Abstract
Background
Safely and effectively discharging a patient from the hospital requires working within a multidisciplinary team. However, little is known about how perceptions of responsibility among the team impact discharge communication practices.
Objective
Our study attempts to understand residents’ perceptions of who is primarily responsible for discharge education, how these perceptions affect their own reported communication with patients, and how residents envision improving multidisciplinary communication around discharges.
Design
A multi-institutional cross-sectional survey.
Participants
Internal medicine (IM) residents from seven US residency programs at academic medical centers were invited to participate between March and May 2019, via email of an electronic link to the survey.
Main Measures
Data collected included resident perception of who on the multidisciplinary team is primarily responsible for discharge communication, their own reported discharge communication practices, and open-ended comments on ways discharge multidisciplinary team communication could be improved.
Key Results
Of the 613 resident responses (63% response rate), 35% reported they were unsure which member of the multidisciplinary team is primarily responsible for discharge education. Residents who believed it was either the intern’s or the resident’s primary responsibility had 4.28 (95% CI, 2.51–7.30) and 3.01 (95% CI, 1.66–5.71) times the odds, respectively, of reporting doing discharge communication practices frequently compared to those who were not sure who was primarily responsible. To improve multidisciplinary discharge communication, residents called for the following among team members: (1) clarifying roles and responsibilities for communication with patients, (2) setting expectations for communication among multidisciplinary team members, and (3) redefining culture around discharges.
Conclusions
Residents report a lack of understanding of who is responsible for discharge education. This diffusion of ownership impacts how much residents invest in patient education, with more perceived responsibility associated with more frequent discharge communication.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-020-06508-4.
KEY WORDS: discharge communication, multidisciplinary team, transitions of care
INTRODUCTION
Discharging patients from the hospital is a complex and often chaotic process. Multidisciplinary teams are required to communicate with the patient and with one another to coordinate care for soon-to-be-discharged patients.1 This process often leaves patients with unanswered questions about medication changes, follow-up plans, and symptom management.2–4 It is vital for teams to work in a coordinated fashion to ensure the patient leaves the hospital prepared for the next care setting.
Limited single-site studies have explored multidisciplinary roles and responsibility around discharge communication and have identified differing perceptions. One study identified discharge education with patients as a shared responsibility.5 In another study, inter-professional team members disagreed on the residents’ roles.6 However, with multiple stakeholders responsible for the discharge, limited time, and competing clinical duties, diffusion of responsibility may result in relinquished ownership, and mandated administrative discharge tasks are often prioritized over taking the time to communicate discharge plans with patients.7–9 Therefore, we sought to characterize perceptions of primary responsibility of discharge education, as we hypothesized that this default understanding of responsibility will prevail in the demanding clinical environment; currently, who is or ought to be predominantly responsible is not well-established. We also sought to assess to what degree these views of primary responsibility impact a resident’s own patient education practices at discharge.
Residents can offer insights on the workings of multidisciplinary teams at discharge, since they play a central role in the transitions of care process within academic hospital systems.1 Therefore, we also aimed to examine residents’ proposed areas for improvement with multidisciplinary communication at discharge.
METHODS
We conducted a cross-sectional survey of internal medicine (IM) residents at seven US residency programs.10 We recruited a convenience sample of programs for geographic diversity by leveraging professional and personal connections with educational leaders. Between March and May 2019, we emailed all IM residents at each participating institution an electronic link of the survey (REDCap Version 9.1.23, Nashville, TN). We sent up to two reminders to non-responders. The Institutional Review Boards at each participating institution approved the protocol, and participants’ survey responses implied their consent.
Instrument Design
Survey questions were constructed based on Transitions of Care consensus from national societies11–13 and health services research,14, 15 as well as interviews and focus groups with residents and junior faculty. We conducted iterative pilot testing and refinement of the questionnaire with cognitive interviews. The data presented in this study is a part of a larger survey addressing multiple aspects of discharge education; only questions pertinent to understanding resident perceptions of roles and responsibilities are presented in Appendix 1.
