Abstract
Stem cell therapies are successfully used in various fields of medicine. This new approach of research is also expanding in ophthalmology. Huge investments, resources and important clinical trials have been performed in stem cell research and in potential therapies. In recent years, great strides have been made in genetic research, which permitted and enhanced the differentiation of stem cells. Moreover, the possibility of exploiting stem cells from other districts (such as adipose, dental pulp, bone marrow stem cells, etc.) for the treatment of ophthalmic diseases, renders this topic fascinating. Furthermore, great strides have been made in biomedical engineering, which have proposed new materials and three-dimensional structures useful for cell therapy of the eye. The encouraging results obtained on clinical trials conducted on animals have given a significant boost in the creation of study protocols also in humans. Results are limited to date, but clinical trials continue to evolve. Our attention is centered on the literature reported over the past 20 years, considering animal (the most represented in literature) and human clinical trials, which are limiting. The aim of our review is to present a brief overview of the main types of treatments based on stem cells in the field of ophthalmic pathologies.
Keywords: Stem cells, Multipotent mesenchymal cells, Adipose stem cells, Novel therapies, Eye pathology, Cornea, Cell therapies, New materials
Core Tip: Stem cell therapies have shown great potential in ophthalmopathies. Interesting results have arisen in the treatment of ocular surface diseases and for their neuroprotective effect. Stem cells can be transplanted, injected or topically applied. The main goals of treatments include preventing vision loss, restoring sight, recreating the connections with the central nervous system, and regenerating eye tissues. Recent discoveries have permitted the use of stem cells taken from other districts. From literature analysis, it is clear that stem cells can provide a potentially successful solution; however, ethical issues, costs and possible long term side effects limit the current use.
INTRODUCTION
Numerous studies in scientific medical literature continually show that cell therapy tends to be an effective alternative and innovative method to regenerate damaged tissue[1]. In the last decades, studies have shown that stem cell therapies can bring substantial benefits to patients suffering from a wide range of diseases and injuries[2]. For this reason, huge investments, resources and important clinical trials have been performed in stem cell research and potential therapies based on stem cells. In these past years, there has been a continuing expansion in the number and types of stem cells assessed for potential treatment use. Stem cells are now being used in various fields of medicine, ranging from hematology to cardiology, in addition to neurology, plastic surgery, dentistry, etc.[3-5]. Although literature has reported limited success to date, clinical trials continue to evolve as our understanding enhances regarding the physiology and mechanisms underlying potential healing benefits behind stem cells. Recent advancements in regenerative medicine have also considered the use of stem cells for cellular repair and regeneration[6].
Stem cell therapies have shown great potential in numerous studies reported in literature concerning injuries and diseases of the eye[3]. This progress is a result of several factors, including the relatively small numbers of cells required, easy accessibility for surgery and straightforward assessment and visualization of grafts. Numerous types of cells have been used in clinical trials for the eye[2]. Research on stem cell therapies has been applied to almost all parts of the eye.
Based on our preliminary animal experiments regarding stem cells therapies in corneal healing[3,7], and the growing number of studies that show great clinical potentials of stem cells for this therapeutic approach, we decided to assess the literature reported in the last 20 years. Considering that the number of studies reported in literature since 2000 is immense, and our experience in this field is limiting, we do not intend to provide an exhaustive meta-analysis, but a quick overview of the use of stem cells for ophthalmology treatment; thus, we apologize in advance if opinion leaders and experts in this field of study have not been cited in our paper. The aim of our review is to present a brief overview of the main types of treatments based on stem cells in the field of ophthalmic pathologies, by briefly addressing the what, why, which, how, when and where of this issue. We have tried to concentrate or review on pertinent human studies; however, considering most of the literature to date tends to be based on animal experimentation, mention has also been made regarding this vast body of literature.
MATERIALS AND METHODS
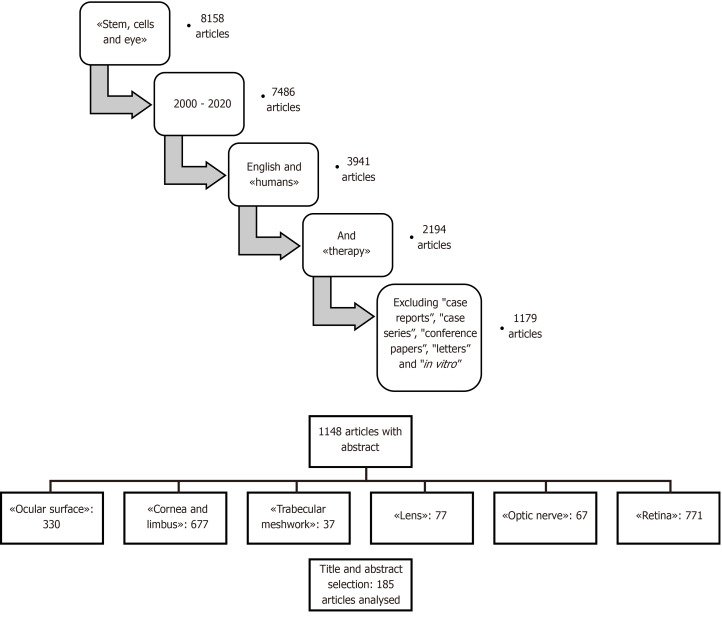
We conducted a search of the literature published between January 1, 2000, to December 20, 2020, using MEDLINE (PubMed). The database was first searched using the key words “stem, cell and eye”, in which 7486 studies were found. We considered only studies in English and those referring to humans, thus reducing the count to 3941. The reference lists of all retrieved articles were scanned to identify additional relevant studies. We then considered only articles based on “stem cells therapy” (2194 papers), and we excluded “case reports”, “case series”, “conference papers”, “letters” and “in vitro” (1179 articles). Results were then divided and sorted by when/where stem cells were used, which included: Ocular surface; corneal epithelium, stroma, endothelium, limbus; trabecular meshwork; lens; optic nerve; retina. The details regarding the selection of papers considered in the manuscript are listed in Figure 1.
Figure 1.
The selection of PubMed literature published from 2000 to 2020, which was considered in the manuscript.
Only articles with abstracts were considered (1148 articles). After a selection by title and abstract, 185 articles were analyzed. A quality score was calculated for each article using a checklist from the American Society of Plastic Surgeons guidelines for therapeutic studies[7]. Each study was appraised by at least two reviewers (GM and MZ), and rating decisions were based on the consensus of the reviewing authors. A summary of the most significant studies and conclusions is reported in Tables 1 and 2.
Table 1.
Clinical trials in ocular diseases
|
Ophthalmic disease
|
Ref.
|
Stem cells used
|
In animals or humans
|
Conclusions
|
| Ocular surface, cornea and limbus | Kenyon and Tseng[52], 1989 | Limbal tissue autograft transplantation (LSCs) | Humans | Patients have consistently shown improved visual acuity, rapid surface healing, stable epithelial adhesion without recurrent erosion, arrest or regression of corneal neovascularization |
| Lindberg et al[53], 1993 | LSCs | Humans | Corneal epithelial stem cells are located in the limbus and indicate that cultured autologous limbal cells may function as grafts to permanently restore the corneal epithelium after severe ocular surface injury | |
| Ma et al[54], 2006 | MSCs like LSCs on amniotic membrane | Animals | Therapeutic effect due to the inhibition of inflammation and neovascularization | |
| Kwitko et al[57], 1995 | Conjunctival autograft transplantation | Humans | Conjunctival transplantation proved to be an adequate method of treating severe bilateral surface disorders, with minimal complications | |
| Croasdale et al[58], 1999 | Keratolimbal allograft | Humans | KLAL transplantation for patients with severe ocular-surface disease is an important management option | |
| Tsai et al[59], 2000 | Limbal epithelial cells | Humans | By 1 mo, the ocular surface was covered with corneal epithelium, and the clarity of the cornea was improved in 83% of patients | |
| Sangwan et al[60], 2012 | Limbal tissue | Humans | After surgery, a completely epithelialized, avascular and stable corneal surface was seen in all recipient eyes by 6 wk | |
| Kushnerev et al[61], 2016 | Dental pulp stem cells | Animals | Dental pulp stem cells were successfully isolated, labeled, and delivered to the corneal surface | |
| Chan et al[66], 2013 | iPSCs | Animals | hES cells can be induced to differentiate into keratocytes in vitro. Pluripotent stem cells may provide a renewable source of material for development of treatment of corneal stromal opacities | |
| Susaimanickam et al[67], 2017 | iPSCs | Animals | PSC-derived corneal epithelial cells offer an alternative tissue source for regenerating different layers of the cornea and eliminate the need for complicated cell enrichment procedures | |
| Zeppier et al[3], 2017 | MSCs | Animals | Better corneal repair in epithelium and stromal layers in stem cell treated eyes | |
| Reinshagen et al[68], 2011 | BM-MSCs | Animals | BM-MSCs could differentiate into cornel epithelial like cells in vivo in rat damaged corneas | |
| Gu et al[70], 2009 | BM-MSCs | Animals | BM-MSCs could differentiate into cornel epithelial like cells | |
| Beyazyildiz et al[46], 2014 | MSCs | Animals | Topical application of MSCs could be a safe and effective method for the treatment of DES | |
| Reza et al[73], 2011 | LSCs | Animals | Transplantation of a bioengineered CLEC-muc sheet in limbal stem cell-deficient rabbit eyes resulted in regeneration of a smooth, clear corneal surface | |
| Nishida et al[76], 2004 | Oral mucosal stem cells | Humans | Complete reepithelialization of the corneal surfaces occurred within 1 wk in all four treated eyes. Corneal transparency was restored and postoperative visual acuity improved | |
| Corneal stroma and endothelium | Sepsakos et al[79], 2017 | Ocular surface SCs | Humans | Without addressing the underlying stem cell deficiency, keratoplasty in patients with total limbal stem cell deficiency will ultimately fail in all cases |
| Naylor et al[81], 2016 | iPSCs | Humans | The hiPSC-derived NCCs acquired a keratocyte-like morphology and an expression profile similar to corneal keratocytes in vivo | |
| Alió Del Barrio et al[84], 2017 | ASCs | Humans | Safety of corneal stromal transplantation of autologous ASCs in humans, showing cell survival in vivo and the ability of these cells to produce a low amount of new collagen in patients with advanced keratoconus | |
| Coulson-Thomas et al[85], 2013 | UC-MSCs | Animals | UC-MSCs transplantation may be a feasible alternative to keratoplasty in treating congenital disorders of the cornea secondary to keratocyte dysfunction | |
| Yam et al[88], 2018 | Perodontal ligament SCs | Animals | Potential translation of PDL cells for regenerative corneal cell therapy for corneal opacities | |
| Joyce et al[89], 2012 | UC-MSCs | Animals | UCB MSCs are able to "home" to areas of injured corneal endothelium and that the phenotype of UCB MSCs can be altered toward that of HCEC-like cells | |
| Trabecular meshwork | Abu-Hassan et al[93], 2015 | iPSCs | Animals | TM-like iPSCs became similar to TM cells in both morphology and expression patterns. When transplanted, they were able to fully restore intraocular pressure homeostatic function |
| Manuguerra-Gagné et al[95], 2013 | MSCs | Animals | MSC and their secreted factors induced reactivation of a progenitor cell pool found in the ciliary body and increased cellular proliferation | |
| Lens | Lin et al[96], 2016 | LECs | Both | Surgical method of cataract removal that preserves endogenous LECs and achieves functional lens regeneration in rabbits and macaques, as well as in human infants with cataracts |
| Murphy et al[98], 2018 | PSCs | Animals | We demonstrate large-scale production of light-focusing human micro-lenses from spheroidal masses of human lens epithelial cells purified from differentiating pluripotent stem cells | |
| ON | Kuwahara et al[102], 2015 | hESCs | Animals | Multipotent stem cells within the CM contribute to de novo retinal tissue growth |
| Mesentier-Louro et al[105], 2019 | iPSCs | Animals | Between 1% and 7% of iPSCs-derived RGCs integrated into the ganglion cell layer after intravitreal injection, and about 20% after combined injection of RGCs and iPSCs | |
| Zhang et al[107], 2015 | UC-MSCs | Animals | Human umbilical cord blood stem cells and brain-derived neurotrophic factor effectively repair the injured optical nerve, improve biomechanical properties, and contribute to the recovery after injury |
ASC: Adipose-derived stem cell; BM-MSC: Bone marrow-mesenchymal stem cell; CLEs: Cutaneous lupus erythematosus; CM: Ciliary margin; DES: Discrete event simulation; HCEC: Human corneal endothelial cell; hESCs: Human embryonic stem cells; hiPSC: Human-induced pluripotent stem cells; iPSC: induced pluripotent stem cell; KLAL: Keratolimbal allograft; LEC: Lens epithelial stem/progenitor cell; LSC: Limbal stem cell; MSC: Mesenchymal stem cell; NCC: Neurocysticercosis; ON: Optic nerve; PDL: Periodontal ligament; PSC: Pluripotent stem cell; RGC: Retinal ganglion cell; TM: Trabecular meshwork; UC-MSCs: Umbilical cord-mesenchymal stem cell; UCB: Umbilical cord blood.
