysis patients (over 40 years old) in five hospitals in Zhengzhou city, China |
Total score: 18. 50 ± 6. 08 Score of application ability: 11. 83 ± 4. 04 Score of evaluation ability: 4.41 ± 1. 63 Score of decision-making ability: 2. 25 ± 0. 99 |
Quality of life, interpersonal relationships, somatic symptoms, fatigue, depression, sense of frustration | Senile maintained-hemodialysis patients’ e-health literacy level was low. In order to improve patients’ quality of life, it is suggested to improve the patients’ electronic health literacy. |
| Hanhan Zhou 2018 | 228 elderly people (over 60 years old) from eight communities in Jiangsu Province, China |
Average score: 1.51 ± 0.96 Average score of application ability: 1.52 ± 0.96 Average score of evaluation ability: 1.50 ± 0.98 Average score of decision-making ability: 1.51 ± 1.03 |
Credibility perception of finding health resources online, socioeconomic status (average monthly household income, educational attainment), family members teaching how to use internet to find health resources |
Seniors in communities with high socioeconomic status have more abilities and opportunities to use social resources, which is conducive to the improvement of their e-health literacy. Family members teach that using the Internet to find health resources can better improve the ability of seniors in the community to search, understand and evaluate health information on electronic resources, as well as their ability to use the information obtained to process and solve health problems. |
| Shaojie Li 2019 | 1201 elderly people (over 60 years old) from 24 communities randomly selected from Jinan city, China |
Total score: 17.24 ± 9.34 There were 133 elderly people scored more than 32 points The qualification rate of e-health literacy was 11. 1% |
Educational attainment, type of household registration, type of medical insurance, whether being the main person to taking care of grandchildren, whether their parents being alive, pension model, self-assessment of health status, self-assessment of life stress | E-health literacy of the elderly is at a low level, and comprehensive intervention mechanisms of government, community, and family should be established. |
| Zhen Liu 2020 | 472 elderly people (over 60 years old) from rural areas in Zhengzhou city, China | Total score: 13.76 ± 7.30 | Gender, age, marital status and frequency of Internet usage | Rural elderly people have a low level of e-health literacy, which has many influencing factors. Medical staff should take effective auxiliary interventions to improve the quality of life of patients. |
| Lindsay Zibrik 2015 | Including 338 Chinese senior immigrants in British Columbia (75% over 60 years old) | Chinese immigrant seniors in British Columbia had low e-health literacy levels (specific data not mentioned) | Age, income, educational attainment, gender, English proficiency, accessibility barriers and attitudes, cultural barriers | Age, gender, income and educational attainment are significantly related to eHEALS outcomes. Language, accessibility, attitude, and cultural barriers compound e-health literacy barriers in Chinese immigrant seniors. E-health tools for self-management must be culturally-tailored and designed to serve diverse populations. Partnership with community organizations is an appropriate platform to facilitate e-health driven knowledge translation within multicultural communities. |
Table 2.