For the outcome variable, we identified six patient communication domains as crucial to be addressed with patients at hospital discharge: purpose of medication changes,16, 17 follow-up appointments and their purpose (e.g., pending tests),14, 18 self-management of disease,3, 4, 19, 20 symptom expectations,3, 19 red flags,14, 20 and teach back of understanding of the discharge plan.21, 22 Residents rated the frequency that they addressed each of these communication domains using a 5-point scale: 1 = rarely (0 to 20%), 2 = not usually (21 to 40%), 3 = sometimes (41 to 60%), 4 = often (61 to 80%), or 5 = almost always (> 80%).
Independent variables included which team member the resident believes is primarily responsible for and best suited for educating patients before discharge. Residents during cognitive interviews consistently interpreted “patient education at discharge” as encompassing the six discharge education practices asked about earlier in the survey. Additionally, since none of the sites in the study had role designations among post-graduate years or members of the multidisciplinary team for each discharge education domain, we felt comfortable asking about perceived responsibility of overall patient education at discharge. Finally, we asked what perceived factors might keep the resident from consistently performing comprehensive discharge education with patients.
Analysis
We described residents’ perceptions of the team member that is primarily responsible and best suited for discharge education as well as factors for not comprehensively addressing discharge education. For each communication practice, we characterized the residents that answered “often (61%-80%)” or “almost always (>80%)” as residents who addressed that domain with patients “frequently.”
We sought to determine whether the six discharge communication practice items were measuring a single construct by conducting a principal components analysis. Factor analysis of these six items loaded to a single construct with factor loadings for each item ranging from 0.621 to 0.733. We then used Cronbach’s alpha to determine internal consistency of these items as a single measure of discharge practice behavior. The Cronbach alpha for the six discharge communication domains was 0.838, demonstrating acceptable levels of internal consistency. Based on these results, we averaged each resident’s response for the six discharge practices on a 1 to 5 scale into a mean discharge communication score, with 1 representing rarely doing the six communication practices and 5 representing almost always addressing each of them.
To model the relationship between attribution of discharge responsibility and exemplary discharge patient communication practices, we dichotomized the mean discharge communication practice score into ≥ 4 (the six communication practices done in aggregate at least “frequently,” > 60% of time) and < 4 (done less than frequently, < 60%). We used multiple logistic regression to assess the relationship between residents’ perceptions of who is primarily responsible for discharge education and the residents’ dichotomized discharge communication scores. The cutoff for significance was determined to be p value of ≤ 0.05.
Two authors (ZK, ST) used content analysis for the free response question on suggested areas for improvement with multidisciplinary communication.23 Each coder independently developed a preliminary codebook after reviewing all survey results, followed by iterative revision and discussion, ultimately combining codes into a single codebook. Discussion of coding and attention to relationships yielded key themes.
RESULTS
Of the 966 internal medicine residents invited to participate across the seven institutions, 613 (63%) responded. Table 1 shows the distribution of response rate among post-graduate years and program sites.
Table 1.
Response Rates of Internal Medicine Residency Programs and Post-Graduate Year
| Training program | Respondents/total residents at program (%) |
|---|---|
| Baylor College | 127/215 (59%) |
| Cornell University | 77/132 (58%) |
| New York University | 111/174 (64%) |
| Temple University | 60/104 (58%) |
| University of Arkansas | 69/82 (84%) |
| University of California San Francisco | 118/176 (67%) |
| University of Iowa | 50/82 (60%) |
| Post-Graduate Year (PGY) | Respondents (% of n = 613) |
| PGY-1 | 244 (36%) |
| PGY-2 | 191 (31%) |
| PGY-3 | 196 (33%) |
Perception of Primary Responsibility vs. Best Suited for Discharge Education
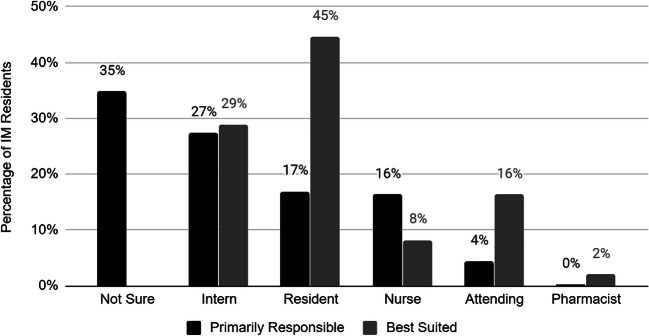
There was considerable variability among residents’ perceptions of who is primarily responsible for and best suited to perform hospital discharge education with patients (Fig. 1). The most common response (35%) was that residents were not sure who was primarily responsible for patient education at discharge, followed by the intern (27%), the resident (17%), the nurse (16%), and the attending (4%). In contrast, about half (45%) pointed to the senior resident on the team as best suited to be primarily responsible for discharge education. Less than a third (29%) believed the intern was best suited, while 16% believed it was the attending. Less than a tenth (8%) of residents believed nurses were best suited.
