Key Points
Question
What is the best preoperative imaging modality for localization of primary hyperparathyroidism?
Findings
In this systematic review and network meta-analysis of direct comparative studies using 2 or more imaging modalities, choline positron emission tomography and computed tomography (PET-CT) clearly showed the best performance for localization of primary hyperparathyroidism in both patient-based and lesion-based analyses. Even in chronological analysis to investigate the changes in imaging methods over time, choline PET-CT showed the highest surface under the cumulative ranking curve value, followed by the CT category in patient-based analysis after 2010.
Meaning
This study suggests that choline PET-CT would be the best preoperative imaging modality for localization of primary hyperparathyroidism.
Abstract
Importance
Accurate preoperative localization of primary hyperparathyroidism (pHPT) is an important and challenging issue for a successful parathyroidectomy. Although new imaging modalities have been introduced during the past decade, direct comparative studies on advanced imaging techniques are limited.
Objective
To compare the performance of different preoperative imaging modalities for the localization of pHPT by performing a network meta-analysis (NMA).
Data Sources
PubMed, Embase, and the Cochrane Library were searched from the earliest available indexing date through September 28, 2020.
Study Selection
The inclusion criteria were diagnostic tests with sensitivities of 2 or more different preoperative imaging modalities for the same indivduals.
Data Extraction and Synthesis
Two researchers independently reviewed the literature according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension statement of health care intervention guidelines for network meta-analyses.
Main Outcomes and Measures
After classifying various imaging modalities into 8 representative imaging categories, the pooled estimation between the odds ratio and 95% credible intervals (CrIs) was calculated in the sensitivity for localization of pHPT. The surface under the cumulative ranking curve (SUCRA) values were obtained to calculate the probability of each imaging modality being the most effective diagnostic method.
Results
A total of 8495 patients from 119 direct comparative studies using 2 or more imaging modalities for localization of pHPT were included. The sensitivity of choline positron emission tomography and computed tomography (PET-CT) was significantly higher than that of technetium 99m sestamibi single-photon emission computed tomography (MIBI SPECT) in both patient-based and lesion-based analyses (patient-based analysis: odds ratio, 5.22; 95% CrI, 2.36-11.80; lesion-based analysis: odds ratio, 17.70; 95% CrI, 5.79-60.10). Among 8 representative imaging modality categories, choline PET-CT showed the highest SUCRA value in both patient-based and lesion-based analyses. In patient-based analysis after 2010, choline PET-CT showed the highest SUCRA value, followed by the CT category, although MIBI SPECT had the highest SUCRA value in analysis before 2009.
Conclusions and Relevance
The results from this network meta-analysis suggest that choline PET-CT showed the best performance in both patient-based and lesion-based analyses and that choline PET-CT would be the best preoperative imaging modality for localization of pHPT.
This systematic review and network meta-analysis compares the performance of different preoperative imaging modalities for localization of primary hyperparathyroidism.
Introduction
Surgical resection of abnormal parathyroid glands through neck exploration is the mainstay for curative treatment in patients with primary hyperparathyroidism (pHPT). Minimally invasive parathyroidectomy has recently become the standard surgical technique for pHPT with the help of image-guided focused exploration, which is associated with advantages in terms of operation time, length of hospital stay, cost, and patient satisfaction.1,2 Thus, a confident and accurate preoperative localization by noninvasive imaging studies is an important and challenging issue for successful parathyroidectomy.
Although ultrasonography (US) may be the most commonly used imaging modality in the preoperative setting of pHPT owing to its widespread availability, the sensitivity of US widely varies, with well-recognized operator-dependent properties.3 Parathyroid scintigraphy has historically been established as a preoperative localization technique for pHPT either with dual tracer subtraction, such as technetium (Tc) 99m sestamibi (MIBI)–Tc 99m pertechnetate, or dual phase of single tracer using MIBI. With the development of tomographic imaging and hybrid technology, single-photon emission computed tomography (SPECT) combined with computed tomography (CT) using MIBI showed better results than SPECT or planar scintigraphy in localizing pHPT lesions.4,5
Four-dimensional CT (4D-CT) using the unique perfusion characteristics of the parathyroid lesion is a new imaging modality for localization of pHPT that showed more accurate results compared with both US and MIBI SPECT.3 Positron emission tomography (PET) is another state-of-the-art imaging technology that provides functional information like scintigraphy with better spatial resolution. Positron emission tomography–CT with carbon 11–labeled methionine (MET) or F 18 fluorocholine (FCH) showed high diagnostic performance and is considered a promising imaging modality for localization of pHPT.6 Recently, radiolabeled choline (FCH or carbon 11–labeled choline [CCH]) PET-CT has shown excellent diagnostic performance, making it an ideal replacement for other current imaging methods.7,8 However, to our knowledge, there is no meta-analysis comparing the results of each advanced imaging modality, such as FCH PET-CT, MET PET-CT, or 4D-CT, for localization of pHPT, and direct comparative studies are also limited.
This study aimed to investigate and compare the performance of different preoperative imaging modalities for localization of pHPT by performing a network meta-analysis (NMA) using published direct comparison studies with 2 or more imaging modalities to provide more evidence-based data for guidelines on the appropriate use of these imaging modalities for patients with pHPT. Additional NMA was performed by separating studies before 2009 and those after 2010 to investigate the changes in imaging technology over time.
Methods
This systematic review and NMA was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extension statement for NMA of health care intervention guidelines.9,10
Data Sources and Search Strategy
We conducted electronic English-language literature searches on PubMed, Embase, and Cochrane Library databases for human clinical research from the earliest available indexing date through September 28, 2020. Moreover, we manually searched the reference lists of identified publications for additional studies. The search strategy included both subject headings (MeSH terms) and keywords for the target condition (pHPT), imaging techniques, and outcomes (eTable 1 in the Supplement). We used a search algorithm based on a combination of the following terms: (1) “primary hyperparathyroidism” OR “parathyroid adenoma” and (2) “positron emission tomography” OR “PET” OR “single photon emission computed tomography” OR “SPECT” OR “scintigraphy” OR “scan” OR “ultrasonography” OR “ultrasound” OR “US” OR “computed tomography” OR “CT” OR “magnetic resonance imaging” OR “MRI” and (3) “detection” OR “localization” OR “diagnosis.” The same search formula was adopted for the Embase search using Emtree terms.
Inclusion and Exclusion Criteria for Study Selection
The inclusion criteria for relevant studies were as follows: (1) the study design should be diagnostic tests; (2) the patient population should be consisted of individuals with pHPT; (3) the index test should be noninvasive imaging methods in a preoperative setting; (4) the sensitivity of 2 or more different imaging modalities for localization of pHPT should be compared for the same individuals; and (5) histopathologic analysis should be available as a reference standard. Duplicated publications were excluded, as were publications such as case reports, review articles, meta-analyses, letters, and short communications, which do not contain original data. In addition, articles were excluded if there were no direct comparison data, fewer than 10 participants, or insufficient data for sensitivity calculation. Two of us (S.-W.L. and S.-J.K.) independently reviewed the titles and abstracts of the retrieved articles, applying the mentioned selection criteria. The same researchers independently evaluated the full texts of the included articles to assess their eligibility for inclusion in the present review.
Data Extraction and Quality Assessment
Data on the following aspects were collected: basic study information (first author, year of publication, and country of study conducted), study design (prospective or retrospective), patient characteristics (number, mean age, and sex of patients), analysis method (patient-based or lesion-based analysis), and technical aspects. Each study was analyzed to retrieve the sensitivity of each preoperative imaging modality for localization of pHPT according to the reference standard. Only studies with such complete information were included in the meta-analysis. The overall quality of the included studies in this review was critically appraised by 2 of us (S.-W.L. and S.-J.K.) and independently based on the 15-item modified Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2).11 Discrepancies were resolved by discussion. The QUADAS-2 includes the following domains: patient selection, reference standard, index text, flow of patients through the study, timing of index tests, and a relevant reference standard. Review Manager, version 5.4.1 (Cochrane Collaboration) was used to assess the quality. Publication bias was explained by funnel plots. Asymmetry findings in funnel plots indicate publication bias.
Data Synthesis and Statistical Analysis
Network meta-analysis was performed for different imaging modalities that were used for preoperative localization of pHPT. To reduce the number of treatments, various imaging modalities were classified into 8 representative imaging categories, and then NMA was performed for the different imaging categories in both patient-based and lesion-based analyses. In addition, NMA was performed by separating studies before 2009 and those after 2010 in chronological order to investigate the changes in imaging methods over time.
A direct comparison of various treatment methods was conducted using a traditional pairwise meta-analysis, and the results showed the pooled estimation between the odds ratio (OR) and 95% credible intervals (CrIs) in the sensitivity for localization of pHPT. Heterogeneity was analyzed by the χ2 test and the I2 statistic.12,13 Bayesian NMA and specific graphical analysis were performed with the “gemtc” package in R, version 3.6.0 software (R Group for Statistical Computing) and Stata, version 13.1 software (StataCorp LLC) according to previous reports.14,15 In the outcome models of both patient-based and lesion-based NMAs, we selected the random-effects model that had 4 chains, 5000 burn-ins, 10 000 iterations, and an interval of 1 to sufficiently remove the effect of the initial values, increase the iterations and extraction interval, and minimize the Markov chain Monte Carlo error and deviance information criterion variation, with almost no variations and stability of various plots.16,17 Consistency was evaluated by examining the agreement between the direct and indirect treatment effects. A consistency test in the assumptions of NMA is a critical tool that assesses the applicability of NMA results. The node-splitting analysis method was used to assess the presence of inconsistency for any treatment contrast in the network because it evaluates whether the direct evidence and indirect evidence for a particular node are consistent.18 To provide assistance in the interpretation of ORs, the surface under the cumulative ranking curve (SUCRA) was used to calculate the probability of each imaging category being the most effective diagnostic method based on a bayesian approach using probability values. The larger the SUCRA value, the better the rank of intervention.19,20
Results
Literature Search and Selection of Studies
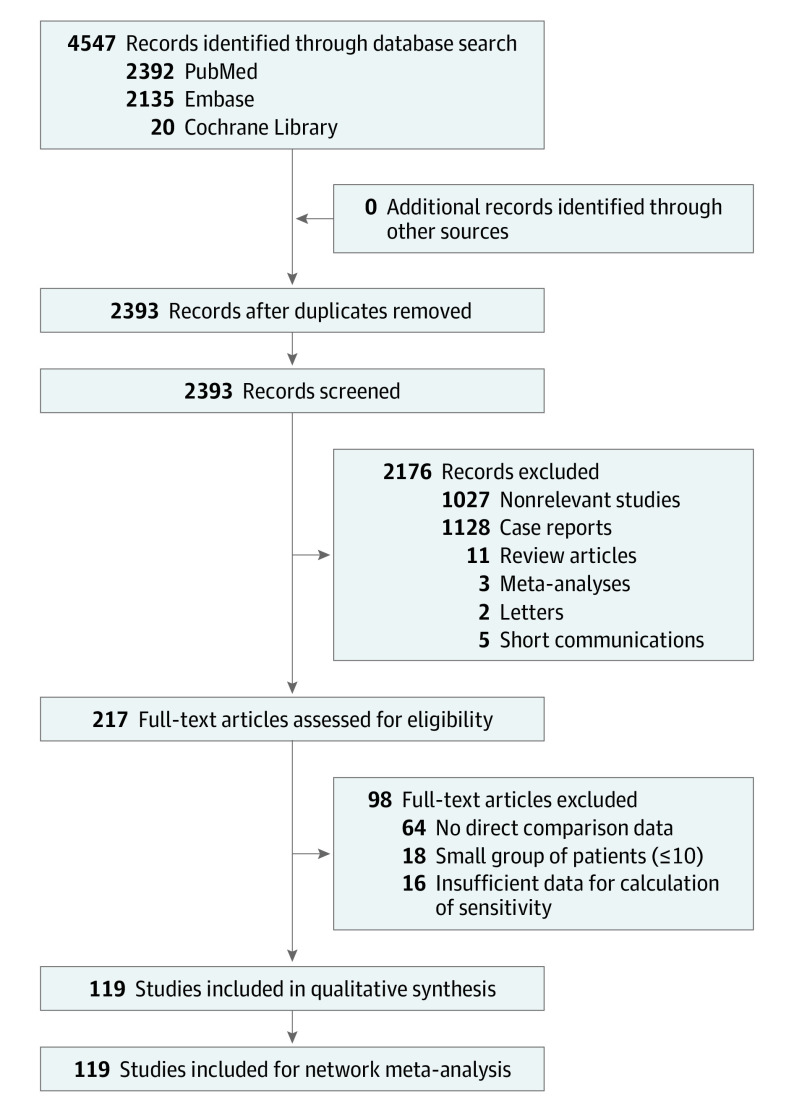
We identified 2392 articles from PubMed, 2135 articles from Embase, and 20 articles from the Cochrane Library through comprehensive electronic literature searches and cross-check of reference lists; 2154 duplicate records among these were excluded. Among the remaining 2393 records, 2176 records (1027 nonrelevant articles to this meta-analysis, 1128 case reports, 11 review articles, 3 meta-analyses, 2 letters, and 5 short communications) were excluded by reviewing the titles and abstracts. The eligibility of the remaining 217 full-text articles was evaluated based on their presentation of sufficient direct comparison data on the performance of 2 or more imaging modalities for localization of pHPT. A total of 119 articles were finally selected for this NMA. A list of the 119 included studies and their main characteristics are presented in eTable 2 in the Supplement. The flow of study selection is presented in Figure 1.