Table 2.
Retinal diseases and therapies
|
Ophthalmic disease
|
Ref.
|
Stem cells used
|
In animals or in humans
|
Conclusions
|
| Retina | Van Meurs et al[109], 2004 | RPE cells | Humans | A pigmented area was seen in the extraction bed of the neovascular membrane in only one patient |
| Tucker et al[110], 2011 | iPSCs | Animals | Adult fibroblast-derived iPSCs provide a viable source for the production of retinal precursors to be used for transplantation and treatment of retinal degenerative disease | |
| Lamba et al[111], 2006 | hESCs | Animals | hES cell derived retinal progenitors integrate with the degenerated mouse retina and increase in their expression of photoreceptor-specific markers | |
| Nakano et al[48], 2012 | IPSCs/hESCs | Humans | We demonstrate that an optic cup structure can form by self-organization in hESC culture | |
| Gonzalez-Cordero et al[113], 2013 | ESCs | Animals | We show that rod precursors integrate within degenerate retinas of adult mice and mature into outer segment-bearing photoreceptors | |
| Schwartz et al[40], 2015 | hESCs | Humans | First evidence of the medium-term to long-term safety, graft survival, and possible biological activity of pluripotent stem cell progeny in individuals with macular diseases | |
| Schwartz et al[114], 2012 | hESCs | Humans | The hESC-derived RPE cells showed no signs of hyperproliferation, tumorigenicity, ectopic tissue formation, or apparent rejection after 4 mo | |
| Gaddam et al[120], 2019 | Adult stem cells | Humans | The paracrine nature of adipose stem cells, in particular, has been highlighted as a potential solution to the lack of a homing and conducive environment that poses a challenge to the implantation of exogenous stem cells in the target tissue |
hESCs: Human embryonic stem cells; iPSC: induced pluripotent stem cell; RPE: Retinal pigment epithelium.
What are stem cells
In brief, stem cells are undifferentiated cells that are present in the embryonic, fetal and adult stages of life and give rise to differentiated cells, which are the building blocks of tissue and organs. In the post-natal and adult stages of life, tissue-specific stem cells are found in differentiated organs and are instrumental in repair following injury to the organ. The main characteristics of stem cells are self-renewal (the ability to proliferate extensively), clonality (usually arising from a single cell) and potency (the ability to differentiate into different cell types)[8].
Stem cells can be classified as totipotent (zygote), pluripotent [embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs)], multipotent [mesenchymal stem cells (MSCs)] and oligopotent. Totipotent cells form embryonic and extra-embryonic tissues. Pluripotent cells form all three germ layers, while multipotent cells generate cells limited to one germ layer.
The human body develops from the zygote and blastocyst from which ESCs are derived into germ layers endoderm, mesoderm and ectoderm. Specific organs arise from germ layers. Some of the progenitor cells that have contributed to organ formation do not terminally differentiate but are retained as tissue stem cells and can be found in bone marrow, bone, blood, muscle, liver, brain, adipose tissue, skin and gastrointestinal tract[9]. The tissue stem cells may be called progenitor cells since they give rise to terminally differentiated and specialized cells of the tissue or organ. These cells may be dormant within tissues; however, have the ability to proliferate under circumstances of injury and repair[10]. The dynamics of tissue stem cells or progenitor cells varies from tissue to tissue. In bone marrow, liver, lung and gut, for example, stem cells regularly proliferate to supplement cells during normal turnover of cells or tissue injury. In other organs, however, like pancreas, heart or nervous system, stem cells proliferate to replace damaged cells following injury[11,12].
Why use stem cells in ocular diseases
The human eye is a remarkable structure produced from the coordinated development of multiple tissues. It is the result of a combination of tissues deriving from neuroectodermal (e.g., retina), ectodermal (e.g., lens and cornea) and mesodermal lines. Diseases and injuries that compromise the function of any of these major ocular tissues can lead to blindness[13,14]. Considering the fundamental importance and influence on quality of life of sight, research has invested enormous resources and studies towards the search for new therapies to prevent and treat ocular disorders. There is a notable history of trail-blazing work in ocular medicine, exemplified by tissue transplantation, the use of laser therapy, the recent gene-therapy and cell therapy[14]. Due to burden of eye disease, and its relative ease of accessibility, the eye is a prime target for stem cell transplantation therapies, in which complications tend to be rare (e.g., overgrowth and tumor formation)[15]. In addition, advanced methods currently exist to examine easily and thoroughly assess the clinical results of eye transplant therapies. Modern technology is readily available to provide a non-invasive quantifiable visualization of most structures of the eye, and visual functions can routinely be assessed rapidly, quantitatively and accurately.
Which stem cells can be considered for treatment in ophthalmology
Human pluripotent stem cells: ESCs and iPSCs: Human pluripotent stem cells (hPSCs) have been considered promising sources for regenerating damaged tissues and organs because of their ability to differentiate into cells from three embryonic germ layers[16]. These cells can also be maintained in an undifferentiated state for a prolonged period in culture[8]. There are numerous scientific studies regarding therapy with hPSCs, specifically, in the form of iPSCs. Several studies have reported the use of iPSCs in retinal degenerative pathologies[2,17,18]. hPSCs have the greatest potential for cell replacement and can be successfully pre-differentiated prior to transplantation in the eye. iPSCs are pluripotent stem cells generated from somatic cells by cellular genetic reprogramming using defined transcription factors[8]. First described in 2007 by Takahashi et al[19], iPSCs used in the experiments were derived from skin fibroblasts produced using retroviral technology[19]. iPSCs provide a unique in vitro model that allows the generation of retinal progenitor cells. An advantage of iPSCs made from a patient’s own cells could reduce the need for immunoprotective regimens post-transplantation[15]. It has been demonstrated that these iPSCs have similar characteristics features of PSCs, conserving the possibility to generate tissues from each of the three germ layers[20]. The greatest problem reported regarding iPSCs was genomic instability, which may induce teratoma. The aim of research in recent years has been to create safety protocols capable of guaranteeing genomic stability[21]. The greatest success of hPSCs has been in retinal pigment epithelial cell (RPE)/photoreceptor replacement for aged-related macular degeneration (AMD), but studies have also reported the potential successful use in almost all structures of the eye[22,23].
Adult stem cells: The use of adult stem cells represents an easier route to regenerative-cell therapies. The ability of some adult tissues (i.e. skin, haemopoietic system, bone, liver, etc.) to repair or renew, indicates the presence of stem or progenitor cells[9]. Numerous clinical trials based on the use of adult stem cells have also been developed in the field of ophthalmology.
Considering that the component of the eye, mainly the retina, is directly derived from the central nervous system (CNS), studies regarding cell therapy have shown to be difficult, limiting, yet potentially fascinating. The nervous system was thought to be rigidly constructed, with no capacity for physical repair. However, studies of nerve development have led to isolation of cells from the developing and mature mammalian CNS that shows numerous properties of stem cells [neural stem cells (NSCs)][9]. NSCs have been studied with success in spinal cord injury and traumatic brain injury[24]. NSCs secrete trophic factors, and therapies involving these cells may have potential for the neuroprotection of photoreceptors rather than replacement of retinal neurons, including retinal ganglion cells (RGC)[22,25].
Bone marrow stem cells (BMSCs) are progenitors of bone, cartilage and skeletal tissues, in addition to the hematopoiesis-supporting stroma and adipocyte cells. These cells can differentiate into mesenchymal cells, visceral mesoderm, neuroectoderm and endoderm characteristics in vitro[26]. In ophthalmology, BMSCs can be used to prevent graft vs host disease in corneal transplantation. These cells have also been studied in retinal diseases. The rationale for exploring the use of BMSCs as a potential therapy is a paracrine trophic effect on degenerating ischemic retina[22,27].
The previous view of adult stem cells has been that the differentiation potential was strictly limited to cell lineages found within the tissue of origin studied in tissues such as skin and bone marrow. During the past few years, this view has changed. Several studies have shown apparent plasticity of adult stem cells, like the ability to differentiate to cell types other than the tissue of origin[9]. This remarkable finding challenged the long-held assumption that truly multipotent or pluripotent stem cells did not persist beyond early stages in embryogenesis.
Multipotent stem cells can be inserted in this context because they express markers of pluripotency previously seen only in ESCs or pregastrulation embryos[9]. The most commonly studied multipotent SCs in ophthalmopathies are MSCs. MSCs are classically the “post-natal, self-renewing and multipotent stem cells giving rise to all skeletal tissues”[2]. They have been found in different fetal tissues, in extraembryonic tissues [placenta, umbilical cord (UC) and amniotic fluid] and in adult tissues (bone marrow, peripheral blood, adipose tissue, dermis, synovium, periosteoum, cartilage, skeletal muscle, fallopian tubes, menstrual blood, gingiva and dental tissue and eye)[28]. Placental and adipose-derived MSCs are, by far, considered in the largest number of clinical trials.
Fetal MSCs are scarcely considered in reported studies probably due to the difficulties in achieving sufficient cell numbers after expansion[29].
UC-MSCs have excellent proliferation and differentiation properties. These cells are readily available in large quantities and cultured rapidly. Moreover, UC incorporates both mesenchymal and epithelial stem cells with anti-inflammatory and immune-privilege properties that can be differentiated into corneal epithelial, stromal and endothelial cells[29].