Summary of the quality assessment of the included studies using the Mixed Methods Appraisal Tool (MMAT)
| Types of study design | Methodological quality criteria | Ge Zang 2017 | Hanhan Zhou 2018 | Shaojie Li 2019 | Zhen Liu 2020 | Lindsay Zibrik 2015 |
|---|---|---|---|---|---|---|
| Screening questions (for all types) | S1. Are there clear research questions? | √ | √ | √ | √ | √ |
| S2. Do the collected data make it possible to address the research questions? | √ | √ | √ | √ | √ | |
| 1. Qualitative | 1.1. Is the qualitative approach appropriate to answer the research question? | – | – | – | – | √ |
| 1.2. Are the qualitative data collection methods adequate to address the research question? | – | – | – | – | √ | |
| 1.3. Are the findings adequately derived from the data? | – | – | – | – | √ | |
| 1.4. Is the interpretation of results sufficiently substantiated by data? | – | – | – | – | √ | |
| 1.5. Is there coherence between qualitative data sources, collection, analysis and interpretation? | – | – | – | – | √ | |
| 2. Quantitative descriptive | 4.1. Is the sampling strategy relevant to address the research question? | √ | ? | √ | √ | √ |
| 4.2. Is the sample representative of the target population? | √ | √ | √ | √ | √ | |
| 4.3. Are the measurements appropriate? | √ | √ | √ | √ | √ | |
| 4.4. Is the risk of nonresponse bias low? | ? | ? | √ | ? | ? | |
| 4.5. Is the statistical analysis appropriate to answer the research question? | √ | √ | √ | √ | √ | |
| 3. Mixed methods | 5.1. Is there an adequate rationale for using a mixed methods design to address the research question? | – | – | – | – | √ |
| 5.2. Are the different components of the study effectively integrated to answer the research question? | – | – | – | – | √ | |
| 5.3. Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | – | – | – | – | √ | |
| 5.4. Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | – | – | – | – | √ | |
| 5.5. Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? | – | – | – | – | √ |
Note: “√” = yes; “×” = no; “?” = cannot tell; “-” = not applicable
Measurement of E-health literacy
In terms of the measurement of individual e-health literacy level, the included studies used the same screening tool: the e-Health Literacy Scale (eHEALS). This tool was originally formulated by Norman and introduced to China by Guo et al. (2013). The scale is a 5-point Likert scale containing eight items and three dimensions, including application ability, evaluation ability, and decision-making ability of online health information and services.
Current status of e-health literacy among Chinese older adults
The four studies conducted in China (Li et al. 2019; Liu et al. 2020; Zang et al. 2017; Zhou and Zheng 2018) had explored different elderly populations including hemodialysis patients and older adults residing in the community. All of them found that the e-health literacy among Chinese older adults was at a low level, with average scores less than 20, while a perfect score of e-health literacy is 40 points and a score of 32 or more is identified as qualified e-health literacy (Li et al. 2019; Meng and Shen 2018). In addition, the average scores in the three dimensions of the eHEALS scale were similar, and were at a low level as well. The study conducted in British Columbia (Zibrik et al. 2015) noted that Chinese immigrant seniors had low e-health literacy levels without giving specific data.
Influencing factors of e-health literacy at the individual level
Based on the social-ecological model, the individual level refers to the characteristics of individuals that influence their e-health literacy (Bronfenbrenner 2005). In this systematic review, influencing factors at the individual level included age, gender, educational attainment, socioeconomic status, physical and psychological health conditions, frequency of internet usage, and credibility perception of online health resources.
Younger elderly people were more likely to have higher e-health literacy level than the older ones. The studies indicated that the differences in e-health literacy among the elderly were statistically significant among different age groups (Liu et al. 2020). Older adults aged 60 to 69 were approximately four times (OR = 4.37, P < 0.05) more likely to master how to answer health-related questions using the internet than those aged greater than 80 (Zibrik et al. 2015). The e-health literacy of elderly males was higher than that of females in rural China (Liu et al. 2020). Female elderly immigrants in British Columbia were less likely to know how to find helpful health resource on the internet and have fewer skills to evaluate health resources than elderly males (Zibrik et al. 2015). In addition, married older adults had higher levels of e-health literacy (Liu et al. 2020). Educational attainment was positively associated with e-health literacy among the older adults (Li et al. 2019; Zang et al. 2017; Zhou and Zheng 2018; Zibrik et al. 2015). Li et al. found that the percentages of qualified e-health literacy were significantly higher for better-educated older adults, with 5.6% for primary school or below, 15.1% for the junior high school, 22.6% for the senior high school, and 44.1% for the university or above (Li et al. 2019).
