Abstract
Tooth-related diseases and tooth loss are widespread and are a major public health issue. The loss of teeth can affect chewing, speech, appearance and even psychology. Therefore, the science of tooth regeneration has emerged, and attention has focused on tooth regeneration based on the principles of tooth development and stem cells combined with tissue engineering technology. As undifferentiated stem cells in normal tooth tissues, dental mesenchymal stem cells (DMSCs), which are a desirable source of autologous stem cells, play a significant role in tooth regeneration. Researchers hope to reconstruct the complete tooth tissues with normal functions and vascularization by utilizing the odontogenic differentiation potential of DMSCs. Moreover, DMSCs also have the ability to differentiate towards cells of other tissue types due to their multipotency. This review focuses on the multipotential capacity of DMSCs to differentiate into various tissues, such as bone, cartilage, tendon, vessels, neural tissues, muscle-like tissues, hepatic-like tissues, eye tissues and glands and the influence of various regulatory factors, such as non-coding RNAs, signaling pathways, inflammation, aging and exosomes, on the odontogenic/osteogenic differentiation of DMSCs in tooth regeneration. The application of DMSCs in regenerative medicine and tissue engineering will be improved if the differentiation characteristics of DMSCs can be fully utilized, and the factors that regulate their differentiation can be well controlled.
Keywords: Dental mesenchymal stem cells, Regenerative medicine, Tissue engineering, Multipotency, Odontogenic differentiation, Osteogenic differentiation
Core Tip: Dental mesenchymal stem cells have been widely used in tissue engineering and regenerative medicine due to their multipotential differentiation ability. We herein discuss the multipotency of dental mesenchymal stem cells and some related factors influencing the odontogenic/osteogenic differentiation, which provide guidance for fully utilizing the multipotency of dental mesenchymal stem cells.
INTRODUCTION
Over the past three decades, in the search for treatments for a variety of degenerative diseases and irreversible forms of tissue and organ damage, the emerging field of tissue engineering and regenerative medicine (TERM) has attracted a lot of interest, and great efforts have been made to realize the regeneration of different types of tissues and organs to restore normal physiology and body function. As one of the important aspects of regenerative medicine, tissue engineering mainly takes advantages of the following three methods: (1) Cell/biomaterial complex systems with cell-seeded biomaterials implanted into the body to restore and regenerate tissues/organs; (2) Cell systems, such as stem cell transplantation; and (3) Biomaterial systems implanted into the body and integrated into tissues[1]. As a vital part of TERM, a suitable source of stem cells is a significant initial requirement. Since the 1990s, the field of stem cell biology has gradually developed and rapidly become a main research trend in regenerative medicine. Induced pluripotent stem cells, progenitor cells from various tissues, human embryonic stem cells and adult stem cells are all potential seed cells for TERM[2]. Cells derived from induced pluripotent stem cells or differentiated from human embryonic stem cells can be used to build related tissue cell models. Progenitor cells and adult stem cells from various tissues can differentiate into mature tissues.
As adult stem cells, dental mesenchymal stem cells (DMSCs), including dental pulp stem cells (DPSCs), periodontal ligament stem cells (PDLSCs), stem cells from apical papilla (SCAPs), gingival mesenchymal stem cells (GMSCs), stem cells from human exfoliated deciduous teeth (SHED) and dental follicle stem cells (DFSCs) have been widely studied because of their ready availability, easy accessibility and lack of complex ethical issues. DMSCs have multiple differentiation potential and can differentiate into a variety of tissue-like cells under specific induction conditions, providing potential seed cells for TERM. For example, SHED are capable of inhibiting bone loss, decreasing neuronal apoptosis and forming pancreatic islet-like clusters[3-5]. DPSCs can differentiate into myogenic lineage and corneal stromal-like constructs[6,7] and can also reduce bone loss in an osteoporosis mouse model, prevent retinal ganglion cell loss and repair spinal cord injury[8-10].
DMSCs, in particular, have great potential for application in engineering regeneration of dental tissues. In 2006, Sonoyama et al[11] transplanted a hydroxyapatite/SCAP-Gelfoam/PDLSC structure into a swine alveolar socket, which regenerated mineralized root-like tissue and formed periodontal ligament space[11]. In 2012, Guo et al[12] identified a method of combining DFSCs with treated dentin matrix scaffolds in the alveolar fossa that proved to be a promising strategy for tooth root regeneration[12]. In 2013, Iohara et al[13] transplanted autologous DPSCs with granulocyte-colony stimulating factor into a dog pulpectomized tooth and found that newly formed pulp tissue, including innervation and vasculature, fully filled in the root canal[13].
Efforts have been made to promote tooth regeneration by DMSCs, but many factors affect this complex regeneration process, such as correlative non-coding RNAs, signaling pathways, inflammation, aging and exosomes. In the process of induced differentiation of DMSCs, many non-coding RNAs, including microRNAs and long noncoding RNAs (lncRNAs) and related signaling pathways are involved to regulate the expression of odontogenic/osteogenic differentiation genes. In addition, donor age, cell senescence and the complex oral inflammatory microenvironment also pose great challenges to tooth regeneration by DMSCs. Moreover, the hot topic of research in recent years, exosomes, which carry a variety of contents, have also captured the attention of researchers in inducing the differentiation of DMSCs. If we can regulate these factors well, it will enable a big step forward in the application of DMSCs in the field of tooth regeneration. This review focuses on the multidirectional differentiation potential of DMSCs and the effect of the above-mentioned factors on the odontogenic/ osteogenic differentiation of DMSCs in the field of tooth regeneration, hoping to provide a reference for the efficient use of DMSCs.
DIVERSE DIFFERENTIATION OF DMSCS
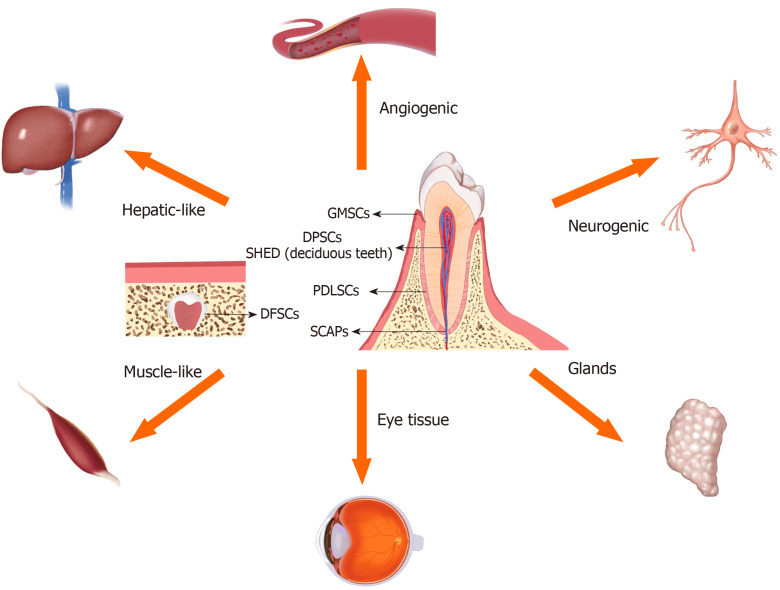
In addition to the odontogenic differentiation ability of DMSCs, in recent years the research on the differentiation of DMSCs into other tissue-like cells, such as osteogenesis, chondrogenesis, angiogenesis, neurogenesis and differentiation potential toward tendon-like cells, insulin-producing cells, hepatic-like cells, corneal stromal-like cells, etc. has become popular (Figure 1). To explore the diverse differentiation ability of DMSCs is an issue worth exploring.
Figure 1.
Location of dental mesenchymal stem cells and their diverse differentiation potential. Dental mesenchymal stem cells can be isolated from different tissues of the teeth. Dental mesenchymal stem cells have multidifferentiation ability and can differentiate into many tissue-like cells. DPSCs: Dental pulp stem cells; PDLSCs: Periodontal ligament stem cells; SCAPs: Stem cells from apical papilla; GMSCs: Gingival mesenchymal stem cells; SHED: Stem cells from human exfoliated deciduous teeth; DFSCs: Dental follicle stem cells.
DPSCs
In 2000, Gronthos et al[14] identified that DPSCs can form alizarin red-positive condensed nodules with high levels of calcium cultivated by L-ascorbate-2-phosphate, glucocorticoid, dexamethasone and inorganic phosphate[14]. As a seed cell for bone regeneration, DPSCs usually attached to some materials for bone defect models. For example, Wongsupa et al[15] fabricated a scaffold combination of poly-ε-caprolactone–biphasic calcium phosphate with the modified melt stretching and multilayer deposition technique seeded with human DPSCs (hDPSCs), which increased the newly formed bone in calvarial defects rabbit models[15]. However, Jin et al[16] showed that adipose tissue-derived stem cells exhibited greater osteogenic differentiation potential compared to DPSCs[16].
In vitro, DPSCs can differentiate into chondroblasts, which suggests that it can be useful for cartilage injuries[17]. CD146 marked DPSCs can express the chondrogenic inducing factor transforming growth factor (TGF)-β3 and form three-dimensional cartilage constructs when seeded on poly-L-lactic acid/polyethylene glycol electrospun fiber scaffolds[18]. Costal chondrocytes are able to supply a chondro-inductive niche that promote the DPSCs to undergo chondrogenic differentiation and enhance the formation of cartilage[19]. Xenotransplantation of DPSCs in platelet-rich plasma and 3% alginate hydrogels significantly regenerated cartilage in rabbit models of cartilage damage[20,21].
In 2016, Chen et al[22] first identified expression of tendon-related markers such as scleraxis, tenascin-C, tenomodulin, eye absent homologue 2, collagen I and collagen VI in dental pulp tissues. Also, DPSCs seeded in aligned polyglycolic acid fiber scaffolds can promote the expression of tendon-related markers under mechanical stimulation and form mature tendon-like tissue in a mouse model[22]. As neural crest-derived cells, DPSCs can be induced to differentiate into neuron-like cells with the use of growth factors, including basic fibroblast growth factor and epidermal growth factor, which are preferable to the chemical-induction method[23-25]. DPSCs transplanted into a rat model of middle cerebral artery occlusion, peripheral nerve injuries and retinal injury expressed related neuronal markers[26-28].
Three-dimensional culture promoted the differentiation of hDPSCs into insulin-producing cells[29], and pancreatic islets were also generated from DPSCs[30]. The potential toward insulin-producing cells of hDPSCs was superior to human PDLSCs (hPDLSCs)[31]. DPSCs also exhibited angiogenic potential when implanted into mouse brain and into a rat model of acute myocardial infarction by promoting neovasculogenesis[32,33]. Furthermore, DPSCs differentiated into bladder smooth muscle cells in a particular culture medium[34], while the Wnt-GSK3β/β-catenin pathway played an important role in this process[35]. DPSCs had the potential to form a high-purity hepatic lineage when cultured in serum-free medium[36], and DPSCs derived from cryopreserved dental pulp tissue of vital extracted diseased teeth also showed the potential to differentiate into hepatic-like cells[37]. Additionally, DPSCs had the capacity to differentiate into melanocyte-like cells when cultured in a specific melanocyte differentiating medium[38].
PDLSCs and GMSCs
PDLSCs have great osteogenic differentiation potential. Kato et al[39] observed that PDLSCs have the highest levels of some bone differentiation markers without osteogenic differentiation among mesenchymal stromal cells derived from bone marrow and adipose-derived mesenchymal stem cells[39]. Seeded on nanohydroxyapatite-coated genipin-chitosan conjunction scaffold, PDLSCs exhibited significantly greater viability and alkaline phosphatase activity and promoted calvarial bone repair[40]. Moshaverinia et al[41,42] reported that PDLSCs and GMSCs capsulated in an injectable arginine-glycine-aspartic acid tripeptide-coupled alginate microsphere delivery system promoted bone regeneration and chondrogenesis, respectively, for a calvarial defect animal and subcutaneous implantation of nude mice, and PDLSCs showed significantly higher osteogenic and chondrogenic differentiation capability compared with GMSCs.
In 2021, Shen et al[43] showed that 6-bromoindir-ubin-3’-oxime promoted mineralized nodule formation in PDLSCs[43]. PDLSCs from beagle dogs and humans can both be induced to differentiate into neural-like cells by various protocols[44,45], and the Wnt/β-catenin signaling pathway has been implicated in this process[46]. Bueno et al[47] found that the nuclear shape of hPDLSC-derived neural-like cells was similar to cells in neurogenic niches from adult mouse brain, and no cell proliferation occurred in the course of neurogenesis. The potential for neurogenesis is improved by the addition of specific short peptides or phytocompounds[48-50]. As another stem cell type derived from periodontal tissue, GMSCs also have neurogenic differentiation potential and displayed action potential capacity when tested by a neurosphere-mediated induction method[51], while hypoxia preconditioning activated more genes associated with neuronal development[52]. In addition, over prolonged passages, human GMSCs have been found to spontaneously differentiate into neural precursor cells[53].
Encapsulated PDLSCs and GMSCs in an alginate/hyaluronic acid three-dimensional scaffold promoted the regeneration of neurogenic tissue[54]. Besides, PDLSCs had the ability to differentiate into corneal stromal keratocyte-like cells[55] and constructed a multilamellar human corneal stromal-like tissue in vitro when seeded onto orthogonally aligned, multilayered silk membranes and supplemented with the neuropeptide substance P[56]. PDLSCs also could be directed to develop into retinal progenitors and islet-like cell clusters with competence for photoreceptor differentiation and secretion of insulin[57,58]. Moreover, both PDLSCs and GMSCs differentiated into tendon-like cells using an injectable and biodegradable arginine-glycine-aspartic acid tripeptide-coupled alginate hydrogel scaffold[59]. The GMSCs could also be induced to differentiate into functional keratinocytes when treated with Acalypha indica in a three-dimensional microenvironment[60].
DFSCs
Human DFSCs can differentiate to osteogenic lineage cells in osteogenic induction medium without dexamethasone, and BMP6 is a key gene in the osteogenic differentiation[61]. Plasma rich in growth factors and soluble silica can promote osteogenic differentiation of DFSCs[62,63]. Lucaciu et al[64] indicated that DFSCs could be used for promoting bone regeneration on titanium implant surfaces[64]. DFSCs were loaded into poly-ε-caprolactone scaffold and implanted into skulls defects of Sprague Dawley rats, and bone regeneration was observed[65]. Undifferentiated DFSCs expressed some neural markers, such as nestin, β-III-tubulin and S100β and exhibited a spindle-like morphology[66]. Using a two-step strategy for neuronal differentiation, DFSCs could be differentiated into neurosphere-like cell clusters, and finally developed a cellular morphology with small bodies and long cellular extrusions while exhibiting increased expression of neural cell markers[67].
It has been suggested that human DFSCs may have the potential to differentiation toward the glial lineage rather than the neuronal lineage[66]. Induced cardiomyocytes derived from DFSCs, which were cultured in medium with suberoylanilide hydroxamic acid, could be intraperitoneally injected into experimental mice and exhibited homing capacity into the heart muscle[68]. Comparing the differentiation potential toward pancreatic β cell-like cells among the stem cells from dental pulp, papilla and follicle, the DFSCs demonstrated higher potency and secreted more insulin upon glucose challenge[69]. Furthermore, epithelial stem-like cells from the human dental follicle were able to differentiate into salivary gland acinar and duct cells[70].
SHED
SHED represent a promising cell source for bone regeneration, which are usually combined with many biomaterials. Combined hydroxyapatite scaffold and SHED can promote alveolar bone regeneration, and interleukin-17A can enhance osteogenic differentiation of SHED, both due to increasing osteoprotegerin/receptor activator of nuclear factor κB ligand ratio[71,72]. FGF-2 pretreated SHED represent a faster formation of intramembranous bone after implanted in craniofacial bone defects than hypoxia pretreated[73]. A carbon nanomaterial named graphene oxide quantum dots promotes osteogenic differentiation of SHED via the Wnt/β-catenin signaling pathway[74]. In addition, SHED have the chondrogenic differentiation ability. After transplantation into the subcutaneous space on the back of nude mice, SHED recombined with β-TCP scaffolds were able to produce new cartilage-like tissues[75].