Figure 1.
Residents’ perception on who is primarily responsible and best suited for discharge education with patients (n = 613).
Discharge Communication Practices
Less than three-quarters of the residents reported frequently addressing the purpose of medication changes (71%) and red flags signs (69%). About half of residents reported addressing the purpose of follow-up appointments (52%), symptom expectations (47%), and self-management of disease (39%) on a regular basis. Less than a fifth (17%) of residents reported asking patients to teach back the discharge plan frequently. Table 2 shows the distribution of the frequency of each of the six discharge communication practices.
Table 2.
IM Residents' Self-Reported Frequency of Reviewing Key Domains with Patients Before Discharge (n = 613)
| Rarely (0 to 20%) |
Not usually (21 to 40%) |
Sometimes (41 to 60%) |
Often (61 to 80%) |
Almost always (> 80%) |
|
|---|---|---|---|---|---|
| Purpose of medication changes | 20 (3.0) | 36 (5.9) | 119 (19.5) | 175 (28.6) | 261 (42.7) |
| Red flags | 29 (4.8) | 50 (8.2) | 110 (18.0) | 205 (33.4) | 217 (35.5) |
| Purpose of follow-up appointments | 53 (8.7) | 73 (11.9) | 166 (27.1) | 171 (27.8) | 149 (24.4) |
| Symptom expectations | 37 (6.1) | 94 (15.3) | 191 (31.2) | 178 (29.1) | 112 (18.3) |
| Self-management of disease | 56 (9.1) | 123 (20.1) | 196 (31.9) | 169 (27.6) | 69 (11.3) |
| Teach back discharge plan | 166 (27.2) | 167 (27.3) | 174 (28.5) | 81 (13.3) | 23 (3.8) |
The average resident’s mean discharge communication score was 3.36 (95% C.I 3.29, 3.42). There were 169 (28%) residents who had a mean discharge communication score ≥ 4.
Factors Contributing to Inconsistent Comprehensive Discharge Education
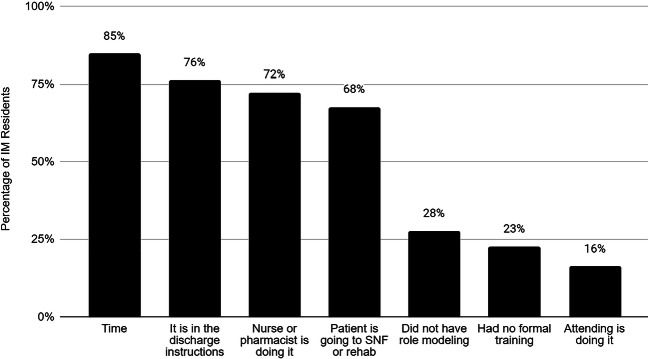
When asked the reason they do not practice comprehensive discharge education, as in Figure 2, the majority reported time (85%) as a barrier. About three-quarters (76%) of IM residents said that it was because the information was already in the discharge instructions, while 72% cited nurses or pharmacists doing discharge education. Lastly, 68% of residents pointed to the disposition of patients to skilled nursing facilities as a factor for not further educating patients in preparation for discharge.
Figure 2.