The older adults’ household income was found to positively correlate with their e-health literacy level (Zhou and Zheng 2018; Zibrik et al. 2015). Older adults with household income more than $60,000 were three times more likely to know about identifying the quality of online health resources than those less than $40,000 (OR = −3.01, P < 0.001, Zibrik et al. 2015). Type of household registration was also identified as an influencing factor. The urban elderly people’s qualified rate of e-health literacy (eHEALS score > 32) was significantly higher than that of the elderly in rural areas (Li et al. 2019). Additionally, the type of medical insurance also mattered. The elderly with urban basic medical insurance or NCMS medical insurance had higher e-health literacy than those without these medical insurances (Li et al. 2019). Type of pension mode was identified as an influencing factor of older adults’ e-health literacy. Older participants with family pensions (Li et al. 2019) were more likely to have lower levels of e-health literacy compared those with other types of pension mode.
Poor self-assessment of health status, self-assessment of life stress, poor quality of life, poor interpersonal relationship, somatic symptoms, fatigue, depression, and sense of frustration were also related to lower e-health literacy (Li et al. 2019; Zang et al. 2017; Zhou and Zheng 2018).
The elderly who used the internet frequently have relatively high e-health literacy (Liu et al. 2020). A positive correlation was also found between the credibility perception and the e-health literacy among the elderly (Zhou and Zheng 2018). This was congruent with the results of Zibrik et al. indicating the relationship between accessibility challenges and attitudes and e-health literacy among elderly Chinese immigrants (Zibrik et al. 2015). According to their qualitative results, accessibility challenges and attitudes about technology centered on three themes: lack of access, usability challenges associated with aging, and attitudes about technology (Zibrik et al. 2015).
Influencing factors of e-health literacy at the interpersonal level
Based on the social-ecological model, the interpersonal level refers to meaningful one-on-one interactions (Bronfenbrenner 2005). In this systematic review, influencing factors at the interpersonal level included marital status, being family caretaker and being taught how to use the internet to find health resources. Older adults who were married had higher e-health literacy. The study of Li and research team showed that the elderly people who were the main person taking care of grandchildren and those whose parents were alive, were prone to have high e-health literacy level (Li et al. 2019). In addition, older adults who were taught how to use the internet to find health resources were more likely to have higher e-health literacy than those who were not. The average score on the eHEALS of those who were often be taught was 2.10 ± 1.21, while that of those who were never been taught was 1.37 ± 0.74 (Zhou and Zheng 2018).
Influencing factors of e-health literacy at the social/community level
Based on the social-ecological model, the social/community level refers to norms and values of cultures and subcultures or societal influences (Bronfenbrenner 2005). In this systematic review, influencing factors at the social/community level included language barriers and cultural barriers. For elderly Chinese immigrants, language barriers and cultural barriers were demonstrated as risk factors of their low e-health literacy. Zibrik et al. (2015) showed that limited English proficiency compounded low e-health literacy levels among elderly Chinese immigrants in British Columbia. Cultural understandings of illness and health were also found to be related to their low e-health literacy.
Discussion
With the advancement of information technology and the increased availability of online health information, the ability to access and use online health information becomes overwhelmingly important for older adults (Lustria et al. 2011). After reviewing the related studies, it was evident that Chinese elderly people have a low level of e-health literacy, which was consistent with the results of other studies (Hoogland et al. 2020; Shiferaw et al. 2020). Therefore, it is important to take preventive measures against risk factors of low e-health literacy at the individual, the interpersonal, and the social/community level.