In 2011, SHED were successfully induced to differentiate into neural-like cells by a simple short-term growth factor-mediated induction protocol[76], and then in 2013, a novel three-stage method was established[77]. Yang et al[78] found that Noggin overexpression combined with the Rho kinase inhibitor Y-27632 exhibited a synergistic effect in promoting differentiation of SHED into neuron-like cells[78]. The lncRNA C21orf121 promotes SHED differentiation into neuronal cells by upregulating the expression of BMP2, acting as a competing endogenous RNA to compete with BMP2 binding to miR-140-5p[79]. SHED in polyglycolic acid tubes combined with autografting can regenerate the mandibular branch of the rat facial nerve[80]. Also, SHED have been used to repair a Parkinsonian rat model, an acute contused spinal cord injury model and a model of diabetic peripheral neuropathy[81-83].
In addition, SHED can differentiate into angiogenic endothelial cells, and when cultured with decellularized extracellular matrix of human umbilical vein endothelial cells can improve endothelial differentiation[84,85]. Using shear stress via the downstream pathway of vascular endothelial-derived growth factor-Notch signaling or by inhibiting TGF-β signaling in SHED can enhance endothelial differentiation[86,87]. SHED transplanted into immunodeficient mice using Matrigel with human umbilical vein endothelial cells form extensive vessel-like structures[88].
SHED also have the potential for hepatic differentiation, which can be improved by using liquorice or angelica extracts in the culture medium[89]. CD117+ SHED hepatically differentiated in vitro were used to repair either acute liver injury or induced secondary biliary cirrhosis in a rat model[90]. Meanwhile SHED or SHED-converted hepatocyte-like cell-based spheroids transplanted into a CCl4-induced chronic liver fibrosis mouse model improved hepatic dysfunction[91,92].
Furthermore, SHED can differentiate into epidermal cells and accelerate wound repair when seeded onto polyvinyl alcohol/silk fibroin nanofiber dressings[93]. CD117+ SHED also have the potential to differentiate toward all functional endocrine and exocrine subsets of pancreatic cells in serum-free conditions[94]. When cocultured with immortal corneal epithelium cells in vitro, SHED display the potential for transdifferentiation to corneal epithelium-like cells[95]. Li et al[96] indicated that SHED can transdifferentiate into retinal photoreceptor-like cells in vitro and retain good viability in vivo after transplantation into mice with a normal immune system[96]. Moreover, functional smooth muscle cells can be differentiated from SHED by TGF-β1 induction, while the ALK5 signaling pathway may regulate this process[97].
SCAPs
In 2020, Deng et al[98] reported that platelet derived growth factor BB promoted SCAPs osteogenic differentiation and enhanced bone formation in calvarial defects combined with a thermosensitive hydrogel[98]. Both conditioned culture medium containing traditional Chinese herbal remedy, Yunnan Baiyao, and high glucose α-Minimal Essential Medium can promote the odonto/osteogenic differentiation of SCAPs through the nuclear factor κB signaling pathway[99,100]. Depletion of lysine-specific demethylase 2A enhanced the adipogenic and chondrogenic differentiation potentials of SCAPs[101]. In 2020, Yang et al[102] reported that DLX5 and HOXC8 enhanced the expression of chondrogenic markers including type II collagen, type V collagen and sex-determining region Y box protein 9[102].
In 2017, Kim et al[103] first formed a three-dimensional cell-based nerve-like tissue with axons and myelin structures using SCAPs through a three-dimensional organotypic culture method[103]. The secreted frizzled-related protein 2, a Wnt signaling modulator, and insulin-like growth factor (IGF)-2 improved the neurogenic differentiation potential of SCAPs[104,105]. Adding graphene dispersion and water-soluble single-walled carbon nanotubes to the neuroinductive medium enhanced the neural differentiation of SCAPs[106].
SCAPs show angiogenic potential, and SCAPs and/or DPSCs transplanted in three-dimensional-printed hydroxyapatite scaffolds can form vascularized dentin/pulp-like tissue[107]. Coculture of human umbilical vein endothelial cells and SCAPs under hypoxic conditions promotes the construction of vessel-like structures in vitro, and ephrinB2 may play an important role in stabilizing the vascular-like structures[108,109]. Furthermore, erythropoietin enhances the endothelial differentiation of SCAPs[110]. In addition, SCAPs also have hepatogenic potential[111], and mesenchymal stem cells derived from dental papilla can also be differentiated into pancreatic β cell-like cells[69].
MULTIPLE FACTORS INFLUENCING THE ODONTOGENIC/OSTEOGENIC DIFFERENTIATION OF DMSCS
MicroRNAs
MicroRNAs (miRNAs) play important roles in regulating the tooth regeneration process (Table 1). Downregulation of miR-143-5p and miR-143-3p promotes the odontoblastic differentiation of DPSCs through the osteoprotegerin/receptor activator of nuclear factor κB ligand signaling pathway[112,113]. Acting via the p38 mitogen-activated protein kinases (MAPK) signaling pathway, downregulated miR-143-5p and miR-488 are capable of inducing DPSCs to differentiate into odontoblast-like cells by targeting MAPK14 and MAPK1, respectively[114,115]. Wang et al[116] found that miR-125a-3p regulates odontoblastic differentiation of DPSCs in an inflammation model by targeting Fyn, a member of the protein tyrosine kinase Src family[116].
Table 1.
Summary of the microRNAs influencing the odontogenic/osteogenic differentiation of dental mesenchymal stem cells
| Ref. | MicroRNA | Cell type | Signaling pathway or targets | Outcome |
| Zhan et al[112], 2018 | miR-143-5p | DPSCs | OPG/RANKL | Downregulation promoted odontoblastic differentiation |
| Yang et al[113], 2020 | miR-143-3p | DPSCs | OPG/RANKL | Downregulation promoted odontogenic differentiation |
| Wang et al[114], 2019 | miR-143-5p | DPSCs | MAPK14 | Downregulation promoted odontoblastic differentiation |
| Yu et al[115], 2019 | miR-488 | DPSCs | MAPK1 | Downregulation enhanced odontoblastic differentiation |
| Wang et al[116], 2020 | miR-125a-3p | DPSCs | Fyn | Regulated odontoblastic differentiation in an inflammation model |
| Yuan et al[117], 2019 | miR-let-7c-5p | Inflamed human DPSCs | - | Restored the osteogenic differentiation |
| Huang et al[118], 2019 | miR-223-3p | Inflamed human DPSCs | - | Increased the proteins levels of DSPP and DMP-1 |
| Sun et al[119], 2017 | miR-140-5p | DPSCs | - | Inhibited odontoblastic differentiation after LPS treated |
| Liu et al[120], 2019 | miR-508-5p | DPSCs | GPNMB | Inhibited odontogenic differentiation |
| Xu et al[121], 2018 | miR-21 | DPSCs | STAT3 | Downregulation caused the decreasing expression of DMP-1 and DSPP |
| Qiu et al[122], 2019 | miR-146a-5p | STRO-1 + human DPSCs | - | Promoted osteo/odontogenic differentiation |
| Zhang et al[123], 2018 | miR-143 | DPSCs | TNF-α/NF-κB | Suppressed the osteogenic differentiation |
| Yao et al[124], 2019 | miR-215, miR-219a-1-3p | DPSCs | HspB8 | Inhibited the osteogenic differentiation |
| Wei et al[125], 2017 | miR-21 | PDLSCs | Smad5 | Inhibited osteogenesis |
| Li et al[126], 2019 | miR-24-3p | PDLSCs | Smad5 | Inhibited osteogenic differentiation |
| Wei et al[127], 2015 | miR-21 | PDLSCs | ACVR2B | Performed a positive function in mediating the stretch-induced osteogenic differentiation |
| Yao et al[128], 2017; Cao et al[129], 2017 | miR-214 | PDLSCs | ATF4, Wnt/β-catenin | Downregulation decreased the osteogenic differentiation |
| Bao et al[130], 2019 | miR-148a | PDLSCs | - | Downregulation rescued the inhibition of osteogenesis triggered by LPS stimulation |
| Yan et al[131], 2017 | miR-22 | PDLSCs | HDAC6 | Promoted osteogenesis |
| Li et al[132], 2018 | miR-17 | PDLSCs | HDAC9 | Promoted osteogenesis in an inflammation condition |
| Xu et al[133], 2019 | miR-132 | PDLSCs | GDF5, NF-κB | Inhibited the osteogenesis |
| Zhen et al[134], 2017 | miR-31 | PDLSCs | Satb2 | Took part in the high glucose-suppressed osteogenic differentiation |
| Wan et al[135], 2012 | miR-34a | Human dental papilla cells | - | Increased the expression of DSPP and decreased the expression of ALP |
| Sun et al[136], 2014 | miR-34a | SCAPs | - | Upregulated odonto/osteogenic markers |
| Wang et al[137], 2018 | miR hsa-let-7b | SCAPs | MMP1 | Suppressed the odonto/osteogenic differentiation |
| Dernowsek et al[138], 2017 | miR-450a-5p,miR-28-5p | SHED | - | Supported the osteogenesis |
| Klingelhöffer et al[139], 2016 | miR-101 | DFSCs | - | Enhanced the osteogenic differentiation |
| Han et al[140], 2019 | miR-3940-5p | GMSCs | - | Promoted the osteo/dentinogenic differentiation |
DPSCs: Dental pulp stem cells; PDLSCs: Periodontal ligament stem cells; SCAPs: Stem cells from apical papilla; MAPK: Mitogen-activated protein kinases; OPG/RANKL: Osteoprotegerin/receptor activator of nuclear factor κB ligand; GPNMB: Glycoprotein nonmetastatic melanomal protein B; TNF-α: Tumor necrosis factor-α; NF-κB: Nuclear factor κB; ATF4: Activating transcription factor 4; LPS: Lipopolysaccharide; DSPP: Dentine sialophosphoprotein; ALP: Alkaline phosphatase; SHED: Stem cells from human exfoliated deciduous; GMSCs: Gingival mesenchymal stem cells; DFSCs: Dental follicle stem cells; HspB8: Heat shock protein B8; ACVR2B: Activin receptor type IIB; GDF5: Growth differentiation factor 5; MMP1: Matrix metalloproteinase 1; miR: MicroRNA; DMP-1: Dentine matrix protein 1; Smad5: SMAD family member 5.
Meanwhile miR-let-7c-5p can restore the osteogenic differentiation of inflamed DPSCs by suppressing the lipopolysaccharide (LPS)-induced inflammatory phenomena[117]. In inflamed pulp tissues, miR-223-3p is remarkably upregulated, and overexpression of miR-223-3p in DPSCs can increase the protein levels of dentine sialophosphoprotein (DSPP) and dentine matrix protein 1[118]. Sun et al[119] found that during LPS-mediated odontoblastic differentiation of DPSCs, the expression of miR-140-5p is markedly decreased, while when miR-140-5p is expressed in DPSCs after LPS treatment, the odontoblastic differentiation ability is inhibited[119].
Additionally, during odontogenesis of hDPSCs, the expression of miR-508-5p decreases gradually, while significant inhibition of odontogenesis is observed after overexpression of miR-508-5p, which targets glycoprotein nonmetastatic melanomal protein B[120]. Xu et al[121] reported that during odontoblast differentiation of DPSCs, the expression of miR-21 can be regulated by treating with TNF-α, while downregulation of miR-21 causes a decrease in the expression of dentine matrix protein 1 and DSPP by interacting with STAT3[121]. Moreover, miR-146a-5p promotes odontogenic/ osteogenic differentiation of STRO-1+ DPSCs[122]. miR-143 suppresses the osteogenic differentiation of DPSCs by regulating the TNF-α/nuclear factor κB pathway[123], while miR-215 and miR-219a-1-3p inhibit the osteogenic differentiation capability of DPSCs by downregulation of heat shock protein B8[124].
During osteogenic differentiation of PDLSCs, the expression of miR-21 and miR-24-3p decrease, and their downregulation markedly inhibits osteogenesis of hPDLSCs by targeting SMAD family member 5 (Smad5)[125,126]. miR-21 also performs a positive function in mediating the stretch-induced osteogenic differentiation of hPDLSCs by regulating the expression of activin receptor type IIB[127]. Inhibition of miR-214 in PDLSCs can decrease osteogenic differentiation by targeting activating transcription factor 4 and regulating the Wnt/β-catenin signaling pathway[128,129]. Downregulation of miR-148a in PDLSCs rescues the inhibition of osteogenesis triggered by LPS stimulation[130]. miR-22 and miR-17 promote osteogenesis of PDLSCs by inhibiting HDAC6 and HDAC9 expression, respectively, the latter under inflammatory conditions[131,132]. In addition, in osteogenic differentiation of PDLSCs, miR-132 decreases, and overexpression of miR-132 inhibits osteogenesis by targeting growth differentiation factor 5 and activating the nuclear factor κB signaling pathway[133]. Meanwhile miR-31 plays a role in the high glucose-suppressed osteogenic differentiation of PDLSCs by targeting Satb2[134].
Upregulation of miR-34a in human fetal dental papilla cells increases the expression of DSPP and decreases the expression of alkaline phosphatase (ALP)[135]. In addition, miR-34a mimic transfection in SCAPs significantly upregulates odontogenic/ osteogenic markers[136]. miR-hsa-let-7b suppresses the odontogenic/ osteogenic differentiation of SCAPs partly by targeting matrix metalloproteinase 1[137]. Moreover, overexpression of miR-450a-5p or miR-28-5p in SHED supports osteogenesis[138]. miR-101 enhances osteogenic differentiation in human DFSCs[139], and miR-3940-5p promotes the osteo/dentinogenic differentiation of GMSCs[140].
LncRNAs
LncRNAs significantly regulate the multiple differentiations of mesenchymal stem cells, and there are several reports of the regulatory effect of lncRNAs in regenerative engineering of dental-tissue-derived stem cells (Table 2). In 2020, Liu et al[141] identified a total of 89 lncRNAs differentially expressed after osteo/odontogenic induction of hDPSCs, and downregulation of lncRNA SNHG7 was found to inhibit the differentiation of DPSCs, upregulating the expression of miR-1226-3p and miR-210-5p at the same time[141]. In 2020, Chen et al[142] reported that 132 lncRNAs were differentially expressed between the odontoblastic-differentiated and undifferentiated hDPSCs and that lncRNA-G043225 exerted a positive regulatory effect through miR-588 and fibrillin 1[142]. Additionally, 47 lncRNAs were differentially expressed in hDPSCs between normoxic and hypoxic induction conditions, and 561 lncRNAs were differentially expressed between young and old donors in hDPSCs after osteoinduction[143,144]. Overexpression of lncRNAs CCAT1 and lncRNA H19 promotes odontogenic differentiation of hDPSCs by inhibiting expression of miR-218 and regulating expression of the DLX3 gene, respectively[145,146]. Knockdown of lncRNA STL and lncRNA X-inactive specific transcript inhibits the osteogenic potential of DPSCs, and the latter is essential for efficient osteogenic differentiation induced by TNF-α[143,147].
Table 2.