Human adipose-derived stem cells (ASCs) are an easily accessible autologous stem cell source. They have been shown to support the growth of many types of stem cells including human embryonic stem cells (hESCs), iPSCs and limbal stem cells (LSCs)[30]. ASCs resemble BMSCs in terms of morphology, proliferation and multipotency[31]. These cells have been considered for various ocular disorders, from retinal degeneration (neuroprotection and neurogenesis)[22,31] to corneal diseases[1,3,32].
Dental pulp stem cells (DPSCs) were the first human dental stem cells isolated from the dental pulp of permanent teeth[33]. These cells show the unique characteristic of the potential to differentiate into not only typical mesodermal cell lineages but also ectodermal and endodermal cell lineages. DPSCs have exhibited the potential to differentiate into active neurons, cardiomyocytes, myocytes, melanocytes and hepatocyte-like cells. These cells have shown higher angiogenic, neurogenic and regenerative potential when compared to BMSCs. In the field of ophthalmology, these cells have been studied for corneal repair[34], treatment of glaucoma and retinal diseases[35].
Going even more specifically, let us analyze the eye structure. Within the healthy eye, different types of adult stem cells can be found, which can be considered as eye stem cells. Retinal pigment epithelium stem cells (RPESCs) represent one of the latest discoveries in terms of stem cells of the eye. Retinal epithelium arises from the CNS neuro-epithelium. Interestingly, studies have shown how these cells can proliferate in some animal species and in certain conditions (e.g., injury). Salero et al[36] identified a subpopulation of RPE cells that can be activated to self-renew and that exhibit multipotentially, producing either stable RPE progeny or neural, osteo, chondro or adipo-lineage mesenchymal progeny[36]. Studies have demonstrated how RPESCs, to date unknown, can proliferate pathologically in specific conditions, giving rise to retinal disorders. RPESCs are considered as a new type of SC capable of producing both CNS and mesoderm-associated lineages[36]. Autologous RPE cell replacement has provided proof-of-concept evidence that cell therapy may have promising applications for retinal degenerative diseases. RPE cell source, however, is restricted for applications in RPE cell replacement due to the limited number of donor eyes and ethical issues concerning this type of treatment[37].
Hallmark features of the corneal epithelium include the high regenerative potential and the capacity for rapid ocular surface repair through proliferation and centripetal migration of progenitor cell populations residing at the border of the cornea and the sclera in a location called limbus. LSCs represent a quiescent cell population with high proliferative potential, which enables efficient corneal regeneration and repair[38]. LSCs are fundamental for corneal homeostasis. A loss or deficiency [LSC deficiency (LSCD)] of these cells causes the disruption of homeostasis[39]. LSCs can be collected using biopsy and expanded in culture, and then they can be transplanted in the diseased eye[1].
Criteria for selecting stem cells type: As explained above, stem cells for the treatment of ocular disorders can be obtained from the same eye (or fellow eye), from other tissues of the patient, or from a donor. As with all treatments, clinicians seek safe, widely available and economically viable therapies. Obtaining SCs from the patient’s own tissues have changed the therapeutic perspectives. This option has the advantage of not requiring immunosuppressive therapies and guarantees no immune reactions[40]. Another element that guides the choice of SCs is the availability of cells. Alternatives to pluripotent stem and eye tissue cells have been considered in literature, however, these options tend to be limiting due to ethical constraints, possible unknown adverse effects, little availability and unsustainable costs[21,37]. Autologous sources, such as MSCs (UC and adipose stem cells in particular), have been widely studied in recent years because of the large availability and the confirmed safety in other medical uses[3,4], and seem at the moment to preferential options for the future.
How can stem cells be used in clinical research
Multiple techniques to approach stem cell therapy for ophthalmic disorders have been described and studied over time.
Transplantation is the most used technique for stem cell therapy in the eye. SCs can be transplanted either as a cell suspension[40] or on different substrates, like autologous sheets of cells, biomaterial-based patches or three-dimensional (3D) structures[41,42]. SC transplantation is a technique substantially used in all eye structures. The key sites currently targeted include: The cornea, mainly the clear tissue covering the front of the eye that helps focus the incoming light; the neural retina, which contains the photoreceptors; and the RPE, a single layer of pigmented cells that plays a key role in maintaining the photoreceptor cells and the blood-retina barrier[15,41,42].
Stem cells injection (pluripotent, MSCs or hematopoietic stem cells)[27,40] is a procedure still under study today, considered especially for the treatment of AMD. To date, these therapies are not yet proven to be safe and effective in ophthalmic use, however, have shown to be widely validated in other body districts[43]. Several clinical experiments have proposed the injection of SCs into the intravitreal space (exploiting the paracrine effect of SCs) or in the subretinal space; however, results were not as expected, and several collateral effects have been reported in literature[44] that have partially “extinguished” the enthusiasm for results obtained in animal clinical trials.
Topical stem cells therapies (eye drops) have been extensively studied to treat ocular surface diseases. Hematopoietic stem cells from UC blood serum[45] have been proposed for topical treatment of ocular surface diseases. The rationale for applying serum to the ocular surface is that, compared to conventional lubricant treatments, it more closely resembles natural tears due to several of its biochemical constituents. It has produced satisfactory results in terms of efficacy and safety. Moreover, MSCs (in particular BMSCs[46] and ASCs[3]) have been used topically for dry eye syndrome or other corneal injuries or diseases with promising results. The rationale for MSCs eye drops is the wide-ranging differentiation potential, anti-inflammatory and immunomodulatory effects of MSCs[46-49].
In what ocular disorders can stem cells be used
Ocular surface, cornea and limbus: The ocular surface is the interface between the functioning eye and the environment. This surface provides anatomic, physiologic and immunologic protection and comprises the palpebral and bulbar conjunctival epithelium, the corneoscleral limbus, the corneal epithelium and the tear film[50]. The functions of ocular surface include maintaining optical clarity of the cornea and protection of the structures of the eye from microbes, trauma and toxins. Disorders of the ocular surface include a variety of conditions. The most common are dry-eye disease, blepharitis, ocular allergies and pterygia. Less common diseases are LSCD and ocular surface diseases due to systemic diseases. The narrow zone between cornea and bulbar conjunctiva is defined as limbus, which contains layers of cells populated by Langerhans cells, melanocytes and LSCs (the stem cells that generate corneal epithelium). If a patient has an extensive destruction of the limbus, a functional corneal epithelium can no longer be formed, and the cornea reacquires an epithelium by invasion of bulbar conjunctival cells. The only way to prevent the corneal conjunctivation is indeed to restore the limbus. Keratoplasty has been considered the conventional gold standard treatment before the introducing of regenerative medicine[51].
The first attempt to restore limbus, using free limbal tissue grafts from the uninjured eye, was published by Kenyon and Tseng in 1989[52]. The potential of limbus grafts promoted additional studies in this field, which brought the discovery of LSCs[38,53]. In 2006, Ma et al[54] showed how transplantation of human MSCs on amniotic membrane, like LSCs on amniotic membrane, could reconstruct severely damaged rat corneal surface. They demonstrated how the therapeutic effect did not come from epithelial differentiation of MSCs but was probably due to the inhibition of inflammation and neovascularization.
Since then, cultures of LSCs have been used to treat corneal diseases and injuries, initially engrafting the injured eye from the uninjured one[55], then treating bilateral pathologies with expanded cultures of LSCs[56]. The fragility and limited number of active SCs of the corneal epithelium in culture, in addition to the induction of iatrogenic damage to the healthy fellow eye, however, tend to slow-down and limit the clinical application of LSCs. For these reasons, several materials have been proposed to enhance results, which include fibrin glue, amniotic membrane, polymers, collagen sponges or strips and devitalized membrane or polymers[57].
LSCD is the most challenging disease of the ocular surface for ophthalmologists. Corneal LSC grafting procedures have been utilized. This procedure involves either direct transplantation of limbal tissue or transplantation of in vitro expanded cells on a variety of biological or synthetic carrier materials[29]. These techniques include conjunctival limbal autograft, living-related conjunctival allograft[57], keratolimbal allograft[58], autologous ex vivo cultivated limbal epithelial transplantation[59], simple limbal epithelial transplantation[60], cultivated oral mucosal epithelial transplantation[61] and transplantation of peripheral corneal cells[62]. Clinical studies using conjunctival limbal autografts have shown excellent short-term and good long-term results, however, with high risks of complications, which mainly include induced damage to the donor eye[63]. For these reason, other types of stem cells have been proposed to produce LSCs and corneal epithelium cells.
In 2012, an efficient protocol, with positive preliminary results, was proposed to produce corneal epithelial cells from human-iPSCs (hiPSCs)\ESCs obtained from hair follicles or dermal fibroblasts[64]. Results were also then confirmed in successive studies[65,66]. The evolution of this approach led to the creation of corneal organoids from iPSCs[23], initially in two-dimensional, and then in 3D culture systems, with promising results as alternative for the treatment of bilateral LSCD[67].
MSCs have also been considered for ocular surface therapy[3,55]. Preliminary results in animal experiments are encouraging, and the potential is great. Studies have shown how bone marrow-MSCs (BM-MSCs) are safe and can restore corneal epithelia from LSCD with the same results of cultivated limbal epithelial transplantation[68]. BM-MSC associated with amniotic membranes have successfully been evaluated in LSD[69]. Gu et al[70] demonstrated how BM-MSCs could differentiate into cornel epithelial like cells in vivo in rat damaged corneas[70]. MSCs have been proposed also to promote graft survival[71,72]. This can be explained by the potent immunomodulatory properties of SC, suppressing maturation and activation of atrial premature complexes and dendritic cells and cytotoxicity of natural killer cells. Several studies have attempted to exploit these features of MSCs and have shown interesting results by using topical therapies with eye drops containing MSCs (mainly BM-MSC and ASCs)[45,46]. Topical application of MSCs can lead to an increase in aqueous tear volume and improvement in ocular surface evaluation tests. Moreover, it is a safe and easy applicable method.
Cells derived from epithelial UC-MSCs are capable of forming a stratified epithelial layer when seeded on artificial matrices. Reza et al[73] first described the properties of UC-MSCs, finding how they have similar characteristics of LSCs[73]. Garzón et al[74] utilized an epidermal growth factor enriched medium to induce UC-MSCs to transdifferentiate into corneal epithelial cells on a 3D human artificial anterior cornea model[74]. The aim of the use of UC-MSCs derived epithelial cells is to circumvent the problem of the limited amount of limbal tissue available for transplantation, especially in cases of bilateral LSCD[29].
With regards to MSCs, human immature dental pulp and oral mucosa stem cells have been reported to be a promising cell source to correct LSCD, as described by Hassan and AbdelAziz[75] and Nishida et al[76]. Studies about ocular surface diseases and their treatment are reported in Table 1.
Research is currently searching for new ways of applications of stem cells therapy. As described above, MSCs derived exosomes is one of these[28]. The other way recently described to facilitate and carry cells to the ocular surface is the use of contact lenses[77].