Figure 1. Flowchart of the Literature Search.
Databases were searched for eligible direct comparison studies on the performance of 2 or more noninvasive preoperative imaging modalities for localization of primary parahyperthyroidism.
Baseline Characteristics of Included Studies
A total of 8495 patients from 119 direct comparison studies using 2 or more noninvasive preoperative imaging modalities for localization of pHPT were included. Of 119 studies, 48 were performed in a prospective manner. The sensitivity on a per-patient–based analysis was available in 84 studies (Table 1),21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104 whereas the sensitivity on a per-lesion–based analysis was available in 39 studies (Table 2).23,34,37,42,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139 Of the 84 patient-based studies, 47 were reported before 2009, and 37 were reported after 2010. Additional NMA was performed by separating studies before 2009 and those after 2010 to investigate the changes in imaging methods over time.
Table 1. Patient-Based Sensitivities of Each Imaging Modality Category for Localization of Primary Hyperparathyroidism.
| Source | Imaging modalitya | Choline PET-CT, % | MET PET-CT, % | MIBI SPECT, % | MIBI planar, % | Dual tracer, % | US, % | CT, % | MRI, % |
|---|---|---|---|---|---|---|---|---|---|
| Juweid et al,21 2020 | MIBI pinhole vs DT (MIBI-Tc) | NA | NA | NA | 82.4 | 91.2 | NA | NA | NA |
| Okudan et al,22 2019 | MIBI SPECT-CT vs US | NA | NA | 92.8 | NA | NA | 76.0 | NA | NA |
| Parra Ramírez et al,23 2019 | MIBI SPECT vs CE-US | NA | NA | 72.4 | NA | NA | 69.0 | NA | NA |
| Vitetta et al,24 2019 | MIBI planar vs CDHR-US | NA | NA | NA | 71.3 | NA | 89.0 | NA | NA |
| Borumandi et al,25 2019 | MIBI SPECT vs US | NA | NA | 92.2 | NA | NA | 80.0 | NA | NA |
| Bossert et al,26 2019 | FCH PET-CT vs DT (MIBI-Tc) vs US | 88.2 | NA | NA | NA | 17.6 | 82.4 | NA | NA |
| Piccardo et al,27 2019 | FCH PET-CT vs 4D-CT | 80.6 | NA | NA | NA | NA | NA | 74.2 | NA |
| Scattergood et al,28 2019 | MIBI planar vs US | NA | NA | NA | 64.4 | NA | 69.9 | NA | NA |
| Vu et al,29 2019 | MIBI SPECT vs 4D-CT | NA | NA | 67.7 | NA | NA | NA | 87.1 | NA |
| Khafif et al,30 2019 | FCH PET-MRI vs MIBI SPECT vs US | 84.2 | NA | 73.7 | NA | NA | 84.2 | NA | NA |
| Asseeva et al,31 2019 | DT (MIBI-I) pinhole and SPECT-CT vs US | NA | NA | NA | NA | 93.1 | 91.7 | NA | NA |
| Zajíčková et al,32 2018 | FCH PET-CT vs MIBI SPECT-CT vs US | 92.3 | NA | 30.8 | NA | NA | 23.1 | NA | NA |
| Argirò et al,33 2018 | MIBI SPECT vs US vs 3T-MRI | NA | NA | 82.6 | NA | NA | 89.1 | NA | 97.8 |
| Beheshti et al,34 2018 | FCH PET-CT vs MIBI and TF SPECT-CT | 92.7 | NA | 61.0 | NA | NA | NA | NA | NA |
| Hiebert et al,35 2018 | MIBI SPECT-CT vs US vs DE-CT | NA | NA | 65.6 | NA | NA | 40.9 | 83.9 | NA |
| Araz et al,36 2018 | FCH PET-CT vs MIBI SPECT-CT | 95.8 | NA | 79.2 | NA | NA | NA | NA | NA |
| Thanseer et al,37 2017 | FCH PET-CT vs MIBI planar vs US | 100 | NA | NA | 80.7 | NA | 69.3 | NA | NA |
| Tunca et al,38 2017 | MIBI SPECT vs US | NA | NA | 89.1 | NA | NA | 82.0 | NA | NA |
| Frank et al,39 2017 | MIBI SPECT-CT vs 3D-US | NA | NA | 90.4 | NA | NA | 92.3 | NA | NA |
| Seyednejad et al,40 2016 | MIBI SPECT-CT vs US vs DE-CT | NA | NA | 90.0 | NA | NA | 58.3 | 90.0 | NA |
| Tan et al,41 2016 | MIBI planar vs US | NA | NA | NA | 63.8 | NA | 72.4 | NA | NA |
| Galvin et al,42 2016 | MIBI SPECT-CT vs 4D-CT | NA | NA | 47.5 | NA | NA | NA | 80.0 | NA |
| Brown et al,43 2015 | MIBI SPECT-CT vs US vs 4D-CT | NA | NA | 70.1 | NA | NA | 48.5 | 91.8 | NA |
| Hayakawa et al,44 2015 | MET PET-CT vs MIBI SPECT-CT vs MIBI planar | NA | 65.2 | 60.9 | 60.9 | NA | NA | NA | NA |
| Michaud et al,45 2015 | FCH PET-CT vs DT (MIBI-I) vs US | 90.9 | NA | NA | NA | 90.9 | 54.5 | NA | NA |
| Guerin et al,46 2015 | DT (MIBI-I) pinhole-SPECT vs US | NA | NA | NA | NA | 93.3 | 84.4 | NA | NA |
| Noda et al,47 2014 | MIBI planar vs US | NA | NA | NA | 75.4 | NA | 77.0 | NA | NA |
| Orevi et al,48 2014 | CCH PET-CT vs MIBI SPECT-CT | 92.3 | NA | 88.5 | NA | NA | NA | NA | NA |
| Ersoy et al,49 2014 | MIBI planar vs E-US | NA | NA | NA | 77.8 | NA | 97.8 | NA | NA |
| Schalin-Jäntti et al,50 2013 | MET PET-CT vs MIBI SPECT-CT vs DT (MIBI-I) | NA | 78.9 | 26.3 | NA | 63.2 | NA | NA | NA |
| Kwon et al,51 2013 | MIBI planar vs US | NA | NA | NA | 92.2 | NA | 93.1 | NA | NA |
| Kim et al,52 2012 | MIBI SPECT-CT vs MIBI planar | NA | NA | 100 | 62.5 | NA | NA | NA | NA |
| Aschenbach et al,53 2012 | MIBI planar vs dMRA | NA | NA | NA | 80.0 | NA | NA | NA | 93.3 |
| Akbaba et al,54 2012 | MIBI SPECT vs MIBI planar vs US vs MRI | NA | NA | 75.5 | 70.2 | NA | 87.2 | NA | 63.8 |
| Grayev et al,55 2012 | MIBI planar vs 3T-MRI | NA | NA | NA | 72.0 | NA | NA | NA | 64.0 |
| Adler et al,56 2011 | MIBI planar vs US | NA | NA | NA | 63.5 | NA | 58.4 | NA | NA |
| Patel et al,57 2010 | MIBI SPECT-CT vs US | NA | NA | 89.8 | NA | NA | 64.4 | NA | NA |
| Prommegger et al,58 2009 | MIBI SPECT-CT vs CT | NA | NA | 88.7 | NA | NA | NA | 68.8 | NA |
| Thomas et al,59 2009 | MIBI SPECT vs MIBI planar | NA | NA | 66.7 | 41.7 | NA | NA | NA | NA |
| Tresoldi et al,60 2009 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 67.7 | 81.3 | NA | NA |
| Tublin et al,61 2009 | MIBI SPECT vs US | NA | NA | 58.3 | NA | NA | 74.3 | NA | NA |
| Tang et al,62 2008 | MET PET-CT vs MIBI SPECT | NA | 90.9 | 90.9 | NA | NA | NA | NA | NA |
| Ansquer et al,63 2008 | MIBI SPECT vs DT (MIBI-Tc) vs US | NA | NA | 79.6 | NA | 91.8 | 57.1 | NA | NA |
| Boudreaux et al,64 2007 | MIBI planar vs US | NA | NA | NA | 58.1 | NA | 64.6 | NA | NA |
| Prasannan et al,65 2007 | MIBI planar vs S-US | NA | NA | NA | 79.1 | NA | 81.7 | NA | NA |
| Lavely et al,66 2007 | MIBI SPECT-CT vs MIBI planar | NA | NA | 73.0 | 56.5 | NA | NA | NA | NA |
| Ruf et al,67 2007 | MIBI SPECT-CT vs MIBI planar | NA | NA | 92.3 | 76.9 | NA | NA | NA | NA |
| Lo et al,68 2007 | MIBI planar vs US | NA | NA | NA | 89.5 | NA | 57.1 | NA | NA |
| Steward et al,69 2006 | MIBI planar vs S-US | NA | NA | NA | 57.7 | NA | 86.6 | NA | NA |
| Barczynski et al,70 2006 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 84.5 | 87.3 | NA | NA |
| Saeed et al,71 2006 | MIBI planar vs MRI | NA | NA | NA | 65.4 | NA | NA | NA | 73.1 |
| Krausz et al,72 2006 | MIBI SPECT-CT vs MIBI planar | NA | NA | 91.7 | 91.7 | NA | NA | NA | NA |
| Solorzano et al,73 2006 | MIBI SPECT vs S-US | NA | NA | 77.0 | NA | NA | 76.5 | NA | NA |
| Lorberboym et al,74 2005 | MIBI SPECT vs DT (MIBI-Tc) | NA | NA | 95.1 | NA | 68.3 | NA | NA | NA |
| Masatsugu et al,75 2005 | MIBI planar vs US | NA | NA | NA | 83.0 | NA | 71.3 | NA | NA |
| Ruf et al,76 2004 | MIBI SPECT vs MRI | NA | NA | 76.5 | NA | NA | NA | NA | 64.7 |
| Schachter et al,77 2004 | MIBI SPECT vs DT (MIBI-Tc) | NA | NA | 96.3 | NA | 78.0 | NA | NA | NA |
| Saint Marc et al,78 2004 | MIBI planar vs US | NA | NA | NA | 79.7 | NA | 64.7 | NA | NA |
| Lumachi et al,79 2004 | DT (MIBI-Tc) vs CT | NA | NA | NA | NA | 86.0 | NA | 88.4 | NA |
| Lumachi et al,80 2003 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 84.1 | 77.8 | NA | NA |
| Lorberboym et al,81 2003 | MIBI SPECT vs MIBI planar vs DT (MIBI-Tc) | NA | NA | 96.2 | 59.6 | 78.8 | NA | NA | NA |
| Prager et al,82 2003 | MIBI SPECT vs US | NA | NA | 86.3 | NA | NA | 78.6 | NA | NA |
| Leslie et al,83 2002 | MIBI planar vs DT (MIBI-Tc) | NA | NA | NA | 72.1 | 85.3 | NA | NA | NA |
| Haber et al,84 2002 | DT (MIBI-I) vs US | NA | NA | NA | NA | 82.4 | 74.3 | NA | NA |
| Berczi et al,85 2002 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 93.4 | 70.7 | NA | NA |
| Scheiner et al,86 2001 | MIBI SPECT vs US | NA | NA | 67.7 | NA | NA | 64.5 | NA | NA |
| Casara et al,87 2001 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 91.6 | 81.8 | NA | NA |
| Prager et al,88 2001 | MIBI SPECT vs US | NA | NA | 82.6 | NA | NA | 84.7 | NA | NA |
| Feingold et al,89 2000 | MIBI SPECT vs US | NA | NA | 78.0 | NA | NA | 90.5 | NA | NA |