At the individual level, old people’s vision, audition, limbs mobility, and memory are impaired as a result of aging, which makes it difficult for the elderly to seek, find, understand, and apply health information from electronic sources. In addition, socioeconomic status and educational attainment also influenced the access to, and uptake of e-health services (Hardiker and Grant 2011). The results were consistent with those of previous studies worldwide (Hoogland et al. 2020; Shiferaw et al. 2020; Villadsen et al. 2020). These identified non-modifiable factors can be used to determine which individuals are at risk of poor e-health literacy, and to indentify the vulnerable population that medical staff need to target (Cheng et al. 2020). Nokes and Reyes (2019) implemented health education interventions for low-income elderly people (vulnerable population) in America, and the results showed that these interventions improved the elderly’s e-health literacy and chronic disease self-management. Banbury et al. developed and tested an e-health literacy project in Australia, which was specifically designed for the elderly living in the community, resulting in improved access to health information among the older adults (Banbury et al. 2016). Frequent practice of using the internet had a positive association with high e-health literacy (Liu et al. 2020) and reduced anxiety about electronic devices (Pourrazavi et al. 2020). As main healthcare providers, medical staff should carry out relevant training programs for elderly people to practice e-health resources. In order to ensure training effects, training programs must be tailored to the educational needs of elderly people of different ages, gender, educational attainment, and socioeconomic status. In addition, the quality of online health information varies, leading to low credibility perception of e-health resources among the elderly (Lu et al. 2018). This problem is thorny but urgently needs to be solved. Almost all groups, not only the elderly, have doubts about the authenticity and reliability of e-health information (Lu et al. 2018; Zhou and Zheng 2018). Credibility perception of online health resources is a modifiable influencing factor, which can be improved by joint efforts. Partnerships of academic institutions and governmental agencies are needed to establish quality standards and develop a monitoring system for online health information producers (Daraz et al. 2019). The medical staff should provide scientific and accurate e-health information, and introduce some reliable e-health resources to the public, especially the elderly.
At the interpersonal level, the family plays an important role in maintaining and promoting e-health literacy among older adults (Liu et al. 2020). Children’s “digital feedback” (teaching the elderly how to use the internet to find health resources) to their parents is very important in helping the elderly to better adapt to the digital age. Choi and DiNitto (2013b) found the same results, despite different findings from Vroman’s study (Vroman et al. 2015). Therefore, family members should choose suitable ways for the elderly and encourage them to adapt and learn information technology such as WeChat and health-related mobile applications. Some elderly people who experience ageism might be less ready to use e-health resources, perceiving that they are “too old to learn” (Choi et al. 2020). It is necessary for family members to help the elderly overcome perceived ageism and improve their self-efficacy. As evidenced by this review, for these family members, taking care of grandchildren or parents may be an effective motivation, which has a positive correlation with the e-health literacy of the elderly. This may be related to the family responsibility of seeking scientific health information to meet the healthcare needs of their grandchildren and frail parents (Qi 2017). If the older adults’ physical condition permits, they are encouraged to look after grandchildren of their own accord, which may also motivate them to use e-health resources.
At the social/community level, language barriers and cultural barriers influenced the e-health literacy of Chinese immigrants. Our findings were consistent with the lower e-health literacy levels found among adult immigrants in Denmark (Villadsen et al. 2020) and America (Chesser et al. 2014). Language barriers and cultural barriers aggravate the difficulty of the immigrants in accessing and using e-health resources, especially the older adults, because they have to face multiple challenges of language, culture, and technology. In the context of the world’s multiculturalism, cross-cultural care capacity of medical care providers is expected. As suggested above, elderly immigrants also need social support from both medical staff and family members. The Chinese government has issued relevant policies to address the digital divide among the elderly, calling for the development of electronic devices and mobile applications that are more suitable for all elderly people from different cultures, and training programs to practice using these e-health resources.
What is already known on this topic
The uneven level of e-health literacy leads to the emergence of the digital divide in the older adults. Existing evidence has highlighted the low e-health literacy among older adults globally. However, the findings on associated influencing factors remains inconsistent.
What this study adds
To the best of our knowledge, this is the first systematic review of e-health literacy and its influencing factors among Chinese older adults. This study indicated low e-health literacy of elderly Chinese, and it can be affected by a number of influencing factors at the individual, interpersonal, and social/community levels.