Corneal stroma and endothelium: The corneal stroma is the thickest corneal layer (approximately 90% of corneal thickness) and is composed of specialized extracellular matrix components and collagen fibrils. Corneal stromal keratinocytes (CSKs) are the major cell type in corneal stroma and are located between the collagenous lamellae, which are generally quiescent[29]. Corneal insults cause death of CSKs at the injured site. Surviving CSKs near the injured site are activated to proliferate, while some fibroblasts are induced to transform in highly contractile myofibroblasts. When fibroblasts action prevails, scaring and consequent opacity of cornea can occur. The presence of dense opacities and persisting scars can interfere with the passage of light and cause an important loss of visual acuity if the opacity is large and localized in the center of the visual axis of the cornea, thus have an important burden on quality of life of patients[78].
Keratoplasty is a primary treatment option and current gold standard to treat numerous corneal conditions, including corneal injury, corneal dystrophy, keratoconus and corneal infractions. The ever-increasing number of patients needing keratoplasty has led to the shortfall of viable donor corneas. Moreover, it is important to note that post-surgical complications include important and sight threatening conditions, in addition to the risks of transplant rejections and elevated permanently induced astigmatism[23]. Sepsakos et al[79] demonstrated that patients who underwent an ocular surface SCs transplantation (e.g., with LSCs) before keratoplasty have better results than patients that did not do that[79].
Various trials (Table 1) trying to obtain keratinocytes derived from hiPSCs have been proposed in the past several years[80,81]; however, the genetic reprogramming of iPSCs tends to be quite intricate. The differentiation of iPSCs to keratinocytes involves two steps[81]. The possibility of obtaining CSKs from iPSCs is very interesting in animal models; to date, clinical studies involving injection in humans are lacking in literature[82].
MSCs express high levels of hepatocyte growth factor (HGF) in an inflamed environment, as is the case in an injured cornea. HGF inhibits the generation of opacity-inducing myofibroblasts and, alone, can restore corneal transparency in an in vivo model of eye injury[83]. This is the rationale that has been proposed for the use of these cells. All MSCs seem to have similar behavior in vivo, being able to achieve keratocyte differentiation and modulate the corneal stroma. ASCs have been demonstrated to be an ideal source of autologous stem cells, while BM-MSCs have the same profile, but the extraction by bone marrow puncture is more complicated, not free of risks and painful. A pilot study by del Barrio et al[84] demonstrated the apparent safety of corneal stromal transplantation of autologous ASCs in humans, showing cell survival in vivo and the ability of these cells to produce a low amount of new collagen in patients with advanced keratoconus. Several studies on animals have suggested that UC-MSC transplantation may be a feasible alternative to keratoplasty in treating congenital disorders of the cornea secondary to keratocyte dysfunction such as mucopolysaccharidoses, giving rise to potential future possibilities[85,86]. UC-MSCs could represent an attractive alternative, but the autologous use of these cells tends to be expensive and currently almost impossible.
An alternative stem cell population currently reported in clinical trials for the therapy of corneal stroma disorders include corneal stromal stem cells (CSSCs). These cells show similar properties of MSCs and can be obtained by specific cultures of LSCs. Experimental studies have shown that CSSCs can differentiate in CSKs after injection in the stroma[87].
Periodontal ligament stem cells and DPSCs could differentiate in CSKs and prove to be of potential clinical use[28,88].
The corneal endothelium is the posterior corneal surface. It is formed by a monolayer of endothelial cells (CECs) that regulate the stromal hydration, preventing edema and maintaining corneal deturgescence, which are all fundamental for normal vision. These cells are non-mitotic and have limited regenerative capacity. Diseases that affect the corneal endothelium cause stromal edema, central opacity and vision loss. Full thickness or partial corneal transplantation has been the gold standard for endothelial diseases to date; however, preliminary studies have shown that stem cells therapies could be of potential clinical use[28,29]. MSCs could serve as a potential source to generate corneal endothelial cells for the treatment of corneal endothelial diseases, like Fuchs’ endothelial dystrophy and aphakic/pseudophakic bullous keratopathy. Joyce et al[89] demonstrated the potential of UC-MSCs to differentiate in CECs when treated in particular cultures[89]. At this moment, however, there are no concrete data in current literature on the possible application of SCs in human endothelial disorders, which remains to be the primary cause of corneal transplantation[29].
Trabecular meshwork: Glaucoma is a degenerative optic neuropathy affecting approximately 70 million people worldwide. The most frequent cause of glaucoma is the increase of intraocular pressure (IOP) due to an alteration of aqueous outflow. Humor aqueous is continuously produced, and its outflow is controlled by the trabecular meshwork (TM), an avascular tissue located within the uvea and posterior to the corneal margin[90]. TM is populated by specialized cells that decline in number with age, and these cells are particularly low in individuals with primary open glaucoma. It is probable that TM cells become dysfunctional prior to death and increasingly fail to carry out the physiological roles, leading to enhanced aqueous humor outflow resistance and the development of pathologically elevated IOP[91]. Despite the importance of controlling IOP, the ultimate cause of glaucoma-associated vision loss includes axonal damage and the progressive loss of RGCs, the axons of retinal neurons that make up the optic nerve and transmit visual information from the eye to the brain[91]. The presence of MSCs in TM have been suspected for years and then confirmed and propagated in vitro[92].
TM cells are difficult to obtain from a living eye. Studies have faced this problem by using iPSCs generated via genetic reprogramming of adult somatic cells[19]. To date, the use of TM-like cells derived from iPSCs from a patient’s own dermal fibroblasts may offer the best solution to the challenge of TM cell replacement therapy[92]. Abu-Hassan et al[93] evaluated the results of iPSCs derived TM cell transplantation. The study showed that iPSCs differentiate to resemble TM cells in several keyways and have the potential to restore the primary TM cell function, thus maintaining IOP homeostasis[93].
Recently, other stem cells have been proposed to find the possibility of obtaining TM cells (Table 1). MSCs have been used in attempt to repair TM tissue predominantly in animals[94]. Kumar et al[31] described the differentiation of ASCs in TM cells[31], and Manuguerra-Gagné et al[95] studied the regeneration of TM from BM-MSCs with encouraging results[95]. Data in stem cell models are of utmost importance and the basis when designing future studies with potential clinical benefits.
Lens: Cataracts are the leading cause of blindness in the world. The current standard of care in congenital cataracts involves surgical removal of the cataractous lens and implantation of an artificial intraocular lens. Surgery is not free of complications, especially in patients with complicated cataracts and with other underlying ophthalmic conditions.
Human lens regeneration has not been demonstrated yet, however, lens epithelial stem\progenitor cells (LECs) have been isolated[96]. The most significant functions of LECs are sustained self-renewal and protective capacities against external injuries[97,98]. Li et al[99] have recently reported clinical trials on animals and humans (Table 1). They showed that with a new minimally invasive surgical procedure, with preservation of LECs, lens regeneration can be achieved with increased visual axis transparency and decreased rate of complications. The same conclusion has also been reported by Li et al[99]. A further possibility of obtaining lenses through cell differentiation has been proposed by Murphy et al[98], who showed the possibility of creating micro-lenses starting from iPSC differentiation.
Optic nerve
RGCs are a population of CNS neurons located in the innermost layer of the retina and convey visual signals from the retina along their axons to the brain. Axonal injury leads to the functional loss of RGCs and subsequently induces death of neurons. Axon growth is essential for the restoration of neuronal connectivity and reestablishment of a functional visual system after optic nerve injury[100]. Some optic neuropathies are very common, like glaucoma that is the first cause of irreversible blindness; while other conditions tend to be rare. Leber’s hereditary optic neuropathy is just one example of this heterogeneous category of ophthalmic pathologies. There is currently no treatment available for inherited optic neuropathies such as Leber’s hereditary optic neuropathy or dominant optic atrophy. With regards to glaucoma, current treatments aim at lowering the IOP. It is well known how the regenerative potential of the mammalian CNS is very limited. Research regarding the regeneration of elements of the nervous system is thus fascinating and usually limited to animal models.
There are two main objectives of cell therapy, including the delivery of a trophic and neuroprotective support[22,27] and (more ambitious) replacement of lost cells and functional restoration[101]. The first step in developing cell replacement-based strategies for optic nerve regeneration requires a reliable, high-volume source of healthy RGCs[102].
iPSCs\ESCs represent the first source studied for the optical nerve regeneration. Takahashi et al[19] in 2007 reported a remarkable break-through technology whereby adult fibroblasts could be reprogrammed into iPSCs. These transdifferentiated cells exhibit similar characteristics to hESCs, including the ability to propagate indefinitely and the ability to differentiate into many different cell types, including RGCs. As explained by Gokoffski et al[100], there are two different methods for generating RGSs from pluripotent stem cells: Organoid differentiation and planar differentiation. Organoids are self-organized 3D miniature organs developed in vitro from PSCs. Kuwahara et al[102] first developed 3D retinal organoids from hESCs[102]. Planar-derived RGCs are transdifferentiated from traditional two-dimensional cell culture techniques[103,104]. One of the limitations of this technique is the ability of iPSCs\ESCs to integrate into the ganglion cell layer. Preliminary results by Mesentier-Louro et al[105] reported that between 1% to 7% of iPSCs-derived RGCs integrated into the ganglion cell layer after intravitreal injection and about 20% after combined injection of RGCs and iPSCs[105] (Table 1).
The other limitation regarding the use of iPSCs currently being studied involves the possibility of formation of synaptic connections. Axonogenesis of derived RGCs is another crucial point: Neurotrophic factors, which theoretically could promote it, keep RGCs alive longer. The ideal local cellular environment is essential to permit and enhance RGCs in creating new axons; however, neuronal survival does not equate to new axon formation[106]. An additional unresolved question involves the possibility of new axons in establishing functional synapse.
To overcome the difficulties in integrating RGCs, gene therapy has developed possible solutions, which are currently under investigation. Zhang et al[107] demonstrated the utility of pigment epithelium-derived factor[107]. It is constitutively expressed by various ocular tissues, but its exogenous delivery is therapeutically advantageous to promote RGCs survival and axon regeneration. Zhang et al[107] used NSCs as cellular vectors to deliver continuously pigment epithelium-derived factor to adult retinas after optic nerve injury. These studies showed the utility of genetically modified NSCs to protect RGCs and promote axonal regeneration.
The effects of MSCs on RGCs have also been studied (mainly in animals). MSCs provide neuroprotection against RGC death; however, studies showed that these SCs did not tend to integrate[14]. Preliminary studies by Zhang et al[107] have described the possible usefulness of UC-MSCs, which have shown a partial recovery of injured optic nerve.
Retina: Visual signalling starts in photoreceptor cells. In the human retina, rods and cones are responsible for dim light vision and daylight vision, respectively. Rods are located mainly in the peripheral retina, while cones are concentrated in a small portion of the retina, called macula. Bipolar cells receive visual signals from photoreceptors and transmit it to RGCs. RPE cells form a monolayer underneath the outer segment of the photoreceptors, constituting the outer blood-retinal barrier. In the visual system, RPE cells play diverse roles, which include absorption of scattered light, regulation of nutrients, ions and solutes, secretion of growth factors, regulation of the retinal cycle and phagocytosis of photoreceptor outer segment.