| Krausz et al,90 2000 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 75.3 | 66.2 | NA | NA |
| Lumachi et al,91 2000 | DT (MIBI-Tc) vs US | NA | NA | NA | NA | 86.8 | 80.5 | NA | NA |
| Gallowitsch et al,92 2000 | TF SPECT vs DT (TF-Tc) vs US | NA | NA | 87.0 | NA | 87.0 | 78.3 | NA | NA |
| Moka et al,93 2000 | MIBI SPECT vs DT (MIBI-Tc) | NA | NA | 94.6 | NA | 87.0 | NA | NA | NA |
| Moka et al,94 2000 | MIBI SPECT vs DT (MIBI-Tc) | NA | NA | 96.8 | NA | 80.6 | NA | NA | NA |
| Hiromatsu et al,95 2000 | DT (TF-Tc) vs US vs CT vs MRI | NA | NA | NA | NA | 95.0 | 85.0 | 85.0 | 85.0 |
| Catargi et al,96 1999 | DT (MIBI-Tc) vs E-US | NA | NA | NA | NA | 71.4 | 71.4 | NA | NA |
| Hewin et al,97 1997 | DT (Tl-Tc) vs US vs MRI | NA | NA | NA | NA | 59.6 | 38.3 | NA | 72.3 |
| Fayet et al,98 1997 | MIBI planar vs MRI | NA | NA | NA | 82.4 | NA | NA | NA | 88.2 |
| Bonjer et al,99 1997 | MIBI planar vs US | NA | NA | NA | 81.0 | NA | 72.2 | NA | NA |
| Rauth et al,100 1996 | MIBI planar vs DT (Tl-Tc) | NA | NA | NA | 92.9 | 57.1 | NA | NA | NA |
| Light et al,101 1996 | MIBI planar vs US | NA | NA | NA | 86.7 | NA | 57.1 | NA | NA |
| Udén et al,102 1990 | DT (Tl-Tc) vs US vs CT | NA | NA | NA | NA | 56.0 | 50.0 | 70.0 | NA |
| Auffermann et al,103 1988 | DT (Tl-Tc) vs US vs MRI | NA | NA | NA | NA | 70.0 | 55.0 | NA | 85.0 |
| Peck et al,104 1987 | DT (Tl-Tc) vs MRI | NA | NA | NA | NA | 61.1 | NA | NA | 66.7 |
Abbreviations: CCH, carbon 11–labeled choline; CDHR-US, high-resolution US with color Doppler; CE-US, contrast-enhanced US; CT, computed tomography; DE-CT, dual-energy CT; dMRA, dynamic magnetic resonance angiography; DT, dual tracer; E-US, endoscopic US; FCH, F 18 fluorocholine; I, iodine 123; MET, carbon 11–labeled methionine; MIBI, technetium 99m sestamibi; MRI, magnetic resonance imaging; NA, not applicable; PET, positron emission tomography; S-US, surgeon-performed US; SPECT, single-photon emission computed tomography; Tc, technetium 99m pertechnetate; TF, technetium 99m tetrofosmin; Tl, thallium 201; US, ultrasonography; 3D-US, 3-dimensional US; 4D-CT, 4-dimensional CT.
Imaging modalities without available direct comparison data were excluded. Choline PET-CT includes FCH PET-CT, FCH PET-MRI, and CCH PET-CT; MIBI SPECT includes MIBI SPECT-CT, MIBI pinhole SPECT, MIBI SPECT and contrast-enhanced CT, TF SPECT, and TF SPECT-CT; MIBI planar includes MIBI pinhole-TF planar; dual tracer includes MIBI-Tc subtraction, MIBI-I subtraction, TF-Tc subtraction, and Tl-Tc subtraction with planar, pinhole, SPECT, or SPECT-CT; US includes CE-US, CDHR-US, 3D-US, E-US, and S-US; CT includes 4D-CT and DE-CT; and MRI includes 3T-MRI and dMRA.
Table 2. Lesion-Based Sensitivities of Each Imaging Modality Category for Localization of Primary Hyperparathyroidism.
| Source | Imaging modalitya | Choline PET-CT, % | MET PET-CT, % | MIBI SPECT, % | MIBI planar, % | Dual tracer, % | US, % | CT, % | MRI, % |
|---|---|---|---|---|---|---|---|---|---|
| Cuderman et al,105 2020 | FCH PET-CT vs MIBI SPECT-CT vs MIBI planar vs DT (MIBI-Tc) | 93.1 | NA | 55.7 | 38.9 | 41.2 | NA | NA | NA |
| Parra Ramírez et al,23 2019 | MIBI SPECT vs CE-US | NA | NA | 67.7 | NA | NA | 71.0 | NA | NA |
| Yeh et al,106 2019 | MIBI SPECT-CT vs 4D-CT | NA | NA | 58.0 | NA | NA | NA | 79.3 | NA |
| Amadou et al,107 2019 | FCH PET-CT vs MIBI planar vs US | 95.8 | NA | NA | 50.0 | NA | 54.2 | NA | NA |
| Beheshti et al,34 2018 | FCH PET-CT vs MIBI and TF SPECT-CT | 93.7 | NA | 60.8 | NA | NA | NA | NA | NA |
| Cunha-Bezerra et al,108 2018 | MIBI planar vs US vs 4D-CT | NA | NA | NA | 42.9 | NA | 38.1 | 61.9 | NA |
| Thanseer et al,37 2017 | FCH PET-CT vs MIBI planar vs US | 100 | NA | NA | 76.4 | NA | 69.3 | NA | NA |
| Krakauer et al,109 2016 | MIBI planar vs DT (MIBI-I) vs 4D-CT | NA | NA | NA | 64.9 | 92.8 | NA | 57.7 | NA |
| Galvin et al,42 2016 | MIBI SPECT-CT vs 4D-CT | NA | NA | 43.1 | NA | NA | NA | 76.5 | NA |
| Heiba et al,110 2015 | MIBI SPECT-CT vs MIBI pinhole vs DT (MIBI-I) SPECT-CT | NA | NA | 68.0 | 18.3 | 92.8 | NA | NA | NA |
| Suh et al,111 2015 | MIBI SPECT-CT vs US vs 4D-CT | NA | NA | 84.2 | NA | NA | 84.2 | 92.1 | NA |
| Berner et al,112 2015 | DT (MIBI-Tc) SPECT-CT vs US | NA | NA | NA | NA | 70.6 | 60.3 | NA | NA |
| Ozkaya et al,113 2015 | MIBI SPECT vs US | NA | NA | 85.3 | NA | NA | 72.5 | NA | NA |
| D’Agostino et al,114 2013 | DT (MIBI-I) SPECT-CT vs CT | NA | NA | NA | NA | 65.5 | NA | 58.6 | NA |
| Shafiei et al,115 2012 | MIBI SPECT-CT vs MIBI planar | NA | NA | 77.6 | 59.2 | NA | NA | NA | NA |
| Agha et al,116 2012 | MIBI planar vs CE-US vs MRI | NA | NA | NA | 80.6 | NA | 100 | NA | 71.0 |
| Eichhorn-Wharry et al,117 2011 | MIBI SPECT vs 4D-CT | NA | NA | 50.0 | NA | NA | NA | 61.6 | NA |
| Ho Shon et al,118 2008 | MIBI SPECT vs MIBI pinhole vs DT (MIBI-Tc) SPECT | NA | NA | 53.8 | 80.8 | 65.4 | NA | NA | NA |
| Nichols et al,119 2008 | MIBI SPECT vs MIBI planar vs DT (MIBI-Tc) pinhole | NA | NA | 83.0 | 83.5 | 80.1 | NA | NA | NA |
| Carlier et al,120 2008 | MIBI pinhole SPECT vs DT (MIBI-Tc) vs US | NA | NA | 87.3 | NA | 76.4 | 50.9 | NA | NA |
| Taïeb et al,121 2007 | MIBI SPECT vs DT (MIBI-I) pinhole vs US | NA | NA | 77.8 | NA | 86.1 | 77.8 | NA | NA |
| Rodgers et al,122 2006 | MIBI SPECT-CT vs US vs 4D-CT | NA | NA | 32.8 | NA | NA | 29.7 | 70.3 | NA |
| Kebapci et al,123 2004 | MIBI planar vs US | NA | NA | NA | 73.2 | NA | 83.9 | NA | NA |
| Wakamatsu et al,124 2003 | MIBI planar vs DT (MIBI-I) vs US vs MRI | NA | NA | NA | 37.8 | 51.1 | 46.7 | NA | 42.2 |
| Wakamatsu et al,125 2001 | DT (TF-Tc, MIBI-Tc, Tl-Tc) vs US vs MRI | NA | NA | NA | NA | 50.0 | 50.0 | NA | 48.5 |
| Ho Shon et al,126 2001 | MIBI planar vs DT (MIBI-Tc) | NA | NA | NA | 75.6 | 88.5 | NA | NA | NA |
| De Feo et al,127 2000 | MIBI planar vs US vs CT vs MRI | NA | NA | NA | 70.8 | NA | 66.7 | NA | 50.0 |
| Takami et al,128 1999 | MIBI planar vs DT (Tl-Tc) vs US vs CT | NA | NA | NA | 90.7 | 63.0 | 85.2 | 55.6 | NA |
| Gallowitsch et al,129 1997 | TF SPECT vs TF planar vs US | NA | NA | 94.4 | 69.4 | NA | 72.2 | NA | NA |
| Chen et al,130 1997 | MIBI SPECT vs MIBI planar vs DT (MIBI-Tc) | NA | NA | 80.3 | 78.9 | 74.3 | NA | NA | NA |
| Arkles et al,131 1996 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 81.0 | 76.0 | NA | NA |
| Liou et al,132 1996 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 87.5 | 75.0 | NA | NA |
| Billy et al,133 1995 | MIBI planar vs US | NA | NA | NA | 83.3 | NA | 50.0 | NA | NA |
| Gallacher et al,134 1993 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 41.7 | 37.5 | NA | NA |
| Whelan et al,135 1989 | US vs MRI | NA | NA | NA | NA | NA | 50.0 | NA | 65.0 |
| Summers et al,136 1989 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 59.0 | 53.8 | NA | NA |
| Roses et al,137 1989 | DT (Tl-Tc) vs US vs CT | NA | NA | NA | NA | 48.8 | 34.1 | 41.5 | NA |
| Gooding et al,138 1986 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 77.3 | 81.8 | NA | NA |
| Winzelberg et al,139 1985 | DT (Tl-Tc) vs US | NA | NA | NA | NA | 91.7 | 75.0 | NA | NA |
Abbreviations: CE-US, contrast enhanced ultrasonography; CT, computed tomography; DT, dual tracer; FCH, F 18 fluorocholine; I, iodine 123; MET, carbon 11–labeled methionine; MIBI, technetium 99m sestamibi; MRI, magnetic resonance imaging; NA, not applicable; PET, positron emission tomography; SPECT, single-photon emission computed tomography; Tc, technetium 99m pertechnetate; TF, technetium 99m tetrofosmin; Tl, thallium 201; US, ultrasonography; 4D-CT, 4-dimensional CT.
Imaging modalities without available direct comparison data were excluded. MIBI SPECT includes MIBI SPECT-CT, MIBI pinhole SPECT, MIBI SPECT and contrast-enhanced CT, TF SPECT, and TF SPECT-CT; MIBI planar includes MIBI pinhole-TF planar; dual tracer includes MIBI-Tc subtraction, MIBI-I subtraction, TF-Tc subtraction, and Tl-Tc subtraction with planar, pinhole, SPECT, or SPECT-CT; US includes CE-US; and CT includes 4D-CT.
