Abstract
A 9-year-old girl presented a large inflammatory cup-shaped scalp lesion with alopecia surrounded by pustules, dander, and suppuration associated with an occipital inflammatory lymphadenopathy for 1 month. Wood’s light exam was positive as well as KOH mount showing ectothrix type hair involvement. Hair and pus culture on Sabouraud dextrose agar (SDA) added with chloramphenicol and supplemented with cycloheximide isolated a dermatophyte species identified as Microsporum audouinii according to the colonies features. Species identification was confirmed by matrix-assisted laser desorption-ionization–time of flight mass spectrometry (MALDI–TOF MS) and the patient was treated for kerion celsi with terbinafine tablets 125 mg per day associated with a ketoconazole-based shampoo. The evolution was favorable, with hair regrowth after 2 months.
Keywords: Kerion celsi, Microsporum audouinii, terbinafine, tinea capitis
Introduction
Tinea capitis (TC) is a superficial mycosis of the scalp that may have a range of clinical manifestations from seborrheic-like scaling to highly inflamed lesions with deep, tender, and boggy plaques exuding pus known as kerion celsi (KC). 1 This later clinical appearance is the result of a severe inflammatory reaction to TC infections. 2 It is mainly caused by zoophilic dermatophytes such as Trichophyton mentagrophytes and T. verrucosum, 3 occasionally by Microsporum canis. Rarely, KC can be caused by anthropophilic dermatophytes.1,4 Here, we report a case of KC in an immunocompetent girl due to Microsporum audouinii — an anthropophilic dermatophyte.
Case description
This concerns a 9-year-old girl, a school pupil, with no particular medical history. She lives in a rural area of Kolda, a region located at the south in Senegal, with no contact with domestic animals or trauma. She is the oldest of four siblings, all living in apparent good health. First, she consulted a health post for a lesion on the scalp in form of suppurative plaques with alopecia lasting for 1 month. At the health post, she received a Griseofulvin-based treatment per os at 500 mg/day associated with flucloxacillin for 3 weeks. Following lack of improvement on this latter treatment, she was transferred to the dermatology clinic in Aristide Le Dantec University hospital in Dakar.
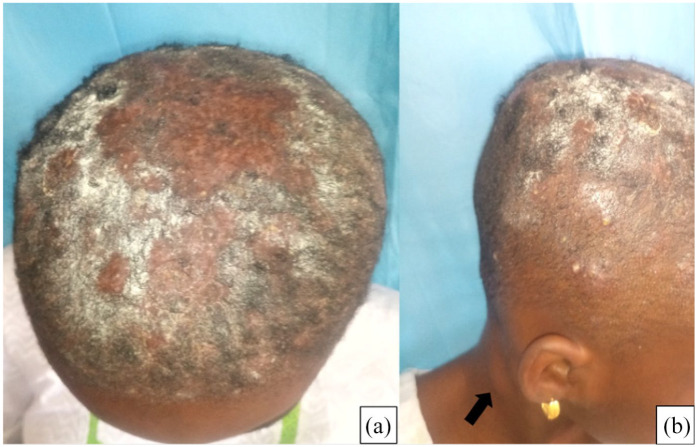
Upon clinical examination in our service, she presented a large inflammatory cup-shaped lesion with alopecia surrounded by pustules, dander, and suppuration in the areas of inflammation. Wood’s light examination was positive, showing a bright green fluorescence. The lesion was associated with an occipital inflammatory lymphadenopathy (Figure 1). She had no fever.
Figure 1.
Large inflammatory cup-shaped lesion with alopecia surrounded by (a) pustules and (b) inflammatory lymphadenopathy (black arrow).
The direct examination of the dander and hair sampled for mycological analysis showed ectothrix type hair involvement while bacterial analysis of the pus was sterile. After 10 days of culture at 25°C on Sabouraud dextrose agar (SDA) added with chloramphenicol and supplemented with cycloheximide, flat, spreading and greyish-white colonies with a dense suede-like to downy surface were isolated. These colonies were yellow-brown to reddish-brown in color on the front with a beige reverse. Under the microscope, a sterile mycelium producing only occasional thick-walled terminal or intercalary chlamydospores was visualized (Figure 2).
Figure 2.