Summary of the long noncoding RNAs influencing the odontogenic/osteogenic differentiation of dental mesenchymal stem cells
| Ref. | LncRNA | Cell type | Signaling pathway or targets | Outcome |
| Liu et al[141], 2020 | lncRNA SNHG7 | DPSCs | miR-1226-3p, miR-210-5p | Downregulation inhibited osteo/odontogenic differentiation |
| Chen et al[142], 2020 | lncRNA-G043225 | DPSCs | miR-588, FBN1 | Positively regulated odontoblastic differentiation |
| Zhong et al[145], 2019 | lncRNA CCAT1 | DPSCs | miR-218 | Overexpression promoted odontogenic differentiation |
| Zeng et al[146], 2018 | lncRNA H19 | DPSCs | DLX3 | Upregulation enhanced odontogenic differentiation |
| Shi et al[143], 2019 | lncRNA STL | DPSCs | - | Knockdown inhibited osteogenesis |
| Tao et al[147], 2019 | lncRNA XIST | DPSCs | - | Downregulation inhibited osteogenic differentiation |
| Zheng et al[149], 2018 | lncRNA MEG8, lncRNA MIR22HG | PDLSCs | - | Downregulation suppressed osteogenic differentiation |
| Liu et al[150], 2019; Deng et al[151], 2018 | lncRNA MEG3 | PDLSCs | miR-27a-3p/IGF1 axis, Wnt/β-catenin | Knockdown inhibited osteogenesis |
| Wang et al[152], 2016 | lncRNA-POIR | PDLSCs | miR-182 | Enhanced osteogenic differentiation |
| Xu et al[153], 2019 | lncRNA-TWIST1 | PDLSCs | TWIST1 | Improved osteogenic differentiation |
| Jia et al[154], 2019 | lncPCAT1 | PDLSCs | - | Reversed the suppression effect of osteogenesis caused by miR-106a-5p overexpression |
| Huang et al[155], 2020 | lncRNA FER1L4 | PDLSCs | miR-874-3p | Promoted osteogenic differentiation |
| Feng et al[156], 2020 | lncRNA XIST | PDLSCs | miR-214-3p | Enhanced osteogenic differentiation |
| He et al[160], 2018 | lncRNA TUG1 | PDLSCs | lin-28 homolog A | Improved osteogenic differentiation |
| Wang et al[161], 2020 | lncRNA DANCR | PDLSCs | - | Positively regulated osteogenic differentiation |
| Li et al[162], 2019 | lncRNA H19 | SCAPs | lncRNA-H19/miR-141/SPAG9/MAPK | Promoted the osteo/odontogenesis |
| Jia et al[157], 2016; Jia et al[158], 2015; Peng et al[159], 2018 | lncRNA ANCR | DPSCs, PDLSCs, SCAPs | Wnt, lncRNA-ANCR/miR-758/Notch2 (PDLSCs) | Downregulation facilitated osteogenic differentiation |
DPSCs: Dental pulp stem cells; FBN1: Fibrillin 1; lncRNAs: Long noncoding RNAs; MAPK: Mitogen-activated protein kinases; MEG3/8: Maternally-expressed 3/8; miR: MicroRNA; IGF1: Insulin-like growth factor 1; PDLSCs: Periodontal ligament stem cells; SCAPs: Stem cells from apical papilla; XIST: X-inactive specific transcript.
In 2016, Qu et al[148] demonstrated that 2171 lncRNAs were differentially expressed between osteogenic-differentiated and undifferentiated PDLSCs, and 393 lncRNAs were strongly associated with osteogenesis-related mRNAs[148]. Zheng et al[149] indicated that downregulation of lncRNA maternally-expressed 8 and lncRNA MIR22HG markedly suppressed the osteogenic differentiation of PDLSCs[149]. Knockdown of lncRNA maternally-expressed 3 inhibits the osteogenesis of PDLSCs in periodontitis via the miR-27a-3p/IGF1 axis, while it plays a positive role in human DFSCs by activating the Wnt/β-catenin signaling pathway[150,151]. In 2016, Wang et al[152] identified a novel lncRNA named lncRNA-POIR, while Xu et al[153] first named lncRNA-TWIST1 in 2019; both are osteogenesis impairment-related lncRNAs of PDLSCs from periodontitis patients and can enhance the osteogenic differentiation of PDLSCs from healthy individuals and periodontitis patients by interacting with miR-182 and inhibiting TWIST1 expression, respectively[152,153]. Prostate cancer-associated ncRNA transcript-1 upregulation reverses the suppression effect of osteogenic differentiation in PDLSCs caused by miR-106a-5p overexpression[154].
LncRNA FER1L4 and lncRNA X-inactive specific transcript can promote the osteogenesis of PDLSCs by sponging miR-874-3p and miR-214-3p, respectively[155,156]. In addition, downregulation of antidifferentiation noncoding RNA can facilitate the osteogenic differentiation of DPSCs, PDLSCs and SCAPs[157], while this regulatory effect on PDLSCs is related to the canonical Wnt signaling pathway[158]. The antidifferentiation noncoding RNA/miR-758/Notch2 axis may also participate[159]. Furthermore, lncRNA TUG1 improves osteogenic differentiation of PDLSCs by regulating the expression of lin-28 homolog A[160]. Knockdown of lncRNA differentiation antagonizing nonprotein coding RNA positively regulates the osteogenic differentiation of PDLSCs[161]. Moreover, lncRNA H19 overexpression promotes the osteo/odontogenesis of SCAPs via the lncRNA-H19/miR-141/SPAG9/MAPK positive feedback loop[162].
Signaling pathways
Wnt signaling pathway: The Wnt/β-catenin signaling pathway plays an important role in regulating DMSC differentiation, which is a key signaling pathway. For odontoblastic differentiation, activating the Wnt/β-catenin signaling pathway partially reverses the vacuolar protein sorting 4B knockdown-driven suppression of odontoblastic differentiation of hDPSCs[163] and rescues the osteoblastic/odontoblastic differentiation of stathmin-deletion hDPSCs[164]. These studies revealed that activation of the Wnt signaling pathway promotes osteogenic/odontoblastic differentiation of DPSCs. However, Scheller et al[165] first reported that Wnt/β-catenin inhibits odontoblastic differentiation of DPSCs in 2008[165]. The reason for the conflicting effects of Wnt signaling on odontoblastic differentiation in these studies is undefined and needs to be further explored. For osteoblastic differentiation, Rolph et al[166] confirmed that ferutinin promoted osteoblastic differentiation of DPSCs by modulating the Wnt/β-catenin signaling pathway[166] when Wnt5a was reported to inhibit osteoblastic differentiation of human periodontal ligament stem cell-like cells[167].
MAPK signaling pathway: The MAPK signaling pathway includes the ERK signaling pathway and the p38/MAPK signaling pathway[168]. In odontoblastic differentiation, one study showed that a combination of mineral trioxide aggregate and propolis significantly promoted the expression of DSPP and Dentine matrix protein 1 as well as mineralized nodule formation through activating the ERK signaling pathway in hDPSCs[169]. Kong et al[170] confirmed that a magnesium-enriched microenvironment enhanced the odontoblastic differentiation of hDPSCs by activating the ERK/BMP2/Smad signaling pathway[170]. In osteoblastic differentiation, berberine was reported to bind to epidermal growth factor receptor in hPDLSCs to activate the ERK signaling pathway and upregulate the nuclear-related gene FOS, thus promoting osteoblastic differentiation of PDLSCs[171]. In addition, mineral trioxide aggregate was confirmed to promote osteo/odontoblastic differentiation of SCAP through activation of the p38 and ERK signaling pathway. Another study showed that parathyroid hormone promoted the osteo/odontoblastic differentiation of DPSCs by activating the ERK and p38 signaling pathway[172].
Mechanistic target of rapamycin signaling pathway: Mechanistic target of rapamycin (mTOR), a highly conserved serine/threonine protein kinase, is involved in regulating interactions between proteins[173]. The mTOR signaling pathway has been confirmed to play a significant role in the osteo/odontoblastic differentiation of DMSCs. Tanaka et al[174] confirmed that inhibiting mTOR signaling promoted osteo/odontoblastic differentiation of SCAPs[174]. However, activation of the mTOR signaling pathway promoted osteogenic differentiation of hDPSCs in the process regulated by IGF-1 in which rapamycin blocked osteogenic differentiation induced by IGF-1[175] while inhibiting mTORC1 limited mineralized nodule formation by SHED[176]. Taken together, these data suggest that the mTOR signaling pathway plays different roles in different cell types of DMSCs.
AKT signaling pathway: The AKT signaling pathway is critical for cell proliferation, growth, metabolism and differentiation, especially in differentiation of DMSCs. Recent studies have shown that metformin and miR-let-7c-5p enhance the osteogenic differentiation of PDLSCs by activation of the AKT signaling pathway[117,177]. Another study reported that activation of the AKT signaling pathway could enhance the osteogenic differentiation of DPSCs in LPS-induced inflammation. In short, the AKT signaling pathway may play a positive role in odontogenic/osteogenic differentiation of DMSCs.
Notch and shh signaling pathway: The Notch signaling pathway is critical for development and cell differentiation. Notch signaling has been confirmed to inhibit odontoblastic differentiation of hDPSCs[178]. Interestingly, another study showed that overexpression of CCN3 activated the Notch signaling pathway to promote odontoblastic differentiation of DPSCs, which suggested that Notch signaling pathway activation promotes odontoblastic differentiation of DPSCs[179]. The reasons for these contradictory effects in odontoblastic differentiation of DPSCs remain undefined and need to be explored.
It is worth noting that the Shh signaling pathway is also involved in odontogenic/ osteogenic differentiation of DMSCs. A recent study has shown that stathmin regulates odontogenic/osteogenic differentiation of DPSCs via the Shh signaling pathway[180].
Inflammation
In an inflammatory microenvironment, DMSCs from inflamed tissue contact and interact closely with extrinsic irritants, local cells or their components, immune cells and multiple soluble regulatory molecules[181]. For example, dental caries are one such gram-negative microbial infection that is primarily responsible for pulpal inflammation. LPS was used to create in vitro inflammatory conditions that initiate infection-stem cell interaction, which has been used widely to induce an inflammatory microenvironment[182].
Immunophenotyping of cell surface antigens by flow cytometry showed that DMSCs and inflamed DMSCs have similar expression patterns of surface markers[181,183]. The cells are positive for STRO-1, CD105, CD73, CD90, CD29 and CD44[184] and negative for CD45, CD34, CD14 and HLA-DR, indicating a mesenchymal stem cell phenotype[183,185-187]. In addition, inflamed DMSCs have the potential to differentiate into multiple lineages. Mesenchymal stem cells isolated from inflamed pulp possess stemness and multidifferentiation potential similar to DPSCs from healthy pulp[185]. Like DPSCs, inflamed DPSCs are capable of adipogenic and osteo/dentinogenic differentiation under the corresponding in vitro induction conditions. However, chronic inflammation impairs differentiation of DPSCs[188]. On the other hand, inflamed DPSCs show increased ALP and osteocalcin. In the inflammatory microenvironment, PDLSCs from inflamed periodontal tissue show higher proliferation rates but express lower levels of osteogenic differentiation markers[189-191]. Both inflamed hPDLSCs and hPDLSCs have been successfully differentiated under osteogenic and adipogenic conditions[192]. Because of evident similarities in their immunomodulatory properties, inflamed PDLSCs can provide a promising alternative to PDLSCs[193]. Cells isolated from human periapical cysts demonstrate a strong osteogenic but weak adipogenic capacity[184,194]. Osteogenic differentiation of inflamed DFSCs results in decreased ALP activity and alizarin red S staining compared to normal DFSCs[195]. Similarly, the osteogenic differentiation of LPS-treated DFSCs is suppressed, and the cells display low levels of TGF-β1 and high levels of TGF-β2.
Aging
Aging is an intricate degenerative process during which the regenerative capacity of MSCs progressively declines[196]. Unavoidably, DMSCs also undergo physiological age-related changes with declines in proliferation and osteo/odontogenic differentiation potentials with increased age[197,198]. Improving the performance of aging DMSCs is important for tissue regeneration engineering. Yi et al[144] demonstrated that the osteogenic potential of DPSCs from young donors was superior to that of those from old donors, and 304 mRNAs and 561 LncRNAs were differentially expressed between age-groups[144]. Wang et al[199] found that miR-433 may be one of the important senescence-related miRNAs of human dental pulp cells, which inhibits mineralization of human dental pulp cells by negatively regulating GRB2 and the RAS–MAPK signaling pathway[199]. SHED and DPSCs undergo senescence, including declines in the proliferation rate and osteogenic differentiation capability, following serial expansion from P4 to P20. SHED exhibit a better performance than DPSCs, which indicates that mineralization capacity is related to replicative senescence in vitro and to donor age[200].
As a significant factor regulating the function of differentiated odontoblasts[201], sclerostin advances the aging process of human dental pulp cells through the Wnt/β-catenin pathway and reduces the proliferation and odontoblastic differentiation capability of senescent human dental pulp cells[202]. The Wnt/β-catenin signaling pathway is one of the important pathways that regulates cell differentiation, increasing the osteogenic/dentinogenic differentiation potential of DPSCs[203]. It has been reported that the rate of dentin deposition and neurogenic differentiation potential declines with advanced age, which may be related to a decrease in endogenous Wnt/β-catenin signaling[204,205].
In 2014, Feng et al[206] compared the characteristics of DPSCs from five different age groups (5–12 years, 12–20 years, 20–35 years, 35–50 years and > 50 years) and found that the expression of p16INK4A markedly increased with age and inhibited osteogenic/odontogenic differentiation when upregulated[206]. Then in 2017, Mas-Bargues et al[207] indicated that p16INK4A also played a part in oxidative stress-related premature senescence of DPSCs caused by long-term culture in 21% ambient oxygen tension compared with 3%-6% physiological oxygen tension[207]. Replicative senescence of DPSCs resulted in decreases of B-lymphoma Mo-MLV insertion region 1, organic carbon, DSP and bone sialoprotein compared with rapidly proliferating cells and increases of p16INK4A, while B-lymphoma Mo-MLV insertion region 1 transduction promoted the expression of organic carbon and DSP, ALP activity and mineralized nodule formation. Therefore, this may indicate that the odontogenic differentiation potential of DPSCs weakens during senescence, partly due to decreased B-lymphoma Mo-MLV insertion region 1 expression[208].
In contrast, Ma et al[209] reported that adult DPSCs cultured in juvenile dental pulp cell-conditioned medium demonstrated decreased osteogenic differentiation capability, whereas juvenile DPSCs induced by adult dental pulp cell-conditioned medium showed improved osteogenic differentiation capability, indicating that the activity of DPSCs can be modulated by the extrinsic microenvironment[209]. A certain degree of inflammatory stimulation promoted the proliferation and mineralization of both adult and juvenile rat DPSCs, but this effect declined with age[210]. Furthermore, Horibe et al[211] isolated a type of mobilized dental pulp stem cells induced by granulocyte colony-stimulating factor from young and old donors, which showed minimal characteristic changes with aging, suggesting that mobilized dental pulp stem cells act as an advantaged source in dental pulp regeneration[211].
Exosomes
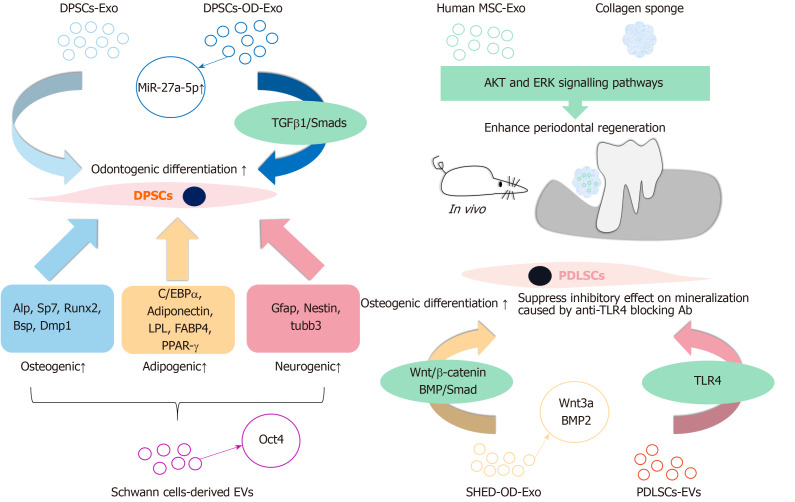
Exosomes are vesicles secreted by different cells with a diameter of 30–100 nm. They can function as carriers for different components to impact intercellular communication, including various miRNAs, lncRNAs and proteins. Exosomes play an important role in mediating some signaling pathways to influence the physiological function of cells. In recent years, increasing research into the effect of exosomes on the odontoblastic/osteogenic differentiation of DMSCs has been proposed (Figure 2).
Figure 2.