Factors for not doing comprehensive discharge education with patients.
Resident Patient Education Practices and Perceptions of Primary Responsibility
After adjusting for PGY-year and institutions, if the resident believed educating patients at discharge was the primary responsibility of the intern, he or she had a 4.28 (95% C.I 2.5, 7.2) times the odds of reporting discharge communication practices as done frequently compared to those who were not sure who was primarily responsible (Fig. 3). Similarly, among residents who said the senior resident was primarily responsible, there was 3.08 (95% C.I 1.66, 5.71) times the odds of discharge communication practices reported as done frequently compared to those who were not sure.
Figure 3.
Odds of overall discharge communication practices reported as done frequently based on perception of primary responsibility.
Content Analysis of Areas of Discharge Multi-Disciplinary Communication that Need Improvement
Analysis of the 257 free-text responses revealed three themes for improvement in multidisciplinary communication when discharging patients from the hospital. The mean discharge communication scores for those that commented (3.45, 95% C.I 3.37,3.51) compared to those that did not (3.38, 95% C.I 3.32, 3.46) were similar (p = 0.36).
(1) Clarifying Roles and Responsibilities for Communication with Patients
Residents reported not understanding the roles of each team member in patient communication at discharge. Residents suggested that better defining these responsibilities could mitigate working under false assumptions. However, while some felt the defined roles should overlap, others felt there should be a division of responsibilities to prevent duplication of work.
Need clarification on who will actually speak to the patient at the bedside to review which parts of the discharge instructions - we assume it is nursing most of the time but it may help to have a physician re-iterate or review the information a second time.
Sometimes I might be assuming that the nurse / case manager / social worker / pharmacist are covering topics that they are not, and vice versa. I do believe that we also do a fair amount of duplication of effort because we don't know that they are also reviewing discharge information
Beyond team members’ responsibilities at discharge, some residents wanted a deeper understanding of team members’ workflow and priorities in an effort to understand the gaps and their own role in educating the patient at discharge.
Sometimes my priorities are not those of the other members of the team. All interns need education on what the nurse discharge process entails so that they can highlight important pieces or fill in gaps, rather than just winging it.
(2) Setting Expectations for Communication amongst Multidisciplinary Team Members
Another area for improvement was communication during multidisciplinary rounds (MDR). Residents expressed strong views on what to share and when. They commented on shifting the focus of MDR from the estimated date of discharge to discharge follow-up plans and readmission prevention.
Can we PLEASE make the estimated day of discharge less of a singular focus? I've had conversations in multidisciplinary rounds that proceed something like, ‘This patient is febrile, still on IV antibiotics, we don’t have adequate source control.’ ‘Ok, can they go home today?’ It’s a frustrating situation when it occurs.
At the same time, residents wanted MDR communication to be efficient with concise targeted plans without side conversations. Residents also had suggestions on the way in which we communicate with each other. They emphasized the need for explicit ownership of a task once it is mentioned and closed loop communication on the outcome of that task. Tasks not heard on rounds or without clear follow through created tension.
People are usually just listening without ownership of tasks on those rounds. I often go through a few hurdles to see if tasks got done. We need specific statements taking up responsibility and communication when it’s done.
(3) Redefining Culture around Discharges
Lastly, residents highlighted the clinical environment that shapes a patient’s transition to outpatient care as an area for change. Residents pointed to a pressurized culture that expected and prioritized the patient’s physical exit from the hospital.
Unfortunately, multidisciplinary rounds have become quite stressful for residents. I believe this comes from such a push to get patients out earlier and earlier. If we think a patient is not safe for discharge, we should not be getting questioned about our reasons to keep the patient another day.
The seemingly competing priorities of each multidisciplinary player were thought to make multidisciplinary communication tense and, at times, inhospitable.
MDR becomes a place where others complain that we're not discharging fast enough and to beat up on clinical decision making. There’s no set agenda, just (another) patient presentation and rapid-fire questioning from random people.
Improve hostility between social work and clinicians regarding trying to get patients out quickly as possible.