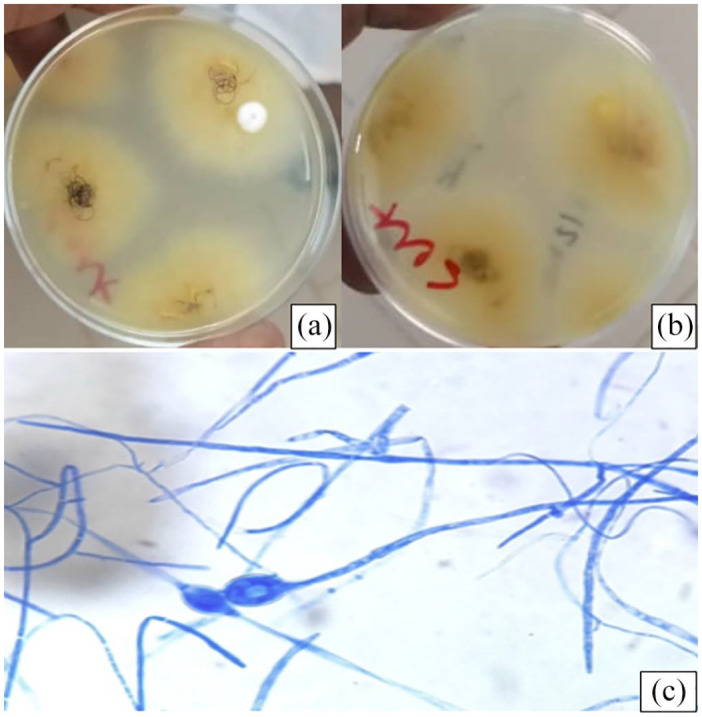
Colonies of Microsporum audouinii isolated from the scalp lesion. Colonies were yellow-brown to reddish-brown on the front (a) with a beige reverse (b) colonies showing sterile mycelium producing only occasional thick-walled terminal or intercalary chlamydospores (c).
Based on macroscopic and microscopic characteristics of these colonies, the identification of M. audouinii was retained. This identification was confirmed by matrix-assisted laser desorption-ionization – time of flight mass spectrometry (MALDI–TOF MS), at the IHU Méditerranée Infection in Marseilles, France.
In view of the severity of this clinical form and the identification of an anthropophilic dermatophyte strain, immunodeficiency was suspected and retroviral serology was investigated. This latter serology was negative. However, blood count revealed neutropenia at 1400/mm3.
Evacuation by manual compression under local anesthesia removed 50 ml of pus. Treatment based on terbinafine per os 125 mg/day associated with a ketoconazole-based shampoo was then started.
The evolution was favorable after 2 months, marked by complete clinical and mycological regression (Figure 3).
Figure 3.
Pictures comparing between the first week of visit in the dermatology service in Aristide Le Dantec University Hospital and the 8-week test-of-cure showing full recovery with early hair regrowth.
Discussion
TCs are contagious dermatophyte infections that affect preferentially children and teenagers. In Africa, TCs are a real health problem due to their endemic character, occurring mainly in school children and pre-school children. In Senegal, prevalence of TC was estimated at 34.51% between 2008 and 2013. 5
Different clinical aspects of TC are described depending to the causative species. Dermatophyte species may cause either ectothrix infection, in which spores cover the surface of the hair shaft, or endothrix infection, in which hyphae form arthrospores within the hair shaft. Examples of ectothrix infection agents are M. canis and M. audouinii while T. soudanense is an agent of endothrix infection. T. tonsurans causes endothrix hair invasion often referred to as “black-dot” because hairs break off close to the surface. 6 Favus is caused by T. schoenleinii and can lead, in the longer term, to scarring and hair loss after formation of a crust, or scutula, along the hair shaft from pus. Likewise, pus formation is also found in kerion, which is an inflammatory pustular folliculitis involving circumscribed scalp areas, most commonly caused by T. verrucosum and T. mentagrophytes.
Kerion represented 6.4% of TC in Italy and 12.8% in Tunisia in 1998 and in 2012, respectively.7,8 In Senegal, the study cited above by Ndiaye et al. published in 2015 showed a proportion of 5.3% for kerion among TC cases. 5 T. mentagrophytes was the main aetiologic agent with a proportion of 86.7% followed by T. erinacei and Nannizia gypsea (ex Microsporum gypseum) with 6.7% for each species. Clinically, KC is a suppurative and painful plaque associated with purulent drainage and regional lymphadenopathy. 9 It is generally localized. 10 However, the clinical form found in our patient with a large inflammatory cup-shaped lesion with alopecia surrounded by pustules is rare. A similar case was reported in China in 2011 with T. mentagrophytes as the causative agent. 11 This clinical aspect would seem from all points of view to be a pyogenic abscess.