Retinal degenerative diseases are characterized by retinal cell loss, such as RPE and/or photoreceptor cell loss in AMD and retinitis pigmentosa, and RGC death in glaucoma, as seen previously. Studies that report retinal diseases and treatment are summarized in Table 2.
Binder et al[108] and van Meurs et al[109] described the therapeutic potential of autologous RPE cells taken from the peripheral region of the retina in AMD. These promising results have prompted research towards stem cell therapies to extend it to degenerative retinal diseases, where cell replacement is needed[37]. Retinal degenerative disorders requiring cell replacement include AMD, retinitis pigmentosa, Stargardt’s disease and glaucoma, which represent current challenges in cell therapy. RPE cell source is restricted for applications in RPE cell replacement, thus stem cells have been studied to solve this limitation.
The greatest potential for cell replacement has been seen with ESC/iPSCs[19], which can be successfully pre-differentiated prior to transplantation in the eye, with the greatest success shown in RPE/photoreceptor replacement for AMD[22]. Studies involving cell reprogramming by Tucker et al[110] and Lamba et al[111] have shown the possibility of creating ESC/iPSC-derived retinal progenitors capable of maturing in RPE or photoreceptors and capable of integrating in the retina[112]. The same results, but with hESCs and hiPSCs, were confirmed by Nakano et al[48] and Gonzalez-Cordero et al[113]. The first clinical trials in humans have been done by Schwartz et al[40,114] in 2012 and 2015[40,114]: They successfully used hESCs-derived RPE cells in Stargardt’s disease without collateral effects (also noted by Mandai et al[17]). Cell reprogramming allows the use of autologous PSCs, which guarantee no immune reactions with respect to allogenic cells. One of the observed collateral effects is the long-term hyperpigmentation of the macula[114]. Potential future alternative approaches include the implant of stem cell derived RPE growing on a bioengineered scaffold, which can improve stability and maintain cell polarization[14].
Considering the functions of RPE on the overlying retina, it is fundamental to know that subretinal RPE transplantation aims at replacing these functions. Transplantation of non-RPE cells has been pursued with the rationale that they may counter disease through trophic factor secretion. For this reason, clinical trials with subretinal UC-MSCs, NSCs and retinal progenitor cells are based on trophic support mechanism of action. These procedures, however, need further studies considering the potential increase of complications[115].
The future of retinal therapies could involve bioengineering. Stern et al[14] have reported that incorporating bioengineering approaches may better preserve retinal layering and integration in vivo models. The possibilities of this approach have been successfully seen in animal clinical trials[116]. Nakano et al[48] has described the formation of optic cup and stratified retina from hPSCs. Several successive studies have confirmed the possibility of creating retinal organoids and layers of differentiated photoreceptors, which can develop outer segment structures[117]. Organoids may prove valuable in producing specific retinal cell types or 3D retinal structures for transplantation. This is particularly important for conditions such as geographic atrophy[14].
An alternative approach to retinal degenerative pathologies with SCs is the possibility of exploiting the paracrine capacities of some type of cells. This stem cell therapy is not disease specific and can have broad clinical applications, as seen previously. This is the potential of BM-MSCs and places them as a candidate cellular therapy to combat ocular neurodegeneration, even if these cells are less ideal for replacement cell therapy[22,27]. Transplantation of BM-MSCs in experimentally induced glaucoma and optic nerve transection show no evidence of the differentiation into mature retinal cells (RPE or photoreceptors), despite some integration into the retina; but, improvement of retinal function by preserving photoreceptors and RPE cell viability have described[118].
ASCs have also been studied for this clinical use, which could prove to be beneficial in eye therapies for the paracrine effects, as seen for disorders of the SNC. Several studies suggest that ASCs have therapeutic potential for neurodegenerative conditions through neurotrophic factor production, with several of the active factors being different from those produced by BM-MSCs and DPSCs[27,119]. ASCs and BM-MSCs have recently been evaluated with promising results in diabetic retinopathy. ASCs have shown the potential to be therapeutically effective in early-stage of diabetic retinopathy through paracrine factors and physical contact with endothelial cells[120].
Limits and why not
Stem cell therapy in ocular diseases certainly represents the future in the treatment of numerous serious eye diseases, especially if organ transplantation can be avoided. One of the main problems of these therapies, mainly the immunological tolerance to transplanted cells, has been solved thanks to the use of autologous cells[17]. Graft vs host disease has been limited in this way. Despite all the advantages and promising results, what we know about stem cells therapies is still incomplete, especially concerning the possible side effects. The tumorigenicity of transplanted stem cells, to date, remains to be the most concerning issue for cell transplantation. Advances in genetic research and reprogramming have made it possible to reduce the incidence of this event[20]. Other side effects may be caused by tissue sampling, particularly if performed in the contralateral, healthy eye. This can be avoided using SCs derived from other tissues, like ASCs[32].
Stem cell transplantation has the huge limit of the survival and engraftment of cells. To improve outcomes, methods considered include pre-treating the host tissue or the SCs culture with growth factors or cytokines, embedding SCs in biomaterials or expanding SCs in culture. Obtaining an adequate number of SCs is fundamental. For example, the expansion of ASCs in culture has been considered, but extensive cultures may change the properties of SCs in vivo, rendering them unfit for restoring injured or diseased tissues. Genetic research is thus of fundamental importance in this field. A further problem related to SCs treatment is the cost of this type of therapy, which is still very high today due to limited cost efficient technology to render this therapy available on a large scale[37]. Conserving samples of one’s own tissue (i.e. adipose stem cells, which are the most represented) taken during other operations, similar to the methods used during lipofilling for aesthetic or reconstructive aims, could be a possible solution. Moreover, the ethical problem of the use and collection of certain cell types, such as ESCs, UC-MSCs and NSCs, remains considerable, which further limits SCs use in clinical trials.
Future prospectives
The vast literature and resources used to date underline the importance of stem cell therapies, especially for the future. To date, the results are still primordial, but the conditions seem leading to an important turning point. Further studies are surely needed to provide additional knowledge behind the mysterious physiological and potentially curative properties of stem cells, which can pave the way to clinical applications in ophthalmic care. Numerous current trials have been proposing different perspectives for the future of cell therapy in ophthalmic diseases. The therapeutic effects of MSCs in regenerative medicine, for example, can also be attributed to exosomes, which are secreted soluble factors[45]. Exosomes are extracellular vesicles that are produced in the endosomal compartment of most eukaryotic cells and contain proteins that regulate tissues biogenesis. Several studies have considered the injection of MSCs exosomes in ocular tissues, with interesting results[28]. Research should not only be limited at stem cell studies alone but also need to include a whole series of innovations brought on by bioengineering and nanotechnology[14,48,118]. Modern studies seem to be aimed at the 3D development of fundamental parts of the eye, the use of specific vectors that can guarantee the replacing of tissues, and organoids[67]. Novel studies are geared at the possibility of reproducing eye tissues in a normal 3D configuration. Transplantation of sophisticated multicellular 3D tissues can be an exciting opportunity. Nakano et al[48] have shown that hPSCs can generate differentiated 3D structures similar to the embryonic eye cup, containing RPE and neural retina. Garzón et al[74] described the generation of the anterior cornea by tissue engineering. In addition, bioengineers have proposed to build ocular structures by incorporating biocompatible materials with stem cells products, for example to create TM or RPE monolayer[47]. Bioengineering is fundamental for the development of optimal cell culture biomaterials for the expansion of SCs and the differentiation into ocular cells[16]. Modified cultures (e.g., using growth factors, biomaterials, injectable hydrogels, scaffolds or membranes containing cells) allow the maturation of cells and dedifferentiation, recreating the micro-environment of the host tissue. Consequently, there is an easier integration and a better survival of these SCs in the recipient site[42]. The advantage of these approaches is to guarantee a reduction of the culture time to obtain a viable ocular tissue (such as a cornea[75]), thus avoiding massive tissue harvesting (preserving LSCs, for example[75]).
CONCLUSION
The potential therapeutic goals include being able to restore the sense of sight in patients who have lost it, by replacing or recreating the damaged eye structures, including restoration of physiological and functional connections with the CNS. Stem cell therapies seem to be interesting and promising, even concerning the more external structures, including the ocular surface and cornea. Finally, the possibility of using these cells topically, without having to subject patients to surgery, organ transplantation or hospitalization, is an element of great importance and hope.
Footnotes
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Manuscript source: Invited manuscript
Peer-review started: January 22, 2021
First decision: February 28, 2021
Article in press: April 26, 2021
Specialty type: Cell and tissue engineering
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Feng MJ, Luo W, Sun SY S-Editor: Fan JR L-Editor: Filipodia P-Editor: Xing YX
Contributor Information
Giovanni Miotti, Department of Plastic Surgery, University Hospital of Udine, Udine 33100, Italy.
Pier Camillo Parodi, Department of Plastic Surgery, University Hospital of Udine, Udine 33100, Italy.
Marco Zeppieri, Department of Ophthalmology, University Hospital of Udine, Udine 33100, Italy. markzeppieri@hotmail.com.
References
- 1.Gurusamy N, Alsayari A, Rajasingh S, Rajasingh J. Adult Stem Cells for Regenerative Therapy. Prog Mol Biol Transl Sci. 2018;160:1–22. doi: 10.1016/bs.pmbts.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 2.Trounson A, McDonald C. Stem Cell Therapies in Clinical Trials: Progress and Challenges. Cell Stem Cell. 2015;17:11–22. doi: 10.1016/j.stem.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Zeppieri M, Salvetat ML, Beltrami A, Cesselli D, Russo R, Alcalde I, Merayo-Lloves J, Brusini P, Parodi PC. Adipose Derived Stem Cells for Corneal Wound Healing after Laser Induced Corneal Lesions in Mice. J Clin Med. 2017;6 doi: 10.3390/jcm6120115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gimble JM, Guilak F, Bunnell BA. Clinical and preclinical translation of cell-based therapies using adipose tissue-derived cells. Stem Cell Res Ther. 2010;1:19. doi: 10.1186/scrt19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Müller P, Beltrami AP, Cesselli D, Pfeiffer P, Kazakov A, Böhm M. Myocardial regeneration by endogenous adult progenitor cells. J Mol Cell Cardiol. 2005;39:377–387. doi: 10.1016/j.yjmcc.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Paliwal S, Chaudhuri R, Agrawal A, Mohanty S. Regenerative abilities of mesenchymal stem cells through mitochondrial transfer. J Biomed Sci. 2018;25:31. doi: 10.1186/s12929-018-0429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Society of Plastic Surgeons. Evidence-based clinical practice guidelines (2011). [cited 3 January 2021]. Available from: https://www.plasticsurgery.org/Medical_Professionals/Health_Policy_and_Advocacy/Health_Policy_Resources/Evidencebased_GuidelinesPractice_Parameters/Description_and_Development_of_Evidence-based_Practice_Guidelines/ASPS_Grade_Recommendation_Scale.html .