To reduce the number of treatments, various imaging modalities were classified into 8 representative imaging categories as follows: (1) choline PET-CT, including FCH PET-CT, FCH PET–magnetic resonance imaging (MRI), and CCH PET-CT; (2) MET PET-CT; (3) MIBI SPECT, including MIBI SPECT-CT, MIBI pinhole SPECT, MIBI SPECT–contrast-enhanced CT, Tc 99m tetrofosmin (TF) SPECT, and TF SPECT-CT; (4) MIBI planar, including MIBI pinhole and TF planar; (5) dual tracer, including MIBI-Tc subtraction, MIBI–iodine 123 subtraction, TF-Tc subtraction, and thallium 201–Tc subtraction with planar, pinhole, SPECT, or SPECT-CT; (6) US, including contrast-enhanced US, high-resolution US with color Doppler, 3-dimensional US, endoscopic US, and surgeon-performed US; (7) CT, including 4D-CT and dual-energy CT (DE-CT); and (8) MRI, including 3T-MRI and dynamic magnetic resonance angiography.
Quality Assessment and Publication Bias
The summary of the risk of bias and applicability concerns based on the 15-item QUADAS-2 is presented in eFigure 1 in the Supplement. The overall quality of the included studies was deemed satisfactory.
The statistical approaches for the publication bias in 119 studies by funnel plots are shown in eFigure 2 in the Supplement. In both outcome models of patient-based and lesion-based NMAs, the individual studies are distributed symmetrically about the combined effect size and toward the top of the graph. Thus, there was no evidence of publication bias in the present NMA.
Evidence Network
Network plots reveal that the MIBI SPECT and US categories detected the higher number of patients with pHPT and have relatively more studies in terms of sensitivity (eFigure 3 in the Supplement).
Inconsistency Tests
The sensitivity of the 8 representative imaging categories was analyzed using inconsistency tests using the node-splitting method. The results showed consistency among the direct evidence and the indirect evidence of all outcomes; therefore, the consistency model was applied in the present study (all P > .05).
Network Meta-analysis
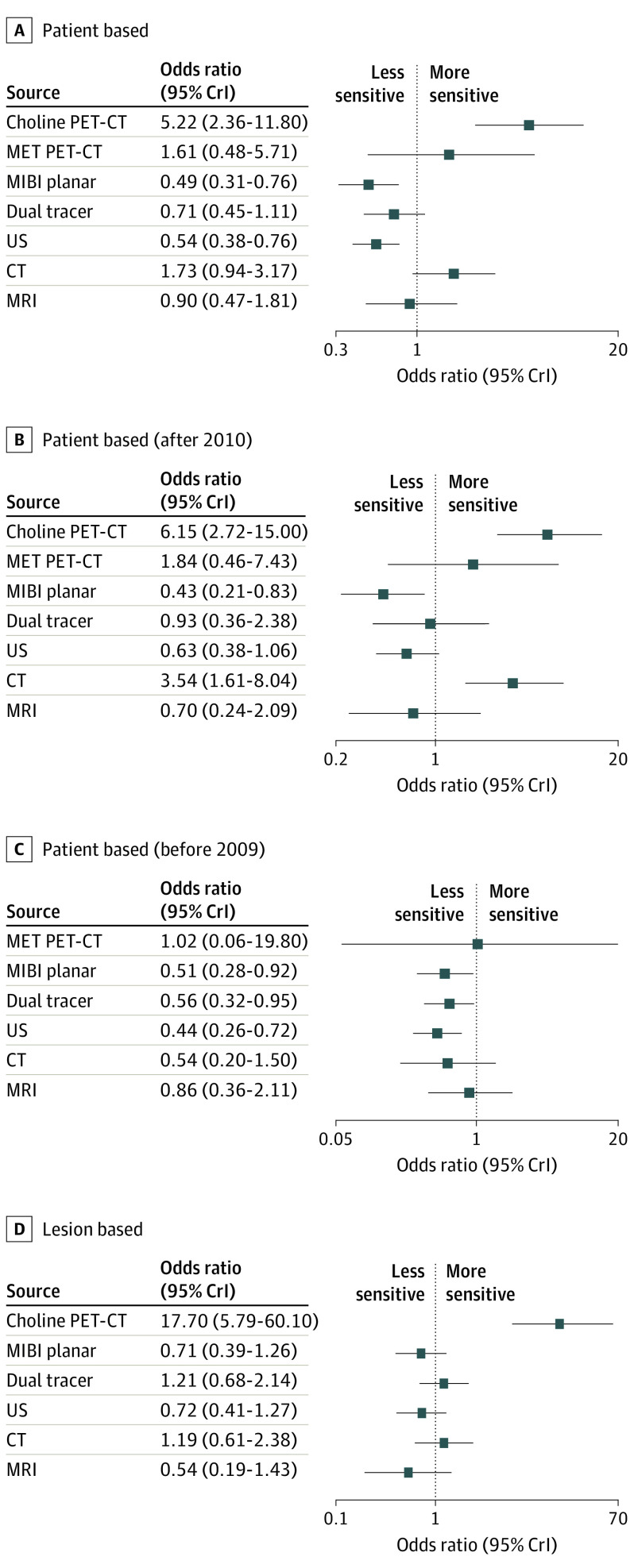
The pooled estimation of the sensitivity for localization of pHPT was analyzed based on the MIBI SPECT category, which is a widely used method among the 8 imaging categories. As shown in Figure 2, the results of the present NMA revealed that the sensitivity of choline PET-CT was significantly higher than that of MIBI SPECT in both patient-based and lesion-based analyses (patient-based analysis: OR, 5.22; 95% CrI, 2.36-11.80; lesion-based analysis: OR, 17.70; 95% CrI, 5.79-60.10). When patient-based NMA was performed on the studies published after 2010, the sensitivities of the choline PET-CT and CT categories were significantly higher than that of MIBI SPECT (choline PET-CT: OR, 6.15; 95% CrI, 2.72-15.00; CT: OR, 3.54; 95% CrI, 1.61-8.04). In the studies published before 2009, there were no direct comparative studies using choline PET-CT or 4D-CT, and none of the imaging modality categories performed significantly better than MIBI SPECT.
Figure 2. Forest Plots of the Sensitivity of 8 Representative Categories of Imaging Modalities for Localization of Primary Parahyperthyroidism.
All modalities are compared with the technetium 99m sestamibi (MIBI) single-photon emission computed tomography (SPECT) category. 95% CrI indicates 95% credible interval; CT, computed tomography; MET, carbon 11–labeled methionine; MRI, magnetic resonance imaging; PET, positron emission tomography; and US, ultrasonography.
SUCRA Values
Table 3 shows the SUCRA values of the diagnostic performance of the 8 representative imaging modality categories for localization of pHPT, which indicated that choline PET-CT showed the highest SUCRA value in both patient-based analyses (0.9897) and lesion-based analyses (1.0000). In a chronological analysis investigating the changes in imaging methods over time, choline PET-CT showed the highest SUCRA value, followed by the CT category, in patient-based analysis after 2010 (choline PET-CT, 0.9703; CT, 0.8440). In the analysis before 2009, when there were no direct comparative studies using choline PET-CT or 4D-CT, MIBI SPECT had the highest SUCRA value (0.8294).
Table 3. SUCRA Values of Various Imaging Modalities for Localization of Primary Hyperparathyroidism.
| Treatmenta | SUCRA values | |||
|---|---|---|---|---|
| Patient based | Patient based (after 2010) | Patient based (before 2009) | Lesion based | |
| Choline PET-CT | 0.9897 | 0.9703 | NA | 1.0000 |
| MET PET-CT | 0.7046 | 0.6701 | 0.6256 | NA |
| MIBI SPECT | 0.5465 | 0.4964 | 0.8294 | 0.5340 |
| MIBI planar | 0.0585 | 0.0481 | 0.3345 | 0.2412 |
| Dual tracer | 0.3241 | 0.4333 | 0.4240 | 0.6964 |
| US | 0.1286 | 0.2335 | 0.1776 | 0.2441 |
| CT | 0.7780 | 0.8440 | 0.3971 | 0.6600 |
| MRI | 0.4700 | 0.3044 | 0.7118 | 0.1245 |
Abbreviations: CT, computed tomography; MET, carbon 11–labeled methionine; MIBI, technetium 99m sestamibi; MRI, magnetic resonance imaging; NA, not available; PET, positron emission tomography; SPECT, single-photon emission computed tomography; SUCRA, surface under the cumulative ranking curve; US, ultrasonography.
Choline PET-CT includes F 18 fluorocholine (FCH) PET-CT, FCH PET-MRI, and carbon 11–labeled choline PET-CT; MIBI SPECT includes MIBI SPECT-CT, MIBI pinhole SPECT, MIBI SPECT and contrast-enhanced CT, technetium 99m tetrofosmin (TF) SPECT, and TF SPECT-CT; MIBI planar includes MIBI pinhole-TF planar; dual tracer includes MIBI–technetium 99m pertechnetate (Tc) subtraction, MIBI–iodine 123 subtraction, TF-Tc subtraction, and thallium 201–Tc subtraction with planar, pinhole, SPECT, or SPECT-CT; US includes contrast-enhanced US, high-resolution US with color Doppler, 3-dimensional US, endoscopic US, and surgeon-performed US; CT includes 4-dimensional CT and dual-energy CT; and MRI includes 3T-MRI and dynamic magnetic resonance angiography.
Discussion
The results of this NMA clearly showed that choline PET-CT, either FCH or CCH, should be the imaging method of choice for localization of pHPT in both patient-based and lesion-based analyses. Even in chronological analysis to investigate the changes in imaging technology over time, choline PET-CT showed the highest SUCRA value, followed by the CT category, in patient-based analysis after 2010.
Among the various imaging methods, traditionally, neck US and parathyroid scintigraphy (either with SPECT or SPECT-CT) using the dual tracer subtraction technique or dual phase of MIBI have been well established for preoperative localization of pHPT, although there was no clear consensus on the optimal imaging approach.7 In a study with a systematic literature review from 1995 to 2003, the sensitivities of MIBI scan and US were 88.4% and 78.6%, respectively, for single adenoma in pHPT.140 The results of our analysis on studies before 2009 showed that MIBI SPECT had the highest SUCRA value, whereas all other imaging modality categories failed to show a statistically significant performance. In studies published before 2009, there were no direct comparative studies using choline PET-CT or 4D-CT.
However, during the past decade, new morphologic, functional, and hybrid imaging technologies have been introduced for preoperative localization of pHPT. Multiphase CT with 4 phases (noncontrast, arterial, venous, and delayed), referred to as 4D-CT, was introduced and is increasingly used for preoperative localization of hyperparathyroidism. Four-dimensional CT has excellent anatomic information, short acquisition time, higher sensitivity for multiglandular disease, and overall superior performance for patients with nonlocalizing or discordant first-line imaging results.141 In contrast with 4D-CT, the DE-CT technique uses the different CT attenuation characteristics of various materials with different tube voltage settings. Multiphase DE-CT was recently introduced as a feasible imaging method for nonlocalizing hyperparathyroidism.142,143 In patient-based analysis after 2010, the CT category consisted of 4 studies with 4D-CT and 2 studies with DE-CT without any conventional CT study.
Since the publication of case reports on incidental localization of parathyroid adenoma while performing CCH or FCH PET-CT for patients with prostate cancer,144,145 a number of studies on radiolabeled choline PET for patients with hyperparathyroidism have been published. Radiolabeled choline is incorporated into the proliferating cell membranes, and the increased uptake of choline in hyperparathyroidism seems to be caused by increased phospholipid-dependent choline kinase activity from an overreleased parathyroid hormone.146 Giovanella et al8 claim that FCH PET-CT will replace other current methods of preoperative parathyroid imaging owing to its excellent diagnostic performance and low radiation burden. In line with their claim, this NMA also revealed that choline PET-CT clearly showed the best performance for localization of pHPT in both patient-based and lesion-based analyses, with the highest SUCRA value among all other imaging modalities. In patient-based NMAs after 2010, the sensitivities of choline PET-CT and CT categories were significantly higher than that of MIBI SPECT. Choline PET-CT had the highest SUCRA value, followed by the CT category, MET PET-CT, and MIBI SPECT in patient-based analysis after 2010, whereas MIBI SPECT had the highest SUCRA value, followed by MRI and MET PET-CT in patient-based analysis before 2009. Although cost-effectiveness, availability, and radiation burden should be considered, it is thought that choline PET-CT and 4D-CT should be performed more preferentially compared with MIBI SPECT or US for preoperative localization of pHPT.