Reported extracellular vesicles that mainly contributed to the odontogenic/osteogenic differentiation process of dental mesenchymal stem cells. Extracellular vesicles (EVs) from a variety of cell sources can influence the osteogenic, adipogenic and neurogenic differentiation process of dental mesenchymal stem cells. Exo: Exosomes; DFSCs: Dental follicle stem cells; LPL: Lipoprotein lipase; MSC: Mesenchymal stem cells; PDLSCs: Periodontal ligament stem cells; PPAR-γ: Peroxisome proliferator-activated receptor-γ; SHED: Stem cells from human exfoliated deciduous teeth; TGFβ1: Transforming growth factor β1.
In 2016, Huang et al[212] indicated that the exosomes derived from hDPSCs cultured with growth (DPSC-Exo) or odontogenic differentiation media (DPSC-OD-Exo) enhanced the odontogenic differentiation of DPSCs in vitro, and DPSC-OD-Exo showed stronger induction differentiation-inducing ability than exosomes derived from hDPSCs cultured with growth media in a three-dimensional environment consisting of type I collagen hydrogels and a tooth root-slice regeneration model[212]. In 2019, Hu et al[213] further identified the miRNA profile of human exosomes derived from hDPSCs cultured with growth media and DPSC-OD-Exo by miRNA sequencing, and the results indicated that miR-27a-5p was highly expressed in DPSC-OD-Exo, promoting odontogenic differentiation of DPSCs through the TGF-β1/Smad signaling pathway[213].
In 2019, Chew et al[214] reported that human MSC exosome-loaded collagen sponge used in an immunocompetent rat model with periodontal intrabony defects significantly repaired the defects by regenerating newly formed bone and periodontal ligament as a result of periodontal ligament cell migration and proliferation[214]. Meanwhile in 2020, Wang et al[215] reported that conditioned SHED-Exos derived from a 3 d osteogenic supernatant improved the osteogenic ability of PDLSCs by activating the BMP/Smad and Wnt/β-catenin signaling pathways and that BMP2 and Wnt3a carried by SHED-Exos played a pivotal part in this process[215].
Moreover, extracellular vesicles (EVs) are a type of mixed vesicles, consisting of endosome-derived exosomes and cell membrane-derived ectosomes. In 2017, Li et al[216] demonstrated that the EVs derived from Schwann cells promoted the osteogenic differentiation of hDPSCs[216]. In 2019, Čebatariūnienė et al[217] indicated that hPDLSC EVs did not influence osteogenic mineralization of PDLSCs but reversed the inhibitory effect on PDLSC osteogenic differentiation of an anti-TLR4 blocking Ab. They also revealed that the EVs may have a potential regulatory ability of genes related to osteogenesis and interfere with TLR4 signaling[217]. Additionally, Pizzicannella et al[218] reported that EVs derived from human GMSCs combined with a three-dimensional polylactide biomaterial enhanced the osteogenic differentiation of human GMSCs in vitro[218].
CONCLUSION
At present, most studies of the multidirectional differentiation of DMSCs focus on the following areas: the regeneration of teeth, bone, cartilage, tendon and blood vessels; the repair of nerve injury; the formation of retina and cornea; and the secretion of insulin. Different types of DMSCs have different abilities towards differentiation into diverse lineages. It is significant to explore the potential of DMSCs to differentiate into various tissues. In addition to the application of oral tissue regeneration, these studies are helpful to the future application of DMSCs in neurovascular injury-related diseases, retinal and corneal injury-related diseases and endocrine diseases such as diabetes. The induction of DMSCs to differentiate insulin-producing cells and neuron-like cells in vitro requires the conditioned-culture medium with a variety of auxiliary inducing factors, like some growth factors and peptides, and sometimes it needs to be induced in several steps, which takes a long time and is relatively complex. The cells induced by the conditioned culture medium express the specific molecules of related tissue-like cells. Researchers detect the specific expression molecules to determine whether the cells differentiate into specific tissue-like cells. Such in vitro differentiation is often limited and may not represent the true differentiation of the cell itself. It is of great significance to improve the induction mode and shorten the induction time for the application of DMSCs in the future. In addition, combining DMSCs with materials possessing good biological compatibility may provide a better approach to tissue regeneration.
Making full use of the odontogenic/osteogenic differentiation ability of DMSCs is of great significance to the application of DMSCs in dental tissue regeneration engineering. In this review, some factors related to the regulation of DMSCs in odontogenic/osteogenic differentiation are reviewed. The regulation process of DMSC odontogenic/osteogenic differentiation is complex. A variety of non-coding RNAs and multiple signaling pathways participate in the differentiation process of DMSCs. The application of DMSCs should consider the donor age and cell aging. With increasing donor age and number of cell passages, differentiation ability may decrease accordingly. At the same time, the future clinical application of DMSCs should account for the impact of the inflammatory microenvironment. How to increase the anti-inflammatory ability of DMSCs is a difficult problem for clinical application of DMSCs in the future. In addition, exosomes, as a crucial medium for communication and transmission of information between cells, have become a hotspot in recent years. In the process of normal tooth development, exosomes also seem to play an important role in regulating gene expression of target cells through their rich and varied contents. Utilizing the characteristics of exosomes endocytosed by cells, discovering other exosomes or transforming contents to promote DMSC odontogenic/osteogenic differentiation will be a future research direction. If we can positively regulate the related factors that advance the odontogenic/osteogenic differentiation of DMSCs and make full use of their differentiation potential, there will be great progress in the application of DMSCs in dental tissue regeneration engineering. Future research should emphasize effectively combining the various types of DMSCs with odontogenic/osteogenic, neurogenic, vascularization and other multipotencies to provide a potential scheme for dental tissue regeneration with normal functions.
Footnotes
Conflict-of-interest statement: Authors declare that they have no conflicts of interest for this article.
Manuscript source: Unsolicited manuscript
Peer-review started: December 21, 2020
First decision: February 14, 2021
Article in press: April 4, 2021
Specialty type: Cell and tissue engineering
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Niyibizi C S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
Contributor Information
Jing-Yao Yin, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Xing-Hong Luo, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Wei-Qing Feng, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Sheng-Hong Miao, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Ting-Ting Ning, Department of Endodontics, Stomatological Hospital, Southern Medical University, Guangzhou 510280, Guangdong Province, China.
Qian Lei, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Tao Jiang, Department of Stomatology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, Guangdong Province, China.
Dan-Dan Ma, Department of Endodontics, Stomatological Hospital, Southern Medical University, Guangzhou 510280, Guangdong Province, China. mdd@smu.edu.cn.
References
- 1.Han F, Wang J, Ding L, Hu Y, Li W, Yuan Z, Guo Q, Zhu C, Yu L, Wang H, Zhao Z, Jia L, Li J, Yu Y, Zhang W, Chu G, Chen S, Li B. Tissue Engineering and Regenerative Medicine: Achievements, Future, and Sustainability in Asia. Front Bioeng Biotechnol. 2020;8:83. doi: 10.3389/fbioe.2020.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Badylak SF, Nerem RM. Progress in tissue engineering and regenerative medicine. Proc Natl Acad Sci USA. 2010;107:3285–3286. doi: 10.1073/pnas.1000256107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma L, Makino Y, Yamaza H, Akiyama K, Hoshino Y, Song G, Kukita T, Nonaka K, Shi S, Yamaza T. Cryopreserved dental pulp tissues of exfoliated deciduous teeth is a feasible stem cell resource for regenerative medicine. PLoS One. 2012;7:e51777. doi: 10.1371/journal.pone.0051777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicola FDC, Marques MR, Odorcyk F, Arcego DM, Petenuzzo L, Aristimunha D, Vizuete A, Sanches EF, Pereira DP, Maurmann N, Dalmaz C, Pranke P, Netto CA. Neuroprotector effect of stem cells from human exfoliated deciduous teeth transplanted after traumatic spinal cord injury involves inhibition of early neuronal apoptosis. Brain Res. 2017;1663:95–105. doi: 10.1016/j.brainres.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 5.Kanafi MM, Rajeshwari YB, Gupta S, Dadheech N, Nair PD, Gupta PK, Bhonde RR. Transplantation of islet-like cell clusters derived from human dental pulp stem cells restores normoglycemia in diabetic mice. Cytotherapy. 2013;15:1228–1236. doi: 10.1016/j.jcyt.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Pisciotta A, Riccio M, Carnevale G, Lu A, De Biasi S, Gibellini L, La Sala GB, Bruzzesi G, Ferrari A, Huard J, De Pol A. Stem cells isolated from human dental pulp and amniotic fluid improve skeletal muscle histopathology in mdx/SCID mice. Stem Cell Res Ther. 2015;6:156. doi: 10.1186/s13287-015-0141-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Syed-Picard FN, Du Y, Lathrop KL, Mann MM, Funderburgh ML, Funderburgh JL. Dental pulp stem cells: a new cellular resource for corneal stromal regeneration. Stem Cells Transl Med. 2015;4:276–285. doi: 10.5966/sctm.2014-0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong F, Shi X, Xiao F, Yang Y, Zhang X, Wang LS, Wu CT, Wang H. Transplantation of Hepatocyte Growth Factor-Modified Dental Pulp Stem Cells Prevents Bone Loss in the Early Phase of Ovariectomy-Induced Osteoporosis. Hum Gene Ther. 2018;29:271–282. doi: 10.1089/hum.2017.091. [DOI] [PubMed] [Google Scholar]
- 9.Mead B, Hill LJ, Blanch RJ, Ward K, Logan A, Berry M, Leadbeater W, Scheven BA. Mesenchymal stromal cell-mediated neuroprotection and functional preservation of retinal ganglion cells in a rodent model of glaucoma. Cytotherapy. 2016;18:487–496. doi: 10.1016/j.jcyt.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 10.Yang C, Li X, Sun L, Guo W, Tian W. Potential of human dental stem cells in repairing the complete transection of rat spinal cord. J Neural Eng. 2017;14:026005. doi: 10.1088/1741-2552/aa596b. [DOI] [PubMed] [Google Scholar]
- 11.Sonoyama W, Liu Y, Fang D, Yamaza T, Seo BM, Zhang C, Liu H, Gronthos S, Wang CY, Wang S, Shi S. Mesenchymal stem cell-mediated functional tooth regeneration in swine. PLoS One. 2006;1:e79. doi: 10.1371/journal.pone.0000079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo W, Gong K, Shi H, Zhu G, He Y, Ding B, Wen L, Jin Y. Dental follicle cells and treated dentin matrix scaffold for tissue engineering the tooth root. Biomaterials. 2012;33:1291–1302. doi: 10.1016/j.biomaterials.2011.09.068. [DOI] [PubMed] [Google Scholar]
- 13.Iohara K, Murakami M, Takeuchi N, Osako Y, Ito M, Ishizaka R, Utunomiya S, Nakamura H, Matsushita K, Nakashima M. A Novel Combinatorial Therapy With Pulp Stem Cells and Granulocyte Colony-Stimulating Factor for Total Pulp Regeneration. Stem Cells Transl Med. 2013;2:818. doi: 10.5966/sctm.2012-0132erratum. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci USA. 2000;97:13625–13630. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wongsupa N, Nuntanaranont T, Kamolmattayakul S, Thuaksuban N. Assessment of bone regeneration of a tissue-engineered bone complex using human dental pulp stem cells/poly(ε-caprolactone)-biphasic calcium phosphate scaffold constructs in rabbit calvarial defects. J Mater Sci Mater Med. 2017;28:77. doi: 10.1007/s10856-017-5883-x. [DOI] [PubMed] [Google Scholar]
- 16.Jin Q, Yuan K, Lin W, Niu C, Ma R, Huang Z. Comparative characterization of mesenchymal stem cells from human dental pulp and adipose tissue for bone regeneration potential. Artif Cells Nanomed Biotechnol. 2019;47:1577–1584. doi: 10.1080/21691401.2019.1594861. [DOI] [PubMed] [Google Scholar]
- 17.Hilkens P, Gervois P, Fanton Y, Vanormelingen J, Martens W, Struys T, Politis C, Lambrichts I, Bronckaers A. Effect of isolation methodology on stem cell properties and multilineage differentiation potential of human dental pulp stem cells. Cell Tissue Res. 2013;353:65–78. doi: 10.1007/s00441-013-1630-x. [DOI] [PubMed] [Google Scholar]
- 18.Rizk A, Rabie AB. Human dental pulp stem cells expressing transforming growth factor β3 transgene for cartilage-like tissue engineering. Cytotherapy. 2013;15:712–725. doi: 10.1016/j.jcyt.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 19.Dai J, Wang J, Lu J, Zou D, Sun H, Dong Y, Yu H, Zhang L, Yang T, Zhang X, Wang X, Shen G. The effect of co-culturing costal chondrocytes and dental pulp stem cells combined with exogenous FGF9 protein on chondrogenesis and ossification in engineered cartilage. Biomaterials. 2012;33:7699–7711. doi: 10.1016/j.biomaterials.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 20.Yanasse RH, De Lábio RW, Marques L, Fukasawa JT, Segato R, Kinoshita A, Matsumoto MA, Felisbino SL, Solano B, Dos Santos RR, Payão SLM. Xenotransplantation of human dental pulp stem cells in platelet-rich plasma for the treatment of full-thickness articular cartilage defects in a rabbit model. Exp Ther Med. 2019;17:4344–4356. doi: 10.3892/etm.2019.7499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mata M, Milian L, Oliver M, Zurriaga J, Sancho-Tello M, de Llano JJM, Carda C. In Vivo Articular Cartilage Regeneration Using Human Dental Pulp Stem Cells Cultured in an Alginate Scaffold: A Preliminary Study. Stem Cells Int. 2017;2017:8309256. doi: 10.1155/2017/8309256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen YY, He ST, Yan FH, Zhou PF, Luo K, Zhang YD, Xiao Y, Lin MK. Dental pulp stem cells express tendon markers under mechanical loading and are a potential cell source for tissue engineering of tendon-like tissue. Int J Oral Sci. 2016;8:213–222. doi: 10.1038/ijos.2016.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Luke AM, Patnaik R, Kuriadom S, Abu-Fanas S, Mathew S, Shetty KP. Human dental pulp stem cells differentiation to neural cells, osteocytes and adipocytes-An in vitro study. Heliyon. 2020;6:e03054. doi: 10.1016/j.heliyon.2019.e03054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rafiee F, Pourteymourfard-Tabrizi Z, Mahmoudian-Sani MR, Mehri-Ghahfarrokhi A, Soltani A, Hashemzadeh-Chaleshtori M, Jami MS. Differentiation of dental pulp stem cells into neuron-like cells. Int J Neurosci. 2020;130:107–116. doi: 10.1080/00207454.2019.1664518. [DOI] [PubMed] [Google Scholar]