- 8.Kolios G, Moodley Y. Introduction to stem cells and regenerative medicine. Respiration. 2013;85:3–10. doi: 10.1159/000345615. [DOI] [PubMed] [Google Scholar]
- 9.Vats A, Bielby RC, Tolley NS, Nerem R, Polak JM. Stem cells. Lancet. 2005;366:592–602. doi: 10.1016/S0140-6736(05)66879-1. [DOI] [PubMed] [Google Scholar]
- 10.He S, Nakada D, Morrison SJ. Mechanisms of stem cell self-renewal. Annu Rev Cell Dev Biol. 2009;25:377–406. doi: 10.1146/annurev.cellbio.042308.113248. [DOI] [PubMed] [Google Scholar]
- 11.Angelini A, Castellani C, Vescovo G, Thiene G. Pathological evidence of stem cell regeneration in the heart. Int J Cardiol. 2004;96:499–504. doi: 10.1016/j.ijcard.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Lodi D, Iannitti T, Palmieri B. Stem cells in clinical practice: applications and warnings. J Exp Clin Cancer Res. 2011;30:9. doi: 10.1186/1756-9966-30-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graw J. Eye development. Curr Top Dev Biol. 2010;90:343–386. doi: 10.1016/S0070-2153(10)90010-0. [DOI] [PubMed] [Google Scholar]
- 14.Stern JH, Tian Y, Funderburgh J, Pellegrini G, Zhang K, Goldberg JL, Ali RR, Young M, Xie Y, Temple S. Regenerating Eye Tissues to Preserve and Restore Vision. Cell Stem Cell. 2018;22:834–849. doi: 10.1016/j.stem.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blenkinsop TA, Corneo B, Temple S, Stern JH. Ophthalmologic stem cell transplantation therapies. Regen Med. 2012;7:32–39. doi: 10.2217/rme.12.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higuchi A, Kumar SS, Benelli G, Alarfaj AA, Munusamy MA, Umezawa A, Murugan K. Stem Cell Therapies for Reversing Vision Loss. Trends Biotechnol. 2017;35:1102–1117. doi: 10.1016/j.tibtech.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 17.Mandai M, Watanabe A, Kurimoto Y, Hirami Y, Morinaga C, Daimon T, Fujihara M, Akimaru H, Sakai N, Shibata Y, Terada M, Nomiya Y, Tanishima S, Nakamura M, Kamao H, Sugita S, Onishi A, Ito T, Fujita K, Kawamata S, Go MJ, Shinohara C, Hata KI, Sawada M, Yamamoto M, Ohta S, Ohara Y, Yoshida K, Kuwahara J, Kitano Y, Amano N, Umekage M, Kitaoka F, Tanaka A, Okada C, Takasu N, Ogawa S, Yamanaka S, Takahashi M. Autologous Induced Stem-Cell-Derived Retinal Cells for Macular Degeneration. N Engl J Med. 2017;376:1038–1046. doi: 10.1056/NEJMoa1608368. [DOI] [PubMed] [Google Scholar]
- 18.Byrne LC. What's old is new again: Autologous stem cell transplant for AMD. Sci Transl Med. 2017;9 doi: 10.1126/scitranslmed.aan2783. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 20.Robinton DA, Daley GQ. The promise of induced pluripotent stem cells in research and therapy. Nature. 2012;481:295–305. doi: 10.1038/nature10761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yoshihara M, Hayashizaki Y, Murakawa Y. Genomic Instability of iPSCs: Challenges Towards Their Clinical Applications. Stem Cell Rev Rep. 2017;13:7–16. doi: 10.1007/s12015-016-9680-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mead B, Berry M, Logan A, Scott RA, Leadbeater W, Scheven BA. Stem cell treatment of degenerative eye disease. Stem Cell Res. 2015;14:243–257. doi: 10.1016/j.scr.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chakrabarty K, Shetty R, Ghosh A. Corneal cell therapy: with iPSCs, it is no more a far-sight. Stem Cell Res Ther. 2018;9:287. doi: 10.1186/s13287-018-1036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lu P, Wang Y, Graham L, McHale K, Gao M, Wu D, Brock J, Blesch A, Rosenzweig ES, Havton LA, Zheng B, Conner JM, Marsala M, Tuszynski MH. Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell. 2012;150:1264–1273. doi: 10.1016/j.cell.2012.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuenca N, Fernández-Sánchez L, McGill TJ, Lu B, Wang S, Lund R, Huhn S, Capela A. Phagocytosis of photoreceptor outer segments by transplanted human neural stem cells as a neuroprotective mechanism in retinal degeneration. Invest Ophthalmol Vis Sci. 2013;54:6745–6756. doi: 10.1167/iovs.13-12860. [DOI] [PubMed] [Google Scholar]
- 26.Yang YJ, Li XL, Xue Y, Zhang CX, Wang Y, Hu X, Dai Q. Bone marrow cells differentiation into organ cells using stem cell therapy. Eur Rev Med Pharmacol Sci. 2016;20:2899–2907. [PubMed] [Google Scholar]
- 27.Park SS, Moisseiev E, Bauer G, Anderson JD, Grant MB, Zam A, Zawadzki RJ, Werner JS, Nolta JA. Advances in bone marrow stem cell therapy for retinal dysfunction. Prog Retin Eye Res. 2017;56:148–165. doi: 10.1016/j.preteyeres.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mansoor H, Ong HS, Riau AK, Stanzel TP, Mehta JS, Yam GH. Current Trends and Future Perspective of Mesenchymal Stem Cells and Exosomes in Corneal Diseases. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20122853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ziaei M, Zhang J, Patel DV, McGhee CNJ. Umbilical cord stem cells in the treatment of corneal disease. Surv Ophthalmol. 2017;62:803–815. doi: 10.1016/j.survophthal.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 30.Mei H, González S, Nakatsu MN, Baclagon ER, Chen FV, Deng SX. Human adipose-derived stem cells support the growth of limbal stem/progenitor cells. PLoS One. 2017;12:e0186238. doi: 10.1371/journal.pone.0186238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar A, Xu Y, Yang E, Wang Y, Du Y. Fidelity of long-term cryopreserved adipose-derived stem cells for differentiation into cells of ocular and other lineages. Exp Eye Res. 2019;189:107860. doi: 10.1016/j.exer.2019.107860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zeppieri M, Salvetat ML, Beltrami AP, Cesselli D, Bergamin N, Russo R, Cavaliere F, Varano GP, Alcalde I, Merayo J, Brusini P, Beltrami CA, Parodi PC. Human adipose-derived stem cells for the treatment of chemically burned rat cornea: preliminary results. Curr Eye Res. 2013;38:451–463. doi: 10.3109/02713683.2012.763100. [DOI] [PubMed] [Google Scholar]
- 33.Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci USA. 2000;97:13625–13630. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Syed-Picard FN, Du Y, Lathrop KL, Mann MM, Funderburgh ML, Funderburgh JL. Dental pulp stem cells: a new cellular resource for corneal stromal regeneration. Stem Cells Transl Med. 2015;4:276–285. doi: 10.5966/sctm.2014-0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roozafzoon R, Lashay A, Vasei M, Ai J, Khoshzaban A, Keshel SH, Barabadi Z, Bahrami H. Dental pulp stem cells differentiation into retinal ganglion-like cells in a three dimensional network. Biochem Biophys Res Commun. 2015;457:154–160. doi: 10.1016/j.bbrc.2014.12.069. [DOI] [PubMed] [Google Scholar]
- 36.Salero E, Blenkinsop TA, Corneo B, Harris A, Rabin D, Stern JH, Temple S. Adult human RPE can be activated into a multipotent stem cell that produces mesenchymal derivatives. Cell Stem Cell. 2012;10:88–95. doi: 10.1016/j.stem.2011.11.018. [DOI] [PubMed] [Google Scholar]
- 37.Jin ZB, Gao ML, Deng WL, Wu KC, Sugita S, Mandai M, Takahashi M. Stemming retinal regeneration with pluripotent stem cells. Prog Retin Eye Res. 2019;69:38–56. doi: 10.1016/j.preteyeres.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 38.Schermer A, Galvin S, Sun TT. Differentiation-related expression of a major 64K corneal keratin in vivo and in culture suggests limbal location of corneal epithelial stem cells. J Cell Biol. 1986;103:49–62. doi: 10.1083/jcb.103.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen JJ, Tseng SC. Corneal epithelial wound healing in partial limbal deficiency. Invest Ophthalmol Vis Sci. 1990;31:1301–1314. [PubMed] [Google Scholar]
- 40.Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, Hubschman JP, Davis JL, Heilwell G, Spirn M, Maguire J, Gay R, Bateman J, Ostrick RM, Morris D, Vincent M, Anglade E, Del Priore LV, Lanza R. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt's macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–516. doi: 10.1016/S0140-6736(14)61376-3. [DOI] [PubMed] [Google Scholar]
- 41.Cuevas E, Parmar P, Sowden JC. Restoring Vision Using Stem Cells and Transplantation. Adv Exp Med Biol. 2019;1185:563–567. doi: 10.1007/978-3-030-27378-1_92. [DOI] [PubMed] [Google Scholar]
- 42.Zhong X, Gutierrez C, Xue T, Hampton C, Vergara MN, Cao LH, Peters A, Park TS, Zambidis ET, Meyer JS, Gamm DM, Yau KW, Canto-Soler MV. Generation of three-dimensional retinal tissue with functional photoreceptors from human iPSCs. Nat Commun. 2014;5:4047. doi: 10.1038/ncomms5047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bremond-Gignac D, Copin H, Benkhalifa M. Corneal epithelial stem cells for corneal injury. Expert Opin Biol Ther. 2018;18:997–1003. doi: 10.1080/14712598.2018.1508443. [DOI] [PubMed] [Google Scholar]
- 44.Kuriyan AE, Albini TA, Townsend JH, Rodriguez M, Pandya HK, Leonard RE 2nd, Parrott MB, Rosenfeld PJ, Flynn HW Jr, Goldberg JL. Vision Loss after Intravitreal Injection of Autologous "Stem Cells" for AMD. N Engl J Med. 2017;376:1047–1053. doi: 10.1056/NEJMoa1609583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yoon KC, Heo H, Im SK, You IC, Kim YH, Park YG. Comparison of autologous serum and umbilical cord serum eye drops for dry eye syndrome. Am J Ophthalmol. 2007;144:86–92. doi: 10.1016/j.ajo.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 46.Beyazyıldız E, Pınarlı FA, Beyazyıldız O, Hekimoğlu ER, Acar U, Demir MN, Albayrak A, Kaymaz F, Sobacı G, Delibaşı T. Efficacy of topical mesenchymal stem cell therapy in the treatment of experimental dry eye syndrome model. Stem Cells Int. 2014;2014:250230. doi: 10.1155/2014/250230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Burrello J, Monticone S, Gai C, Gomez Y, Kholia S, Camussi G. Stem Cell-Derived Extracellular Vesicles and Immune-Modulation. Front Cell Dev Biol. 2016;4:83. doi: 10.3389/fcell.2016.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nakano T, Ando S, Takata N, Kawada M, Muguruma K, Sekiguchi K, Saito K, Yonemura S, Eiraku M, Sasai Y. Self-formation of optic cups and storable stratified neural retina from human ESCs. Cell Stem Cell. 2012;10:771–785. doi: 10.1016/j.stem.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 49.Hynes SR, Lavik EB. A tissue-engineered approach towards retinal repair: scaffolds for cell transplantation to the subretinal space. Graefes Arch Clin Exp Ophthalmol. 2010;248:763–778. doi: 10.1007/s00417-009-1263-7. [DOI] [PubMed] [Google Scholar]