Residents believed the lack of shared understanding among the different roles fed the general sense of disregard when something went wrong.
We (residents) have NO idea how work is divided between other members and they often seem to expect that we would/should know the various distinctions of their roles (i.e. who plans for rehab vs SNF vs home oxygen vs VNS). Also, there is often (depending on the floor) a culture of disrespect from case managers and social workers towards residents about these issues.
DISCUSSION
Residents in our multi-institutional survey had widely varying perceptions of which member of the hospital ward team has primary ownership of discharge education with patients. Our findings suggest that these perceptions of primary responsibility affected the extent of residents’ own communication with patients at discharge. These results imply that residents are operating without a shared mental model of roles and responsibilities at this vulnerable time in patients’ care. This dispersed ownership of patient education may help explain why readmitted patients point to suboptimal communication and inadequate understanding of discharge plans as contributors to their readmissions.24, 25 Guidelines for communication among practitioners regarding the shared work of discharge education are scarce.5 And even though residents who feel more responsible report performing more discharge education, how to most effectively work with an multidisciplinary team to perform this multidisciplinary task, remains uncertain.
It is striking that 72% of residents cited nurses or pharmacists doing discharge education as a reason for not providing comprehensive patient education themselves, yet only 8% believe the nurse or pharmacist is best suited for patient discharge education. It is possible that limited time, as well as diffusion and lack of clarity of responsibility, contributes to this discrepancy. Role ambiguity and diffusion of responsibility among teams have been described in prior literature as barriers to effective transitions of care delivery.7, 26–29 Healthcare providers often report being accustomed to poor communication and teamwork, operating in a “culture of low expectations.”30 Additionally, there can be poor overlap of priorities for patients,1, 30, 31 as discharges are often subdivided into social, physical, and medical goals for patients32 without a shared, summative plan.
The question remains: how can we operate with a shared mental model for each patient and their unique transitions-of-care needs? This is an especially perplexing question because increased shared understanding is the intention behind many already adopted interprofessional interventions, such as multidisciplinary rounds, decision-making tools, and designated lists of patients to be discharged.33, 34 However, the fidelity of sustaining quality improvement efforts can be difficult to implement and measure.35
The residents’ suggested areas for improvement align with core competencies developed by the Interprofessional Education Collaborative (IPEC) that graduate programs from various healthcare disciplines must demonstrate for interprofessional teamwork (Fig. 4).36 However, these formative interprofessional education (IPE) experiences required in graduate school do not seem to translate in the postgraduate period, particularly in the demanding clinical context of discharges. Our results suggest reexamining post-graduate IPE to address difficulties with patient discharges.37 Discharges can be moving-targets, and shared situational awareness can optimize team performance: hospital teams can employ evidence-based models, such as TeamSTEPPS to delineate explicit roles and responsibility for patients being discharged, enhance communication with each other, and create an environment of mutual respect.38
Figure 4.
Themes for improvement of multidisciplinary discharge communication align with core competencies of interprofessional collaboration.
Nevertheless, we cannot ask more from trainees or teams without critically evaluating the system-level factors that facilitate or impede multidisciplinary communication and patient education. Soon-to-be-discharged patients demand attention, time, and space: in 2010, one study showed increased odds of adjusted, 30-day readmissions for every additional discharge that an intern completed on the day of patient discharge.39 Additionally, residents pointed to the use of discharge paperwork and nursing instructions as a reason for not comprehensively addressing discharge education themselves. Yet, these same physicians-in-training may not know what nursing staff do at discharge or may not have seen how information is conveyed in written form to patients, and therefore cannot be sure their post-discharge plans are being effectively passed on. Many hospitals have also moved to discharges earlier in the day, which adds time pressure to the immense cognitive load of discharge care.40, 41 The clinical and educational enterprise must work together to rethink work structures that can ultimately affect patient morbidity post-discharge. We hope our results provide an impetus for reflection and shed light on the varying assumptions that residents operate with to tackle the cognitive effort that discharges entail.