Essentially, KC is caused by zoophilic dermatophytes that do not seem suited to humans such as T. mentagrophytes (domestic animals: horses), T. verrucosum (cattle), or M. canis (dogs, cats, rodents).12,13 Telluric dermatophytes are implicated rarely. A case of KC due to Nannizia gypsea was reported in 2016 in France. 14 Anthropophilic dermatophytes as M. audouinii are basically responsible for discrete forms of TC that are non-inflammatory. Nevertheless, the possibility that KC may be caused by M. audouinii, although unusual, should be considered. The first case of KC involving M. audouinii was reported in 1960 in Japan. 15 Another case implicating the same dermatophyte species was reported in 2013 in Portugal. 1
The visible disparities between different manifestations of the same underlying infection raise the question of whether all strains of M. audouinii present a similar virulence. Even drug resistance may be related to specific genotypes. Polymorphism of dermatophyte strains is significant and may reveal particular virulence factors, associated in particular to the expression of different proteinases and/or keratinases, an important subject to investigate in future research.16,17
The principal treatment of KC is prompt systemic therapy because topical agents do not penetrate the hair follicle.18,19 Griseofulvin is the treatment of choice for cases due to Microsporum spp. because of its safety. 20 However, as the patient had already been put on griseofulvin treatment without improvement, we opted to change to terbinafine – a broad-spectrum agent whose efficacy and safety have been demonstrated – which led to a good result in our patient.9,18
In conclusion, highly inflammatory cases of TC due to M. audouinii can also be seen, although a clinical pattern of highly inflammatory TC is not expected when anthropophilic agents are concerned. Hence, mycological diagnosis is important to avoid unnecessary surgical drainage.
Acknowledgments
We thank Pr Stéphane RANQUE, Institut Méditerranée Infection, Marseille, for his help with the MALDI-TOF MS device.
Footnotes
Author contributions: Khadim Diongue and Aminata Deh were responsible for the study design; Aminata Deh was involved in clinical management whereas Khadim Diongue was responsible for biological aspects. Khadim Diongue and Aminata Deh wrote the manuscript; Saer Diadie, Boubacar-Ahy Diatta, Khadim Diop, Niar Ndour, Maodo Ndiaye, Moussa Diallo, and Suzanne-Oumou Nianga revised the manuscript. All authors approved the final version of the manuscript.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical statement: This case was documented in accordance with the Declaration of Helsinki. This case was a hospital-based research conducted in the context of routine care. No approval was required. However, written informed consent was obtained from the legal guardian (the mother) for publication of this case report and accompanying images.
ORCID iD: Khadim Diongue  https://orcid.org/0000-0002-7033-1169
https://orcid.org/0000-0002-7033-1169
Contributor Information
Aminata Deh, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal.
Khadim Diongue, Service of Parasitology and Mycology, Faculty of Medicine, Pharmacy and Odontology, Cheikh Anta Diop University of Dakar, Avenue Cheikh Anta Diop, Dakar BO 3005, Senegal; Laboratory of Parasitology and Mycology, Aristide Le Dantec Hospital, Dakar, Senegal.
Saer Diadie, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal.
Boubacar-Ahy Diatta, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal.
Khadim Diop, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal.
Niar Ndour, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal.
Maodo Ndiaye, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal; Service of Dermatology and Venerology, Faculty of Medecine, Pharmacy and Odontology, Cheikh Anta Diop University of Dakar, Dakar BO 3005, Senegal.
Moussa Diallo, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal; Service of Dermatology and Venerology, Faculty of Medecine, Pharmacy and Odontology, Cheikh Anta Diop University of Dakar, Dakar BO 3005, Senegal.
Suzanne-Oumou Niang, Clinic of Dermatology, Aristide Le Dantec Hospital, Dakar, Senegal; Service of Dermatology and Venerology, Faculty of Medecine, Pharmacy and Odontology, Cheikh Anta Diop University of Dakar, Dakar BO 3005, Senegal.