- 50.Lee WB, Mannis MJ. Historical Concepts of Ocular Surface Disease. Cornea, Conjunctiva and Tear Film 2013; 3-10. [Google Scholar]
- 51.Oie Y, Nishida K. Regenerative medicine for the cornea. Biomed Res Int. 2013;2013:428247. doi: 10.1155/2013/428247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709–22; discussion 722. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- 53.Lindberg K, Brown ME, Chaves HV, Kenyon KR, Rheinwald JG. In vitro propagation of human ocular surface epithelial cells for transplantation. Invest Ophthalmol Vis Sci. 1993;34:2672–2679. [PubMed] [Google Scholar]
- 54.Ma Y, Xu Y, Xiao Z, Yang W, Zhang C, Song E, Du Y, Li L. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24:315–321. doi: 10.1634/stemcells.2005-0046. [DOI] [PubMed] [Google Scholar]
- 55.Pellegrini G, Traverso CE, Franzi AT, Zingirian M, Cancedda R, De Luca M. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet. 1997;349:990–993. doi: 10.1016/S0140-6736(96)11188-0. [DOI] [PubMed] [Google Scholar]
- 56.Pellegrini G, Rama P, Mavilio F, De Luca M. Epithelial stem cells in corneal regeneration and epidermal gene therapy. J Pathol. 2009;217:217–228. doi: 10.1002/path.2441. [DOI] [PubMed] [Google Scholar]
- 57.Kwitko S, Marinho D, Barcaro S, Bocaccio F, Rymer S, Fernandes S, Neumann J. Allograft conjunctival transplantation for bilateral ocular surface disorders. Ophthalmology. 1995;102:1020–1025. doi: 10.1016/s0161-6420(95)30918-9. [DOI] [PubMed] [Google Scholar]
- 58.Croasdale CR, Schwartz GS, Malling JV, Holland EJ. Keratolimbal allograft: recommendations for tissue procurement and preparation by eye banks, and standard surgical technique. Cornea. 1999;18:52–58. doi: 10.1097/00003226-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 59.Tsai RJ, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med. 2000;343:86–93. doi: 10.1056/NEJM200007133430202. [DOI] [PubMed] [Google Scholar]
- 60.Sangwan VS, Basu S, MacNeil S, Balasubramanian D. Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br J Ophthalmol. 2012;96:931–934. doi: 10.1136/bjophthalmol-2011-301164. [DOI] [PubMed] [Google Scholar]
- 61.Kushnerev E, Shawcross SG, Sothirachagan S, Carley F, Brahma A, Yates JM, Hillarby MC. Regeneration of Corneal Epithelium With Dental Pulp Stem Cells Using a Contact Lens Delivery System. Invest Ophthalmol Vis Sci. 2016;57:5192–5199. doi: 10.1167/iovs.15-17953. [DOI] [PubMed] [Google Scholar]
- 62.Huang SU, Yoon JJ, Ismail S, McGhee JJ, Sherwin T. Sphere-forming cells from peripheral cornea demonstrate a wound-healing response to injury. Cell Biol Int. 2015;39:1274–1287. doi: 10.1002/cbin.10501. [DOI] [PubMed] [Google Scholar]
- 63.Yin J, Jurkunas U. Limbal Stem Cell Transplantation and Complications. Semin Ophthalmol. 2018;33:134–141. doi: 10.1080/08820538.2017.1353834. [DOI] [PubMed] [Google Scholar]
- 64.Shalom-Feuerstein R, Serror L, De La Forest Divonne S, Petit I, Aberdam E, Camargo L, Damour O, Vigouroux C, Solomon A, Gaggioli C, Itskovitz-Eldor J, Ahmad S, Aberdam D. Pluripotent stem cell model reveals essential roles for miR-450b-5p and miR-184 in embryonic corneal lineage specification. Stem Cells. 2012;30:898–909. doi: 10.1002/stem.1068. [DOI] [PubMed] [Google Scholar]
- 65.Erbani J, Aberdam D, Larghero J, Vanneaux V. Pluripotent Stem Cells and Other Innovative Strategies for the Treatment of Ocular Surface Diseases. Stem Cell Rev Rep. 2016;12:171–178. doi: 10.1007/s12015-016-9643-y. [DOI] [PubMed] [Google Scholar]
- 66.Chan AA, Hertsenberg AJ, Funderburgh ML, Mann MM, Du Y, Davoli KA, Mich-Basso JD, Yang L, Funderburgh JL. Differentiation of human embryonic stem cells into cells with corneal keratocyte phenotype. PLoS One. 2013;8:e56831. doi: 10.1371/journal.pone.0056831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Susaimanickam PJ, Maddileti S, Pulimamidi VK, Boyinpally SR, Naik RR, Naik MN, Reddy GB, Sangwan VS, Mariappan I. Generating minicorneal organoids from human induced pluripotent stem cells. Development. 2017;144:2338–2351. doi: 10.1242/dev.143040. [DOI] [PubMed] [Google Scholar]
- 68.Reinshagen H, Auw-Haedrich C, Sorg RV, Boehringer D, Eberwein P, Schwartzkopff J, Sundmacher R, Reinhard T. Corneal surface reconstruction using adult mesenchymal stem cells in experimental limbal stem cell deficiency in rabbits. Acta Ophthalmol. 2011;89:741–748. doi: 10.1111/j.1755-3768.2009.01812.x. [DOI] [PubMed] [Google Scholar]
- 69.Calonge M, Pérez I, Galindo S, Nieto-Miguel T, López-Paniagua M, Fernández I, Alberca M, García-Sancho J, Sánchez A, Herreras JM. A proof-of-concept clinical trial using mesenchymal stem cells for the treatment of corneal epithelial stem cell deficiency. Transl Res. 2019;206:18–40. doi: 10.1016/j.trsl.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 70.Gu S, Xing C, Han J, Tso MO, Hong J. Differentiation of rabbit bone marrow mesenchymal stem cells into corneal epithelial cells in vivo and ex vivo. Mol Vis. 2009;15:99–107. [PMC free article] [PubMed] [Google Scholar]
- 71.Oh JY, Kim MK, Shin MS, Lee HJ, Ko JH, Wee WR, Lee JH. The anti-inflammatory and anti-angiogenic role of mesenchymal stem cells in corneal wound healing following chemical injury. Stem Cells. 2008;26:1047–1055. doi: 10.1634/stemcells.2007-0737. [DOI] [PubMed] [Google Scholar]
- 72.De Miguel MP, Fuentes-Julián S, Blázquez-Martínez A, Pascual CY, Aller MA, Arias J, Arnalich-Montiel F. Immunosuppressive properties of mesenchymal stem cells: advances and applications. Curr Mol Med. 2012;12:574–591. doi: 10.2174/156652412800619950. [DOI] [PubMed] [Google Scholar]
- 73.Reza HM, Ng BY, Gimeno FL, Phan TT, Ang LP. Umbilical cord lining stem cells as a novel and promising source for ocular surface regeneration. Stem Cell Rev Rep. 2011;7:935–947. doi: 10.1007/s12015-011-9245-7. [DOI] [PubMed] [Google Scholar]
- 74.Garzón I, Martín-Piedra MA, Alfonso-Rodríguez C, González-Andrades M, Carriel V, Martínez-Gómez C, Campos A, Alaminos M. Generation of a biomimetic human artificial cornea model using Wharton's jelly mesenchymal stem cells. Invest Ophthalmol Vis Sci. 2014;55:4073–4083. doi: 10.1167/iovs.14-14304. [DOI] [PubMed] [Google Scholar]
- 75.Hassan NT, AbdelAziz NA. Oral Mucosal Stem Cells, Human Immature Dental Pulp Stem Cells and Hair Follicle Bulge Stem Cells as Adult Stem Cells Able to Correct Limbal Stem Cell Deficiency. Curr Stem Cell Res Ther. 2018;13:356–361. doi: 10.2174/1574888X13666180223124936. [DOI] [PubMed] [Google Scholar]
- 76.Nishida K, Yamato M, Hayashida Y, Watanabe K, Yamamoto K, Adachi E, Nagai S, Kikuchi A, Maeda N, Watanabe H, Okano T, Tano Y. Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. N Engl J Med. 2004;351:1187–1196. doi: 10.1056/NEJMoa040455. [DOI] [PubMed] [Google Scholar]
- 77.Bobba S, Di Girolamo N. Contact Lenses: A Delivery Device for Stem Cells to Treat Corneal Blindness. Optom Vis Sci. 2016;93:412–418. doi: 10.1097/OPX.0000000000000699. [DOI] [PubMed] [Google Scholar]
- 78.West-Mays JA, Dwivedi DJ. The keratocyte: corneal stromal cell with variable repair phenotypes. Int J Biochem Cell Biol. 2006;38:1625–1631. doi: 10.1016/j.biocel.2006.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sepsakos L, Cheung AY, Holland EJ. Outcomes of Keratoplasty After Ocular Surface Stem Cell Transplantation. Cornea. 2017;36:1025–1030. doi: 10.1097/ICO.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 80.Joseph R, Srivastava OP, Pfister RR. Modeling Keratoconus Using Induced Pluripotent Stem Cells. Invest Ophthalmol Vis Sci. 2016;57:3685–3697. doi: 10.1167/iovs.16-19105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Naylor RW, McGhee CN, Cowan CA, Davidson AJ, Holm TM, Sherwin T. Derivation of Corneal Keratocyte-Like Cells from Human Induced Pluripotent Stem Cells. PLoS One. 2016;11:e0165464. doi: 10.1371/journal.pone.0165464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Yam GH, Fuest M, Yusoff NZBM, Goh TW, Bandeira F, Setiawan M, Seah XY, Lwin NC, Stanzel TP, Ong HS, Mehta JS. Safety and Feasibility of Intrastromal Injection of Cultivated Human Corneal Stromal Keratocytes as Cell-Based Therapy for Corneal Opacities. Invest Ophthalmol Vis Sci. 2018;59:3340–3354. doi: 10.1167/iovs.17-23575. [DOI] [PubMed] [Google Scholar]
- 83.Mittal SK, Omoto M, Amouzegar A, Sahu A, Rezazadeh A, Katikireddy KR, Shah DI, Sahu SK, Chauhan SK. Restoration of Corneal Transparency by Mesenchymal Stem Cells. Stem Cell Reports. 2016;7:583–590. doi: 10.1016/j.stemcr.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Alió Del Barrio JLA, El Zarif M, de Miguel MP, Azaar A, Makdissy N, Harb W, El Achkar I, Arnalich-Montiel F, Alió JL. Cellular Therapy With Human Autologous Adipose-Derived Adult Stem Cells for Advanced Keratoconus. Cornea. 2017;36:952–960. doi: 10.1097/ICO.0000000000001228. [DOI] [PubMed] [Google Scholar]