The influencing factors at the interpersonal level have a great impact on the e-health literacy of the elderly in China. The elderly’s responsibility to look after their grandchildren and frail parents, and their children’s “digital feedback” has positive association with their e-health literacy. Our study highlights family support and tailored training programs to improve the e-health literacy of older adults.
Limitations
Although this review was based on a systematic and validated procedure, there were still some limitations. First, there were relatively few researches on e-health literacy among Chinese older adults. The number of articles included in this review was relatively small. Second, we did not conduct a meta-analysis, so the estimation of effect was not conducted. Third, the methodological quality of included studies was varied, with one only at moderate level.
Conclusions
Our review shows that the e-health literacy among Chinese older adults needs to be improved, and there are many associated influencing factors. In the digital age, aiming at enhancing older adults’ e-health literacy, medical staff should provide enough detailed health resources with guaranteed authenticity and reliability for elderly people with poor e-health literacy. Relevant training programs tailored to varied educational needs of the elderly with different age, gender, educational attainment, and socioeconomic status should also be carried out in the near future. Family members can try to support the elderly by encouraging them to look after grandchildren of their own accord and teaching them how to use e-health resources in appropriate ways. Further studies using more robust methodology are needed to examine the impact of these factors on e-health literacy among older adults.
Acknowledgements
Not applicable.
Authorship contribution statement
Shi, Zhang, Ma, and Chen designed the study. Shi and Ma conducted literature research, selection and quality appraisal. Shi and Ma wrote the first draft. Zhang and Chen revised it critically for important intellectual content.
Funding
This study was not funded.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuxin Shi and Denghui Ma contributed equally to this work.
Contributor Information
Yuxin Shi, Email: 2019203050023@whu.edu.cn.
Denghui Ma, Email: 2018203050027@whu.edu.cn.
Jun Zhang, Email: junz@whu.edu.cn.
Bowen Chen, Email: 823996171@qq.com.
References
- Arcury TA, Sandberg JC, Melius KP, et al. Older adult internet use and eHealth literacy. J Appl Gerontol. 2020;39(2):141–150. doi: 10.1177/0733464818807468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azeez NA, der Vyver CV. Security and privacy issues in e-health cloud-based system: a comprehensive content analysis. Egypt Inform J. 2019;20(2):97–108. doi: 10.1016/j.eij.2018.12.001. [DOI] [Google Scholar]
- Banbury A, Parkinson L, Nancarrow S, Dart J, Gray LC, Buckley J. Delivering patient education by group videoconferencing into the home: lessons learnt from the Telehealth Literacy Project. J Telemed Telecare. 2016;22(8):483–488. doi: 10.1177/1357633X16674359. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Making human beings human: bioecological perspectives on human development. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- Center China Internet Network Information (2020) The 46th China statistical report on internet development. CCINI, Beijing. http://www.cnnic.cn/gywm/xwzx/rdxw/202009/t20200929_71255.htm. Accessed 9 September 2020
- Cheng C, Beauchamp A, Elsworth GR, Osborne RH. Applying the electronic health literacy lens: systematic review of electronic health interventions targeted at socially disadvantaged groups. J Med Internet Res. 2020;22(8):e18476. doi: 10.2196/18476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherid C, Baghdadli A, Wall M, et al. Current level of technology use, health and eHealth literacy in older Canadians with a recent fracture—a survey in orthopedic clinics. Osteoporosis Int. 2020;31(7):1333–1340. doi: 10.1007/s00198-020-05359-3. [DOI] [PubMed] [Google Scholar]