- 25.Osathanon T, Sawangmake C, Nowwarote N, Pavasant P. Neurogenic differentiation of human dental pulp stem cells using different induction protocols. Oral Dis. 2014;20:352–358. doi: 10.1111/odi.12119. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Zhou Y, Li H, Wang R, Yang D, Li B, Cao X, Fu J. Transplanted Dental Pulp Stem Cells Migrate to Injured Area and Express Neural Markers in a Rat Model of Cerebral Ischemia. Cell Physiol Biochem. 2018;45:258–266. doi: 10.1159/000486772. [DOI] [PubMed] [Google Scholar]
- 27.Sanen K, Martens W, Georgiou M, Ameloot M, Lambrichts I, Phillips J. Engineered neural tissue with Schwann cell differentiated human dental pulp stem cells: potential for peripheral nerve repair? J Tissue Eng Regen Med. 2017;11:3362–3372. doi: 10.1002/term.2249. [DOI] [PubMed] [Google Scholar]
- 28.Bray AF, Cevallos RR, Gazarian K, Lamas M. Human dental pulp stem cells respond to cues from the rat retina and differentiate to express the retinal neuronal marker rhodopsin. Neuroscience. 2014;280:142–155. doi: 10.1016/j.neuroscience.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 29.Xu B, Fan D, Zhao Y, Li J, Wang Z, Wang J, Wang X, Guan Z, Niu B. Three-Dimensional Culture Promotes the Differentiation of Human Dental Pulp Mesenchymal Stem Cells Into Insulin-Producing Cells for Improving the Diabetes Therapy. Front Pharmacol. 2019;10:1576. doi: 10.3389/fphar.2019.01576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yagi Mendoza H, Yokoyama T, Tanaka T, Ii H, Yaegaki K. Regeneration of insulin-producing islets from dental pulp stem cells using a 3D culture system. Regen Med. 2018;13:673–687. doi: 10.2217/rme-2018-0074. [DOI] [PubMed] [Google Scholar]
- 31.Sawangmake C, Nowwarote N, Pavasant P, Chansiripornchai P, Osathanon T. A feasibility study of an in vitro differentiation potential toward insulin-producing cells by dental tissue-derived mesenchymal stem cells. Biochem Biophys Res Commun. 2014;452:581–587. doi: 10.1016/j.bbrc.2014.08.121. [DOI] [PubMed] [Google Scholar]
- 32.Luzuriaga J, Pastor-Alonso O, Encinas JM, Unda F, Ibarretxe G, Pineda JR. Human Dental Pulp Stem Cells Grown in Neurogenic Media Differentiate Into Endothelial Cells and Promote Neovasculogenesis in the Mouse Brain. Front Physiol. 2019;10:347. doi: 10.3389/fphys.2019.00347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gandia C, Armiñan A, García-Verdugo JM, Lledó E, Ruiz A, Miñana MD, Sanchez-Torrijos J, Payá R, Mirabet V, Carbonell-Uberos F, Llop M, Montero JA, Sepúlveda P. Human dental pulp stem cells improve left ventricular function, induce angiogenesis, and reduce infarct size in rats with acute myocardial infarction. Stem Cells. 2008;26:638–645. doi: 10.1634/stemcells.2007-0484. [DOI] [PubMed] [Google Scholar]
- 34.Song B, Jiang W, Alraies A, Liu Q, Gudla V, Oni J, Wei X, Sloan A, Ni L, Agarwal M. Bladder Smooth Muscle Cells Differentiation from Dental Pulp Stem Cells: Future Potential for Bladder Tissue Engineering. Stem Cells Int. 2016;2016:6979368. doi: 10.1155/2016/6979368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang W, Wang D, Alraies A, Liu Q, Zhu B, Sloan AJ, Ni L, Song B. Wnt-GSK3β/β-Catenin Regulates the Differentiation of Dental Pulp Stem Cells into Bladder Smooth Muscle Cells. Stem Cells Int. 2019;2019:8907570. doi: 10.1155/2019/8907570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ishkitiev N, Yaegaki K, Imai T, Tanaka T, Nakahara T, Ishikawa H, Mitev V, Haapasalo M. High-purity hepatic lineage differentiated from dental pulp stem cells in serum-free medium. J Endod. 2012;38:475–480. doi: 10.1016/j.joen.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 37.Chen YK, Huang AH, Chan AW, Lin LM. Human dental pulp stem cells derived from cryopreserved dental pulp tissues of vital extracted teeth with disease demonstrate hepatic-like differentiation. J Tissue Eng Regen Med. 2016;10:475–485. doi: 10.1002/term.1763. [DOI] [PubMed] [Google Scholar]
- 38.Paino F, Ricci G, De Rosa A, D'Aquino R, Laino L, Pirozzi G, Tirino V, Papaccio G. Ecto-mesenchymal stem cells from dental pulp are committed to differentiate into active melanocytes. Eur Cell Mater. 2010;20:295–305. doi: 10.22203/ecm.v020a24. [DOI] [PubMed] [Google Scholar]
- 39.Kato T, Hattori K, Deguchi T, Katsube Y, Matsumoto T, Ohgushi H, Numabe Y. Osteogenic potential of rat stromal cells derived from periodontal ligament. J Tissue Eng Regen Med. 2011;5:798–805. doi: 10.1002/term.379. [DOI] [PubMed] [Google Scholar]
- 40.Ge S, Zhao N, Wang L, Yu M, Liu H, Song A, Huang J, Wang G, Yang P. Bone repair by periodontal ligament stem cellseeded nanohydroxyapatite-chitosan scaffold. Int J Nanomedicine. 2012;7:5405–5414. doi: 10.2147/IJN.S36714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moshaverinia A, Chen C, Xu X, Akiyama K, Ansari S, Zadeh HH, Shi S. Bone regeneration potential of stem cells derived from periodontal ligament or gingival tissue sources encapsulated in RGD-modified alginate scaffold. Tissue Eng Part A. 2014;20:611–621. doi: 10.1089/ten.tea.2013.0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moshaverinia A, Xu X, Chen C, Akiyama K, Snead ML, Shi S. Dental mesenchymal stem cells encapsulated in an alginate hydrogel co-delivery microencapsulation system for cartilage regeneration. Acta Biomater. 2013;9:9343–9350. doi: 10.1016/j.actbio.2013.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shen S, Zhang Y, Zhang S, Wang B, Shang L, Shao J, Lin M, Cui Y, Sun S, Ge S. 6-Bromoindirubin-3'-oxime Promotes Osteogenic Differentiation of Periodontal Ligament Stem Cells and Facilitates Bone Regeneration in a Mouse Periodontitis Model. ACS Biomater Sci Eng. 2021;7:232–241. doi: 10.1021/acsbiomaterials.0c01078. [DOI] [PubMed] [Google Scholar]
- 44.Li X, Gong P, Liao D. In vitro neural/glial differentiation potential of periodontal ligament stem cells. Arch Med Sci. 2010;6:678–685. doi: 10.5114/aoms.2010.17080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fortino VR, Chen RS, Pelaez D, Cheung HS. Neurogenesis of neural crest-derived periodontal ligament stem cells by EGF and bFGF. J Cell Physiol. 2014;229:479–488. doi: 10.1002/jcp.24468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liao D, Li X, Dong Y, Sun G. The Role of Wnt/β-Catenin Signaling Pathway in the Transdifferentiation from Periodontal Ligament Stem Cells to Schwann Cells. Cell Reprogram. 2017;19:384–388. doi: 10.1089/cell.2017.0017. [DOI] [PubMed] [Google Scholar]
- 47.Bueno C, Martínez-Morga M, Martínez S. Non-proliferative neurogenesis in human periodontal ligament stem cells. Sci Rep. 2019;9:18038. doi: 10.1038/s41598-019-54745-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Caputi S, Trubiani O, Sinjari B, Trofimova S, Diomede F, Linkova N, Diatlova A, Khavinson V. Effect of short peptides on neuronal differentiation of stem cells. Int J Immunopathol Pharmacol. 2019;33:2058738419828613. doi: 10.1177/2058738419828613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lanza Cariccio V, Scionti D, Raffa A, Iori R, Pollastro F, Diomede F, Bramanti P, Trubiani O, Mazzon E. Treatment of Periodontal Ligament Stem Cells with MOR and CBD Promotes Cell Survival and Neuronal Differentiation via the PI3K/Akt/mTOR Pathway. Int J Mol Sci. 2018:19. doi: 10.3390/ijms19082341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Romeo L, Diomede F, Gugliandolo A, Scionti D, Lo Giudice F, Lanza Cariccio V, Iori R, Bramanti P, Trubiani O, Mazzon E. Moringin Induces Neural Differentiation in the Stem Cell of the Human Periodontal Ligament. Sci Rep. 2018;8:9153. doi: 10.1038/s41598-018-27492-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li D, Zou XY, El-Ayachi I, Romero LO, Yu Z, Iglesias-Linares A, Cordero-Morales JF, Huang GT. Human Dental Pulp Stem Cells and Gingival Mesenchymal Stem Cells Display Action Potential Capacity In Vitro after Neuronogenic Differentiation. Stem Cell Rev Rep. 2019;15:67–81. doi: 10.1007/s12015-018-9854-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gugliandolo A, Diomede F, Scionti D, Bramanti P, Trubiani O, Mazzon E. The Role of Hypoxia on the Neuronal Differentiation of Gingival Mesenchymal Stem Cells: A Transcriptional Study. Cell Transplant. 2019;28:538–552. doi: 10.1177/0963689718814470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rajan TS, Scionti D, Diomede F, Piattelli A, Bramanti P, Mazzon E, Trubiani O. Prolonged Expansion Induces Spontaneous Neural Progenitor Differentiation from Human Gingiva-Derived Mesenchymal Stem Cells. Cell Reprogram. 2017;19:389–401. doi: 10.1089/cell.2017.0012. [DOI] [PubMed] [Google Scholar]
- 54.Ansari S, Diniz IM, Chen C, Sarrion P, Tamayol A, Wu BM, Moshaverinia A. Human Periodontal Ligament- and Gingiva-derived Mesenchymal Stem Cells Promote Nerve Regeneration When Encapsulated in Alginate/Hyaluronic Acid 3D Scaffold. Adv Healthc Mater. 2017:6. doi: 10.1002/adhm.201700670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yam GH, Teo EP, Setiawan M, Lovatt MJ, Yusoff NZBM, Fuest M, Goh BT, Mehta JS. Postnatal periodontal ligament as a novel adult stem cell source for regenerative corneal cell therapy. J Cell Mol Med. 2018;22:3119–3132. doi: 10.1111/jcmm.13589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen J, Zhang W, Kelk P, Backman LJ, Danielson P. Substance P and patterned silk biomaterial stimulate periodontal ligament stem cells to form corneal stroma in a bioengineered three-dimensional model. Stem Cell Res Ther. 2017;8:260. doi: 10.1186/s13287-017-0715-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Huang L, Liang J, Geng Y, Tsang WM, Yao X, Jhanji V, Zhang M, Cheung HS, Pang CP, Yam GH. Directing adult human periodontal ligament-derived stem cells to retinal fate. Invest Ophthalmol Vis Sci. 2013;54:3965–3974. doi: 10.1167/iovs.13-11910. [DOI] [PubMed] [Google Scholar]
- 58.Lee JS, An SY, Kwon IK, Heo JS. Transdifferentiation of human periodontal ligament stem cells into pancreatic cell lineage. Cell Biochem Funct. 2014;32:605–611. doi: 10.1002/cbf.3057. [DOI] [PubMed] [Google Scholar]
- 59.Moshaverinia A, Xu X, Chen C, Ansari S, Zadeh HH, Snead ML, Shi S. Application of stem cells derived from the periodontal ligament or gingival tissue sources for tendon tissue regeneration. Biomaterials. 2014;35:2642–2650. doi: 10.1016/j.biomaterials.2013.12.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Murugan Girija D, Kalachaveedu M, Ranga Rao S, Subbarayan R. Transdifferentiation of human gingival mesenchymal stem cells into functional keratinocytes by Acalypha indica in three-dimensional microenvironment. J Cell Physiol. 2018;233:8450–8457. doi: 10.1002/jcp.26807. [DOI] [PubMed] [Google Scholar]
- 61.Takahashi K, Ogura N, Aonuma H, Ito K, Ishigami D, Kamino Y, Kondoh T. Bone morphogenetic protein 6 stimulates mineralization in human dental follicle cells without dexamethasone. Arch Oral Biol. 2013;58:690–698. doi: 10.1016/j.archoralbio.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 62.Okada H, Takahashi K, Ogura N, Tomoki R, Ito K, Kondoh T. Plasma rich in growth factors stimulates proliferation, migration, and gene expression associated with bone formation in human dental follicle cells. J Dent Sci. 2016;11:245–252. doi: 10.1016/j.jds.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Uribe P, Johansson A, Jugdaohsingh R, Powell JJ, Magnusson C, Davila M, Westerlund A, Ransjö M. Soluble silica stimulates osteogenic differentiation and gap junction communication in human dental follicle cells. Sci Rep. 2020;10:9923. doi: 10.1038/s41598-020-66939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lucaciu O, Soriţău O, Gheban D, Ciuca DR, Virtic O, Vulpoi A, Dirzu N, Câmpian R, Băciuţ G, Popa C, Simon S, Berce P, Băciuţ M, Crisan B. Dental follicle stem cells in bone regeneration on titanium implants. BMC Biotechnol. 2015;15:114. doi: 10.1186/s12896-015-0229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rezai-Rad M, Bova JF, Orooji M, Pepping J, Qureshi A, Del Piero F, Hayes D, Yao S. Evaluation of bone regeneration potential of dental follicle stem cells for treatment of craniofacial defects. Cytotherapy. 2015;17:1572–1581. doi: 10.1016/j.jcyt.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kanao S, Ogura N, Takahashi K, Ito K, Suemitsu M, Kuyama K, Kondoh T. Capacity of Human Dental Follicle Cells to Differentiate into Neural Cells In Vitro. Stem Cells Int. 2017;2017:8371326. doi: 10.1155/2017/8371326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Völlner F, Ernst W, Driemel O, Morsczeck C. A two-step strategy for neuronal differentiation in vitro of human dental follicle cells. Differentiation. 2009;77:433–441. doi: 10.1016/j.diff.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 68.Sung IY, Son HN, Ullah I, Bharti D, Park JM, Cho YC, Byun JH, Kang YH, Sung SJ, Kim JW, Rho GJ, Park BW. Cardiomyogenic Differentiation of Human Dental Follicle-derived Stem Cells by Suberoylanilide Hydroxamic Acid and Their In Vivo Homing Property. Int J Med Sci. 2016;13:841–852. doi: 10.7150/ijms.16573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shivakumar SB, Lee HJ, Son YB, Bharti D, Ock SA, Lee SL, Kang YH, Park BW, Rho GJ. In vitro differentiation of single donor derived human dental mesenchymal stem cells into pancreatic β cell-like cells. Biosci Rep. 2019:39. doi: 10.1042/BSR20182051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xu QL, Furuhashi A, Zhang QZ, Jiang CM, Chang TH, Le AD. Induction of Salivary Gland-Like Cells from Dental Follicle Epithelial Cells. J Dent Res. 2017;96:1035–1043. doi: 10.1177/0022034517711146. [DOI] [PubMed] [Google Scholar]