- 85.Coulson-Thomas VJ, Caterson B, Kao WW. Transplantation of human umbilical mesenchymal stem cells cures the corneal defects of mucopolysaccharidosis VII mice. Stem Cells. 2013;31:2116–2126. doi: 10.1002/stem.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Liu H, Zhang J, Liu CY, Wang IJ, Sieber M, Chang J, Jester JV, Kao WW. Cell therapy of congenital corneal diseases with umbilical mesenchymal stem cells: lumican null mice. PLoS One. 2010;5:e10707. doi: 10.1371/journal.pone.0010707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Funderburgh JL, Funderburgh ML, Du Y. Stem Cells in the Limbal Stroma. Ocul Surf. 2016;14:113–120. doi: 10.1016/j.jtos.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yam GH, Teo EP, Setiawan M, Lovatt MJ, Yusoff NZBM, Fuest M, Goh BT, Mehta JS. Postnatal periodontal ligament as a novel adult stem cell source for regenerative corneal cell therapy. J Cell Mol Med. 2018;22:3119–3132. doi: 10.1111/jcmm.13589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Joyce NC, Harris DL, Markov V, Zhang Z, Saitta B. Potential of human umbilical cord blood mesenchymal stem cells to heal damaged corneal endothelium. Mol Vis. 2012;18:547–564. [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu W, Godwin CR, Cheng L, Scheetz TE, Kuehn MH. Transplantation of iPSC-TM stimulates division of trabecular meshwork cells in human eyes. Sci Rep. 2020;10:2905. doi: 10.1038/s41598-020-59941-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chamling X, Sluch VM, Zack DJ. The Potential of Human Stem Cells for the Study and Treatment of Glaucoma. Invest Ophthalmol Vis Sci. 2016;57:ORSFi1–ORSFi6. doi: 10.1167/iovs.15-18590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ding QJ, Zhu W, Cook AC, Anfinson KR, Tucker BA, Kuehn MH. Induction of trabecular meshwork cells from induced pluripotent stem cells. Invest Ophthalmol Vis Sci. 2014;55:7065–7072. doi: 10.1167/iovs.14-14800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Abu-Hassan DW, Li X, Ryan EI, Acott TS, Kelley MJ. Induced pluripotent stem cells restore function in a human cell loss model of open-angle glaucoma. Stem Cells. 2015;33:751–761. doi: 10.1002/stem.1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pearson C, Martin K. Stem cell approaches to glaucoma: from aqueous outflow modulation to retinal neuroprotection. Prog Brain Res. 2015;220:241–256. doi: 10.1016/bs.pbr.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 95.Manuguerra-Gagné R, Boulos PR, Ammar A, Leblond FA, Krosl G, Pichette V, Lesk MR, Roy DC. Transplantation of mesenchymal stem cells promotes tissue regeneration in a glaucoma model through laser-induced paracrine factor secretion and progenitor cell recruitment. Stem Cells. 2013;31:1136–1148. doi: 10.1002/stem.1364. [DOI] [PubMed] [Google Scholar]
- 96.Lin H, Ouyang H, Zhu J, Huang S, Liu Z, Chen S, Cao G, Li G, Signer RA, Xu Y, Chung C, Zhang Y, Lin D, Patel S, Wu F, Cai H, Hou J, Wen C, Jafari M, Liu X, Luo L, Qiu A, Hou R, Chen B, Chen J, Granet D, Heichel C, Shang F, Li X, Krawczyk M, Skowronska-Krawczyk D, Wang Y, Shi W, Chen D, Zhong Z, Zhong S, Zhang L, Morrison SJ, Maas RL, Zhang K, Liu Y. Lens regeneration using endogenous stem cells with gain of visual function. Nature. 2016;531:323–328. doi: 10.1038/nature17181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu Z, Wang R, Lin H, Liu Y. Lens regeneration in humans: using regenerative potential for tissue repairing. Ann Transl Med. 2020;8:1544. doi: 10.21037/atm-2019-rcs-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Murphy P, Kabir MH, Srivastava T, Mason ME, Dewi CU, Lim S, Yang A, Djordjevic D, Killingsworth MC, Ho JWK, Harman DG, O'Connor MD. Light-focusing human micro-lenses generated from pluripotent stem cells model lens development and drug-induced cataract in vitro. Development. 2018;145 doi: 10.1242/dev.155838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Li HJ, Sun ZL, Yang XT, Zhu L, Feng DF. Exploring Optic Nerve Axon Regeneration. Curr Neuropharmacol. 2017;15:861–873. doi: 10.2174/1570159X14666161227150250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gokoffski KK, Lam P, Alas BF, Peng MG, Ansorge HRR. Optic Nerve Regeneration: How Will We Get There? J Neuroophthalmol. 2020;40:234–242. doi: 10.1097/WNO.0000000000000953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rabesandratana O, Goureau O, Orieux G. Pluripotent Stem Cell-Based Approaches to Explore and Treat Optic Neuropathies. Front Neurosci. 2018;12:651. doi: 10.3389/fnins.2018.00651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuwahara A, Ozone C, Nakano T, Saito K, Eiraku M, Sasai Y. Generation of a ciliary margin-like stem cell niche from self-organizing human retinal tissue. Nat Commun. 2015;6:6286. doi: 10.1038/ncomms7286. [DOI] [PubMed] [Google Scholar]
- 103.Laha B, Stafford BK, Huberman AD. Regenerating optic pathways from the eye to the brain. Science. 2017;356:1031–1034. doi: 10.1126/science.aal5060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wu S, Chang KC, Nahmou M, Goldberg JL. Induced Pluripotent Stem Cells Promote Retinal Ganglion Cell Survival After Transplant. Invest Ophthalmol Vis Sci. 2018;59:1571–1576. doi: 10.1167/iovs.17-23648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mesentier-Louro LA, Rosso P, Carito V, Mendez-Otero R, Santiago MF, Rama P, Lambiase A, Tirassa P. Nerve Growth Factor Role on Retinal Ganglion Cell Survival and Axon Regrowth: Effects of Ocular Administration in Experimental Model of Optic Nerve Injury. Mol Neurobiol. 2019;56:1056–1069. doi: 10.1007/s12035-018-1154-1. [DOI] [PubMed] [Google Scholar]
- 106.Zhang WM Md, Zhang ZR Md, Zhang YG Md, Gao YS Md. Neural Stem Cell-based Intraocular Administration of Pigment Epithelium-derived Factor Promotes Retinal Ganglion Cell Survival and Axon Regeneration after Optic Nerve Crush Injury in Rat: An Experimental Study. Iran J Med Sci. 2016;41:382–390. [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang ZJ, Li YJ, Liu XG, Huang FX, Liu TJ, Jiang DM, Lv XM, Luo M. Human umbilical cord blood stem cells and brain-derived neurotrophic factor for optic nerve injury: a biomechanical evaluation. Neural Regen Res. 2015;10:1134–1138. doi: 10.4103/1673-5374.160110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Binder S, Stanzel BV, Krebs I, Glittenberg C. Transplantation of the RPE in AMD. Prog Retin Eye Res. 2007;26:516–554. doi: 10.1016/j.preteyeres.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 109.van Meurs JC, ter Averst E, Hofland LJ, van Hagen PM, Mooy CM, Baarsma GS, Kuijpers RW, Boks T, Stalmans P. Autologous peripheral retinal pigment epithelium translocation in patients with subfoveal neovascular membranes. Br J Ophthalmol. 2004;88:110–113. doi: 10.1136/bjo.88.1.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tucker BA, Park IH, Qi SD, Klassen HJ, Jiang C, Yao J, Redenti S, Daley GQ, Young MJ. Transplantation of adult mouse iPS cell-derived photoreceptor precursors restores retinal structure and function in degenerative mice. PLoS One. 2011;6:e18992. doi: 10.1371/journal.pone.0018992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lamba DA, Karl MO, Ware CB, Reh TA. Efficient generation of retinal progenitor cells from human embryonic stem cells. Proc Natl Acad Sci USA. 2006;103:12769–12774. doi: 10.1073/pnas.0601990103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Osakada F, Jin ZB, Hirami Y, Ikeda H, Danjyo T, Watanabe K, Sasai Y, Takahashi M. In vitro differentiation of retinal cells from human pluripotent stem cells by small-molecule induction. J Cell Sci. 2009;122:3169–3179. doi: 10.1242/jcs.050393. [DOI] [PubMed] [Google Scholar]
- 113.Gonzalez-Cordero A, West EL, Pearson RA, Duran Y, Carvalho LS, Chu CJ, Naeem A, Blackford SJI, Georgiadis A, Lakowski J, Hubank M, Smith AJ, Bainbridge JWB, Sowden JC, Ali RR. Photoreceptor precursors derived from three-dimensional embryonic stem cell cultures integrate and mature within adult degenerate retina. Nat Biotechnol. 2013;31:741–747. doi: 10.1038/nbt.2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Schwartz SD, Hubschman JP, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, Mickunas E, Gay R, Klimanskaya I, Lanza R. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 2012;379:713–720. doi: 10.1016/S0140-6736(12)60028-2. [DOI] [PubMed] [Google Scholar]
- 115.Sugino IK, Sun Q, Springer C, Cheewatrakoolpong N, Liu T, Li H, Zarbin MA. Two Bioactive Molecular Weight Fractions of a Conditioned Medium Enhance RPE Cell Survival on Age-Related Macular Degeneration and Aged Bruch's Membrane. Transl Vis Sci Technol. 2016;5:8. doi: 10.1167/tvst.5.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hirano M, Yamamoto A, Yoshimura N, Tokunaga T, Motohashi T, Ishizaki K, Yoshida H, Okazaki K, Yamazaki H, Hayashi S, Kunisada T. Generation of structures formed by lens and retinal cells differentiating from embryonic stem cells. Dev Dyn. 2003;228:664–671. doi: 10.1002/dvdy.10425. [DOI] [PubMed] [Google Scholar]
- 117.Lakowski J, Welby E, Budinger D, Di Marco F, Di Foggia V, Bainbridge JWB, Wallace K, Gamm DM, Ali RR, Sowden JC. Isolation of Human Photoreceptor Precursors via a Cell Surface Marker Panel from Stem Cell-Derived Retinal Organoids and Fetal Retinae. Stem Cells. 2018;36:709–722. doi: 10.1002/stem.2775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Tzameret A, Sher I, Belkin M, Treves AJ, Meir A, Nagler A, Levkovitch-Verbin H, Barshack I, Rosner M, Rotenstreich Y. Transplantation of human bone marrow mesenchymal stem cells as a thin subretinal layer ameliorates retinal degeneration in a rat model of retinal dystrophy. Exp Eye Res. 2014;118:135–144. doi: 10.1016/j.exer.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 119.Mead B, Logan A, Berry M, Leadbeater W, Scheven BA. Paracrine-mediated neuroprotection and neuritogenesis of axotomised retinal ganglion cells by human dental pulp stem cells: comparison with human bone marrow and adipose-derived mesenchymal stem cells. PLoS One. 2014;9:e109305. doi: 10.1371/journal.pone.0109305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gaddam S, Periasamy R, Gangaraju R. Adult Stem Cell Therapeutics in Diabetic Retinopathy. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20194876. [DOI] [PMC free article] [PubMed] [Google Scholar]