Limitations
This study has some limitations. First, various imaging modalities were classified into 8 representative imaging categories to reduce the number of treatments, which may not reflect the characteristics of specific imaging methods. For example, the US category included contrast-enhanced US, high-resolution US with color Doppler, 3-dimensional US, endoscopic US, surgeon-performed US, and radiologist-performed US. Some of the various US methods may have showed better performance, but they were not analyzed individually. The choline PET-CT category also consisted of 9 studies with FCH PET-CT, 1 study with FCH PET-MRI, and 1 study with CCH PET-CT. The characteristics of PET-MRI and PET-CT may be different, but they were not analyzed individually. However, we tried to compare the overall flow of the imaging techniques for localization of pHPT rather than focusing on the individual characteristics of a small number of studies. Second, because this NMA was based on head-to-head comparison studies, studies using a single imaging method or a different number of patients for each imaging method were excluded even if 2 or more imaging modalities were compared.
Conclusions
Choline PET-CT clearly showed the best performance for localization of pHPT in both patient-based and lesion-based analyses. Even in chronological analysis that investigated the changes in imaging methods over time, choline PET-CT showed the highest SUCRA value, followed by the CT category, in patient-based analysis after 2010. Thus, choline PET-CT would be the best preoperative imaging modality for localization of pHPT. Further direct comparative studies between choline PET-CT and 4D-CT are needed to establish their role in surgical treatment by localizing pHPT.
eFigure 1. Risk of Bias and Applicability Concerns Graph Based on 15-Item Modified Quality Assessment of Diagnostic Accuracy Studies
eFigure 2. Funnel Plots for Eight Representative Categories of Various Imaging Modalities for pHPT Localization in Both Patient- and Lesion-Based Analyses
eFigure 3. Evidence Network Plots of Diagnostic Value of Eight Representative Categories of Various Imaging Modalities for pHPT Localization in Both Patient- and Lesion-Based Analyses
eTable 1. Search Queries
eTable 2. Characteristics of the Enrolled Studies
eReferences
References
- 1.Udelsman R, Lin Z, Donovan P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg. 2011;253(3):585-591. doi: 10.1097/SLA.0b013e318208fed9 [DOI] [PubMed] [Google Scholar]
- 2.Kunstman JW, Udelsman R. Superiority of minimally invasive parathyroidectomy. Adv Surg. 2012;46:171-189. doi: 10.1016/j.yasu.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 3.Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19(2):577-583. doi: 10.1245/s10434-011-1870-5 [DOI] [PubMed] [Google Scholar]
- 4.Wei WJ, Shen CT, Song HJ, Qiu ZL, Luo QY. Comparison of SPET/CT, SPET and planar imaging using 99mTc-MIBI as independent techniques to support minimally invasive parathyroidectomy in primary hyperparathyroidism: a meta-analysis. Hell J Nucl Med. 2015;18(2):127-135. doi: 10.1967/s002449910207 [DOI] [PubMed] [Google Scholar]
- 5.Treglia G, Sadeghi R, Schalin-Jäntti C, et al. Detection rate of (99m) Tc-MIBI single photon emission computed tomography (SPECT)/CT in preoperative planning for patients with primary hyperparathyroidism: a meta-analysis. Head Neck. 2016;38(suppl 1):E2159-E2172. doi: 10.1002/hed.24027 [DOI] [PubMed] [Google Scholar]
- 6.Kluijfhout WP, Pasternak JD, Drake FT, et al. Use of PET tracers for parathyroid localization: a systematic review and meta-analysis. Langenbecks Arch Surg. 2016;401(7):925-935. doi: 10.1007/s00423-016-1425-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Treglia G, Piccardo A, Imperiale A, et al. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2019;46(3):751-765. doi: 10.1007/s00259-018-4123-z [DOI] [PubMed] [Google Scholar]
- 8.Giovanella L, Bacigalupo L, Treglia G, Piccardo A. Will 18F-fluorocholine PET/CT replace other methods of preoperative parathyroid imaging? Endocrine. 2021;71(2):285-297. doi: 10.1007/s12020-020-02487-y [DOI] [PubMed] [Google Scholar]
- 9.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777-784. doi: 10.7326/M14-2385 [DOI] [PubMed] [Google Scholar]
- 10.McInnes MDF, Moher D, Thombs BD, et al. ; PRISMA-DTA Group . Preferred Reporting Items for a Systematic Review and Meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388-396. doi: 10.1001/jama.2017.19163 [DOI] [PubMed] [Google Scholar]
- 11.Whiting PF, Rutjes AW, Westwood ME, et al. ; QUADAS-2 Group . QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529-536. doi: 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 12.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shim S, Yoon BH, Shin IS, Bae JM. Network meta-analysis: application and practice using Stata. Epidemiol Health. 2017;39:e2017047. doi: 10.4178/epih.e2017047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shim SR, Kim SJ, Lee J, Rücker G. Network meta-analysis: application and practice using R software. Epidemiol Health. 2019;41:e2019013. doi: 10.4178/epih.e2019013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105-3124. doi: 10.1002/sim.1875 [DOI] [PubMed] [Google Scholar]
- 17.Spiegelhalter DJ, Best NG, Carlin BR, van der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc B. 2002;64:583-616. doi: 10.1111/1467-9868.00353 [DOI] [Google Scholar]
- 18.Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7-8):932-944. doi: 10.1002/sim.3767 [DOI] [PubMed] [Google Scholar]
- 19.Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15:58. doi: 10.1186/s12874-015-0060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163-171. doi: 10.1016/j.jclinepi.2010.03.016 [DOI] [PubMed] [Google Scholar]
- 21.Juweid ME, Omari Y, Khawaja N, et al. Use of pinhole dual-phase Tc-99m sestamibi vs combined Tc-99m sestamibi and Tc-99m pertechnetate scintigraphy in patients with hyperparathyroidism where single-photon emission computed tomography/computed tomography is unavailable. Nucl Med Commun. 2020;41(2):87-95. doi: 10.1097/MNM.0000000000001124 [DOI] [PubMed] [Google Scholar]
- 22.Okudan B, Seven B, Coskun N, Albayrak A. Comparison between single-photon emission computed tomography/computed tomography and ultrasound in preoperative detection of parathyroid adenoma: retrospective review of an institutional experience. Nucl Med Commun. 2019;40(12):1211-1215. doi: 10.1097/MNM.0000000000001104 [DOI] [PubMed] [Google Scholar]
- 23.Parra Ramírez P, Santiago Hernando A, Barquiel Alcalá B, Martín Rojas-Marcos P, Lisbona Catalán A, Álvarez Escolá C. Potential utility of contrast-enhanced ultrasound in the preoperative evaluation of primary hyperparathyroidism. J Ultrasound Med. 2019;38(10):2565-2571. doi: 10.1002/jum.14949 [DOI] [PubMed] [Google Scholar]
- 24.Vitetta GM, Ravera A, Mensa G, et al. Actual role of color-doppler high-resolution neck ultrasonography in primary hyperparathyroidism: a clinical review and an observational study with a comparison of 99mTc-sestamibi parathyroid scintigraphy. J Ultrasound. 2019;22(3):291-308. doi: 10.1007/s40477-018-0332-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borumandi F, Daultrey H, Laji K, Bosman D, Ashford N, Alam P. Detectability and surgical outcomes in parathyroid surgery—a single-centre experience. Br J Oral Maxillofac Surg. 2019;57(4):330-335. doi: 10.1016/j.bjoms.2019.03.007 [DOI] [PubMed] [Google Scholar]
- 26.Bossert I, Chytiris S, Hodolic M, et al. PETC/CT with 18F-choline localizes hyperfunctioning parathyroid adenomas equally well in normocalcemic hyperparathyroidism as in overt hyperparathyroidism. J Endocrinol Invest. 2019;42(4):419-426. doi: 10.1007/s40618-018-0931-z [DOI] [PubMed] [Google Scholar]
- 27.Piccardo A, Trimboli P, Rutigliani M, et al. Additional value of integrated 18F-choline PET/4D contrast-enhanced CT in the localization of hyperfunctioning parathyroid glands and correlation with molecular profile. Eur J Nucl Med Mol Imaging. 2019;46(3):766-775. doi: 10.1007/s00259-018-4147-4 [DOI] [PubMed] [Google Scholar]
- 28.Scattergood S, Marsden M, Kyrimi E, Ishii H, Doddi S, Sinha P. Combined ultrasound and sestamibi scintigraphy provides accurate preoperative localisation for patients with primary hyperparathyroidism. Ann R Coll Surg Engl. 2019;101(2):97-102. doi: 10.1308/rcsann.2018.0158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vu TH, Schellingerhout D, Guha-Thakurta N, et al. Solitary parathyroid adenoma localization in technetium Tc99m sestamibi SPECT and multiphase multidetector 4D CT. AJNR Am J Neuroradiol. 2019;40(1):142-149. doi: 10.3174/ajnr.A5901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khafif A, Masalha M, Landsberg R, et al. The role of F18-fluorocholine positron emission tomography/magnetic resonance imaging in localizing parathyroid adenomas. Eur Arch Otorhinolaryngol. 2019;276(5):1509-1516. doi: 10.1007/s00405-019-05301-2 [DOI] [PubMed] [Google Scholar]
- 31.Asseeva P, Paladino NC, Guerin C, et al. Value of 123I/99mTc-sestamibi parathyroid scintigraphy with subtraction SPECT/CT in primary hyperparathyroidism for directing minimally invasive parathyroidectomy. Am J Surg. 2019;217(1):108-113. doi: 10.1016/j.amjsurg.2018.06.027 [DOI] [PubMed] [Google Scholar]
- 32.Zajíčková K, Zogala D, Kubinyi J. Parathyroid imaging by (18)F-fluorocholine PET/CT in patients with primary hyperparathyroidism and inconclusive conventional methods: clinico-pathological correlations. Physiol Res. 2018;67(suppl 3):S551-S557. doi: 10.33549/physiolres.934029 [DOI] [PubMed] [Google Scholar]
- 33.Argirò R, Diacinti D, Sacconi B, et al. Diagnostic accuracy of 3T magnetic resonance imaging in the preoperative localisation of parathyroid adenomas: comparison with ultrasound and 99mTc-sestamibi scans. Eur Radiol. 2018;28(11):4900-4908. doi: 10.1007/s00330-018-5437-8 [DOI] [PubMed] [Google Scholar]
- 34.Beheshti M, Hehenwarter L, Paymani Z, et al. 18F-fluorocholine PET/CT in the assessment of primary hyperparathyroidism compared with 99mTc-MIBI or 99mTc-tetrofosmin SPECT/CT: a prospective dual-centre study in 100 patients. Eur J Nucl Med Mol Imaging. 2018;45(10):1762-1771. doi: 10.1007/s00259-018-3980-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hiebert J, Hague C, Hou S, Wiseman SM. Dual energy computed tomography should be a first line preoperative localization imaging test for primary hyperparathyroidism patients. Am J Surg. 2018;215(5):788-792. doi: 10.1016/j.amjsurg.2017.11.048 [DOI] [PubMed] [Google Scholar]