- 71.Prahasanti C, Subrata LH, Saskianti T, Suardita K, Ernawati DS. Combined Hydroxyapatite Scaffold and Stem Cell from Human Exfoliated Deciduous Teeth Modulating Alveolar Bone Regeneration via Regulating Receptor Activator of Nuclear Factor-Κb and Osteoprotegerin System. Iran J Med Sci. 2019;44:415–421. doi: 10.30476/IJMS.2019.44962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sebastian AA, Kannan TP, Norazmi MN, Nurul AA. Interleukin-17A promotes osteogenic differentiation by increasing OPG/RANKL ratio in stem cells from human exfoliated deciduous teeth (SHED) J Tissue Eng Regen Med. 2018;12:1856–1866. doi: 10.1002/term.2706. [DOI] [PubMed] [Google Scholar]
- 73.Novais A, Lesieur J, Sadoine J, Slimani L, Baroukh B, Saubaméa B, Schmitt A, Vital S, Poliard A, Hélary C, Rochefort GY, Chaussain C, Gorin C. Priming Dental Pulp Stem Cells from Human Exfoliated Deciduous Teeth with Fibroblast Growth Factor-2 Enhances Mineralization Within Tissue-Engineered Constructs Implanted in Craniofacial Bone Defects. Stem Cells Transl Med. 2019;8:844–857. doi: 10.1002/sctm.18-0182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang X, Zhao Q, Chen J, Liu J, Lin J, Lu J, Li W, Yu D, Zhao W. Graphene Oxide Quantum Dots Promote Osteogenic Differentiation of Stem Cells from Human Exfoliated Deciduous Teeth via the Wnt/β-Catenin Signaling Pathway. Stem Cells Int. 2021;2021:8876745. doi: 10.1155/2021/8876745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chen K, Xiong H, Xu N, Shen Y, Huang Y, Liu C. Chondrogenic potential of stem cells from human exfoliated deciduous teeth in vitro and in vivo. Acta Odontol Scand. 2014;72:664–672. doi: 10.3109/00016357.2014.888756. [DOI] [PubMed] [Google Scholar]
- 76.Nourbakhsh N, Soleimani M, Taghipour Z, Karbalaie K, Mousavi SB, Talebi A, Nadali F, Tanhaei S, Kiyani GA, Nematollahi M, Rabiei F, Mardani M, Bahramiyan H, Torabinejad M, Nasr-Esfahani MH, Baharvand H. Induced in vitro differentiation of neural-like cells from human exfoliated deciduous teeth-derived stem cells. Int J Dev Biol. 2011;55:189–195. doi: 10.1387/ijdb.103090nn. [DOI] [PubMed] [Google Scholar]
- 77.Jarmalavičiūtė A, Tunaitis V, Strainienė E, Aldonytė R, Ramanavičius A, Venalis A, Magnusson KE, Pivoriūnas A. A New Experimental Model for Neuronal and Glial Differentiation Using Stem Cells Derived from Human Exfoliated Deciduous Teeth. J Mol Neurosci. 2013 doi: 10.1007/s12031-013-0046-0. [DOI] [PubMed] [Google Scholar]
- 78.Yang S, Xin C, Zhang B, Zhang H, Hao Y. Synergistic effects of Rho kinase inhibitor Y-27632 and Noggin overexpression on the proliferation and neuron-like cell differentiation of stem cells derived from human exfoliated deciduous teeth. IUBMB Life. 2020;72:665–676. doi: 10.1002/iub.2208. [DOI] [PubMed] [Google Scholar]
- 79.Liu J, Zhang ZY, Yu H, Yang AP, Hu PF, Liu Z, Wang M. Long noncoding RNA C21orf121/bone morphogenetic protein 2/microRNA-140-5p gene network promotes directed differentiation of stem cells from human exfoliated deciduous teeth to neuronal cells. J Cell Biochem. 2018 doi: 10.1002/jcb.27313. [DOI] [PubMed] [Google Scholar]
- 80.Pereira LV, Bento RF, Cruz DB, Marchi C, Salomone R, Oiticicca J, Costa MP, Haddad LA, Mingroni-Netto RC, Costa HJZR. Stem Cells from Human Exfoliated Deciduous Teeth (SHED) Differentiate in vivo and Promote Facial Nerve Regeneration. Cell Transplant. 2019;28:55–64. doi: 10.1177/0963689718809090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang N, Lu X, Wu S, Li X, Duan J, Chen C, Wang W, Song H, Tong J, Li S, Liu Y, Kang X, Wang X, Han F. Intrastriatal transplantation of stem cells from human exfoliated deciduous teeth reduces motor defects in Parkinsonian rats. Cytotherapy. 2018;20:670–686. doi: 10.1016/j.jcyt.2018.02.371. [DOI] [PubMed] [Google Scholar]
- 82.Taghipour Z, Karbalaie K, Kiani A, Niapour A, Bahramian H, Nasr-Esfahani MH, Baharvand H. Transplantation of undifferentiated and induced human exfoliated deciduous teeth-derived stem cells promote functional recovery of rat spinal cord contusion injury model. Stem Cells Dev. 2012;21:1794–1802. doi: 10.1089/scd.2011.0408. [DOI] [PubMed] [Google Scholar]
- 83.Xie J, Rao N, Zhai Y, Li J, Zhao Y, Ge L, Wang Y. Therapeutic effects of stem cells from human exfoliated deciduous teeth on diabetic peripheral neuropathy. Diabetol Metab Syndr. 2019;11:38. doi: 10.1186/s13098-019-0433-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sakai VT, Zhang Z, Dong Z, Neiva KG, Machado MA, Shi S, Santos CF, Nör JE. SHED differentiate into functional odontoblasts and endothelium. J Dent Res. 2010;89:791–796. doi: 10.1177/0022034510368647. [DOI] [PubMed] [Google Scholar]
- 85.Gong T, Heng BC, Xu J, Zhu S, Yuan C, Lo EC, Zhang C. Decellularized extracellular matrix of human umbilical vein endothelial cells promotes endothelial differentiation of stem cells from exfoliated deciduous teeth. J Biomed Mater Res A. 2017;105:1083–1093. doi: 10.1002/jbm.a.36003. [DOI] [PubMed] [Google Scholar]
- 86.Wang P, Zhu S, Yuan C, Wang L, Xu J, Liu Z. Shear stress promotes differentiation of stem cells from human exfoliated deciduous teeth into endothelial cells via the downstream pathway of VEGF-Notch signaling. Int J Mol Med. 2018;42:1827–1836. doi: 10.3892/ijmm.2018.3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Xu JG, Gong T, Wang YY, Zou T, Heng BC, Yang YQ, Zhang CF. Inhibition of TGF-β Signaling in SHED Enhances Endothelial Differentiation. J Dent Res. 2018;97:218–225. doi: 10.1177/0022034517733741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kim JH, Kim GH, Kim JW, Pyeon HJ, Lee JC, Lee G, Nam H. In Vivo Angiogenic Capacity of Stem Cells from Human Exfoliated Deciduous Teeth with Human Umbilical Vein Endothelial Cells. Mol Cells. 2016;39:790–796. doi: 10.14348/molcells.2016.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Su WT, Chen XW. Stem cells from human exfoliated deciduous teeth differentiate into functional hepatocyte-like cells by herbal medicine. Biomed Mater Eng. 2014;24:2243–2247. doi: 10.3233/BME-141036. [DOI] [PubMed] [Google Scholar]
- 90.Ishkitiev N, Yaegaki K, Imai T, Tanaka T, Fushimi N, Mitev V, Okada M, Tominaga N, Ono S, Ishikawa H. Novel management of acute or secondary biliary liver conditions using hepatically differentiated human dental pulp cells. Tissue Eng Part A. 2015;21:586–593. doi: 10.1089/ten.tea.2014.0162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yamaza T, Alatas FS, Yuniartha R, Yamaza H, Fujiyoshi JK, Yanagi Y, Yoshimaru K, Hayashida M, Matsuura T, Aijima R, Ihara K, Ohga S, Shi S, Nonaka K, Taguchi T. In vivo hepatogenic capacity and therapeutic potential of stem cells from human exfoliated deciduous teeth in liver fibrosis in mice. Stem Cell Res Ther. 2015;6:171. doi: 10.1186/s13287-015-0154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Takahashi Y, Yuniartha R, Yamaza T, Sonoda S, Yamaza H, Kirino K, Yoshimaru K, Matsuura T, Taguchi T. Therapeutic potential of spheroids of stem cells from human exfoliated deciduous teeth for chronic liver fibrosis and hemophilia A. Pediatr Surg Int. 2019;35:1379–1388. doi: 10.1007/s00383-019-04564-4. [DOI] [PubMed] [Google Scholar]
- 93.Huang TY, Wang GS, Tseng CC, Su WT. Epidermal cells differentiated from stem cells from human exfoliated deciduous teeth and seeded onto polyvinyl alcohol/silk fibroin nanofiber dressings accelerate wound repair. Mater Sci Eng C Mater Biol Appl. 2019;104:109986. doi: 10.1016/j.msec.2019.109986. [DOI] [PubMed] [Google Scholar]
- 94.Ishkitiev N, Yaegaki K, Kozhuharova A, Tanaka T, Okada M, Mitev V, Fukuda M, Imai T. Pancreatic differentiation of human dental pulp CD117⁺ stem cells. Regen Med. 2013;8:597–612. doi: 10.2217/rme.13.42. [DOI] [PubMed] [Google Scholar]
- 95.Tsai CL, Chuang PC, Kuo HK, Chen YH, Su WH, Wu PC. Differentiation of Stem Cells From Human Exfoliated Deciduous Teeth Toward a Phenotype of Corneal Epithelium In Vitro. Cornea. 2015;34:1471–1477. doi: 10.1097/ICO.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 96.Li X, Xie J, Zhai Y, Fang T, Rao N, Hu S, Yang L, Zhao Y, Wang Y, Ge L. Differentiation of Stem Cells from Human Exfoliated Deciduous Teeth into Retinal Photoreceptor-Like Cells and Their Sustainability In Vivo. Stem Cells Int. 2019;2019:2562981. doi: 10.1155/2019/2562981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Xu JG, Zhu SY, Heng BC, Dissanayaka WL, Zhang CF. TGF-β1-induced differentiation of SHED into functional smooth muscle cells. Stem Cell Res Ther. 2017;8:10. doi: 10.1186/s13287-016-0459-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Deng J, Pan J, Han X, Yu L, Chen J, Zhang W, Zhu L, Huang W, Liu S, You Z, Liu Y. PDGFBB-modified stem cells from apical papilla and thermosensitive hydrogel scaffolds induced bone regeneration. Chem Biol Interact. 2020;316:108931. doi: 10.1016/j.cbi.2019.108931. [DOI] [PubMed] [Google Scholar]
- 99.Pang X, Wang Y, Wu J, Zhou Z, Xu T, Jin L, Yu Y, Li Z, Gobin R, Xue C, Yu J. Yunnan Baiyao Conditioned Medium Promotes the Odonto/Osteogenic Capacity of Stem Cells from Apical Papilla via Nuclear Factor Kappa B Signaling Pathway. Biomed Res Int. 2019;2019:9327386. doi: 10.1155/2019/9327386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang Y, Wang Y, Lu Y, Yu J. High Glucose Enhances the Odonto/Osteogenic Differentiation of Stem Cells from Apical Papilla via NF-KappaB Signaling Pathway. Biomed Res Int. 2019;2019:5068258. doi: 10.1155/2019/5068258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dong R, Yao R, Du J, Wang S, Fan Z. Depletion of histone demethylase KDM2A enhanced the adipogenic and chondrogenic differentiation potentials of stem cells from apical papilla. Exp Cell Res. 2013;319:2874–2882. doi: 10.1016/j.yexcr.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 102.Yang H, Cao Y, Zhang J, Liang Y, Su X, Zhang C, Liu H, Han X, Ge L, Fan Z. DLX5 and HOXC8 enhance the chondrogenic differentiation potential of stem cells from apical papilla via LINC01013. Stem Cell Res Ther. 2020;11:271. doi: 10.1186/s13287-020-01791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kim BC, Jun SM, Kim SY, Kwon YD, Choe SC, Kim EC, Lee JH, Kim J, Suh JF, Hwang YS. Engineering three dimensional micro nerve tissue using postnatal stem cells from human dental apical papilla. Biotechnol Bioeng. 2017;114:903–914. doi: 10.1002/bit.26205. [DOI] [PubMed] [Google Scholar]
- 104.Lin X, Dong R, Diao S, Yu G, Wang L, Li J, Fan Z. SFRP2 enhanced the adipogenic and neuronal differentiation potentials of stem cells from apical papilla. Cell Biol Int. 2017;41:534–543. doi: 10.1002/cbin.10757. [DOI] [PubMed] [Google Scholar]
- 105.Diao S, Yang H, Cao Y, Yang D, Fan Z. IGF2 enhanced the osteo-/dentinogenic and neurogenic differentiation potentials of stem cells from apical papilla. J Oral Rehabil. 2020;47 Suppl 1:55–65. doi: 10.1111/joor.12859. [DOI] [PubMed] [Google Scholar]
- 106.Simonovic J, Toljic B, Nikolic N, Peric M, Vujin J, Panajotovic R, Gajic R, Bekyarova E, Cataldi A, Parpura V, Milasin J. Differentiation of stem cells from apical papilla into neural lineage using graphene dispersion and single walled carbon nanotubes. J Biomed Mater Res A. 2018;106:2653–2661. doi: 10.1002/jbm.a.36461. [DOI] [PubMed] [Google Scholar]
- 107.Hilkens P, Bronckaers A, Ratajczak J, Gervois P, Wolfs E, Lambrichts I. The Angiogenic Potential of DPSCs and SCAPs in an In Vivo Model of Dental Pulp Regeneration. Stem Cells Int. 2017;2017:2582080. doi: 10.1155/2017/2582080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yuan C, Wang P, Zhu L, Dissanayaka WL, Green DW, Tong EH, Jin L, Zhang C. Coculture of stem cells from apical papilla and human umbilical vein endothelial cell under hypoxia increases the formation of three-dimensional vessel-like structures in vitro. Tissue Eng Part A. 2015;21:1163–1172. doi: 10.1089/ten.tea.2014.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yuan C, Wang P, Zhu S, Zou T, Wang S, Xu J, Heng BC, Diogenes A, Zhang C. EphrinB2 Stabilizes Vascularlike Structures Generated by Endothelial Cells and Stem Cells from Apical Papilla. J Endod. 2016;42:1362–1370. doi: 10.1016/j.joen.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 110.Koutsoumparis A, Vassili A, Bakopoulou A, Ziouta A, Tsiftsoglou AS. Erythropoietin (rhEPOa) promotes endothelial transdifferentiation of stem cells of the apical papilla (SCAP) Arch Oral Biol. 2018;96:96–103. doi: 10.1016/j.archoralbio.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 111.Kumar A, Kumar V, Rattan V, Jha V, Pal A, Bhattacharyya S. Molecular spectrum of secretome regulates the relative hepatogenic potential of mesenchymal stem cells from bone marrow and dental tissue. Sci Rep. 2017;7:15015. doi: 10.1038/s41598-017-14358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhan FL, Liu XY, Wang XB. The Role of MicroRNA-143-5p in the Differentiation of Dental Pulp Stem Cells into Odontoblasts by Targeting Runx2 via the OPG/RANKL Signaling Pathway. J Cell Biochem. 2018;119:536–546. doi: 10.1002/jcb.26212. [DOI] [PubMed] [Google Scholar]
- 113.Yang C, Jia R, Zuo Q, Zheng Y, Wu Q, Luo B, Lin P, Yin L. microRNA-143-3p regulates odontogenic differentiation of human dental pulp stem cells through regulation of the osteoprotegerin-RANK ligand pathway by targeting RANK. Exp Physiol. 2020;105:876–885. doi: 10.1113/EP087992. [DOI] [PubMed] [Google Scholar]
- 114.Wang BL, Wang Z, Nan X, Zhang QC, Liu W. Downregulation of microRNA-143-5p is required for the promotion of odontoblasts differentiation of human dental pulp stem cells through the activation of the mitogen-activated protein kinases 14-dependent p38 mitogen-activated protein kinases signaling pathway. J Cell Physiol. 2019;234:4840–4850. doi: 10.1002/jcp.27282. [DOI] [PubMed] [Google Scholar]
- 115.Yu D, Zhao X, Cheng JZ, Wang D, Zhang HH, Han GH. Downregulated microRNA-488 enhances odontoblast differentiation of human dental pulp stem cells via activation of the p38 MAPK signaling pathway. J Cell Physiol. 2019;234:1442–1451. doi: 10.1002/jcp.26950. [DOI] [PubMed] [Google Scholar]
- 116.Wang J, Zheng Y, Bai B, Song Y, Zheng K, Xiao J, Liang Y, Bao L, Zhou Q, Ji L, Feng X. MicroRNA-125a-3p participates in odontoblastic differentiation of dental pulp stem cells by targeting Fyn. Cytotechnology. 2020;72:69–79. doi: 10.1007/s10616-019-00358-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yuan H, Zhao H, Wang J, Zhang H, Hong L, Li H, Che H, Zhang Z. MicroRNA let-7c-5p promotes osteogenic differentiation of dental pulp stem cells by inhibiting lipopolysaccharide-induced inflammation via HMGA2/PI3K/Akt signal blockade. Clin Exp Pharmacol Physiol. 2019;46:389–397. doi: 10.1111/1440-1681.13059. [DOI] [PubMed] [Google Scholar]