Limitations to our study include risk of social desirability bias, as answers may not always accurately represent actual behaviors of respondents. On the other hand, their reported communication may be affected when recalling specific patients with delirium or dementia, or those discharged to rehabilitation centers. Asking about responsibility of discharge education may be an oversimplification since there are many components of discharge education. However, our cognitive interviews revealed that residents answered with the other survey items on discharge communication in mind. Additionally, there was a lack of input from other interdisciplinary team members or patients involved in the discharge process. Lastly, none of the sites in our study had role designations among the multidisciplinary team, and therefore our findings may not be generalizable to sites with more robust responsibility designations or additional discharge personnel.
Future steps include (1) exploring how residents learn about responsibilities around discharge education to guide interventions, such that all residents have the same messaging on ownership of discharge education tasks, and (2) developing guidelines delineating the shared versus unique responsibilities among team members for specific discharge education practices
CONCLUSION
Developing proficiency in team collaboration to discharge patients effectively and safely is a critical skill in hospital medicine. This study demonstrates that normative beliefs of discharge education responsibility may influence reported discharge communication practices. Residents call for clarity around which team member is responsible for which parts of patient discharge education, how we communicate with each other, and why cultural tensions exist around discharges.
Supplementary Information
(DOCX 16 kb)
Acknowledgments
The authors would like to thank Shreya Singhal for statistical assistance as well as Amy Ou MD, Masha Slavin MD, Bilal Alqam MD, Marina.Baskharoun MD, Alice Tang MD, Albin Mammen MD and Dharmini Pandya for help distributing the survey.
Funding
Dr. Shreya P. Trivedi’s time was supported by Health Resources and Services Administration-T32 grant (T32HP22238).
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pinelli VA, Papp KK, Gonzalo JD. Interprofessional Communication Patterns During Patient Discharges: A Social Network Analysis. J Gen Intern Med. 2015;30(9):1299–1306. doi: 10.1007/s11606-015-3415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center. JAMA Intern Med. 2013;173(18):1715–1722. doi: 10.1001/jamainternmed.2013.9318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holland DE, Mistiaen P, Bowles KH. Problems and unmet needs of patients discharged “home to self-care”. Prof Case Manag. 2011;16(5):240–250. doi: 10.1097/NCM.0b013e31822361d8. [DOI] [PubMed] [Google Scholar]
- 4.Cain CH, Neuwirth E, Bellows J, Zuber C, Green J. Patient experiences of transitioning from hospital to home: an ethnographic quality improvement project. J Hosp Med. 2012;7(5):382–387. doi: 10.1002/jhm.1918. [DOI] [PubMed] [Google Scholar]
- 5.Ashbrook L, Mourad M, Sehgal N. Communicating discharge instructions to patients: a survey of nurse, intern, and hospitalist practices. J Hosp Med. 2013;8(1):36–41. doi: 10.1002/jhm.1986. [DOI] [PubMed] [Google Scholar]
- 6.Card SE, Ward HA, Chipperfield D, Sheppard MS. Postgraduate internal medicine residents’ roles at patient discharge - do their perceived roles and perceptions by other health care providers correlate? J Interprof Care. 2014;28(1):76–78. doi: 10.3109/13561820.2013.800849. [DOI] [PubMed] [Google Scholar]