- 36.Araz M, Soydal Ç, Özkan E, et al. The efficacy of fluorine-18-choline PET/CT in comparison with 99mTc-MIBI SPECT/CT in the localization of a hyperfunctioning parathyroid gland in primary hyperparathyroidism. Nucl Med Commun. 2018;39(11):989-994. doi: 10.1097/MNM.0000000000000899 [DOI] [PubMed] [Google Scholar]
- 37.Thanseer N, Bhadada SK, Sood A, et al. Comparative effectiveness of ultrasonography, 99mTc-sestamibi, and 18F-fluorocholine PET/CT in detecting parathyroid adenomas in patients with primary hyperparathyroidism. Clin Nucl Med. 2017;42(12):e491-e497. doi: 10.1097/RLU.0000000000001845 [DOI] [PubMed] [Google Scholar]
- 38.Tunca F, Akici M, Işcan Y, Cem Sormaz I, Giles Senyurek Y, Terzioğlu T. The impact of combined interpretation of localization studies on image-guided surgical approaches for primary hyperparathyroidism. Minerva Endocrinol. 2017;42(3):213-222. doi: 10.23736/S0391-1977.16.02396-8 [DOI] [PubMed] [Google Scholar]
- 39.Frank SJ, Goldman-Yassen AE, Koenigsberg T, Libutti SK, Koenigsberg M. Sensitivity of 3-dimensional sonography in preoperative evaluation of parathyroid glands in patients with primary hyperparathyroidism. J Ultrasound Med. 2017;36(9):1897-1904. doi: 10.1002/jum.14245 [DOI] [PubMed] [Google Scholar]
- 40.Seyednejad N, Healy C, Tiwari P, et al. Dual-energy computed tomography: a promising novel preoperative localization study for treatment of primary hyperparathyroidism. Am J Surg. 2016;211(5):839-845. doi: 10.1016/j.amjsurg.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 41.Tan MZ, Ng JC, Eisman JA, Ng DC, Hansen L, Chandran M. A retrospective review of imaging and operative modalities performed in patients with primary hyperparathyroidism at a mid-volume surgical centre in Southeast Asia. Ann Acad Med Singap. 2016;45(5):191-197. [PubMed] [Google Scholar]
- 42.Galvin L, Oldan JD, Bahl M, Eastwood JD, Sosa JA, Hoang JK. Parathyroid 4D CT and scintigraphy: what factors contribute to missed parathyroid lesions? Otolaryngol Head Neck Surg. 2016;154(5):847-853. doi: 10.1177/0194599816630711 [DOI] [PubMed] [Google Scholar]
- 43.Brown SJ, Lee JC, Christie J, et al. Four-dimensional computed tomography for parathyroid localization: a new imaging modality. ANZ J Surg. 2015;85(6):483-487. doi: 10.1111/ans.12571 [DOI] [PubMed] [Google Scholar]
- 44.Hayakawa N, Nakamoto Y, Kurihara K, et al. A comparison between 11C-methionine PET/CT and MIBI SPECT/CT for localization of parathyroid adenomas/hyperplasia. Nucl Med Commun. 2015;36(1):53-59. doi: 10.1097/MNM.0000000000000216 [DOI] [PubMed] [Google Scholar]
- 45.Michaud L, Balogova S, Burgess A, et al. A pilot comparison of 18F-fluorocholine PET/CT, ultrasonography and 123I/99mTc-sestaMIBI dual-phase dual-isotope scintigraphy in the preoperative localization of hyperfunctioning parathyroid glands in primary or secondary hyperparathyroidism: influence of thyroid anomalies. Medicine (Baltimore). 2015;94(41):e1701. doi: 10.1097/MD.0000000000001701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guerin C, Lowery A, Gabriel S, et al. Preoperative imaging for focused parathyroidectomy: making a good strategy even better. Eur J Endocrinol. 2015;172(5):519-526. doi: 10.1530/EJE-14-0964 [DOI] [PubMed] [Google Scholar]
- 47.Noda S, Onoda N, Kashiwagi S, et al. Strategy of operative treatment of hyperparathyroidism using US scan and (99m)Tc-MIBI SPECT/CT. Endocr J. 2014;61(3):225-230. doi: 10.1507/endocrj.EJ13-0292 [DOI] [PubMed] [Google Scholar]
- 48.Orevi M, Freedman N, Mishani E, Bocher M, Jacobson O, Krausz Y. Localization of parathyroid adenoma by 11C-choline PET/CT: preliminary results. Clin Nucl Med. 2014;39(12):1033-1038. doi: 10.1097/RLU.0000000000000607 [DOI] [PubMed] [Google Scholar]
- 49.Ersoy R, Ersoy O, Evranos Ogmen B, et al. Diagnostic value of endoscopic ultrasonography for preoperative localization of parathyroid adenomas. Endocrine. 2014;47(1):221-226. doi: 10.1007/s12020-013-0152-3 [DOI] [PubMed] [Google Scholar]
- 50.Schalin-Jäntti C, Ryhänen E, Heiskanen I, et al. Planar scintigraphy with 123I/99mTc-sestamibi, 99mTc-sestamibi SPECT/CT, 11C-methionine PET/CT, or selective venous sampling before reoperation of primary hyperparathyroidism? J Nucl Med. 2013;54(5):739-747. doi: 10.2967/jnumed.112.109561 [DOI] [PubMed] [Google Scholar]
- 51.Kwon JH, Kim EK, Lee HS, Moon HJ, Kwak JY. Neck ultrasonography as preoperative localization of primary hyperparathyroidism with an additional role of detecting thyroid malignancy. Eur J Radiol. 2013;82(1):e17-e21. doi: 10.1016/j.ejrad.2012.08.003 [DOI] [PubMed] [Google Scholar]
- 52.Kim YI, Jung YH, Hwang KT, Lee HY. Efficacy of 99mTc-sestamibi SPECT/CT for minimally invasive parathyroidectomy: comparative study with 99mTc-sestamibi scintigraphy, SPECT, US and CT. Ann Nucl Med. 2012;26(10):804-810. doi: 10.1007/s12149-012-0641-0 [DOI] [PubMed] [Google Scholar]
- 53.Aschenbach R, Tuda S, Lamster E, et al. Dynamic magnetic resonance angiography for localization of hyperfunctioning parathyroid glands in the reoperative neck. Eur J Radiol. 2012;81(11):3371-3377. doi: 10.1016/j.ejrad.2012.05.023 [DOI] [PubMed] [Google Scholar]
- 54.Akbaba G, Berker D, Isik S, et al. A comparative study of pre-operative imaging methods in patients with primary hyperparathyroidism: ultrasonography, 99mTc sestamibi, single photon emission computed tomography, and magnetic resonance imaging. J Endocrinol Invest. 2012;35(4):359-364. doi: 10.3275/7764 [DOI] [PubMed] [Google Scholar]
- 55.Grayev AM, Gentry LR, Hartman MJ, Chen H, Perlman SB, Reeder SB. Presurgical localization of parathyroid adenomas with magnetic resonance imaging at 3.0 T: an adjunct method to supplement traditional imaging. Ann Surg Oncol. 2012;19(3):981-989. doi: 10.1245/s10434-011-2046-z [DOI] [PubMed] [Google Scholar]
- 56.Adler JT, Chen H, Schaefer S, Sippel RS. What is the added benefit of cervical ultrasound to 99mTc-sestamibi scanning in primary hyperparathyroidism? Ann Surg Oncol. 2011;18(10):2907-2911. doi: 10.1245/s10434-011-1724-1 [DOI] [PubMed] [Google Scholar]
- 57.Patel CN, Salahudeen HM, Lansdown M, Scarsbrook AF. Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localization of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol. 2010;65(4):278-287. doi: 10.1016/j.crad.2009.12.005 [DOI] [PubMed] [Google Scholar]
- 58.Prommegger R, Wimmer G, Profanter C, et al. Virtual neck exploration: a new method for localizing abnormal parathyroid glands. Ann Surg. 2009;250(5):761-765. doi: 10.1097/SLA.0b013e3181bd906b [DOI] [PubMed] [Google Scholar]
- 59.Thomas DL, Bartel T, Menda Y, Howe J, Graham MM, Juweid ME. Single photon emission computed tomography (SPECT) should be routinely performed for the detection of parathyroid abnormalities utilizing technetium-99m sestamibi parathyroid scintigraphy. Clin Nucl Med. 2009;34(10):651-655. doi: 10.1097/RLU.0b013e3181b591c9 [DOI] [PubMed] [Google Scholar]
- 60.Tresoldi S, Pompili G, Maiolino R, et al. Primary hyperparathyroidism: can ultrasonography be the only preoperative diagnostic procedure? Radiol Med. 2009;114(7):1159-1172. doi: 10.1007/s11547-009-0447-x [DOI] [PubMed] [Google Scholar]
- 61.Tublin ME, Pryma DA, Yim JH, et al. Localization of parathyroid adenomas by sonography and technetium tc 99m sestamibi single-photon emission computed tomography before minimally invasive parathyroidectomy: are both studies really needed? J Ultrasound Med. 2009;28(2):183-190. doi: 10.7863/jum.2009.28.2.183 [DOI] [PubMed] [Google Scholar]
- 62.Tang BN, Moreno-Reyes R, Blocklet D, et al. Accurate pre-operative localization of pathological parathyroid glands using 11C-methionine PET/CT. Contrast Media Mol Imaging. 2008;3(4):157-163. doi: 10.1002/cmmi.243 [DOI] [PubMed] [Google Scholar]
- 63.Ansquer C, Mirallié E, Carlier T, Abbey-Huguenin H, Aubron F, Kraeber-Bodéré F. Preoperative localization of parathyroid lesions. Value of 99mTc-MIBI tomography and factors influencing detection. Nuklearmedizin. 2008;47(4):158-162. doi: 10.3413/nukmed-0108 [DOI] [PubMed] [Google Scholar]
- 64.Boudreaux BA, Magnuson JS, Asher SA, Desmond R, Peters GE. The role of ultrasonography in parathyroid surgery. Arch Otolaryngol Head Neck Surg. 2007;133(12):1240-1244. doi: 10.1001/archotol.133.12.1240 [DOI] [PubMed] [Google Scholar]
- 65.Prasannan S, Davies G, Bochner M, Kollias J, Malycha P. Minimally invasive parathyroidectomy using surgeon-performed ultrasound and sestamibi. ANZ J Surg. 2007;77(9):774-777. doi: 10.1111/j.1445-2197.2007.04227.x [DOI] [PubMed] [Google Scholar]
- 66.Lavely WC, Goetze S, Friedman KP, et al. Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m)Tc-sestamibi parathyroid scintigraphy. J Nucl Med. 2007;48(7):1084-1089. doi: 10.2967/jnumed.107.040428 [DOI] [PubMed] [Google Scholar]
- 67.Ruf J, Seehofer D, Denecke T, et al. Impact of image fusion and attenuation correction by SPECT-CT on the scintigraphic detection of parathyroid adenomas. Nuklearmedizin. 2007;46(1):15-21. doi: 10.1055/s-0037-1616620 [DOI] [PubMed] [Google Scholar]
- 68.Lo CY, Lang BH, Chan WF, Kung AW, Lam KS. A prospective evaluation of preoperative localization by technetium-99m sestamibi scintigraphy and ultrasonography in primary hyperparathyroidism. Am J Surg. 2007;193(2):155-159. doi: 10.1016/j.amjsurg.2006.04.020 [DOI] [PubMed] [Google Scholar]
- 69.Steward DL, Danielson GP, Afman CE, Welge JA. Parathyroid adenoma localization: surgeon-performed ultrasound versus sestamibi. Laryngoscope. 2006;116(8):1380-1384. doi: 10.1097/01.mlg.0000227957.06529.22 [DOI] [PubMed] [Google Scholar]
- 70.Barczynski M, Golkowski F, Konturek A, et al. Technetium-99m-sestamibi subtraction scintigraphy vs ultrasonography combined with a rapid parathyroid hormone assay in parathyroid aspirates in preoperative localization of parathyroid adenomas and in directing surgical approach. Clin Endocrinol (Oxf). 2006;65(1):106-113. doi: 10.1111/j.1365-2265.2006.02556.x [DOI] [PubMed] [Google Scholar]
- 71.Saeed S, Yao M, Philip B, Blend M. Localizing hyperfunctioning parathyroid tissue: MRI or nuclear study or both? Clin Imaging. 2006;30(4):257-265. doi: 10.1016/j.clinimag.2006.02.007 [DOI] [PubMed] [Google Scholar]