- 118.Huang X, Liu F, Hou J, Chen K. Inflammation-induced overexpression of microRNA-223-3p regulates odontoblastic differentiation of human dental pulp stem cells by targeting SMAD3. Int Endod J. 2019;52:491–503. doi: 10.1111/iej.13032. [DOI] [PubMed] [Google Scholar]
- 119.Sun DG, Xin BC, Wu D, Zhou L, Wu HB, Gong W, Lv J. miR-140-5p-mediated regulation of the proliferation and differentiation of human dental pulp stem cells occurs through the lipopolysaccharide/toll-like receptor 4 signaling pathway. Eur J Oral Sci. 2017;125:419–425. doi: 10.1111/eos.12384. [DOI] [PubMed] [Google Scholar]
- 120.Liu F, Wang X, Yang Y, Hu R, Wang W, Wang Y. The suppressive effects of miR-508-5p on the odontogenic differentiation of human dental pulp stem cells by targeting glycoprotein non-metastatic melanomal protein B. Stem Cell Res Ther. 2019;10:35. doi: 10.1186/s13287-019-1146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Xu K, Xiao J, Zheng K, Feng X, Zhang J, Song D, Wang C, Shen X, Zhao X, Wei C, Huang D, Feng G. MiR-21/STAT3 Signal Is Involved in Odontoblast Differentiation of Human Dental Pulp Stem Cells Mediated by TNF-α. Cell Reprogram. 2018;20:107–116. doi: 10.1089/cell.2017.0042. [DOI] [PubMed] [Google Scholar]
- 122.Qiu Z, Lin S, Hu X, Zeng J, Xiao T, Ke Z, Lv H. Involvement of miR-146a-5p/neurogenic locus notch homolog protein 1 in the proliferation and differentiation of STRO-1+ human dental pulp stem cells. Eur J Oral Sci. 2019;127:294–303. doi: 10.1111/eos.12624. [DOI] [PubMed] [Google Scholar]
- 123.Zhang P, Yang W, Wang G, Li Y. miR-143 suppresses the osteogenic differentiation of dental pulp stem cells by inactivation of NF-κB signaling pathway via targeting TNF-α. Arch Oral Biol. 2018;87:172–179. doi: 10.1016/j.archoralbio.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 124.Yao S, Li C, Budenski AM, Li P, Ramos A, Guo S. Expression of microRNAs targeting heat shock protein B8 during in vitro expansion of dental pulp stem cells in regulating osteogenic differentiation. Arch Oral Biol. 2019;107:104485. doi: 10.1016/j.archoralbio.2019.104485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wei F, Yang S, Guo Q, Zhang X, Ren D, Lv T, Xu X. MicroRNA-21 regulates Osteogenic Differentiation of Periodontal Ligament Stem Cells by targeting Smad5. Sci Rep. 2017;7:16608. doi: 10.1038/s41598-017-16720-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li Z, Sun Y, Cao S, Zhang J, Wei J. Downregulation of miR-24-3p promotes osteogenic differentiation of human periodontal ligament stem cells by targeting SMAD family member 5. J Cell Physiol. 2019;234:7411–7419. doi: 10.1002/jcp.27499. [DOI] [PubMed] [Google Scholar]
- 127.Wei F, Liu D, Feng C, Zhang F, Yang S, Hu Y, Ding G, Wang S. microRNA-21 mediates stretch-induced osteogenic differentiation in human periodontal ligament stem cells. Stem Cells Dev. 2015;24:312–319. doi: 10.1089/scd.2014.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yao S, Zhao W, Ou Q, Liang L, Lin X, Wang Y. MicroRNA-214 Suppresses Osteogenic Differentiation of Human Periodontal Ligament Stem Cells by Targeting ATF4. Stem Cells Int. 2017;2017:3028647. doi: 10.1155/2017/3028647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cao F, Zhan J, Chen X, Zhang K, Lai R, Feng Z. miR-214 promotes periodontal ligament stem cell osteoblastic differentiation by modulating Wnt/βcatenin signaling. Mol Med Rep. 2017;16:9301–9308. doi: 10.3892/mmr.2017.7821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Bao L, Zhang X, Xu Y, Wang M, Song Y, Gu Y, Zheng Y, Xiao J, Wang Y, Zhou Q, Qian J, Liang Y, Ji L, Feng X. Dysfunction of MiR-148a-NRP1 Functional Axis Suppresses Osteogenic Differentiation of Periodontal Ligament Stem Cells Under Inflammatory Microenvironment. Cell Reprogram. 2019;21:314–322. doi: 10.1089/cell.2019.0026. [DOI] [PubMed] [Google Scholar]
- 131.Yan GQ, Wang X, Yang F, Yang ML, Zhang GR, Wang GK, Zhou Q. MicroRNA-22 Promoted Osteogenic Differentiation of Human Periodontal Ligament Stem Cells by Targeting HDAC6. J Cell Biochem. 2017;118:1653–1658. doi: 10.1002/jcb.25931. [DOI] [PubMed] [Google Scholar]
- 132.Li L, Liu W, Wang H, Yang Q, Zhang L, Jin F, Jin Y. Mutual inhibition between HDAC9 and miR-17 regulates osteogenesis of human periodontal ligament stem cells in inflammatory conditions. Cell Death Dis. 2018;9:480. doi: 10.1038/s41419-018-0480-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xu Y, Ren C, Zhao X, Wang W, Zhang N. microRNA-132 inhibits osteogenic differentiation of periodontal ligament stem cells via GDF5 and the NF-κB signaling pathway. Pathol Res Pract. 2019;215:152722. doi: 10.1016/j.prp.2019.152722. [DOI] [PubMed] [Google Scholar]
- 134.Zhen L, Jiang X, Chen Y, Fan D. MiR-31 is involved in the high glucose-suppressed osteogenic differentiation of human periodontal ligament stem cells by targeting Satb2. Am J Transl Res. 2017;9:2384–2393. [PMC free article] [PubMed] [Google Scholar]
- 135.Wan M, Gao B, Sun F, Tang Y, Ye L, Fan Y, Klein OD, Zhou X, Zheng L. microRNA miR-34a regulates cytodifferentiation and targets multi-signaling pathways in human dental papilla cells. PLoS One. 2012;7:e50090. doi: 10.1371/journal.pone.0050090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Sun F, Wan M, Xu X, Gao B, Zhou Y, Sun J, Cheng L, Klein OD, Zhou X, Zheng L. Crosstalk between miR-34a and Notch Signaling Promotes Differentiation in Apical Papilla Stem Cells (SCAPs) J Dent Res. 2014;93:589–595. doi: 10.1177/0022034514531146. [DOI] [PubMed] [Google Scholar]
- 137.Wang Y, Pang X, Wu J, Jin L, Yu Y, Gobin R, Yu J. MicroRNA hsa-let-7b suppresses the odonto/osteogenic differentiation capacity of stem cells from apical papilla by targeting MMP1. J Cell Biochem. 2018;119:6545–6554. doi: 10.1002/jcb.26737. [DOI] [PubMed] [Google Scholar]
- 138.Dernowsek JA, Pereira MC, Fornari TA, Macedo C, Assis AF, Donate PB, Bombonato-Prado KF, Passos-Bueno MR, Passos GA. Posttranscriptional Interaction Between miR-450a-5p and miR-28-5p and STAT1 mRNA Triggers Osteoblastic Differentiation of Human Mesenchymal Stem Cells. J Cell Biochem. 2017;118:4045–4062. doi: 10.1002/jcb.26060. [DOI] [PubMed] [Google Scholar]
- 139.Klingelhöffer C, Codrin C, Ettl T, Reichert T, Morsczeck C. miRNA-101 supports the osteogenic differentiation in human dental follicle cells. Arch Oral Biol. 2016;72:47–50. doi: 10.1016/j.archoralbio.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 140.Han X, Yang H, Cao Y, Ge L, Han N, Zhang C, Fan Z, Yao R. The miR-3940-5p inhibits cell proliferation of gingival mesenchymal stem cells. Oral Dis. 2019;25:1363–1373. doi: 10.1111/odi.13092. [DOI] [PubMed] [Google Scholar]
- 141.Liu Z, Xu S, Dao J, Gan Z, Zeng X. Differential expression of lncRNA/miRNA/mRNA and their related functional networks during the osteogenic/odontogenic differentiation of dental pulp stem cells. J Cell Physiol. 2020;235:3350–3361. doi: 10.1002/jcp.29223. [DOI] [PubMed] [Google Scholar]
- 142.Chen Z, Zhang K, Qiu W, Luo Y, Pan Y, Li J, Yang Y, Wu B, Fang F. Genome-wide identification of long noncoding RNAs and their competing endogenous RNA networks involved in the odontogenic differentiation of human dental pulp stem cells. Stem Cell Res Ther. 2020;11:114. doi: 10.1186/s13287-020-01622-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Shi R, Yang H, Lin X, Cao Y, Zhang C, Fan Z, Hou B. Analysis of the characteristics and expression profiles of coding and noncoding RNAs of human dental pulp stem cells in hypoxic conditions. Stem Cell Res Ther. 2019;10:89. doi: 10.1186/s13287-019-1192-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yi Q, Liu O, Yan F, Lin X, Diao S, Wang L, Jin L, Wang S, Lu Y, Fan Z. Analysis of Senescence-Related Differentiation Potentials and Gene Expression Profiles in Human Dental Pulp Stem Cells. Cells Tissues Organs. 2017;203:1–11. doi: 10.1159/000448026. [DOI] [PubMed] [Google Scholar]
- 145.Zhong YX, Li WS, Liao LS, Liang L. LncRNA CCAT1 promotes cell proliferation and differentiation via negative modulation of miRNA-218 in human DPSCs. Eur Rev Med Pharmacol Sci. 2019;23:3575–3583. doi: 10.26355/eurrev_201905_17779. [DOI] [PubMed] [Google Scholar]
- 146.Zeng L, Sun S, Han D, Liu Y, Liu H, Feng H, Wang Y. Long non-coding RNA H19/SAHH axis epigenetically regulates odontogenic differentiation of human dental pulp stem cells. Cell Signal. 2018;52:65–73. doi: 10.1016/j.cellsig.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 147.Tao R, Li YX, Liu YK, Liu F, Zhou ZY. Profiling lncRNA alterations during TNFα induced osteogenic differentiation of dental pulp stem cells. Mol Med Rep. 2019;19:2831–2836. doi: 10.3892/mmr.2019.9894. [DOI] [PubMed] [Google Scholar]
- 148.Qu Q, Fang F, Wu B, Hu Y, Chen M, Deng Z, Ma D, Chen T, Hao Y, Ge Y. Potential Role of Long Non-Coding RNA in Osteogenic Differentiation of Human Periodontal Ligament Stem Cells. J Periodontol. 2016;87:e127–e137. doi: 10.1902/jop.2016.150592. [DOI] [PubMed] [Google Scholar]
- 149.Zheng Y, Li X, Huang Y, Jia L, Li W. Time series clustering of mRNA and lncRNA expression during osteogenic differentiation of periodontal ligament stem cells. PeerJ. 2018;6:e5214. doi: 10.7717/peerj.5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Liu Y, Liu C, Zhang A, Yin S, Wang T, Wang Y, Wang M, Liu Y, Ying Q, Sun J, Wei F, Liu D, Wang C, Ge S. Down-regulation of long non-coding RNA MEG3 suppresses osteogenic differentiation of periodontal ligament stem cells (PDLSCs) through miR-27a-3p/IGF1 axis in periodontitis. Aging (Albany NY) 2019;11:5334–5350. doi: 10.18632/aging.102105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Deng L, Hong H, Zhang X, Chen D, Chen Z, Ling J, Wu L. Down-regulated lncRNA MEG3 promotes osteogenic differentiation of human dental follicle stem cells by epigenetically regulating Wnt pathway. Biochem Biophys Res Commun. 2018;503:2061–2067. doi: 10.1016/j.bbrc.2018.07.160. [DOI] [PubMed] [Google Scholar]
- 152.Wang L, Wu F, Song Y, Li X, Wu Q, Duan Y, Jin Z. Long noncoding RNA related to periodontitis interacts with miR-182 to upregulate osteogenic differentiation in periodontal mesenchymal stem cells of periodontitis patients. Cell Death Dis. 2016;7:e2327. doi: 10.1038/cddis.2016.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Xu Y, Qin W, Guo D, Liu J, Zhang M, Jin Z. LncRNA-TWIST1 Promoted Osteogenic Differentiation Both in PPDLSCs and in HPDLSCs by Inhibiting TWIST1 Expression. Biomed Res Int. 2019;2019:8735952. doi: 10.1155/2019/8735952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Jia B, Qiu X, Chen J, Sun X, Zheng X, Zhao J, Li Q, Wang Z. A feed-forward regulatory network lncPCAT1/miR-106a-5p/E2F5 regulates the osteogenic differentiation of periodontal ligament stem cells. J Cell Physiol. 2019;234:19523–19538. doi: 10.1002/jcp.28550. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 155.Huang Y, Han Y, Guo R, Liu H, Li X, Jia L, Zheng Y, Li W. Long non-coding RNA FER1L4 promotes osteogenic differentiation of human periodontal ligament stromal cells via miR-874-3p and vascular endothelial growth factor A. Stem Cell Res Ther. 2020;11:5. doi: 10.1186/s13287-019-1519-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Feng Y, Wan P, Yin L. Long Noncoding RNA X-Inactive Specific Transcript (XIST) Promotes Osteogenic Differentiation of Periodontal Ligament Stem Cells by Sponging MicroRNA-214-3p. Med Sci Monit. 2020;26:e918932. doi: 10.12659/MSM.918932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Jia Q, Chen X, Jiang W, Wang W, Guo B, Ni L. The Regulatory Effects of Long Noncoding RNA-ANCR on Dental Tissue-Derived Stem Cells. Stem Cells Int. 2016;2016:3146805. doi: 10.1155/2016/3146805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Jia Q, Jiang W, Ni L. Down-regulated non-coding RNA (lncRNA-ANCR) promotes osteogenic differentiation of periodontal ligament stem cells. Arch Oral Biol. 2015;60:234–241. doi: 10.1016/j.archoralbio.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 159.Peng W, Deng W, Zhang J, Pei G, Rong Q, Zhu S. Long noncoding RNA ANCR suppresses bone formation of periodontal ligament stem cells via sponging miRNA-758. Biochem Biophys Res Commun. 2018;503:815–821. doi: 10.1016/j.bbrc.2018.06.081. [DOI] [PubMed] [Google Scholar]
- 160.He Q, Yang S, Gu X, Li M, Wang C, Wei F. Long noncoding RNA TUG1 facilitates osteogenic differentiation of periodontal ligament stem cells via interacting with Lin28A. Cell Death Dis. 2018;9:455. doi: 10.1038/s41419-018-0484-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Wang Z, Huang Y, Tan L. Downregulation of lncRNA DANCR promotes osteogenic differentiation of periodontal ligament stem cells. BMC Dev Biol. 2020;20:2. doi: 10.1186/s12861-019-0206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Li Z, Yan M, Yu Y, Wang Y, Lei G, Pan Y, Li N, Gobin R, Yu J. LncRNA H19 promotes the committed differentiation of stem cells from apical papilla via miR-141/SPAG9 pathway. Cell Death Dis. 2019;10:130. doi: 10.1038/s41419-019-1337-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Pan Y, Lu T, Peng L, Chen Z, Li M, Zhang K, Xiong F, Wu B. Vacuolar protein sorting 4B regulates the proliferation and odontoblastic differentiation of human dental pulp stem cells through the Wnt-β-catenin signalling pathway. Artif Cells Nanomed Biotechnol. 2019;47:2575–2584. doi: 10.1080/21691401.2019.1629950. [DOI] [PubMed] [Google Scholar]
- 164.Zhang X, Ning T, Wang H, Xu S, Yu H, Luo X, Hao C, Wu B, Ma D. Stathmin regulates the proliferation and odontoblastic/osteogenic differentiation of human dental pulp stem cells through Wnt/β-catenin signaling pathway. J Proteomics. 2019;202:103364. doi: 10.1016/j.jprot.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 165.Scheller EL, Chang J, Wang CY. Wnt/beta-catenin inhibits dental pulp stem cell differentiation. J Dent Res. 2008;87:126–130. doi: 10.1177/154405910808700206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Rolph DN, Deb M, Kanji S, Greene CJ, Das M, Joseph M, Aggarwal R, Leblebicioglu B, Das H. Ferutinin directs dental pulp-derived stem cells towards the osteogenic lineage by epigenetically regulating canonical Wnt signaling. Biochim Biophys Acta Mol Basis Dis. 2020;1866:165314. doi: 10.1016/j.bbadis.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hasegawa D, Wada N, Yoshida S, Mitarai H, Arima M, Tomokiyo A, Hamano S, Sugii H, Maeda H. Wnt5a suppresses osteoblastic differentiation of human periodontal ligament stem cell-like cells via Ror2/JNK signaling. J Cell Physiol. 2018;233:1752–1762. doi: 10.1002/jcp.26086. [DOI] [PubMed] [Google Scholar]