- 7.Greysen SR, Schiliro D, Horwitz LI, Curry L, Bradley EH. “Out of sight, out of mind”: housestaff perceptions of quality-limiting factors in discharge care at teaching hospitals. J Hosp Med. 2012;7(5):376–381. doi: 10.1002/jhm.1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nordmark S, Zingmark K, Lindberg I. Process evaluation of discharge planning implementation in healthcare using normalization process theory. BMC Med Inform Decis Mak. 2016;16:48. doi: 10.1186/s12911-016-0285-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin F, Chaboyer W, Wallis M, Miller A. Factors contributing to the process of intensive care patient discharge: an ethnographic study informed by activity theory. Int J Nurs Stud. 2013;50(8):1054–1066. doi: 10.1016/j.ijnurstu.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Trivedi SP, Kopp Z, Tang AJ, Mammen A, Pandya D, Horwitz LI, Schwartz MD. Educational Lapses and Signals in Discharge Communication Practices: A Multi-Institutional Survey of Internal Medicine Residents [in press]. Acad Med. [DOI] [PubMed]
- 11.Yam CH, Wong EL, Cheung AW, Chan FW, Wong FY, Yeoh EK. Framework and components for effective discharge planning system: a Delphi methodology. BMC Health Serv Res. 2012;12:396. doi: 10.1186/1472-6963-12-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine. J Gen Intern Med. 2009;24(8):971–976. doi: 10.1007/s11606-009-0969-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burke RE, Kripalani S, Vasilevskis EE, Schnipper JL. Moving beyond readmission penalties: creating an ideal process to improve transitional care. J Hosp Med. 2013;8(2):102–109. doi: 10.1002/jhm.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hansen LO, Greenwald JL, Budnitz T, et al. Project BOOST: Effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421–427. doi: 10.1002/jhm.2054. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell SE, Gardiner PM, Sadikova E, et al. Patient activation and 30-day post-discharge hospital utilization. J Gen Intern Med. 2014;29(2):349–355. doi: 10.1007/s11606-013-2647-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hohmann C, Neumann-Haefelin T, Klotz JM, Freidank A, Radziwill R. Adherence to hospital discharge medication in patients with ischemic stroke: a prospective, interventional 2-phase study. Stroke. 2013;44(2):522–524. doi: 10.1161/STROKEAHA.112.678847. [DOI] [PubMed] [Google Scholar]
- 17.Daliri S, Bekker CL, Buurman BM, Scholte Op Reimer WJM, van den Bemt BJF, Karapinar-Çarkit F. Barriers and facilitators with medication use during the transition from hospital to home: a qualitative study among patients. BMC Health Serv Res. 2019;19(1):204. doi: 10.1186/s12913-019-4028-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balaban RB, Weissman JS, Samuel PA, Woolhandler S. Redefining and redesigning hospital discharge to enhance patient care: a randomized controlled study. J Gen Intern Med. 2008;23(8):1228–1233. doi: 10.1007/s11606-008-0618-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burke RE, Guo R, Prochazka AV, Misky GJ. Identifying keys to success in reducing readmissions using the ideal transitions in care framework. BMC Health Serv Res. 2014;14:423. doi: 10.1186/1472-6963-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coleman EA, Parry C, Chalmers S, Min S-J. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 21.White M, Garbez R, Carroll M, Brinker E, Howie-Esquivel J. Is “teach-back” associated with knowledge retention and hospital readmission in hospitalized heart failure patients? J Cardiovasc Nurs. 2013;28(2):137–146. doi: 10.1097/JCN.0b013e31824987bd. [DOI] [PubMed] [Google Scholar]
- 22.Oh EG, Lee HJ, Yang YL, Kim YM. Effectiveness of Discharge Education With the Teach-Back Method on 30-Day Readmission: A Systematic Review. J Patient Saf 13, 2019. doi:10.1097/PTS.0000000000000596 [DOI] [PubMed]
- 23.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 24.Howard-Anderson J, Busuttil A, Lonowski S, Vangala S, Afsar-Manesh N. From discharge to readmission: Understanding the process from the patient perspective. J Hosp Med. 2016;11(6):407–412. doi: 10.1002/jhm.2560. [DOI] [PubMed] [Google Scholar]
- 25.Auerbach AD, Kripalani S, Vasilevskis EE, et al. Preventability and Causes of Readmissions in a National Cohort of General Medicine Patients. JAMA Intern Med. 2016;176(4):484–493. doi: 10.1001/jamainternmed.2015.7863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prusaczyk B, Kripalani S, Dhand A. Networks of hospital discharge planning teams and readmissions. J Interprof Care. 2018;29:1–8. doi: 10.1080/13561820.2018.1515193. [DOI] [PubMed] [Google Scholar]