References
- 1. Fernandes S, Amaro C, Martins ML, et al. Kerion caused by Microsporum audouinii in a child. Med Mycol Case Rep 2013; 2: 52–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Feetham JE, Sargant N. Kerion Celsi: a misdiagnosed scalp infection. Arch Dis Child 2016; 101: 503. [DOI] [PubMed] [Google Scholar]
- 3. Liu ZH, Zhang Y, Zhu J, et al. Successful treatment of severe kerion Celsi in an immunocompromised girl with evacuation of pus, terbinafine and short course glucocorticosteroids. J Mycol Med 2016; 26: 42–45. [DOI] [PubMed] [Google Scholar]
- 4. Proudfoot LE, Morris-Jones R. Kerion Celsi. N Engl J Med 2012; 366: 1142. [DOI] [PubMed] [Google Scholar]
- 5. Ndiaye M, Diongue K, Seck MC, et al. Profil épidémiologique des teignes du cuir chevelu à Dakar (Sénégal). Bilan d’une étude rétrospective de six ans (2008 - 2013). J Mycol Med 2015; 25: 169–176. [DOI] [PubMed] [Google Scholar]
- 6. Ghannoum MA, Isham NC. Dermatophytes and dermatophytoses. In: Dismukes WE, Pappas PG, Sobel JD. (eds) Clinical mycology. 2nd ed. New York: Oxford University Press, 2009. [Google Scholar]
- 7. Aste N, Pau M, Biggio P. Kerion Celsi: une étude épidémiologique clinique. Mycoses 1998; 41: 169–173. [DOI] [PubMed] [Google Scholar]
- 8. Chami I, Boudaya S, Meziou TJ, et al. Profil épidémio-clinique des teignes inflammatoires dans la région de Sfax (Tunisie). Annales de Dermatologie et de Vénéréologie 2012; 139: B254. DOI: 10.1016/j.annder.2012.10.457. [DOI] [Google Scholar]
- 9. Isa-Isa R, Arenas R, Isa M. Inflammatory tinea capitis: kerion, dermatophytic granuloma, and mycetoma. Clin Dermatol 2010; 28: 133–136. [DOI] [PubMed] [Google Scholar]
- 10. Rebollo N, López-Barcenas AP, Arenas R. Tinea capitis. Actas Dermosifiliogr 2008; 99: 91–100. [PubMed] [Google Scholar]
- 11. Jaspers GJ, Werrij BG, Jagtman BA, et al. Severe kerion celsi due to Trichophyton mentagrophytes: a case report. Acta Paediatrica 2011; 100: e181–e183. [DOI] [PubMed] [Google Scholar]
- 12. Elewski BE. Tinea capitis: a current perspective. J Am Acad Dermatol 2000; 42: 1–20. [DOI] [PubMed] [Google Scholar]
- 13. Patel GA, Schwartz RA. Tinea capitis: still an unsolved problem? Mycoses 2011; 54: 183–188. [DOI] [PubMed] [Google Scholar]
- 14. Hoarau G, Miquel J, Picot S. Kerion Celsi caused by Microsporum gypseum. J Pediatr 2016; 178: 296. [DOI] [PubMed] [Google Scholar]
- 15. Kutomi M, Nishikawa T, Nakayama H. A case of Kerion Celsi due to Microsporum audouinii. Journal japonais de mycologie médicale 1980; 21: 184–187. [Google Scholar]
- 16. Giddey K, Favre B, Quadroni M, et al. Closely related dermatophyte species produce different patterns of secreted proteins. FEMS Microbiol Lett 2007; 267: 95–101. [DOI] [PubMed] [Google Scholar]
- 17. Sharma R, Hoog S, Presber W, et al. A virulent genotype of Microsporum canis is responsible for the majority of human infections. J Med Microbiol 2007; 56: 1377–1385. [DOI] [PubMed] [Google Scholar]
- 18. Kakourou T, Uksal U. European society for pediatric dermatology. Guidelines for the management of tinea capitis in children. Pediatr Dermatol 2010; 27: 226–228. [DOI] [PubMed] [Google Scholar]
- 19. Higgins EM, Fuller LC, Smith CH. Guidelines for the management of tinea capitis. Br J Dermatol 2000; 143: 53–58. [DOI] [PubMed] [Google Scholar]
- 20. Gupta AK, Drummond-Main C. Meta-analysis of randomized, controlled trials comparing particular doses of griseofulvin and terbinafine for the treatment of tinea capitis. Pediatr Dermatol 2013; 30: 1–6. [DOI] [PubMed] [Google Scholar]