- 72.Krausz Y, Bettman L, Guralnik L, et al. Technetium-99m-MIBI SPECT/CT in primary hyperparathyroidism. World J Surg. 2006;30(1):76-83. doi: 10.1007/s00268-005-7849-2 [DOI] [PubMed] [Google Scholar]
- 73.Solorzano CC, Carneiro-Pla DM, Irvin GL III. Surgeon-performed ultrasonography as the initial and only localizing study in sporadic primary hyperparathyroidism. J Am Coll Surg. 2006;202(1):18-24. doi: 10.1016/j.jamcollsurg.2005.08.014 [DOI] [PubMed] [Google Scholar]
- 74.Lorberboym M, Ezri T, Schachter PP. Preoperative technetium Tc 99m sestamibi SPECT imaging in the management of primary hyperparathyroidism in patients with concomitant multinodular goiter. Arch Surg. 2005;140(7):656-660. doi: 10.1001/archsurg.140.7.656 [DOI] [PubMed] [Google Scholar]
- 75.Masatsugu T, Yamashita H, Noguchi S, et al. Significant clinical differences in primary hyperparathyroidism between patients with and those without concomitant thyroid disease. Surg Today. 2005;35(5):351-356. doi: 10.1007/s00595-004-2952-9 [DOI] [PubMed] [Google Scholar]
- 76.Ruf J, Lopez Hänninen E, Steinmüller T, et al. Preoperative localization of parathyroid glands: use of MRI, scintigraphy, and image fusion. Nuklearmedizin. 2004;43(3):85-90. doi: 10.1055/s-0038-1625596 [DOI] [PubMed] [Google Scholar]
- 77.Schachter PP, Issa N, Shimonov M, Czerniak A, Lorberboym M. Early, postinjection MIBI-SPECT as the only preoperative localizing study for minimally invasive parathyroidectomy. Arch Surg. 2004;139(4):433-437. doi: 10.1001/archsurg.139.4.433 [DOI] [PubMed] [Google Scholar]
- 78.Saint Marc O, Cogliandolo A, Pidoto RR, Pozzo A. Prospective evaluation of ultrasonography plus MIBI scintigraphy in selecting patients with primary hyperparathyroidism for unilateral neck exploration under local anaesthesia. Am J Surg. 2004;187(3):388-393. doi: 10.1016/j.amjsurg.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 79.Lumachi F, Tregnaghi A, Zucchetta P, et al. Technetium-99m sestamibi scintigraphy and helical CT together in patients with primary hyperparathyroidism: a prospective clinical study. Br J Radiol. 2004;77(914):100-103. doi: 10.1259/bjr/44399050 [DOI] [PubMed] [Google Scholar]
- 80.Lumachi F, Marzola MC, Zucchetta P, Tregnaghi A, Cecchin D, Bui F. Hyperfunctioning parathyroid tumours in patients with thyroid nodules: sensitivity and positive predictive value of high-resolution ultrasonography and 99mTc-sestamibi scintigraphy. Endocr Relat Cancer. 2003;10(3):419-423. doi: 10.1677/erc.0.0100419 [DOI] [PubMed] [Google Scholar]
- 81.Lorberboym M, Minski I, Macadziob S, Nikolov G, Schachter P. Incremental diagnostic value of preoperative 99mTc-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med. 2003;44(6):904-908. [PubMed] [Google Scholar]
- 82.Prager G, Czerny C, Ofluoglu S, et al. Impact of localization studies on feasibility of minimally invasive parathyroidectomy in an endemic goiter region. J Am Coll Surg. 2003;196(4):541-548. doi: 10.1016/S1072-7515(02)01897-5 [DOI] [PubMed] [Google Scholar]
- 83.Leslie WD, Dupont JO, Bybel B, Riese KT. Parathyroid 99mTc-sestamibi scintigraphy: dual-tracer subtraction is superior to double-phase washout. Eur J Nucl Med Mol Imaging. 2002;29(12):1566-1570. doi: 10.1007/s00259-002-0944-9 [DOI] [PubMed] [Google Scholar]
- 84.Haber RS, Kim CK, Inabnet WB. Ultrasonography for preoperative localization of enlarged parathyroid glands in primary hyperparathyroidism: comparison with (99m)technetium sestamibi scintigraphy. Clin Endocrinol (Oxf). 2002;57(2):241-249. doi: 10.1046/j.1365-2265.2002.01583.x [DOI] [PubMed] [Google Scholar]
- 85.Berczi C, Mezõsi E, Galuska L, et al. Technetium-99m-sestamibi/pertechnetate subtraction scintigraphy vs ultrasonography for preoperative localization in primary hyperparathyroidism. Eur Radiol. 2002;12(3):605-609. doi: 10.1007/s003300101045 [DOI] [PubMed] [Google Scholar]
- 86.Scheiner JD, Dupuy DE, Monchik JM, Noto RB, Cronan JJ. Pre-operative localization of parathyroid adenomas: a comparison of power and colour Doppler ultrasonography with nuclear medicine scintigraphy. Clin Radiol. 2001;56(12):984-988. doi: 10.1053/crad.2001.0793 [DOI] [PubMed] [Google Scholar]
- 87.Casara D, Rubello D, Pelizzo MR, Shapiro B. Clinical role of 99mTcO4/MIBI scan, ultrasound and intra-operative gamma probe in the performance of unilateral and minimally invasive surgery in primary hyperparathyroidism. Eur J Nucl Med. 2001;28(9):1351-1359. doi: 10.1007/s002590100564 [DOI] [PubMed] [Google Scholar]
- 88.Prager G, Czerny C, Kurtaran A, et al. Minimally invasive open parathyroidectomy in an endemic goiter area: a prospective study. Arch Surg. 2001;136(7):810-816. doi: 10.1001/archsurg.136.7.810 [DOI] [PubMed] [Google Scholar]
- 89.Feingold DL, Alexander HR, Chen CC, et al. Ultrasound and sestamibi scan as the only preoperative imaging tests in reoperation for parathyroid adenomas. Surgery. 2000;128(6):1103-1109. doi: 10.1067/msy.2000.109963 [DOI] [PubMed] [Google Scholar]
- 90.Krausz Y, Lebensart PD, Klein M, et al. Preoperative localization of parathyroid adenoma in patients with concomitant thyroid nodular disease. World J Surg. 2000;24(12):1573-1578. doi: 10.1007/s002680010280 [DOI] [PubMed] [Google Scholar]
- 91.Lumachi F, Zucchetta P, Marzola MC, et al. Advantages of combined technetium-99m-sestamibi scintigraphy and high-resolution ultrasonography in parathyroid localization: comparative study in 91 patients with primary hyperparathyroidism. Eur J Endocrinol. 2000;143(6):755-760. doi: 10.1530/eje.0.1430755 [DOI] [PubMed] [Google Scholar]
- 92.Gallowitsch HJ, Mikosch P, Kresnik E, Unterweger O, Lind P. Comparison between 99mTc-tetrofosmin/pertechnetate subtraction scintigraphy and 99mTc-tetrofosmin SPECT for preoperative localization of parathyroid adenoma in an endemic goiter area. Invest Radiol. 2000;35(8):453-459. doi: 10.1097/00004424-200008000-00001 [DOI] [PubMed] [Google Scholar]
- 93.Moka D, Voth E, Dietlein M, Larena-Avellaneda A, Schicha H. Technetium 99m-MIBI-SPECT: a highly sensitive diagnostic tool for localization of parathyroid adenomas. Surgery. 2000;128(1):29-35. doi: 10.1067/msy.2000.107066 [DOI] [PubMed] [Google Scholar]
- 94.Moka D, Eschner W, Voth E, Dietlein M, Larena-Avellaneda A, Schicha H. Iterative reconstruction: an improvement of technetium-99m MIBI SPET for the detection of parathyroid adenomas? Eur J Nucl Med. 2000;27(5):485-489. doi: 10.1007/s002590050532 [DOI] [PubMed] [Google Scholar]
- 95.Hiromatsu Y, Ishibashi M, Nishida H, Okuda S, Miyake I. Technetium-99m tetrofosmin parathyroid imaging in patients with primary hyperparathyroidism. Intern Med. 2000;39(2):101-106. doi: 10.2169/internalmedicine.39.101 [DOI] [PubMed] [Google Scholar]
- 96.Catargi B, Raymond JM, Lafarge-Gense V, Leccia F, Roger P, Tabarin A. Localization of parathyroid tumors using endoscopic ultrasonography in primary hyperparathyroidism. J Endocrinol Invest. 1999;22(9):688-692. doi: 10.1007/BF03343630 [DOI] [PubMed] [Google Scholar]
- 97.Hewin DF, Brammar TJ, Kabala J, Farndon JR. Role of preoperative localization in the management of primary hyperparathyroidism. Br J Surg. 1997;84(10):1377-1380. [PubMed] [Google Scholar]
- 98.Fayet P, Hoeffel C, Fulla Y, et al. Technetium-99m sestamibi scintigraphy, magnetic resonance imaging and venous blood sampling in persistent and recurrent hyperparathyroidism. Br J Radiol. 1997;70(833):459-464. doi: 10.1259/bjr.70.833.9227226 [DOI] [PubMed] [Google Scholar]
- 99.Bonjer HJ, Bruining HA, Valkema R, et al. Single radionuclide scintigraphy with 99mtechnetium-sestamibi and ultrasonography in hyperparathyroidism. Eur J Surg. 1997;163(1):27-32. [PubMed] [Google Scholar]
- 100.Rauth JD, Sessions RB, Shupe SC, Ziessman HA. Comparison of Tc-99m MIBI and TI-201/Tc-99m pertechnetate for diagnosis of primary hyperparathyroidism. Clin Nucl Med. 1996;21(8):602-608. doi: 10.1097/00003072-199608000-00002 [DOI] [PubMed] [Google Scholar]
- 101.Light VL, McHenry CR, Jarjoura D, Sodee DB, Miron SD. Prospective comparison of dual-phase technetium-99m-sestamibi scintigraphy and high resolution ultrasonography in the evaluation of abnormal parathyroid glands. Am Surg. 1996;62(7):562-567. [PubMed] [Google Scholar]
- 102.Udén P, Aspelin P, Berglund J, et al. Preoperative localization in unilateral parathyroid surgery: a cost-benefit study on ultrasound, computed tomography and scintigraphy. Acta Chir Scand. 1990;156(1):29-35. [PubMed] [Google Scholar]
- 103.Auffermann W, Gooding GA, Okerlund MD, et al. Diagnosis of recurrent hyperparathyroidism: comparison of MR imaging and other imaging techniques. AJR Am J Roentgenol. 1988;150(5):1027-1033. doi: 10.2214/ajr.150.5.1027 [DOI] [PubMed] [Google Scholar]
- 104.Peck WW, Higgins CB, Fisher MR, Ling M, Okerlund MD, Clark OH. Hyperparathyroidism: comparison of MR imaging with radionuclide scanning. Radiology. 1987;163(2):415-420. doi: 10.1148/radiology.163.2.3562820 [DOI] [PubMed] [Google Scholar]
- 105.Cuderman A, Senica K, Rep S, et al. 18F-fluorocholine PET/CT in primary hyperparathyroidism: superior diagnostic performance to conventional scintigraphic imaging for localization of hyperfunctioning parathyroid glands. J Nucl Med. 2020;61(4):577-583. doi: 10.2967/jnumed.119.229914 [DOI] [PubMed] [Google Scholar]
- 106.Yeh R, Tay YD, Tabacco G, et al. Diagnostic performance of 4D CT and sestamibi SPECT/CT in localizing parathyroid adenomas in primary hyperparathyroidism. Radiology. 2019;291(2):469-476. doi: 10.1148/radiol.2019182122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Amadou C, Bera G, Ezziane M, et al. 18F-fluorocholine PET/CT and parathyroid 4D computed tomography for primary hyperparathyroidism: the challenge of reoperative patients. World J Surg. 2019;43(5):1232-1242. doi: 10.1007/s00268-019-04910-6 [DOI] [PubMed] [Google Scholar]
- 108.Cunha-Bezerra P, Vieira R, Amaral F, et al. Better performance of four-dimension computed tomography as a localization procedure in normocalcemic primary hyperparathyroidism. J Med Imaging Radiat Oncol. 2018;62(4):493-498. doi: 10.1111/1754-9485.12728 [DOI] [PubMed] [Google Scholar]
- 109.Krakauer M, Wieslander B, Myschetzky PS, et al. A prospective comparative study of parathyroid dual-phase scintigraphy, dual-isotope subtraction scintigraphy, 4D-CT, and ultrasonography in primary hyperparathyroidism. Clin Nucl Med. 2016;41(2):93-100. doi: 10.1097/RLU.0000000000000988 [DOI] [PubMed] [Google Scholar]