- Chesser A, Burke A, Reyes J, Rohrberg T. Navigating the digital divide: a systematic review of eHealth literacy in underserved populations in the United States. Informat Health Social Care. 2014;41(1):1–19. doi: 10.3109/17538157.2014.948171. [DOI] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. 2013;15(5):e93. doi: 10.2196/jmir.2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM. Internet use among older adults: association with health needs, psychological capital, and social capital. J Med Internet Res. 2013;15(5):e97. doi: 10.2196/jmir.2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi EY, Kim Y, Chipalo E, Lee HY, Meeks S. Does perceived ageism widen the digital divide? And does it vary by gender? Gerontologist. 2020;60(7):1213–1223. doi: 10.1093/geront/gnaa066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daraz L, Morrow AS, Ponce OJ, et al. Can patients trust online health Information a meta-narrative systematic review addressing the quality of health Information on the internet. J Gen Intern Med. 2019;34(9):1884–1891. doi: 10.1007/s11606-019-05109-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox G, Connolly R. Mobile health technology adoption across generations: narrowing the digital divide. Inform Syst. 2018;28(6):995–1019. doi: 10.1111/isj.12179. [DOI] [Google Scholar]
- Graffigna G, Barello S, Bonanomi A, Riva G. Factors affecting patients’ online health information-seeking behaviours: the role of the patient health engagement (PHE) model. Patient Educ Couns. 2017;100(10):1918–1927. doi: 10.1016/j.pec.2017.05.033. [DOI] [PubMed] [Google Scholar]
- Guo S, Yu X, Sun Y, Nie D, Li X, Wang L. Exploration on chinesization and applicability of eHEALS. Chin J Health Educ. 2013;29(02):106–108. doi: 10.16168/j.cnki.issn.1002-9982.201. [DOI] [Google Scholar]
- Hardiker NR, Grant MJ. Factors that influence public engagement with eHealth: a literature review. Int J Med Inform. 2011;80(1):1–12. doi: 10.1016/j.ijmedinf.2010.10.017. [DOI] [PubMed] [Google Scholar]
- Hong Y, Zhou Z, Fang Y, Shi L. The digital divide and health disparities in China: evidence from a national survey and policy implications. J Med Internet Res. 2017;19(9):e317. doi: 10.2196/jmir.7786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong QN, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Infor. 2018;34(4):285–291. doi: 10.3233/EFI-180221. [DOI] [Google Scholar]
- Hoogland AI, Mansfield J, Lafranchise EA, Bulls HW, Johnstone PA, Jim HSL. eHealth literacy in older adults with cancer. J Geriatr Oncol. 2020;11(6):1020–1022. doi: 10.1016/j.jgo.2019.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S, Xu H, Cui G. Analysis of eHealth literacy and its influencing factors among the elderly. Chin J Disease Control Prevent. 2019;23(11):1318–1322. doi: 10.16462/j.cnki.zhjbkz.2019.11.004. [DOI] [Google Scholar]
- Lin C, Broström A, Griffiths MD, Pakpour AH. Psychometric evaluation of the Persian eHealth literacy scale (eHEALS) among Iranians with heart failure. Eval Health Prof. 2019;43(4):222–229. doi: 10.1177/0163278719827997. [DOI] [PubMed] [Google Scholar]
- Liu Z, Zhang H, Zhang Y, et al. Current situation and influencing factors of e-health literacy among rural older adults in Zhengzhou. Modern Prevent Med. 2020;47(2):283–309. [Google Scholar]
- Lu X, Zhang R, Wu W, Shang X, Liu M. Relationship between internet health Information and patient compliance based on trust: empirical study. J Med Internet Res. 2018;20(8):e253. doi: 10.2196/jmir.9364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustria MLA, Smith SA, Hinnant CC. Exploring digital divides: an examination of eHealth technology use in health information seeking, communication and personal health information management in the USA. Health Informatics J. 2011;17(3):224–243. doi: 10.1177/1460458211414843. [DOI] [PubMed] [Google Scholar]