- 27.Hesselink G, Schoonhoven L, Plas M, Wollersheim H, Vernooij-Dassen M. Quality and safety of hospital discharge: a study on experiences and perceptions of patients, relatives and care providers. Int J Qual Health Care. 2013;25(1):66–74. doi: 10.1093/intqhc/mzs066. [DOI] [PubMed] [Google Scholar]
- 28.Waring J, Marshall F, Bishop S, et al.An Ethnographic Study of Knowledge Sharing across the Boundaries between Care Processes, Services and Organisations: The Contributions to “safe” Hospital Discharge. NIHR Journals Library; 2015. [PubMed]
- 29.Burke RE, Lawrence E, Ladebue A, et al. How Hospital Clinicians Select Patients for Skilled Nursing Facilities. J Am Geriatr Soc. 2017;65(11):2466–2472. doi: 10.1111/jgs.14954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Evanoff B, Potter P, Wolf L, Grayson D, Dunagan C, Boxerman S. Can We Talk? Priorities for Patient Care Differed Among Health Care Providers. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation (Volume 1: Research Findings). Agency for Healthcare Research and Quality (US); 2011. [PubMed]
- 31.Prystajecky M, Lee T, Abonyi S, Perry R, Ward H. A case study of healthcare providers’ goals during interprofessional rounds. J Interprof Care. 2017;31(4):463–469. doi: 10.1080/13561820.2017.1306497. [DOI] [PubMed] [Google Scholar]
- 32.Goldman J, Reeves S, Wu R, Silver I, MacMillan K, Kitto S. A sociological exploration of the tensions related to interprofessional collaboration in acute-care discharge planning. J Interprof Care. 2016;30(2):217–225. doi: 10.3109/13561820.2015.1072803. [DOI] [PubMed] [Google Scholar]
- 33.Bowles KH, Holland DE, Potashnik SL. Implementation and testing of interdisciplinary decision support tools to standardize discharge planning. NI 2012 (2012). 2012;2012:41. [PMC free article] [PubMed]
- 34.Huynh E, Basic D, Gonzales R, Shanley C. Structured interdisciplinary bedside rounds do not reduce length of hospital stay and 28-day re-admission rate among older people hospitalised with acute illness: an Australian study. Aust Health Rev. 2017;41(6):599–605. doi: 10.1071/AH16019. [DOI] [PubMed] [Google Scholar]
- 35.Woodcock T, Liberati EG, Dixon-Woods M. A mixed-methods study of challenges experienced by clinical teams in measuring improvement. BMJ Qual Saf 24, 2019. doi:10.1136/bmjqs-2018-009048 [DOI] [PMC free article] [PubMed]
- 36.Brashers V, Haizlip J, Owen JA. The ASPIRE Model: Grounding the IPEC core competencies for interprofessional collaborative practice within a foundational framework. J Interprof Care. 2020;34(1):128–132. doi: 10.1080/13561820.2019.1624513. [DOI] [PubMed] [Google Scholar]
- 37.Al Achkar M, Hanauer M, Colavecchia C, Seehusen DA. Interprofessional education in graduate medical education: survey study of residency program directors. BMC Med Educ. 2018;18(1):11. doi: 10.1186/s12909-017-1104-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clancy CM, Tornberg DN. TeamSTEPPS: Assuring Optimal Teamwork in Clinical Settings. Am J Med Qual. 2019;34(5):436–438. doi: 10.1177/1062860619873181. [DOI] [PubMed] [Google Scholar]
- 39.Mueller SK, Donzé J, Schnipper JL. Intern workload and discontinuity of care on 30-day readmission. Am J Med. 2013;126(1):81–88. doi: 10.1016/j.amjmed.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 40.Haferbecker D, Fakeye O, Medina SP, Fieldston ES. Perceptions of educational experience and inpatient workload among pediatric residents. Hosp Pediatr. 2013;3(3):276–284. doi: 10.1542/hpeds.2012-0068. [DOI] [PubMed] [Google Scholar]
- 41.Knutsen Glette M, Kringeland T, Røise O, Wiig S. Hospital physicians’ views on discharge and readmission processes: a qualitative study from Norway. BMJ Open. 2019;9(8):e031297. doi: 10.1136/bmjopen-2019-031297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 16 kb)