- 110.Heiba SI, Jiang M, Rivera J, et al. Direct comparison of neck pinhole dual-tracer and dual-phase MIBI accuracies with and without SPECT/CT for parathyroid adenoma detection and localization. Clin Nucl Med. 2015;40(6):476-482. doi: 10.1097/RLU.0000000000000778 [DOI] [PubMed] [Google Scholar]
- 111.Suh YJ, Choi JY, Kim SJ, et al. Comparison of 4D CT, ultrasonography, and 99mTc sestamibi SPECT/CT in localizing single-gland primary hyperparathyroidism. Otolaryngol Head Neck Surg. 2015;152(3):438-443. doi: 10.1177/0194599814562195 [DOI] [PubMed] [Google Scholar]
- 112.Berner AM, Haroon A, Nowosinska E, et al. Localization of parathyroid disease with ‘sequential multiphase and dual-tracer’ technique and comparison with neck ultrasound. Nucl Med Commun. 2015;36(1):45-52. doi: 10.1097/MNM.0000000000000215 [DOI] [PubMed] [Google Scholar]
- 113.Ozkaya M, Elboga U, Sahin E, et al. Evaluation of conventional imaging techniques on preoperative localization in primary hyperparathyroidism. Bosn J Basic Med Sci. 2015;15(1):61-66. doi: 10.17305/bjbms.2015.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.D’Agostino J, Diana M, Vix M, et al. Three-dimensional metabolic and radiologic gathered evaluation using VR-RENDER fusion: a novel tool to enhance accuracy in the localization of parathyroid adenomas. World J Surg. 2013;37(7):1618-1625. doi: 10.1007/s00268-013-2021-x [DOI] [PubMed] [Google Scholar]
- 115.Shafiei B, Hoseinzadeh S, Fotouhi F, et al. Preoperative 99mTc-sestamibi scintigraphy in patients with primary hyperparathyroidism and concomitant nodular goiter: comparison of SPECT-CT, SPECT, and planar imaging. Nucl Med Commun. 2012;33(10):1070-1076. doi: 10.1097/MNM.0b013e32835710b6 [DOI] [PubMed] [Google Scholar]
- 116.Agha A, Hornung M, Rennert J, et al. Contrast-enhanced ultrasonography for localization of pathologic glands in patients with primary hyperparathyroidism. Surgery. 2012;151(4):580-586. doi: 10.1016/j.surg.2011.08.010 [DOI] [PubMed] [Google Scholar]
- 117.Eichhorn-Wharry LI, Carlin AM, Talpos GB. Mild hypercalcemia: an indication to select 4-dimensional computed tomography scan for preoperative localization of parathyroid adenomas. Am J Surg. 2011;201(3):334-338. doi: 10.1016/j.amjsurg.2010.08.033 [DOI] [PubMed] [Google Scholar]
- 118.Ho Shon IA, Yan W, Roach PJ, et al. Comparison of pinhole and SPECT 99mTc-MIBI imaging in primary hyperparathyroidism. Nucl Med Commun. 2008;29(11):949-955. doi: 10.1097/MNM.0b013e328309789e [DOI] [PubMed] [Google Scholar]
- 119.Nichols KJ, Tomas MB, Tronco GG, et al. Preoperative parathyroid scintigraphic lesion localization: accuracy of various types of readings. Radiology. 2008;248(1):221-232. doi: 10.1148/radiol.2481071066 [DOI] [PubMed] [Google Scholar]
- 120.Carlier T, Oudoux A, Mirallié E, et al. 99mTc-MIBI pinhole SPECT in primary hyperparathyroidism: comparison with conventional SPECT, planar scintigraphy and ultrasonography. Eur J Nucl Med Mol Imaging. 2008;35(3):637-643. doi: 10.1007/s00259-007-0625-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Taïeb D, Hassad R, Sebag F, et al. Tomoscintigraphy improves the determination of the embryologic origin of parathyroid adenomas, especially in apparently inferior glands: imaging features and surgical implications. J Nucl Med Technol. 2007;35(3):135-139. doi: 10.2967/jnmt.107.039743 [DOI] [PubMed] [Google Scholar]
- 122.Rodgers SE, Hunter GJ, Hamberg LM, et al. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140(6):932-940. doi: 10.1016/j.surg.2006.07.028 [DOI] [PubMed] [Google Scholar]
- 123.Kebapci M, Entok E, Kebapci N, Adapinar B. Preoperative evaluation of parathyroid lesions in patients with concomitant thyroid disease: role of high resolution ultrasonography and dual phase technetium 99m sestamibi scintigraphy. J Endocrinol Invest. 2004;27(1):24-30. doi: 10.1007/BF03350906 [DOI] [PubMed] [Google Scholar]
- 124.Wakamatsu H, Noguchi S, Yamashita H, et al. Parathyroid scintigraphy with 99mTc-MIBI and 123I subtraction: a comparison with magnetic resonance imaging and ultrasonography. Nucl Med Commun. 2003;24(7):755-762. doi: 10.1097/00006231-200307000-00004 [DOI] [PubMed] [Google Scholar]
- 125.Wakamatsu H, Noguchi S, Yamashita H, et al. Technetium-99m tetrofosmin for parathyroid scintigraphy: a direct comparison with (99m)Tc-MIBI, (201)Tl, MRI and US. Eur J Nucl Med. 2001;28(12):1817-1827. doi: 10.1007/s002590100627 [DOI] [PubMed] [Google Scholar]
- 126.Ho Shon IA, Roach PJ, Bernard EJ, Delbridge LW. Optimal pinhole techniques for preoperative localization with Tc-99m MIBI for primary hyperparathyroidism. Clin Nucl Med. 2001;26(12):1002-1009. doi: 10.1097/00003072-200112000-00002 [DOI] [PubMed] [Google Scholar]
- 127.De Feo ML, Colagrande S, Biagini C, et al. Parathyroid glands: combination of (99m)Tc MIBI scintigraphy and US for demonstration of parathyroid glands and nodules. Radiology. 2000;214(2):393-402. doi: 10.1148/radiology.214.2.r00fe04393 [DOI] [PubMed] [Google Scholar]
- 128.Takami H, Oshima M, Sugawara I, et al. Pre-operative localization and tissue uptake study in parathyroid imaging with technetium-99m-sestamibi. Aust N Z J Surg. 1999;69(9):629-631. doi: 10.1046/j.1440-1622.1999.01652.x [DOI] [PubMed] [Google Scholar]
- 129.Gallowitsch HJ, Mikosch P, Kresnik E, Gomez I, Lind P. Technetium 99m tetrofosmin parathyroid imaging: results with double-phase study and SPECT in primary and secondary hyperparathyroidism. Invest Radiol. 1997;32(8):459-465. doi: 10.1097/00004424-199708000-00005 [DOI] [PubMed] [Google Scholar]
- 130.Chen CC, Holder LE, Scovill WA, Tehan AM, Gann DS. Comparison of parathyroid imaging with technetium-99m-pertechnetate/sestamibi subtraction, double-phase technetium-99m-sestamibi and technetium-99m-sestamibi SPECT. J Nucl Med. 1997;38(6):834-839. [PubMed] [Google Scholar]
- 131.Arkles LB, Jones T, Hicks RJ, De Luise MA, Chou ST. Impact of complementary parathyroid scintigraphy and ultrasonography on the surgical management of hyperparathyroidism. Surgery. 1996;120(5):845-851. doi: 10.1016/S0039-6060(96)80093-6 [DOI] [PubMed] [Google Scholar]
- 132.Liou MJ, Huang HS, Lin JD, et al. The accuracy of ultrasonography and 201Tl-99mTc subtraction scan in localization of parathyroid lesions. Changgeng Yi Xue Za Zhi. 1996;19(2):121-128. [PubMed] [Google Scholar]
- 133.Billy HT, Rimkus DR, Hartzman S, Latimer RG. Technetium-99m-sestamibi single agent localization versus high resolution ultrasonography for the preoperative localization of parathyroid glands in patients with primary hyperparathyroidism. Am Surg. 1995;61(10):882-888. [PubMed] [Google Scholar]
- 134.Gallacher SJ, Kelly P, Shand J, et al. A comparison of 10 MHz ultrasound and 201-thallium/99m-technetium subtraction scanning in primary hyperparathyroidism. Postgrad Med J. 1993;69(811):376-380. doi: 10.1136/pgmj.69.811.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Whelan PJ, Rotstein LE, Rosen IB, Kucharczyk W. Do we really need another localizing technique for parathyroid glands? Am J Surg. 1989;158(4):382-384. doi: 10.1016/0002-9610(89)90139-6 [DOI] [PubMed] [Google Scholar]
- 136.Summers GW, Dodge DL, Kammer H. Accuracy and cost-effectiveness of preoperative isotope and ultrasound imaging in primary hyperparathyroidism. Otolaryngol Head Neck Surg. 1989;100(3):210-217. doi: 10.1177/019459988910000307 [DOI] [PubMed] [Google Scholar]
- 137.Roses DF, Sudarsky LA, Sanger J, Raghavendra BN, Reede DL, Blum M. The use of preoperative localization of adenomas of the parathyroid glands by thallium-technetium subtraction scintigraphy, high-resolution ultrasonography and computed tomography. Surg Gynecol Obstet. 1989;168(2):99-106. [PubMed] [Google Scholar]
- 138.Gooding GA, Okerlund MD, Stark DD, Clark OH. Parathyroid imaging: comparison of double-tracer (T1-201, Tc-99m) scintigraphy and high-resolution US. Radiology. 1986;161(1):57-64. doi: 10.1148/radiology.161.1.3020610 [DOI] [PubMed] [Google Scholar]
- 139.Winzelberg GG, Hydovitz JD, O’Hara KR, et al. Parathyroid adenomas evaluated by Tl-201/Tc-99m pertechnetate subtraction scintigraphy and high-resolution ultrasonography. Radiology. 1985;155(1):231-235. doi: 10.1148/radiology.155.1.2983373 [DOI] [PubMed] [Google Scholar]
- 140.Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132(3):359-372. doi: 10.1016/j.otohns.2004.10.005 [DOI] [PubMed] [Google Scholar]
- 141.Bunch PM, Kelly HR. Preoperative imaging techniques in primary hyperparathyroidism: a review. JAMA Otolaryngol Head Neck Surg. 2018;144(10):929-937. doi: 10.1001/jamaoto.2018.1671 [DOI] [PubMed] [Google Scholar]
- 142.Roskies M, Liu X, Hier MP, et al. 3-Phase dual-energy CT scan as a feasible salvage imaging modality for the identification of non-localizing parathyroid adenomas: a prospective study. J Otolaryngol Head Neck Surg. 2015;44:44. doi: 10.1186/s40463-015-0098-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Woisetschläger M, Gimm O, Johansson K, Wallin G, Albert-Garcia I, Spångeus A. Dual energy 4D-CT of parathyroid adenomas not clearly localized by sestamibi scintigraphy and ultrasonography—a retrospective study. Eur J Radiol. 2020;124:108821. doi: 10.1016/j.ejrad.2020.108821 [DOI] [PubMed] [Google Scholar]
- 144.Mapelli P, Busnardo E, Magnani P, et al. Incidental finding of parathyroid adenoma with 11C-choline PET/CT. Clin Nucl Med. 2012;37(6):593-595. doi: 10.1097/RLU.0b013e31824c5ffc [DOI] [PubMed] [Google Scholar]
- 145.Quak E, Lheureux S, Reznik Y, Bardet S, Aide N. F18-choline, a novel PET tracer for parathyroid adenoma? J Clin Endocrinol Metab. 2013;98(8):3111-3112. doi: 10.1210/jc.2013-2084 [DOI] [PubMed] [Google Scholar]
- 146.Evangelista L, Ravelli I, Magnani F, et al. 18F-choline PET/CT and PET/MRI in primary and recurrent hyperparathyroidism: a systematic review of the literature. Ann Nucl Med. 2020;34(9):601-619. doi: 10.1007/s12149-020-01507-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Risk of Bias and Applicability Concerns Graph Based on 15-Item Modified Quality Assessment of Diagnostic Accuracy Studies
eFigure 2. Funnel Plots for Eight Representative Categories of Various Imaging Modalities for pHPT Localization in Both Patient- and Lesion-Based Analyses
eFigure 3. Evidence Network Plots of Diagnostic Value of Eight Representative Categories of Various Imaging Modalities for pHPT Localization in Both Patient- and Lesion-Based Analyses
eTable 1. Search Queries
eTable 2. Characteristics of the Enrolled Studies
eReferences