- Meng S, Shen C. Current situation of eHealth literacy and health behaviors of college students in Nanjing. Chin J Health Educ. 2018;34(03):254–257. doi: 10.16168/j.cnki.issn.1002-9982.2018.03.014. [DOI] [Google Scholar]
- National Bureau of Statistics of China . China statistical yearbook. Beijing: China Statistics Press; 2020. [Google Scholar]
- Nokes KM, Reyes DM. Do brief educational sessions increase electronic health literacy of low-income persons living with HIV/AIDS? Comput Inform Nurs. 2019;37(6):315–320. doi: 10.1097/CIN.0000000000000515. [DOI] [PubMed] [Google Scholar]
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. 2006;8(2):e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R. Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53. doi: 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Paige SR, Miller MD, Krieger JL, Stellefson M, Cheong J. Electronic health literacy across the lifespan: measurement invariance study. J Med Internet Res. 2018;20(7):e10434. doi: 10.2196/10434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pourrazavi S, Kouzekanani K, Bazargan-Hejazi S, Shaghaghi A, Hashemiparast M, Fathifar Z, Allahverdipour H. Theory-based E-health literacy interventions in older adults: a systematic review. Arch Public Health. 2020;78(1):1–8. doi: 10.1186/s13690-020-00455-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi W. Factors influencing Information seeking behavior of rural migrant grandparent caregivers. Library Tribune. 2017;37(09):79–90. [Google Scholar]
- Shiferaw KB, Tilahun BC, Endehabtu BF, Gullslett MK, Mengiste SA. E-health literacy and associated factors among chronic patients in a low-income country: a cross-sectional survey. BMC Med Inform Decis Mak. 2020;20(1):181. doi: 10.1186/s12911-020-01202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha P, Fick DM. Family caregiver’s experience of caring for an older adult with delirium: a systematic review. Int J Older People Nursing. 2020;15(4):e12321. doi: 10.1111/opn.12321. [DOI] [PubMed] [Google Scholar]
- Villadsen SF, Hadi H, Ismail I, Osborne RH, Ekstrøm CT, Kayser L. Ehealth literacy and health literacy among immigrants and their descendants compared with women of Danish origin: a cross-sectional study using a multidimensional approach among pregnant women. BMJ Open. 2020;10(5):e37076. doi: 10.1136/bmjopen-2020-037076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vroman KG, Arthanat S, Lysack C. “Who over 65 is online?” older adults’ dispositions toward information communication technology. Comput Human Behav. 2015;43:156–166. doi: 10.1016/j.chb.2014.10.018. [DOI] [Google Scholar]
- Walker DM, Hefner JL, Fareed N, Huerta TR, McAlearney AS. Exploring the digital divide: age and race disparities in use of an inpatient portal. Telemed J E Health. 2020;26(5):603–613. doi: 10.1089/tmj.2019.0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Chen Z, Zhang M, et al. Study of the prevalence and disease burden of chronic disease in the elderly in China. Chin J Epidemiol. 2019;40(3):227–283. doi: 10.3760/cma.J.issn.0254-6450.2019.03.005. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2018) Digital health. World Health Organization, Geneva. http://appswhoint/gb/ebwha/pdf_files/WHA71/A71_R7-enpdf?ua=1 Accept 26 May 2018
- Zang G, Shi Q, Xu T, Dong Y. The related research of elderly hemodialysis patients’ electronic health literacy to the quality of life. Modern Prevent Med. 2017;44(04):672–675. [Google Scholar]
- Zhou H, Zheng A. Analysis of current situation and influencing factors of community elderly electronic health literacy. J Nanjing Med Univ (Social Sci) 2018;18(06):455–458. doi: 10.7655/NYDXBSS20180610. [DOI] [Google Scholar]
- Zibrik L, Khan S, Bangar N, Stacy E, Novak Lauscher H, Ho K. Patient and community centered eHealth: exploring eHealth barriers and facilitators for chronic disease self-management within British Columbia’s immigrant Chinese and Punjabi seniors. Health Policy Techn. 2015;4(4):348–356. doi: 10.1016/j.hlpt.2015.08.002. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.