- 168.Chen Z, Gibson TB, Robinson F, Silvestro L, Pearson G, Xu B, Wright A, Vanderbilt C, Cobb MH. MAP kinases. Chem Rev. 2001;101:2449–2476. doi: 10.1021/cr000241p. [DOI] [PubMed] [Google Scholar]
- 169.Kim JH, Kim SY, Woo SM, Jeong HN, Jung JY, Kim SM, Lim HS. Combination of mineral trioxide aggregate and propolis promotes odontoblastic differentiation of human dental pulp stem cells through ERK signaling pathway. Food Sci Biotechnol. 2019;28:1801–1809. doi: 10.1007/s10068-019-00609-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kong Y, Hu X, Zhong Y, Xu K, Wu B, Zheng J. Magnesium-enriched microenvironment promotes odontogenic differentiation in human dental pulp stem cells by activating ERK/BMP2/Smads signaling. Stem Cell Res Ther. 2019;10:378. doi: 10.1186/s13287-019-1493-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Liu J, Zhao X, Pei D, Sun G, Li Y, Zhu C, Qiang C, Sun J, Shi J, Dong Y, Gou J, Wang S, Li A. The promotion function of Berberine for osteogenic differentiation of human periodontal ligament stem cells via ERK-FOS pathway mediated by EGFR. Sci Rep. 2018;8:2848. doi: 10.1038/s41598-018-21116-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Ge X, Li Z, Jing S, Wang Y, Li N, Lu J, Yu J. Parathyroid hormone enhances the osteo/odontogenic differentiation of dental pulp stem cells via ERK and P38 MAPK pathways. J Cell Physiol. 2020;235:1209–1221. doi: 10.1002/jcp.29034. [DOI] [PubMed] [Google Scholar]
- 173.Tao Z, Barker J, Shi SD, Gehring M, Sun S. Steady-state kinetic and inhibition studies of the mammalian target of rapamycin (mTOR) kinase domain and mTOR complexes. Biochemistry. 2010;49:8488–8498. doi: 10.1021/bi100673c. [DOI] [PubMed] [Google Scholar]
- 174.Tanaka Y, Sonoda S, Yamaza H, Murata S, Nishida K, Hama S, Kyumoto-Nakamura Y, Uehara N, Nonaka K, Kukita T, Yamaza T. Suppression of AKT-mTOR signal pathway enhances osteogenic/dentinogenic capacity of stem cells from apical papilla. Stem Cell Res Ther. 2018;9:334. doi: 10.1186/s13287-018-1077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Feng X, Huang D, Lu X, Feng G, Xing J, Lu J, Xu K, Xia W, Meng Y, Tao T, Li L, Gu Z. Insulin-like growth factor 1 can promote proliferation and osteogenic differentiation of human dental pulp stem cells via mTOR pathway. Dev Growth Differ. 2014;56:615–624. doi: 10.1111/dgd.12179. [DOI] [PubMed] [Google Scholar]
- 176.Kim JK, Baker J, Nor JE, Hill EE. mTor plays an important role in odontoblast differentiation. J Endod. 2011;37:1081–1085. doi: 10.1016/j.joen.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 177.Jia L, Xiong Y, Zhang W, Ma X, Xu X. Metformin promotes osteogenic differentiation and protects against oxidative stress-induced damage in periodontal ligament stem cells via activation of the Akt/Nrf2 signaling pathway. Exp Cell Res. 2020;386:111717. doi: 10.1016/j.yexcr.2019.111717. [DOI] [PubMed] [Google Scholar]
- 178.Zhang C, Chang J, Sonoyama W, Shi S, Wang CY. Inhibition of human dental pulp stem cell differentiation by Notch signaling. J Dent Res. 2008;87:250–255. doi: 10.1177/154405910808700312. [DOI] [PubMed] [Google Scholar]
- 179.Wang X, He H, Wu X, Hu J, Tan Y. Promotion of dentin regeneration via CCN3 modulation on Notch and BMP signaling pathways. Biomaterials. 2014;35:2720–2729. doi: 10.1016/j.biomaterials.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 180.Ma D, Yu H, Xu S, Wang H, Zhang X, Ning T, Wu B. Stathmin inhibits proliferation and differentiation of dental pulp stem cells via sonic hedgehog/Gli. J Cell Mol Med. 2018;22:3442–3451. doi: 10.1111/jcmm.13621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Zhou Y, Zheng L, Zhou X, Li J, Xu X. Dental Mesenchymal Stem Cells in Inflamed Microenvironment: Potentials and Challenges for Regeneration. Curr Stem Cell Res Ther. 2015;10:412–421. doi: 10.2174/1574888x10666150312102324. [DOI] [PubMed] [Google Scholar]
- 182.Bindal P, Ramasamy TS, Kasim NHA, Gnanasegaran N, Chai WL. Immune responses of human dental pulp stem cells in lipopolysaccharide-induced microenvironment. Cell Biol Int. 2018;42:832–840. doi: 10.1002/cbin.10938. [DOI] [PubMed] [Google Scholar]
- 183.Soancă A, Lupse M, Moldovan M, Pall E, Cenariu M, Roman A, Tudoran O, Surlin P, Șorițău O. Applications of inflammation-derived gingival stem cells for testing the biocompatibility of dental restorative biomaterials. Ann Anat. 2018;218:28–39. doi: 10.1016/j.aanat.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 184.Liao J, Al Shahrani M, Al-Habib M, Tanaka T, Huang GT. Cells isolated from inflamed periapical tissue express mesenchymal stem cell markers and are highly osteogenic. J Endod. 2011;37:1217–1224. doi: 10.1016/j.joen.2011.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Lee S, Zhang QZ, Karabucak B, Le AD. DPSCs from Inflamed Pulp Modulate Macrophage Function via the TNF-α/IDO Axis. J Dent Res. 2016;95:1274–1281. doi: 10.1177/0022034516657817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Dokić J, Tomić S, Cerović S, Todorović V, Rudolf R, Colić M. Characterization and immunosuppressive properties of mesenchymal stem cells from periapical lesions. J Clin Periodontol. 2012;39:807–816. doi: 10.1111/j.1600-051X.2012.01917.x. [DOI] [PubMed] [Google Scholar]
- 187.Zhai Y, Wang Y, Rao N, Li J, Li X, Fang T, Zhao Y, Ge L. Activation and Biological Properties of Human β Defensin 4 in Stem Cells Derived From Human Exfoliated Deciduous Teeth. Front Physiol. 2019;10:1304. doi: 10.3389/fphys.2019.01304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Boyle M, Chun C, Strojny C, Narayanan R, Bartholomew A, Sundivakkam P, Alapati S. Chronic inflammation and angiogenic signaling axis impairs differentiation of dental-pulp stem cells. PLoS One. 2014;9:e113419. doi: 10.1371/journal.pone.0113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Xu XY, He XT, Wang J, Li X, Xia Y, Tan YZ, Chen FM. Role of the P2X7 receptor in inflammation-mediated changes in the osteogenesis of periodontal ligament stem cells. Cell Death Dis. 2019;10:20. doi: 10.1038/s41419-018-1253-y. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 190.Zhai QM, Li B, Wang ZW, Liu L, Jin Y, Jin F. [Endoplasmic reticulum-mitochondrial contact regulates osteogenic differentiation of periodontal ligament stem cells via mitofusion 2 in inflammatory microenvironment] Zhonghua Kou Qiang Yi Xue Za Zhi. 2018;53:453–458. doi: 10.3760/cma.j.issn.1002-0098.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 191.Tang HN, Xia Y, Yu Y, Wu RX, Gao LN, Chen FM. Stem cells derived from "inflamed" and healthy periodontal ligament tissues and their sheet functionalities: a patient-matched comparison. J Clin Periodontol. 2016;43:72–84. doi: 10.1111/jcpe.12501. [DOI] [PubMed] [Google Scholar]
- 192.Park JC, Kim JM, Jung IH, Kim JC, Choi SH, Cho KS, Kim CS. Isolation and characterization of human periodontal ligament (PDL) stem cells (PDLSCs) from the inflamed PDL tissue: in vitro and in vivo evaluations. J Clin Periodontol. 2011;38:721–731. doi: 10.1111/j.1600-051X.2011.01716.x. [DOI] [PubMed] [Google Scholar]
- 193.Li C, Wang X, Tan J, Wang T, Wang Q. The immunomodulatory properties of periodontal ligament stem cells isolated from inflamed periodontal granulation. Cells Tissues Organs. 2014;199:256–265. doi: 10.1159/000367986. [DOI] [PubMed] [Google Scholar]
- 194.Marrelli M, Paduano F, Tatullo M. Cells isolated from human periapical cysts express mesenchymal stem cell-like properties. Int J Biol Sci. 2013;9:1070–1078. doi: 10.7150/ijbs.6662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Um S, Lee JH, Seo BM. TGF-β2 downregulates osteogenesis under inflammatory conditions in dental follicle stem cells. Int J Oral Sci. 2018;10:29. doi: 10.1038/s41368-018-0028-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Alt EU, Senst C, Murthy SN, Slakey DP, Dupin CL, Chaffin AE, Kadowitz PJ, Izadpanah R. Aging alters tissue resident mesenchymal stem cell properties. Stem Cell Res. 2012;8:215–225. doi: 10.1016/j.scr.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 197.Iezzi I, Cerqueni G, Licini C, Lucarini G, Mattioli Belmonte M. Dental pulp stem cells senescence and regenerative potential relationship. J Cell Physiol. 2019;234:7186–7197. doi: 10.1002/jcp.27472. [DOI] [PubMed] [Google Scholar]
- 198.Wu W, Zhou J, Xu CT, Zhang J, Jin YJ, Sun GL. Derivation and growth characteristics of dental pulp stem cells from patients of different ages. Mol Med Rep. 2015;12:5127–5134. doi: 10.3892/mmr.2015.4106. [DOI] [PubMed] [Google Scholar]
- 199.Wang K, Li L, Wu J, Qiu Q, Zhou F, Wu H. The different expression profiles of microRNAs in elderly and young human dental pulp and the role of miR-433 in human dental pulp cells. Mech Ageing Dev. 2015;146-148:1–11. doi: 10.1016/j.mad.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 200.Wang H, Zhong Q, Yang T, Qi Y, Fu M, Yang X, Qiao L, Ling Q, Liu S, Zhao Y. Comparative characterization of SHED and DPSCs during extended cultivation in vitro. Mol Med Rep. 2018;17:6551–6559. doi: 10.3892/mmr.2018.8725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Naka T, Yokose S. Spatiotemporal expression of sclerostin in odontoblasts during embryonic mouse tooth morphogenesis. J Endod. 2011;37:340–345. doi: 10.1016/j.joen.2010.11.025. [DOI] [PubMed] [Google Scholar]
- 202.Ou Y, Zhou Y, Liang S, Wang Y. Sclerostin promotes human dental pulp cells senescence. PeerJ. 2018;6:e5808. doi: 10.7717/peerj.5808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Bakopoulou A, Leyhausen G, Volk J, Papachristou E, Koidis P, Geurtsen W. Wnt/β-catenin signaling regulates Dental Pulp Stem Cells' responses to pulp injury by resinous monomers. Dent Mater. 2015;31:542–555. doi: 10.1016/j.dental.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 204.Zhao Y, Yuan X, Bellido T, Helms JA. A Correlation between Wnt/Beta-catenin Signaling and the Rate of Dentin Secretion. J Endod. 2019;45:1357–1364.e1. doi: 10.1016/j.joen.2019.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Feng X, Xing J, Feng G, Sang A, Shen B, Xu Y, Jiang J, Liu S, Tan W, Gu Z, Li L. Age-dependent impaired neurogenic differentiation capacity of dental stem cell is associated with Wnt/β-catenin signaling. Cell Mol Neurobiol. 2013;33:1023–1031. doi: 10.1007/s10571-013-9965-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Feng X, Xing J, Feng G, Huang D, Lu X, Liu S, Tan W, Li L, Gu Z. p16(INK4A) mediates age-related changes in mesenchymal stem cells derived from human dental pulp through the DNA damage and stress response. Mech Ageing Dev. 2014;141-142:46–55. doi: 10.1016/j.mad.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 207.Mas-Bargues C, Viña-Almunia J, Inglés M, Sanz-Ros J, Gambini J, Ibáñez-Cabellos JS, García-Giménez JL, Viña J, Borrás C. Role of p16INK4a and BMI-1 in oxidative stress-induced premature senescence in human dental pulp stem cells. Redox Biol. 2017;12:690–698. doi: 10.1016/j.redox.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Mehrazarin S, Oh JE, Chung CL, Chen W, Kim RH, Shi S, Park NH, Kang MK. Impaired odontogenic differentiation of senescent dental mesenchymal stem cells is associated with loss of Bmi-1 expression. J Endod. 2011;37:662–666. doi: 10.1016/j.joen.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ma D, Ma Z, Zhang X, Wang W, Yang Z, Zhang M, Wu G, Lu W, Deng Z, Jin Y. Effect of age and extrinsic microenvironment on the proliferation and osteogenic differentiation of rat dental pulp stem cells in vitro. J Endod. 2009;35:1546–1553. doi: 10.1016/j.joen.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 210.Ning T, Shao J, Zhang X, Luo X, Huang X, Wu H, Xu S, Wu B, Ma D. Ageing affects the proliferation and mineralization of rat dental pulp stem cells under inflammatory conditions. Int Endod J. 2020;53:72–83. doi: 10.1111/iej.13205. [DOI] [PubMed] [Google Scholar]
- 211.Horibe H, Murakami M, Iohara K, Hayashi Y, Takeuchi N, Takei Y, Kurita K, Nakashima M. Isolation of a stable subpopulation of mobilized dental pulp stem cells (MDPSCs) with high proliferation, migration, and regeneration potential is independent of age. PLoS One. 2014;9:e98553. doi: 10.1371/journal.pone.0098553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Huang CC, Narayanan R, Alapati S, Ravindran S. Exosomes as biomimetic tools for stem cell differentiation: Applications in dental pulp tissue regeneration. Biomaterials. 2016;111:103–115. doi: 10.1016/j.biomaterials.2016.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Hu X, Zhong Y, Kong Y, Chen Y, Feng J, Zheng J. Lineage-specific exosomes promote the odontogenic differentiation of human dental pulp stem cells (DPSCs) through TGFβ1/smads signaling pathway via transfer of microRNAs. Stem Cell Res Ther. 2019;10:170. doi: 10.1186/s13287-019-1278-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Chew JRJ, Chuah SJ, Teo KYW, Zhang S, Lai RC, Fu JH, Lim LP, Lim SK, Toh WS. Mesenchymal stem cell exosomes enhance periodontal ligament cell functions and promote periodontal regeneration. Acta Biomater. 2019;89:252–264. doi: 10.1016/j.actbio.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 215.Wang M, Li J, Ye Y, He S, Song J. SHED-derived conditioned exosomes enhance the osteogenic differentiation of PDLSCs via Wnt and BMP signaling in vitro. Differentiation. 2020;111:1–11. doi: 10.1016/j.diff.2019.10.003. [DOI] [PubMed] [Google Scholar]
- 216.Li Z, Liang Y, Pan K, Li H, Yu M, Guo W, Chen G, Tian W. Schwann cells secrete extracellular vesicles to promote and maintain the proliferation and multipotency of hDPCs. Cell Prolif. 2017:50. doi: 10.1111/cpr.12353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Čebatariūnienė A, Kriaučiūnaitė K, Prunskaitė J, Tunaitis V, Pivoriūnas A. Extracellular Vesicles Suppress Basal and Lipopolysaccharide-Induced NFκB Activity in Human Periodontal Ligament Stem Cells. Stem Cells Dev. 2019;28:1037–1049. doi: 10.1089/scd.2019.0021. [DOI] [PubMed] [Google Scholar]
- 218.Pizzicannella J, Diomede F, Gugliandolo A, Chiricosta L, Bramanti P, Merciaro I, Orsini T, Mazzon E, Trubiani O. 3D Printing PLA/Gingival Stem Cells/ EVs Upregulate miR-2861 and -210 during Osteoangiogenesis Commitment. Int J Mol Sci. 2019:20. doi: 10.3390/ijms20133256. [DOI] [PMC free article] [PubMed] [Google Scholar]